Psychotropic Drug Effects on Steroid Stress Hormone Release and Possible Mechanisms Involved
Abstract
1. Introduction
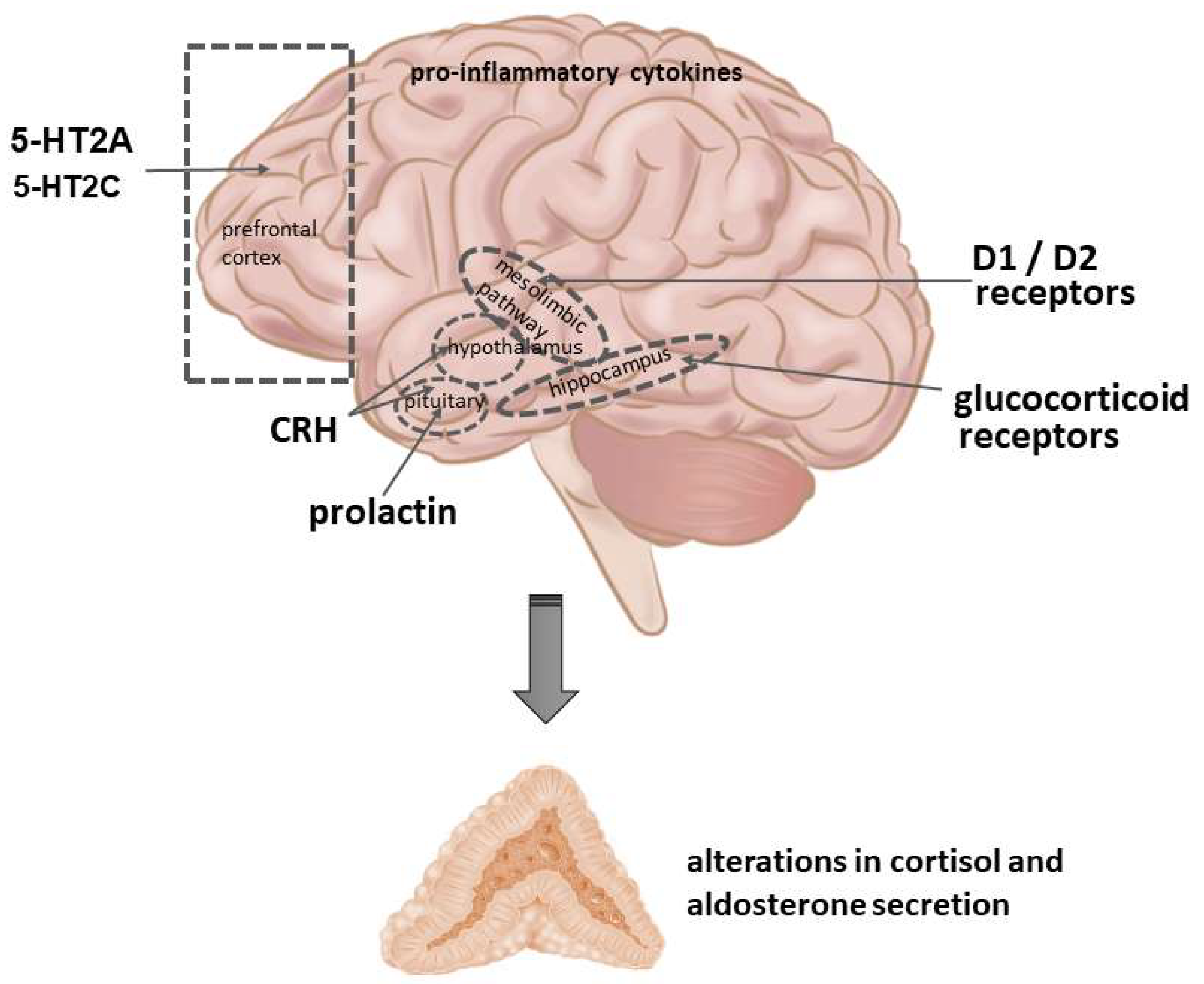
2. Potential Molecular Mechanisms to Influence Adrenocortical Function
2.1. Neurotransmitter Receptors
2.2. Cytokines
2.3. Endocrine Factors
2.4. Trophic Factors and Adult Neurogenesis
2.5. Hypothalamic Clock Gene Regulatory Mechanisms
2.6. Epigenetic and Glucocorticoid Receptor-Related Factors
2.7. Enzymes Involved in Steroidogenesis and Signaling Pathways
3. Antipsychotic Drugs, Lithium and Cortisol Release
3.1. Effects of Antipsychotic Drugs on Cortisol Release in Healthy Subjects
3.1.1. Single Treatments
3.1.2. Repeated Treatments
3.2. Effects of Antipsychotic Drugs and Lithium on Cortisol Release in Patients
3.2.1. Repeated Treatments
3.2.2. Long-Term Treatments
4. Antipsychotic Drugs, Lithium and Aldosterone Release
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jezova, D.; Herman, J.P. Stress and stress-related disease states as topics of multi-approach research. Stress 2020, 23, 615–616. [Google Scholar] [CrossRef]
- Koolhaas, J.; Bartolomucci, A.; Buwalda, B.; de Boer, S.; Flügge, G.; Korte, S.M.; Meerlo, P.; Murison, R.; Olivier, B.; Palanza, P.; et al. Stress revisited: A critical evaluation of the stress concept. Neurosci. Biobehav. Rev. 2011, 35, 1291–1301. [Google Scholar] [CrossRef]
- Jezová, D.; Juránková, E.; Mosnárová, A.; Kriska, M.; Skultétyová, I. Neuroendocrine response during stress with relation to gender differences. Acta Neurobiol. Exp. 1996, 56, 779–785. [Google Scholar]
- Jezova, D.; Hlavacova, N. Endocrine Factors in Stress and Psychiatric Disorders: Focus on Anxiety and Salivary Steroids. Ann. N. Y. Acad. Sci. 2008, 1148, 495–503. [Google Scholar] [CrossRef]
- Jezova, D.; Balagova, L.; Chmelova, M.; Hlavacova, N. Classical Steroids in a New Fashion: Focus on Testosterone and Aldosterone. Curr. Protein Pept. Sci. 2019, 20, 1112–1118. [Google Scholar] [CrossRef]
- Murck, H.; Adolf, C.; Schneider, A.; Schlageter, L.; Heinrich, D.; Ritzel, K.; Sturm, L.; Quinkler, M.; Beuschlein, F.; Reincke, M.; et al. Differential effects of reduced mineralocorticoid receptor activation by unilateral adrenalectomy vs. mineralocorticoid antagonist treatment in patients with primary aldosteronism—Implications for depression and anxiety. J. Psychiatr. Res. 2021, 137, 376–382. [Google Scholar] [CrossRef]
- Geerling, J.C.; Kawata, M.; Loewy, A.D. Aldosterone-sensitive neurons in the rat central nervous system. J. Comp. Neurol. 2006, 494, 515–527. [Google Scholar] [CrossRef]
- Hlavacova, N.; Jezova, D. Chronic treatment with the mineralocorticoid hormone aldosterone results in increased anxiety-like behavior. Horm. Behav. 2008, 54, 90–97. [Google Scholar] [CrossRef]
- Hlavacova, N.; Wes, P.D.; Ondrejcakova, M.; Flynn, M.E.; Poundstone, P.K.; Babic, S.; Murck, H.; Jezova, D. Subchronic treatment with aldosterone induces depression-like behaviours and gene expression changes relevant to major depressive disorder. Int. J. Neuropsychopharmacol. 2012, 15, 247–265. [Google Scholar] [CrossRef]
- Sullivan, R.M.; Dufresne, M.M. Mesocortical dopamine and HPA axis regulation: Role of laterality and early environment. Brain Res. 2006, 1076, 49–59. [Google Scholar] [CrossRef]
- Belda, X.; Armario, A. Dopamine D1 and D2 dopamine receptors regulate immobilization stress-induced activation of the hypothalamus-pituitary-adrenal axis. Psychopharmacology 2009, 206, 355–365. [Google Scholar] [CrossRef]
- Ježová, D.; Jurčovičová, J.; Vigaš, M.; Murgaš, K.; Labrie, F. Increase in plasma ACTH after dopaminergic stimulation in rats. Psychopharmacology 1985, 85, 201–203. [Google Scholar] [CrossRef]
- Borowsky, B.; Kuhn, C.M. D1 and D2 Dopamine Receptors Stimulate Hypothalamo-Pituitary-Adrenal Activity in Rats. Neuropharmacology 1992, 31, 671–678. [Google Scholar] [CrossRef]
- Foreman, M.M.; Fuller, R.W.; Hynes, M.D.; Gidda, J.S.; Nichols, C.L.; Schaus, J.M.; Kornfeld, E.C.; Clemens, J.A. Preclinical studies on quinelorane, a potent and highly selective D2-dopaminergic agonist. J. Pharmacol. Exp. Ther. 1989, 250, 227–235. [Google Scholar]
- Oswald, L.M.; Wong, D.F.; McCaul, M.; Zhou, Y.; Kuwabara, H.; Choi, L.; Brasic, J.; Wand, G.S. Relationships Among Ventral Striatal Dopamine Release, Cortisol Secretion, and Subjective Responses to Amphetamine. Neuropsychopharmacology 2005, 30, 821–832. [Google Scholar] [CrossRef]
- Wand, G.S.; Oswald, L.M.; McCaul, M.E.; Wong, D.F.; Johnson, E.; Zhou, Y.; Kuwabara, H.; Kumar, A. Association of Amphetamine-Induced Striatal Dopamine Release and Cortisol Responses to Psychological Stress. Neuropsychopharmacology 2007, 32, 2310–2320. [Google Scholar] [CrossRef]
- Amenta, F.; Chiandussi, L.; Mancini, M.; Ricci, A.; Schena, M.; Veglio, F. Pharmacological characterization and autoradiographic localization of dopamine receptors in the human adrenal cortex. Eur. J. Endocrinol. 1994, 131, 91–96. [Google Scholar] [CrossRef]
- Carey, R.M.; Thorner, M.O.; Ortt, E.M. Dopaminergic Inhibition of Metoclopramide-induced Aldosterone Secretion in Man. Dissociation of Responses to Dopamine and Bromocriptine. J. Clin. Investig. 1980, 66, 10–18. [Google Scholar] [CrossRef]
- Nagahama, S.; Fujimaki, M.; Kawabe, H.; Nakamura, R.; Saito, I.; Saruta, T. Effect of Metoclopramide on the Secretion of Aldosterone and Other Adrenocortical Steroids. Clin. Endocrinol. 1983, 18, 287–293. [Google Scholar] [CrossRef]
- Jungmann, E.; Wächtler, M.; Schwedes, U.; Usadel, K.H.; Schöffling, K. The effect of metoclopramide and haloperidol on plasma renin activity and aldosterone levels in rats. Res. Exp. Med. 1983, 183, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Hampton, T.; Ganguly, A. Metoclopramide Fails to Stimulate Aldosterone Secretion and Inhibits Serotonin-Mediated Aldosterone Secretion in the Rat. Horm. Metab. Res. 1986, 18, 754–756. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.D.; Chen, Y.M.; Chu, T.S.; Chueh, S.C.; Wu, M.H.; Bor-Shen, H. Expression and Localization of Human Dopamine D2 and D4 Receptor mRNA in the Adrenal Gland, Aldosterone-Producing Adenoma, and Pheochromocytoma. J. Clin. Endocrinol. Metab. 2001, 86, 4460–4467. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meltzer, H.; Massey, B. The role of serotonin receptors in the action of atypical antipsychotic drugs. Curr. Opin. Pharmacol. 2011, 11, 59–67. [Google Scholar] [CrossRef]
- Seibyl, J.P.; Krystal, J.H.; Price, L.H.; Woods, S.W.; D’Amico, C.; Heninger, G.R.; Charney, D.S. Effects of ritanserin on the behavioral, neuroendocrine, and cardiovascular responses to meta-chlorophenylpiperazine in healthy human subjects. Psychiatry Res. 1991, 38, 227–236. [Google Scholar] [CrossRef]
- Van De Kar, L.D.; Javed, A.; Zhang, Y.; Serres, F.; Raap, D.K.; Gray, T.S.; Raap, D.K. 5-HT2A Receptors Stimulate ACTH, Corticosterone, Oxytocin, Renin, and Prolactin Release and Activate Hypothalamic CRF and Oxytocin-Expressing Cells. J. Neurosci. 2001, 21, 3572–3579. [Google Scholar] [CrossRef]
- Hemrick-Luecke, S.K.; Evans, D.C. Comparison of the potency of MDL 100,907 and SB 242084 in blocking the serotonin (5-HT)(2) receptor agonist-induced increases in rat serum corticosterone concentrations: Evidence for 5-HT(2A) receptor mediation of the HPA axis. Neuropharmacology 2002, 42, 162–169. [Google Scholar] [CrossRef]
- Hegde, S.S.; Eglen, R.M. Peripheral 5-HT4 Receptors. FASEB J. 1996, 10, 1398–1407. [Google Scholar] [CrossRef]
- Contesse, V.; Lenglet, S.; Grumolato, L.; Anouar, Y.; Lihrmann, I.; Lefebvre, H.; Delarue, C.; Vaudry, H. Pharmacological and Molecular Characterization of 5-Hydroxytryptamine7 Receptors in the Rat Adrenal Gland. Mol. Pharmacol. 1999, 56, 552–561. [Google Scholar] [CrossRef] [PubMed]
- Pace, T.W.W.; Hu, F.; Miller, A.H. Cytokine-effects on glucocorticoid receptor function: Relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav. Immun. 2007, 21, 9–19. [Google Scholar] [CrossRef]
- Pace, T.W.W.; Miller, A.H. Cytokines and Glucocorticoid Receptor Signaling. Relevance to Major Depression. Ann. N. Y. Acad. Sci. 2009, 1179, 86–105. [Google Scholar] [CrossRef] [PubMed]
- Zunszain, P.A.; Anacker, C.; Cattaneo, A.; de Carvalho, L.A.; Pariante, C.M. Glucocorticoids, cytokines and brain abnormalities in depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 722–729. [Google Scholar] [CrossRef]
- Sugino, H.; Futamura, T.; Mitsumoto, Y.; Maeda, K.; Marunaka, Y. Atypical antipsychotics suppress production of proinflammatory cytokines and up-regulate interleukin-10 in lipopolysaccharide-treated mice. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2009, 33, 303–307. [Google Scholar] [CrossRef]
- Handley, R.; Mondelli, V.; Zelaya, F.; Marques, T.R.; Taylor, H.; Reinders, A.A.; Chaddock, C.; McQueen, G.; Hubbard, K.M.F.; Papadopoulos, A.; et al. Effects of antipsychotics on cortisol, interleukin-6 and hippocampal perfusion in healthy volunteers. Schizophr. Res. 2016, 174, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Mohanty, B. Atypical antipsychotic drug modulates early life infection induced impairment of hypothalamic-pituitary-adrenal axis: An age related study in mice. Eur. J. Pharmacol. 2020, 872, 172978. [Google Scholar] [CrossRef]
- Gustafson, P.; Kokay, I.; Sapsford, T.; Bunn, S.; Grattan, D. Prolactin regulation of the HPA axis is not mediated by a direct action upon CRH neurons: Evidence from the rat and mouse. Brain Struct. Funct. 2017, 222, 3191–3204. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.L.; Jiang, P.; Tan, Q.Y.; Dang, R.L.; Tang, M.M.; Xue, Y.; Deng, Y.; Zhang, B.K.; Fang, P.F.; Xu, P.; et al. Therapeutic efficacy of atypical antipsychotic drugs by targeting multiple stress-related metabolic pathways. Transl. Psychiatry 2017, 7, e1130. [Google Scholar] [CrossRef]
- Park, S.W.; Choi, S.M.; Lee, J.G.; Lee, C.H.; Lee, S.J.; Kim, N.R.; Kim, Y.H. Differential Effects of Ziprasidone and Haloperidol on Immobilization-Stress-Induced CRF mRNA Expression in the Hypothalamic Paraventricular Nucleus of Rats. Neuropsychobiology 2011, 63, 29–34. [Google Scholar] [CrossRef]
- Basta-Kaim, A.; Budziszewska, B.; Jaworska-Feil, L.; Tetich, M.; Kubera, M.; Leśkiewicz, M.; Otczyk, M.; Lasoń, W. Antipsychotic Drugs Inhibit the Human Corticotropin-Releasing-Hormone Gene Promoter Activity in Neuro-2A Cells—An Involvement of Protein Kinases. Neuropsychopharmacology 2006, 31, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Babic, S.; Ondrejcakova, M.; Bakos, J.; Racekova, E.; Jezova, D. Cell proliferation in the hippocampus and in the heart is modified by exposure to repeated stress and treatment with memantine. J. Psychiatr. Res. 2012, 46, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Dremencov, E.; Jezova, D.; Barak, S.; Gaburjakova, J.; Gaburjakova, M.; Kutna, V.; Ovsepian, S.V. Trophic factors as potential therapies for treatment of major mental disorders. Neurosci. Lett. 2021, 764, 136194. [Google Scholar] [CrossRef]
- Issa, G.; Wilson, C.; Terry, A.; Pillai, A. An inverse relationship between cortisol and BDNF levels in schizophrenia: Data from human postmortem and animal studies. Neurobiol. Dis. 2010, 39, 327–333. [Google Scholar] [CrossRef]
- Osacka, J.; Koprdova, R.; Tillinger, A.; Pirnik, Z.; Kiss, A. Haloperidol and aripiprazole impact on the BDNF and glucocorticoid receptor levels in the rat hippocampus and prefrontal cortex: Effect of the chronic mild stress. Endocr. Regul. 2021, 55, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Morais, M.; Patrício, P.; Mateus-Pinheiro, A.; Alves, N.D.; Machado-Santos, A.R.; Correia, J.S.; Pereira, J.; Pinto, L.; Sousa, N.; Bessa, J.M. The modulation of adult neuroplasticity is involved in the mood-improving actions of atypical antipsychotics in an animal model of depression. Transl. Psychiatry 2017, 7, e1146. [Google Scholar] [CrossRef] [PubMed]
- Ashton, A.; Jagannath, A. Disrupted Sleep and Circadian Rhythms in Schizophrenia and Their Interaction with Dopamine Signaling. Front. Neurosci. 2020, 14, 636. [Google Scholar] [CrossRef]
- Moon, E.; Lavin, P.; Storch, K.-F.; Linnaranta, O. Effects of antipsychotics on circadian rhythms in humans: A systematic review and meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 108, 110162. [Google Scholar] [CrossRef]
- Ayalon, L.; Hermesh, H.; Dagan, Y. Case Study of Circadian Rhythm Sleep Disorder Following Haloperidol Treatment: Reversal by Risperidone and Melatonin. Chronobiol. Int. 2002, 19, 947–959. [Google Scholar] [CrossRef] [PubMed]
- Wirz-Justice, A.; Cajochen, C.; Nussbaum, P. A schizophrenic patient with an arrhythmic circadian rest-activity cycle. Psychiatry Res. 1997, 73, 83–90. [Google Scholar] [CrossRef]
- Wirz-Justice, A.; Haug, H.J.; Cajochen, C. Disturbed Circadian Rest-Activity Cycles in Schizophrenia Patients: An Effect of Drugs? Schizophr. Bull. 2001, 27, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Choi, J.-W.; Kang, S.-G.; Hwang, S.H.; Kim, S.J.; Lee, Y.J. Comparison of the Effects of Quetiapine XR and Lithium Monotherapy on Actigraphy-Measured Circadian Parameters in Patients with Bipolar II Depression. J. Clin. Psychopharmacol. 2017, 37, 351–354. [Google Scholar] [CrossRef]
- Matsui, K.; Takaesu, Y.; Inoue, T.; Inada, K.; Nishimura, K. Effect of aripiprazole on non-24-hour sleep–wake rhythm disorder comorbid with major depressive disorder: A case report. Neuropsychiatr. Dis. Treat. 2017, 13, 1367–1371. [Google Scholar] [CrossRef]
- Suzuki, H.; Hibino, H.; Inoue, Y.; Mikami, K. Effect of aripiprazole monotherapy in a patient presenting with delayed sleep phase syndrome associated with depressive symptoms. Psychiatry Clin. Neurosci. 2018, 72, 375–376. [Google Scholar] [CrossRef] [PubMed]
- Wirz-Justice, A.; Werth, E.; Savaskan, E.; Knoblauch, V.; Gasio, P.F.; Müller-Spahn, F. Haloperidol Disrupts, Clozapine Reinstates the Circadian Rest-Activity Cycle in a Patient with Early-Onset Alzheimer Disease. Alzheimer Dis. Assoc. Disord. 2000, 14, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Viyoch, J.; Matsunaga, N.; Yoshida, M.; To, H.; Higuchi, S.; Ohdo, S. Effect of Haloperidol on mPer1 Gene Expression in Mouse Suprachiasmatic Nuclei. J. Biol. Chem. 2005, 280, 6309–6315. [Google Scholar] [CrossRef]
- Coogan, A.N.; Papachatzaki, M.M.; Clemens, C.; Baird, A.; Donev, R.M.; Joosten, J.; Zachariou, V.; Thome, J. Haloperidol alters circadian clock gene product expression in the mouse brain. World J. Biol. Psychiatry 2011, 12, 638–644. [Google Scholar] [CrossRef]
- Vadnie, C.A.; McClung, C.A. Circadian Rhythm Disturbances in Mood Disorders: Insights into the Role of the Suprachiasmatic Nucleus. Neural Plast. 2017, 2017, 1–28. [Google Scholar] [CrossRef]
- Chung, S.; Lee, E.J.; Cha, H.K.; Kim, J.; Kim, D.; Son, G.H.; Kim, K. Cooperative roles of the suprachiasmatic nucleus central clock and the adrenal clock in controlling circadian glucocorticoid rhythm. Sci. Rep. 2017, 7, srep46404. [Google Scholar] [CrossRef] [PubMed]
- Brivio, P.; Sbrini, G.; Tarantini, L.; Parravicini, C.; Gruca, P.; Lason, M.; Litwa, E.; Favero, C.; Riva, M.; Eberini, I.; et al. Stress Modifies the Expression of Glucocorticoid-Responsive Genes by Acting at Epigenetic Levels in the Rat Prefrontal Cortex: Modulatory Activity of Lurasidone. Int. J. Mol. Sci. 2021, 22, 6197. [Google Scholar] [CrossRef]
- Basta-Kaim, A.; Budziszewska, B.; Jaworska-Feil, L.; Leśkiewicz, M.; Tetich, M.; Kubera, M.; Scharpe, S.; Lasoń, W. Opposite effects of clozapine and sulpiride on the lipopolysaccharide-induced inhibition of the GR-mediated gene transcription in fibroblast cells. Pol. J. Pharmacol. 2003, 55, 1153–1158. [Google Scholar] [PubMed]
- Basta-Kaim, A.; Budziszewska, B.; Jaworska-Feil, L.; Tetich, M.; Leśkiewicz, M.; Kubera, M.; Lasoń, W. Chlorpromazine inhibits the glucocorticoid receptor-mediated gene transcription in a calcium-dependent manner. Neuropharmacology 2002, 43, 1035–1043. [Google Scholar] [CrossRef]
- Dwivedi, Y.; Rizavi, H.S.; Pandey, G.N. Differential effects of haloperidol and clozapine on [(3)H]cAMP binding, protein kinase A (PKA) activity, and mRNA and protein expression of selective regulatory and catalytic subunit isoforms of PKA in rat brain. J. Pharmacol. Exp. Ther. 2002, 301, 197–209. [Google Scholar] [CrossRef]
- Pozzi, L.; Håkansson, K.; Usiello, A.; Borgkvist, A.; Lindskog, M.; Greengard, P.; Fisone, G. Opposite Regulation by Typical and Atypical Anti-Psychotics of ERK1/2, CREB and Elk-1 Phosphorylation in Mouse Dorsal Striatum. J. Neurochem. 2003, 86, 451–459. [Google Scholar] [CrossRef]
- Chan, M.Y.; Hung, F.; Mo-Yin, C. A study on the effects of chlorpromazine and desipramine on rat adrenal steroidogenesis and cholesterol esterase activity. Biochem. Pharmacol. 1983, 32, 1713–1715. [Google Scholar] [CrossRef] [PubMed]
- Rang, H.P.; Ritter, J.; Flower, R.J.; Henderson, G. Antidepressant drugs. In Rang & Dale’s Pharmacology; Churchill Livingstone: London, UK, 2016; pp. 586–588. [Google Scholar]
- Singer, I.; Rotenberg, D.; Puschett, J.B. Lithium-induced nephrogenic diabetes insipidus: In vivo and in vitro studies. J. Clin. Investig. 1972, 51, 1081–1091. [Google Scholar] [CrossRef][Green Version]
- Emerson, C.H.; Dysno, W.L.; Utiger, R.D. Serum Thyrotropin and Thyroxine Concentrations in Patients Recieving Lithium Carbonate. J. Clin. Endocrinol. Metab. 1973, 36, 338–346. [Google Scholar] [CrossRef]
- Valvassori, S.S.; Resende, W.R.; Dal-Pont, G.; Sangaletti-Pereira, H.; Gava, F.F.; Peterle, B.R.; Carvalho, A.F.; Varela, R.B.; Dal-Pizzol, F.; Quevedo, J. Lithium ameliorates sleep deprivation-induced mania-like behavior, hypothalamic-pituitary-adrenal (HPA) axis alterations, oxidative stress and elevations of cytokine concentrations in the brain and serum of mice. Bipolar Disord. 2017, 19, 246–258. [Google Scholar] [CrossRef] [PubMed]
- Cohrs, S.; Röher, C.; Jordan, W.; Meier, A.; Huether, G.; Wuttke, W.; Rüther, E.; Rodenbeck, A. The atypical antipsychotics olanzapine and quetiapine, but not haloperidol, reduce ACTH and cortisol secretion in healthy subjects. Psychopharmacology 2006, 185, 11–18. [Google Scholar] [CrossRef]
- Wetzel, H.; Wiesner, J.; Hiemke, C.; Benkert, O. Acute antagonism of dopamine D2-like receptors by amisulpride: Effects on hormone secretion in healthy volunteers. J. Psychiatr. Res. 1994, 28, 461–473. [Google Scholar] [CrossRef]
- Laakmann, G.; Wittmann, M.; Gugath, M.; Mueller, O.A.; Treusch, J.; Wahlster, U.; Stalla, G.K. Effects of psychotropic drugs (desimipramine, chlorimipramine, sulpiride and diazepam) on the human HPA axis. Psychopharmacology 1984, 84, 66–70. [Google Scholar] [CrossRef]
- Von Bahr, C.; Wiesel, F.-A.; Movin, G.; Eneroth, P.; Jansson, P.; Nilsson, L.; Ogenstad, S. Neuroendocrine responses to single oral doses of remoxipride and sulpiride in healthy female and male volunteers. Psychopharmacology 1991, 103, 443–448. [Google Scholar] [CrossRef]
- De Koning, P.; De Vries, M.H. A comparison of the neuro-endocrinological and temperature effects of DU 29894, flesinoxan, sulpiride and haloperidol in normal volunteers. Br. J. Clin. Pharmacol. 1995, 39, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Jezová-Repceková, D.; Klimes, I.; Jurcovicová, J.; Vigas, M. Effect of adrenergic receptor blockade on cortisol and GH response to insulin-induced hypoglycemia in man. Int. J. Clin. Pharm. Biopharm. 1979, 17, 64–67. [Google Scholar]
- Hennig, J.; Rzepka, U.; Mai, B.; Netter, P. Suppression of HPA-axis activity by haloperidol after experimentally induced heat stress. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 1995, 19, 603–614. [Google Scholar] [CrossRef]
- Hahn, M.K.; Wolever, T.M.; Arenovich, T.; Teo, C.; Giacca, A.; Powell, V.; Clarke, L.; Fletcher, P.; Cohn, T.; McIntyre, R.S.; et al. Acute Effects of Single-Dose Olanzapine on Metabolic, Endocrine, and Inflammatory Markers in Healthy Controls. J. Clin. Psychopharmacol. 2013, 33, 740–746. [Google Scholar] [CrossRef] [PubMed]
- de Borja Gonçalves Guerra, A.; Castel, S.; Benedito-Silva, A.A.; Calil, H.M. Neuroendocrine Effects of Quetiapine in Healthy Volunteers. Int. J. Neuropsychopharmacol. 2005, 8, 49–57. [Google Scholar] [CrossRef] [PubMed]
- von Bardeleben, U.; Benkert, O.; Hoisboer, F. Clinical and Neuroendocrine Effects of Zotepine—A New Neuroleptic Drug. Pharmacopsychiatry 1987, 20, 28–34. [Google Scholar] [CrossRef]
- Vidarsdottir, S.; Roelfsema, F.; Frolich, M.; Pijl, H. Olanzapine shifts the temporal relationship between the daily acrophase of serum prolactin and cortisol concentrations rhythm in healthy men. Psychoneuroendocrinology 2009, 34, 705–712. [Google Scholar] [CrossRef]
- Meier, A.; Neumann, A.-C.; Jordan, W.; Huether, G.; Rodenbeck, A.; Rüther, E.; Cohrs, S. Ziprasidone decreases cortisol excretion in healthy subjects. Br. J. Clin. Pharmacol. 2005, 60, 330–336. [Google Scholar] [CrossRef]
- Cohrs, S.; Pohlmann, K.; Guan, Z.; Jordan, W.; Meier, A.; Huether, G.; Rodenbeck, A. Quetiapine reduces nocturnal urinary cortisol excretion in healthy subjects. Psychopharmacology 2004, 174, 414–420. [Google Scholar] [CrossRef]
- Sarubin, N.; Nothdurfter, C.; Schmotz, C.; Wimmer, A.-M.; Trummer, J.; Lieb, M.; Uhr, M.; Baghai, T.C.; Wetter, T.C.; Bühner, M.; et al. Impact on cortisol and antidepressant efficacy of quetiapine and escitalopram in depression. Psychoneuroendocrinology 2014, 39, 141–151. [Google Scholar] [CrossRef]
- Cookson, J.; Silverstone, T.; Besser, G.; Williams, S. Plasma corticosteroids in mania: The effects of pimozide. Neuropharmacology 1980, 19, 1243–1244. [Google Scholar] [CrossRef]
- Cookson, J.C.; Silverstone, T.; William, S.; Besser, G.M. Plasma Cortisol Levels in Mania: Associated Clinical Ratings and Changes during Treatment with Haloperidol. Br. J. Psychiatry 1985, 146, 498–502. [Google Scholar] [CrossRef]
- Venkatasubramanian, G.; Chittiprol, S.; Neelakantachar, N.; Shetty, T.; Gangadhar, B. Effect of antipsychotic treatment on Insulin-like Growth Factor-1 and cortisol in schizophrenia: A longitudinal study. Schizophr. Res. 2010, 119, 131–137. [Google Scholar] [CrossRef]
- Woldesenbet, Y.M.; Alenko, A.; Bukata, I.T.; Gedefaw, L.; Fikru, C. The status of serum cortisol before and after treatment of schizophrenia and its correlation to disease severity and improvement: A longitudinal study. SAGE Open Med. 2021, 9, 20503121211056216. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Zhou, D.F.; Cao, L.Y.; Wu, G.Y.; Shen, Y.C. Cortisol and Cytokines in Chronic and Treatment-Resistant Patients with Schizophrenia: Association with Psychopathology and Response to Antipsychotics. Neuropsychopharmacology 2005, 30, 1532–1538. [Google Scholar] [CrossRef] [PubMed]
- Mann, K.; Rossbach, W.; Müller, M.J.; Müller-Siecheneder, F.; Pott, T.; Linde, I.; Dittmann, R.W.; Hiemke, C. Nocturnal hormone profiles in patients with schizophrenia treated with olanzapine. Psychoneuroendocrinology 2006, 31, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Morinobu, S.; Ichimura, M.; Asakawa, A.; Inui, A.; Hosoda, H.; Kangawa, K.; Yamawaki, S. Decreased levels of ghrelin, cortisol, and fasting blood sugar, but not n-octanoylated ghrelin, in Japanese schizophrenic inpatients treated with olanzapine. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2008, 32, 1527–1532. [Google Scholar] [CrossRef] [PubMed]
- Breier, A.; Buchanan, R.W.; Waltrip, R.W.; Listwak, S.; Holmes, C.; Goldstein, D.S. The Effect of Clozapine on Plasma Norepinephrine: Relationship to Clinical Efficacy. Neuropsychopharmacology 1994, 10, 1–7. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Pivac, N.; Mihaljevic-Peles, A.; Mustapic, M.; Relja, M.; Ljubicic, D.; Marcinko, D.; Muck-Seler, D. The effects of olanzapine and fluphenazine on plasma cortisol, prolactin and muscle rigidity in schizophrenic patients: A double blind study. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2007, 31, 399–402. [Google Scholar] [CrossRef]
- Smigan, L.; Perris, C. Cortisol Changes in Long-Term Lithium Therapy. Neuropsychobiology 1984, 11, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.H.; DeLeon-Jones, F.A.; Schickler, R.; Nasr, S.; Mayer, M.; Hurks, C. Symptomatic reactive hypoglycemia during glucose tolerance test in lithium-treated patients. Metabolism 1986, 35, 634–639. [Google Scholar] [CrossRef]
- Bschor, T.; Adli, M.; Baethge, C.; Eichmann, U.; Ising, M.; Uhr, M.; Modell, S.; Künzel, H.; Müller-Oerlinghausen, B.; Bauer, M. Lithium Augmentation Increases the ACTH and Cortisol Response in the Combined DEX/CRH Test in Unipolar Major Depression. Neuropsychopharmacology 2002, 27, 470–478. [Google Scholar] [CrossRef][Green Version]
- Bschor, T.; Ritter, D.; Winkelmann, P.; Erbe, S.; Uhr, M.; Ising, M.; Lewitzka, U. Lithium Monotherapy Increases ACTH and Cortisol Response in the Dex/CRH Test in Unipolar Depressed Subjects. A Study with 30 Treatment-Naive Patients. PLoS ONE 2011, 6, e27613. [Google Scholar] [CrossRef]
- Houtepen, L.; Boks, M.; Kahn, R.; Joëls, M.; Vinkers, C. Antipsychotic use is associated with a blunted cortisol stress response: A study in euthymic bipolar disorder patients and their unaffected siblings. Eur. Neuropsychopharmacol. 2015, 25, 77–84. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rossini Gajšak, L.; Vogrinc, Ž.; Čelić Ružić, M.; Bošnjak Kuharić, D.; Bošković, M.; Koričančić Makar, A.; Makarić, P.; Er-makora, V.; Kekin, I.; Bajić, Ž.; et al. Salivary cortisol response to psychosocial stress in patients with first-episode psychosis. Croat. Med J. 2021, 62, 80–89. [Google Scholar] [CrossRef]
- Vaessen, T.; Kasanova, Z.; Hernaus, D.; Lataster, J.; Collip, D.; van Nierop, M.; Myin-Germeys, I. Overall cortisol, diurnal slope, and stress reactivity in psychosis: An experience sampling approach. Psychoneuroendocrinology 2018, 96, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Costa, G.; Frisina, N.; Pasquale, R. Increased Aldosterone Secretion Induced by Sulpiride. Clin. Endocrinol. 1980, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Izakova, L.; Hlavacova, N.; Jezova, D. Steroid stress hormone changes throughout the menstrual cycle: A rise in evening aldosterone concentration in early luteal phase precedes the symptoms of premenstrual syndrome. J. Neuroendocr. 2021, 33, e13043. [Google Scholar] [CrossRef]
- Robertson, D.; Michelakis, A.M. The Effect of Chlorpromazine on Plasma Renin Activity and Aldosterone in Man. J. Clin. Endocrinol. Metab. 1975, 41, 1166–1168. [Google Scholar] [CrossRef]
- Liberini, P.; Nisoli, E.; Missale, C.; Turrina, C.; Frisoni, G.B.; Caruso, R.; Spano, P.F. Increase of Aldosterone Secretion Following Acute Haloperidol Administration: Possible Clinical Implications. Int. Clin. Psychopharmacol. 1996, 11, 67–70. [Google Scholar] [CrossRef]
- Warner, M.D.; Gillespie, H.; Pavlou, S.N.; Nader, S.; Peabody, C.A. The effect of haloperidol on aldosterone secretion. Psychoneuroendocrinology 1992, 17, 517–521. [Google Scholar] [CrossRef]
- Shirley, D.G.; Singer, D.R.J.; Sagnella, G.A.; Buckley, M.G.; Miller, M.A.; Markandu, N.D.; MacGregor, G.A. Effect of a single test dose of lithium carbonate on sodium and potassium excretion in man. Clin. Sci. 1991, 81, 59–63. [Google Scholar] [CrossRef]
- Ustohal, L.; Hlavacova, N.; Mayerova, M.; Ceskova, E.; Jezova, D. Aldosterone and aldosterone/cortisol ratio is higher in serum of long-term compared to first episode schizophrenia patients: A pilot study. J. Psychiatr. Res. 2018, 104, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Kudoh, A.; Kudo, M.; Ishihara, H.; Matsuki, A. Increased plasma vasopressin and atrial natriuretic peptide in chronic schizophrenic patients during abdominal surgery. Neuropsychobiology 1998, 37, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, E.; Amdisen, A.; Darling, S. Plasma Aldosterone and Magnesium in Serum and Urine during Lithium Treatment. Int. Pharm. 1977, 12, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Stewart, P.M.; Atherden, S.M.; Stewart, S.E.; Whalley, L.; Edwards, C.R.; Padfield, P.L. Lithium Carbonate—A Competitive Aldosterone Antagonist? Br. J. Psychiatry 1988, 153, 205–207. [Google Scholar] [CrossRef]
- Hansen, H.E.; Pedersen, E.B.; Amdisen, A. Renal Function and Plasma Aldosterone during Acute Lithium Intoxication. Acta Med. Scand. 1979, 205, 593–597. [Google Scholar] [CrossRef]
- Borges, S.; Gayer-Anderson, C.; Mondelli, V. A systematic review of the activity of the hypothalamic–pituitary–adrenal axis in first episode psychosis. Psychoneuroendocrinology 2013, 38, 603–611. [Google Scholar] [CrossRef]

| Study | Drug (s) | Duration of Treatment | Participants | Biological Fluid | Cortisol Secretion | Refs. |
|---|---|---|---|---|---|---|
| Handley et al. (2016) | haloperidol (3 mg) | single dose | healthy (n = 17) | saliva | ↓ | [33] |
| aripiprazole (10 mg) | single dose | healthy (n = 17) | saliva | – | ||
| Cohrs et al. (2006) | haloperidol (3 mg) | single dose | healthy (n = 11) | plasma | – | [67] |
| quetiapine (50 mg) | single dose | healthy (n = 11) | plasma | ↓ | ||
| olanzapine (5 mg) | single dose | healthy (n = 11) | plasma | ↓ | ||
| Wetzel et al. (1994) | amisulpride (20 mg) | single dose | healthy (n = 8) | plasma | – | [68] |
| amisulpride (100 mg) | single dose | healthy (n = 8) | plasma | – | ||
| Laakmann et al. (1984) | sulpiride (100 mg) | single dose | healthy (n = 6) | plasma | – | [69] |
| von Bahr et al. (1991) | sulpiride (200 mg) | single dose | healthy (n = 12) | serum | – | [70] |
| remoxipride (100 mg) | single dose | healthy (n = 12) | serum | – | ||
| de Konnig and de Vries (1995) | sulpiride (400 mg) | single dose | healthy (n = 19) | plasma | – | [71] |
| haloperidol (3 mg) | single dose | healthy (n = 19) | plasma | – | ||
| Henning et al. (1995) | haloperidol (3 mg) | single dose | healthy (n = 40) | saliva | ↓ stress-induced | [73] |
| Hahn et al. (2013) | olanzapine (10 mg) | single dose | healthy (n = 12) | serum | ↓ | [74] |
| de Borja Goncalves Guerra et al. (2005) | quetiapine (150 mg) | single dose | healthy (n = 15) | plasma | ↓ | [75] |
| von Bardeleben et al. (1987) | zotepine (25 mg) | single dose | healthy (n = 6) | plasma | – | [76] |
| Jezova-Repcekova et al. (1979) | pimozide (4 mg) | two doses | healthy (n = 8) | plasma | – stress-induced | [72] |
| Vidarsdottir et al. (2009) | olanzapine (10 mg) | 8 days | healthy (n = 12) | plasma | ↓ | [77] |
| Meier et al. (2005) | ziprasidone (40 mg) | 5 days | healthy (n = 11) | urine | ↓ stress-induced | [78] |
| Cohrs et al. (2004) | quetiapine (25 mg) | 4 days | healthy (n = 13) | urine | ↓ stress-induced | [79] |
| quetiapine (100 mg) | 4 days | healthy (n = 13) | urine | ↓ stress-induced |
| Study | Drug (s) | Duration of Treatment | Participants | Biological Fluid | Cortisol Secretion | Refs. |
|---|---|---|---|---|---|---|
| Sarubin et al. (2014) | quetiapine (300 mg) | 1 week | MDD patients (n = 23) | blood | ↓ | [80] |
| Cookson et al. (1980) | pimozide (32 mg) | 2 weeks | BD patients (n = 6) | plasma | ↓ | [81] |
| Cookson et al. (1985) | haloperidol (2.5–40 mg) | 3 days | BD patients (n = 31) | plasma | ↓ | [82] |
| Venkatasubramanian et al. (2010) | risperidone (4–10 mg) | 12 weeks | SZ patients (n = 17) | serum | ↓ | [83] |
| olanzapine (7.5–15 mg) | 12 weeks | SZ patients (n = 14) | serum | ↓ | ||
| Woldesenbet et al. (2021) | risperidone, haloperidol, chlorpromazine, olanzapine, modecate | 8 weeks | SZ patients (n = 34) | serum | ↓ | [84] |
| Zhang et al. (2005) | risperidone (6 mg) | 12 weeks | SZ patients (n = 41) | serum | ↓ | [85] |
| haloperidol (20 mg) | 12 weeks | SZ patients (n = 37) | serum | ↓ | ||
| Mann et al. (2006) | olanzapine (15–20 mg) | 4 weeks | SZ patients (n = 10) | serum | ↓ | [86] |
| Tanaka et al. (2008) | olanzapine (20 mg) | 16 weeks | SZ patients (n = 28) | plasma | ↓ | [87] |
| Breier et al. (1994) | clozapine (400 mg) | 10 weeks | SZ patients (n = 11) | plasma | – | [88] |
| haloperidol (20 mg) | 10 weeks | SZ patients (n = 15) | plasma | – | ||
| Jakovljevic et al. (2007) | olanzapine (5–20 mg) | 22 weeks | SZ patients (n = 12) | plasma | – | [89] |
| Smigan and Perris (1984) | lithium (unspecified) | 1 year | various patients (n = 53) | serum | ↓ | [90] |
| Shah et al. (1986) | lithium (unspecified) | 6 months | BD patients (n = 9) | serum | ↑ stress-induced | [91] |
| Bschor et al. (2002) | lithium (900 mg) | 4 weeks | MDD patients (n = 24) | plasma | ↑ stress-induced | [92] |
| Bschor et al. (2011) | lithium (900 mg) | 4 weeks | MDD patients (n = 30) | plasma | ↑ stress-induced | [93] |
| Houtepen et al. (2015) | various antipsychotics | unspecified | BD patients (n = 49) | saliva | ↓ stress-induced | [94] |
| Rossini Gajsak et al. (2021) | various antipsychotics | unspecified | SZ patients (n = 53) | saliva | ↓ stress-induced | [95] |
| Vaessen et al. (2018) | various antipsychotics | 1 year | psychotic patients (n = 49) | saliva | – stress-induced | [96] |
| Study | Drug (s) | Duration of Treatment | Participants | Biological Fluid | Aldosterone Secretion | Refs. |
|---|---|---|---|---|---|---|
| Costa et al. (1980) | sulpiride (100 mg) | single dose | healthy (n = 7) | plasma | ↑ | [97] |
| Robertson and Michelakis (1975) | chlorpromazine (10 mg) | single dose | SZ patients (n = 12) | plasma | ↑ | [99] |
| Liberini et al. (1996) | haloperidol (2 mg) | single dose | SZ patients (n = 7) | plasma | ↑ | [100] |
| Warner et al. (1992) | haloperidol (0.02 mg/kg BW) | single dose | SZ patients (n = 12) | serum | – | [101] |
| Shirley et al. (1991) | lithium (300 mg) | single dose | healthy (n = 15) | plasma | – | [102] |
| lithium (600 mg) | single dose | healthy (n = 15) | plasma | – | ||
| Ustohal et al. (2018) | various antipsychotics | unspecified | SZ patients (n = 36) | serum | ↑ | [103] |
| Kudoh et al. (1998) | chlorpromazine, perphenazine | long-term | SZ patients (n = 18) | plasma | ↓ stress-induced | [104] |
| Pedersen et al. (1977) | lithium (600 mg) | 3 months | BD patients (n = 8) | plasma | – | [105] |
| lithium (unspecified) | 3 months–20 year | BD patients (n = 27) | plasma | – | ||
| Stewart et al. (1988) | lithium (unspecified) | 0.5–18 years | BD patients (n = 16) | plasma | ↑ | [106] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romanova, Z.; Hlavacova, N.; Jezova, D. Psychotropic Drug Effects on Steroid Stress Hormone Release and Possible Mechanisms Involved. Int. J. Mol. Sci. 2022, 23, 908. https://doi.org/10.3390/ijms23020908
Romanova Z, Hlavacova N, Jezova D. Psychotropic Drug Effects on Steroid Stress Hormone Release and Possible Mechanisms Involved. International Journal of Molecular Sciences. 2022; 23(2):908. https://doi.org/10.3390/ijms23020908
Chicago/Turabian StyleRomanova, Zuzana, Natasa Hlavacova, and Daniela Jezova. 2022. "Psychotropic Drug Effects on Steroid Stress Hormone Release and Possible Mechanisms Involved" International Journal of Molecular Sciences 23, no. 2: 908. https://doi.org/10.3390/ijms23020908
APA StyleRomanova, Z., Hlavacova, N., & Jezova, D. (2022). Psychotropic Drug Effects on Steroid Stress Hormone Release and Possible Mechanisms Involved. International Journal of Molecular Sciences, 23(2), 908. https://doi.org/10.3390/ijms23020908







