The Neurobiological Links between Stress and Traumatic Brain Injury: A Review of Research to Date
Abstract
:1. Introduction
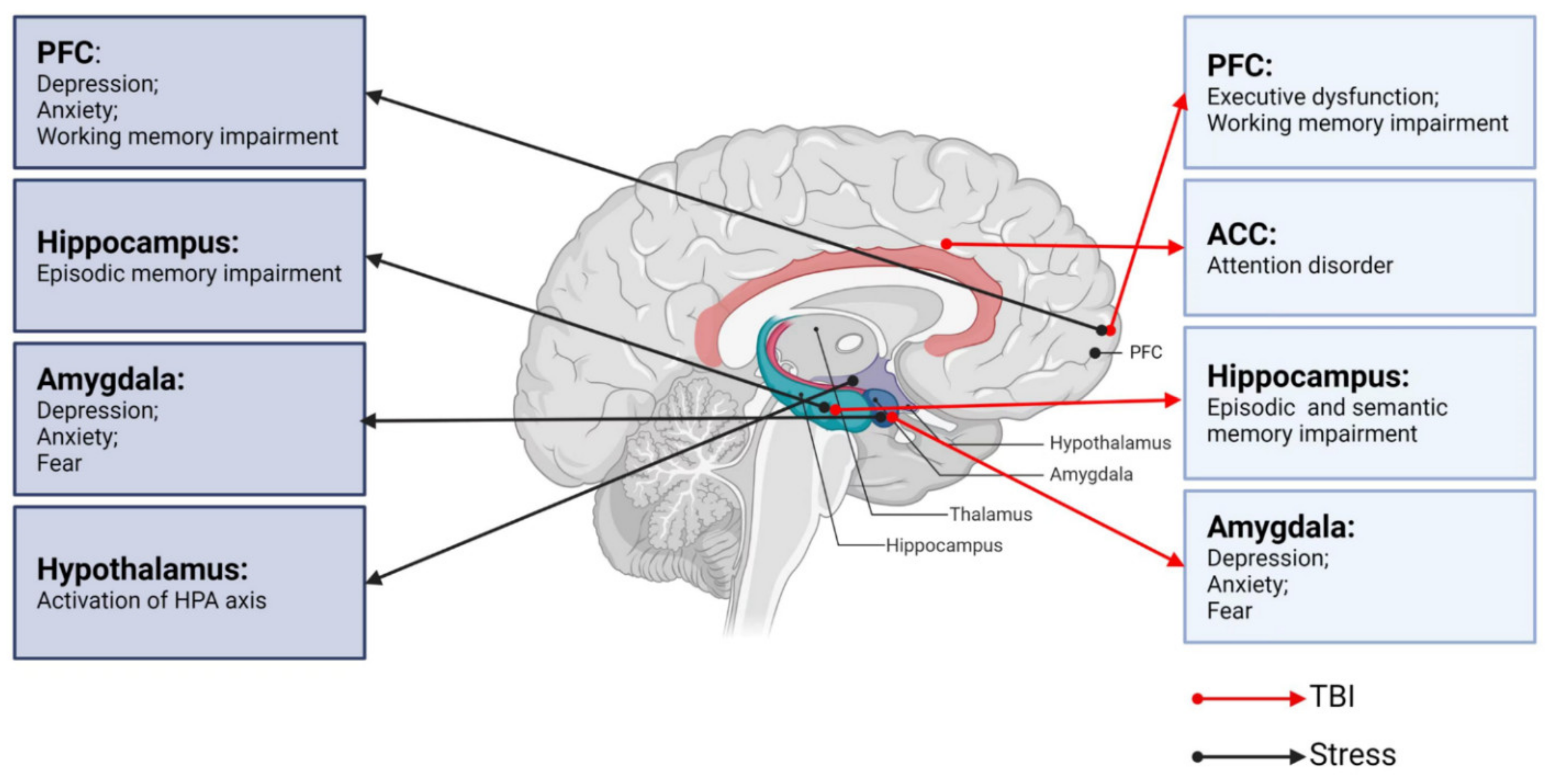
2. Neurobiological Links between TBI and Neurological Dysfunctions
2.1. TBI and Cognitive Impairments
2.2. TBI and Emotional/Behavioral Disturbances
3. Neurobiological Links between Stress and Key Brain Regions
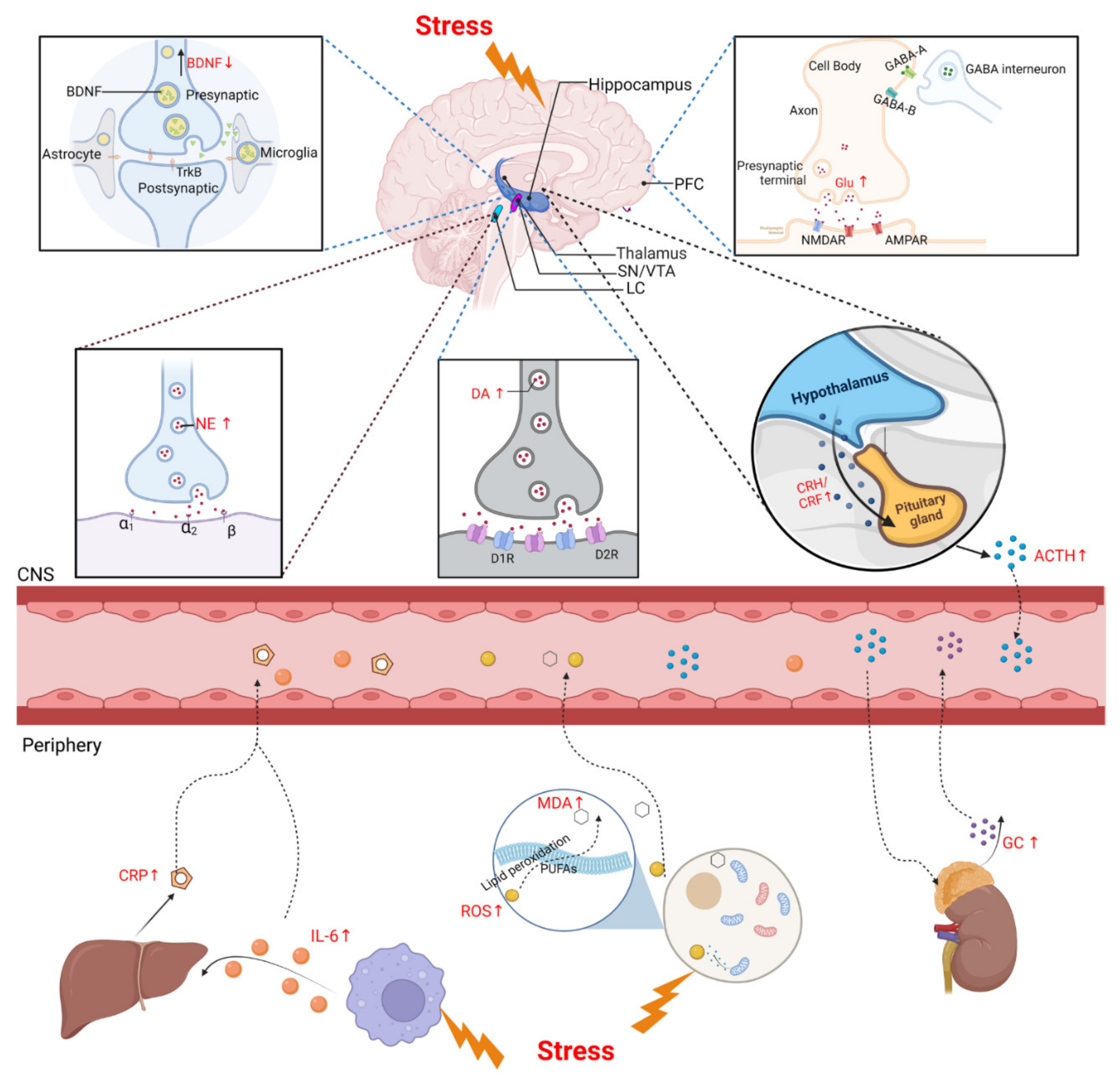
3.1. Stress and the HPA Axis
3.2. Stress and the LC-NE System
3.3. Stress and the PFC
3.4. Stress and Hippocampus
3.5. Stress and Amygdala
4. Neurobiological Links between Stress and TBI
4.1. TBI and Post-Injury Stress
4.2. TBI and Pre-Injury Stress
5. The Biomarkers of Stress
5.1. Stress and Neuroendocrine Factors
5.1.1. GCs
5.1.2. CRF
5.2. Stress and Neurotrophic Factors
5.2.1. BDNF
5.2.2. Vascular Endothelial Growth Factor (VEGF)
5.3. Stress and Neurotransmitters
5.3.1. DA
5.3.2. NE
5.3.3. Glu and GABA
5.4. Stress and Inflammatory Factors
5.4.1. IL-6
5.4.2. CRP
5.5. Stress and Oxidative Stress
5.5.1. ROS
5.5.2. MDA
6. Conclusions and Expectation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TBI | traumatic brain injury |
| PFC | prefrontal cortex |
| HPA | hypothalamic–pituitary–adrenal |
| LC-NE | locus coeruleus–norepinephrine |
| TNF | tumor necrosis factor |
| TLR | toll-like receptor |
| ROS | reactive oxygen species |
| RIPK | receptor interacting protein kinase |
| MLKL | mixed lineage kinase domain-like |
| ACC | anterior cingulate cortex |
| DG | dentate gyrus |
| mPFC | medial PFC |
| dPFC | dorsolateral PFC |
| BLA | basolateral amygdala |
| CeA | central amygdala |
| Glu | glutamate |
| γ-GABA | γ-aminobutyric acid |
| CeL | centrolateral |
| CeM | centromedial |
| snRNA-seq | single-nucleus RNA sequencing |
| CRH | corticotropin-releasing hormone |
| PVN | paraventricular nucleus |
| AVP | arginine vasopressin |
| ACTH | adrenocorticotropic hormone |
| GCs | glucocorticoids |
| MR | mineralocorticoid receptor |
| GR | glucocorticoid receptor |
| CNS | central nervous system |
| PNs | pyramidal neurons |
| PV | parvalbumin |
| SST | somatostatin |
| E/I | excitatory and inhibitory |
| SNARE | soluble N-ethylmaleimide-sensitive factor attachment protein receptor |
| NMDAR | N-methyl d-aspartate receptor |
| AMPAR | alpha-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptor |
| DA | dopamine |
| VTA | ventral tegmental area |
| D1R | D1 receptor |
| DEX | dexamethasone |
| FKBP5 | FK506-binding protein 5 |
| CRF | corticotropin releasing factor |
| PTSD | post-trauma brain injury |
| mFPI | mild fluid-percussion injury |
| BDNF | brain-derived neurotrophic factor |
| RS | restraint stress |
| CCI | controlled cortical injury |
| ERS | endoplasmic reticulum stress |
| RUS | repeated unpredictable stress |
| r-mTBI | repetitive mild TBI |
| rcTBI | repetitive concussive TBI |
| ETC | electron transport chain |
| PDH | pyruvate dehydrogenase |
| bTBI | blast-induced TBI |
| CK | creatine kinase |
| NF-H | neurofilaments-heavy |
| NSE | neuron-specific enolase |
| GFAP | glial fibrillary acidic protein |
| VEGF | vascular endothelial growth factor |
| SF | sleep fragmentation |
| HCC | hair cortisol concentrations |
| CHI | closed head injury |
| CVS | chronic variable stress |
| AST | attentional set-shifting test |
| sEPSCs | spontaneous excitatory postsynaptic currents |
| EPM | elevated plus maze |
| 5-HTP | 5-hydroxytryptophan |
| 5-HIAA | 5-hydroxyindoleacetic acid |
| CRS | chronic RS |
| BBB | blood–brain barrier |
| TrkB | tropomyosin-related kinase receptor |
| VEGF | vascular endothelial growth factor |
| SN | substantia nigra |
| CUMS | chronic unpredictable mild stress |
| RSDS | repeated social defeat stress |
| MDA | malondialdehyde |
| UCH-L1 | ubiquitin carboxy-terminal hydrolase L1 |
| DTI | diffusion tensor imaging |
| SWI | susceptibility weighted imaging |
| fMRI | functional MRI |
References
- Maas, A.I.R.; Menon, D.K.; Adelson, P.D.; Andelic, N.; Bell, M.J.; Belli, A.; Bragge, P.; Brazinova, A.; Büki, A.; Chesnut, R.M.; et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017, 16, 987–1048. [Google Scholar] [CrossRef]
- Feigin, V.L.; Theadom, A.; Barker-Collo, S.; Starkey, N.J.; McPherson, K.; Kahan, M.; Dowell, A.; Brown, P.; Parag, V.; Kydd, R.; et al. Incidence of traumatic brain injury in New Zealand: A population-based study. Lancet Neurol. 2013, 12, 53–64. [Google Scholar] [CrossRef]
- Jiang, J.-Y.; Gao, G.-Y.; Feng, J.-F.; Mao, Q.; Chen, L.-G.; Yang, X.-F.; Liu, J.-F.; Wang, Y.-H.; Qiu, B.-H.; Huang, X.-J. Traumatic brain injury in China. Lancet Neurol. 2019, 18, 286–295. [Google Scholar] [CrossRef]
- Howe, E.I.; Langlo, K.S.; Terjesen, H.C.A.; Røe, C.; Schanke, A.K.; Søberg, H.L.; Sveen, U.; Aas, E.; Enehaug, H.; Alves, D.E.; et al. Combined cognitive and vocational interventions after mild to moderate traumatic brain injury: Study protocol for a randomized controlled trial. Trials 2017, 18, 483. [Google Scholar] [CrossRef]
- Markovic, S.J.; Fitzgerald, M.; Peiffer, J.J.; Scott, B.R.; Rainey-Smith, S.R.; Sohrabi, H.R.; Brown, B.M. The impact of exercise, sleep, and diet on neurocognitive recovery from mild traumatic brain injury in older adults: A narrative review. Ageing Res. Rev. 2021, 68, 101322. [Google Scholar] [CrossRef]
- Fischer, J.T.; Bickart, K.C.; Giza, C.; Babikian, T. A Review of Family Environment and Neurobehavioral Outcomes Following Pediatric Traumatic Brain Injury: Implications of Early Adverse Experiences, Family Stress, and Limbic Development. Biol. Psychiatry 2022, 91, 488–497. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Liu, T.H.; He, Y.; Pan, H.Q.; Zhang, W.H.; Yin, X.P.; Tian, X.L.; Li, B.M.; Wang, X.D.; Holmes, A.; et al. Chronic Stress Remodels Synapses in an Amygdala Circuit-Specific Manner. Biol. Psychiatry 2019, 85, 189–201. [Google Scholar] [CrossRef]
- Merino, E.; Raya-Salom, D.; Teruel-Martí, V.; Adell, A.; Cervera-Ferri, A.; Martínez-Ricós, J. Effects of Acute Stress on the Oscillatory Activity of the Hippocampus–Amygdala–Prefrontal Cortex Network. Neuroscience 2021, 476, 72–89. [Google Scholar] [CrossRef]
- Kazakou, P.; Nicolaides, N.C.; Chrousos, G.P. Basic Concepts and Hormonal Regulators of the Stress System. Horm. Res. Paediatr. 2022. [Google Scholar] [CrossRef]
- Menon, D.K.; Schwab, K.; Wright, D.W.; Maas, A.I. Demographics and Clinical Assessment Working Group of the International and Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health. Position statement: Definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 2010, 91, 1637–1640. [Google Scholar] [CrossRef]
- Pavlovic, D.; Pekic, S.; Stojanovic, M.; Popovic, V. Traumatic brain injury: Neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary 2019, 22, 270–282. [Google Scholar] [CrossRef]
- Andriessen, T.M.; Jacobs, B.; Vos, P.E. Clinical characteristics and pathophysiological mechanisms of focal and diffuse traumatic brain injury. J. Cell. Mol. Med. 2010, 14, 2381–2392. [Google Scholar] [CrossRef]
- Pudenz, R.H.; Shelden, C.H. The Lucite Calvarium—A Method for Direct Observation of the Brain: II. Cranial Trauma and Brain Movement. J. Neurosurg. 1946, 3, 487–505. [Google Scholar] [CrossRef]
- McGinn, M.J.; Povlishock, J.T. Pathophysiology of Traumatic Brain Injury. Neurosurg. Clin. N. Am. 2016, 27, 397–407. [Google Scholar] [CrossRef]
- Stocchetti, N.; Carbonara, M.; Citerio, G.; Ercole, A.; Skrifvars, M.B.; Smielewski, P.; Zoerle, T.; Menon, D.K. Severe traumatic brain injury: Targeted management in the intensive care unit. Lancet Neurol. 2017, 16, 452–464. [Google Scholar] [CrossRef]
- Pearn, M.L.; Niesman, I.R.; Egawa, J.; Sawada, A.; Almenar-Queralt, A.; Shah, S.B.; Duckworth, J.L.; Head, B.P. Pathophysiology Associated with Traumatic Brain Injury: Current Treatments and Potential Novel Therapeutics. Cell. Mol. Neurobiol. 2017, 37, 571–585. [Google Scholar] [CrossRef]
- Wang, K.; Cui, D.M.; Gao, L. Traumatic brain injury: A review of characteristics, molecular basis and management. Front. Biosci. 2016, 21, 890–899. [Google Scholar]
- Sullivan, P.G.; Rabchevsky, A.G.; Waldmeier, P.C.; Springer, J.E. Mitochondrial permeability transition in CNS trauma: Cause or effect of neuronal cell death? J. Neurosci. Res. 2005, 79, 231–239. [Google Scholar] [CrossRef]
- Khatri, N.; Thakur, M.; Pareek, V.; Kumar, S.; Sharma, S.; Datusalia, K.A. Oxidative Stress: Major Threat in Traumatic Brain Injury. CNS Neurol. Disord. Drug Targets 2018, 17, 689–695. [Google Scholar] [CrossRef]
- Anthonymuthu, T.S.; Kenny, E.M.; Bayır, H. Therapies targeting lipid peroxidation in traumatic brain injury. Brain Res. 2016, 1640, 57–76. [Google Scholar] [CrossRef] [PubMed]
- Ladak, A.A.; Enam, S.A.; Ibrahim, M.T. A Review of the Molecular Mechanisms of Traumatic Brain Injury. World Neurosurg. 2019, 131, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Akamatsu, Y.; Hanafy, K.A. Cell Death and Recovery in Traumatic Brain Injury. Neurotherapeutics 2020, 17, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Wehn, A.C.; Khalin, I.; Duering, M.; Hellal, F.; Culmsee, C.; Vandenabeele, P.; Plesnila, N.; Terpolilli, N.A. RIPK1 or RIPK3 deletion prevents progressive neuronal cell death and improves memory function after traumatic brain injury. Acta Neuropathol. Commun. 2021, 9, 138. [Google Scholar] [CrossRef] [PubMed]
- Walker, K.R.; Tesco, G. Molecular mechanisms of cognitive dysfunction following traumatic brain injury. Front. Aging Neurosci. 2013, 5, 29. [Google Scholar] [CrossRef]
- Teasdale, G.; Jennett, B. Assessment of Coma and Impaired Consciousness. Lancet 1974, 304, 81–84. [Google Scholar] [CrossRef]
- Friedland, D.; Swash, M. Post-traumatic amnesia and confusional state: Hazards of retrospective assessment. J. Neurol. Neurosurg. Psychiatry 2016, 87, 1068–1074. [Google Scholar] [CrossRef]
- Rao, V.; Syeda, A.; Roy, D.; Peters, M.E.; Vaishnavi, S. Neuropsychiatric aspects of concussion: Acute and chronic sequelae. Concussion 2017, 2, CNC29. [Google Scholar] [CrossRef]
- Tucker, L.B.; Velosky, A.G.; McCabe, J.T. Applications of the Morris water maze in translational traumatic brain injury research. Neurosci. Biobehav. Rev. 2018, 88, 187–200. [Google Scholar] [CrossRef]
- Stocchetti, N.; Zanier, E.R. Chronic impact of traumatic brain injury on outcome and quality of life: A narrative review. Crit. Care 2016, 20, 148. [Google Scholar] [CrossRef]
- Rabinowitz, A.R.; Levin, H.S. Cognitive sequelae of traumatic brain injury. Psychiatr. Clin. N. Am. 2014, 37, 1–11. [Google Scholar] [CrossRef]
- Funahashi, S. Neuronal mechanisms of executive control by the prefrontal cortex. Neurosci. Res. 2001, 39, 147–165. [Google Scholar] [CrossRef]
- Levin, H.S.; Hanten, G. Executive functions after traumatic brain injury in children. Pediatr. Neurol. 2005, 33, 79–93. [Google Scholar] [CrossRef]
- Wood, R.L.; Worthington, A. Neurobehavioral Abnormalities Associated with Executive Dysfunction after Traumatic Brain Injury. Front. Behav. Neurosci. 2017, 11, 195. [Google Scholar] [CrossRef]
- Alexander, G.E.; DeLong, M.R.; Strick, P.L. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu. Rev. Neurosci. 1986, 9, 357–381. [Google Scholar] [CrossRef]
- De Simoni, S.; Jenkins, P.O.; Bourke, N.J.; Fleminger, J.J.; Hellyer, P.J.; Jolly, A.E.; Patel, M.C.; Cole, J.H.; Leech, R.; Sharp, D.J. Altered caudate connectivity is associated with executive dysfunction after traumatic brain injury. Brain 2018, 141, 148–164. [Google Scholar] [CrossRef]
- Bamford, I.J.; Bamford, N.S. The Striatum’s Role in Executing Rational and Irrational Economic Behaviors. Neuroscientist 2019, 25, 475–490. [Google Scholar] [CrossRef]
- Ketchesin, K.D.; Zong, W.; Hildebrand, M.A.; Seney, M.L.; Cahill, K.M.; Scott, M.R.; Shankar, V.G.; Glausier, J.R.; Lewis, D.A.; Tseng, G.C.; et al. Diurnal rhythms across the human dorsal and ventral striatum. Proc. Natl. Acad. Sci. USA 2021, 118, e2016150118. [Google Scholar] [CrossRef]
- McColgan, P.; Seunarine, K.K.; Razi, A.; Cole, J.H.; Gregory, S.; Durr, A.; Roos, R.A.; Stout, J.C.; Landwehrmeyer, B.; Scahill, R.I.; et al. Selective vulnerability of Rich Club brain regions is an organizational principle of structural connectivity loss in Huntington’s disease. Brain 2015, 138, 3327–3344. [Google Scholar] [CrossRef]
- Ndayisaba, A.; Jellinger, K.; Berger, T.; Wenning, G.K. TNFα inhibitors as targets for protective therapies in MSA: A viewpoint. J. Neuroinflamm. 2019, 16, 80. [Google Scholar] [CrossRef]
- Elliott, R. Executive functions and their disorders: Imaging in clinical neuroscience. Br. Med. Bull. 2003, 65, 49–59. [Google Scholar] [CrossRef]
- Mennes, M.; Vega Potler, N.; Kelly, C.; Di Martino, A.; Castellanos, F.X.; Milham, M.P. Resting state functional connectivity correlates of inhibitory control in children with attention-deficit/hyperactivity disorder. Front. Psychiatry 2011, 2, 83. [Google Scholar] [CrossRef] [PubMed]
- Paterno, R.; Folweiler, K.A.; Cohen, A.S. Pathophysiology and Treatment of Memory Dysfunction after Traumatic Brain Injury. Curr. Neurol. Neurosci. Rep. 2017, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Vakil, E.; Greenstein, Y.; Weiss, I.; Shtein, S. The Effects of Moderate-to-Severe Traumatic Brain Injury on Episodic Memory: A Meta-Analysis. Neuropsychol. Rev. 2019, 29, 270–287. [Google Scholar] [CrossRef] [PubMed]
- Le Fur, C.; Câmara-Costa, H.; Francillette, L.; Opatowski, M.; Toure, H.; Brugel, D.; Laurent-Vannier, A.; Meyer, P.; Watier, L.; Dellatolas, G.; et al. Executive functions and attention 7years after severe childhood traumatic brain injury: Results of the Traumatisme Grave de l’Enfant (TGE) cohort. Ann. Phys. Rehabil. Med. 2020, 63, 270–279. [Google Scholar] [CrossRef]
- Ornstein, T.J.; Sagar, S.; Schachar, R.J.; Ewing-Cobbs, L.; Chapman, S.B.; Dennis, M.; Saunders, A.E.; Yang, T.T.; Levin, H.S.; Max, J.E. Neuropsychological performance of youth with secondary attention-deficit/hyperactivity disorder 6- and 12-months after traumatic brain injury. J. Int. Neuropsychol. Soc. 2014, 20, 971–981. [Google Scholar] [CrossRef]
- Anderson, V.; Eren, S.; Dob, R.; Le Brocque, R.; Iselin, G.; Davern, T.J.; McKinlay, L.; Kenardy, J. Early Attention Impairment and Recovery Profiles After Childhood Traumatic Brain Injury. J. Head Trauma Rehabil. 2012, 27, 199–209. [Google Scholar] [CrossRef]
- Shah, S.A.; Goldin, Y.; Conte, M.M.; Goldfine, A.M.; Mohamadpour, M.; Fidali, B.C.; Cicerone, K.; Schiff, N.D. Executive attention deficits after traumatic brain injury reflect impaired recruitment of resources. NeuroImage Clin. 2017, 14, 233–241. [Google Scholar] [CrossRef]
- Cazalis, F.; Babikian, T.; Giza, C.; Copeland, S.; Hovda, D.; Asarnow, R.F. Pivotal role of anterior cingulate cortex in working memory after traumatic brain injury in youth. Front. Neurol. 2011, 1, 158. [Google Scholar] [CrossRef]
- Xuan, B.; Mackie, M.A.; Spagna, A.; Wu, T.; Tian, Y.; Hof, P.R.; Fan, J. The activation of interactive attentional networks. Neuroimage 2016, 129, 308–319. [Google Scholar] [CrossRef]
- Bush, G.; Luu, P.; Posner, M.I. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn. Sci. 2000, 4, 215–222. [Google Scholar] [CrossRef]
- Schneider, K.N.; Sciarillo, X.A.; Nudelman, J.L.; Cheer, J.F.; Roesch, M.R. Anterior Cingulate Cortex Signals Attention in a Social Paradigm that Manipulates Reward and Shock. Curr. Biol. 2020, 30, 3724–3735.e2. [Google Scholar] [CrossRef]
- Sheth, C.; Rogowska, J.; Legarreta, M.; McGlade, E.; Yurgelun-Todd, D. Functional connectivity of the anterior cingulate cortex in Veterans with mild traumatic brain injury. Behav. Brain Res. 2021, 396, 112882. [Google Scholar] [CrossRef]
- Whiting, M.D.; Hamm, R.J. Mechanisms of anterograde and retrograde memory impairment following experimental traumatic brain injury. Brain Res. 2008, 1213, 69–77. [Google Scholar] [CrossRef]
- Cowan, N. Chapter 20 What are the differences between long-term, short-term, and working memory? In Essence of Memory; Elsevier: Amsterdam, The Netherlands, 2008; pp. 323–338. [Google Scholar]
- Fortier-Lebel, O.; Jobin, B.; Lecuyer-Giguere, F.; Gaubert, M.; Giguere, J.F.; Gagnon, J.F.; Boller, B.; Frasnelli, J. Verbal Episodic Memory Alterations and Hippocampal Atrophy in Acute Mild Traumatic Brain Injury. J. Neurotrauma 2021, 38, 1506–1514. [Google Scholar] [CrossRef]
- Klooster, N.B.; Tranel, D.; Duff, M.C. The hippocampus and semantic memory over time. Brain Lang. 2020, 201, 104711. [Google Scholar] [CrossRef]
- Manns, J.R.; Hopkins, R.O.; Squire, L.R. Semantic Memory and the Human Hippocampus. Neuron 2003, 38, 127–133. [Google Scholar] [CrossRef]
- Van der Horn, H.J.; Liemburg, E.J.; Scheenen, M.E.; de Koning, M.E.; Marsman, J.B.; Spikman, J.M.; van der Naalt, J. Brain network dysregulation, emotion, and complaints after mild traumatic brain injury. Hum. Brain Mapp. 2016, 37, 1645–1654. [Google Scholar] [CrossRef]
- Simic, G.; Tkalcic, M.; Vukic, V.; Mulc, D.; Spanic, E.; Sagud, M.; Olucha-Bordonau, F.E.; Vuksic, M.; Hof, P.R. Understanding Emotions: Origins and Roles of the Amygdala. Biomolecules 2021, 11, 823. [Google Scholar] [CrossRef]
- Han, K.; Chapman, S.B.; Krawczyk, D.C. Altered Amygdala Connectivity in Individuals with Chronic Traumatic Brain Injury and Comorbid Depressive Symptoms. Front. Neurol. 2015, 6, 231. [Google Scholar] [CrossRef]
- Young, L.R.; Yu, W.; Holloway, M.; Rodgers, B.N.; Chapman, S.B.; Krawczyk, D.C. Amygdala activation as a marker for selective attention toward neutral faces in a chronic traumatic brain injury population. Neuropsychologia 2017, 104, 214–222. [Google Scholar] [CrossRef]
- Celeghin, A.; Galetto, V.; Tamietto, M.; Zettin, M. Emotion Recognition in Low-Spatial Frequencies Is Partly Preserved following Traumatic Brain Injury. BioMed Res. Int. 2019, 2019, 9562935. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.W.; Shiue, Y.L.; Liao, J.C.; Wee, H.Y.; Wang, C.C.; Chio, C.C.; Chang, C.H.; Hu, C.Y.; Kuo, J.R. Simvastatin Therapy in the Acute Stage of Traumatic Brain Injury Attenuates Brain Trauma-Induced Depression-Like Behavior in Rats by Reducing Neuroinflammation in the Hippocampus. Neurocrit. Care 2017, 26, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Silver, J.M.; McAllister, T.W.; Arciniegas, D.B. Depression and Cognitive Complaints Following Mild Traumatic Brain Injury. Am. J. Psychiatry 2009, 166, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Anand, A.; Li, Y.; Wang, Y.; Wu, J.; Gao, S.; Bukhari, L.; Mathews, V.P.; Kalnin, A.; Lowe, M.J. Activity and connectivity of brain mood regulating circuit in depression: A functional magnetic resonance study. Biol. Psychiatry 2005, 57, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Matthews, S.C.; Strigo, I.A.; Simmons, A.N.; Yang, T.T.; Paulus, M.P. Decreased functional coupling of the amygdala and supragenual cingulate is related to increased depression in unmedicated individuals with current major depressive disorder. J. Affect. Disord. 2008, 111, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Suckling, J.; Ooi, C.; Fu, C.H.; Williams, S.C.; Walsh, N.D.; Mitterschiffthaler, M.T.; Pich, E.M.; Bullmore, E. Functional coupling of the amygdala in depressed patients treated with antidepressant medication. Neuropsychopharmacology 2008, 33, 1909–1918. [Google Scholar] [CrossRef]
- Beitchman, J.A.; Griffiths, D.R.; Hur, Y.; Ogle, S.B.; Bromberg, C.E.; Morrison, H.W.; Lifshitz, J.; Adelson, P.D.; Thomas, T.C. Experimental Traumatic Brain Injury Induces Chronic Glutamatergic Dysfunction in Amygdala Circuitry Known to Regulate Anxiety-Like Behavior. Front. Neurosci. 2019, 13, 1434. [Google Scholar] [CrossRef]
- Figueiredo, T.H.; Harbert, C.L.; Pidoplichko, V.; Almeida-Suhett, C.P.; Pan, H.; Rossetti, K.; Braga, M.F.M.; Marini, A.M. Alpha-Linolenic Acid Treatment Reduces the Contusion and Prevents the Development of Anxiety-Like Behavior Induced by a Mild Traumatic Brain Injury in Rats. Mol. Neurobiol. 2018, 55, 187–200. [Google Scholar] [CrossRef]
- Treadway, M.T.; Waskom, M.L.; Dillon, D.G.; Holmes, A.J.; Park, M.T.M.; Chakravarty, M.M.; Dutra, S.J.; Polli, F.E.; Iosifescu, D.V.; Fava, M.; et al. Illness progression, recent stress, and morphometry of hippocampal subfields and medial prefrontal cortex in major depression. Biol. Psychiatry 2015, 77, 285–294. [Google Scholar] [CrossRef]
- Liu, W.; Ge, T.; Leng, Y.; Pan, Z.; Fan, J.; Yang, W.; Cui, R. The Role of Neural Plasticity in Depression: From Hippocampus to Prefrontal Cortex. Neural Plast. 2017, 2017, 6871089. [Google Scholar] [CrossRef]
- Jang, S.H.; Yi, J.H.; Kwon, H.G. Injury of the dorsolateral prefronto-thalamic tract in a patient with depression following mild traumatic brain injury: A case report. Medicine 2016, 95, e5009. [Google Scholar] [CrossRef]
- Palacios, E.M.; Sala-Llonch, R.; Junque, C.; Fernandez-Espejo, D.; Roig, T.; Tormos, J.M.; Bargallo, N.; Vendrell, P. Long-term declarative memory deficits in diffuse TBI: Correlations with cortical thickness, white matter integrity and hippocampal volume. Cortex 2013, 49, 646–657. [Google Scholar] [CrossRef]
- Bae, S.; Sheth, C.; Legarreta, M.; McGlade, E.; Lyoo, I.K.; Yurgelun-Todd, D.A. Volume and shape analysis of the Hippocampus and amygdala in veterans with traumatic brain injury and posttraumatic stress disorder. Brain Imaging Behav. 2020, 14, 1850–1864. [Google Scholar] [CrossRef]
- Janak, P.H.; Tye, K.M. From circuits to behaviour in the amygdala. Nature 2015, 517, 284–292. [Google Scholar] [CrossRef]
- Babaev, O.; Piletti Chatain, C.; Krueger-Burg, D. Inhibition in the amygdala anxiety circuitry. Exp. Mol. Med. 2018, 50, 1–16. [Google Scholar] [CrossRef]
- Orsini, C.A.; Maren, S. Neural and cellular mechanisms of fear and extinction memory formation. Neurosci. Biobehav. Rev. 2012, 36, 1773–1802. [Google Scholar] [CrossRef]
- Tye, K.M.; Prakash, R.; Kim, S.Y.; Fenno, L.E.; Grosenick, L.; Zarabi, H.; Thompson, K.R.; Gradinaru, V.; Ramakrishnan, C.; Deisseroth, K. Amygdala circuitry mediating reversible and bidirectional control of anxiety. Nature 2011, 471, 358–362. [Google Scholar] [CrossRef]
- Agoglia, A.E.; Herman, M.A. The center of the emotional universe: Alcohol, stress, and CRF1 amygdala circuitry. Alcohol 2018, 72, 61–73. [Google Scholar] [CrossRef]
- LeDoux, J.E. Emotion circuits in the brain. Annu. Rev. Neurosci. 2000, 23, 155–184. [Google Scholar] [CrossRef]
- Duvarci, S.; Pare, D. Amygdala microcircuits controlling learned fear. Neuron 2014, 82, 966–980. [Google Scholar] [CrossRef]
- Ehrlich, I.; Humeau, Y.; Grenier, F.; Ciocchi, S.; Herry, C.; Luthi, A. Amygdala inhibitory circuits and the control of fear memory. Neuron 2009, 62, 757–771. [Google Scholar] [CrossRef]
- Makkar, S.R.; Zhang, S.Q.; Cranney, J. Behavioral and neural analysis of GABA in the acquisition, consolidation, reconsolidation, and extinction of fear memory. Neuropsychopharmacology 2010, 35, 1625–1652. [Google Scholar] [CrossRef]
- Shi, Y.; Wu, X.; Zhou, J.; Cui, W.; Wang, J.; Hu, Q.; Zhang, S.; Han, L.; Zhou, M.; Luo, J.; et al. Single-Nucleus RNA Sequencing Reveals that Decorin Expression in the Amygdala Regulates Perineuronal Nets Expression and Fear Conditioning Response after Traumatic Brain Injury. Adv. Sci. 2022, 9, e2104112. [Google Scholar] [CrossRef]
- Ramlackhansingh, A.F.; Brooks, D.J.; Greenwood, R.J.; Bose, S.K.; Turkheimer, F.E.; Kinnunen, K.M.; Gentleman, S.; Heckemann, R.A.; Gunanayagam, K.; Gelosa, G.; et al. Inflammation after trauma: Microglial activation and traumatic brain injury. Ann. Neurol. 2011, 70, 374–383. [Google Scholar] [CrossRef]
- Johnson, V.E.; Stewart, J.E.; Begbie, F.D.; Trojanowski, J.Q.; Smith, D.H.; Stewart, W. Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain 2013, 136, 28–42. [Google Scholar] [CrossRef]
- The National Academies of Sciences, Engineering, and Medicine. Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans; The National Academies Press: Washington, DC, USA, 2019; p. 210. [Google Scholar]
- Bay, E.; de-Leon, M.B. Chronic Stress and Fatigue-Related Quality of Life After Mild to Moderate Traumatic Brain Injury. J. Head Trauma Rehabil. 2011, 26, 355–363. [Google Scholar] [CrossRef]
- Chrousos, G.P. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 2009, 5, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Dragoş, D.; Tănăsescu, M.D. The effect of stress on the defense systems. J. Med. Life 2010, 3, 10–18. [Google Scholar] [PubMed]
- McEwen, B.S.; Gianaros, P.J. Stress- and allostasis-induced brain plasticity. Annu. Rev. Med. 2011, 62, 431–445. [Google Scholar] [CrossRef] [PubMed]
- Joëls, M.; Pu, Z.; Wiegert, O.; Oitzl, M.S.; Krugers, H.J. Learning under stress: How does it work? Trends Cogn. Sci. 2006, 10, 152–158. [Google Scholar] [CrossRef]
- Liston, C.; Miller, M.M.; Goldwater, D.S.; Radley, J.J.; Rocher, A.B.; Hof, P.R.; Morrison, J.H.; McEwen, B.S. Stress-induced alterations in prefrontal cortical dendritic morphology predict selective impairments in perceptual attentional set-shifting. J. Neurosci. 2006, 26, 7870–7874. [Google Scholar] [CrossRef]
- Gameiro, G.H.; Gameiro, P.H.; da Silva Andrade, A.; Pereira, L.F.; Arthuri, M.T.; Marcondes, F.K.; de Arruda Veiga, M.C.F. Nociception- and anxiety-like behavior in rats submitted to different periods of restraint stress. Physiol. Behav. 2006, 87, 643–649. [Google Scholar] [CrossRef]
- Buynitsky, T.; Mostofsky, D.I. Restraint stress in biobehavioral research: Recent developments. Neurosci. Biobehav. Rev. 2009, 33, 1089–1098. [Google Scholar] [CrossRef]
- McEwen, B.S.; Gianaros, P.J. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann. N. Y. Acad. Sci. 2010, 1186, 190–222. [Google Scholar] [CrossRef]
- Herman, J.P.; McKlveen, J.M.; Ghosal, S.; Kopp, B.; Wulsin, A.; Makinson, R.; Scheimann, J.; Myers, B. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Compr. Physiol. 2016, 6, 603–621. [Google Scholar] [CrossRef]
- Herman, J.P.; Tasker, J.G. Paraventricular Hypothalamic Mechanisms of Chronic Stress Adaptation. Front. Endocrinol. 2016, 7, 137. [Google Scholar] [CrossRef]
- Joels, M. Corticosteroids and the brain. J. Endocrinol. 2018, 238, R121–R130. [Google Scholar] [CrossRef]
- Jankord, R.; Herman, J.P. Limbic regulation of hypothalamo-pituitary-adrenocortical function during acute and chronic stress. Ann. N. Y. Acad. Sci. 2008, 1148, 64–73. [Google Scholar] [CrossRef]
- Ding, X.F.; Zhao, X.H.; Tao, Y.; Zhong, W.C.; Fan, Q.; Diao, J.X.; Liu, Y.L.; Chen, Y.Y.; Chen, J.X.; Lv, Z.P. Xiao Yao San Improves Depressive-Like Behaviors in Rats with Chronic Immobilization Stress through Modulation of Locus Coeruleus-Norepinephrine System. Evid. Based Complement. Altern. Med. 2014, 2014, 605914. [Google Scholar] [CrossRef]
- Schwarz, L.A.; Luo, L. Organization of the locus coeruleus-norepinephrine system. Curr. Biol. 2015, 25, R1051–R1056. [Google Scholar] [CrossRef]
- Arnsten, A.F. Through the looking glass: Differential noradenergic modulation of prefrontal cortical function. Neural Plast. 2000, 7, 133–146. [Google Scholar] [CrossRef]
- Benarroch, E.E. Locus coeruleus. Cell Tissue Res. 2018, 373, 221–232. [Google Scholar] [CrossRef]
- Harris, K.D.; Shepherd, G.M.G. The neocortical circuit: Themes and variations. Nat. Neurosci. 2015, 18, 170–181. [Google Scholar] [CrossRef]
- McKlveen, J.M.; Moloney, R.D.; Scheimann, J.R.; Myers, B.; Herman, J.P. “Braking” the Prefrontal Cortex: The Role of Glucocorticoids and Interneurons in Stress Adaptation and Pathology. Biol. Psychiatry 2019, 86, 669–681. [Google Scholar] [CrossRef]
- McKlveen, J.M.; Myers, B.; Herman, J.P. The medial prefrontal cortex: Coordinator of autonomic, neuroendocrine and behavioural responses to stress. J. Neuroendocrinol. 2015, 27, 446–456. [Google Scholar] [CrossRef]
- McKlveen, J.M.; Morano, R.L.; Fitzgerald, M.; Zoubovsky, S.; Cassella, S.N.; Scheimann, J.R.; Ghosal, S.; Mahbod, P.; Packard, B.A.; Myers, B.; et al. Chronic Stress Increases Prefrontal Inhibition: A Mechanism for Stress-Induced Prefrontal Dysfunction. Biol. Psychiatry 2016, 80, 754–764. [Google Scholar] [CrossRef]
- Popoli, M.; Yan, Z.; McEwen, B.S.; Sanacora, G. The stressed synapse: The impact of stress and glucocorticoids on glutamate transmission. Nat. Rev. Neurosci. 2011, 13, 22–37. [Google Scholar] [CrossRef]
- Musazzi, L.; Milanese, M.; Farisello, P.; Zappettini, S.; Tardito, D.; Barbiero, V.S.; Bonifacino, T.; Mallei, A.; Baldelli, P.; Racagni, G.; et al. Acute stress increases depolarization-evoked glutamate release in the rat prefrontal/frontal cortex: The dampening action of antidepressants. PLoS ONE 2010, 5, e8566. [Google Scholar] [CrossRef]
- Yuen, E.Y.; Wei, J.; Liu, W.; Zhong, P.; Li, X.; Yan, Z. Repeated stress causes cognitive impairment by suppressing glutamate receptor expression and function in prefrontal cortex. Neuron 2012, 73, 962–977. [Google Scholar] [CrossRef]
- Segovia, G.; del Arco, A.; Mora, F. Environmental enrichment, prefrontal cortex, stress, and aging of the brain. J. Neural Transm. 2009, 116, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Xing, B.; Li, Y.-C.; Gao, W.-J. Norepinephrine versus dopamine and their interaction in modulating synaptic function in the prefrontal cortex. Brain Res. 2016, 1641, 217–233. [Google Scholar] [CrossRef]
- Arnsten, A.F.T. Stress signalling pathways that impair prefrontal cortex structure and function. Nat. Rev. Neurosci. 2009, 10, 410–422. [Google Scholar] [CrossRef] [PubMed]
- Aston-Jones, G.; Cohen, J.D. An integrative theory of locus coeruleus-norepinephrine function: Adaptive Gain and Optimal Performance. Annu. Rev. Neurosci. 2005, 28, 403–450. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, S.; Gobeske, K.T.; Auerbach, J.; Taylor, J.R.; Arnsten, A.F.T. A role for norepinephrine in stress-induced cognitive deficits: α-1-adrenoceptor mediation in the prefrontal cortex. Biol. Psychiatry 1999, 46, 1266–1274. [Google Scholar] [CrossRef]
- Ramos, B.P.; Arnsten, A.F.T. Adrenergic pharmacology and cognition: Focus on the prefrontal cortex. Pharmacol. Ther. 2007, 113, 523–536. [Google Scholar] [CrossRef]
- Murphy, B.L.; Arnsten, A.F.; Goldman-Rakic, P.S.; Roth, R.H. Increased dopamine turnover in the prefrontal cortex impairs spatial working memory performance in rats and monkeys. Proc. Natl. Acad. Sci. USA 1996, 93, 1325–1329. [Google Scholar] [CrossRef]
- Mizoguchi, K.; Yuzurihara, M.; Ishige, A.; Sasaki, H.; Chui, D.-H.; Tabira, T. Chronic Stress Induces Impairment of Spatial Working Memory Because of Prefrontal Dopaminergic Dysfunction. J. Neurosci. 2000, 20, 1568–1574. [Google Scholar] [CrossRef]
- Lupien, S.J.; Maheu, F.; Tu, M.; Fiocco, A.; Schramek, T.E. The effects of stress and stress hormones on human cognition: Implications for the field of brain and cognition. Brain Cogn. 2007, 65, 209–237. [Google Scholar] [CrossRef]
- Chaouloff, F.; Groc, L. Temporal modulation of hippocampal excitatory transmission by corticosteroids and stress. Front. Neuroendocrinol. 2011, 32, 25–42. [Google Scholar] [CrossRef]
- Gugustea, R.; Jia, Z. Genetic manipulations of AMPA glutamate receptors in hippocampal synaptic plasticity. Neuropharmacology 2021, 194, 108630. [Google Scholar] [CrossRef]
- Kauer, J.A.; Malenka, R.C.; Nicoll, R.A. NMDA application potentiates synaptic transmission in the hippocampus. Nature 1988, 334, 250–252. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, J.B.; Conrad, C.D. The impact from the aftermath of chronic stress on hippocampal structure and function: Is there a recovery? Front. Neuroendocrinol. 2018, 49, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Gould, E.; Tanapat, P. Stress and hippocampal neurogenesis. Biol. Psychiatry 1999, 46, 1472–1479. [Google Scholar] [CrossRef]
- Fuchs, E.; Flügge, G.; Ohl, F.; Lucassen, P.; Vollmann-Honsdorf, G.K.; Michaelis, T. Psychosocial stress, glucocorticoids, and structural alterations in the tree shrew hippocampus. Physiol. Behav. 2001, 73, 285–291. [Google Scholar] [CrossRef]
- Vyas, A.; Pillai, A.G.; Chattarji, S. Recovery after chronic stress fails to reverse amygdaloid neuronal hypertrophy and enhanced anxiety-like behavior. Neuroscience 2004, 128, 667–673. [Google Scholar] [CrossRef]
- Conrad, C.D.; Ortiz, J.B.; Judd, J.M. Chronic stress and hippocampal dendritic complexity: Methodological and functional considerations. Physiol. Behav. 2017, 178, 66–81. [Google Scholar] [CrossRef]
- Zhang, X.; Ge, T.T.; Yin, G.; Cui, R.; Zhao, G.; Yang, W. Stress-Induced Functional Alterations in Amygdala: Implications for Neuropsychiatric Diseases. Front. Neurosci. 2018, 12, 367. [Google Scholar] [CrossRef]
- Winklewski, P.J.; Radkowski, M.; Wszedybyl-Winklewska, M.; Demkow, U. Stress Response, Brain Noradrenergic System and Cognition. Adv. Exp. Med. Biol. 2017, 980, 67–74. [Google Scholar] [CrossRef]
- Liu, W.Z.; Zhang, W.H.; Zheng, Z.H.; Zou, J.X.; Liu, X.X.; Huang, S.H.; You, W.J.; He, Y.; Zhang, J.Y.; Wang, X.D.; et al. Identification of a prefrontal cortex-to-amygdala pathway for chronic stress-induced anxiety. Nat. Commun. 2020, 11, 2221. [Google Scholar] [CrossRef]
- Vyas, A.; Mitra, R.; Shankaranarayana Rao, B.S.; Chattarji, S. Chronic Stress Induces Contrasting Patterns of Dendritic Remodeling in Hippocampal and Amygdaloid Neurons. J. Neurosci. 2002, 22, 6810–6818. [Google Scholar] [CrossRef]
- Sawamura, T.; Klengel, T.; Armario, A.; Jovanovic, T.; Norrholm, S.D.; Ressler, K.J.; Andero, R. Dexamethasone Treatment Leads to Enhanced Fear Extinction and Dynamic Fkbp5 Regulation in Amygdala. Neuropsychopharmacology 2016, 41, 832–846. [Google Scholar] [CrossRef] [PubMed]
- Rainnie, D.G.; Bergeron, R.; Sajdyk, T.J.; Patil, M.; Gehlert, D.R.; Shekhar, A. Corticotrophin releasing factor-induced synaptic plasticity in the amygdala translates stress into emotional disorders. J. Neurosci. 2004, 24, 3471–3479. [Google Scholar] [CrossRef]
- Lankford, K.L.; Letourneau, P.C. Evidence that calcium may control neurite outgrowth by regulating the stability of actin filaments. J. Cell Biol. 1989, 109, 1229–1243. [Google Scholar] [CrossRef]
- Taylor, A.N.; Rahman, S.U.; Tio, D.L.; Sanders, M.J.; Bando, J.K.; Truong, A.H.; Prolo, P. Lasting Neuroendocrine-Immune Effects of Traumatic Brain Injury in Rats. J. Neurotrauma 2006, 23, 1802–1813. [Google Scholar] [CrossRef]
- Tapp, Z.M.; Godbout, J.P.; Kokiko-Cochran, O.N. A Tilted Axis: Maladaptive Inflammation and HPA Axis Dysfunction Contribute to Consequences of TBI. Front. Neurol. 2019, 10, 345. [Google Scholar] [CrossRef]
- Juruena, M.F.; Eror, F.; Cleare, A.J.; Young, A.H. The Role of Early Life Stress in HPA Axis and Anxiety. In Anxiety Disorders: Rethinking and Understanding Recent Discoveries; Kim, Y.-K., Ed.; Springer: Singapore, 2020; pp. 141–153. [Google Scholar]
- Griesbach, G.S.; Vincelli, J.; Tio, D.L.; Hovda, D.A. Effects of acute restraint-induced stress on glucocorticoid receptors and brain-derived neurotrophic factor after mild traumatic brain injury. Neuroscience 2012, 210, 393–402. [Google Scholar] [CrossRef]
- Rowe, R.K.; Ortiz, J.B.; Thomas, T.C. Mild and Moderate Traumatic Brain Injury and Repeated Stress Affect Corticosterone in the Rat. Neurotrauma Rep. 2020, 1, 113–124. [Google Scholar] [CrossRef]
- Gao, C.; Chen, X.; Xu, H.; Guo, H.; Zheng, L.; Yan, Y.N.; Ren, Z.; Luo, C.; Gao, Y.; Wang, Z.; et al. Restraint Stress Delays the Recovery of Neurological Impairments and Exacerbates Brain Damages through Activating Endoplasmic Reticulum Stress-mediated Neurodegeneration/Autophagy/Apopotosis post Moderate Traumatic Brain Injury. Mol. Neurobiol. 2022, 59, 1560–1576. [Google Scholar] [CrossRef]
- Algamal, M.; Saltiel, N.; Pearson, A.J.; Ager, B.; Burca, I.; Mouzon, B.; Diamond, D.M.; Mullan, M.; Ojo, J.O.; Crawford, F. Impact of Repetitive Mild Traumatic Brain Injury on Behavioral and Hippocampal Deficits in a Mouse Model of Chronic Stress. J. Neurotrauma 2019, 36, 2590–2607. [Google Scholar] [CrossRef]
- Klemenhagen, K.C.; O’Brien, S.P.; Brody, D.L. Repetitive concussive traumatic brain injury interacts with post-injury foot shock stress to worsen social and depression-like behavior in mice. PLoS ONE 2013, 8, e74510. [Google Scholar] [CrossRef]
- Xing, G.; Barry, E.S.; Benford, B.; Grunberg, N.E.; Li, H.; Watson, W.D.; Sharma, P. Impact of repeated stress on traumatic brain injury-induced mitochondrial electron transport chain expression and behavioral responses in rats. Front. Neurol. 2013, 4, 196. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.K.; Kovesdi, E.; Gyorgy, A.B.; Wingo, D.; Kamnaksh, A.; Walker, J.; Long, J.B.; Agoston, D.V. Stress and traumatic brain injury: A behavioral, proteomics, and histological study. Front. Neurol. 2011, 2, 12. [Google Scholar] [CrossRef] [PubMed]
- Doulames, V.M.; Vilcans, M.; Lee, S.; Shea, T.B. Social interaction attenuates the extent of secondary neuronal damage following closed head injury in mice. Front. Behav. Neurosci. 2015, 9, 275. [Google Scholar] [CrossRef] [PubMed]
- Khodaie, B.; Lotfinia, A.A.; Ahmadi, M.; Lotfinia, M.; Jafarian, M.; Karimzadeh, F.; Coulon, P.; Gorji, A. Structural and functional effects of social isolation on the hippocampus of rats with traumatic brain injury. Behav. Brain Res. 2015, 278, 55–65. [Google Scholar] [CrossRef]
- Griesbach, G.S.; Tio, D.L.; Vincelli, J.; McArthur, D.L.; Taylor, A.N. Differential effects of voluntary and forced exercise on stress responses after traumatic brain injury. J. Neurotrauma 2012, 29, 1426–1433. [Google Scholar] [CrossRef]
- Tapp, Z.M.; Cornelius, S.; Oberster, A.; Kumar, J.E.; Atluri, R.; Witcher, K.G.; Oliver, B.; Bray, C.; Velasquez, J.; Zhao, F.; et al. Sleep fragmentation engages stress-responsive circuitry, enhances inflammation and compromises hippocampal function following traumatic brain injury. Exp. Neurol. 2022, 353, 114058. [Google Scholar] [CrossRef]
- Ramos-Cejudo, J.; Genfi, A.; Abu-Amara, D.; Debure, L.; Qian, M.; Laska, E.; Siegel, C.; Milton, N.; Newman, J.; Blessing, E.; et al. CRF serum levels differentiate PTSD from healthy controls and TBI in military veterans. Psychiatr. Res. Clin. Pract. 2021, 3, 153–162. [Google Scholar] [CrossRef]
- Fesharaki-Zadeh, A.; Miyauchi, J.T.; St Laurent-Arriot, K.; Tsirka, S.E.; Bergold, P.J. Increased Behavioral Deficits and Inflammation in a Mouse Model of Co-Morbid Traumatic Brain Injury and Post-Traumatic Stress Disorder. ASN Neuro 2020, 12, 1759091420979567. [Google Scholar] [CrossRef]
- Sanchez, C.M.; Titus, D.J.; Wilson, N.M.; Freund, J.E.; Atkins, C.M. Early Life Stress Exacerbates Outcome after Traumatic Brain Injury. J. Neurotrauma 2021, 38, 555–565. [Google Scholar] [CrossRef]
- Lajud, N.; Roque, A.; Cheng, J.P.; Bondi, C.O.; Kline, A.E. Early Life Stress Preceding Mild Pediatric Traumatic Brain Injury Increases Neuroinflammation but Does Not Exacerbate Impairment of Cognitive Flexibility during Adolescence. J. Neurotrauma 2021, 38, 411–421. [Google Scholar] [CrossRef]
- Diaz-Chavez, A.; Lajud, N.; Roque, A.; Cheng, J.P.; Melendez-Herrera, E.; Valdez-Alarcon, J.J.; Bondi, C.O.; Kline, A.E. Early life stress increases vulnerability to the sequelae of pediatric mild traumatic brain injury. Exp. Neurol. 2020, 329, 113318. [Google Scholar] [CrossRef]
- Klein, R.C.; Acheson, S.K.; Qadri, L.H.; Dawson, A.A.; Rodriguiz, R.M.; Wetsel, W.C.; Moore, S.D.; Laskowitz, D.T.; Dawson, H.N. Opposing effects of traumatic brain injury on excitatory synaptic function in the lateral amygdala in the absence and presence of preinjury stress. J. Neurosci. Res. 2016, 94, 579–589. [Google Scholar] [CrossRef]
- Davies, D.R.; Olson, D.; Meyer, D.L.; Scholl, J.L.; Watt, M.J.; Manzerra, P.; Renner, K.J.; Forster, G.L. Mild Traumatic Brain Injury with Social Defeat Stress Alters Anxiety, Contextual Fear Extinction, and Limbic Monoamines in Adult Rats. Front. Behav. Neurosci. 2016, 10, 71. [Google Scholar] [CrossRef]
- Stam, R. PTSD and stress sensitisation: A tale of brain and body: Part 1: Human studies. Neurosci. Biobehav. Rev. 2007, 31, 530–557. [Google Scholar] [CrossRef]
- Daskalakis, N.P.; Provost, A.C.; Hunter, R.G.; Guffanti, G. Noncoding RNAs: Stress, Glucocorticoids, and Posttraumatic Stress Disorder. Biol. Psychiatry 2018, 83, 849–865. [Google Scholar] [CrossRef]
- Molaie, A.M.; Maguire, J. Neuroendocrine Abnormalities Following Traumatic Brain Injury: An Important Contributor to Neuropsychiatric Sequelae. Front. Endocrinol. 2018, 9, 176. [Google Scholar] [CrossRef]
- Steudte-Schmiedgen, S.; Stalder, T.; Schönfeld, S.; Wittchen, H.-U.; Trautmann, S.; Alexander, N.; Miller, R.; Kirschbaum, C. Hair cortisol concentrations and cortisol stress reactivity predict PTSD symptom increase after trauma exposure during military deployment. Psychoneuroendocrinology 2015, 59, 123–133. [Google Scholar] [CrossRef]
- Salberg, S.; Sgro, M.; Brady, R.D.; Noel, M.; Mychasiuk, R. The Development of Adolescent Chronic Pain following Traumatic Brain Injury and Surgery: The Role of Diet and Early Life Stress. Dev. Neurosci. 2020, 42, 2–11. [Google Scholar] [CrossRef]
- Algamal, M.; Pearson, A.J.; Hahn-Townsend, C.; Burca, I.; Mullan, M.; Crawford, F.; Ojo, J.O. Repeated unpredictable stress and social isolation induce chronic HPA axis dysfunction and persistent abnormal fear memory. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110035. [Google Scholar] [CrossRef]
- Mourtzi, N.; Sertedaki, A.; Charmandari, E. Glucocorticoid Signaling and Epigenetic Alterations in Stress-Related Disorders. Int. J. Mol. Sci. 2021, 22, 5964. [Google Scholar] [CrossRef]
- De Kloet, E.R.; Meijer, O.C.; de Nicola, A.F.; de Rijk, R.H.; Joels, M. Importance of the brain corticosteroid receptor balance in metaplasticity, cognitive performance and neuro-inflammation. Front. Neuroendocrinol. 2018, 49, 124–145. [Google Scholar] [CrossRef] [PubMed]
- Raul, J.S.; Cirimele, V.; Ludes, B.; Kintz, P. Detection of physiological concentrations of cortisol and cortisone in human hair. Clin. Biochem. 2004, 37, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Iob, E.; Steptoe, A. Cardiovascular Disease and Hair Cortisol: A Novel Biomarker of Chronic Stress. Curr. Cardiol. Rep. 2019, 21, 116. [Google Scholar] [CrossRef] [PubMed]
- Dedic, N.; Chen, A.; Deussing, J.M. The CRF Family of Neuropeptides and their Receptors—Mediators of the Central Stress Response. Curr. Mol. Pharmacol. 2018, 11, 4–31. [Google Scholar] [CrossRef]
- Wisłowska-Stanek, A.; Lehner, M.; Skórzewska, A.; Krząścik, P.; Płaźnik, A. Behavioral effects and CRF expression in brain structures of high- and low-anxiety rats after chronic restraint stress. Behav. Brain Res. 2016, 310, 26–35. [Google Scholar] [CrossRef]
- Futch, H.S.; McFarland, K.N.; Moore, B.D.; Kuhn, M.Z.; Giasson, B.I.; Ladd, T.B.; Scott, K.A.; Shapiro, M.R.; Nosacka, R.L.; Goodwin, M.S.; et al. An anti-CRF antibody suppresses the HPA axis and reverses stress-induced phenotypes. J. Exp. Med. 2019, 216, 2479–2491. [Google Scholar] [CrossRef]
- Schmidt, H.D.; Banasr, M.; Duman, R.S. Future Antidepressant Targets: Neurotrophic Factors and Related Signaling Cascades. Drug Discov. Today Ther. Strateg. 2008, 5, 151–156. [Google Scholar] [CrossRef]
- Nobis, A.; Zalewski, D.; Waszkiewicz, N. Peripheral Markers of Depression. J. Clin. Med. 2020, 9, 3793. [Google Scholar] [CrossRef]
- Zhang, J.C.; Yao, W.; Hashimoto, K. Brain-derived Neurotrophic Factor (BDNF)-TrkB Signaling in Inflammation-related Depression and Potential Therapeutic Targets. Curr. Neuropharmacol. 2016, 14, 721–731. [Google Scholar] [CrossRef]
- Kojima, M.; Matsui, K.; Mizui, T. BDNF pro-peptide: Physiological mechanisms and implications for depression. Cell Tissue Res. 2019, 377, 73–79. [Google Scholar] [CrossRef]
- Duman, R.S. BDNF, 5-HT, and Anxiety: Identification of a Critical Periadolescent Developmental Period. Am. J. Psychiatry 2017, 174, 1137–1139. [Google Scholar] [CrossRef]
- Pan, W.; Banks, W.A.; Fasold, M.B.; Bluth, J.; Kastin, A.J. Transport of brain-derived neurotrophic factor across the blood–brain barrier. Neuropharmacology 1998, 37, 1553–1561. [Google Scholar] [CrossRef]
- Karege, F.; Perret, G.; Bondolfi, G.; Schwald, M.; Bertschy, G.; Aubry, J.-M. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002, 109, 143–148. [Google Scholar] [CrossRef]
- Klein, A.B.; Williamson, R.; Santini, M.A.; Clemmensen, C.; Ettrup, A.; Rios, M.; Knudsen, G.M.; Aznar, S. Blood BDNF concentrations reflect brain-tissue BDNF levels across species. Int. J. Neuropsychopharmacol. 2011, 14, 347–353. [Google Scholar] [CrossRef]
- Leal, G.; Bramham, C.R.; Duarte, C.B. Chapter Eight—BDNF and Hippocampal Synaptic Plasticity. In Vitamins and Hormones; Litwack, G., Ed.; Academic Press: Cambridge, MA, USA, 2017; Volume 104, pp. 153–195. [Google Scholar]
- Bennett, M.R.; Lagopoulos, J. Stress and trauma: BDNF control of dendritic-spine formation and regression. Prog. Neurobiol. 2014, 112, 80–99. [Google Scholar] [CrossRef]
- Domingues, M.; Casaril, A.M.; Birmann, P.T.; Bampi, S.R.; Lourenço, D.d.A.; Vieira, B.M.; Dapper, L.H.; Lenardão, E.J.; Sonego, M.; Collares, T.; et al. Effects of a selanylimidazopyridine on the acute restraint stress-induced depressive- and anxiety-like behaviors and biological changes in mice. Behav. Brain Res. 2019, 366, 96–107. [Google Scholar] [CrossRef]
- Ma, Z.; Wang, G.; Cui, L.; Wang, Q. Myricetin Attenuates Depressant-Like Behavior in Mice Subjected to Repeated Restraint Stress. Int. J. Mol. Sci. 2015, 16, 28377–28385. [Google Scholar] [CrossRef]
- St-Cyr, S.; McGowan, P.O. Programming of stress-related behavior and epigenetic neural gene regulation in mice offspring through maternal exposure to predator odor. Front. Behav. Neurosci. 2015, 9, 145. [Google Scholar] [CrossRef]
- Lakshminarasimhan, H.; Chattarji, S. Stress leads to contrasting effects on the levels of brain derived neurotrophic factor in the hippocampus and amygdala. PLoS ONE 2012, 7, e30481. [Google Scholar] [CrossRef]
- Ieraci, A.; Mallei, A.; Musazzi, L.; Popoli, M. Physical exercise and acute restraint stress differentially modulate hippocampal brain-derived neurotrophic factor transcripts and epigenetic mechanisms in mice. Hippocampus 2015, 25, 1380–1392. [Google Scholar] [CrossRef]
- Luoni, A.; Berry, A.; Raggi, C.; Bellisario, V.; Cirulli, F.; Riva, M.A. Sex-Specific Effects of Prenatal Stress on Bdnf Expression in Response to an Acute Challenge in Rats: A Role for Gadd45β. Mol. Neurobiol. 2016, 53, 7037–7047. [Google Scholar] [CrossRef] [PubMed]
- Sun, P.; Wei, S.; Wei, X.; Wang, J.; Zhang, Y.; Qiao, M.; Wu, J. Anger Emotional Stress Influences VEGF/VEGFR2 and Its Induced PI3K/AKT/mTOR Signaling Pathway. Neural Plast. 2016, 2016, 4129015. [Google Scholar] [CrossRef] [PubMed]
- Heine, V.M.; Zareno, J.; Maslam, S.; Joëls, M.; Lucassen, P.J. Chronic stress in the adult dentate gyrus reduces cell proliferation near the vasculature and VEGF and Flk-1 protein expression. Eur. J. Neurosci. 2005, 21, 1304–1314. [Google Scholar] [CrossRef] [PubMed]
- Elfving, B.; Jakobsen, J.L.; Madsen, J.C.B.; Wegener, G.; Müller, H.K. Chronic restraint stress increases the protein expression of VEGF and its receptor VEGFR-2 in the prefrontal cortex. Synapse 2015, 69, 190–194. [Google Scholar] [CrossRef]
- Uysal, N.; Sisman, A.R.; Dayi, A.; Ozbal, S.; Cetin, F.; Baykara, B.; Aksu, I.; Tas, A.; Cavus, S.A.; Gonenc-Arda, S.; et al. Acute footshock-stress increases spatial learning–memory and correlates to increased hippocampal BDNF and VEGF and cell numbers in adolescent male and female rats. Neurosci. Lett. 2012, 514, 141–146. [Google Scholar] [CrossRef]
- Baik, J.-H. Stress and the dopaminergic reward system. Exp. Mol. Med. 2020, 52, 1879–1890. [Google Scholar] [CrossRef]
- Mesman, S.; Smidt, M.P. Acquisition of the Midbrain Dopaminergic Neuronal Identity. Int. J. Mol. Sci. 2020, 21, 4638. [Google Scholar] [CrossRef]
- Cabib, S.; Puglisi-Allegra, S. The mesoaccumbens dopamine in coping with stress. Neurosci. Biobehav. Rev. 2012, 36, 79–89. [Google Scholar] [CrossRef]
- Holly, E.N.; Miczek, K.A. Ventral tegmental area dopamine revisited: Effects of acute and repeated stress. Psychopharmacology 2016, 233, 163–186. [Google Scholar] [CrossRef]
- Cao, G.; Meng, G.; Zhu, L.; Zhu, J.; Dong, N.; Zhou, X.; Zhang, S.; Zhang, Y. Susceptibility to chronic immobilization stress-induced depressive-like behaviour in middle-aged female mice and accompanying changes in dopamine D1 and GABA(A) receptors in related brain regions. Behav. Brain Funct. 2021, 17. [Google Scholar] [CrossRef]
- Mangiavacchi, S.; Masi, F.; Scheggi, S.; Leggio, B.; De Montis, M.G.; Gambarana, C. Long-term behavioral and neurochemical effects of chronic stress exposure in rats. J. Neurochem. 2001, 79, 1113–1121. [Google Scholar] [CrossRef]
- Perez-Caballero, L.; Torres-Sanchez, S.; Romero-López-Alberca, C.; González-Saiz, F.; Mico, J.A.; Berrocoso, E. Monoaminergic system and depression. Cell Tissue Res. 2019, 377, 107–113. [Google Scholar] [CrossRef]
- Sanchez, A. Changes in norepinephrine and epinephrine concentrations in adrenal gland of the rats submitted to acute immobilization stress. Pharmacol. Res. 2003, 48, 607–613. [Google Scholar] [CrossRef]
- Tillage, R.P.; Foster, S.L.; Lustberg, D.; Liles, L.C.; McCann, K.E.; Weinshenker, D. Co-released norepinephrine and galanin act on different timescales to promote stress-induced anxiety-like behavior. Neuropsychopharmacology 2021, 46, 1535–1543. [Google Scholar] [CrossRef]
- Yang, H.-L.; Li, M.-M.; Zhou, M.-F.; Xu, H.-S.; Huan, F.; Liu, N.; Gao, R.; Wang, J.; Zhang, N.; Jiang, L. Links Between Gut Dysbiosis and Neurotransmitter Disturbance in Chronic Restraint Stress-Induced Depressive Behaviours: The Role of Inflammation. Inflammation 2021, 44, 2448–2462. [Google Scholar] [CrossRef]
- Sahoo, S.; Kharkar, P.S.; Sahu, N.U.; Brijesh, S. Anxiolytic activity of Psidium guajava in mice subjected to chronic restraint stress and effect on neurotransmitters in brain. Phytother. Res. 2021, 35, 1399–1415. [Google Scholar] [CrossRef]
- Patterson-Buckendahl, P.; Pohorecky, L.A.; Kubovcakova, L.; Krizanova, O.; Martin, R.B.; Martinez, D.A.; Kvetňanský, R. Ethanol and Stress Activate Catecholamine Synthesis in the Adrenal. Ann. N. Y. Acad. Sci. 2008, 1148, 542–551. [Google Scholar] [CrossRef]
- Yamaguchi, N.; Kakinuma, Y.; Yakura, T.; Naito, M.; Okada, S. Glucose infusion suppresses acute restraint stress-induced peripheral and central sympathetic responses in rats. Auton. Neurosci. 2022, 239, 102957. [Google Scholar] [CrossRef]
- Zhang, Z.-Q.; Wang, X.; Xue, B.-H.; Zhao, Y.; Xie, F.; Wang, S.-D.; Xue, C.; Wang, Y.; Zhang, Y.-S.; Qian, L.-J. Chronic stress promotes glioma cell proliferation via the PI3K/Akt signaling pathway. Oncol. Rep. 2021, 46, 202. [Google Scholar] [CrossRef]
- Sears, S.M.; Hewett, S.J. Influence of glutamate and GABA transport on brain excitatory/inhibitory balance. Exp. Biol. Med. 2021, 246, 1069–1083. [Google Scholar] [CrossRef]
- Shaye, H.; Stauch, B.; Gati, C.; Cherezov, V. Molecular mechanisms of metabotropic GABA(B) receptor function. Sci. Adv. 2021, 7. [Google Scholar] [CrossRef] [PubMed]
- Roy, U.; Stute, L.; Höfling, C.; Hartlage-Rübsamen, M.; Matysik, J.; Roβner, S.; Alia, A. Sex- and age-specific modulation of brain GABA levels in a mouse model of Alzheimer’s disease. Neurobiol. Aging 2018, 62, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Shirayama, Y.; Takahashi, M.; Osone, F.; Hara, A.; Okubo, T. Myo-inositol, Glutamate, and Glutamine in the Prefrontal Cortex, Hippocampus, and Amygdala in Major Depression. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2017, 2, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Venero, C.; Borrell, J. Rapid glucocorticoid effects on excitatory amino acid levels in the hippocampus: A microdialysis study in freely moving rats. Eur. J. Neurosci. 1999, 11, 2465–2473. [Google Scholar] [CrossRef]
- Yuen, E.Y.; Liu, W.; Karatsoreos, I.N.; Feng, J.; McEwen, B.S.; Yan, Z. Acute stress enhances glutamatergic transmission in prefrontal cortex and facilitates working memory. Proc. Natl. Acad. Sci. USA 2009, 106, 14075–14079. [Google Scholar] [CrossRef]
- Ma, K.; Xu, A.; Cui, S.; Sun, M.R.; Xue, Y.C.; Wang, J.H. Impaired GABA synthesis, uptake and release are associated with depression-like behaviors induced by chronic mild stress. Transl. Psychiatry 2016, 6, e910. [Google Scholar] [CrossRef]
- Umamaheswaran, S.; Dasari, S.K.; Yang, P.; Lutgendorf, S.K.; Sood, A.K. Stress, inflammation, and eicosanoids: An emerging perspective. Cancer Metastasis Rev. 2018, 37, 203–211. [Google Scholar] [CrossRef]
- Elenkov, I.J. Neurohormonal-cytokine interactions: Implications for inflammation, common human diseases and well-being. Neurochem. Int. 2008, 52, 40–51. [Google Scholar] [CrossRef]
- Busillo, J.M.; Azzam, K.M.; Cidlowski, J.A. Glucocorticoids sensitize the innate immune system through regulation of the NLRP3 inflammasome. J. Biol. Chem. 2011, 286, 38703–38713. [Google Scholar] [CrossRef]
- Miller, A.H.; Maletic, V.; Raison, C.L. Inflammation and its discontents: The role of cytokines in the pathophysiology of major depression. Biol. Psychiatry 2009, 65, 732–741. [Google Scholar] [CrossRef]
- Amin, S.N.; Hassan, S.S.; Khashaba, A.S.; Youakim, M.F.; Latif, N.S.A.; Rashed, L.A.; Yassa, H.D. Hippocampal and Cerebellar Changes in Acute Restraint Stress and the Impact of Pretreatment with Ceftriaxone. Brain Sci. 2020, 10, 193. [Google Scholar] [CrossRef]
- Jankord, R.; Zhang, R.; Flak, J.N.; Solomon, M.B.; Albertz, J.; Herman, J.P. Stress activation of IL-6 neurons in the hypothalamus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R343. [Google Scholar] [CrossRef]
- Zhu, Y.; Klomparens, E.A.; Guo, S.; Geng, X. Neuroinflammation caused by mental stress: The effect of chronic restraint stress and acute repeated social defeat stress in mice. Neurol. Res. 2019, 41, 762–769. [Google Scholar] [CrossRef]
- Menard, C.; Pfau, M.L.; Hodes, G.E.; Kana, V.; Wang, V.X.; Bouchard, S.; Takahashi, A.; Flanigan, M.E.; Aleyasin, H.; LeClair, K.B.; et al. Social stress induces neurovascular pathology promoting depression. Nat. Neurosci. 2017, 20, 1752–1760. [Google Scholar] [CrossRef]
- Noushad, S.; Ahmed, S.; Ansari, B.; Mustafa, U.-H.; Saleem, Y.; Hazrat, H. Physiological biomarkers of chronic stress: A systematic review. Int. J. Health Sci. 2021, 15, 46–59. [Google Scholar]
- Wright, K.P., Jr.; Drake, A.L.; Frey, D.J.; Fleshner, M.; Desouza, C.A.; Gronfier, C.; Czeisler, C.A. Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain Behav. Immun. 2015, 47, 24–34. [Google Scholar] [CrossRef]
- Blossom, V.; Gokul, M.; Kumar, N.A.; Kini, R.D.; Nayak, S.; Bhagyalakshmi, K. Chronic unpredictable stress-induced inflammation and quantitative analysis of neurons of distinct brain regions in Wistar rat model of comorbid depression. Vet. World 2020, 13, 1870–1874. [Google Scholar] [CrossRef]
- Cobley, J.N.; Fiorello, M.L.; Bailey, D.M. 13 reasons why the brain is susceptible to oxidative stress. Redox Biol. 2018, 15, 490–503. [Google Scholar] [CrossRef]
- Huang, T.T.; Leu, D.; Zou, Y. Oxidative stress and redox regulation on hippocampal-dependent cognitive functions. Arch. Biochem. Biophys. 2015, 576, 2–7. [Google Scholar] [CrossRef]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017, 2017, 8416763. [Google Scholar] [CrossRef]
- Marrocco, I.; Altieri, F.; Peluso, I. Measurement and Clinical Significance of Biomarkers of Oxidative Stress in Humans. Oxid. Med. Cell. Longev. 2017, 2017, 6501046. [Google Scholar] [CrossRef]
- Zhang, H.; Wei, M.; Sun, Q.; Yang, T.; Lu, X.; Feng, X.; Song, M.; Cui, L.; Fan, H. Lycopene ameliorates chronic stress-induced hippocampal injury and subsequent learning and memory dysfunction through inhibiting ROS/JNK signaling pathway in rats. Food Chem. Toxicol. 2020, 145, 111688. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Lee, J.-S.; Kim, H.-G.; Kim, W.-Y.; Lee, S.-B.; Choi, Y.-H.; Son, C.-G. The ethanol extract of Aquilariae Lignum ameliorates hippocampal oxidative stress in a repeated restraint stress mouse model. BMC Complement. Altern. Med. 2017, 17, 397. [Google Scholar] [CrossRef]
- Novaes, L.S.; dos Santos, N.B.; Dragunas, G.; Perfetto, J.G.; Leza, J.C.; Scavone, C.; Munhoz, C.D. Repeated Restraint Stress Decreases Na, K-ATPase Activity via Oxidative and Nitrosative Damage in the Frontal Cortex of Rats. Neuroscience 2018, 393, 273–283. [Google Scholar] [CrossRef]
- Colaianna, M.; Schiavone, S.; Zotti, M.; Tucci, P.; Morgese, M.G.; Bäckdahl, L.; Holmdahl, R.; Krause, K.-H.; Cuomo, V.; Trabace, L. Neuroendocrine profile in a rat model of psychosocial stress: Relation to oxidative stress. Antioxid. Redox Signal. 2013, 18, 1385–1399. [Google Scholar] [CrossRef]
- Tebay, L.E.; Robertson, H.; Durant, S.T.; Vitale, S.R.; Penning, T.M.; Dinkova-Kostova, A.T.; Hayes, J.D. Mechanisms of activation of the transcription factor Nrf2 by redox stressors, nutrient cues, and energy status and the pathways through which it attenuates degenerative disease. Free Radic. Biol. Med. 2015, 88, 108–146. [Google Scholar] [CrossRef]
- MacDowell, K.S.; Caso, J.R.; Martín-Hernández, D.; Moreno, B.M.; Madrigal, J.L.M.; Micó, J.A.; Leza, J.C.; García-Bueno, B. The Atypical Antipsychotic Paliperidone Regulates Endogenous Antioxidant/Anti-Inflammatory Pathways in Rat Models of Acute and Chronic Restraint Stress. Neurotherapeutics 2016, 13, 833–843. [Google Scholar] [CrossRef]
- Tsikas, D. Assessment of lipid peroxidation by measuring malondialdehyde (MDA) and relatives in biological samples: Analytical and biological challenges. Anal. Biochem. 2017, 524, 13–30. [Google Scholar] [CrossRef]
- Su, L.J.; Zhang, J.H.; Gomez, H.; Murugan, R.; Hong, X.; Xu, D.; Jiang, F.; Peng, Z.Y. Reactive Oxygen Species-Induced Lipid Peroxidation in Apoptosis, Autophagy, and Ferroptosis. Oxid. Med. Cell. Longev. 2019, 2019, 5080843. [Google Scholar] [CrossRef]
- Salehi, A.; Rabiei, Z.; Setorki, M. Effect of gallic acid on chronic restraint stress-induced anxiety and memory loss in male BALB/c mice. Iran J. Basic Med. Sci. 2018, 21, 1232–1237. [Google Scholar] [CrossRef]
- Samarghandian, S.; Samini, F.; Azimi-Nezhad, M.; Farkhondeh, T. Anti-oxidative effects of safranal on immobilization-induced oxidative damage in rat brain. Neurosci. Lett. 2017, 659, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Mazereeuw, G.; Herrmann, N.; Andreazza, A.C.; Khan, M.M.; Lanctôt, K.L. A meta-analysis of lipid peroxidation markers in major depression. Neuropsychiatr. Dis. Treat. 2015, 11, 2479–2491. [Google Scholar] [CrossRef] [PubMed]
- Abdelhak, A.; Foschi, M.; Abu-Rumeileh, S.; Yue, J.K.; D’Anna, L.; Huss, A.; Oeckl, P.; Ludolph, A.C.; Kuhle, J.; Petzold, A.; et al. Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nat. Rev. Neurol. 2022, 18, 158–172. [Google Scholar] [CrossRef] [PubMed]
- Bouvier, D.; Oris, C.; Brailova, M.; Durif, J.; Sapin, V. Interest of blood biomarkers to predict lesions in medical imaging in the context of mild traumatic brain injury. Clin. Biochem. 2020, 85, 5–11. [Google Scholar] [CrossRef]
| Stress Models | TBI Models | Neurological Impairments and Mechanisms | References |
|---|---|---|---|
| RS/DEX # | mFPI | Hippocampus GR ↑; Hippocampus pro-BDNF ↓. | [139] |
| RS # | FPI | Plasma corticosterone level at the acute stage post-stressor initiation ↑. | [140] |
| CRS # | Moderate CCI | Motor deficits and cognitive impairment ↑; Anxiety-like behaviors and lesion volume ↑; BBB leakage, ERS, apoptosis, and autophagy ↑. | [141] |
| RUS # | r-mTBI | Traumatic memory impairments and anxiety-like and passive stress-coping behaviors ↓; Dendritic spine GluN2A/GluN2B ratio ↓; Pro-BDNF level in the hippocampus ↓; Astrogliosis in the corpus callosum ↑. | [142] |
| Foot shock # | rcTBI | Cognitive impairments ↑; Depression-like behaviors ↑. | [143] |
| Repeated immobilization and tail-shock stress # | mFPI | Anxiety and memory impairments ↑; Abnormal mitochondrial ETC complex and PDH enzyme expressions in hippocampus. | [144] |
| Repetitive unpredictable stressors # | bTBI | Anxiety-like behaviors ↑; Spatial memory impairments ↑; Corticosterone, CK-BB, NF-H, NSE, GFAP, and VEGF in the blood serum and the above protein levels in the hippocampus and the PFC ↑. | [145] |
| Social isolation # | CHI | Cognitive impairment ↑; Serum corticosterone ↑; Corticosterone ↑. | [146] |
| Social isolation # | A penetrating injury | Memory impairments ↑; Dark neurons and apoptotic cells in the hippocampal CA3 region ↑. | [147] |
| Forced wheel exercise # | FPI | Plasma corticosterone and ACTH ↑. | [148] |
| SF # | FPI | The upstream regulator NR3C1 that encodes GR ↓; Cortical microgliosis ↑; Pro-inflammatory glial signaling genes ↑; Neuronal activity in the hippocampus ↑; Neuronal activity in PVN ↓; Hippocampal-dependent cognition ↓. | [149] |
| PTSD (human) # | TBI | CRF ↓. | [150] |
| PTSD # | CHI | Behavioral impairments and neuroinflammation ↑; Microglia number in DG, CA1, and CA3 ↑. | [151] |
| Maternal separation @ | FPI | Hippocampal-dependent learning deficits ↑; Cortical atrophy ↑; GCs in blood serum ↑. | [152] |
| Maternal separation @ | Mild CCI | Executive function (-); Hippocampal IL-1β ↑; Plasma corticosterone level ↑. | [153] |
| Maternal separation @ | CCI | Spatial learning and memory deficits ↓; Contralateral CA1 microglial activation ↑. | [154] |
| Foot shock @ | CCI | sEPSC in lateral amygdala pyramidal-like neurons ↓. | [155] |
| Social defeat @ | Mild CCI | Anxiety-like behaviors ↑; 5-HTP and 5-HIAA in hippocampus and amygdala ↑; DA in dorsal hippocampus ↑; NE in the amygdala ↑. | [156] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, L.; Pang, Q.; Xu, H.; Guo, H.; Liu, R.; Wang, T. The Neurobiological Links between Stress and Traumatic Brain Injury: A Review of Research to Date. Int. J. Mol. Sci. 2022, 23, 9519. https://doi.org/10.3390/ijms23179519
Zheng L, Pang Q, Xu H, Guo H, Liu R, Wang T. The Neurobiological Links between Stress and Traumatic Brain Injury: A Review of Research to Date. International Journal of Molecular Sciences. 2022; 23(17):9519. https://doi.org/10.3390/ijms23179519
Chicago/Turabian StyleZheng, Lexin, Qiuyu Pang, Heng Xu, Hanmu Guo, Rong Liu, and Tao Wang. 2022. "The Neurobiological Links between Stress and Traumatic Brain Injury: A Review of Research to Date" International Journal of Molecular Sciences 23, no. 17: 9519. https://doi.org/10.3390/ijms23179519
APA StyleZheng, L., Pang, Q., Xu, H., Guo, H., Liu, R., & Wang, T. (2022). The Neurobiological Links between Stress and Traumatic Brain Injury: A Review of Research to Date. International Journal of Molecular Sciences, 23(17), 9519. https://doi.org/10.3390/ijms23179519





