The Physiological Function and Potential Role of the Ubiquitous Na+/H+ Exchanger Isoform 8 (NHE8): An Overview Data
Abstract
:1. Introduction
1.1. NHEs Classification
1.2. The Molecular Structure of NHEs
2. NHE8 in the Gastrointestinal Tract
2.1. The Gender-Specific Compensation in the Intestine
2.2. NHE8: The Bridge NHE Isoform for the Secretory Lineage?
2.3. Lack of NHE8 as a Cause of Dysbiosis
2.4. The Relationship between NHE8 and Diarrhea
2.5. The Relationship between NHE8 and Colitis-Associated Colorectal Cancer
3. The Role of NHE8 in the Kidney
4. NHE8 Expression in the Eyes
5. NHE8 in the Testis: Another Fertility Related NHE Isoform
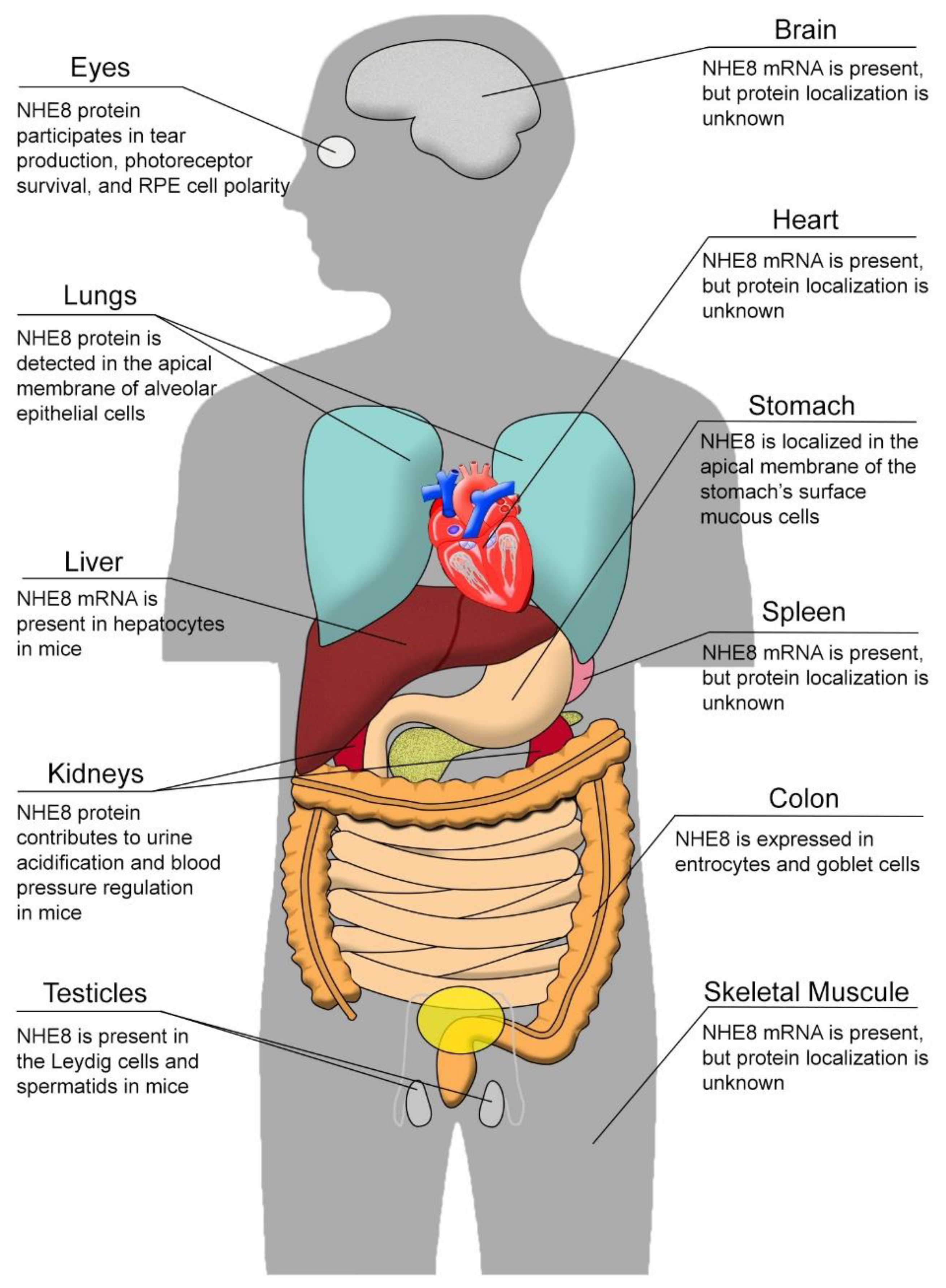
6. NHE8 in Other Organs
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Mitchell, P.; Moyle, J. Acid-base titration across the membrane system of rat-liver mitochondria. Catalysis by uncouplers. Biochem. J. 1967, 104, 588–600. [Google Scholar] [CrossRef] [PubMed]
- Lane, N. Proton gradients at the origin of life. Bioessays 2017, 39, 1600217. [Google Scholar] [CrossRef] [PubMed]
- Janecke, A.R.; Heinz-Erian, P.; Yin, J.; Petersen, B.S.; Franke, A.; Lechner, S.; Fuchs, I.; Melancon, S.; Uhlig, H.H.; Travis, S.; et al. Reduced sodium/proton exchanger NHE3 activity causes congenital sodium diarrhea. Hum. Mol. Genet. 2015, 24, 6614–6623. [Google Scholar] [CrossRef] [PubMed]
- Ronald, A.; Hoekstra, R.A. Autism spectrum disorders and autistic traits: A decade of new twin studies. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2011, 156B, 255–274. [Google Scholar] [CrossRef] [PubMed]
- Kondapalli, K.C.; Hack, A.; Schushan, M.; Landau, M.; Ben-Tal, N.; Rao, R. Functional evaluation of autism-associated mutations in NHE9. Nat. Commun. 2013, 4, 2510. [Google Scholar] [CrossRef]
- Jadeja, S.; Barnard, A.R.; McKie, L.; Cross, S.H.; White, J.K.; Sanger Mouse Genetics, P.; Robertson, M.; Budd, P.S.; MacLaren, R.E.; Jackson, I.J. Mouse slc9a8 mutants exhibit retinal defects due to retinal pigmented epithelium dysfunction. Investig. Ophthalmol. Vis. Sci. 2015, 56, 3015–3026. [Google Scholar] [CrossRef]
- Xia, C.H.; Liu, H.; Cheung, D.; Tang, F.; Chang, B.; Li, M.; Gong, X. NHE8 is essential for RPE cell polarity and photoreceptor survival. Sci. Rep. 2015, 5, 9358. [Google Scholar] [CrossRef]
- Zachos, N.C.; Tse, M.; Donowitz, M. Molecular physiology of intestinal Na+/H+ exchange. Annu. Rev. Physiol. 2005, 67, 411–443. [Google Scholar] [CrossRef]
- Xu, H.; Chen, H.; Dong, J.; Lynch, R.; Ghishan, F.K. Gastrointestinal distribution and kinetic characterization of the sodium-hydrogen exchanger isoform 8 (NHE8). Cell Physiol. Biochem. 2008, 21, 109–116. [Google Scholar] [CrossRef]
- Chen, J.S.; Reddy, V.; Chen, J.H.; Shlykov, M.A.; Zheng, W.H.; Cho, J.; Yen, M.R.; Saier, M.H., Jr. Phylogenetic characterization of transport protein superfamilies: Superiority of SuperfamilyTree programs over those based on multiple alignments. J. Mol. Microbiol. Biotechnol. 2011, 21, 83–96. [Google Scholar] [CrossRef] [Green Version]
- Saier, M.H., Jr.; Reddy, V.S.; Tsu, B.V.; Ahmed, M.S.; Li, C.; Moreno-Hagelsieb, G. The Transporter Classification Database (TCDB): Recent advances. Nucleic Acids Res. 2016, 44, D372–D379. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.F.; Counillon, L. The SLC9A-C Mammalian Na(+)/H(+) Exchanger Family: Molecules, Mechanisms, and Physiology. Physiol. Rev. 2019, 99, 2015–2113. [Google Scholar] [CrossRef] [PubMed]
- Damkier, H.H.; Prasad, V.; Hubner, C.A.; Praetorius, J. Nhe1 is a luminal Na+/H+ exchanger in mouse choroid plexus and is targeted to the basolateral membrane in Ncbe/Nbcn2-null mice. Am. J. Physiol. Cell Physiol. 2009, 296, C1291–C1300. [Google Scholar] [CrossRef]
- Counillon, L.; Pouyssegur, J.; Reithmeier, R.A. The Na+/H+ exchanger NHE-1 possesses N- and O-linked glycosylation restricted to the first N-terminal extracellular domain. Biochemistry 1994, 33, 10463–10469. [Google Scholar] [CrossRef]
- Lin, K.; Yang, N.; Luo, W.; Qian, J.F.; Zhu, W.W.; Ye, S.J.; Yuan, C.X.; Xu, D.Y.; Liang, G.; Huang, W.J.; et al. Direct cardio-protection of Dapagliflozin against obesity-related cardiomyopathy via NHE1/MAPK signaling. Acta Pharmacol. Sin. 2022. [Google Scholar] [CrossRef]
- Masereel, B.; Pochet, L.; Laeckmann, D. An overview of inhibitors of Na(+)/H(+) exchanger. Eur. J. Med. Chem. 2003, 38, 547–554. [Google Scholar] [CrossRef]
- Orlowski, J.; Kandasamy, R.A.; Shull, G.E. Molecular cloning of putative members of the Na/H exchanger gene family. cDNA cloning, deduced amino acid sequence, and mRNA tissue expression of the rat Na/H exchanger NHE-1 and two structurally related proteins. J. Biol. Chem. 1992, 267, 9331–9339. [Google Scholar] [CrossRef]
- Schultheis, P.J.; Clarke, L.L.; Meneton, P.; Harline, M.; Boivin, G.P.; Stemmermann, G.; Duffy, J.J.; Doetschman, T.; Miller, M.L.; Shull, G.E. Targeted disruption of the murine Na+/H+ exchanger isoform 2 gene causes reduced viability of gastric parietal cells and loss of net acid secretion. J. Clin. Investig. 1998, 101, 1243–1253. [Google Scholar] [CrossRef]
- Uniprot.org. 2022. Available online: https://www.uniprot.org/ (accessed on 1 September 2022).
- Gurney, M.A.; Laubitz, D.; Ghishan, F.K.; Kiela, P.R. Pathophysiology of Intestinal Na(+)/H(+) exchange. Cell Mol. Gastroenterol. Hepatol. 2017, 3, 27–40. [Google Scholar] [CrossRef]
- Daniel, H. Molecular and integrative physiology of intestinal peptide transport. Annu. Rev. Physiol. 2004, 66, 361–384. [Google Scholar] [CrossRef]
- Johansson, S.; Rosenbaum, D.P.; Palm, J.; Stefansson, B.; Knutsson, M.; Lisbon, E.A.; Hilgendorf, C. Tenapanor administration and the activity of the H(+) -coupled transporter PepT1 in healthy volunteers. Br. J. Clin. Pharmacol. 2017, 83, 2008–2014. [Google Scholar] [CrossRef] [PubMed]
- Pizzonia, J.H.; Biemesderfer, D.; Abu-Alfa, A.K.; Wu, M.S.; Exner, M.; Isenring, P.; Igarashi, P.; Aronson, P.S. Immunochemical characterization of Na+/H+ exchanger isoform NHE4. Am. J. Physiol. 1998, 275, F510–F517. [Google Scholar] [CrossRef] [PubMed]
- Chambrey, R.; Achard, J.M.; Warnock, D.G. Heterologous expression of rat NHE4: A highly amiloride-resistant Na+/H+ exchanger isoform. Am. J. Physiol. 1997, 272 Pt 1, C90–C98. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.H.; Numata, Y.; Numata, M. Endosomal Na+/H+ exchanger NHE5 influences MET recycling and cell migration. Mol. Biol. Cell 2016, 27, 702–715. [Google Scholar] [CrossRef] [PubMed]
- Diering, G.H.; Numata, M. Endosomal pH in neuronal signaling and synaptic transmission: Role of Na(+)/H(+) exchanger NHE5. Front. Physiol. 2014, 4, 412. [Google Scholar] [CrossRef]
- Garlid, K.D. Mitochondrial cation transport: A progress report. J. Bioenerg. Biomembr. 1994, 26, 537–542. [Google Scholar] [CrossRef]
- Pescosolido, M.F.; Stein, D.M.; Schmidt, M.; El Achkar, C.M.; Sabbagh, M.; Rogg, J.M.; Tantravahi, U.; McLean, R.L.; Liu, J.S.; Poduri, A.; et al. Genetic and phenotypic diversity of NHE6 mutations in Christianson syndrome. Ann. Neurol. 2014, 76, 581–593. [Google Scholar] [CrossRef]
- Ohgaki, R.; Matsushita, M.; Kanazawa, H.; Ogihara, S.; Hoekstra, D.; van Ijzendoorn, S.C. The Na+/H+ exchanger NHE6 in the endosomal recycling system is involved in the development of apical bile canalicular surface domains in HepG2 cells. Mol. Biol. Cell 2010, 21, 1293–1304. [Google Scholar] [CrossRef]
- Xian, X.; Pohlkamp, T.; Durakoglugil, M.S.; Wong, C.H.; Beck, J.K.; Lane-Donovan, C.; Plattner, F.; Herz, J. Reversal of ApoE4-induced recycling block as a novel prevention approach for Alzheimer’s disease. Elife 2018, 7. [Google Scholar] [CrossRef]
- Numata, M.; Orlowski, J. Molecular cloning and characterization of a novel (Na+,K+)/H+ exchanger localized to the trans-Golgi network. J. Biol. Chem. 2001, 276, 17387–17394. [Google Scholar] [CrossRef] [Green Version]
- Kagami, T.; Chen, S.; Memar, P.; Choi, M.; Foster, L.J.; Numata, M. Identification and biochemical characterization of the SLC9A7 interactome. Mol. Membr. Biol. 2008, 25, 436–447. [Google Scholar] [CrossRef] [PubMed]
- Nikolovska, K.; Seidler, U.E.; Stock, C. The Role of Plasma Membrane Sodium/Hydrogen Exchangers in Gastrointestinal Functions: Proliferation and Differentiation, Fluid/Electrolyte Transport and Barrier Integrity. Front. Physiol. 2022, 13, 899286. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhang, B.; Li, J.; Chen, H.; Tooley, J.; Ghishan, F.K. Epidermal growth factor inhibits intestinal NHE8 expression via reducing its basal transcription. Am. J. Physiol. Cell Physiol. 2010, 299, C51–C57. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, N.; Tanaka, S.; Teko, Y.; Mitsui, K.; Kanazawa, H. Four Na+/H+ exchanger isoforms are distributed to Golgi and post-Golgi compartments and are involved in organelle pH regulation. J. Biol. Chem. 2005, 280, 1561–1572. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Ghishan, F.K.; Kiela, P.R. SLC9 Gene Family: Function, Expression, and Regulation. Compr. Physiol. 2018, 8, 555–583. [Google Scholar] [CrossRef]
- Kujala, M.; Hihnala, S.; Tienari, J.; Kaunisto, K.; Hastbacka, J.; Holmberg, C.; Kere, J.; Hoglund, P. Expression of ion transport-associated proteins in human efferent and epididymal ducts. Reproduction 2007, 133, 775–784. [Google Scholar] [CrossRef]
- Wang, D.; King, S.M.; Quill, T.A.; Doolittle, L.K.; Garbers, D.L. A new sperm-specific Na+/H+ exchanger required for sperm motility and fertility. Nat. Cell Biol. 2003, 5, 1117–1122. [Google Scholar] [CrossRef]
- Mine, Y.; Shuto, T.; Nikawa, H.; Kawai, T.; Ohara, M.; Kawahara, K.; Ohta, K.; Kukita, T.; Terada, Y.; Makihira, S. Inhibition of RANKL-dependent cellular fusion in pre-osteoclasts by amiloride and a NHE10-specific monoclonal antibody. Cell Biol. Int. 2015, 39, 696–709. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, T.; Park, E.S.; Yang, S.; Jeong, D.; Choi, Y.; Rho, J. NHE10, an osteoclast-specific member of the Na+/H+ exchanger family, regulates osteoclast differentiation and survival [corrected]. Biochem. Biophys. Res. Commun. 2008, 369, 320–326. [Google Scholar] [CrossRef]
- Windler, F.; Bonigk, W.; Korschen, H.G.; Grahn, E.; Strunker, T.; Seifert, R.; Kaupp, U.B. The solute carrier SLC9C1 is a Na(+)/H(+)-exchanger gated by an S4-type voltage-sensor and cyclic-nucleotide binding. Nat. Commun. 2018, 9, 2809. [Google Scholar] [CrossRef] [Green Version]
- Ye, G.; Chen, C.; Han, D.; Xiong, X.; Kong, Y.; Wan, B.; Yu, L. Cloning of a novel human NHEDC1 (Na+/H+ exchanger like domain containing 1) gene expressed specifically in testis. Mol. Biol. Rep. 2006, 33, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Xiang, M.; Feng, M.; Muend, S.; Rao, R. A human Na+/H+ antiporter sharing evolutionary origins with bacterial NhaA may be a candidate gene for essential hypertension. Proc. Natl. Acad. Sci. USA 2007, 104, 18677–18681. [Google Scholar] [CrossRef] [PubMed]
- Deisl, C.; Simonin, A.; Anderegg, M.; Albano, G.; Kovacs, G.; Ackermann, D.; Moch, H.; Dolci, W.; Thorens, B.; Hediger, M.A.; et al. Sodium/hydrogen exchanger NHA2 is critical for insulin secretion in beta-cells. Proc. Natl. Acad. Sci. USA 2013, 110, 10004–10009. [Google Scholar] [CrossRef]
- Sardet, C.; Franchi, A.; Pouyssegur, J. Molecular cloning, primary structure, and expression of the human growth factor-activatable Na+/H+ antiporter. Cell 1989, 56, 271–280. [Google Scholar] [CrossRef]
- Orlowski, J.; Grinstein, S. Diversity of the mammalian sodium/proton exchanger SLC9 gene family. Pflugers Arch. 2004, 447, 549–565. [Google Scholar] [CrossRef]
- Tse, C.M.; Brant, S.R.; Walker, M.S.; Pouyssegur, J.; Donowitz, M. Cloning and sequencing of a rabbit cDNA encoding an intestinal and kidney-specific Na+/H+ exchanger isoform (NHE-3). J. Biol. Chem. 1992, 267, 9340–9346. [Google Scholar] [CrossRef]
- Malakooti, J.; Dahdal, R.Y.; Schmidt, L.; Layden, T.J.; Dudeja, P.K.; Ramaswamy, K. Molecular cloning, tissue distribution, and functional expression of the human Na(+)/H(+) exchanger NHE2. Am. J. Physiol. 1999, 277, G383–G390. [Google Scholar] [CrossRef]
- Orlowski, J.; Grinstein, S. Na+/H+ exchangers of mammalian cells. J. Biol. Chem. 1997, 272, 22373–22376. [Google Scholar] [CrossRef]
- Khurana, S.; Nath, S.K.; Levine, S.A.; Bowser, J.M.; Tse, C.M.; Cohen, M.E.; Donowitz, M. Brush border phosphatidylinositol 3-kinase mediates epidermal growth factor stimulation of intestinal NaCl absorption and Na+/H+ exchange. J. Biol. Chem. 1996, 271, 9919–9927. [Google Scholar] [CrossRef]
- Xu, H.; Collins, J.F.; Bai, L.; Kiela, P.R.; Lynch, R.M.; Ghishan, F.K. Epidermal growth factor regulation of rat NHE2 gene expression. Am. J. Physiol. Cell Physiol. 2001, 281, C504–C513. [Google Scholar] [CrossRef]
- Xu, H.; Zhang, B.; Li, J.; Chen, H.; Wang, C.; Ghishan, F.K. Transcriptional inhibition of intestinal NHE8 expression by glucocorticoids involves Pax5. Am. J. Physiol. Gastrointest. Liver Physiol. 2010, 299, G921–G927. [Google Scholar] [CrossRef]
- Schultheis, P.J.; Clarke, L.L.; Meneton, P.; Miller, M.L.; Soleimani, M.; Gawenis, L.R.; Riddle, T.M.; Duffy, J.J.; Doetschman, T.; Wang, T.; et al. Renal and intestinal absorptive defects in mice lacking the NHE3 Na+/H+ exchanger. Nat. Genet. 1998, 19, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Ledoussal, C.; Woo, A.L.; Miller, M.L.; Shull, G.E. Loss of the NHE2 Na(+)/H(+) exchanger has no apparent effect on diarrheal state of NHE3-deficient mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2001, 281, G1385–G1396. [Google Scholar] [CrossRef]
- Xu, H.; Li, J.; Chen, R.; Zhang, B.; Wang, C.; King, N.; Chen, H.; Ghishan, F.K. NHE2X3 DKO mice exhibit gender-specific NHE8 compensation. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 300, G647–G653. [Google Scholar] [CrossRef] [PubMed]
- Barker, N. Adult intestinal stem cells: Critical drivers of epithelial homeostasis and regeneration. Nat. Rev. Mol. Cell Biol. 2014, 15, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Umar, S. Intestinal stem cells. Curr. Gastroenterol. Rep. 2010, 12, 340–348. [Google Scholar] [CrossRef]
- Maloy, K.J.; Powrie, F. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 2011, 474, 298–306. [Google Scholar] [CrossRef]
- Zhang, S.; Qiang, R.; Dong, Y.; Zhang, Y.; Chen, Y.; Zhou, H.; Gao, X.; Chai, R. Hair cell regeneration from inner ear progenitors in the mammalian cochlea. Am. J. Stem Cells 2020, 9, 25–35. [Google Scholar]
- Bray, S.J. Notch signalling: A simple pathway becomes complex. Nat. Rev. Mol. Cell Biol. 2006, 7, 678–689. [Google Scholar] [CrossRef]
- Xu, H.; Zhang, B.; Li, J.; Wang, C.; Chen, H.; Ghishan, F.K. Impaired mucin synthesis and bicarbonate secretion in the colon of NHE8 knockout mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, G335–G343. [Google Scholar] [CrossRef]
- Wang, A.; Li, J.; Zhao, Y.; Johansson, M.E.; Xu, H.; Ghishan, F.K. Loss of NHE8 expression impairs intestinal mucosal integrity. Am. J. Physiol. Gastrointest. Liver Physiol. 2015, 309, G855–G864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernardazzi, C.; Pego, B.; de Souza, H.S. Neuroimmunomodulation in the Gut: Focus on Inflammatory Bowel Disease. Mediators Inflamm. 2016, 2016, 1363818. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Xu, H.; Zhang, B.; Johansson, M.E.; Li, J.; Hansson, G.C.; Ghishan, F.K. NHE8 plays an important role in mucosal protection via its effect on bacterial adhesion. Am. J. Physiol. Cell Physiol. 2013, 305, C121–C128. [Google Scholar] [CrossRef] [PubMed]
- Bernardazzi, C.; Xu, H.; Tong, H.; Laubitz, D.; Figliuolo da Paz, V.; Curiel, L.; Ghishan, F.K. An indisputable role of NHE8 in mucosal protection. Am. J. Physiol. Gastrointest. Liver Physiol. 2020, 319, G421–G431. [Google Scholar] [CrossRef]
- Kiela, P.R.; Ghishan, F.K. Ion transport in the intestine. Curr. Opin. Gastroenterol. 2009, 25, 87–91. [Google Scholar] [CrossRef]
- Sheikh, I.A.; Koley, H.; Chakrabarti, M.K.; Hoque, K.M. The Epac1 signaling pathway regulates Cl- secretion via modulation of apical KCNN4c channels in diarrhea. J. Biol. Chem. 2013, 288, 20404–20415. [Google Scholar] [CrossRef]
- Petri, W.A., Jr.; Miller, M.; Binder, H.J.; Levine, M.M.; Dillingham, R.; Guerrant, R.L. Enteric infections, diarrhea, and their impact on function and development. J. Clin. Investig. 2008, 118, 1277–1290. [Google Scholar] [CrossRef]
- Aronson, P.S. Ion exchangers mediating NaCl transport in the renal proximal tubule. Cell Biochem. Biophys. 2002, 36, 147–153. [Google Scholar] [CrossRef]
- Lewin, M.J. The somatostatin receptor in the GI tract. Annu. Rev. Physiol. 1992, 54, 455–468. [Google Scholar] [CrossRef]
- Wang, C.; Xu, H.; Chen, H.; Li, J.; Zhang, B.; Tang, C.; Ghishan, F.K. Somatostatin stimulates intestinal NHE8 expression via p38 MAPK pathway. Am. J. Physiol. Cell Physiol. 2011, 300, C375–C382. [Google Scholar] [CrossRef]
- Lei, X.; Cai, L.; Li, X.; Xu, H.; Geng, C.; Wang, C. Up-regulation of NHE8 by somatostatin ameliorates the diarrhea symptom in infectious colitis mice model. Korean J. Physiol. Pharmacol. 2018, 22, 269–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Cai, L.; Xu, H.; Geng, C.; Lu, J.; Tao, L.; Sun, D.; Ghishan, F.K.; Wang, C. Somatostatin regulates NHE8 protein expression via the ERK1/2 MAPK pathway in DSS-induced colitis mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 311, G954–G963. [Google Scholar] [CrossRef] [PubMed]
- Hammer, A.M.; Morris, N.L.; Earley, Z.M.; Choudhry, M.A. The First Line of Defense: The Effects of Alcohol on Post-Burn Intestinal Barrier, Immune Cells, and Microbiome. Alcohol. Res. 2015, 37, 209–222. [Google Scholar] [PubMed]
- Koveitypour, Z.; Panahi, F.; Vakilian, M.; Peymani, M.; Seyed Forootan, F.; Nasr Esfahani, M.H.; Ghaedi, K. Signaling pathways involved in colorectal cancer progression. Cell Biosci. 2019, 9, 97. [Google Scholar] [CrossRef]
- Pandurangan, A.K.; Divya, T.; Kumar, K.; Dineshbabu, V.; Velavan, B.; Sudhandiran, G. Colorectal carcinogenesis: Insights into the cell death and signal transduction pathways: A review. World J. Gastrointest. Oncol. 2018, 10, 244–259. [Google Scholar] [CrossRef]
- Yoshimoto, A.N.; Bernardazzi, C.; Carneiro, A.J.; Elia, C.C.; Martinusso, C.A.; Ventura, G.M.; Castelo-Branco, M.T.; de Souza, H.S. Hedgehog pathway signaling regulates human colon carcinoma HT-29 epithelial cell line apoptosis and cytokine secretion. PLoS ONE 2012, 7, e45332. [Google Scholar] [CrossRef]
- Preisler, L.; Habib, A.; Shapira, G.; Kuznitsov-Yanovsky, L.; Mayshar, Y.; Carmel-Gross, I.; Malcov, M.; Azem, F.; Shomron, N.; Kariv, R.; et al. Heterozygous APC germline mutations impart predisposition to colorectal cancer. Sci. Rep. 2021, 11, 5113. [Google Scholar] [CrossRef]
- Aghabozorgi, A.S.; Bahreyni, A.; Soleimani, A.; Bahrami, A.; Khazaei, M.; Ferns, G.A.; Avan, A.; Hassanian, S.M. Role of adenomatous polyposis coli (APC) gene mutations in the pathogenesis of colorectal cancer; current status and perspectives. Biochimie 2019, 157, 64–71. [Google Scholar] [CrossRef]
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 2010, 127, 2893–2917. [Google Scholar] [CrossRef]
- Lin, Y.; Chang, G.; Wang, J.; Jin, W.; Wang, L.; Li, H.; Ma, L.; Li, Q.; Pang, T. NHE1 mediates MDA-MB-231 cells invasion through the regulation of MT1-MMP. Exp. Cell Res. 2011, 317, 2031–2040. [Google Scholar] [CrossRef]
- Zhang, M.; Li, T.; Zhu, J.; Tuo, B.; Liu, X. Physiological and pathophysiological role of ion channels and transporters in the colorectum and colorectal cancer. J. Cell Mol. Med. 2020, 24, 9486–9494. [Google Scholar] [CrossRef] [PubMed]
- Cardone, R.A.; Casavola, V.; Reshkin, S.J. The role of disturbed pH dynamics and the Na+/H+ exchanger in metastasis. Nat. Rev. Cancer 2005, 5, 786–795. [Google Scholar] [CrossRef] [PubMed]
- Laubitz, D.; Harrison, C.A.; Midura-Kiela, M.T.; Ramalingam, R.; Larmonier, C.B.; Chase, J.H.; Caporaso, J.G.; Besselsen, D.G.; Ghishan, F.K.; Kiela, P.R. Reduced Epithelial Na+/H+ Exchange Drives Gut Microbial Dysbiosis and Promotes Inflammatory Response in T Cell-Mediated Murine Colitis. PLoS ONE 2016, 11, e0152044. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Chen, H.; Dong, J.; Li, J.; Chen, R.; Uno, J.K.; Ghishan, F.K. Tumor necrosis factor-{alpha} downregulates intestinal NHE8 expression by reducing basal promoter activity. Am. J. Physiol. Cell Physiol. 2009, 296, C489–C497. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Li, J.; Chen, H.; Ghishan, F.K. NHE8 Deficiency Promotes Colitis-Associated Cancer in Mice via Expansion of Lgr5-Expressing Cells. Cell Mol. Gastroenterol. Hepatol. 2019, 7, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Nakhoul, N.; Batuman, V. Role of proximal tubules in the pathogenesis of kidney disease. Contrib. Nephrol. 2011, 169, 37–50. [Google Scholar] [CrossRef]
- Becker, A.M.; Zhang, J.; Goyal, S.; Dwarakanath, V.; Aronson, P.S.; Moe, O.W.; Baum, M. Ontogeny of NHE8 in the rat proximal tubule. Am. J. Physiol. Renal Physiol. 2007, 293, F255–F261. [Google Scholar] [CrossRef]
- Choi, J.Y.; Shah, M.; Lee, M.G.; Schultheis, P.J.; Shull, G.E.; Muallem, S.; Baum, M. Novel amiloride-sensitive sodium-dependent proton secretion in the mouse proximal convoluted tubule. J. Clin. Investig. 2000, 105, 1141–1146. [Google Scholar] [CrossRef]
- Goyal, S.; Vanden Heuvel, G.; Aronson, P.S. Renal expression of novel Na+/H+ exchanger isoform NHE8. Am. J. Physiol. Renal Physiol. 2003, 284, F467–F473. [Google Scholar] [CrossRef]
- Gattineni, J.; Sas, D.; Dagan, A.; Dwarakanath, V.; Baum, M. Effect of thyroid hormone on the postnatal renal expression of NHE8. Am. J. Physiol. Renal Physiol. 2008, 294, F198–F204. [Google Scholar] [CrossRef]
- Twombley, K.; Gattineni, J.; Bobulescu, I.A.; Dwarakanath, V.; Baum, M. Effect of metabolic acidosis on neonatal proximal tubule acidification. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R1360–R1368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pirojsakul, K.; Gattineni, J.; Dwarakanath, V.; Baum, M. Renal NHE expression and activity in neonatal NHE3- and NHE8-null mice. Am. J. Physiol. Renal Physiol. 2015, 308, F31–F38. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Bobulescu, I.A.; Goyal, S.; Aronson, P.S.; Baum, M.G.; Moe, O.W. Characterization of Na+/H+ exchanger NHE8 in cultured renal epithelial cells. Am. J. Physiol. Renal Physiol. 2007, 293, F761–F766. [Google Scholar] [CrossRef] [PubMed]
- Joseph, C.; Twombley, K.; Gattineni, J.; Zhang, Q.; Dwarakanath, V.; Baum, M. Acid increases NHE8 surface expression and activity in NRK cells. Am. J. Physiol. Renal Physiol. 2012, 302, F495–F503. [Google Scholar] [CrossRef]
- Baum, M.; Twombley, K.; Gattineni, J.; Joseph, C.; Wang, L.; Zhang, Q.; Dwarakanath, V.; Moe, O.W. Proximal tubule Na+/H+ exchanger activity in adult NHE8-/-, NHE3-/-, and NHE3-/-/NHE8-/- mice. Am. J. Physiol. Renal Physiol. 2012, 303, F1495–F1502. [Google Scholar] [CrossRef]
- Miyake, H.; Mori, N.; Mano, H.; Imanaka, T.; Nakamura, M. Development of a highly sensitive and reliable enzyme-linked immunosorbent assay for MUC5AC in human tears extracted from Schirmer strips. Clin. Ophthalmol. 2018, 12, 1571–1580. [Google Scholar] [CrossRef]
- The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul. Surf. 2007, 5, 75–92. [CrossRef]
- Mazzoni, F.; Safa, H.; Finnemann, S.C. Understanding photoreceptor outer segment phagocytosis: Use and utility of RPE cells in culture. Exp. Eye Res. 2014, 126, 51–60. [Google Scholar] [CrossRef]
- Xia, C.H.; Ferguson, I.; Li, M.; Kim, A.; Onishi, A.; Li, L.; Su, B.; Gong, X. Essential function of NHE8 in mouse retina demonstrated by AAV-mediated CRISPR/Cas9 knockdown. Exp. Eye Res. 2018, 176, 29–39. [Google Scholar] [CrossRef]
- Zegers-Hochschild, F.; Adamson, G.D.; Dyer, S.; Racowsky, C.; de Mouzon, J.; Sokol, R.; Rienzi, L.; Sunde, A.; Schmidt, L.; Cooke, I.D.; et al. The International Glossary on Infertility and Fertility Care, 2017. Hum. Reprod. 2017, 32, 1786–1801. [Google Scholar] [CrossRef]
- Cavallini, G. Male idiopathic oligoasthenoteratozoospermia. Asian J. Androl. 2006, 8, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Vander Borght, M.; Wyns, C. Fertility and infertility: Definition and epidemiology. Clin. Biochem. 2018, 62, 2–10. [Google Scholar] [CrossRef]
- Xu, H.; Chen, H.; Li, J.; Zhao, Y.; Ghishan, F.K. Disruption of NHE8 expression impairs Leydig cell function in the testes. Am. J. Physiol. Cell Physiol. 2015, 308, C330–C338. [Google Scholar] [CrossRef]
- Hihnala, S.; Kujala, M.; Toppari, J.; Kere, J.; Holmberg, C.; Hoglund, P. Expression of SLC26A3, CFTR and NHE3 in the human male reproductive tract: Role in male subfertility caused by congenital chloride diarrhoea. Mol. Hum. Reprod. 2006, 12, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Oberheide, K.; Puchkov, D.; Jentsch, T.J. Loss of the Na(+)/H(+) exchanger NHE8 causes male infertility in mice by disrupting acrosome formation. J. Biol. Chem. 2017, 292, 10845–10854. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Clarke, L.; Nie, R.; Carnes, K.; Lai, L.W.; Lien, Y.H.; Verkman, A.; Lubahn, D.; Fisher, J.S.; Katzenellenbogen, B.S.; et al. Estrogen action and male fertility: Roles of the sodium/hydrogen exchanger-3 and fluid reabsorption in reproductive tract function. Proc. Natl. Acad. Sci. USA 2001, 98, 14132–14137. [Google Scholar] [CrossRef] [PubMed]
- Golkowski, M.; Shimizu-Albergine, M.; Suh, H.W.; Beavo, J.A.; Ong, S.E. Studying mechanisms of cAMP and cyclic nucleotide phosphodiesterase signaling in Leydig cell function with phosphoproteomics. Cell. Signal. 2016, 28, 764–778. [Google Scholar] [CrossRef]
- Cao, L.; Yuan, Z.; Liu, M.; Stock, C. (Patho-)Physiology of Na(+)/H(+) Exchangers (NHEs) in the Digestive System. Front. Physiol. 2019, 10, 1566. [Google Scholar] [CrossRef]
- Xu, H.; Chen, R.; Ghishan, F.K. Subcloning, localization, and expression of the rat intestinal sodium-hydrogen exchanger isoform 8. Am. J. Physiol. Gastrointest. Liver Physiol. 2005, 289, G36–G41. [Google Scholar] [CrossRef]
- Kinaneh, S.; Knany, Y.; Khoury, E.E.; Ismael-Badarneh, R.; Hamoud, S.; Berger, G.; Abassi, Z.; Azzam, Z.S. Identification, localization and expression of NHE isoforms in the alveolar epithelial cells. PLoS ONE 2021, 16, e0239240. [Google Scholar] [CrossRef]

| Subdivision | Coding Gene | Molecular Weight | Inhibitors | Localization | Function | Ref. |
|---|---|---|---|---|---|---|
| NHE1 | SLC9A1 | 820aa, ~90 kDa | Amiloride, EIPA, HMA, DMA, HOE-694, SM-20550, S-3226, Clonidine, Cimetidine | It is ubiquitously expressed in nearly all mammalian tissue types and localized basolaterally in every epithelial cell, except in the choroid plexus and syncytio-throphoblast of the human placenta where it expresses apically | It regulates cell volume, intracellular pH, proliferation, differentiation, and apoptosis | [8,13,14,15,16] |
| NHE2 | SLC9A2 | 812aa, ~90 kDa | Amiloride, EIPA, DMA, S-3226 | Highly expressed in intestine and kidney | The physiologic role of NHE2 still remains elusive despite its wide expression pattern with higher expression levels in the intestine and the kidney | [16,17,18,19] |
| NHE3 | SLC9A3 | 834aa, ~92 kDa | Amiloride, Tenapanor, HMA, DMA, HOE-694, Zoniporide, S-3226, Clonidine, Cimetidine | Highly expressed in intestine and kidney | It plays an important role in mediating intestinal electroneutral NaCl absorption in mammals. It also contributes to the absorption of other nutrients, such as amino acids and dipeptides through H+ gradients | [8,16,19,20,21,22] |
| NHE4 | SLC9A4 | 798aa, ~70 kDa | Amiloride, EIPA | NHE4 is highly expressed in the stomach while its expression is low in kidney, intestine, brain, ureter, skeletal muscle, heart, liver, and spleen | It plays a major role in intracellular pH homeostasis | [16,19,23,24] |
| NHE5 | SLC9A5 | 896aa, ~100 kDa | Amiloride, EIPA, HMA, HOE-694, Cimetidine | Predominantly expressed in brain | It regulates growth factor signaling, integrin trafficking, and degradation of glioma cells. It also functions as a negative regulator of dendritic spine growth | [16,19,25,26] |
| NHE6 | SLC9A6 | 669aa, ~85 kDa | Rimeporide | It is highly expressed in skeletal muscles, brain, and heart | It functions to regulate intramitochondrial Na+ and H+ gradients | [19,27,28,29,30] |
| NHE7 | SLC9A7 | 725aa, ~80 kDa | Amiloride | Predominantly localized in the trans-Golgi network | It is prominently expressed in the trans-Golgi network and in the mid-trans-Golgi stacks, and functions as a K+/H+ exchanger in controlling organelle volume through transmembrane K+ flux | [16,19,31,32] |
| NHE8 | SLC9A8 | 581aa, ~65 kDa | HOE-642, S-3226 | NHE8 protein has been detected in the plasma membrane, Golgi apparatus, and endosomes. It is ubiquitously expressed in many tissues | NHE8 is involved in electroneutral NaCl transport, cell volume regulation, cellular adhesion, migration, and proliferation | [6,7,9,19,33,34] |
| NHE9 | SLC9A9 | 645aa, ~72 kDa | Unknown | It is expressed mostly in heart, skeletal muscle, and brain | It transports the protons out of the endosomal lumen in exchange for Na+/K+, thus controlling the pH of endosomal lumens | [35,36] |
| NHE10 | SLC9C1 | 1177aa, ~135 kDa | Unknown | Predominantly expressed in testis and in osteoclasts | NHE10 is associated with sperm motility and fertility, and it is required for osteoclasts differentiation and survivor | [19,37,38,39,40,41] |
| NHE11 | SLC9C2 | 1124aa, ~130 kDa | Unknown | Expressed in the brain, choroid plexus, testis, and uterine tube | Unknown | [19] |
| NHA1 | SLC9B1 | 515aa, ~55 kDa | Unknown | Expressed in testis | It regulates the pH and the cell volume | [19,42] |
| NHA2 | SLC9B2 | 537aa, ~57 kDa | Phloretin | It is ubiquitously expressed in mouse tissues | It regulates the pH and the cell volume | [19,43,44] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernardazzi, C.; Sheikh, I.A.; Xu, H.; Ghishan, F.K. The Physiological Function and Potential Role of the Ubiquitous Na+/H+ Exchanger Isoform 8 (NHE8): An Overview Data. Int. J. Mol. Sci. 2022, 23, 10857. https://doi.org/10.3390/ijms231810857
Bernardazzi C, Sheikh IA, Xu H, Ghishan FK. The Physiological Function and Potential Role of the Ubiquitous Na+/H+ Exchanger Isoform 8 (NHE8): An Overview Data. International Journal of Molecular Sciences. 2022; 23(18):10857. https://doi.org/10.3390/ijms231810857
Chicago/Turabian StyleBernardazzi, Claudio, Irshad Ali Sheikh, Hua Xu, and Fayez K. Ghishan. 2022. "The Physiological Function and Potential Role of the Ubiquitous Na+/H+ Exchanger Isoform 8 (NHE8): An Overview Data" International Journal of Molecular Sciences 23, no. 18: 10857. https://doi.org/10.3390/ijms231810857





