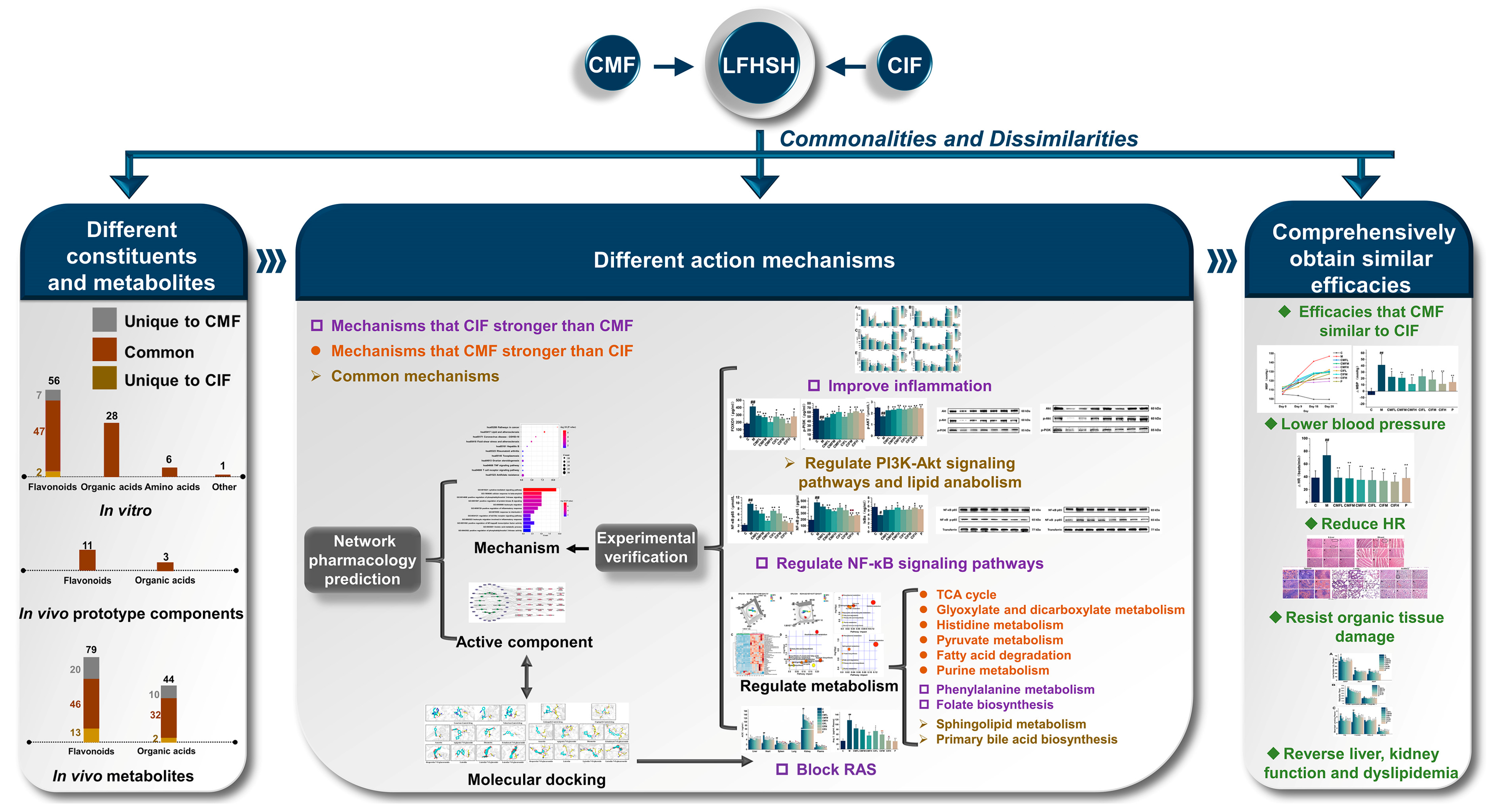
Comparison of the Chemical Components, Efficacy and Mechanisms of Action of Chrysanthemum morifolium Flower and Its Wild Relative Chrysanthemum indicum Flower against Liver-Fire Hyperactivity Syndrome of Hypertension via Integrative Analyses
Abstract
1. Introduction
2. Results
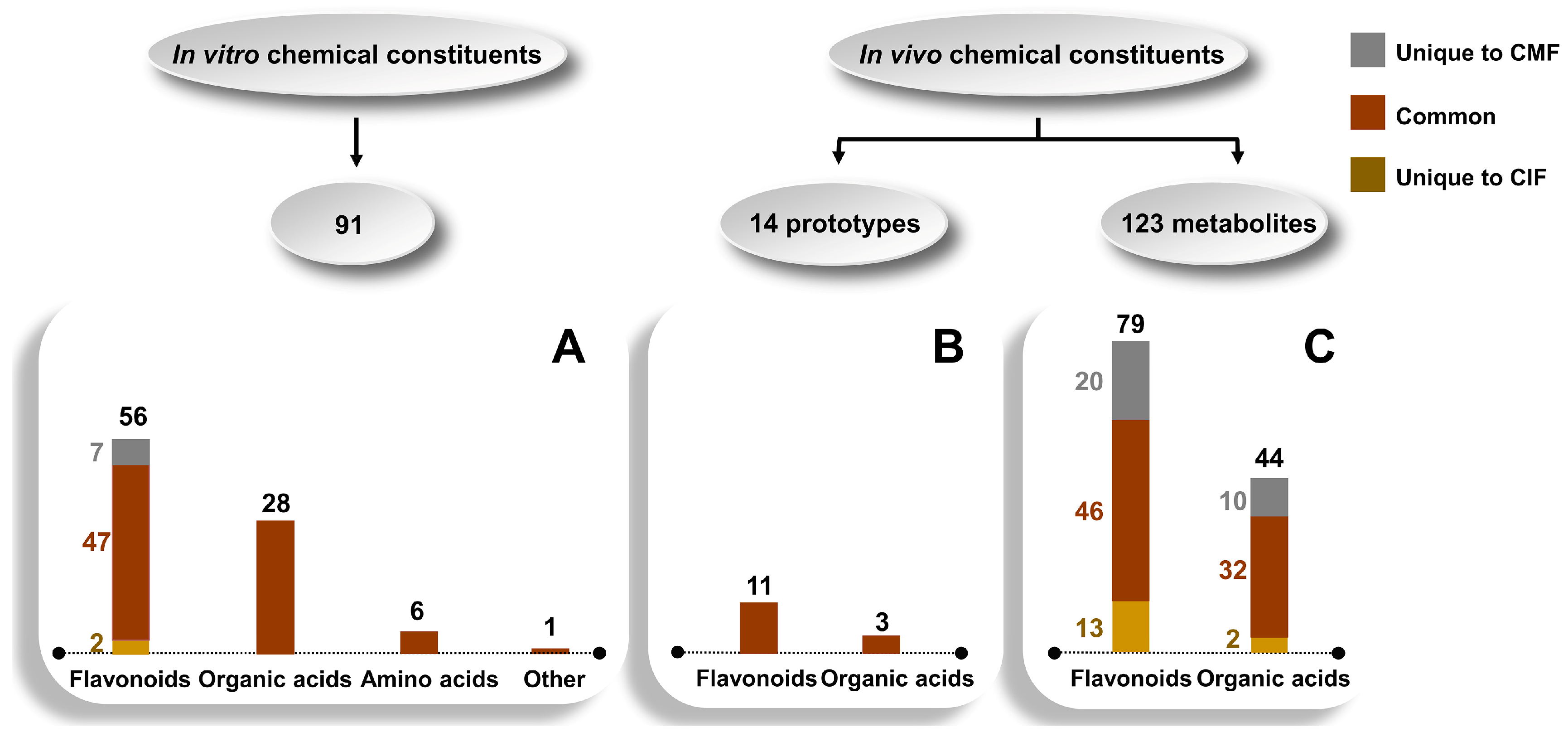
2.1. Comparison of the Chemical Constituents of CMF and CIF In Vitro and In Vivo
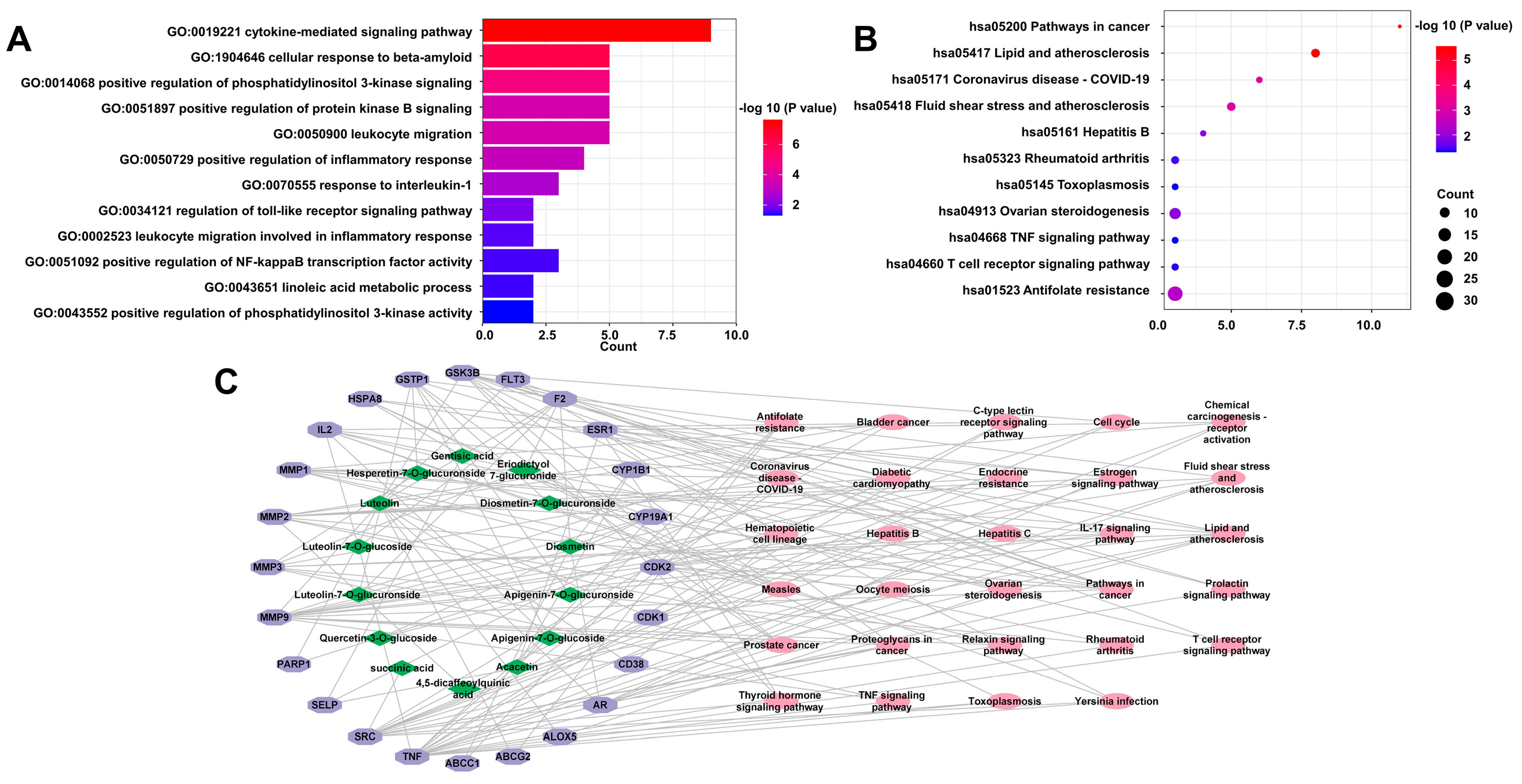
2.2. Network Pharmacology Predictive Analysis
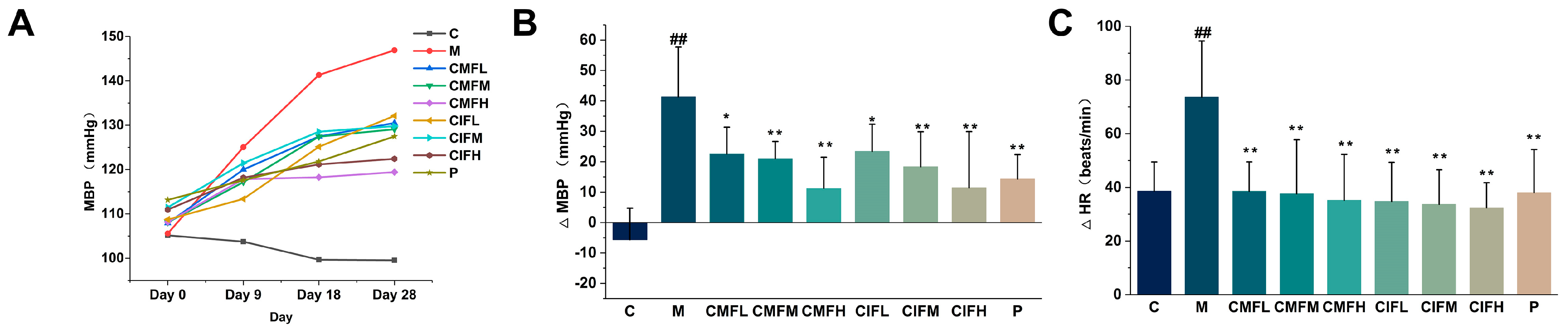
2.3. Blood Pressure Regulation Activity
2.4. HR Measurements
2.5. Assessment of Resistance to Functional and Organ Damage
2.5.1. Efficacy in Resistance to Liver and Kidney Function Damage
2.5.2. Efficacy in Reversing Dyslipidemia
2.5.3. Histopathological Examination of Liver, Heart, Spleen, Lung, and Kidney Tissue
2.6. Influence on Inflammatory Cytokines and Key Enzymes in LFHSH Rats
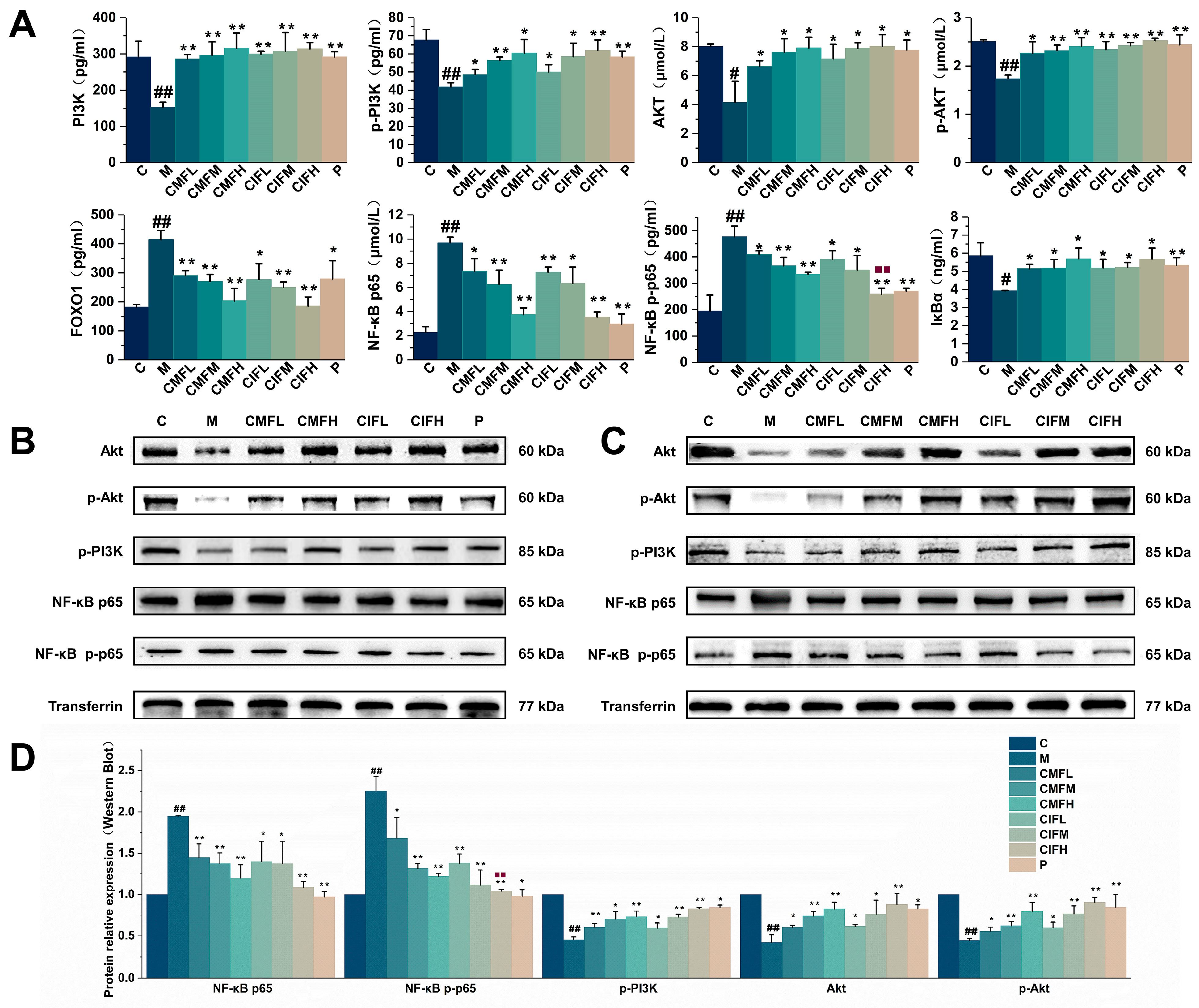
2.7. Assessment of Proteins Associated with NF-κB and PI3K-Akt Signaling Pathways
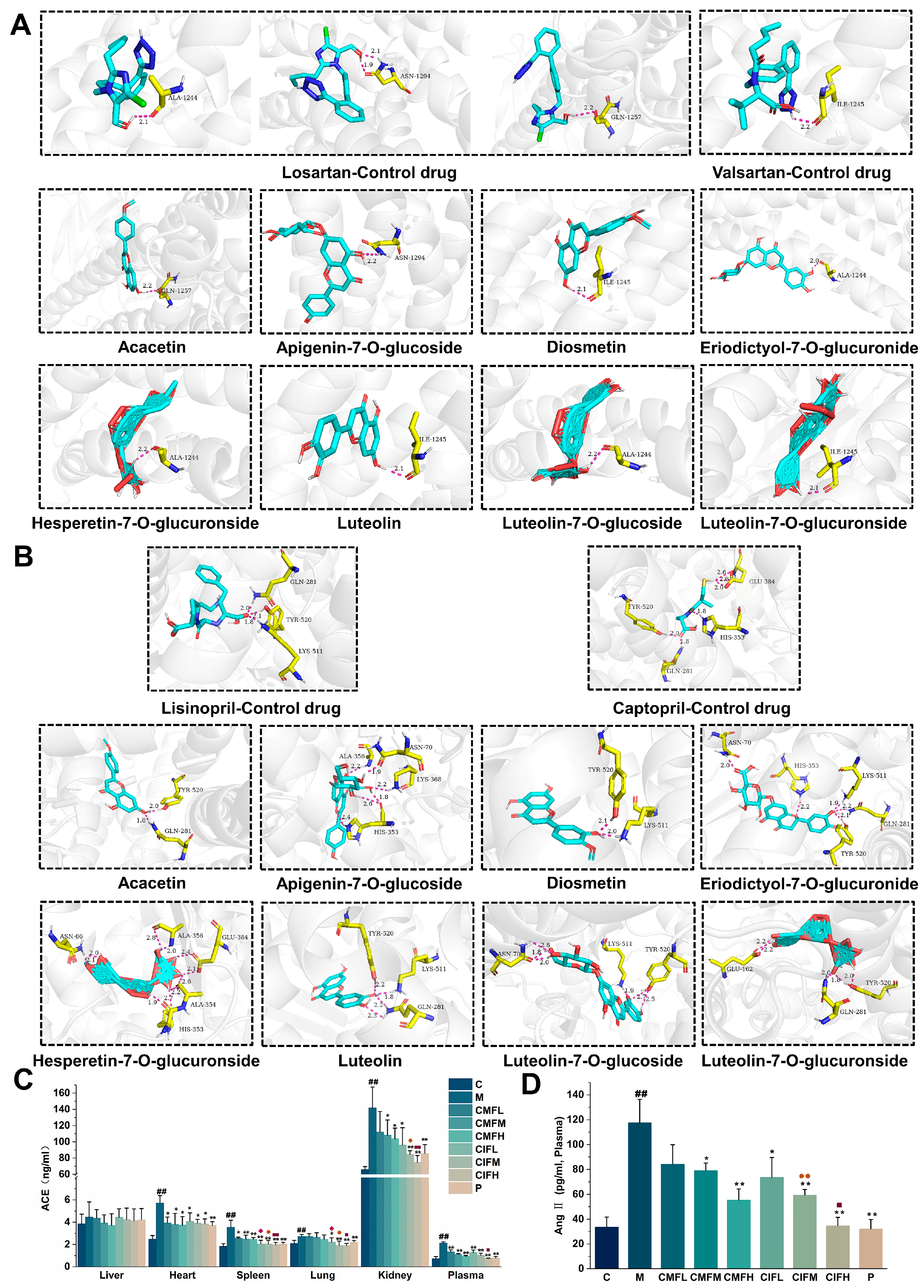
2.8. Regulation of RAS
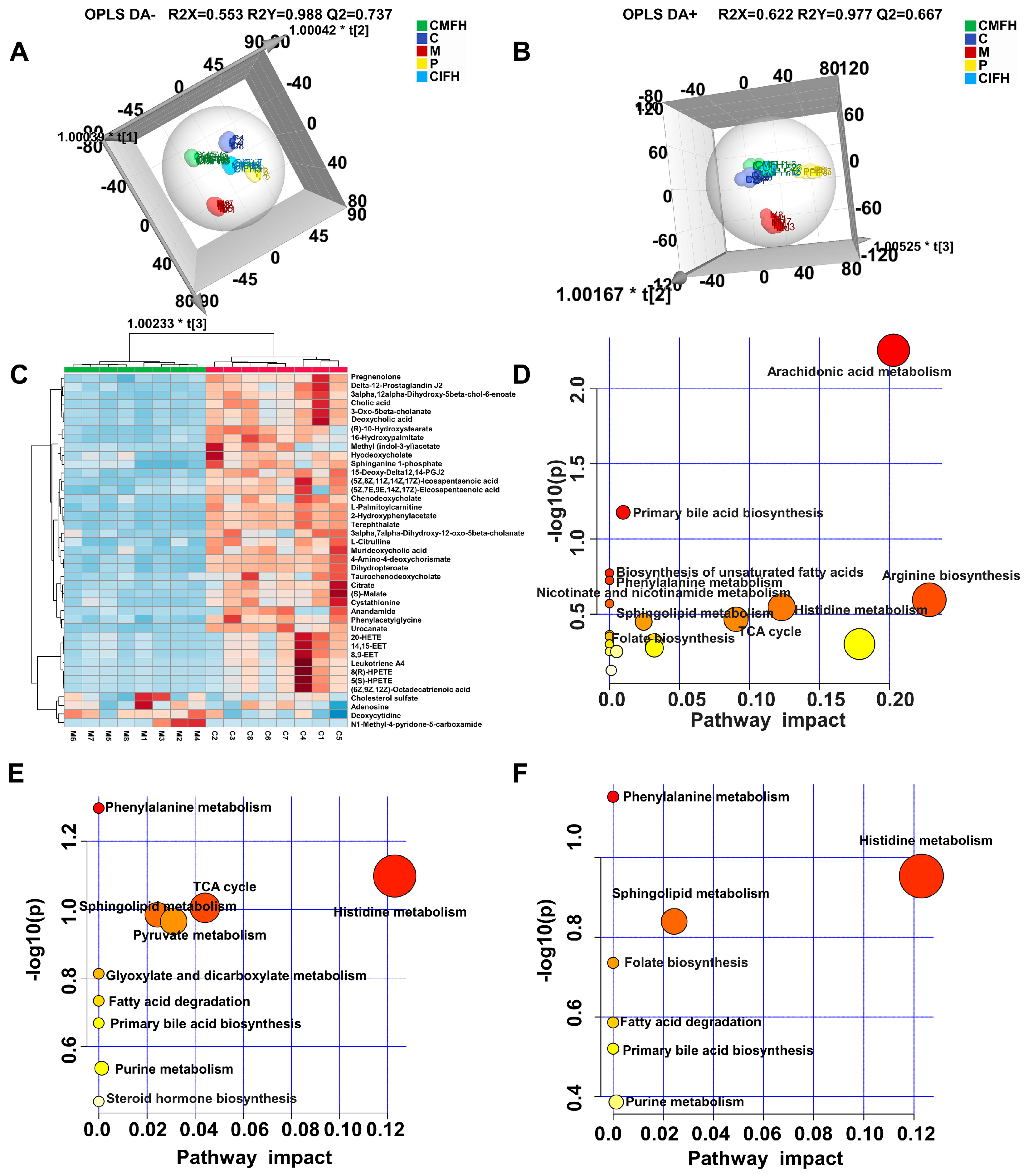
2.9. Non-Targeted Metabolomics Analysis
3. Discussion
4. Material and Methods
4.1. Materials
4.2. Animals and Groupings
4.3. Animal Experimental Design and Sample Collection
4.4. Component Identification Experiment
4.5. Network Pharmacology Analysis
4.6. Hematoxylin-Eosin (H&E) Staining
4.7. Blood Pressure and Heart Rate (HR) Measurements
4.8. ELISA
4.9. Western Blot Analysis of Serum Key Target Proteins
4.10. Molecular Docking
4.11. Plasma Non-Targeted Metabolomics Study
4.12. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Z.M.; Wang, B.X.; Ou, W.S.; Lv, Y.H.; Li, M.M.; Miao, Z.; Wang, S.X.; Fei, J.C.; Guo, T. Administration of losartan improves aortic arterial stiffness and reduces the occurrence of acute coronary syndrome in aged patients with essential hypertension. J. Cell. Biochem. 2019, 120, 5713–5721. [Google Scholar] [CrossRef] [PubMed]
- Sierra, C. Essential hypertension, cerebral white matter pathology and ischemic stroke. Curr. Med. Chem. 2014, 21, 2156–2164. [Google Scholar] [CrossRef] [PubMed]
- Francois, A.G.; Joel, M. Is Plasma Renin Activity Genetically Determined and How Much Does It Matter for Treating Hypertension? Circ. Genom. Precis. Med. 2018, 11, e002139. [Google Scholar]
- Zhang, G.X.; Liu, Y.Y.; Qiu, Y.M.; Zhang, J.N.; Sun, J.P.; Zhou, Z.; Wang, Z.C.; Zeng, P.S.; Tao, J.; He, J. Circulating senescent angiogenic T cells are linked with endothelial dysfunction and systemic inflammation in hypertension. J. Hypertens. 2021, 39, 970–978. [Google Scholar] [CrossRef]
- Chakraborty, S.; Mandal, J.; Yang, T.; Cheng, X.; Yeo, J.Y.; McCarthy, C.G.; Wenceslau, C.F.; Koch, L.G.; Hill, J.W.; Vijay-Kumar, M.; et al. Metabolites and Hypertension: Insights into Hypertension as a Metabolic Disorder: 2019 Harriet Dustan Award. Hypertension 2020, 75, 1386–1396. [Google Scholar] [CrossRef]
- Wang, X.J.; Gao, X.; Zhang, A.H.; Wu, F.F.; Yan, G.L.; Sun, H. High-throughput metabolomics for evaluating the efficacy and discovering the metabolic mechanism of Luozhen capsules from the excessive liver-fire syndrome of hypertension. RSC Adv. 2019, 9, 32141–32153. [Google Scholar] [CrossRef]
- Wu, W.T.; Yang, S.H.; Liu, P.; Yin, L.; Gong, Q.F.; Zhu, W.F. Systems Pharmacology-Based Strategy to Investigate Pharmacological Mechanisms of Radix Puerariae for Treatment of Hypertension. Front. Pharmacol. 2020, 11, 345–361. [Google Scholar] [CrossRef]
- Chen, S.; Liu, J.; Dong, G.Q.; Zhang, X.T.; Liu, Y.; Sun, W.; Liu, A. Flavonoids and caffeoylquinic acids in Chrysanthemum morifolium Ramat flowers: A potentially rich source of bioactive compounds. Food Chem. 2020, 344, 128733. [Google Scholar] [CrossRef]
- Shao, Y.H.; Sun, Y.D.; Li, D.; Chen, Y.P. Chrysanthemum indicum L.: A Comprehensive Review of its Botany, Phytochemistry and Pharmacology. Am. J. Chin. Med. 2020, 48, 871–897. [Google Scholar] [CrossRef]
- Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China; Chemical Industry Press: Beijing, China, 2020. [Google Scholar]
- Lin, L.Z.; Harnly, J.M. Identification of the phenolic components of chrysanthemum flower (Chrysanthemum morifolium Ramat). Food Chem. 2010, 120, 319–326. [Google Scholar] [CrossRef]
- Wang, J.; Xiong, X.J.; Liu, W. Traditional Chinese Medicine Syndromes for Essential Hypertension: A Literature Analysis of 13,272 Patients. Evid. Based Complement. Altern. Med. 2014, 2014, 418206. [Google Scholar] [CrossRef] [PubMed]
- Pei, L.X.; Shu, S.N.; Wang, X.Y.; Ji, B.Y. Effect of chrysanthemum extract on myocardial fibrosis in rats with renovascular hypertension. J. Tradit. Chin. Med. 2019, 39, 542–549. [Google Scholar]
- Shen, T.; Xing, G.X.; Zhu, J.F.; Cai, Y.; Zhang, S.X.; Xu, G.; Feng, Y.; Li, D.H.; Rao, J.Y.; Shi, R. Effects of 12-Week Supplementation of a Polyherbal Formulation in Old Adults with Prehypertension/Hypertension: A Randomized, Double-Blind, Placebo-Controlled Trial. Evid. Based Complement. Altern. Med. 2019, 2019, 7056872. [Google Scholar] [CrossRef]
- Lv, G.Y.; Zhang, Y.P.; Gao, J.L.; Yu, J.J.; Lei, J.; Zhang, Z.R.; Li, B.; Zhan, R.J.; Chen, S.H. Combined antihypertensive effect of luteolin and buddleoside enriched extracts in spontaneously hypertensive rats. J. Ethnopharmacol. 2013, 150, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.G.; Luo, G.; Dong, L.; Mazhar, M.; Wang, L.; He, W.L.; Liu, Y.; Wu, Q.B.; Zhou, H.; Yang, S.J. Network Pharmacology and In vitro Experimental Verification Reveal the Mechanism of the Hirudin in Suppressing Myocardial Hypertrophy. Front. Pharmacol. 2022, 13, 914518. [Google Scholar] [CrossRef] [PubMed]
- Pinzi, L.; Rastelli, G. Molecular Docking: Shifting Paradigms in Drug Discovery. Int. J. Mol. Sci. 2019, 20, 4331. [Google Scholar] [CrossRef]
- Zhang, C.; Mo, Y.Y.; Feng, S.S.; Meng, M.W.; Chen, S.Y.; Huang, H.M.; Ling, X.; Song, H.; Liang, Y.H.; Ou, S.F.; et al. Urinary metabonomics study of anti-depressive mechanisms of Millettia speciosa Champ on rats with chronic unpredictable mild stress-induced depression. J. Pharm. Biomed. Anal. 2021, 205, 114338. [Google Scholar] [CrossRef]
- Miguel-Carrasco, J.L.; Mate, A.; Monserrat, M.T.; Arias, J.L.; Aramburu, O.; Vázquez, C.M. The role of inflammatory markers in the cardioprotective effect of L-carnitine in L-NAME-induced hypertension. Am. J. Hypertens. 2008, 21, 1231–1237. [Google Scholar] [CrossRef]
- Javaud, N.; Fain, O. Awareness is still warranted for ARBs. J. Intern. Med. 2019, 285, 550–552. [Google Scholar] [CrossRef]
- Wang, Y.Y. The scientific nature of traditional Chinese medicine in the post-modern era. J. Tradit. Chin. Med. Sci. 2019, 6, 195–200. [Google Scholar] [CrossRef]
- Xu, J.; Yang, Y. Traditional Chinese medicine in the Chinese health care system. Health Policy 2009, 90, 133–139. [Google Scholar] [CrossRef]
- Leong, F.; Hua, X.; Wang, M.; Chen, T.K.; Song, Y.L.; Tu, P.F.; Chen, X.J. Quality standard of traditional Chinese medicines: Comparison between European Pharmacopoeia and Chinese Pharmacopoeia and recent advances. Chin. Med. 2020, 15, 76. [Google Scholar] [CrossRef]
- Xiang, Z.F.; Lan, Y.Y.L.; Shuang, C.S.; Hua, W.G.; Man, L.R. Revealing the potential pharmacological mechanism of traditional Chinese medicine by integrating metabolite profiling of a Q-marker and network pharmacology, prim-O-glucosylcimifugin as an example. New J. Chem. 2021, 45, 15571–15581. [Google Scholar]
- Cheng, W.M.; Li, J.; You, T.P.; Hu, C.M. Anti-inflammatory and immunomodulatory activities of the extracts from the inflorescence of Chrysanthemum indicum Linné. J. Ethnopharmacol. 2005, 101, 334–337. [Google Scholar] [CrossRef]
- Zheng, S.B.; Tang, J.; Zhu, J.K. Simultaneous Determination of Total Flavonoids and Organic Acids in Chrysanthemum by UV-Visible Spectrophotometry. Asian J. Chem. 2014, 26, 6409–6413. [Google Scholar] [CrossRef]
- Alam, M.A.; Subhan, N.; Rahman, M.M.; Uddin, S.J.; Reza, H.M.; Sarker, S.D. Effect of citrus flavonoids, naringin and naringenin, on metabolic syndrome and their mechanisms of action. Adv. Nutr. 2014, 5, 404–417. [Google Scholar] [CrossRef]
- Huang, X.Y.; Wu, P.L.; Huang, F.F.; Xu, M.; Chen, M.Y.; Huang, K.T.; Li, G.P.; Xu, M.H.; Yao, D.; Wang, L.X. Baicalin attenuates chronic hypoxia-induced pulmonary hypertension via adenosine A2A receptor-induced SDF-1/CXCR4/PI3K/AKT signaling. J. Biomed. Sci. 2017, 24, 52. [Google Scholar] [CrossRef]
- Lin, Y.; Shi, R.X.; Wang, X.; Shen, H.M. Luteolin, a flavonoid with potential for cancer prevention and therapy. Curr. Cancer Drug Targets 2008, 8, 634–646. [Google Scholar] [CrossRef]
- Atsuyoshi, N.; Daisuke, S.; Junpei, Y.; Kazuo, K.H.; Yasuaki, H.; Hirokazu, K. Antidiabetic-like Effects of Naringenin-7-O-glucoside from Edible Chrysanthemum “Kotobuki” and Naringenin by Activation of the PI3K/Akt Pathway and PPARγ. Chem. Biodivers. 2019, 16, e1800434. [Google Scholar]
- Nélida, N.; Cristina, T.; Alberto, G.; Guillermo, S.H. Phenolics from the Bolivian highlands food plant Ombrophytum subterraneum (Aspl.) B. Hansen (Balanophoraceae): Antioxidant and α-glucosidase inhibitory activity. Food Res. Int. 2020, 137, 109382. [Google Scholar]
- Ajebli, M.; Eddouks, M. Phytotherapy of Hypertension: An Updated Overview. Endocr. Metab. Immune Disord. Drug Targets 2020, 20, 812–839. [Google Scholar] [CrossRef]
- Kim, S.H.; Lim, K.R.; Seo, J.H.; Ryu, D.R.; Lee, B.K.; Cho, B.R.; Chun, K.J. Higherheart rate variability as a predictor of atrial fibrillation in patients with hypertension. Sci. Rep. 2022, 12, 3702. [Google Scholar] [CrossRef]
- Lorenzo, F.; Vicente, P.; Ana, P.; Manuel, P.; Vicente, G.; Vicente, M.; Vicente, B.; Vicente, B.G.; Josep, R. Twenty-four-hour ambulatory heart rate and organ damage in primary hypertension. Blood Press. 2010, 19, 104–109. [Google Scholar]
- Hong, X.Q.; Wongtongkam, N.; Ward, P.R.; Xiao, S.Y.; Wang, S.L.; Peng, Q.; Zuo, Q.; Zeng, D.; Wang, J.; Wang, C.X.; et al. An association of serum ALT with elevated blood pressure in senior adults: A case-control study. Clin. Exp. Hypertens. 2016, 38, 691–695. [Google Scholar] [CrossRef]
- Alberto, M.; Laura, S.; Gianluca, R.; Gioia, T.; Salvatore, L. The Effects of a New Generation of Nutraceutical Compounds on Lipid Profile and Glycaemia in Subjects with Pre-hypertension. High Blood Press. Cardiovasc. Prev. 2019, 26, 345–350. [Google Scholar]
- Irena, K.; Zaneta, P.; Natalia, D.; Magdalena, A.; Alicja, L. Canonical Wnt signaling in the kidney in different hypertension models. Hypertens. Res. 2021, 44, 1054–1066. [Google Scholar]
- Chen, Y.Q.; Fan, X.H.; Zhou, L.P.; Hu, F.Y.; Wang, P.L. Screening and evaluation of quality markers from Shuangshen Pingfei granules for idiopathic pulmonary fibrosis using network pharmacology and pharmacodynamic, phytochemical, and pharmacokinetic analyses. Phytomedicine 2022, 100, 154040. [Google Scholar]
- Yu, Z.Y.; Wu, Y.L.; Ma, Y.J.; Cheng, Y.S.; Song, G.H.; Zhang, F. Systematic analysis of the mechanism of aged citrus peel (Chenpi) in oral squamous cell carcinoma treatment via network pharmacology, molecular docking and experimental validation. J. Funct. Foods 2022, 91, 105012. [Google Scholar] [CrossRef]
- Wang, T.Y.; Lin, S.; Li, H.; Liu, R.; Liu, Z.H.; Xu, H.R.; Li, Q.; Bi, K.S. A stepwise integrated multi-system to screen quality markers of Chinese classic prescription Qingzao Jiufei decoction on the treatment of acute lung injury by combining ‘network pharmacology-metabolomics-PK/PD modeling’. Phytomedicine 2020, 78, 153313. [Google Scholar] [CrossRef]
- Gan, Z.Y.; Huang, D.; Jiang, J.Y.; Li, Y.; Li, H.Q.; Ke, Y. Captopril alleviates hypertension-induced renal damage, inflammation, and NF-κB activation. Braz. J. Med. Biol. Res. 2018, 51, e7338. [Google Scholar] [CrossRef]
- Khaliq, O.P.; Murugesan, S.; Moodley, J.; Mackraj, I. Differential expression of miRNAs are associated with the insulin signaling pathway in preeclampsia and gestational hypertension. Clin. Exp. Hypertens. 2018, 40, 744–751. [Google Scholar] [CrossRef]
- Bushra, S.; Hassan, M.M.; Shah, S.; Haseeb, A. Ziziphus Oxyphylla hydro-methanolic extract ameliorates hypertension in L-NAME induced hypertensive rats through NO/cGMP pathway and suppression of oxidative stress related inflammatory biomarkers. J. Ethnopharmacol. 2021, 285, 114825. [Google Scholar]
- Wang, L.; Lu, Y.Y.; Zhang, X.; Zhang, Y.; Jiang, D.S.; Dong, X.M.; Deng, S.; Yang, L.; Guan, Y.; Zhu, L.H.; et al. Mindin is a critical mediator of ischemic brain injury in an experimental stroke model. Exp. Neurol. 2013, 247, 506–516. [Google Scholar] [CrossRef]
- Yin, H.; Zhou, H.X.; Kang, Y.; Zhang, X.J.; Duan, X.X.; Alnabhan, R.; Liang, S.; Scott, D.A.; Lamont, R.J.; Shang, J.; et al. Syk negatively regulates TLR4-mediated IFNβ and IL-10 production and promotes inflammatory responses in dendritic cells. BBA-Gen Subj. 2016, 1860, 588–598. [Google Scholar] [CrossRef]
- Lee, H.; Jeong, J.H.; Ryu, J.H. Lignan from Alnus japonica Inhibits Adipocyte Differentiation via Cell Cycle and FOXO1 Regulation. Molecules 2020, 25, 3346. [Google Scholar] [CrossRef]
- Zhou, X.; Shang, D.W.; Zhang, T.L.; Li, L.; Zhou, Y.; Lu, W. Modeling of angiotensin II–angiotensin-(1-7) counterbalance in disease progression in spontaneously hypertensive rats treated with/without perindopril. Pharmacol. Res. 2012, 66, 177–184. [Google Scholar] [CrossRef]
- de Alcantara Santos, S.; Vinicius, G.; Santos, S.K.A.; Sanches, A.D.; Rodolfo, D.P.V.; Nádia, B.; Nestor, S.; Flávio, A.; Elena, C.D.; Sousa, C.T. Resistance exercise shifts the balance of renin-angiotensin system toward ACE2/Ang 1-7 axis and reduces inflammation in the kidney of diabetic rats. Life Sci. 2021, 287, 120058. [Google Scholar] [CrossRef]
- Yuwen, Y.; Han, X.J.; Weng, W.L.; Zhao, X.Y.; Liu, Y.Q.; Li, W.Q.; Liu, D.S.; Wang, Y.P.; Lu, A.P. Appraisal of the Quality and Contents of Clinical Practice Guidelines for Hypertension Management in Chinese Medicine: A Systematic Review. Chin. J. Integr. Med. 2018, 24, 545–550. [Google Scholar] [CrossRef]
- Huang, Y.P.; Wu, J.F.; Yin, J.Y.; Lin, Q.C. Study on Plasma Endothelin, Angiotensin II Thromboxame A2 in Different TCM Type of Grade 2 Hypertension and Effect of Tetrametuyl Pyrazine. Chin. J. Inf. Tradit. Chin. Med. 2002, 9, 18–25. (In Chinese) [Google Scholar]
- Miura, K.; Stamler, J.; Brown, I.J.; Ueshima, H.; Nakagawa, H.; Sakurai, M.; Chan, Q.; Appel, L.J.; Okayama, A.; Okuda, N.; et al. Relationship of dietary monounsaturated fatty acids to blood pressure: The International Study of Macro/Micronutrients and Blood Pressure. J. Hypertens. 2013, 31, 1144–1150. [Google Scholar] [CrossRef]
- Yang, M.X.; Yu, Z.; Deng, S.F.; Chen, X.M.; Chen, L.; Guo, Z.Y.; Zheng, H.; Chen, L.; Cai, D.J.; Wen, B.; et al. A Targeted Metabolomics MRM-MS Study on Identifying Potential Hypertension Biomarkers in Human Plasma and Evaluating Acupuncture Effects. Sci. Rep. 2016, 6, 25871. [Google Scholar] [CrossRef]
- Yang, P.F.; Zhao, X.R.; Zhou, L.X.; Jin, Y.X.; Zheng, X.W.; Ouyang, Y.N.; Chen, M.; Zeng, L.; Chen, S.; Chen, X.B.; et al. Protective effect of oral histidine on hypertension in Dahl salt-sensitive rats induced by high-salt diet. Life Sci. 2021, 270, 119134. [Google Scholar] [CrossRef]
- Heikal, L.; Starr, A.; Hussein, D.; Prieto-Lloret, J.; Aaronson, P.; Dailey, L.A.; Nandi, M. l-Phenylalanine Restores Vascular Function in Spontaneously Hypertensive Rats through Activation of the GCH1-GFRP Complex. JACC Basic Transl. Sci. 2018, 3, 366–377. [Google Scholar] [CrossRef]
- Zheng, X.W.; Zhao, X.R.; Jin, Y.X.; Zhou, L.X.; Yang, P.F.; Ahmad, H.; Tian, Z.M. High salt diet contributes to hypertension by weakening the medullary tricarboxylic acid cycle and antioxidant system in Dahl salt-sensitive rats. Biochimie 2021, 181, 154–161. [Google Scholar] [CrossRef]
- Surawee, C.; Grace, Y.Z.; Cheryl, T.M.J.; Christopher, W.; Gillian, D.; Yasmin, D.; Edward, D.N.; Mahesh, A.; Wei, Z.; Mark, C.J.; et al. Endothelial GTPCH (GTP Cyclohydrolase 1) and Tetrahydrobiopterin Regulate Gestational Blood Pressure, Uteroplacental Remodeling, and Fetal Growth. Hypertension 2021, 78, 1871–1884. [Google Scholar]
- Sui, J.; He, M.Q.; Wang, Y.; Zhao, X.R.; He, Y.Z.; Shi, B.Y. Sphingolipid metabolism in type 2 diabetes and associated cardiovascular complications. Exp. Ther. Med. 2019, 18, 3603–3614. [Google Scholar]
- Kurlak, L.O.; Williams, P.J.; Bulmer, J.N.; Pipkin, F.B.; Mistry, H.D. Placental expression of adenosine A 2A receptor and hypoxia inducible factor-1 alpha in early pregnancy, term and pre-eclamptic pregnancies: Interactions with placental renin-angiotensin system. Placenta 2015, 36, 611–613. [Google Scholar] [CrossRef]



| Indicator | Sample | Differences in Intervention Effect | ||
|---|---|---|---|---|
| CMF Superior to CIF (p < 0.05) | CIF Superior to CMF (p < 0.05) | CMF Similar Effective to CIF (p > 0.05) | ||
| Liver and kidney function, and blood lipid indexes | Plasma | None | None | AKP, ALT, AST, BUN, CRE, TG, T-CHO, LDL-C |
| Inflammatory mediators | Liver | None | IL-4 | COX-2 |
| Heart | None | TNF-α, COX-2 | IL-4, IL-10 | |
| Spleen | None | IL-10, COX-2 | None | |
| Lung | None | IL-4, IL-6, IL-10 | COX-2 | |
| Kidney | None | TNF-α, IL-1β, IL-4, IL-6, IL-10, COX-2 | None | |
| Plasma | None | None | IL-1β, IL-4, IL-6, IL-10, COX-2 | |
| Key proteins in NF-κB and PI3K-Akt signaling pathway | Serum | None | NF-κB p-p65 | PI3K, p-PI3K, Akt, p-Akt, FOXO1, NF-κB p65, IκBα |
| Effector molecules of RAS | Liver | None | None | None |
| Heart | None | None | ACE | |
| Spleen | None | ACE | None | |
| Lung | None | ACE | None | |
| Kidney | None | ACE | None | |
| Plasma | None | ACE, Ang II | None | |
| Metabolites | Plasma | (S)-Malate, 15-Deoxy-Delta12,14-PGJ2, Adenosine, L-palmitoylcarnitine, Urocanate | 2-Hydroxyphenylacetate, 4-Amino-4-deoxychorismate, Dihydropteroate, Terephthalate | Cholesterol sulfate, Methyl (indol-3-yl)acetate, Anandamide, Chenodeoxycholate, Hyodeoxycholate, Murideoxycholic acid, Sphinganine 1-phosphate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Li, Y.; Guo, W.; Yang, X.; Qu, J.; Gao, M.; Chen, S.; Dong, J.; Li, Q.; Wang, T. Comparison of the Chemical Components, Efficacy and Mechanisms of Action of Chrysanthemum morifolium Flower and Its Wild Relative Chrysanthemum indicum Flower against Liver-Fire Hyperactivity Syndrome of Hypertension via Integrative Analyses. Int. J. Mol. Sci. 2022, 23, 13767. https://doi.org/10.3390/ijms232213767
Wang Y, Li Y, Guo W, Yang X, Qu J, Gao M, Chen S, Dong J, Li Q, Wang T. Comparison of the Chemical Components, Efficacy and Mechanisms of Action of Chrysanthemum morifolium Flower and Its Wild Relative Chrysanthemum indicum Flower against Liver-Fire Hyperactivity Syndrome of Hypertension via Integrative Analyses. International Journal of Molecular Sciences. 2022; 23(22):13767. https://doi.org/10.3390/ijms232213767
Chicago/Turabian StyleWang, Yue, Yangyu Li, Wei Guo, Xiao Yang, Jiameng Qu, Mang Gao, Shuting Chen, Jiangru Dong, Qing Li, and Tiejie Wang. 2022. "Comparison of the Chemical Components, Efficacy and Mechanisms of Action of Chrysanthemum morifolium Flower and Its Wild Relative Chrysanthemum indicum Flower against Liver-Fire Hyperactivity Syndrome of Hypertension via Integrative Analyses" International Journal of Molecular Sciences 23, no. 22: 13767. https://doi.org/10.3390/ijms232213767
APA StyleWang, Y., Li, Y., Guo, W., Yang, X., Qu, J., Gao, M., Chen, S., Dong, J., Li, Q., & Wang, T. (2022). Comparison of the Chemical Components, Efficacy and Mechanisms of Action of Chrysanthemum morifolium Flower and Its Wild Relative Chrysanthemum indicum Flower against Liver-Fire Hyperactivity Syndrome of Hypertension via Integrative Analyses. International Journal of Molecular Sciences, 23(22), 13767. https://doi.org/10.3390/ijms232213767






