The Role of RNA-Binding Proteins in Hematological Malignancies
Abstract
1. Introduction
2. RNA-Binding Proteins
3. mRNA Regulation by RBPs
3.1. mRNA 5′ Capping
3.2. Splicing of Pre-mRNAs
3.3. Cleavage and 3′ End Formation
3.4. mRNA Export
3.5. mRNA Stability
3.6. Translation
3.7. RNA Editing
4. RNA-Binding Proteins in Hematological Malignancies
4.1. RBM39–mRNA Splicing
4.2. Musashi Proteins (MSI1 and MSI2)-mRNA Translation
4.3. IGF2BP3–mRNA Localization, mRNA Stability and mRNA Degradation
4.4. hnRNP K–mRNA Localization, Transcription, Translation and Splicing
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Swerdlow, S.C.E.; Harris, N.; Jaffe, E.; Pileri, S.; Stein, H.; Thiele, J.; Vardiman, J. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th ed.; World Health Organization: Geneva, Switzerland, 2017.
- Global Cancer Observatory. Available online: https://gco.iarc.fr/ (accessed on 6 August 2022).
- Keykhaei, M.; Masinaei, M.; Mohammadi, E.; Azadnajafabad, S.; Rezaei, N.; Saeedi Moghaddam, S.; Rezaei, N.; Nasserinejad, M.; Abbasi-Kangevari, M.; Malekpour, M.R.; et al. A global, regional, and national survey on burden and Quality of Care Index (QCI) of hematologic malignancies; global burden of disease systematic analysis 1990–2017. Exp. Hematol. Oncol. 2021, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Pulte, D.; Jansen, L.; Brenner, H. Changes in long term survival after diagnosis with common hematologic malignancies in the early 21st century. Blood Cancer J. 2020, 10, 56. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Liu, D. Antibody-drug conjugates in clinical trials for lymphoid malignancies and multiple myeloma. J. Hematol. Oncol. 2019, 12, 94. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Liu, M.; Zhang, Y.; Wang, X. Bispecific T cell engagers: An emerging therapy for management of hematologic malignancies. J. Hematol. Oncol. 2021, 14, 75. [Google Scholar] [CrossRef]
- Allahyari, H.; Heidari, S.; Ghamgosha, M.; Saffarian, P.; Amani, J. Immunotoxin: A new tool for cancer therapy. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2017, 39, 1010428317692226. [Google Scholar] [CrossRef]
- Salik, B.; Smyth, M.J.; Nakamura, K. Targeting immune checkpoints in hematological malignancies. J. Hematol. Oncol. 2020, 13, 111. [Google Scholar] [CrossRef]
- Gill, S.; Brudno, J.N. CAR T-Cell Therapy in Hematologic Malignancies: Clinical Role, Toxicity, and Unanswered Questions. Am. Soc. Clin. Oncol. Educ. Book. Am. Soc. Clin. Oncol. Annu. Meet. 2021, 41, 1–20. [Google Scholar] [CrossRef]
- Lamb, M.G.; Rangarajan, H.G.; Tullius, B.P.; Lee, D.A. Natural killer cell therapy for hematologic malignancies: Successes, challenges, and the future. Stem Cell Res. Ther. 2021, 12, 211. [Google Scholar] [CrossRef]
- Pinto, V.; Bergantim, R.; Caires, H.R.; Seca, H.; Guimaraes, J.E.; Vasconcelos, M.H. Multiple Myeloma: Available Therapies and Causes of Drug Resistance. Cancers 2020, 12, 407. [Google Scholar] [CrossRef]
- Zhang, J.; Gu, Y.; Chen, B. Mechanisms of drug resistance in acute myeloid leukemia. OncoTargets Ther. 2019, 12, 1937–1945. [Google Scholar] [CrossRef] [PubMed]
- Camicia, R.; Winkler, H.C.; Hassa, P.O. Novel drug targets for personalized precision medicine in relapsed/refractory diffuse large B-cell lymphoma: A comprehensive review. Mol. Cancer 2015, 14, 207. [Google Scholar] [CrossRef] [PubMed]
- Glisovic, T.; Bachorik, J.L.; Yong, J.; Dreyfuss, G. RNA-binding proteins and post-transcriptional gene regulation. FEBS Lett. 2008, 582, 1977–1986. [Google Scholar] [CrossRef] [PubMed]
- Hodson, D.J.; Screen, M.; Turner, M. RNA-binding proteins in hematopoiesis and hematological malignancy. Blood 2019, 133, 2365–2373. [Google Scholar] [CrossRef]
- Zandhuis, N.D.; Nicolet, B.P.; Wolkers, M.C. RNA-Binding Protein Expression Alters Upon Differentiation of Human B Cells and T Cells. Front. Immunol. 2021, 12, 717324. [Google Scholar] [CrossRef]
- Feng, M.; Xie, X.; Han, G.; Zhang, T.; Li, Y.; Li, Y.; Yin, R.; Wang, Q.; Zhang, T.; Wang, P.; et al. YBX1 is required for maintaining myeloid leukemia cell survival by regulating BCL2 stability in an m6A-dependent manner. Blood 2021, 138, 71–85. [Google Scholar] [CrossRef]
- Lovci, M.T.; Bengtson, M.H.; Massirer, K.B. Post-Translational Modifications and RNA-Binding Proteins. Adv. Exp. Med. Biol. 2016, 907, 297–317. [Google Scholar] [CrossRef]
- Carotenuto, P.; Pecoraro, A.; Palma, G.; Russo, G.; Russo, A. Therapeutic Approaches Targeting Nucleolus in Cancer. Cells 2019, 8, 1090. [Google Scholar] [CrossRef]
- Gallardo, M.; Lee, H.J.; Zhang, X.; Bueso-Ramos, C.; Pageon, L.R.; McArthur, M.; Multani, A.; Nazha, A.; Manshouri, T.; Parker-Thornburg, J.; et al. hnRNP K Is a Haploinsufficient Tumor Suppressor that Regulates Proliferation and Differentiation Programs in Hematologic Malignancies. Cancer Cell 2015, 28, 486–499. [Google Scholar] [CrossRef]
- Gallardo, M.; Malaney, P.; Aitken, M.J.L.; Zhang, X.; Link, T.M.; Shah, V.; Alybayev, S.; Wu, M.H.; Pageon, L.R.; Ma, H.; et al. Uncovering the Role of RNA-Binding Protein hnRNP K in B-Cell Lymphomas. J. Natl. Cancer Inst. 2020, 112, 95–106. [Google Scholar] [CrossRef]
- Anantharaman, V.; Koonin, E.V.; Aravind, L. Comparative genomics and evolution of proteins involved in RNA metabolism. Nucleic Acids Res. 2002, 30, 1427–1464. [Google Scholar] [CrossRef] [PubMed]
- Hentze, M.W.; Castello, A.; Schwarzl, T.; Preiss, T. A brave new world of RNA-binding proteins. Nat. Rev. Mol. Cell Biol. 2018, 19, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Van Nostrand, E.L.; Freese, P.; Pratt, G.A.; Wang, X.; Wei, X.; Xiao, R.; Blue, S.M.; Chen, J.Y.; Cody, N.A.L.; Dominguez, D.; et al. A large-scale binding and functional map of human RNA-binding proteins. Nature 2020, 583, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Lukong, K.E.; Chang, K.W.; Khandjian, E.W.; Richard, S. RNA-binding proteins in human genetic disease. Trends Genet. TIG 2008, 24, 416–425. [Google Scholar] [CrossRef]
- Valverde, R.; Edwards, L.; Regan, L. Structure and function of KH domains. FEBS J. 2008, 275, 2712–2726. [Google Scholar] [CrossRef]
- Du, Z.; Lee, J.K.; Fenn, S.; Tjhen, R.; Stroud, R.M.; James, T.L. X-ray crystallographic and NMR studies of protein-protein and protein-nucleic acid interactions involving the KH domains from human poly(C)-binding protein-2. RNA 2007, 13, 1043–1051. [Google Scholar] [CrossRef]
- Bomsztyk, K.; Denisenko, O.; Ostrowski, J. hnRNP K: One protein multiple processes. BioEssays News Rev. Mol. Cell. Dev. Biol. 2004, 26, 629–638. [Google Scholar] [CrossRef]
- Shibata, R.; Bessho, Y.; Shinkai, A.; Nishimoto, M.; Fusatomi, E.; Terada, T.; Shirouzu, M.; Yokoyama, S. Crystal structure and RNA-binding analysis of the archaeal transcription factor NusA. Biochem. Biophys. Res. Commun. 2007, 355, 122–128. [Google Scholar] [CrossRef]
- Daubner, G.M.; Brummer, A.; Tocchini, C.; Gerhardy, S.; Ciosk, R.; Zavolan, M.; Allain, F.H. Structural and functional implications of the QUA2 domain on RNA recognition by GLD-1. Nucleic Acids Res. 2014, 42, 8092–8105. [Google Scholar] [CrossRef]
- Teplova, M.; Malinina, L.; Darnell, J.C.; Song, J.; Lu, M.; Abagyan, R.; Musunuru, K.; Teplov, A.; Burley, S.K.; Darnell, R.B.; et al. Protein-RNA and protein-protein recognition by dual KH1/2 domains of the neuronal splicing factor Nova-1. Structure 2011, 19, 930–944. [Google Scholar] [CrossRef]
- Lewis, H.A.; Musunuru, K.; Jensen, K.B.; Edo, C.; Chen, H.; Darnell, R.B.; Burley, S.K. Sequence-specific RNA binding by a Nova KH domain: Implications for paraneoplastic disease and the fragile X syndrome. Cell 2000, 100, 323–332. [Google Scholar] [CrossRef]
- Baber, J.L.; Libutti, D.; Levens, D.; Tjandra, N. High precision solution structure of the C-terminal KH domain of heterogeneous nuclear ribonucleoprotein K, a c-myc transcription factor. J. Mol. Biol. 1999, 289, 949–962. [Google Scholar] [CrossRef] [PubMed]
- Oberstrass, F.C.; Auweter, S.D.; Erat, M.; Hargous, Y.; Henning, A.; Wenter, P.; Reymond, L.; Amir-Ahmady, B.; Pitsch, S.; Black, D.L.; et al. Structure of PTB bound to RNA: Specific binding and implications for splicing regulation. Science 2005, 309, 2054–2057. [Google Scholar] [CrossRef]
- Agrawal, A.A.; Salsi, E.; Chatrikhi, R.; Henderson, S.; Jenkins, J.L.; Green, M.R.; Ermolenko, D.N.; Kielkopf, C.L. An extended U2AF(65)-RNA-binding domain recognizes the 3’ splice site signal. Nat. Commun. 2016, 7, 10950. [Google Scholar] [CrossRef]
- Okuwaki, M.; Saotome-Nakamura, A.; Yoshimura, M.; Saito, S.; Hirawake-Mogi, H.; Sekiya, T.; Nagata, K. RNA-recognition motifs and glycine and arginine-rich region cooperatively regulate the nucleolar localization of nucleolin. J. Biochem. 2021, 169, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Hargous, Y.; Hautbergue, G.M.; Tintaru, A.M.; Skrisovska, L.; Golovanov, A.P.; Stevenin, J.; Lian, L.Y.; Wilson, S.A.; Allain, F.H. Molecular basis of RNA recognition and TAP binding by the SR proteins SRp20 and 9G8. EMBO J. 2006, 25, 5126–5137. [Google Scholar] [CrossRef]
- Dominguez, C.; Allain, F.H. NMR structure of the three quasi RNA recognition motifs (qRRMs) of human hnRNP F and interaction studies with Bcl-x G-tract RNA: A novel mode of RNA recognition. Nucleic Acids Res. 2006, 34, 3634–3645. [Google Scholar] [CrossRef]
- Krepl, M.; Blatter, M.; Clery, A.; Damberger, F.F.; Allain, F.H.T.; Sponer, J. Structural study of the Fox-1 RRM protein hydration reveals a role for key water molecules in RRM-RNA recognition. Nucleic Acids Res. 2017, 45, 8046–8063. [Google Scholar] [CrossRef]
- Zearfoss, N.R.; Deveau, L.M.; Clingman, C.C.; Schmidt, E.; Johnson, E.S.; Massi, F.; Ryder, S.P. A conserved three-nucleotide core motif defines Musashi RNA binding specificity. J. Biol. Chem. 2014, 289, 35530–35541. [Google Scholar] [CrossRef]
- Bussiere, D.E.; Xie, L.; Srinivas, H.; Shu, W.; Burke, A.; Be, C.; Zhao, J.; Godbole, A.; King, D.; Karki, R.G.; et al. Structural basis of indisulam-mediated RBM39 recruitment to DCAF15 E3 ligase complex. Nat. Chem. Biol. 2020, 16, 15–23. [Google Scholar] [CrossRef]
- Berg, J.M.; Godwin, H.A. Lessons from zinc-binding peptides. Annu. Rev. Biophys. Biomol. Struct. 1997, 26, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Hale, M.A.; Richardson, J.I.; Day, R.C.; McConnell, O.L.; Arboleda, J.; Wang, E.T.; Berglund, J.A. An engineered RNA binding protein with improved splicing regulation. Nucleic Acids Res. 2018, 46, 3152–3168. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Searles, M.A.; Klug, A. Crystal structure of a zinc-finger-RNA complex reveals two modes of molecular recognition. Nature 2003, 426, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Loughlin, F.E.; Mansfield, R.E.; Vaz, P.M.; McGrath, A.P.; Setiyaputra, S.; Gamsjaeger, R.; Chen, E.S.; Morris, B.J.; Guss, J.M.; Mackay, J.P. The zinc fingers of the SR-like protein ZRANB2 are single-stranded RNA-binding domains that recognize 5’ splice site-like sequences. Proc. Natl. Acad. Sci. USA 2009, 106, 5581–5586. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Barraud, P. Functions of double-stranded RNA-binding domains in nucleocytoplasmic transport. RNA Biol. 2014, 11, 1226–1232. [Google Scholar] [CrossRef]
- Brooks, R.; Eckmann, C.R.; Jantsch, M.F. The double-stranded RNA-binding domains of Xenopus laevis ADAR1 exhibit different RNA-binding behaviors. FEBS Lett. 1998, 434, 121–126. [Google Scholar] [CrossRef]
- Doyle, M.; Badertscher, L.; Jaskiewicz, L.; Guttinger, S.; Jurado, S.; Hugenschmidt, T.; Kutay, U.; Filipowicz, W. The double-stranded RNA binding domain of human Dicer functions as a nuclear localization signal. RNA 2013, 19, 1238–1252. [Google Scholar] [CrossRef]
- Wang, S.; Hu, Y.; Overgaard, M.T.; Karginov, F.V.; Uhlenbeck, O.C.; McKay, D.B. The domain of the Bacillus subtilis DEAD-box helicase YxiN that is responsible for specific binding of 23S rRNA has an RNA recognition motif fold. RNA 2006, 12, 959–967. [Google Scholar] [CrossRef]
- Lorsch, J.R.; Herschlag, D. The DEAD box protein eIF4A. 2. A cycle of nucleotide and RNA-dependent conformational changes. Biochemistry 1998, 37, 2194–2206. [Google Scholar] [CrossRef]
- Bates, G.J.; Nicol, S.M.; Wilson, B.J.; Jacobs, A.M.; Bourdon, J.C.; Wardrop, J.; Gregory, D.J.; Lane, D.P.; Perkins, N.D.; Fuller-Pace, F.V. The DEAD box protein p68: A novel transcriptional coactivator of the p53 tumour suppressor. EMBO J. 2005, 24, 543–553. [Google Scholar] [CrossRef]
- Gustafson, E.A.; Wessel, G.M. DEAD-box helicases: Posttranslational regulation and function. Biochem. Biophys. Res. Commun. 2010, 395, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zamore, P.D.; Hall, T.M. Crystal structure of a Pumilio homology domain. Mol. Cell 2001, 7, 855–865. [Google Scholar] [CrossRef]
- Wang, M.; Oge, L.; Perez-Garcia, M.D.; Hamama, L.; Sakr, S. The PUF Protein Family: Overview on PUF RNA Targets, Biological Functions, and Post Transcriptional Regulation. Int. J. Mol. Sci. 2018, 19, 410. [Google Scholar] [CrossRef]
- Oberstrass, F.C.; Lee, A.; Stefl, R.; Janis, M.; Chanfreau, G.; Allain, F.H. Shape-specific recognition in the structure of the Vts1p SAM domain with RNA. Nat. Struct. Mol. Biol. 2006, 13, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Ou, H.D.; Lohr, F.; Vogel, V.; Mantele, W.; Dotsch, V. Structural evolution of C-terminal domains in the p53 family. EMBO J. 2007, 26, 3463–3473. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Hota, P.K.; Chugha, P.; Guo, H.; Miao, H.; Zhang, L.; Kim, S.J.; Stetzik, L.; Wang, B.C.; Buck, M. NMR structure of a heterodimeric SAM:SAM complex: Characterization and manipulation of EphA2 binding reveal new cellular functions of SHIP2. Structure 2012, 20, 41–55. [Google Scholar] [CrossRef]
- Fu, X.D.; Ares, M., Jr. Context-dependent control of alternative splicing by RNA-binding proteins. Nat. Rev. Genet. 2014, 15, 689–701. [Google Scholar] [CrossRef]
- Muller-McNicoll, M.; Neugebauer, K.M. How cells get the message: Dynamic assembly and function of mRNA-protein complexes. Nat. Rev. Genet. 2013, 14, 275–287. [Google Scholar] [CrossRef]
- Keene, J.D. Minireview: Global regulation and dynamics of ribonucleic Acid. Endocrinology 2010, 151, 1391–1397. [Google Scholar] [CrossRef]
- Raghavan, A.; Ogilvie, R.L.; Reilly, C.; Abelson, M.L.; Raghavan, S.; Vasdewani, J.; Krathwohl, M.; Bohjanen, P.R. Genome-wide analysis of mRNA decay in resting and activated primary human T lymphocytes. Nucleic Acids Res. 2002, 30, 5529–5538. [Google Scholar] [CrossRef]
- Gebauer, F.; Hentze, M.W. Molecular mechanisms of translational control. Nat. Rev. Mol. Cell Biol. 2004, 5, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Muckenthaler, M.; Gray, N.K.; Hentze, M.W. IRP-1 binding to ferritin mRNA prevents the recruitment of the small ribosomal subunit by the cap-binding complex eIF4F. Mol. Cell 1998, 2, 383–388. [Google Scholar] [CrossRef]
- Neve, J.; Patel, R.; Wang, Z.; Louey, A.; Furger, A.M. Cleavage and polyadenylation: Ending the message expands gene regulation. RNA Biol. 2017, 14, 865–890. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, S.M.; Fortes, P.; Izaurralde, E.; Mattaj, I.W.; Gilmartin, G.M. Participation of the nuclear cap binding complex in pre-mRNA 3’ processing. Proc. Natl. Acad. Sci. USA 1997, 94, 11893–11898. [Google Scholar] [CrossRef]
- Bauren, G.; Belikov, S.; Wieslander, L. Transcriptional termination in the Balbiani ring 1 gene is closely coupled to 3’-end formation and excision of the 3’-terminal intron. Genes Dev. 1998, 12, 2759–2769. [Google Scholar] [CrossRef]
- Schoenberg, D.R.; Maquat, L.E. Re-capping the message. Trends Biochem. Sci. 2009, 34, 435–442. [Google Scholar] [CrossRef]
- Schwer, B.; Mao, X.; Shuman, S. Accelerated mRNA decay in conditional mutants of yeast mRNA capping enzyme. Nucleic Acids Res. 1998, 26, 2050–2057. [Google Scholar] [CrossRef]
- Gingras, A.C.; Raught, B.; Sonenberg, N. eIF4 initiation factors: Effectors of mRNA recruitment to ribosomes and regulators of translation. Annu. Rev. Biochem. 1999, 68, 913–963. [Google Scholar] [CrossRef]
- Wahl, M.C.; Will, C.L.; Luhrmann, R. The spliceosome: Design principles of a dynamic RNP machine. Cell 2009, 136, 701–718. [Google Scholar] [CrossRef]
- Han, J.; Xiong, J.; Wang, D.; Fu, X.D. Pre-mRNA splicing: Where and when in the nucleus. Trends Cell Biol. 2011, 21, 336–343. [Google Scholar] [CrossRef]
- Perales, R.; Bentley, D. “Cotranscriptionality”: The transcription elongation complex as a nexus for nuclear transactions. Mol. Cell 2009, 36, 178–191. [Google Scholar] [CrossRef] [PubMed]
- Cooper, T.A.; Wan, L.; Dreyfuss, G. RNA and disease. Cell 2009, 136, 777–793. [Google Scholar] [CrossRef]
- Proudfoot, N.J.; Furger, A.; Dye, M.J. Integrating mRNA processing with transcription. Cell 2002, 108, 501–512. [Google Scholar] [CrossRef]
- Proudfoot, N. New perspectives on connecting messenger RNA 3’ end formation to transcription. Curr. Opin. Cell Biol. 2004, 16, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Ohno, M. Size matters in RNA export. RNA Biol. 2012, 9, 1413–1417. [Google Scholar] [CrossRef] [PubMed]
- McCloskey, A.; Taniguchi, I.; Shinmyozu, K.; Ohno, M. hnRNP C tetramer measures RNA length to classify RNA polymerase II transcripts for export. Science 2012, 335, 1643–1646. [Google Scholar] [CrossRef]
- Stewart, M. Ratcheting mRNA out of the nucleus. Mol. Cell 2007, 25, 327–330. [Google Scholar] [CrossRef]
- Wu, X.; Brewer, G. The regulation of mRNA stability in mammalian cells: 2.0. Gene 2012, 500, 10–21. [Google Scholar] [CrossRef]
- Balagopal, V.; Fluch, L.; Nissan, T. Ways and means of eukaryotic mRNA decay. Biochim. Biophys. Acta 2012, 1819, 593–603. [Google Scholar] [CrossRef]
- Vasudevan, S.; Tong, Y.; Steitz, J.A. Switching from repression to activation: microRNAs can up-regulate translation. Science 2007, 318, 1931–1934. [Google Scholar] [CrossRef]
- Sheets, M.D.; Fox, C.A.; Hunt, T.; Vande Woude, G.; Wickens, M. The 3’-untranslated regions of c-mos and cyclin mRNAs stimulate translation by regulating cytoplasmic polyadenylation. Genes Dev. 1994, 8, 926–938. [Google Scholar] [CrossRef] [PubMed]
- Iguchi, N.; Tobias, J.W.; Hecht, N.B. Expression profiling reveals meiotic male germ cell mRNAs that are translationally up- and down-regulated. Proc. Natl. Acad. Sci. USA 2006, 103, 7712–7717. [Google Scholar] [CrossRef] [PubMed]
- Quinones-Valdez, G.; Tran, S.S.; Jun, H.I.; Bahn, J.H.; Yang, E.W.; Zhan, L.; Brümmer, A.; Wei, X.; Van Nostrand, E.L.; Prat, G.A.; et al. Regulation of RNA editing by RNA-binding proteins in human cells. Commun. Biol. 2019, 2, 19. [Google Scholar] [CrossRef]
- Brooke, G.N.; Culley, R.L.; Dart, D.A.; Mann, D.J.; Gaughan, L.; McCracken, S.R.; Robson, C.N.; Spencer-Dene, B.; Gamble, S.C.; Powell, S.M.; et al. FUS/TLS is a novel mediator of androgen-dependent cell-cycle progression and prostate cancer growth. Cancer Res. 2011, 71, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Zapater, E.; Pineda, D.; Martinez-Bosch, N.; Fernandez-Miranda, G.; Iglesias, M.; Alameda, F.; Moreno, M.; Eliscovich, C.; Eyras, E.; Real, F.X.; et al. Key contribution of CPEB4-mediated translational control to cancer progression. Nat. Med. 2011, 18, 83–90. [Google Scholar] [CrossRef]
- Pereira, B.; Billaud, M.; Almeida, R. RNA-Binding Proteins in Cancer: Old Players and New Actors. Trends Cancer 2017, 3, 506–528. [Google Scholar] [CrossRef]
- Wurth, L.; Papasaikas, P.; Olmeda, D.; Bley, N.; Calvo, G.T.; Guerrero, S.; Cerezo-Wallis, D.; Martinez-Useros, J.; Garcia-Fernandez, M.; Huttelmaier, S.; et al. UNR/CSDE1 Drives a Post-transcriptional Program to Promote Melanoma Invasion and Metastasis. Cancer Cell 2019, 36, 337. [Google Scholar] [CrossRef]
- Qi, Z.; Takamatsu, H.; Espinoza, J.L.; Lu, X.; Sugimori, N.; Yamazaki, H.; Okawa, K.; Nakao, S. Autoantibodies specific to hnRNP K: A new diagnostic marker for immune pathophysiology in aplastic anemia. Ann. Hematol. 2010, 89, 1255–1263. [Google Scholar] [CrossRef]
- Aguilar-Garrido, P.V.M.; Hernández Sánchez, M.; Navarro Aguadero, M.Á.; Malaney, P.; Aitken, M.J.L.; Zhang, X.; Young, K.H.; Duan, R.; Hu, P.; Kornblau, S.; et al. S104: RBPs dysregulation cause hyper-nucleoli and ribosome gain-of-function driving bone marrow failure. HemaSphere 2022, 6, 5–6. [Google Scholar] [CrossRef]
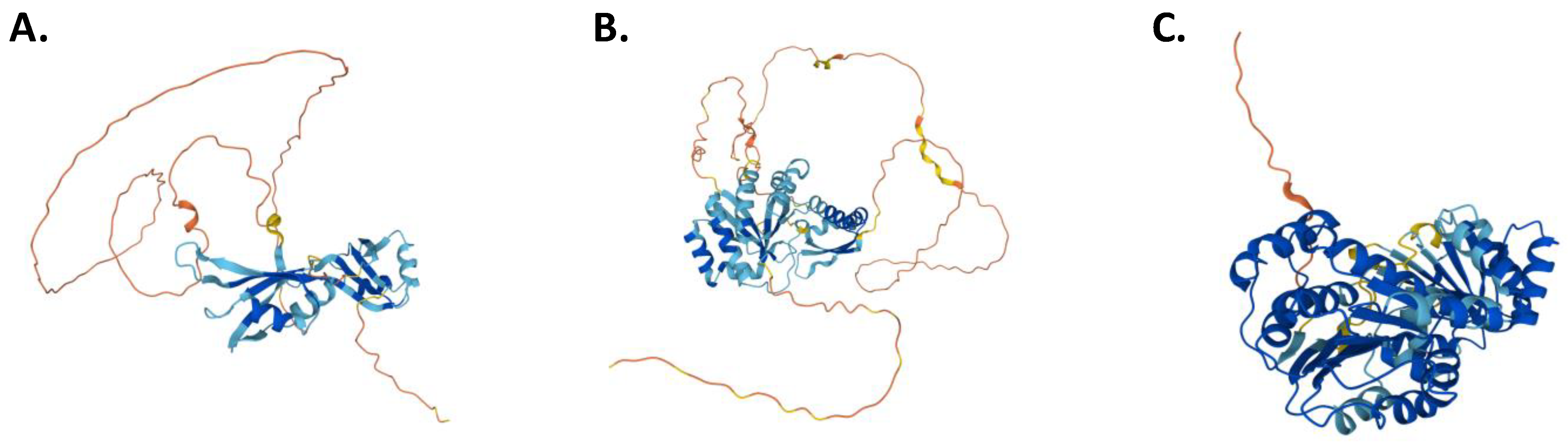
- Jumper, J.; Evans, R.; Pritzel, A.; Green, T.; Figurnov, M.; Ronneberger, O.; Tunyasuvunakool, K.; Bates, R.; Žídek, A.; Potapenko, A.; et al. Highly accurate protein structure prediction with AlphaFold. Nature 2021, 596, 583–589. [Google Scholar] [CrossRef]
- Varadi, M.; Anyango, S.; Deshpande, M.; Nair, S.; Natassia, C.; Yordanova, G.; Yuan, D.; Stroe, O.; Wood, G.; Laydon, A.; et al. AlphaFold Protein Structure Database: Massively expanding the structural coverage of protein-sequence space with high-accuracy models. Nucleic Acids Res. 2022, 50, D439–D444. [Google Scholar] [CrossRef] [PubMed]
- Grech, G.; von Lindern, M. The Role of Translation Initiation Regulation in Haematopoiesis. Comp. Funct. Genom. 2012, 2012, 576540. [Google Scholar] [CrossRef] [PubMed]
- Barboro, P.; Ferrari, N.; Balbi, C. Emerging roles of heterogeneous nuclear ribonucleoprotein K (hnRNP K) in cancer progression. Cancer Lett. 2014, 352, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Malaney, P.; Velasco-Estevez, M.; Aguilar-Garrido, P.; Aitken, M.J.L.; Chan, L.E.; Zhang, X.; Post, S.M.; Gallardo, M. The Emicro-hnRNP K Murine Model of Lymphoma: Novel Insights into the Role of hnRNP K in B-Cell Malignancies. Front. Immunol. 2021, 12, 634584. [Google Scholar] [CrossRef]
- Moumen, A.; Masterson, P.; O’Connor, M.J.; Jackson, S.P. hnRNP K: An HDM2 target and transcriptional coactivator of p53 in response to DNA damage. Cell 2005, 123, 1065–1078. [Google Scholar] [CrossRef]
- Yang, X.; Wen, Y.; Liu, S.; Duan, L.; Liu, T.; Tong, Z.; Wang, Z.; Gu, Y.; Xi, Y.; Wang, X.; et al. LCDR regulates the integrity of lysosomal membrane by hnRNP K-stabilized LAPTM5 transcript and promotes cell survival. Proc. Natl. Acad. Sci. USA 2022, 119, e2110428119. [Google Scholar] [CrossRef]
- Grimwade, D.; Walker, H.; Oliver, F.; Wheatley, K.; Harrison, C.; Harrison, G.; Rees, J.; Hann, I.; Stevens, R.; Burnett, A.; et al. The importance of diagnostic cytogenetics on outcome in AML: Analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood 1998, 92, 2322–2333. [Google Scholar] [CrossRef]
- Dayyani, F.; Wang, J.; Yeh, J.R.; Ahn, E.Y.; Tobey, E.; Zhang, D.E.; Bernstein, I.D.; Peterson, R.T.; Sweetser, D.A. Loss of TLE1 and TLE4 from the del(9q) commonly deleted region in AML cooperates with AML1-ETO to affect myeloid cell proliferation and survival. Blood 2008, 111, 4338–4347. [Google Scholar] [CrossRef]
- Kronke, J.; Bullinger, L.; Teleanu, V.; Tschurtz, F.; Gaidzik, V.I.; Kuhn, M.W.; Rucker, F.G.; Holzmann, K.; Paschka, P.; Kapp-Schworer, S.; et al. Clonal evolution in relapsed NPM1-mutated acute myeloid leukemia. Blood 2013, 122, 100–108. [Google Scholar] [CrossRef]
- Nika, E.; Brugnoli, F.; Piazzi, M.; Lambertini, E.; Grassilli, S.; Bavelloni, A.; Piva, R.; Capitani, S.; Bertagnolo, V. hnRNP K in PU.1-containing complexes recruited at the CD11b promoter: A distinct role in modulating granulocytic and monocytic differentiation of AML-derived cells. Biochem. J. 2014, 463, 115–122. [Google Scholar] [CrossRef]
- Eiring, A.M.; Neviani, P.; Santhanam, R.; Oaks, J.J.; Chang, J.S.; Notari, M.; Willis, W.; Gambacorti-Passerini, C.; Volinia, S.; Marcucci, G.; et al. Identification of novel posttranscriptional targets of the BCR/ABL oncoprotein by ribonomics: Requirement of E2F3 for BCR/ABL leukemogenesis. Blood 2008, 111, 816–828. [Google Scholar] [CrossRef] [PubMed]
- Notari, M.; Neviani, P.; Santhanam, R.; Blaser, B.W.; Chang, J.S.; Galietta, A.; Willis, A.E.; Roy, D.C.; Caligiuri, M.A.; Marcucci, G.; et al. A MAPK/HNRPK pathway controls BCR/ABL oncogenic potential by regulating MYC mRNA translation. Blood 2006, 107, 2507–2516. [Google Scholar] [CrossRef] [PubMed]
- Taggart, J.; Ho, T.C.; Amin, E.; Xu, H.; Barlowe, T.S.; Perez, A.R.; Durham, B.H.; Tivnan, P.; Okabe, R.; Chow, A.; et al. MSI2 is required for maintaining activated myelodysplastic syndrome stem cells. Nat. Commun. 2016, 7, 10739. [Google Scholar] [CrossRef]
- Mancarella, C.; Scotlandi, K. IGF2BP3 From Physiology to Cancer: Novel Discoveries, Unsolved Issues, and Future Perspectives. Front. Cell Dev. Biol. 2019, 7, 363. [Google Scholar] [CrossRef] [PubMed]
- Palanichamy, J.K.; Tran, T.M.; Howard, J.M.; Contreras, J.R.; Fernando, T.R.; Sterne-Weiler, T.; Katzman, S.; Toloue, M.; Yan, W.; Basso, G.; et al. RNA-binding protein IGF2BP3 targeting of oncogenic transcripts promotes hematopoietic progenitor proliferation. J. Clin. Investig. 2016, 126, 1495–1511. [Google Scholar] [CrossRef] [PubMed]
- Makinen, A.; Nikkila, A.; Haapaniemi, T.; Oksa, L.; Mehtonen, J.; Vanska, M.; Heinaniemi, M.; Paavonen, T.; Lohi, O. IGF2BP3 Associates with Proliferative Phenotype and Prognostic Features in B-Cell Acute Lymphoblastic Leukemia. Cancers 2021, 13, 1505. [Google Scholar] [CrossRef] [PubMed]
- Sakakibara, S.; Nakamura, Y.; Satoh, H.; Okano, H. Rna-binding protein Musashi2: Developmentally regulated expression in neural precursor cells and subpopulations of neurons in mammalian CNS. J. Neurosci. Off. J. Soc. Neurosci. 2001, 21, 8091–8107. [Google Scholar] [CrossRef]
- Nakamura, M.; Okano, H.; Blendy, J.A.; Montell, C. Musashi, a neural RNA-binding protein required for Drosophila adult external sensory organ development. Neuron 1994, 13, 67–81. [Google Scholar] [CrossRef]
- Kharas, M.G.; Lengner, C.J.; Al-Shahrour, F.; Bullinger, L.; Ball, B.; Zaidi, S.; Morgan, K.; Tam, W.; Paktinat, M.; Okabe, R.; et al. Musashi-2 regulates normal hematopoiesis and promotes aggressive myeloid leukemia. Nat. Med. 2010, 16, 903–908. [Google Scholar] [CrossRef]
- Xu, C.; Chen, X.; Zhang, X.; Zhao, D.; Dou, Z.; Xie, X.; Li, H.; Yang, H.; Li, Q.; Zhang, H.; et al. RNA-binding protein 39: A promising therapeutic target for cancer. Cell Death Discov. 2021, 7, 214. [Google Scholar] [CrossRef]
- Xu, Y.; Nijhuis, A.; Keun, H.C. RNA-binding motif protein 39 (RBM39): An emerging cancer target. Br. J. Pharmacol. 2022, 179, 2795–2812. [Google Scholar] [CrossRef] [PubMed]
- Mercier, I.; Gonzales, D.M.; Quann, K.; Pestell, T.G.; Molchansky, A.; Sotgia, F.; Hulit, J.; Gandara, R.; Wang, C.; Pestell, R.G.; et al. CAPER, a novel regulator of human breast cancer progression. Cell Cycle 2014, 13, 1256–1264. [Google Scholar] [CrossRef] [PubMed]
- Komeno, Y.; Huang, Y.J.; Qiu, J.; Lin, L.; Xu, Y.; Zhou, Y.; Chen, L.; Monterroza, D.D.; Li, H.; DeKelver, R.C.; et al. SRSF2 is Essential for Hematopoiesis, and its Myeloidysplastic Syndrome-Related Mutations Dysregulate Alternatie pre-mRNA Splicing. Mol. Cell Biol. 2015, 35, 3071–3082. [Google Scholar] [CrossRef]
- Dolashad, H.; Pellagati, A.; Fernandez-Mercado, M.; Yip, B.H.; Malcovati, L.; Attwood, M.; Przychodzen, B.; Sahgal, N.; Kanapin, A.A.; Lockstone, H.; et al. Disruption of SF3B1 results in deregulated expression and splicing of key genes and pathways in myelodysplastic syndrome hematopoietic stem and progenitor cells. Leukemia 2015, 29, 1092–1103. [Google Scholar] [CrossRef]
- Baou, M.; Norton, J.D.; Murphy, J.J. AU-rich RNA binding proteins in hematopoiesis and leukemogenesis. Blood 2011, 118, 5732–5740. [Google Scholar] [CrossRef] [PubMed]
- Dowhan, D.H.; Hong, E.P.; Auboeuf, D.; Dennis, A.P.; Wilson, M.M.; Berget, S.M.; O’Malley, B.W. Steroid hormone receptor coactivation and alternative RNA splicing by U2AF65-related proteins CAPERalpha and CAPERbeta. Mol. Cell 2005, 17, 429–439. [Google Scholar] [CrossRef]
- Jung, D.J.; Na, S.Y.; Na, D.S.; Lee, J.W. Molecular cloning and characterization of CAPER, a novel coactivator of activating protein-1 and estrogen receptors. J. Biol. Chem. 2002, 277, 1229–1234. [Google Scholar] [CrossRef]
- Song, Y.; Guo, Y.; Li, X.; Sun, R.; Zhu, M.; Shi, J.; Tan, Z.; Zhang, L.; Huang, J. RBM39 Alters Phosphorylation of c-Jun and Binds to Viral RNA to Promote PRRSV Proliferation. Front. Immunol. 2021, 12, 664417. [Google Scholar] [CrossRef]
- Mai, S.; Qu, X.; Li, P.; Ma, Q.; Liu, X.; Cao, C. Functional interaction between nonreceptor tyrosine kinase c-Abl and SR-Rich protein RBM39. Biochem. Biophys. Res. Commun. 2016, 473, 355–360. [Google Scholar] [CrossRef]
- Campbell, M.C.; Pontiggia, L.; Russell, A.Y.; Schwarting, R.; Camacho, J.; Jasmin, J.F.; Mercier, I. CAPER as a therapeutic target for triple negative breast cancer. Oncotarget 2018, 9, 30340–30354. [Google Scholar] [CrossRef]
- Chai, Y.; Liu, X.; Dai, L.; Li, Y.; Liu, M.; Zhang, J.Y. Overexpression of HCC1/CAPERalpha may play a role in lung cancer carcinogenesis. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014, 35, 6311–6317. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.; Lu, S.X.; Pastore, A.; Chen, X.; Imig, J.; Chun-Wei Lee, S.; Hockemeyer, K.; Ghebrechristos, Y.E.; Yoshimi, A.; Inoue, D.; et al. Targeting an RNA-Binding Protein Network in Acute Myeloid Leukemia. Cancer Cell 2019, 35, 369–384.e367. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.; Xu, X.; Zhang, Z.; Ma, C.; Xiang, R.; Liu, J.; Xu, W.; Wu, C.; Li, J.; Zhan, F.; et al. Hypoxia-induced long non-coding RNA DARS-AS1 regulates RBM39 stability to promote myeloma malignancy. Haematologica 2020, 105, 1630–1640. [Google Scholar] [CrossRef]
- Okano, H.; Imai, T.; Okabe, M. Musashi: A translational regulator of cell fate. J. Cell Sci. 2002, 115, 1355–1359. [Google Scholar] [CrossRef]
- Okano, H.; Kawahara, H.; Toriya, M.; Nakao, K.; Shibata, S.; Imai, T. Function of RNA-binding protein Musashi-1 in stem cells. Exp. Cell Res. 2005, 306, 349–356. [Google Scholar] [CrossRef]
- Forouzanfar, M.; Lachinani, L.; Dormiani, K.; Nasr-Esfahani, M.H.; Gure, A.O.; Ghaedi, K. Intracellular functions of RNA-binding protein, Musashi1, in stem and cancer cells. Stem Cell Res. Ther. 2020, 11, 193. [Google Scholar] [CrossRef]
- Wuebben, E.L.; Mallanna, S.K.; Cox, J.L.; Rizzino, A. Musashi2 is required for the self-renewal and pluripotency of embryonic stem cells. PLoS ONE 2012, 7, e34827. [Google Scholar] [CrossRef] [PubMed]
- Kudinov, A.E.; Karanicolas, J.; Golemis, E.A.; Boumber, Y. Musashi RNA-Binding Proteins as Cancer Drivers and Novel Therapeutic Targets. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2017, 23, 2143–2153. [Google Scholar] [CrossRef]
- Li, M.; Li, A.Q.; Zhou, S.L.; Lv, H.; Wei, P.; Yang, W.T. RNA-binding protein MSI2 isoforms expression and regulation in progression of triple-negative breast cancer. J. Exp. Clin. Cancer Res. 2020, 39, 92. [Google Scholar] [CrossRef]
- MacNicol, M.C.; Cragle, C.E.; McDaniel, F.K.; Hardy, L.L.; Wang, Y.; Arumugam, K.; Rahmatallah, Y.; Glazko, G.V.; Wilczynska, A.; Childs, G.V.; et al. Evasion of regulatory phosphorylation by an alternative spliced isoform of Musashi2. Sci. Rep. 2017, 7, 11503. [Google Scholar] [CrossRef]
- Kharas, M.G.; Lengner, C.J. Stem Cells, Cancer, and MUSASHI in Blood and Guts. Trends Cancer 2017, 3, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Gonen, M.; Vu, L.; Minuesa, G.; Tivnan, P.; Barlowe, T.S.; Taggart, J.; Lu, Y.; Deering, R.P.; Hacohen, N.; et al. Musashi2 sustains the mixed-lineage leukemia-driven stem cell regulatory program. J. Clin. Investig. 2015, 125, 1286–1298. [Google Scholar] [CrossRef]
- Imai, T.; Tokunaga, A.; Yoshida, T.; Hashimoto, M.; Mikoshiba, K.; Weinmaster, G.; Nakafuku, M.; Okano, H. The neural RNA-binding protein Musashi1 translationally regulates mammalian numb gene expression by interacting with its mRNA. Mol. Cell. Biol. 2001, 21, 3888–3900. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Kwon, H.Y.; Zimdahl, B.; Congdon, K.L.; Blum, J.; Lento, W.E.; Zhao, C.; Lagoo, A.; Gerrard, G.; Foroni, L.; et al. Regulation of myeloid leukaemia by the cell-fate determinant Musashi. Nature 2010, 466, 765–768. [Google Scholar] [CrossRef] [PubMed]
- Palacios, F.; Yan, X.J.; Ferrer, G.; Chen, S.S.; Vergani, S.; Yang, X.; Gardner, J.; Barrientos, J.C.; Rock, P.; Burack, R.; et al. Musashi 2 influences chronic lymphocytic leukemia cell survival and growth making it a potential therapeutic target. Leukemia 2021, 35, 1037–1052. [Google Scholar] [CrossRef]
- Minuesa, G.; Albanese, S.K.; Xie, W.; Kazansky, Y.; Worroll, D.; Chow, A.; Schurer, A.; Park, S.M.; Rotsides, C.Z.; Taggart, J.; et al. Small-molecule targeting of MUSASHI RNA-binding activity in acute myeloid leukemia. Nat. Commun. 2019, 10, 2691. [Google Scholar] [CrossRef]
- Nielsen, J.; Christiansen, J.; Lykke-Andersen, J.; Johnsen, A.H.; Wewer, U.M.; Nielsen, F.C. A family of insulin-like growth factor II mRNA-binding proteins represses translation in late development. Mol. Cell. Biol. 1999, 19, 1262–1270. [Google Scholar] [CrossRef]
- Nielsen, J.; Kristensen, M.A.; Willemoes, M.; Nielsen, F.C.; Christiansen, J. Sequential dimerization of human zipcode-binding protein IMP1 on RNA: A cooperative mechanism providing RNP stability. Nucleic Acids Res. 2004, 32, 4368–4376. [Google Scholar] [CrossRef]
- Farina, K.L.; Huttelmaier, S.; Musunuru, K.; Darnell, R.; Singer, R.H. Two ZBP1 KH domains facilitate beta-actin mRNA localization, granule formation, and cytoskeletal attachment. J. Cell Biol. 2003, 160, 77–87. [Google Scholar] [CrossRef]
- Schneider, T.; Hung, L.H.; Aziz, M.; Wilmen, A.; Thaum, S.; Wagner, J.; Janowski, R.; Muller, S.; Schreiner, S.; Friedhoff, P.; et al. Combinatorial recognition of clustered RNA elements by the multidomain RNA-binding protein IMP3. Nat. Commun. 2019, 10, 2266. [Google Scholar] [CrossRef]
- Bell, J.L.; Wachter, K.; Muhleck, B.; Pazaitis, N.; Kohn, M.; Lederer, M.; Huttelmaier, S. Insulin-like growth factor 2 mRNA-binding proteins (IGF2BPs): Post-transcriptional drivers of cancer progression? Cell. Mol. Life Sci. CMLS 2013, 70, 2657–2675. [Google Scholar] [CrossRef] [PubMed]
- Lederer, M.; Bley, N.; Schleifer, C.; Huttelmaier, S. The role of the oncofetal IGF2 mRNA-binding protein 3 (IGF2BP3) in cancer. Semin. Cancer Biol. 2014, 29, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Rivera Vargas, T.; Boudoukha, S.; Simon, A.; Souidi, M.; Cuvellier, S.; Pinna, G.; Polesskaya, A. Post-transcriptional regulation of cyclins D1, D3 and G1 and proliferation of human cancer cells depend on IMP-3 nuclear localization. Oncogene 2014, 33, 2866–2875. [Google Scholar] [CrossRef] [PubMed]
- Mizutani, R.; Imamachi, N.; Suzuki, Y.; Yoshida, H.; Tochigi, N.; Oonishi, T.; Suzuki, Y.; Akimitsu, N. Oncofetal protein IGF2BP3 facilitates the activity of proto-oncogene protein eIF4E through the destabilization of EIF4E-BP2 mRNA. Oncogene 2016, 35, 3495–3502. [Google Scholar] [CrossRef]
- Zhao, W.; Lu, D.; Liu, L.; Cai, J.; Zhou, Y.; Yang, Y.; Zhang, Y.; Zhang, J. Insulin-like growth factor 2 mRNA binding protein 3 (IGF2BP3) promotes lung tumorigenesis via attenuating p53 stability. Oncotarget 2017, 8, 93672–93687. [Google Scholar] [CrossRef]
- Tran, T.M.; Philipp, J.; Bassi, J.S.; Nibber, N.; Draper, J.M.; Lin, T.L.; Palanichamy, J.K.; Jaiswal, A.K.; Silva, O.; Paing, M.; et al. The RNA-binding protein IGF2BP3 is critical for MLL-AF4-mediated leukemogenesis. Leukemia 2022, 36, 68–79. [Google Scholar] [CrossRef]
- Canella, A.; Cordero Nieves, H.; Sborov, D.W.; Cascione, L.; Radomska, H.S.; Smith, E.; Stiff, A.; Consiglio, J.; Caserta, E.; Rizzotto, L.; et al. HDAC inhibitor AR-42 decreases CD44 expression and sensitizes myeloma cells to lenalidomide. Oncotarget 2015, 6, 31134–31150. [Google Scholar] [CrossRef]
- Gou, J.; Li, H.; Bi, J.; Pang, X.; Li, X.; Wang, Y. Transfer of IGF2BP3 Through Ara-C-Induced Apoptotic Bodies Promotes Survival of Recipient Cells. Front. Oncol. 2022, 12, 801226. [Google Scholar] [CrossRef]
- Makeyev, A.V.; Liebhaber, S.A. The poly(C)-binding proteins: A multiplicity of functions and a search for mechanisms. Rna 2002, 8, 265–278. [Google Scholar] [CrossRef]
- Michael, W.M.; Eder, P.S.; Dreyfuss, G. The K nuclear shuttling domain: A novel signal for nuclear import and nuclear export in the hnRNP K protein. EMBO J. 1997, 16, 3587–3598. [Google Scholar] [CrossRef]
- Moumen, A.; Magill, C.; Dry, K.L.; Jackson, S.P. ATM-dependent phosphorylation of heterogeneous nuclear ribonucleoprotein K promotes p53 transcriptional activation in response to DNA damage. Cell Cycle 2013, 12, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Tang, F.; Li, W.; Chen, Y.; Wang, D.; Han, J.; Liu, D. Downregulation of hnRNP K by RNAi inhibits growth of human lung carcinoma cells. Oncol. Lett. 2014, 7, 1073–1077. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, D.; Wang, X.; Mei, H.; Fang, E.; Ye, L.; Song, H.; Yang, F.; Li, H.; Huang, K.; Zheng, L.; et al. Long Noncoding RNA pancEts-1 Promotes Neuroblastoma Progression through hnRNPK-Mediated beta-Catenin Stabilization. Cancer Res. 2018, 78, 1169–1183. [Google Scholar] [CrossRef]
- Qin, G.; Tu, X.; Li, H.; Cao, P.; Chen, X.; Song, J.; Han, H.; Li, Y.; Guo, B.; Yang, L.; et al. Long Noncoding RNA p53-Stabilizing and Activating RNA Promotes p53 Signaling by Inhibiting Heterogeneous Nuclear Ribonucleoprotein K deSUMOylation and Suppresses Hepatocellular Carcinoma. Hepatology 2020, 71, 112–129. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhou, C.; Chang, Y.; Zhang, Z.; Hu, Y.; Zhang, F.; Lu, Y.; Zheng, L.; Zhang, W.; Li, X.; et al. Long non-coding RNA CASC11 interacts with hnRNP-K and activates the WNT/beta-catenin pathway to promote growth and metastasis in colorectal cancer. Cancer Lett. 2016, 376, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Sweetser, D.A.; Peniket, A.J.; Haaland, C.; Blomberg, A.A.; Zhang, Y.; Zaidi, S.T.; Dayyani, F.; Zhao, Z.; Heerema, N.A.; Boultwood, J.; et al. Delineation of the minimal commonly deleted segment and identification of candidate tumor-suppressor genes in del(9q) acute myeloid leukemia. Genes Chromosomes Cancer 2005, 44, 279–291. [Google Scholar] [CrossRef]
- Evans, J.R.; Mitchell, S.A.; Spriggs, K.A.; Ostrowski, J.; Bomsztyk, K.; Ostarek, D.; Willis, A.E. Members of the poly (rC) binding protein family stimulate the activity of the c-myc internal ribosome entry segment in vitro and in vivo. Oncogene 2003, 22, 8012–8020. [Google Scholar] [CrossRef]
- Prieto, C.; Kharas, M.G. RNA Regulators in Leukemia and Lymphoma. Cold Spring Harb. Perspect. Med. 2020, 10, a034967. [Google Scholar] [CrossRef]
- Shen, L.; Shi, Q.; Wang, W. Double agents: Genes with both oncogenic and tumor-suppressor functions. Oncogenesis 2018, 7, 25. [Google Scholar] [CrossRef]
- Mohibi, S.; Chen, X.; Zhang, J. Cancer the’RBP’eutics-RNA-binding proteins as therapeutic targets for cancer. Pharmacol. Ther. 2019, 203, 107390. [Google Scholar] [CrossRef]
- Azmi, A.S.; Uddin, M.H.; Mohammad, R.M. The nuclear export protein XPO1-from biology to targeted therapy. Nat. Rev. Clin. Oncol. 2021, 18, 152–169. [Google Scholar] [CrossRef] [PubMed]
- Flach, J.; Jann, J.C.; Knaflic, A.; Riabov, V.; Streuer, A.; Altrock, E.; Xu, Q.; Schmitt, N.; Obländer, J.; Nowak, V.; et al. Replication stress signaling is a therapeutic target in myelodysplastic syndromes with splicing factor mutations. Haematologica 2021, 106, 2906. [Google Scholar] [CrossRef] [PubMed]
| Type of Binding Domain | Structure Interface | Interaction between RBP and RNA | Nucleic Acid Affinity | RBPs Containing RBDs |
|---|---|---|---|---|
| KH type I (hnRNP K homology type I) | Structure approximately 70 amino acids long. It typically adopts βααββα, forming by a β-sheet composed of 3 antiparallel β-strands and 3 α-helices [27,28] | Four single-stranded nucleotides are recognized by the invariant Gly–X–X–Gly motif, the near helices, and the β-strand that follows α2 (type I) | C-rich ssDNA and ssRNA [27,28] | hnRNP K [29], Nus A [30], SF1 [31], Nova-2 [32] |
| KH type II (hnRNP K homology type II) | Structure approximately 70 amino acids long. It is displayed as a αββααβ [27] | Same as KH I, where four single-stranded nucleotides are recognized by α3 (instead of α2 as in KH I) | C-rich ssDNA and ssRNA [27,28] | hnRNP K [29], Nus A [30], SF1 [31], Nova-2 [32] |
| KH type III (hnRNP K homology type III) | Structure approximately 75-80 amino acids long. It typically adopts a spatial configuration of βααββα, forming a 3-stranded β-sheet held against a 3-helix cluster [27] | Same as KH type I | C-rich ssDNA and ssRNA [27,28] | Nova-2 [33], hnRNP K [34] |
| RRMs (RNA recognition motifs) | Structure approximately 80-90 amino acids long. It typically adopts topology of βαββαβ, forming a 4-stranded β-sheet and 2 α-helices [35] | Main interaction between the binding domain and RNA is mediated through the β-sheet | Polypyrimidine (mainly C- and U-rich sequences) ssRNA [35,36] | U2AF65 [36], nucleolin [37], SRp20 [38], hnRNP F [39], FOX1 [40], Musashi 1, Musashi 2 [41], RBM39 [42] |
| ZnF (Zinc Fingers) | Structure approximately 30 amino acids long. It displays a ββα topology, forming a β-hairpin and an α-helix together with a Zn2+ ion [43] | Binding to nucleic acids through the α-helix | dsDNA, ssRNA, dsRNA [44] | MBNL1 [44], TFIIIA [45], ZRANB2 [46] |
| dsRBDs (double-stranded RNA binding domains) | Structure approximately 65-70 amino acids long. It typically adopts a αβββα topology, where 2 α-helices are packed along a 3-stranded anti-parallel β-sheet [47] | Binding to dsRNA backbone through α2 and the β1- β2 loop. Additional interactions occur through the α1 | dsRNA [47] | ADAR1 [48], Dicer [49] |
| DEAD-box | Structure approximately 300-400 amino acids long. It adopts a βαββαβ topology, forming a 4-stranded β-sheet and 2 α-helices, similar to RRM binding domains [50] | Helicase core binds to the backbone of the RNA, without contact with the nucleotides | Polypyrimidine ssRNA [50] | eIF4A1/DDX2 [51], p68 [52], p72 [53] |
| PUF (Pumilio-fem-3 binding factor) | Structure approximately 6-8 tandem copies of a 35 amino acids long sequence. It adopts a topology of 3 α- helices, forming a triangle [54] | Binding to RNA is through the α 2 in each tandem repeat | ssRNA [55] | PUM1, PUM2 [55] |
| SAM (Sterile alpha motif) | Structure approximately 150-160 amino acids long. It displays a topology of 6 α-helices, packed by a hydrophobic core [56] | Traditionally known to bind protein, but has recently been shown to bind RNA | Hairpin RNA [56] | p63, p73 [57], p73, EPHA2 [58] |
| RBP | RNA Binding Motif | Role in Normal Hematopoiesis | Related Hematological Malignancies |
|---|---|---|---|
| ADAR1 | dsRBD [48] | Regulation of HSCs differentiation via base editing activity | Enhanced editing activity in CML, increasing self-renewal capacity |
| DDX3X, DDX5 | DEAD Box [51] | Essential for the innate immune response and normal hematopoiesis | Frequently mutated in hematological malignances, and upregulated upon Imatinib treatment |
| DDX21 | DEAD Box [51] | HSCs self-renewal | Increases leukemia stem cell proliferation in AML |
| EIF4E | DEAD Box | Transcription factor, cell differentiation [94] | Blockage of myeloid differentiation, leading to leukemogenesis |
| hnRNP K | KH1, KH2, KH3 [95] | DNA damage response and cell cycle arrest [96,97] | Deletion in AML [98,99,100,101], overexpression in CML [102,103], oncogen in DLBCL [22] and MM [104] |
| IGF2BP3 | RRM, KH [105] | Self-renewal of HSCs [106] | B-ALL cell survival [106], MLL [107], and therapeutic resistance in MM [108] |
| MSI2 | RRM [41] | Self-renewal of HSCs [109] | Upregulated in most hematological malignancies and associated to poor prognosis [110,111] |
| RBM39 | RRM [42] | Part of the spliceosome [112] | AML malignant cell growth and maintenance [113], as well as myeloma progression [114] |
| SRSF2 | RRM [38] | Essential for myeloid hematopoiesis [115] | Mutations associated to poor survival in MDS [115] |
| SF3B1 | RRM [36] | HSCs homeostasis [116] | Mutations associated with MDS [116] |
| ZFP36 | ZnF [43] | Hematopoiesis and cell differentiation [117] | Loss of function leads to leukemogenesis [117] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguilar-Garrido, P.; Otero-Sobrino, Á.; Navarro-Aguadero, M.Á.; Velasco-Estévez, M.; Gallardo, M. The Role of RNA-Binding Proteins in Hematological Malignancies. Int. J. Mol. Sci. 2022, 23, 9552. https://doi.org/10.3390/ijms23179552
Aguilar-Garrido P, Otero-Sobrino Á, Navarro-Aguadero MÁ, Velasco-Estévez M, Gallardo M. The Role of RNA-Binding Proteins in Hematological Malignancies. International Journal of Molecular Sciences. 2022; 23(17):9552. https://doi.org/10.3390/ijms23179552
Chicago/Turabian StyleAguilar-Garrido, Pedro, Álvaro Otero-Sobrino, Miguel Ángel Navarro-Aguadero, María Velasco-Estévez, and Miguel Gallardo. 2022. "The Role of RNA-Binding Proteins in Hematological Malignancies" International Journal of Molecular Sciences 23, no. 17: 9552. https://doi.org/10.3390/ijms23179552
APA StyleAguilar-Garrido, P., Otero-Sobrino, Á., Navarro-Aguadero, M. Á., Velasco-Estévez, M., & Gallardo, M. (2022). The Role of RNA-Binding Proteins in Hematological Malignancies. International Journal of Molecular Sciences, 23(17), 9552. https://doi.org/10.3390/ijms23179552







