Genetic Deletion of Mmp9 Does Not Reduce Airway Inflammation and Structural Lung Damage in Mice with Cystic Fibrosis-like Lung Disease
Abstract
1. Introduction
2. Results
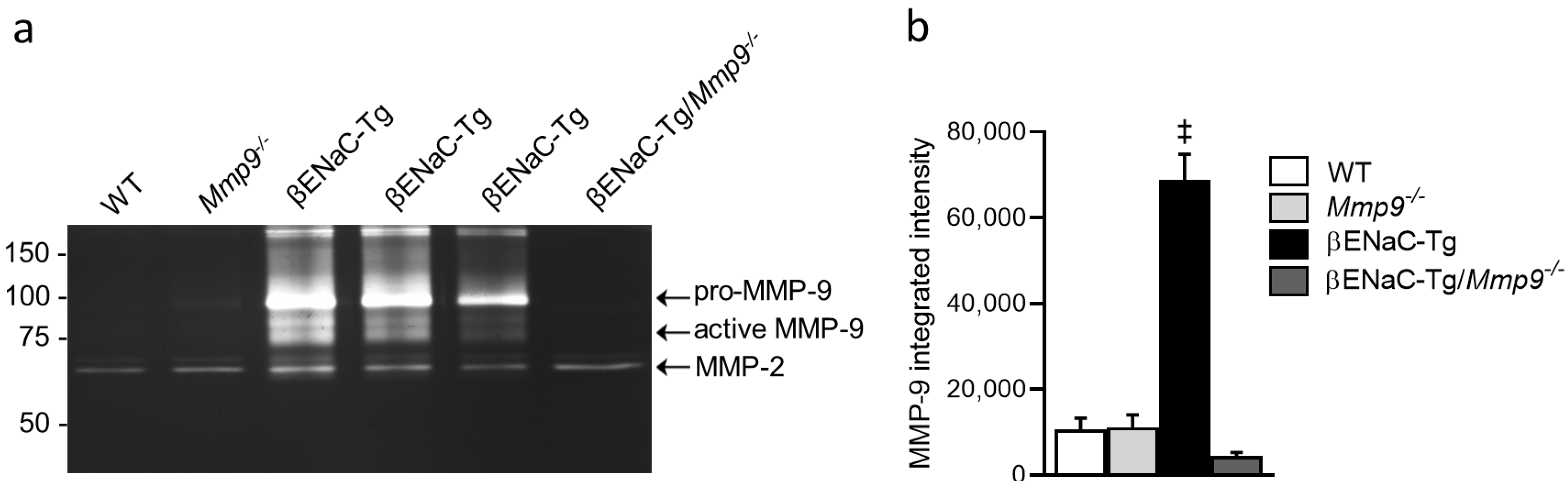
2.1. MMP-9 Protein Levels ArFe Elevated in BAL Fluid of βENaC-Tg Mice
2.2. Lack of MMP-9 Does Not Reduce Mortality in βENaC-Tg Mice
2.3. Genetic Deletion of Mmp9 Does Not Reduce Airway Inflammation in βENaC-Tg Mice
2.4. Genetic Deletion of Mmp9 Has No Effect on Goblet Cell Metaplasia and Increased Mucin Expression, but Partially Reduces Mucus Obstruction in βENaC-Tg Mice
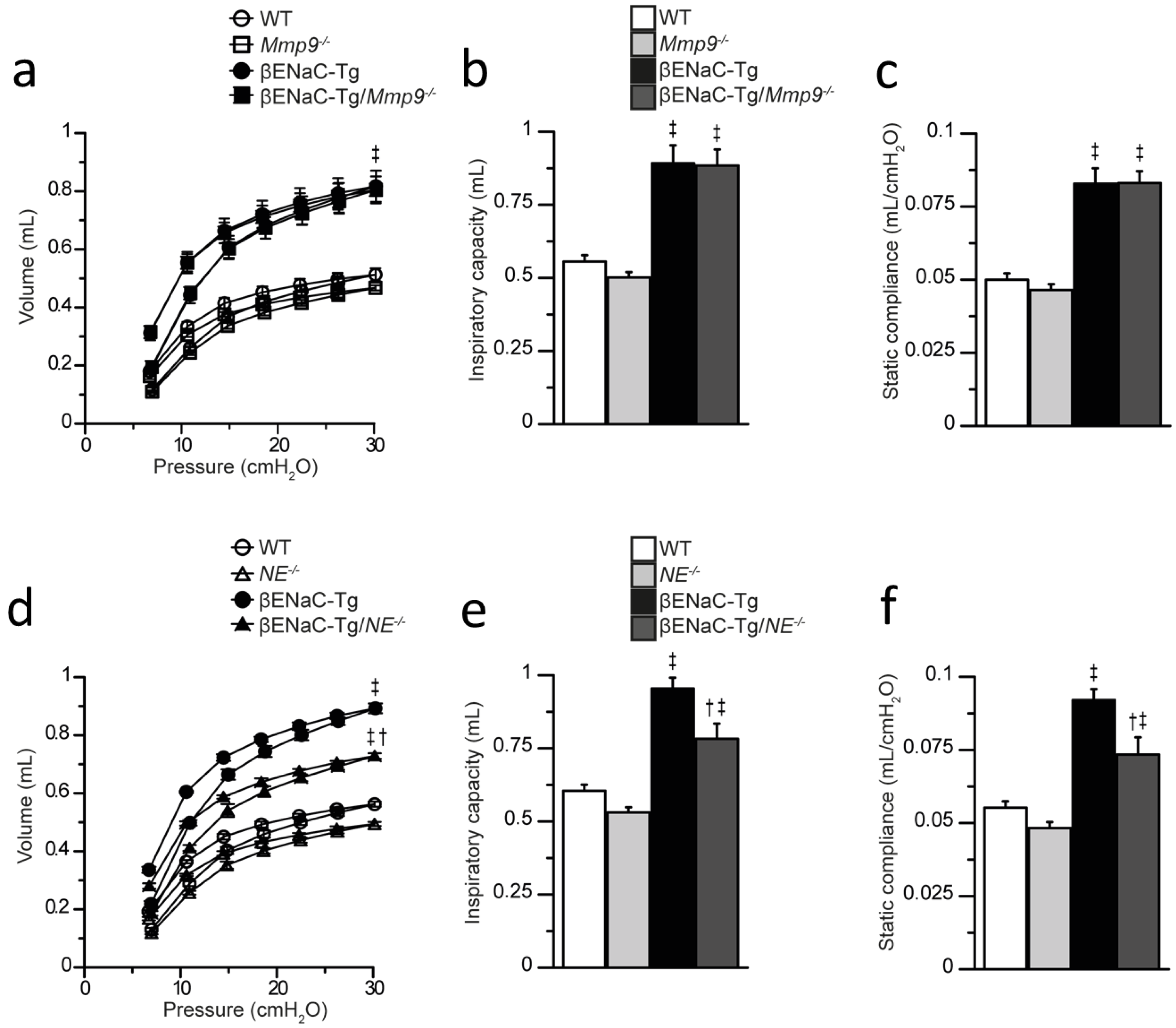
2.5. Genetic Deletion of Mmp9 Does Not Reduce Emphysema-like Structural Lung Damage in βENaC-Tg Mice
2.6. Genetic Deletion of NE, but Not Mmp9 Improves Lung Function Impairment in βENaC-Tg Mice
3. Discussion
4. Materials and Methods
4.1. Experimental Animals
4.2. Genotyping
4.3. Bronchoalveolar Lavage (BAL) and Differential Cell Count
4.4. Gelatin Zymography
4.5. Cytokine Measurements
4.6. Lung Histology
4.7. Real-Time Reverse Transcriptase Quantitative Polymerase Chain Reaction (RT-qPCR)
4.8. Lung Function Testing
4.9. Statistics
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Elborn, J.S. Cystic Fibrosis. Lancet 2016, 388, 2519–2531. [Google Scholar] [CrossRef]
- Mall, M.A.; Hartl, D. CFTR: Cystic Fibrosis and Beyond. Eur. Respir. J. 2014, 44, 1042–1054. [Google Scholar] [CrossRef] [PubMed]
- McKelvey, M.C.; Weldon, S.; McAuley, D.F.; Mall, M.A.; Taggart, C.C. Targeting Proteases in Cystic Fibrosis Lung Disease. Paradigms, Progress, and Potential. Am. J. Respir. Crit. Care Med. 2020, 201, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Taggart, C.; Mall, M.A.; Lalmanach, G.; Cataldo, D.; Ludwig, A.; Janciauskiene, S.; Heath, N.; Meiners, S.; Overall, C.M.; Schultz, C.; et al. Protean Proteases: At the Cutting Edge of Lung Diseases. Eur. Respir. J. 2017, 49, 1501200. [Google Scholar] [CrossRef] [PubMed]
- McKelvey, M.C.; Brown, R.; Ryan, S.; Mall, M.A.; Weldon, S.; Taggart, C.C. Proteases, Mucus, and Mucosal Immunity in Chronic Lung Disease. Int. J. Mol. Sci. 2021, 22, 5018. [Google Scholar] [CrossRef]
- Margaroli, C.; Garratt, L.W.; Horati, H.; Dittrich, A.S.; Rosenow, T.; Montgomery, S.T.; Frey, D.L.; Brown, M.R.; Schultz, C.; Guglani, L.; et al. Elastase Exocytosis by Airway Neutrophils Associates with Early Lung Damage in Cystic Fibrosis Children. Am. J. Respir. Crit. Care Med. 2018, 199, 873–881. [Google Scholar] [CrossRef]
- Dittrich, A.S.; Kühbandner, I.; Gehrig, S.; Rickert-Zacharias, V.; Twigg, M.; Wege, S.; Taggart, C.C.; Herth, F.; Schultz, C.; Mall, M.A. Elastase Activity on Sputum Neutrophils Correlates with Severity of Lung Disease in Cystic Fibrosis. Eur. Respir. J. 2018, 51, 1701910. [Google Scholar] [CrossRef]
- Sly, P.D.; Wainwright, C.E. Diagnosis and Early Life Risk Factors for Bronchiectasis in Cystic Fibrosis: A Review. Expert Rev. Respir. Med. 2016, 10, 1003–1010. [Google Scholar] [CrossRef]
- Gehrig, S.; Duerr, J.; Weitnauer, M.; Wagner, C.J.; Graeber, S.Y.; Schatterny, J.; Hirtz, S.; Belaaouaj, A.; Dalpke, A.H.; Schultz, C.; et al. Lack of Neutrophil Elastase Reduces Inflammation, Mucus Hypersecretion, and Emphysema, but Not Mucus Obstruction, in Mice with Cystic Fibrosis-like Lung Disease. Am. J. Respir. Crit. Care Med. 2014, 189, 1082–1092. [Google Scholar] [CrossRef]
- Mall, M.A.; Button, B.; Johannesson, B.; Zhou, Z.; Livraghi, A.; Caldwell, R.A.; Schubert, S.C.; Schultz, C.; O’Neal, W.K.; Pradervand, S.; et al. Airway Surface Liquid Volume Regulation Determines Different Airway Phenotypes in Liddle Compared with BetaENaC-Overexpressing Mice. J. Biol. Chem. 2010, 285, 26945–26955. [Google Scholar] [CrossRef]
- Giacalone, V.D.; Margaroli, C.; Mall, M.A.; Tirouvanziam, R. Neutrophil Adaptations upon Recruitment to the Lung: New Concepts and Implications for Homeostasis and Disease. Int. J. Mol. Sci. 2020, 21, 851. [Google Scholar] [CrossRef] [PubMed]
- Balázs, A.; Mall, M.A. Mucus Obstruction and Inflammation in Early Cystic Fibrosis Lung Disease: Emerging Role of the IL-1 Signaling Pathway. Pediatr. Pulmonol. 2019, 54 (Suppl. 3), S5–S12. [Google Scholar] [CrossRef] [PubMed]
- Gaggar, A.; Hector, A.; Bratcher, P.E.; Mall, M.A.; Griese, M.; Hartl, D. The Role of Matrix Metalloproteases in Cystic Fibrosis Lung Disease. Eur. Respir. J. 2011, 38, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, J.J.; Senior, R.M. Matrix Metalloproteinase-9 in Lung Remodeling. Am. J. Respir. Cell Mol. Biol. 2003, 28, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Pandey, K.C.; De, S.; Mishra, P.K. Role of Proteases in Chronic Obstructive Pulmonary Disease. Front. Pharmacol. 2017, 8, 512. [Google Scholar] [CrossRef]
- Wells, J.M.; Gaggar, A.; Blalock, J.E. MMP Generated Matrikines. Matrix Biol. 2015, 44–46, 122–129. [Google Scholar] [CrossRef]
- Stamenkovic, I. Extracellular Matrix Remodelling: The Role of Matrix Metalloproteinases. J. Pathol. 2003, 200, 448–464. [Google Scholar] [CrossRef]
- Vandooren, J.; Van den Steen, P.E.; Opdenakker, G. Biochemistry and Molecular Biology of Gelatinase B or Matrix Metalloproteinase-9 (MMP-9): The next Decade. Crit. Rev. Biochem. Mol. Biol. 2013, 48, 222–272. [Google Scholar] [CrossRef]
- Jackson, P.L.; Xu, X.; Wilson, L.; Weathington, N.M.; Clancy, J.P.; Blalock, J.E.; Gaggar, A. Human Neutrophil Elastase-Mediated Cleavage Sites of MMP-9 and TIMP-1: Implications to Cystic Fibrosis Proteolytic Dysfunction. Mol. Med. 2010, 16, 159–166. [Google Scholar] [CrossRef]
- Liu, Z.; Zhou, X.; Shapiro, S.D.; Shipley, J.M.; Twining, S.S.; Diaz, L.A.; Senior, R.M.; Werb, Z. The Serpin A1-Proteinase Inhibitor Is a Critical Substrate for Gelatinase B/MMP-9 In Vivo. Cell 2000, 102, 647–655. [Google Scholar] [CrossRef]
- Sagel, S.D.; Kapsner, R.K.; Osberg, I. Induced Sputum Matrix Metalloproteinase-9 Correlates with Lung Function and Airway Inflammation in Children with Cystic Fibrosis. Pediatr. Pulmonol. 2005, 39, 224–232. [Google Scholar] [CrossRef]
- Delacourt, C.; Le Bourgeois, M.; D’Ortho, M.P.; Doit, C.; Scheinmann, P.; Navarro, J.; Harf, A.; Hartmann, D.J.; Lafuma, C. Imbalance between 95 kDa Type IV Collagenase and Tissue Inhibitor of Metalloproteinases in Sputum of Patients with Cystic Fibrosis. Am. J. Respir. Crit. Care Med. 1995, 152, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Ratjen, F.; Hartog, C.-M.; Paul, K.; Wermelt, J.; Braun, J. Matrix Metalloproteases in BAL Fluid of Patients with Cystic Fibrosis and Their Modulation by Treatment with Dornase Alpha. Thorax 2002, 57, 930–934. [Google Scholar] [CrossRef] [PubMed]
- Veraar, C.; Kliman, J.; Benazzo, A.; Oberndorfer, F.; Laggner, M.; Hacker, P.; Raunegger, T.; Janik, S.; Jaksch, P.; Klepetko, W.; et al. Potential Novel Biomarkers for Chronic Lung Allograft Dysfunction and Azithromycin Responsive Allograft Dysfunction. Sci. Rep. 2021, 11, 6799. [Google Scholar] [CrossRef]
- Garratt, L.W.; Sutanto, E.N.; Ling, K.-M.; Looi, K.; Iosifidis, T.; Martinovich, K.M.; Shaw, N.C.; Kicic-Starcevich, E.; Knight, D.A.; Ranganathan, S.; et al. Matrix Metalloproteinase Activation by Free Neutrophil Elastase Contributes to Bronchiectasis Progression in Early Cystic Fibrosis. Eur. Respir. J. 2015, 46, 384–394. [Google Scholar] [CrossRef] [PubMed]
- Zhou-Suckow, Z.; Duerr, J.; Hagner, M.; Agrawal, R.; Mall, M.A. Airway Mucus, Inflammation and Remodeling: Emerging Links in the Pathogenesis of Chronic Lung Diseases. Cell Tissue Res. 2017, 367, 537–550. [Google Scholar] [CrossRef]
- Zhou, Z.; Duerr, J.; Johannesson, B.; Schubert, S.C.; Treis, D.; Harm, M.; Graeber, S.Y.; Dalpke, A.; Schultz, C.; Mall, M.A. The ENaC-Overexpressing Mouse as a Model of Cystic Fibrosis Lung Disease. J. Cyst. Fibros. 2011, 10 (Suppl. 2), S172–S182. [Google Scholar] [CrossRef]
- Jia, J.; Conlon, T.M.; Ballester Lopez, C.; Seimetz, M.; Bednorz, M.; Zhou-Suckow, Z.; Weissmann, N.; Eickelberg, O.; Mall, M.A.; Yildirim, A.Ö. Cigarette Smoke Causes Acute Airway Disease and Exacerbates Chronic Obstructive Lung Disease in Neonatal Mice. Am. J. Physiol. Lung Cell Mol. Physiol. 2016, 311, L602–L610. [Google Scholar] [CrossRef]
- Mall, M.; Grubb, B.R.; Harkema, J.R.; O’Neal, W.K.; Boucher, R.C. Increased Airway Epithelial Na+ Absorption Produces Cystic Fibrosis-like Lung Disease in Mice. Nat. Med. 2004, 10, 487–493. [Google Scholar] [CrossRef]
- Mall, M.A.; Harkema, J.R.; Trojanek, J.B.; Treis, D.; Livraghi, A.; Schubert, S.; Zhou, Z.; Kreda, S.M.; Tilley, S.L.; Hudson, E.J.; et al. Development of Chronic Bronchitis and Emphysema in β-Epithelial Na+ Channel–Overexpressing Mice. Am. J. Respir. Crit. Care Med. 2008, 177, 730–742. [Google Scholar] [CrossRef]
- Fritzsching, B.; Zhou-Suckow, Z.; Trojanek, J.B.; Schubert, S.C.; Schatterny, J.; Hirtz, S.; Agrawal, R.; Muley, T.; Kahn, N.; Sticht, C.; et al. Hypoxic Epithelial Necrosis Triggers Neutrophilic Inflammation via IL-1 Receptor Signaling in Cystic Fibrosis Lung Disease. Am. J. Respir. Crit. Care Med. 2015, 191, 902–913. [Google Scholar] [CrossRef]
- Johannesson, B.; Hirtz, S.; Schatterny, J.; Schultz, C.; Mall, M.A. CFTR Regulates Early Pathogenesis of Chronic Obstructive Lung Disease in ΒENaC-Overexpressing Mice. PLoS ONE 2012, 7, e44059. [Google Scholar] [CrossRef] [PubMed]
- Livraghi, A.; Grubb, B.R.; Hudson, E.J.; Wilkinson, K.J.; Sheehan, J.K.; Mall, M.A.; O’Neal, W.K.; Boucher, R.C.; Randell, S.H. Airway and Lung Pathology Due to Mucosal Surface Dehydration in β-Epithelial Na+ Channel-Overexpressing Mice: Role of TNFα and IL-4Rα Signaling, Influence of Neonatal Development, and Limited Efficacy of Glucocorticoid Treatment. J. Immunol. 2009, 182, 4357–4367. [Google Scholar] [CrossRef] [PubMed]
- Trojanek, J.B.; Cobos-Correa, A.; Diemer, S.; Kormann, M.; Schubert, S.C.; Zhou-Suckow, Z.; Agrawal, R.; Duerr, J.; Wagner, C.J.; Schatterny, J.; et al. Airway Mucus Obstruction Triggers Macrophage Activation and MMP12-Dependent Emphysema. Am. J. Respir. Cell Mol. Biol. 2014, 51, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Hagner, M.; Albrecht, M.; Guerra, M.; Braubach, P.; Halle, O.; Zhou-Suckow, Z.; Butz, S.; Jonigk, D.; Hansen, G.; Schultz, C.; et al. IL-17A from Innate and Adaptive Lymphocytes Contributes to Inflammation and Damage in Cystic Fibrosis Lung Disease. Eur. Respir. J. 2021, 57, 1900716. [Google Scholar] [CrossRef]
- Hey, J.; Paulsen, M.; Toth, R.; Weichenhan, D.; Butz, S.; Schatterny, J.; Liebers, R.; Lutsik, P.; Plass, C.; Mall, M.A. Epigenetic Reprogramming of Airway Macrophages Promotes Polarization and Inflammation in Muco-Obstructive Lung Disease. Nat. Commun. 2021, 12, 6520. [Google Scholar] [CrossRef]
- Seys, L.J.M.; Verhamme, F.M.; Dupont, L.L.; Desauter, E.; Duerr, J.; Agircan, A.S.; Conickx, G.; Joos, G.F.; Brusselle, G.G.; Mall, M.A.; et al. Airway Surface Dehydration Aggravates Cigarette Smoke-Induced Hallmarks of COPD in Mice. PLoS ONE 2015, 10, e0129897. [Google Scholar] [CrossRef]
- Stahr, C.S.; Samarage, C.R.; Donnelley, M.; Farrow, N.; Morgan, K.S.; Zosky, G.; Boucher, R.C.; Siu, K.K.W.; Mall, M.A.; Parsons, D.W.; et al. Quantification of Heterogeneity in Lung Disease with Image-Based Pulmonary Function Testing. Sci. Rep. 2016, 6, 29438. [Google Scholar] [CrossRef]
- Zhu, L.; Duerr, J.; Zhou-Suckow, Z.; Wagner, W.; Weinheimer, O.; Salomon, J.; Leitz, D.; Konietzke, P.; Yu, H.; Ackermann, M.; et al. ΜCT to Quantify Muco-Obstructive Lung Disease and Effects of Neutrophil Elastase Knockout in Mice. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2022, 322, L401–L411. [Google Scholar] [CrossRef]
- Small, D.M.; Brown, R.R.; Doherty, D.F.; Abladey, A.; Zhou-Suckow, Z.; Delaney, R.J.; Kerrigan, L.; Dougan, C.M.; Borensztajn, K.S.; Holsinger, L.; et al. Targeting of Cathepsin S Reduces Cystic Fibrosis-like Lung Disease. Eur. Respir. J. 2019, 53, 1801523. [Google Scholar] [CrossRef]
- Brown, R.; Small, D.M.; Doherty, D.F.; Holsinger, L.; Booth, R.; Williams, R.; Ingram, R.J.; Elborn, J.S.; Mall, M.A.; Taggart, C.C.; et al. Therapeutic Inhibition of Cathepsin S Reduces Inflammation and Mucus Plugging in Adult ΒENaC-Tg Mice. Mediat. Inflamm. 2021, 2021, e6682657. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, S.Y.; Bak, S.M.; Suh, I.B.; Lee, S.Y.; Shin, C.; Shim, J.J.; In, K.H.; Kang, K.H.; Yoo, S.H. Effects of Matrix Metalloproteinase Inhibitor on LPS-Induced Goblet Cell Metaplasia. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2004, 287, L127–L133. [Google Scholar] [CrossRef] [PubMed]
- Harijith, A.; Choo-Wing, R.; Cataltepe, S.; Yasumatsu, R.; Aghai, Z.H.; Janér, J.; Andersson, S.; Homer, R.J.; Bhandari, V. A Role for Matrix Metalloproteinase 9 in IFNγ-Mediated Injury in Developing Lungs. Am. J. Respir. Cell Mol. Biol. 2011, 44, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Chen, H.; Xu, W.; Zhang, W.; Buckley, S.; Zheng, S.G.; Warburton, D.; Kolb, M.; Gauldie, J.; Shi, W. Molecular Mechanisms of MMP9 Overexpression and Its Role in Emphysema Pathogenesis of Smad3-Deficient Mice. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2012, 303, L89–L96. [Google Scholar] [CrossRef]
- Foronjy, R.; Nkyimbeng, T.; Wallace, A.; Thankachen, J.; Okada, Y.; Lemaitre, V.; D’Armiento, J. Transgenic Expression of Matrix Metalloproteinase-9 Causes Adult-Onset Emphysema in Mice Associated with the Loss of Alveolar Elastin. Am. J. Physiol. Lung Cell Mol. Physiol. 2008, 294, L1149–L1157. [Google Scholar] [CrossRef]
- Atkinson, J.J.; Lutey, B.A.; Suzuki, Y.; Toennies, H.M.; Kelley, D.G.; Kobayashi, D.K.; Ijem, W.G.; Deslee, G.; Moore, C.H.; Jacobs, M.E.; et al. The Role of Matrix Metalloproteinase-9 in Cigarette Smoke–induced Emphysema. Am. J. Respir. Crit. Care Med. 2011, 183, 876–884. [Google Scholar] [CrossRef]
- Brass, D.M.; Hollingsworth, J.W.; Cinque, M.; Li, Z.; Potts, E.; Toloza, E.; Foster, W.M.; Schwartz, D.A. Chronic LPS Inhalation Causes Emphysema-Like Changes in Mouse Lung That Are Associated with Apoptosis. Am. J. Respir. Cell Mol. Biol. 2008, 39, 584–590. [Google Scholar] [CrossRef]
- Gehrig, S.; Mall, M.A.; Schultz, C. Spatially Resolved Monitoring of Neutrophil Elastase Activity with Ratiometric Fluorescent Reporters. Angew. Chem. Int. Ed. Engl. 2012, 51, 6258–6261. [Google Scholar] [CrossRef]
- Vu, T.H.; Shipley, J.M.; Bergers, G.; Berger, J.E.; Helms, J.A.; Hanahan, D.; Shapiro, S.D.; Senior, R.M.; Werb, Z. MMP-9/Gelatinase B Is a Key Regulator of Growth Plate Angiogenesis and Apoptosis of Hypertrophic Chondrocytes. Cell 1998, 93, 411–422. [Google Scholar] [CrossRef]
- Belaaouaj, A.; McCarthy, R.; Baumann, M.; Gao, Z.; Ley, T.J.; Abraham, S.N.; Shapiro, S.D. Mice Lacking Neutrophil Elastase Reveal Impaired Host Defense against Gram Negative Bacterial Sepsis. Nat. Med. 1998, 4, 615–618. [Google Scholar] [CrossRef]
- Toth, M.; Sohail, A.; Fridman, R. Assessment of Gelatinases (MMP-2 and MMP-9) by Gelatin Zymography. In Metastasis Research Protocols; Dwek, M., Brooks, S.A., Schumacher, U., Eds.; Humana Press: Totowa, NJ, USA, 2012; pp. 121–135. ISBN 978-1-61779-854-2. [Google Scholar]
- Scherle, W. A Simple Method for Volumetry of Organs in Quantitative Stereology. Mikroskopie 1970, 26, 57–60. [Google Scholar] [PubMed]
- Saetta, M.; Shiner, R.J.; Angus, G.E.; Kim, W.D.; Wang, N.S.; King, M.; Ghezzo, H.; Cosio, M.G. Destructive Index: A Measurement of Lung Parenchymal Destruction in Smokers. Am. Rev. Respir. Dis. 1985, 131, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Stereological Methods. Vol. 1. Practical Methods for Biological Morphometry. By Ewald R. Weibel. J. Microsc. 1981, 121, 131–132. [CrossRef]
- Pfaffl, M.W. A New Mathematical Model for Relative Quantification in Real-Time RT–PCR. Nucleic Acids Res. 2001, 29, e45. [Google Scholar] [CrossRef] [PubMed]
- Wielpütz, M.O.; Eichinger, M.; Zhou, Z.; Leotta, K.; Hirtz, S.; Bartling, S.H.; Semmler, W.; Kauczor, H.-U.; Puderbach, M.; Mall, M.A. In Vivo Monitoring of Cystic Fibrosis-like Lung Disease in Mice by Volumetric Computed Tomography. Eur. Respir. J. 2011, 38, 1060–1070. [Google Scholar] [CrossRef]
- Salazar, E.; Knowles, J.H. An Analysis of Pressure-Volume Characteristics of the Lungs. J. Appl. Physiol. 1964, 19, 97–104. [Google Scholar] [CrossRef]




| Gene Name | Primer Name | Sequence (5′→3′) | Annealing Temperature |
|---|---|---|---|
| Scnn1b | forward | CTT CCA AGA GTT CAA CTA CCG | 56 °C |
| reverse | TCT ACC AGC TCA GCC AGA GTG | ||
| Mmp9 | WT forward | GTG GGA CCA TCA TAA CAT CAC A | 60 °C |
| WT reverse | CTC GCG GCA AGT CTT CAG AGT A | ||
| KO forward | CTG AAT GAA CTG CAG GAC GA | ||
| KO reverse | ATA CTT TCT CGG CAG GAG CA | ||
| NE | forward | GGA ACT TCG TCA TGT CAG CA | 60 °C |
| WT reverse | TGC ACA GAG AAG GTC TGT CG | ||
| KO reverse | TGG ATG TGG AAT GTG TGC GAG |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wagner, C.; Balázs, A.; Schatterny, J.; Zhou-Suckow, Z.; Duerr, J.; Schultz, C.; Mall, M.A. Genetic Deletion of Mmp9 Does Not Reduce Airway Inflammation and Structural Lung Damage in Mice with Cystic Fibrosis-like Lung Disease. Int. J. Mol. Sci. 2022, 23, 13405. https://doi.org/10.3390/ijms232113405
Wagner C, Balázs A, Schatterny J, Zhou-Suckow Z, Duerr J, Schultz C, Mall MA. Genetic Deletion of Mmp9 Does Not Reduce Airway Inflammation and Structural Lung Damage in Mice with Cystic Fibrosis-like Lung Disease. International Journal of Molecular Sciences. 2022; 23(21):13405. https://doi.org/10.3390/ijms232113405
Chicago/Turabian StyleWagner, Claudius, Anita Balázs, Jolanthe Schatterny, Zhe Zhou-Suckow, Julia Duerr, Carsten Schultz, and Marcus A. Mall. 2022. "Genetic Deletion of Mmp9 Does Not Reduce Airway Inflammation and Structural Lung Damage in Mice with Cystic Fibrosis-like Lung Disease" International Journal of Molecular Sciences 23, no. 21: 13405. https://doi.org/10.3390/ijms232113405
APA StyleWagner, C., Balázs, A., Schatterny, J., Zhou-Suckow, Z., Duerr, J., Schultz, C., & Mall, M. A. (2022). Genetic Deletion of Mmp9 Does Not Reduce Airway Inflammation and Structural Lung Damage in Mice with Cystic Fibrosis-like Lung Disease. International Journal of Molecular Sciences, 23(21), 13405. https://doi.org/10.3390/ijms232113405






