Aflibercept versus Faricimab in the Treatment of Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema: A Review
Abstract
:1. Introduction
2. nAMD and DME as Global Health Care Problems
3. Pathogenesis of nAMD and DME
3.1. nAMD
3.2. DME
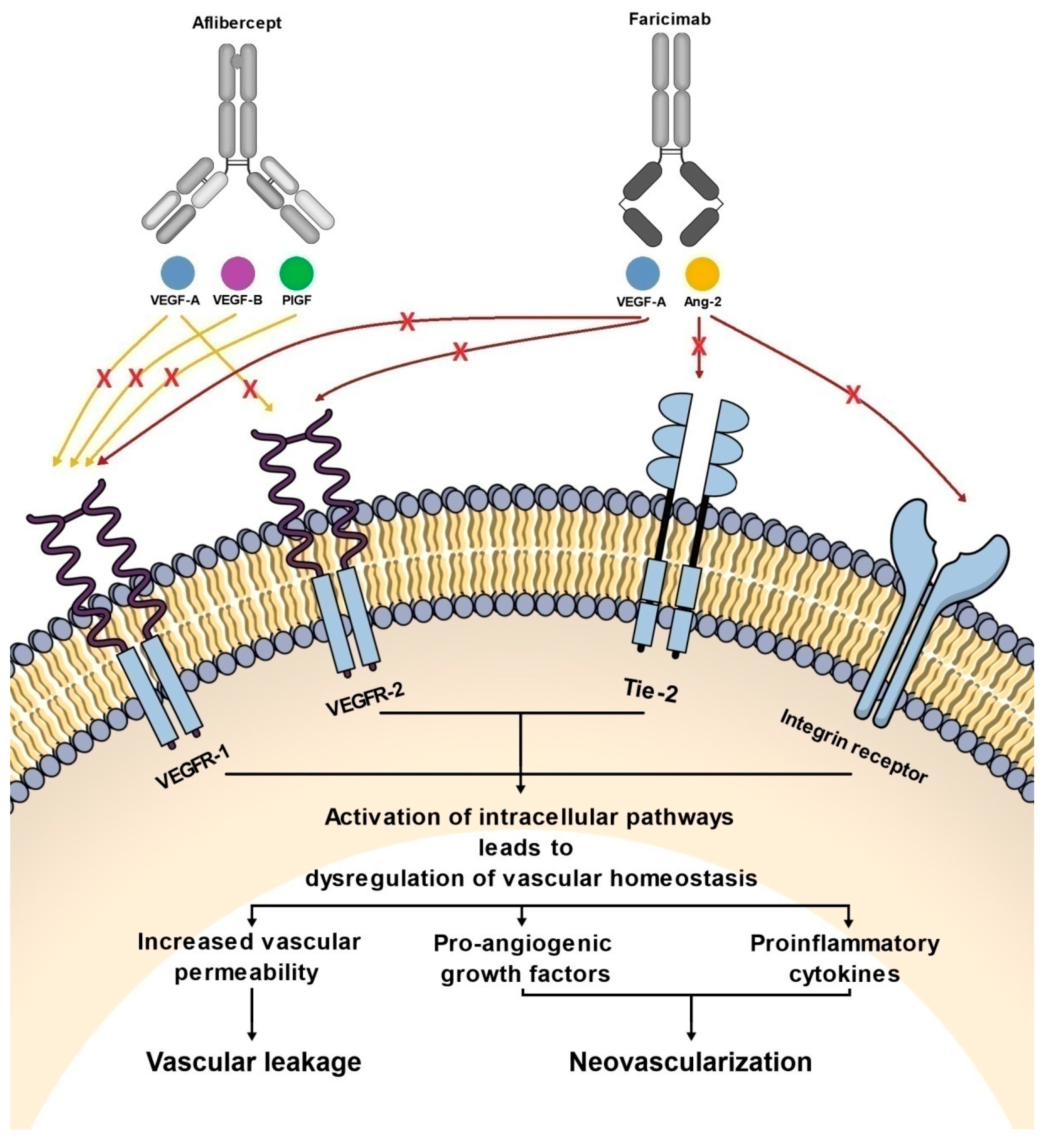
4. The Role of the VEGF and Ang-Tie Pathways in the Pathogenesis of DME and nAMD
4.1. VEGF Pathway
4.2. Ang/Tie Pathway
5. Aflibercept and Faricimab: Molecular Characteristics
6. Summary of Preclinical Studies of Aflibercept and Faricimab
6.1. Preclinical Studies of Aflibercept
6.2. Preclinical Studies of Faricimab
7. Clinical Trials of Aflibercept and Faricimab
7.1. Clinical Trials of Aflibercept
7.1.1. Phase I Trials for nAMD: CLEAR-AMD I and CLEAR-IT I
7.1.2. Phase I Trial for DME
7.1.3. Phase II Trial for nAMD: CLEAR-IT-2
7.1.4. Phase II Trial for DME: DA VINCI Study
7.1.5. Phase III Trials for nAMD: VIEW 1 and VIEW 2
7.1.6. Phase III Trials for DME: VIVID and VISTA
7.2. Clinical Trials of Faricimab
7.2.1. Phase I Clinical Trial
7.2.2. Phase II Clinical Trials for nAMD: AVENUE and STAIRWAY
7.2.3. Phase II Clinical Trial for DME: BOULEVARD
7.2.4. Phase III Clinical Trials for nAMD: TENAYA and LUCERNE
7.2.5. Phase III Clinical Trials for DME: YOSEMITE and RHINE
8. Summary of Pre-Clinical and Clinical Trials of Aflibercept and Faricimab
9. Advances in the Treatment of nAMD and DME
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jaki Mekjavić, P.; Jūratė Balčiūnienė, V.; Ćeklić, L.; Ernest, J.; Jamrichova, Z.; Zsolt Nagy, Z.; Petkova, I.; Teper, S.; Gardašević Topčić, I.; Veith, M. The Burden of Macular Diseases in Central and Eastern Europe-Implications for Healthcare Systems. Value Health Reg. Issues 2019, 19, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Nicolò, M.; Ferro Desideri, L.; Vagge, A.; Traverso, C.E. Faricimab: An investigational agent targeting the Tie-2/angiopoietin pathway and VEGF-A for the treatment of retinal diseases. Expert Opin. Investig. Drugs 2021, 30, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Regula, J.T.; Lundh von Leithner, P.; Foxton, R.; Barathi, V.A.; Cheung, C.M.; Bo Tun, S.B.; Wey, Y.S.; Iwata, D.; Dostalek, M.; Moelleken, J.; et al. Targeting key angiogenic pathways with a bispecific CrossMAb optimized for neovascular eye diseases. EMBO Mol. Med. 2016, 8, 1265–1288. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Zhao, L.; Li, Y.; Liu, Y.; Xiao, W.; Song, Y.; Luo, L.; Huang, D.; Yancopoulos, G.D.; Wiegand, S.J.; et al. A subretinal matrigel rat choroidal neovascularization (CNV) model and inhibition of CNV and associated inflammation and fibrosis by VEGF trap. Investig. Ophthalmol. Vis. Sci. 2010, 51, 6009–6017. [Google Scholar] [CrossRef]
- Daien, V.; Eldem, B.M.; Talks, J.S.; Korobelnik, J.F.; Mitchell, P.; Finger, R.P.; Sakamoto, T.; Wong, T.Y.; Evuarherhe, O.; Carter, G.; et al. Real-world data in retinal diseases treated with anti-vascular endothelial growth factor (anti-VEGF) therapy—A systematic approach to identify and characterize data sources. BMC Ophthalmol. 2019, 19, 206. [Google Scholar] [CrossRef]
- Chopra, R.; Preston, G.C.; Keenan, T.; Mulholland, P.; Patel, P.J.; Balaskas, K.; Hamilton, R.D.; Keane, P.A. Intravitreal injections: Past trends and future projections within a UK tertiary hospital. Eye 2022, 36, 1373–1378. [Google Scholar] [CrossRef]
- Ohr, M.; Kaiser, P.K. Aflibercept in wet age-related macular degeneration: A perspective review. Ther. Adv. Chronic Dis. 2012, 3, 153–161. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Bandello, F.; Loewenstein, A. Faricimab: Expanding horizon beyond VEGF. Eye 2020, 34, 802–804. [Google Scholar] [CrossRef]
- Khanani, A.M.; Guymer, R.H.; Basu, K.; Boston, H.; Heier, J.S.; Korobelnik, J.F.; Quezada-Ruiz, C. TENAYA and LUCERNE: Rationale and design for the phase 3 clinical trials of faricimab for neovascular age-related macular degeneration. Ophthalmol. Sci. 2021, 1, 100076. [Google Scholar] [CrossRef]
- Ng, D.S.; Yip, Y.W.; Bakthavatsalam, M.; Chen, L.J.; Ng, T.K.; Lai, T.Y.; Pang, C.P.; Brelén, M.E. Elevated angiopoietin 2 in aqueous of patients with neovascular age related macular degeneration correlates with disease severity at presentation. Sci. Rep. 2017, 7, 45081. [Google Scholar] [CrossRef] [Green Version]
- Semeraro, F.; Morescalchi, F.; Duse, S.; Parmeggiani, F.; Gambicorti, E.; Costagliola, C. Aflibercept in wet AMD: Specific role and optimal use. Drug Des. Devel. Ther. 2013, 7, 711–722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spooner, K.L.; Guinan, G.; Koller, S.; Hong, T.; Chang, A.A. Burden Of Treatment Among Patients Undergoing Intravitreal Injections For Diabetic Macular Oedema In Australia. Diabetes Metab. Syndr. Obes. 2019, 12, 1913–1921. [Google Scholar] [CrossRef] [Green Version]
- Hussain, R.M.; Neiweem, A.E.; Kansara, V.; Harris, A.; Ciulla, T.A. Tie-2/Angiopoietin pathway modulation as a therapeutic strategy for retinal disease. Expert Opin. Investig. Drugs 2019, 28, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Heier, J.S.; Do, D.V.; Mirando, A.C.; Pandey, N.B.; Sheng, H.; Heah, T. The Tie2 signaling pathway in retinal vascular diseases: A novel therapeutic target in the eye. Int. J. Retin. Vitr. 2020, 6, 48. [Google Scholar] [CrossRef] [PubMed]
- Sahni, J.; Patel, S.S.; Dugel, P.U.; Khanani, A.M.; Jhaveri, C.D.; Wykoff, C.C.; Hershberger, V.S.; Pauly-Evers, M.; Sadikhov, S.; Szczesny, P.; et al. Simultaneous Inhibition of Angiopoietin-2 and Vascular Endothelial Growth Factor-A with Faricimab in Diabetic Macular Edema: BOULEVARD Phase 2 Randomized Trial. Ophthalmology 2019, 126, 1155–1170. [Google Scholar] [CrossRef] [Green Version]
- Heier, J.S.; Khanani, A.M.; Quezada Ruiz, C.; Basu, K.; Ferrone, P.J.; Brittain, C.; Figueroa, M.S.; Lin, H.; Holz, F.G.; Patel, V.; et al. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): Two randomised, double-masked, phase 3, non-inferiority trials. Lancet 2022, 399, 729–740. [Google Scholar] [CrossRef]
- Wykoff, C.C.; Abreu, F.; Adamis, A.P.; Basu, K.; Eichenbaum, D.A.; Haskova, Z.; Lin, H.; Loewenstein, A.; Mohan, S.; Pearce, I.A.; et al. Efficacy, durability, and safety of intravitreal faricimab with extended dosing up to every 16 weeks in patients with diabetic macular oedema (YOSEMITE and RHINE): Two randomised, double-masked, phase 3 trials. Lancet 2022, 399, 741–755. [Google Scholar] [CrossRef]
- Wykoff, C.C.; Campochiaro, P.A.; Pieramici, D.J.; Khanani, A.M.; Gune, S.; Maia, M.; Kågedal, M.; Ding, H.T.; Maass, K.F. Pharmacokinetics of the Port Delivery System with Ranibizumab in the Ladder Phase 2 Trial for Neovascular Age-Related Macular Degeneration. Ophthalmol. Ther. 2022, 1–13. [Google Scholar] [CrossRef]
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.; Klein, R.; Cheng, C.Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. 2014, 2, e106–e116. [Google Scholar] [CrossRef] [Green Version]
- Al Gwairi, O.; Thach, L.; Zheng, W.; Osman, N.; Little, P.J. Cellular and Molecular Pathology of Age-Related Macular Degeneration: Potential Role for Proteoglycans. J. Ophthalmol. 2016, 2016, 2913612. [Google Scholar] [CrossRef] [Green Version]
- Flores, R.; Carneiro, Â.; Vieira, M.; Tenreiro, S.; Seabra, M.C. Age-Related Macular Degeneration: Pathophysiology, Management, and Future Perspectives. Ophthalmologica 2021, 244, 495–511. [Google Scholar] [CrossRef] [PubMed]
- Iglicki, M.; González, D.P.; Loewenstein, A.; Zur, D. Next-generation anti-VEGF agents for diabetic macular oedema. Eye 2022, 36, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Kuroiwa, D.; Malerbi, F.K.; Regatieri, C. New Insights in Resistant Diabetic Macular Edema. Ophthalmologica 2021, 244, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Korobelnik, J.F.; Brown, D.M.; Schmidt-Erfurth, U.; Do, D.V.; Midena, E.; Boyer, D.S.; Terasaki, H.; Kaiser, P.K.; Marcus, D.M.; et al. Intravitreal Aflibercept for Diabetic Macular Edema: 148-Week Results from the VISTA and VIVID Studies. Ophthalmology 2016, 123, 2376–2385. [Google Scholar] [CrossRef]
- Chawla, A.; Chawla, R.; Jaggi, S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J. Endocrinol. Metab. 2016, 20, 546–551. [Google Scholar] [CrossRef]
- Wang, W.; Lo, A.C.Y. Diabetic Retinopathy: Pathophysiology and Treatments. Int. J. Mol. Sci. 2018, 19, 1816. [Google Scholar] [CrossRef] [Green Version]
- Yun, J.H.; Park, S.W.; Kim, J.H.; Park, Y.J.; Cho, C.H.; Kim, J.H. Angiopoietin 2 induces astrocyte apoptosis via αvβ5-integrin signaling in diabetic retinopathy. Cell Death Dis. 2016, 7, e2101. [Google Scholar] [CrossRef] [Green Version]
- Browning, D.J.; Stewart, M.W.; Lee, C. Diabetic macular edema: Evidence-based management. Indian J. Ophthalmol. 2018, 66, 1736–1750. [Google Scholar] [CrossRef]
- Do, D.V.; Schmidt-Erfurth, U.; Gonzalez, V.H.; Gordon, C.M.; Tolentino, M.; Berliner, A.J.; Vitti, R.; Rückert, R.; Sandbrink, R.; Stein, D.; et al. The DA VINCI Study: Phase 2 primary results of VEGF Trap-Eye in patients with diabetic macular edema. Ophthalmology 2011, 118, 1819–1826. [Google Scholar] [CrossRef]
- Kozak, I.; Gurbaxani, A.; Safar, A.; Rao, P.; Masalmeh, A.; Assaf, H.; Farghaly, M.; Pathak, P.; Natarajan, A.; Saffar, I. Treatment patterns in patients with age-related macular degeneration and diabetic macular edema: A real-world claims analysis in Dubai. PLoS ONE 2021, 16, e0254569. [Google Scholar] [CrossRef]
- Do, D.V.; Nguyen, Q.D.; Boyer, D.; Schmidt-Erfurth, U.; Brown, D.M.; Vitti, R.; Berliner, A.J.; Gao, B.; Zeitz, O.; Ruckert, R.; et al. One-year outcomes of the da Vinci Study of VEGF Trap-Eye in eyes with diabetic macular edema. Ophthalmology 2012, 119, 1658–1665. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.; Knudtson, M.D.; Lee, K.E.; Gangnon, R.; Klein, B.E. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XXII the twenty-five-year progression of retinopathy in persons with type 1 diabetes. Ophthalmology 2018, 115, 1859–1868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.; Aziz, A.A.; Shafi, N.A.; Abbas, T.; Khanani, A.M. Targeting Angiopoietin in Retinal Vascular Diseases: A Literature Review and Summary of Clinical Trials Involving Faricimab. Cells 2020, 9, 1869. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Kaiser, P.K. Intravitreal aflibercept for neovascular age-related macular degeneration. Immunotherapy 2013, 5, 121–130. [Google Scholar] [CrossRef]
- Korobelnik, J.F.; Do, D.V.; Schmidt-Erfurth, U.; Boyer, D.S.; Holz, F.G.; Heier, J.S.; Midena, E.; Kaiser, P.K.; Terasaki, H.; Marcus, D.M.; et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology 2014, 121, 2247–2254. [Google Scholar] [CrossRef]
- Chen, J.H.; Lin, X.; Bu, C.; Zhang, X. Role of advanced glycation end products in mobility and considerations in possible dietary and nutritional intervention strategies. Nutr. Metab. 2018, 15, 72. [Google Scholar] [CrossRef]
- Park, S.W.; Yun, J.H.; Kim, J.H.; Kim, K.W.; Cho, C.H.; Kim, J.H. Angiopoietin 2 induces pericyte apoptosis via α3β1 integrin signaling in diabetic retinopathy. Diabetes 2014, 63, 3057–3068. [Google Scholar] [CrossRef] [Green Version]
- Beltramo, E.; Porta, M. Pericyte loss in diabetic retinopathy: Mechanisms and consequences. Curr. Med. Chem. 2013, 20, 3218–3225. [Google Scholar] [CrossRef] [Green Version]
- Chang, M.L.; Wu, C.H.; Jiang-Shieh, Y.F.; Shieh, J.Y.; Wen, C.Y. Reactive changes of retinal astrocytes and Müller glial cells in kainate-induced neuroexcitotoxicity. J. Anat. 2007, 210, 54–65. [Google Scholar] [CrossRef]
- Doganay, S.; Evereklioglu, C.; Er, H.; Türköz, Y.; Sevinç, A.; Mehmet, N.; Savli, H. Comparison of serum NO, TNF-alpha, IL-1beta, sIL-2R, IL-6 and IL-8 levels with grades of retinopathy in patients with diabetes mellitus. Eye 2002, 16, 163–170. [Google Scholar] [CrossRef]
- Koleva-Georgieva, D.N.; Sivkova, N.P.; Terzieva, D. Serum inflammatory cytokines IL-1beta, IL-6, TNF-alpha and VEGF have influence on the development of diabetic retinopathy. Folia. Med. 2011, 53, 44–50. [Google Scholar]
- Boss, J.D.; Singh, P.K.; Pandya, H.K.; Tosi, J.; Kim, C.; Tewari, A.; Juzych, M.S.; Abrams, G.W.; Kumar, A. Assessment of neurotrophins and inflammatory mediators in vitreous of patients with diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2017, 58, 5594–5603. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Kim, S.; Egashira, K.; Takeya, M.; Ikeda, T.; Mimura, O.; Iwao, H. Molecular mechanism and role of endothelial monocyte chemoattractant protein-1 induction by vascular endothelial growth factor. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 1996–2001. [Google Scholar] [CrossRef] [Green Version]
- Shibuya, M. Vascular Endothelial Growth Factor (VEGF) and Its Receptor (VEGFR) Signaling in Angiogenesis: A Crucial Target for Anti- and Pro-Angiogenic Therapies. Genes Cancer 2011, 2, 1097–1105. [Google Scholar] [CrossRef] [PubMed]
- Leppänen, V.M.; Saharinen, P.; Alitalo, K. Structural basis of Tie2 activation and Tie2/Tie1 heterodimerization. Proc. Natl. Acad. Sci. USA 2017, 114, 4376–4381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peach, C.J.; Mignone, V.W.; Arruda, M.A.; Alcobia, D.C.; Hill, S.J.; Kilpatrick, L.E.; Woolard, J. Molecular Pharmacology of VEGF-A Isoforms: Binding and Signalling at VEGFR2. Int. J. Mol. Sci. 2018, 19, 1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ford, K.M.; Saint-Geniez, M.; Walshe, T.; Zahr, A.; D’Amore, P.A. Expression and role of VEGF in the adult retinal pigment epithelium. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9478–9487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerhardinger, C.; Brown, L.F.; Roy, S.; Mizutani, M.; Zucker, C.L.; Lorenzi, M. Expression of vascular endothelial growth factor in the human retina and in nonproliferative diabetic retinopathy. Am. J. Pathol. 1998, 152, 1453–1462. [Google Scholar]
- Stewart, M.W. The clinical utility of aflibercept for diabetic macular edema. Diabetes Metab. Syndr. Obes. 2015, 8, 473–482. [Google Scholar] [CrossRef] [Green Version]
- Akiri, G.; Nahari, D.; Finkelstein, Y.; Le, S.Y.; Elroy-Stein, O.; Levi, B.Z. Regulation of vascular endothelial growth factor (VEGF) expression is mediated by internal initiation of translation and alternative initiation of transcription. Oncogene 1998, 17, 227–236. [Google Scholar] [CrossRef] [Green Version]
- Saint-Geniez, M.; Maharaj, A.S.; Walshe, T.E.; Tucker, B.A.; Sekiyama, E.; Kurihara, T.; Darland, D.C.; Young, M.J.; D’Amore, P.A. Endogenous VEGF is required for visual function: Evidence for a survival role on müller cells and photoreceptors. PLoS ONE 2008, 3, e3554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watanabe, D.; Suzuma, K.; Suzuma, I.; Ohashi, H.; Ojima, T.; Kurimoto, M.; Murakami, T.; Kimura, T.; Takagi, H. Vitreous levels of angiopoietin 2 and vascular endothelial growth factor in patients with proliferative diabetic retinopathy. Am. J. Ophthalmol. 2005, 139, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Corliss, B.A.; Azimi, M.S.; Munson, J.M.; Peirce, S.M.; Murfee, W.L. Macrophages: An Inflammatory Link Between Angiogenesis and Lymphangiogenesis. Microcirculation 2016, 23, 95–121. [Google Scholar] [CrossRef] [PubMed]
- Rakic, J.M.; Lambert, V.; Devy, L.; Luttun, A.; Carmeliet, P.; Claes, C.; Nguyen, L.; Foidart, J.M.; Noël, A.; Munaut, C. Placental growth factor, a member of the VEGF family, contributes to the development of choroidal neovascularization. Investig. Ophthalmol. Vis. Sci. 2003, 44, 3186–3193. [Google Scholar] [CrossRef] [Green Version]
- Kvanta, A.; Algvere, P.V.; Berglin, L.; Seregard, S. Subfoveal fibrovascular membranes in age-related macular degeneration express vascular endothelial growth factor. Investig. Ophthalmol. Vis. Sci. 1996, 37, 1929–1934. [Google Scholar] [CrossRef]
- Yi, X.; Ogata, N.; Komada, M.; Yamamoto, C.; Takahashi, K.; Omori, K.; Uyama, M. Vascular endothelial growth factor expression in choroidal neovascularization in rats. Graefes Arch. Clin. Exp. Ophthalmol. 1997, 235, 313–319. [Google Scholar] [CrossRef]
- Wada, M.; Ogata, N.; Otsuji, T.; Uyama, M. Expression of vascular endothelial growth factor and its receptor (KDR/flk-1) mRNA in experimental choroidal neovascularization. Curr. Eye Res. 1999, 18, 203–213. [Google Scholar] [CrossRef]
- Al Kahtani, E.; Xu, Z.; Al Rashaed, S.; Wu, L.; Mahale, A.; Tian, J.; Abboud, E.B.; Ghazi, N.G.; Kozak, I.; Gupta, V.; et al. Vitreous levels of placental growth factor correlate with activity of proliferative diabetic retinopathy and are not influenced by bevacizumab treatment. Eye 2017, 31, 529–536. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.; He, J.; Johnson, D.; Wei, Y.; Liu, Y.; Wang, S.; Lutty, G.A.; Duh, E.J.; Semba, R.D. Deletion of placental growth factor prevents diabetic retinopathy and is associated with Akt activation and HIF1α-VEGF pathway inhibition. Diabetes 2015, 64, 200–212. [Google Scholar] [CrossRef] [Green Version]
- Davis, S.; Aldrich, T.H.; Jones, P.F.; Acheson, A.; Compton, D.L.; Jain, V.; Ryan, T.E.; Bruno, J.; Radziejewski, C.; Maisonpierre, P.C.; et al. Isolation of angiopoietin-1, a ligand for the TIE2 receptor, by secretion-trap expression cloning. Cell 1996, 87, 1161–1169. [Google Scholar] [CrossRef] [Green Version]
- Swidzińska, E.; Naumnik, W.; Chyczewska, E. Angiogenesis and neoangiogenesis--the role in lung cancer and other tumors. Pneumonol. Alergol. Pol. 2006, 74, 414–420. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, N.; Parachuri, N.; Bandello, F.; Kuppermann, B.D.; Loewenstein, A. Faricimab: Two in the Bush Is Proving Better than One in the Hand? Ocul. Immunol. Inflamm. 2021, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Takagi, H.; Suzuma, K.; Otani, A.; Matsumura, M.; Honda, Y. Hypoxia and vascular endothelial growth factor selectively up-regulate angiopoietin-2 in bovine microvascular endothelial cells. J. Biol. Chem. 1999, 274, 15732–15739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandriota, S.J.; Pepper, M.S. Regulation of angiopoietin-2 mRNA levels in bovine microvascular endothelial cells by cytokines and hypoxia. Circ. Res. 1998, 83, 852–859. [Google Scholar] [CrossRef] [PubMed]
- Sahni, J.; Dugel, P.U.; Patel, S.S.; Chittum, M.E.; Berger, B.; Del Valle Rubido, M.; Sadikhov, S.; Szczesny, P.; Schwab, D.; Nogoceke, E.; et al. Safety and Efficacy of Different Doses and Regimens of Faricimab vs Ranibizumab in Neovascular Age-Related Macular Degeneration: The AVENUE Phase 2 Randomized Clinical Trial. JAMA Ophthalmol. 2020, 138, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Deering, T.; Oshima, S.; Nambu, H.; Reddy, P.S.; Kaleko, M.; Connelly, S.; Hackett, S.F.; Campochiaro, P.A. Angiopoietin-2 enhances retinal vessel sensitivity to vascular endothelial growth factor. J. Cell. Physiol. 2004, 199, 412–417. [Google Scholar] [CrossRef]
- Joussen, A.M.; Ricci, F.; Paris, L.P.; Korn, C.; Quezada-Ruiz, C.; Zarbin, M. Angiopoietin/Tie2 signalling and its role in retinal and choroidal vascular diseases: A review of preclinical data. Eye 2021, 35, 1305–1316. [Google Scholar] [CrossRef]
- Shirley, M. Faricimab: First Approval. Drugs 2022, 82, 825–830. [Google Scholar] [CrossRef]
- Surowka, M.; Schaefer, W.; Klein, C. Ten years in the making: Application of CrossMab technology for the development of therapeutic bispecific antibodies and antibody fusion proteins. mAbs 2021, 13, 1967714. [Google Scholar] [CrossRef]
- Jakubiak, P.; Alvarez-Sánchez, R.; Fueth, M.; Broders, O.; Kettenberger, H.; Stubenrauch, K.; Caruso, A. Ocular pharmacokinetics of intravitreally injected protein therapeutics: Comparison among standard-of-care formats. Mol. Pharm. 2021, 18, 2208–2217. [Google Scholar] [CrossRef]
- Klein, C.; Schaefer, W.; Regula, J.T. The use of CrossMAb technology for the generation of bi- and multispecific antibodies. mAbs 2016, 8, 1010–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, C.; Schaefer, W.; Regula, J.T.; Dumontet, C.; Brinkmann, U.; Bacac, M.; Umaña, P. Engineering therapeutic bispecific antibodies using CrossMab technology. Methods 2019, 154, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Khanani, A.M.; Patel, S.S.; Ferrone, P.J.; Osborne, A.; Sahni, J.; Grzeschik, S.; Basu, K.; Ehrlich, J.S.; Haskova, Z.; Dugel, P.U. Efficacy of Every Four Monthly and Quarterly Dosing of Faricimab vs Ranibizumab in Neovascular Age-Related Macular Degeneration: The STAIRWAY Phase 2 Randomized Clinical Trial. JAMA Ophthalmol. 2020, 138, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Liang, X.H.; Ferrara, N. Comparing protein VEGF inhibitors: In vitro biological studies. Biochem. Biophys. Res. Commun. 2011, 408, 276–281. [Google Scholar] [CrossRef]
- Saishin, Y.; Saishin, Y.; Takahashi, K.; Lima e Silva, R.; Hylton, D.; Rudge, J.S.; Wiegand, S.J.; Campochiaro, P.A. VEGF-TRAP(R1R2) suppresses choroidal neovascularization and VEGF-induced breakdown of the blood-retinal barrier. J. Cell. Physiol. 2003, 195, 241–248. [Google Scholar] [CrossRef]
- Nork, T.M.; Dubielzig, R.R.; Christian, B.J.; Miller, P.E.; Miller, J.M.; Cao, J.; Zimmer, E.P.; Wiegand, S.J. Prevention of experimental choroidal neovascularization and resolution of active lesions by VEGF trap in nonhuman primates. Arch. Ophthalmol. 2011, 129, 1042–1052. [Google Scholar] [CrossRef] [Green Version]
- Foxton, R.H.; Uhles, S.; Grüner, S.; Revelant, F.; Ullmer, C. Efficacy of simultaneous VEGF-A/ANG-2 neutralization in suppressing spontaneous choroidal neovascularization. EMBO Mol. Med. 2019, 11, e10204. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Shah, S.M.; Hafiz, G.; Quinlan, E.; Sung, J.; Chu, K.; Cedarbaum, J.M.; Campochiaro, P.A.; CLEAR-AMD 1 Study Group. A phase I trial of an IV-administered vascular endothelial growth factor trap for treatment in patients with choroidal neovascularization due to age-related macular degeneration. Ophthalmology 2006, 113, 1522.e1–1522.e14. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Shah, S.M.; Browning, D.J.; Hudson, H.; Sonkin, P.; Hariprasad, S.M.; Kaiser, P.; Slakter, J.S.; Haller, J.; Do, D.V.; et al. A phase I study of intravitreal vascular endothelial growth factor trap-eye in patients with neovascular age-related macular degeneration. Ophthalmology 2009, 116, 2141–2148.e1. [Google Scholar] [CrossRef]
- Do, D.V.; Nguyen, Q.D.; Shah, S.M.; Browning, D.J.; Haller, J.A.; Chu, K.; Yang, K.; Cedarbaum, J.M.; Vitti, R.L.; Ingerman, A.; et al. An exploratory study of the safety, tolerability and bioactivity of a single intravitreal injection of vascular endothelial growth factor Trap-Eye in patients with diabetic macular oedema. Br. J. Ophthalmol. 2009, 93, 144–149. [Google Scholar] [CrossRef]
- Brown, D.M.; Heier, J.S.; Ciulla, T.; Benz, M.; Abraham, P.; Yancopoulos, G.; Stahl, N.; Ingerman, A.; Vitti, R.; Berliner, A.J.; et al. Primary endpoint results of a phase II study of vascular endothelial growth factor trap-eye in wet age-related macular degeneration. Ophthalmology 2011, 118, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Boyer, D.; Nguyen, Q.D.; Marcus, D.; Roth, D.B.; Yancopoulos, G.; Stahl, N.; Ingerman, A.; Vitti, R.; Berliner, A.J.; et al. The 1-year results of CLEAR-IT 2, a phase 2 study of vascular endothelial growth factor trap-eye dosed as-needed after 12-week fixed dosing. Ophthalmology 2011, 118, 1098–1106. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Kaiser, P.K.; Korobelnik, J.F.; Brown, D.M.; Chong, V.; Nguyen, Q.D.; Ho, A.C.; Ogura, Y.; Simader, C.; Jaffe, G.J.; et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: Ninety-six-week results of the VIEW studies. Ophthalmology 2014, 121, 193–201. [Google Scholar] [CrossRef]
- Chakravarthy, U.; Bailey, C.; Brown, D.; Campochiaro, P.; Chittum, M.; Csaky, K.; Tufail, A.; Yates, P.; Cech, P.; Giraudon, M.; et al. Phase I Trial of Anti-Vascular Endothelial Growth Factor/Anti-angiopoietin 2 Bispecific Antibody RG7716 for Neovascular Age-Related Macular Degeneration. Ophthalmol. Retin. 2017, 1, 474–485. [Google Scholar] [CrossRef]
- Khurana, R.N.; Rahimy, E.; Joseph, W.A.; Saroj, N.; Gibson, A.; Vitti, R.; Berliner, A.J.; Chu, K.; Cheng, Y.C.; Boyer, D.S. Extended (every 12 weeks or longer) dosing interval with intravitreal aflibercept and ranibizumab in neovascular age-related macular degeneration: Post hoc analysis of VIEW trials. Am. J. Ophthalmol. 2019, 200, 161–168. [Google Scholar] [CrossRef]
- You, Q.S.; Gaber, R.; Meshi, A.; Ramkumar, H.L.; Alam, M.; Muftuoglu, I.K.; Freeman, W.R. High-dose high-frequency aflibercept for recalcitrant neovascular age-related macular degeneration. Retina 2018, 38, 1156–1165. [Google Scholar] [CrossRef]
- Study of a High-Dose Aflibercept in Participants with Diabetic Eye Disease (PHOTON), NCT04429503. Available online: https://clinicaltrials.gov/ct2/show/NCT04429503 (accessed on 12 August 2022).
- Study to Gather Information on Safety and Use of High Dose Aflibercept Injection Into the Eye in Patients With an Age Related Eye Disorder That Causes Blurred Vision or a Blind Spot Due to Abnormal Blood Vessels That Leak Fluid Into the Light Sensitive Ining Inside the Eye (PULSAR), NCT04423718. Available online: https://clinicaltrials.gov/ct2/show/NCT04423718 (accessed on 12 August 2022).
- Barış, M.E.; Menteş, J.; Afrashi, F.; Nalçaçı, S.; Akkın, C. Subgroups and Features of Poor Responders to Anti-Vascular Endothelial Growth Factor Treatment in Eyes with Neovascular Age-Related Macular Degeneration. Turk. J. Ophthalmol. 2020, 50, 275–282. [Google Scholar] [CrossRef]
- Usui-Ouchi, A.; Tamaki, A.; Sakanishi, Y.; Tamaki, K.; Mashimo, K.; Sakuma, T.; Ebihara, N. Factors Affecting a Short-Term Response to Anti-VEGF Therapy in Diabetic Macular Edema. Life 2021, 11, 83. [Google Scholar] [CrossRef]
- Patel, P.; Sheth, V. New and innovative treatments for neovascular age-related macular degeneration (nAMD). J. Clin. Med. 2021, 10, 2436. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Bandello, F. Brolucizimab—leading an era of structural revolution for long-term VEGF suppression. Eye 2020, 34, 611–613. [Google Scholar] [CrossRef] [PubMed]
- Tadayoni, R.; Sararols, L.; Weissgerber, G.; Verma, R.; Clemens, A.; Holz, F.G. Brolucizumab: A newly developed anti-VEGF molecule for the treatment of neovascular age-related macular degeneration. Ophthalmologica 2021, 244, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Moisseiev, E.; Loewenstein, A. Abicipar pegol—A novel anti-VEGF therapy with a long duration of action. Eye 2020, 34, 605–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Bandello, F. Abicipar pegol: The non-monoclonal antibody anti-VEGF. Eye 2020, 34, 797–801. [Google Scholar] [CrossRef]
- Regillo, C.; Ehrlich, J.S.; Janer, D.; Do, D.V.; Velazquez-Martin, P.; Zawadzki, R.; Perlroth, V. Efficacy, durability and safety of KSI-301 antibody biopolymer conjugate in wet AMD–Year 1 primary endpoint results from the pivotal DAZZLE study. Investig. Ophthalmol. Vis. Sci. 2022, 63, 3122. [Google Scholar]
- O’Neill, H.C.; Limnios, I.J.; Barnett, N.L. Advancing a stem cell therapy for age-related macular degeneration. Curr. Stem. Cell Res. Ther. 2020, 15, 89–97. [Google Scholar] [CrossRef]
- Moore, N.A.; Bracha, P.; Hussain, R.M.; Morral, N.; Ciulla, T.A. Gene therapy for age-related macular degeneration. Expert Opin. Biol. Ther. 2017, 17, 1235–1244. [Google Scholar] [CrossRef]
- de Guimaraes, T.A.C.; Georgiou, M.; Bainbridge, J.W.; Michaelides, M. Gene therapy for neovascular age-related macular degeneration: Rationale, clinical trials and future directions. Br. J. Ophthalmol. 2021, 105, 151–157. [Google Scholar] [CrossRef] [Green Version]
- Chauhan, M.Z.; Rather, P.A.; Samarah, S.M.; Elhusseiny, A.M.; Sallam, A.B. Current and Novel Therapeutic Approaches for Treatment of Diabetic Macular Edema. Cells 2022, 11, 1950. [Google Scholar] [CrossRef]

| Drug’s Name | Aflibercept | Faricimab | Reference | |
|---|---|---|---|---|
| Other used name (s) | VEGF-Trap Eye | RG7716 | [3,11] | |
| Molecular weight | 115-kDa | 150-kDa | [3,11] | |
| Molecular structure | Binding domains of human VEGFR-1 and VEGFR-2 combined with the constant Fc domain of human IgG1 | Two different light chains and two different heavy chains combined with modified human IgG1 | [3,16] | |
| Binding molecules | VEGF-A, VEGF-B, PlGF-1, PlGF-2 | VEGF-A, Ang-2 | [11] | |
| Intravitreal dose used in clinical practice | 2 mg | 6 mg | [3,11] | |
| Date of FDA approval for: | nAMD | 2011 | 2022 | [11,68] |
| DME | 2014 | 2022 | [11,68] | |
| Registered indications | nAMD, DME, myopic choroidal neowascularization, macular edema secondary to retinal vein occlusion | nAMD, DME | [11,16] | |
| Trial Name | Phase | Number of Participants | Study Design | Primary and Secondary End Measurements | Explanatory Comment a,b | Reference |
|---|---|---|---|---|---|---|
| CLEAR-AMD 1 | I | 25 nAMD patients | Single intravenous aflibercept administration at a dose: (1) 0.3 mg/kg; (2) 1.0 mg/kg, (3) 3.0 mg/kg with 4-week observational period and then 3 doses in 2-week intervals (4) Placebo | Assessment of the safety, pharmacokinetics, and biological activity of intravenous aflibercept | - 2 of 5 participants that received a 3.0 mg/kg dose presented toxicity symptoms - One patient developed grade 4 hypertension, and another one had grade 2 proteinuria - BCVA remains unchanged - CRT decreased −10%, −66%, −60%, and −12% in examined groups, respectively - 1.0 mg/kg of aflibercept was a maximally tolerated dose - Patients from the 3.0 mg/kg regimen were withdrawn from the experiment, and the study was terminated | [78] |
| CLEAR-IT 1 | I | 25 nAMD patients | Single IVA injection in doses: (1) 0.05 mg; (2) 0.15 mg; (3) 0.5 mg; (4) 1.0 mg; (5) 2 mg; (6) 4 mg. vs. placebo with 6-week follow-up | Safety assessment | 6-week results: - The mean change of BCVA was +4.43 L (in the 2 mg and 4 mg groups, BCVA gained +13.5 L) - The mean decrease in CRT was −104.5 µm During the study, all dosing regimens had no ocular AEs or SAEs. | [79] |
| CLEAR-IT 2 | II | 159 nAMD patients with subfoveal CNV | Phase 1 (fixed-dosing): 1–12 weeks Five dosing regimens of IVA: (1) 0.5 mg every 4 weeks (2) 2 mg every 4 weeks (3) 0.5 mg every 12 weeks (4) 2 mg every 12 weeks (5) 4 mg every 12 weeks Phase 2: 12–52 weeks Further PRN dosing in all regimens examined in phase 1 | Phase 1 Primary: - Change in CL/LT at week 12 Secondary: - Change in BCVA - Proportion of patients that gained and lost 15 or more litres Phase 2 - Change in CR/LT - Change in CNV lesion size - Mean change in BCVA - Proportion of patients that gained and lost 15 or more L - Time for the first PRN injection - Reinjection frequency - Safety | 12-week results: - The mean decrease in CR/LT in IVA regimens was −119 µm (with the most improvement in (1) and (2) groups - BCVA gain in IVA groups was +5.7 L (with the >8 L gain in (1) and (2) groups) - 98% of patients avoided −15 or more L decrease in BCVA - 18.5% of individuals gained 15 or more liters There were no significant ocular ad systemic AEs. 52-week results: - Mean decrease in CR/LT in IVA regimens was −130 µm (with the most improvement in (1) and (2) groups - CNV lesion size regression was −2.21 mm - BCVA gained in IVA groups was +5.3 L (the most marked improvement was +9 L in (2) group) - Mean 2 injections were administered in IVA regimens - Mean time to the first injection in phase 2 was 129 days - 19% of participants did not need injections in phase 2, and 45% of participants received 1 or 2 injections - 92% of participants avoided −15 or more liters decrease in BCVA - 22% of patients gained 15 or more liters IVA was well tolerated, and ocular as well as systemic AEs were typical to those previously reported in other anti-VEGF agents | [80,81] |
| VIEW-1 and VIEW-2 | III | 2419 nAMD patients with active, sub-foveal CNV | Four dosing regimens in the first 52 weeks: (1) 0.5 mg IVA every 4 weeks (2) 2 mg of IVA every 4 weeks (3) 2 mg of IVA every 8 weeks after 3 injections at 4-week intervals (4) 0.5 mg IVR every 4 weeks 52–96 weeks: PRN dosing regimen in all groups | Primary - Comparison of IVA dosing regimens with the IVR group (testing for non-inferiority—with 10% margin) in the proportion of participants with vision loss <15 L at week 52 and 96 week Secondary: - Change in BCVA - Proportions of patients with +15 letter gain - Change in NEI VFQ-25 score - Change in CNV lesions area - Change in CRT and the persistence of fluid | 52-week results of VIEW 1: - There were of participants with vision loss <15 L 94.4% in IVR arm vs. 95.1%, 95.9%, 95.1% in IVA regimens - The mean change in BCVA was +8.1 ± 15.3, +10.9 ± 13.8, +6.9 ± 13.4, and +7.9 ± 15.0 L, respectively - The mean CRT decreased by −116.8 ± 109.0 µm, −116.5 ± 98.4 µm, and −115.6 ± 104.1 µm in IVA groups, while in the IVR regimen, the mean change was −128.5108.5 µm - Change in the NEI VFQ-25 score was 4.9 ± 14.0 in the IVR arm vs. 6.7 ± 13.5, 4.5 ± 11.9, and5.1 ± 14.7 in patients who received IVA - The mean decrease in CNV lesion area was 4.2 ± 5.6 mm2 in participants following IVR and 4.6 ± 5.5, 3.5 ± 5.3, and 3.4 ± 6.0 in patients treated by IVA - There were no SRF or IRF in 63.6% of patients treated by IVR compared to 64.8%, 56.7%, and 63.4% of patients receiving IVA 52-week results of VIEW-2: - 94.4% of patients followed IVR loose less than 15 L compared to 95.6%, 96.3%, and 95.6% IVA regimens - The mean change in BCVA was +9.4 ± 13.5 in the IVR group vs. +7.6 ± 12.6, +9.7 ± 14.1, and +8.9 ± 14.4 in IVA regimens - The mean CRT reduced −138.5 ± 122.2 µm in participants that received IVR vs. −156.8 ± 122.8 µm, −129.8 ± 114.8 µm, and −149.2 ± 119.7 µm in IVA groups -The mean change in the NEI VFQ-25 score was 6.3 ± 14.8 in the IVR arm vs. 4.5 ± 15.0, 5.1 ± 13.7, and 4.9 ± 14.7 mm2 in patients who received IVA - Decrease in CNV lesion area was 4.2 ± 5.9 mm2 in participants following IVR and 6.0 ± 6.1, 4.2 ± 6.1, and 5.2 ± 5.9 mm2 in patients treated by IVA SRF and IRF were absent in 60.4% of participants in the IVR arm vs. 80.3%, 63.9%, and 71.9% of patients in the IVA groups 96-week combined results of VIEW-1 and VIEW-2: - 91.6% of participants lose <15 L in IVR arm vs. 92.2%, 91.5%, and 92.4% in IVA regimens - The mean BCVA gained +7.9 L in the IVR arm vs. +7.6, +6.6, and +7.6 L in IVA regimens - The mean change in CRT was −118 µm in the IVR arm vs. 113, 128, and 133 µm in IVA regimens - SRF and IRF were absent in 45.5% of participants in the IVR arm vs. 54.4%, 44.6%, and 50.1% of patients in the IVA groups - 73.5/26.5% vs. 86.0%/14.0% vs. 76.0%/24.0% vs. 84.1%/15.9% patients received less/more than 6 injections in PRN phase in IVR, and IVA groups, respectively A similar frequency of AEs and SAEs was observed between examined groups during the first and PRN phase of the study. | [29,82] |
| Trial Name | Phase | Number of Participants | Study Design | Primary and Secondary Outcomes | Explanatory Comment a,b | Reference |
|---|---|---|---|---|---|---|
| - | I | 6 patients with diabetic macular edema | Single 4 mg IVA injection with 6 weeks follow-up | Safety and tolerability of IVA Changes in BCVA and change in CRT at four and six weeks | 4-week results: - The mean BCVA improvement +9 L - Mean CST reduction −49 µm 6-week results: - The mean BCVA improvement +3 L achieved in 4 of 5 participants - The mean CST reduction −34 µm achieved in 4 of 5 participants There were no ocular and systemic side effects | [31] |
| DA VINCI | II | 221 patients with type 1 or type 2 diabetes presented center-involved DME | 5 treatment regimens: (1) Injection of 0.5 mg IVA every 4 weeks (2) Injection of 2 mg of IVA every 4 weeks (3) Injection of 2 mg IVA for the first 3 months, and then in 8-week intervals (4) Injection of 2 mg IVA for the first 3 months, and then PRN treatment (5) Macular laser photocoagulation at baseline and the as needed (with minimum 16-week intervals) + sham injections every 4 weeks | Primary: - Improvement in BCVA at 24 weeks - Assessment of safety and tolerability of IVA injections in DME eyes Secondary: - Change in CRT value from baseline up to 24 weeks - Improvement in BCVA and CRT at 52 weeks - Proportions of eyed gained +15 L at 24 and 52 weeks - Number of focal lasers sessions | 24-week results: - BCVA improvement in IVA regimens ranged from +8.5 to +11.4 vs. +2.5 L in the laser + sham injection arm - Improvement of BCVA in IVA vs. laser arms, respectively: 93% vs. 68% of patients gained +0 L 64% vs. 32% of patients gained +5 L 34% vs. 21% of patients gained +15 L - The mean decrease in CRT values in the IVA regimens ranged from −127.3 µm to −194.5 µm vs. 67.9 µm in the laser + sham injections arm - Mean < 1.7 focal laser sessions were performed in the laser group from baseline up to 24 weeks 52-week results: - BCVA improvement in IVA regimens ranged from +9.7 to +13.1 L vs. −1.3 L in the laser and sham injection arm - From 23.8% to 45.4% vs. 11.4% of patients gained +15 L in IVA vs. laser arms, respectively - From 45% to 71% vs. 30% patients gained +10 L in IVA vs. laser arms, respectively - The mean decrease in CRT values in the IVA regimens ranged from −165.4 µm to −227.4 µm vs. 58.4 µm in the laser + sham injections arm - <1 and 2.5 focal laser sessions were performed in IVA groups vs. laser arm from 24 to 52 weeks - Baseline DRSS value ranged from 31% to 64% in IVA arms vs. 12% in the laser regimen, and at 52 weeks, DRSS value ranged from 0% to 14% in IVA groups vs. 24% in the laser arm Ocular adverse effects were mild and typical for intravitreal injections, while systemic adverse effects were not directly associated with the drug action. | [83,84] |
| VIVID and VISTA | III | 872 patients with type 1 or 2 diabetes presented center involved DME | 3 treatment regimens: (1) Injection of 2 mg of IVA every 4 weeks (2) Injection of 2 mg IVA for the first 5 months, and then in 8-week intervals (3) Macular laser photocoagulation at baseline and the as needed (with minimum 16-weeke intervals) + sham injections every 4 weeks | Primary: - Improvement in BCVA at 52 weeks Secondary: - Mean change in CST at 52 weeks - Proportions of eyed gained +15 at 52 weeks | 52-week results: VIVID: - The mean change of BCVA in IVA arms was +10.5 and +10.7 compared to +1.2 L in the laser group - Participants with a BCVA improvement of +15 L or more accounted for 32.4% and 33.3% in IVA groups vs. 9.1% in the laser arm - The mean change in CST was −195 µm and 192.4 µm in IVA regimens vs. 66.2 µm in the laser group VISTA: -The mean change of BCVA in IVA arms was +12.5 and +10.5 compared to +0.2 L in the laser arm - There were 41.6% and 31.1% vs. 7.8% of participants who gained that +15 L - The mean change in CST was −185.9 µm and 183.1 µm in IVA regimens compared to −73.3 µm in the laser arm 100-week results: VIVID: - The mean change of BCVA in participants following IVA was +11.4 and +9.4 vs. +0.7 L in individuals treated by the laser photocoagulation - 38.2% and 31.1% of patients gained 15 or more L in IVA regimens vs. 12.1% in the laser arm - The mean change in CST was −211.8 ± 150.9 µm and −195.1 ± 141.7 µm in IVA regimens vs. −85.7 ± 179.3 µm in the laser group - 29.3% and 32.6% of participants achieved at least 2-step improvement in DRSS score compared to 8.2% in the laser arm VISTA: - The mean change in BCVA in IVA regimens was +11.5 and 11.1 vs. +0.9 L in the laser arm - 38.3% and 33.1% of participants in IVA groups gained 15 or more L vs. 13.0% in the laser group - CST changed −191.4 ± 180.0 µm; −191.1 ± 160.7 µm, and −83.9 ± 179.3 µm, respectively - Improvement of 2 or more steps in DRSS score was observed in 37.0% and 37.1% in IVA regimens vs. 15.6% in the laser group 148-week results: VIVID: - The mean change in BCVA in IVA arms was +10.3 and +11.7 compared to +1.6 L in the laser arm - 41.2% and 42.2% of eyes gained 15 or more L in IVA regimens vs. 18.9% in the laser group - CST changed −215.2 µm and −202.8 µm in the laser group vs. −122.8 µm in patients following the laser treatment - Improvement in DRSS score of more steps was observed in 44.3% and 47.8% of patients following IVA vs.17.4% of individuals in the laser group VISTA: - The mean change in BCVA in IVA regimens was +10.4 and +10.5 vs. +1.4 L in the laser group - 42.9% and 35.8% of participants treated with IVA gained 15 or more L compared to 13.6% treated by the laser - CST changed −200.4 µm and −190.1 µm in IVA arms vs. −109.8 µm in the laser group - Improvement in DRSS score of more steps was observed in 29.9% and 34.4% of patients following IVA vs. 20.1% of individuals in the laser arm During the VISTA and VIVID studies, the incidence of ocular and non-ocular AEs and SAEs were similar between examined groups. | [24,35] |
| Trial Name | Phase | Number of Participants | Study Design | Primary and Secondary End Measurements | Explanatory Comment a,b | Reference |
|---|---|---|---|---|---|---|
| - | I | 24 nAMD patients | Single IVF injection at a dose: (1) 0.5 mg (2) 1.5 mg (3) 3 mg (4) 6 mg Multiple-dose phase: (1) 3 injections of 3.0 mg IVF (2) 3 injections of 6.0 IVF 4-week follow-up | - Safety and tolerability of IVF - Change in BCVA and CST at 4 weeks | - The mean BCVA changed +7 and +7.5 L in single-dose groups and multiple-dose groups, respectively - The mean CST decreased −42 µm in participants treated with a single IVF dose compared to −117 µm in the multiple-dose group Faricimab was well-tolerated, and there were no AE related to the drug action. | [85] |
| STAIRWAY | II | 76 nAMD patients | Dosing regimens: (1) 0.5 mg ranibizumab every 4 weeks (2) 6.0 mg faricimab every 12 weeks after 4 monthly injections (3) 6.0 mg faricimab every 14 weeks after 4 monthly injections (with re-selection in IVF arms based on disease activity in 24 weeks) | Primary: - The mean change in BCVA at week 40 Secondary: -Change in BCVA measured every 4 weeks - Number of participants with +15, +10, +5, and 0 L gain vision - Mean decrease in CST, CNV lesion area, and leakage area | - In 40 weeks, mean BCVA change was +11.4 L in the IVR arm compared to +9.3 and +12.5 L w IVF arms, respectively - In 52 weeks, the mean BCVA gained +9.6 L after 12.9 injections, while in quarterly dosed faricimab, the mean BCVA changed +10.1 L after 6.7 injections, and in 4 monthly dosed faricimab, the arm mean BCVA gained +11.4 L after 6.2 injections - 33.3%/100% of participants gained/did not lose 15 or more L in the IVR group compared to 38.1%/95.2% and 39.3%/96.4% in INF regimens - The mean CST change was −126.3 µm in IVR arms compared to −138.6 µm and −121.3 µm in IVF groups - The mean CNV lesion size was reduced −4.6 mm2 in IVR, as well as −4.7 mm2 and −3.9 mm2 in IVF groups - Mean change in mean leakage lesion area was −5.3 mm2 in the IVR group vs. −5.0 mm2 and −4.3 mm2 in IVF arms Incidence of AEs and SAEs was similar between examined regimens across the study. | [73] |
| AVENUE | II | 263 nAMD patients | Dosing regimens: (1) 0.5 mg IVR every 4 weeks (2) 1.5 mg IVF every 4 weeks (3) 6.0 mg IVF every 4 weeks (4) 6.0 mg IVF every 4 weeks until week 12 and then every 8 weeks (5) 0.5 mg IVR every 4 weeks until week 8 and then 6.0 mg IVF every 4 weeks | Primary: - Mean BCVA change at week 36 and mean BCVA change for patients with the incomplete response from groups (1) and (5) from weeks 12 to 36 - Percentage of patients with 15 or more L gain - Percentage of patients with BCVA at least/worse than 20/40 - Change in mean CST - Change in CNV lesion area and leakage | 36-week results: - The mean BCVA change was +8.5 L in IVR groups and +10.9, +5.9, and +6.3 L in (2), (3), and (4) groups, respectively - 31.3% of participants gained 15 or more L in IVR group compared to 37.5%, 27.0%, and 22.7% in (2), (3), and (4) groups, respectively - Proportions of patients with BCVA 20/40 or better/worse than 20/40 was: 50.0%/7.8%, 50.0%/7.5%, 40.5%/16.2%, and 43.2%/9.1% for (1), (2), (3), and (4) groups, respectively - The mean CST changed −161.3 µm in the IVR arm compared to −152.2 µm, −190.7 µm, and −151.9 in IVF groups - The mean CNV area changed −2.6 mm2 in IVR arm vs. −3.4 mm2, −2.1 mm2, and −3.1 mm2 in (2), (3), and (4) groups, respectively - The mean change in leakage area was −5.2 mm2 in the IVR arm vs. −4.6 mm2, −3.2 mm2, and −5.4 mm2 in (2), (3), and (4) groups, respectively 36-week results with incomplete response groups (results are provided for (1) and (5) groups), respectively: - The mean change in BCVA was +2.1 vs. +0.6 L - 5.7% and 0% of patients gained +15 or more L - 22.9%/14.3% and 16.2%/13.5% of patients had BCVA of 20/40 or better/or BCVA worse than 20/40 - The mean CST changed −13.0 µm vs. −36.5 µm - The mean CNV area changed −0.5 mm2 vs. −1.4 mm2 - The mean area of leakage decreased −1.9 mm2 vs. −2.0 mm2 | [65] |
| TENAYA and LUCERNE | III | 1329 nAMD patients | (1) 6.0 mg IVF up to 16 weeks after 4 initial doses in 4-week intervals, and then based on the assessment of disease activity at 20- and 24-week doses in 8-, 12- or 16-week intervals until week 60 (2) 2.0 mg IVA in 8-week intervals | Primary: - Mean change in BCVA at week 48 (non-inferiority margin of 4 L) Secondary: - Proportions of patients treated in 8-,12- and 16-week intervals - Percentage of patients gaining ≥ 15, ≥10, ≥5, or ≥0 L and patients with loss ≥ 15, ≥10, or ≥5 L; patients gaining 15 or more L or achieving BCVA ≥ 84 L - The percentage of patients with BCVA 20/40 equal or better, and BCVA 20/200 or worse. Change in CST - Change in CNV lesion and leakage areas - Change in NEI VFQ-25 score - Incidence and severity of AEs | 48-week results: TENAYA: - The mean BCVA change was +5.8 L in IVF groups and +5.1 L in the IVA regimen - The mean CST change was −136.8 μm in IVF regimens and −129.4 μm in the IVA group - Proportion of IVF-treated patients with 8-week, 12-week, and 16-week injection intervals was 20.3%, 34.0%, and 45.7%, respectively - The mean change in CNV lesion and leakage areas were comparable between IVF and IVA groups LUCERNE: - The mean change in BCVA was +6.6 L in IVF groups and +6.6 L in the IVA arm - The mean CST change was −137.1 in IVF groups and −130.8 μm in the IVA arm - Proportion of IVF-treated patients with 8-week, 12-week, and 16-week injection intervals was 22.2%, 32.9%, and 44.9%, respectively - The mean change in CNV lesion and leakage areas were comparable between IVF and IVA groups Summary analysis: - 45.3% and 78.7% of participants received IVF in 16- and 12-week intervals, respectively - 20.0–20.2% of patients in IVF groups gained 15 or more L compared with 15.7–22.2% in the IVA arm - NEI VFQ-25 score was also comparable between the groups In both studies, there were no significant differences among AEs between the examined groups. | [16] |
| Trial Name | Phase | Number of Participants | Study Design | Primary and Secondary Outcomes | Explanatory Comment a,b | Reference |
|---|---|---|---|---|---|---|
| BOULEVARD | II | 229 diabetic patients with center involving DME (168 treatment-naive and 61 non-treatment-naive) | Dosing regimens in treatment-naive patients: (1) 6.0 mg IVF every 4 weeks up to week 20 (2) 1.5 mg IVF every 4 weeks up to week 20 (3) 0.3 mg IVR every 4 weeks up to week 20 with follow-up period up to week 36 Dosing regimens in non-treatment-naive patients: (1) 0.3 mg IVR every 4 weeks up to week 20 (2) 6.0 mg IVF up to week 20 With a follow-up period of up to 36 weeks | Primary: - Mean change in BCVA in treatment-naive patients at week 24 Secondary: - Proportion of patients with 15 or more BCVA L gain - Mean change in CST - Improvement in 2 or more steps in the DRSS score | Results regarding treatment-naive patients: - The mean BCVA changed +13.9 and + 11.7 in IVF groups compared to +10.3 L in the IVR arm, respectively - The mean CST changed −204.7 µm in the IVR group vs. −217.1 µm and −225.8 µm in IVF regimens - Improvement in at least 2 steps in the DRSS score was achieved in 12% of patients treated by IVR vs. 28% and 39% of participants in IVF groups - 35.3% of patients in the IVR arm gained +15 or more L vs. 36.0% and 42.5% of participants in IVF regimens Results regarding non-treatment-naive patients: - The mean BCVA gained +8.3 and +9.6 L in IVR and IVF groups, respectively - The mean CST changed −148.0 µm in IVR regimen vs. −186.6 µm in IVR group - The DRSS score was improved in at least 2 steps in 23% of participants in both groups - The number of individuals with CST of 325 µm or less at week 24 was 53.6% in the IVR arm and 87.0% in the IVF arm Ocular and systemic AEs and SAEs were similar among examined groups. | [15] |
| YOSEMITE and RHINE | III | 1891 diabetic patients with center involving DME | Dosing regimens: (1) six-monthly injections of 6.0 mg IVF at a dose of 6.0 mg and then every 8 weeks (2) four monthly injections of 6.0 mg IVF and then with PTI schedule (intervals were regulated in the range of 4–16 weeks based on the disease activity (3) five monthly IVA injections at a dose of 2.0 mg and then every 8 weeks | Primary: - Mean change in BCVA over weeks 48, 52, and 56 (non-inferiority margin of 4 L) Secondary: - Percentage of patients in PTI groups receiving faricimab in 4-, 8-, 12-, and 16-week intervals - Percentage of participants with CST less than 325 µm and with the absence of IRF or SRF - Number of patients with 15, 10, 5, and 0 letter vision gain and 15, 10, and 5 L vision loss - Number of patients with BCVA 20/40 or better - Percentage of patients with 2 or more step improvement in DRSS at week 52 Safety and tolerability of IVF | YOSEMITE: - The mean BCVA change was +10.7 and +11.6 L in IVF groups compared to +10.9 L in the IVA arm - 10.8%, 15.4%, 21.0%, and 52.8% of patients in the PTI arm received IVF injections at 4-, 8-, 12-, and 16-week intervals - The mean CST changed −206.6 µm and −196.5 µm in the IVF groups compared to −170.3 µm in the IVA arm - In 77–87% and 80–82% of patients, CST less than 325 µm was observed compared to 64–71% in the IVA arm - IRF was absent in 42–48% and 34–43% of participants in IVF groups and 22–25% in the IVA arm - The percentage of patients with 2 or more step reduction in the DRSS score was 46.0% and 42.5% in IVF groups and 35.8% in the IVA group RHINE: - The mean BCVA change was +11.8 and +11.8 L in IVF regimens vs. + 10.3 in the IVA group - 13.3%, 15.6%, 20.1%, and 51.0% of patients in the PTI arm received IVF injections at 4-,8-,12-, and 16-week intervals - The mean CST was reduced −195.8 µm, −187.6 vs. −170.1 µm in the IVA group - In 85–90% and 83–87% of patients CST less than 325 µm was observed compared to 71–77% in the IVA arm - IRF was not detected in 39–43% and 33–41% of participants in IVF groups vs. 23–29% in the IVA arm - The percentage of patients with 2 or more step reduction in the DRSS score was 44.2% and 43.7% in IVF groups and 46.8% in the IVA group In both studies, the incidence of AEs and SAEs was similar between study groups. | [17] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liberski, S.; Wichrowska, M.; Kocięcki, J. Aflibercept versus Faricimab in the Treatment of Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema: A Review. Int. J. Mol. Sci. 2022, 23, 9424. https://doi.org/10.3390/ijms23169424
Liberski S, Wichrowska M, Kocięcki J. Aflibercept versus Faricimab in the Treatment of Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema: A Review. International Journal of Molecular Sciences. 2022; 23(16):9424. https://doi.org/10.3390/ijms23169424
Chicago/Turabian StyleLiberski, Sławomir, Małgorzata Wichrowska, and Jarosław Kocięcki. 2022. "Aflibercept versus Faricimab in the Treatment of Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema: A Review" International Journal of Molecular Sciences 23, no. 16: 9424. https://doi.org/10.3390/ijms23169424
APA StyleLiberski, S., Wichrowska, M., & Kocięcki, J. (2022). Aflibercept versus Faricimab in the Treatment of Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema: A Review. International Journal of Molecular Sciences, 23(16), 9424. https://doi.org/10.3390/ijms23169424






