Design, Synthesis and Evaluation of Novel Molecular Hybrids between Antiglaucoma Drugs and H2S Donors
Abstract
1. Introduction
2. Chemistry
3. Results and Discussion
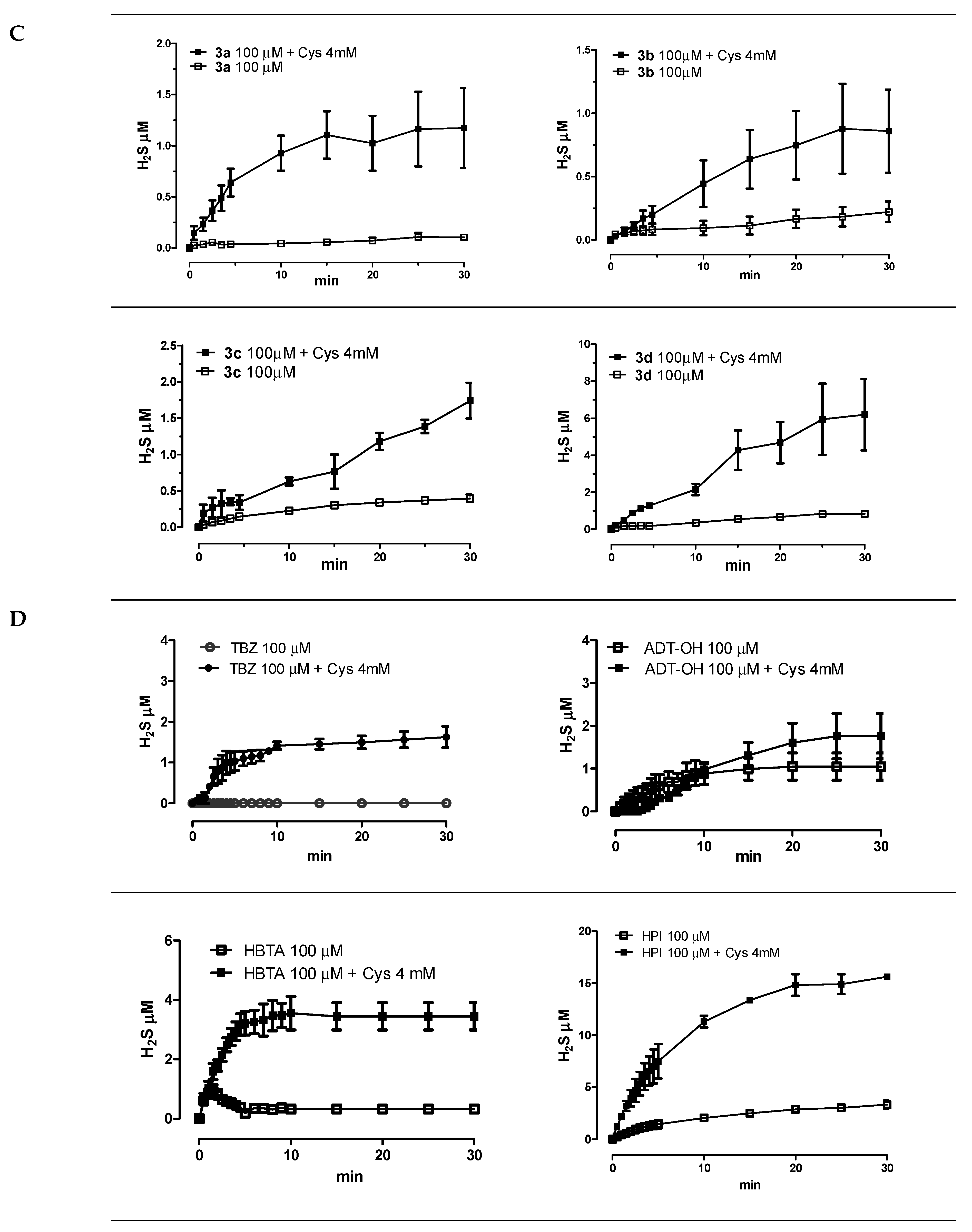
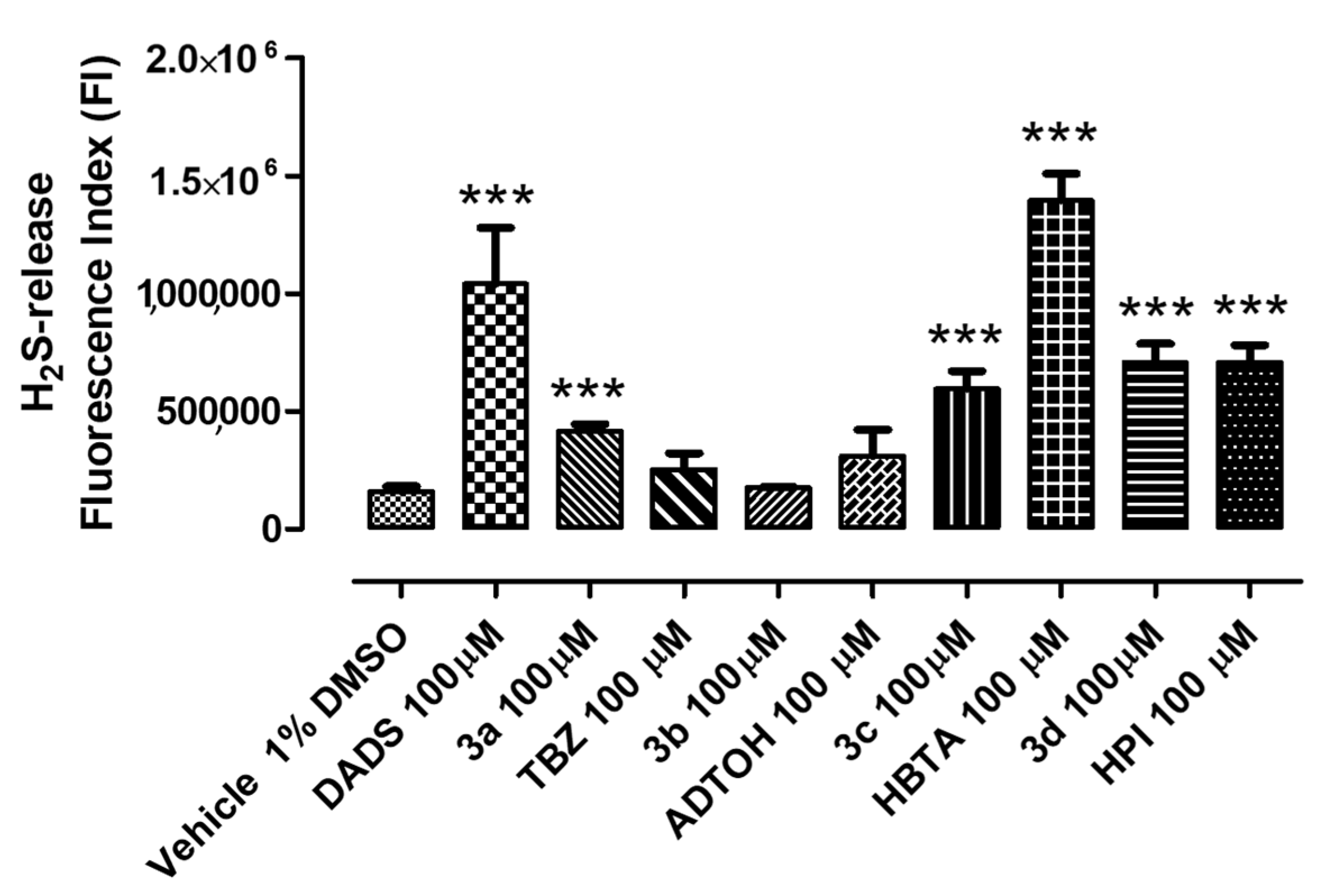
3.1. Amperometric Evaluation of H2S Release
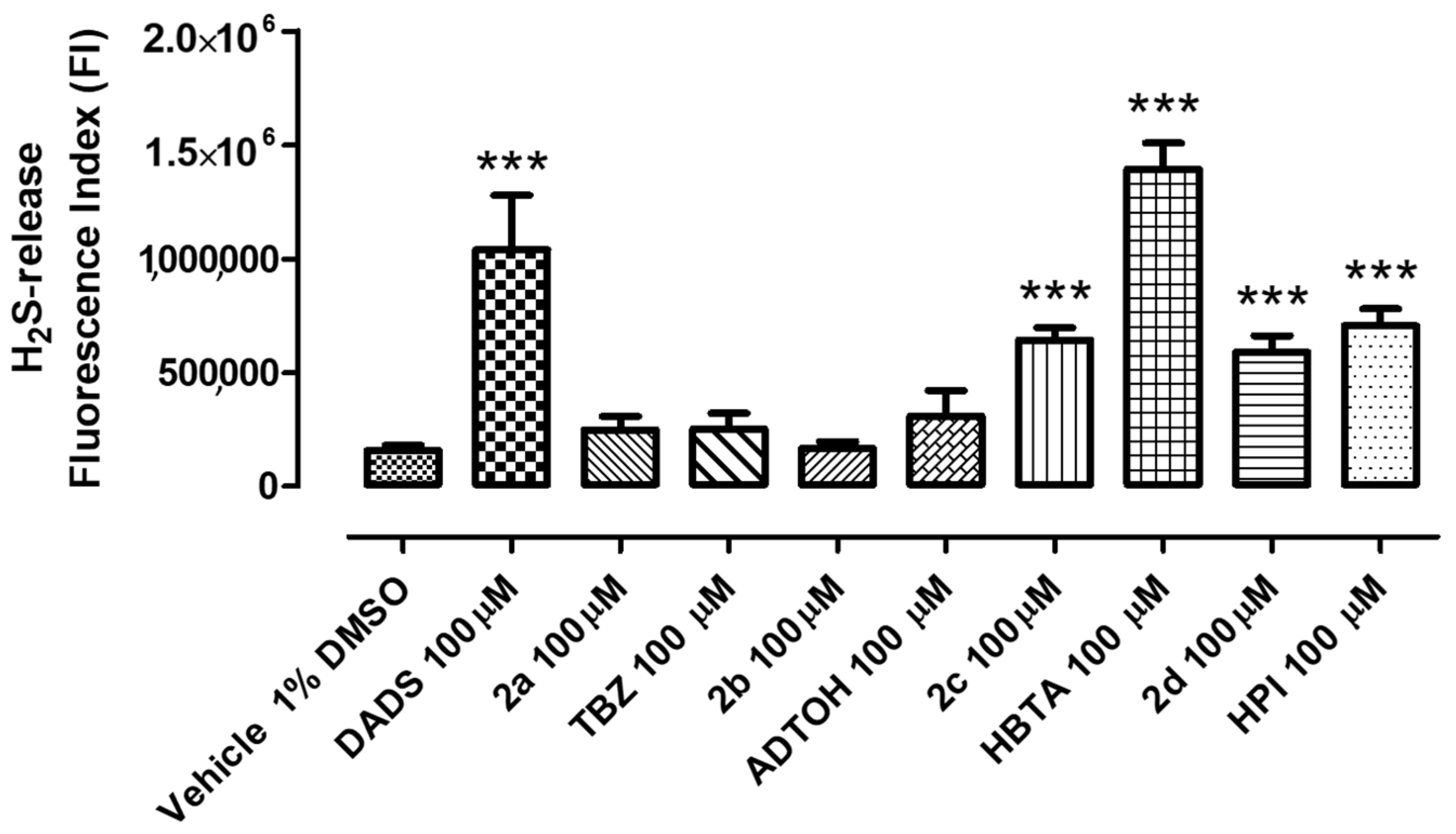
3.2. Intracellular H2S Release in HCEs
4. Experimental Section
4.1. Materials and Methods
4.2. Synthesis of Compounds 1a–1d
4.2.1. 2-(4-Carbamothioylphenoxy)-N-ethyl-N-(2-(3-methoxypropyl)-1,1-dioxido-6-sulfamoyl-3,4-dihydro-2H-thieno[3,2-e][1,2]thiazin-4-yl)acetamide (Brinzolamide–TBZ, Compound 1a)
4.2.2. N-Ethyl-N-(2-(3-methoxypropyl)-1,1-dioxido-6-sulfamoyl-3,4-dihydro-2H-thieno[3,2-e][1,2]thiazin-4-yl)-2-(4-(3-thioxo-3H-1,2-dithiol-5-yl)phenoxy)acetamide (Brinzolamide–ADTOH, Compound 1b)
4.2.3. Ethyl 4-(2-(ethyl(2-(3-methoxypropyl)-1,1-dioxido-6-sulfamoyl-3,4-dihydro-2H-thieno[3,2-e][1,2]thiazin-4-yl)amino)-2-oxoethoxy)benzodithioate (Brinzolamide–HBTA, Compound 1c)
4.2.4. 4-Isothiocyanatophenyl 4-(ethyl(2-(3-methoxypropyl)-1,1-dioxido-6-sulfamoyl-3,4-dihydro-2H-thieno[3,2-e][1,2]thiazin-4-yl)amino)-4-oxobutanoate (Brinzolamide–HPI, Compound 1d)
4.3. Synthesis of Compounds 2a–2d
4.3.1. 2-(4-Carbamothioylphenoxy)-N-(3-(4-(2-(cyclopropylmethoxy ethyl) phenoxy)-2-hydroxypropyl)-N-isopropylacetamide (Betaxolol–TBZ, Compound 2a)
4.3.2. N-(3-(4-(2-(Cyclopropylmethoxy)ethyl)phenoxy)-2-hydroxypropyl)-N-isopropyl-2-(4-(3-thioxo-3H-1,2-dithiol-5-yl)phenoxy)acetamide (Betaxolol–ADTOH, Compound 2b)
4.3.3. Ethyl 4-(2-((3-(4-(2-(cyclopropylmethoxy)ethyl)phenoxy)-2-hydroxypropyl)(isopropyl)amino)-2-oxoethoxy)benzodithioate (Betaxolol–HBTA, Compound 2c)
4.3.4. 1-(4-(2-(Cyclopropylmethoxy)ethyl)phenoxy)-3-(isopropylamino)propan-2-yl (4-isothiocyanatophenyl) Succinate (Betaxolol-HPI, Compound 2d)
4.4. Synthesis of Compounds 3a–3d
4.4.1. 4-Carbamothioylphenyl 4-((5-bromoquinoxalin-6-yl)(4,5-dihydro-1H-imidazol-2-yl)amino)-4-oxobutanoate (Brimonidine–TBZ, Compound 3a)
4.4.2. 4-(3-Thioxo-3H-1,2-dithiol-5-yl)phenyl 4-((5-bromoquinoxalin-6-yl)(4,5-dihydro-1H-imidazol-2-yl)amino)-4-oxobutanoate (Brimonidine–ADTOH, Compound 3b)
4.4.3. 4-((Ethylthio)carbonothioyl)phenyl 4-((5-bromoquinoxalin-6-yl)(4,5-dihydro-1H-imidazol-2-yl)amino)-4-oxobutanoate (Brimonidine–HBTA, Compound 3c)
4.4.4. 4-Isothiocyanatophenyl 4-((5-bromoquinoxalin-6-yl)(4,5-dihydro-1H-imidazol-2-yl)amino)-4-oxobutanoate (Brimonidine–HPI, Compound 3d)
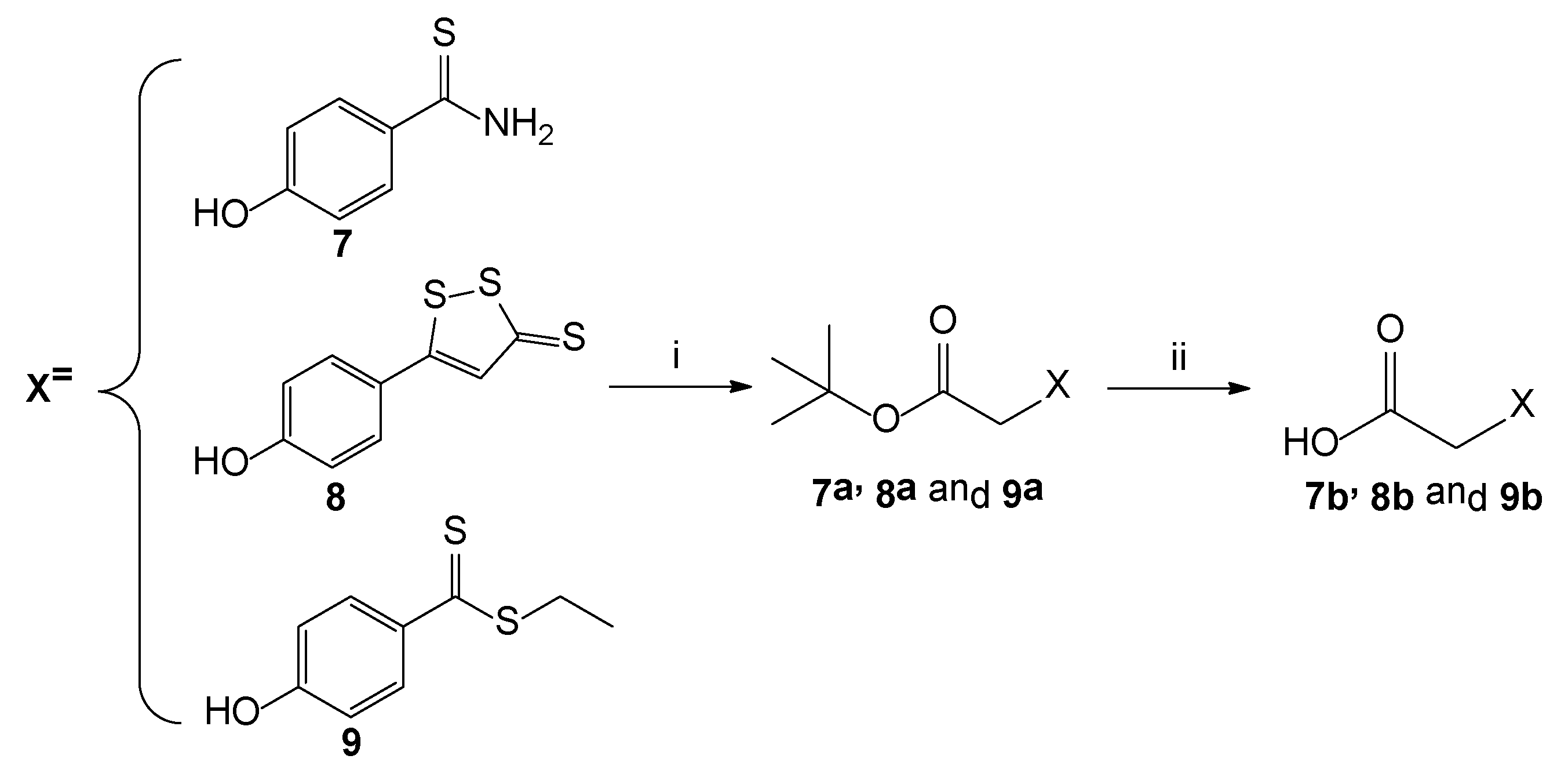
4.5. Synthesis of Intermediates 7a–9a
4.5.1. Tert-butyl 2-(4-carbamothioylphenoxy)acetate (7a)
4.5.2. Tert-butyl 2-(4-(3-thioxo-3H-1,2-dithiol-5-yl)phenoxy)acetate (8a)
4.5.3. Tert-butyl 2-(4-((ethylthio)carbonothioyl)phenoxy)acetate (9a)
4.6. General Procedure for the Synthesis of Intermediates 7b–9b
4.6.1. 2-(4-Carbamothioylphenoxy)acetic acid (7b)
4.6.2. 2-(4-(3-Thioxo-3H-1,2-dithiol-5-yl)phenoxy)acetic acid (8b)
4.6.3. 2-(4-((Ethylthio)carbonothioyl)phenoxy)acetic acid (9b)
4.7. Amperometric Determination of H2S Release
4.8. In Vitro Evaluation
4.8.1. Cell Culture
4.8.2. Evaluation of H2S Release on HCEs
4.8.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Weinreb, R.N.; Aung, T.; Medeiros, F.A. The pathophysiology and treatment of glaucoma: A review. JAMA 2014, 311, 1901–1911. [Google Scholar] [CrossRef] [PubMed]
- Allocco, A.R.; Ponce, J.A.; Riera, M.J.; Magurno, M.G. Critical pathway for primary open angle glaucoma diagnosis. Int. J. Ophthalmol. 2017, 10, 968–972. [Google Scholar] [PubMed]
- Tham, Y.-C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.X.; Xu, L.; Wei, W.B.; Jonas, J.B. Intraocular pressure and its normal range adjusted for ocular and systemic parameters. The Beijing Eye Study 2011. PLoS ONE 2018, 13, e0196926. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Aung, T.; Bourne, R.R.; Bron, A.M.; Ritch, R.; Panda-Jonas, S. Glaucoma. Lancet 2017, 390, 2183–2193. [Google Scholar] [CrossRef]
- Cioffi, C.L. Drug Delivery Challenges and Novel Therapeutic Approaches for Retinal Diseases; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Kang, J.M.; Tanna, A.P. Glaucoma. Med. Clin. N. Am. 2021, 105, 493–510. [Google Scholar] [CrossRef]
- Foster, P.J.; Buhrmann, R.; Quigley, H.A.; Johnson, G.J. The definition and classification of glaucoma in prevalence surveys. Br. J. Ophthalmol. 2002, 86, 238–242. [Google Scholar] [CrossRef]
- Hogan, M.J.; Alvarado, J.A.; Weddell, J.E. Histology of the Human Eye: An Atlas and Textbook; Saunders: Ann Arbor, MI, USA, 1971. [Google Scholar]
- Weinreb, R.N.; Leung, C.K.; Crowston, J.G.; Medeiros, F.A.; Friedman, D.S.; Wiggs, J.L.; Martin, K.R. Primary open-angle glaucoma. Nat. Rev. Dis. Prim. 2016, 2, 16067. [Google Scholar] [CrossRef]
- Kong, X.; Chen, Y.; Chen, X.; Sun, X. Influence of family history as a risk factor on primary angle closure and primary open angle glaucoma in a Chinese population. Ophthalmic Epidemiol. 2011, 18, 226–232. [Google Scholar] [CrossRef]
- Wang, R. Two’s company, three’s a crowd: Can H2S be the third endogenous gaseous transmitter? FASEB J. 2002, 16, 1792–1798. [Google Scholar] [CrossRef]
- Corvino, A.; Frecentese, F.; Magli, E.; Perissutti, E.; Santagada, V.; Scognamiglio, A.; Caliendo, G.; Fiorino, F.; Severino, B. Trends in H(2)S-Donors Chemistry and Their Effects in Cardiovascular Diseases. Antioxidants 2021, 10, 429. [Google Scholar] [CrossRef] [PubMed]
- Zanardo, R.C.; Brancaleone, V.; Distrutti, E.; Fiorucci, S.; Cirino, G.; Wallace, J.L. Hydrogen sulfide is an endogenous modulator of leukocyte-mediated inflammation. FASEB J. 2006, 20, 2118–2120. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Prokosch, V.; Liu, H. Current Perspective of Hydrogen Sulfide as a Novel Gaseous Modulator of Oxidative Stress in Glaucoma. Antioxidants 2021, 10, 671. [Google Scholar] [CrossRef] [PubMed]
- Khattak, S.; Zhang, Q.Q.; Sarfraz, M.; Muhammad, P.; Ngowi, E.E.; Khan, N.H.; Rauf, S.; Wang, Y.Z.; Qi, H.W.; Wang, D.; et al. The Role of Hydrogen Sulfide in Respiratory Diseases. Biomolecules 2021, 11, 682. [Google Scholar] [CrossRef] [PubMed]
- Kimura, H. Production and physiological effects of hydrogen sulfide. Antioxid. Redox Signal. 2014, 20, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Shang, Q.; Yao, J.; Ji, Y. Hydrogen sulfide: A gaseous signaling molecule modulates tissue homeostasis: Implications in ophthalmic diseases. Cell Death Dis. 2019, 10, 293. [Google Scholar] [CrossRef]
- George, A.K.; Homme, R.P.; Stanisic, D.; Tyagi, S.C.; Singh, M. Protecting the aging eye with hydrogen sulfide. Can. J. Physiol. Pharmacol. 2021, 99, 161–170. [Google Scholar] [CrossRef]
- Huang, S.; Huang, P.; Liu, X.; Lin, Z.; Wang, J.; Xu, S.; Guo, L.; Leung, C.K.-s.; Zhong, Y. Relevant variations and neuroprotecive effect of hydrogen sulfide in a rat glaucoma model. Neuroscience 2017, 341, 27–41. [Google Scholar] [CrossRef]
- Liu, H.; Anders, F.; Thanos, S.; Mann, C.; Liu, A.; Grus, F.H.; Pfeiffer, N.; Prokosch-Willing, V. Hydrogen Sulfide Protects Retinal Ganglion Cells Against Glaucomatous Injury In Vitro and In Vivo. Investig. Ophthalmol. Vis. Sci. 2017, 58, 5129–5141. [Google Scholar] [CrossRef]
- Li, P.; Liu, H.; Shi, X.; Prokosch, V. Hydrogen Sulfide: Novel Endogenous and Exogenous Modulator of Oxidative Stress in Retinal Degeneration Diseases. Molecules 2021, 26, 2411. [Google Scholar] [CrossRef]
- Scheid, S.; Goeller, M.; Baar, W.; Wollborn, J.; Buerkle, H.; Schlunck, G.; Lagrèze, W.; Goebel, U.; Ulbrich, F. Hydrogen Sulfide Reduces Ischemia and Reperfusion Injury in Neuronal Cells in a Dose- and Time-Dependent Manner. Int. J. Mol. Sci. 2021, 22, 10099. [Google Scholar] [CrossRef] [PubMed]
- Perrino, E.; Uliva, C.; Lanzi, C.; Soldato, P.D.; Masini, E.; Sparatore, A. New prostaglandin derivative for glaucoma treatment. Bioorg. Med. Chem. Lett. 2009, 19, 1639–1642. [Google Scholar] [CrossRef] [PubMed]
- Corvino, A.; Citi, V.; Fiorino, F.; Frecentese, F.; Magli, E.; Perissutti, E.; Santagada, V.; Calderone, V.; Martelli, A.; Gorica, E.; et al. H(2)S donating corticosteroids: Design, synthesis and biological evaluation in a murine model of asthma. J. Adv. Res. 2022, 35, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Severino, B.; Corvino, A.; Fiorino, F.; Luciano, P.; Frecentese, F.; Magli, E.; Saccone, I.; Di Vaio, P.; Citi, V.; Calderone, V.; et al. 1,2,4-Thiadiazolidin-3,5-diones as novel hydrogen sulfide donors. Eur. J Med. Chem. 2018, 143, 1677–1686. [Google Scholar] [CrossRef] [PubMed]
- Ercolano, G.; De Cicco, P.; Frecentese, F.; Saccone, I.; Corvino, A.; Giordano, F.; Magli, E.; Fiorino, F.; Severino, B.; Calderone, V.; et al. Anti-metastatic Properties of Naproxen-HBTA in a Murine Model of Cutaneous Melanoma. Front. Pharmacol. 2019, 10, 66. [Google Scholar] [CrossRef] [PubMed]
- Giordano, F.; Corvino, A.; Scognamiglio, A.; Citi, V.; Gorica, E.; Fattorusso, C.; Persico, M.; Caliendo, G.; Fiorino, F.; Magli, E.; et al. Hybrids between H(2)S-donors and betamethasone 17-valerate or triamcinolone acetonide inhibit mast cell degranulation and promote hyperpolarization of bronchial smooth muscle cells. Eur. J. Med. Chem. 2021, 221, 113517. [Google Scholar] [CrossRef] [PubMed]
- Martelli, A.; Testai, L.; Citi, V.; Marino, A.; Pugliesi, I.; Barresi, E.; Nesi, G.; Rapposelli, S.; Taliani, S.; Da Settimo, F.; et al. Arylthioamides as H2S Donors: L-Cysteine-Activated Releasing Properties and Vascular Effects in Vitro and in Vivo. ACS Med. Chem. Lett. 2013, 4, 904–908. [Google Scholar] [CrossRef]
- Citi, V.; Corvino, A.; Fiorino, F.; Frecentese, F.; Magli, E.; Perissutti, E.; Santagada, V.; Brogi, S.; Flori, L.; Gorica, E. Structure-activity relationships study of isothiocyanates for H2S releasing properties: 3-Pyridyl-isothiocyanate as a new promising cardioprotective agent. J. Adv. Res. 2021, 27, 41–53. [Google Scholar] [CrossRef]
- Wallace, J.L.; Cirino, G.; Caliendo, G.; Sparatore, A.; Santagada, V.; Fiorucci, S. Derivatives of 4-or 5-Aminosalicylic Acid. U.S. Patent 7910568, 22 March 2011. [Google Scholar]
- Martelli, A.; Citi, V.; Testai, L.; Brogi, S.; Calderone, V. Organic Isothiocyanates as Hydrogen Sulfide Donors. Antioxid. Redox Signal. 2020, 32, 110–144. [Google Scholar] [CrossRef]
- Martelli, A.; Citi, V.; Calderone, V. Vascular Effects of H(2)S-Donors: Fluorimetric Detection of H(2)S Generation and Ion Channel Activation in Human Aortic Smooth Muscle Cells. Methods Mol. Biol. 2019, 2007, 79–87. [Google Scholar]
- Lin, Y.; Yang, X.; Lu, Y.; Liang, D.; Huang, D. Isothiocyanates as H(2)S Donors Triggered by Cysteine: Reaction Mechanism and Structure and Activity Relationship. Org. Lett. 2019, 21, 5977–5980. [Google Scholar] [CrossRef] [PubMed]
- Mannermaa, E.; Vellonen, K.S.; Urtti, A. Drug transport in corneal epithelium and blood-retina barrier: Emerging role of transporters in ocular pharmacokinetics. Adv. Drug Deliv. Rev. 2006, 58, 1136–1163. [Google Scholar] [CrossRef] [PubMed]
- Davies, N.M. Biopharmaceutical considerations in topical ocular drug delivery. Clin. Exp. Pharmacol. Physiol. 2000, 27, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Scozzafava, A.; Menabuoni, L.; Mincione, F.; Briganti, F.; Mincione, G.; Supuran, C.T. Carbonic anhydrase inhibitors. Synthesis of water-soluble, topically effective, intraocular pressure-lowering aromatic/heterocyclic sulfonamides containing cationic or anionic moieties: Is the tail more important than the ring? J. Med. Chem. 1999, 42, 2641–2650. [Google Scholar] [CrossRef] [PubMed]
- Petrović, S.D.; Stojanović, N.D.; Antonović, D.G.; Mijin, D.Ž.; Nikolić, A.D. Conformations of unsymmetrical N-t-butyl-N-substituted 2-phenylacetamides. J. Mol. Struct. 1997, 410–411, 35–38. [Google Scholar] [CrossRef]
- Isbrandt, L.; Tung, W.C.T.; Rogers, M.T. An NMR study of hindered internal rotation in some unsymmetrically N,N-disubstituted acetamides. J. Magn. Reson. 1973, 9, 461–466. [Google Scholar] [CrossRef]
- LaPlanche, L.A.; Rogers, M.T. Configurations in Unsymmetrically N,N-Disubstituted Amides. J. Am. Chem. Soc. 1963, 85, 3728–3730. [Google Scholar] [CrossRef]
- Zheng, Y.; Tice, C.M.; Singh, S.B. Conformational control in structure-based drug design. Bioorg. Med. Chem. Lett. 2017, 27, 2825–2837. [Google Scholar] [CrossRef]
- Lin, V.S.; Chen, W.; Xian, M.; Chang, C.J. Chemical probes for molecular imaging and detection of hydrogen sulfide and reactive sulfur species in biological systems. Chem. Soc. Rev. 2015, 44, 4596–4618. [Google Scholar] [CrossRef]
- Dikopf, M.S.; Vajaranant, T.S.; Edward, D.P. Topical treatment of glaucoma: Established and emerging pharmacology. Expert Opin. Pharmacother. 2017, 18, 885–898. [Google Scholar] [CrossRef]
- Fortunato, S.; Lenzi, C.; Granchi, C.; Citi, V.; Martelli, A.; Calderone, V.; Di Pietro, S.; Signore, G.; Di Bussolo, V.; Minutolo, F. First Examples of H2S-Releasing Glycoconjugates: Stereoselective Synthesis and Anticancer Activities. Bioconj. Chem. 2019, 30, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Testai, L.; Citi, V.; Martelli, A.; Brogi, S.; Calderone, V. Role of hydrogen sulfide in cardiovascular ageing. Pharmacol. Res. 2020, 160, 105125. [Google Scholar] [CrossRef] [PubMed]
- Martelli, A.; Piragine, E.; Gorica, E.; Citi, V.; Testai, L.; Pagnotta, E.; Lazzeri, L.; Pecchioni, N.; Ciccone, V.; Montanaro, R.; et al. The H2S-Donor Erucin Exhibits Protective Effects against Vascular Inflammation in Human Endothelial and Smooth Muscle Cells. Antioxidants 2021, 10, 961. [Google Scholar] [CrossRef] [PubMed]
- Testai, L.; Pagnotta, E.; Piragine, E.; Flori, L.; Citi, V.; Martelli, A.; Di Cesare Mannelli, L.; Ghelardini, C.; Matteo, R.; Suriano, S.; et al. Cardiovascular benefits of Eruca sativa mill. Defatted seed meal extract: Potential role of hydrogen sulfide. Phytother. Res. 2022, 36, 2616–2627. [Google Scholar] [CrossRef] [PubMed]
- Susmit, M.; Farvo, C.; Somnath, S. Unmet needs in glaucoma therapy: The potential role of hydrogen sulfide and its delivery strategies. J. Control. Release 2022, 347, 256–269. [Google Scholar]
- Sampath Kumar, H.M.; Herrmann, L.; Tsogoeva, S.B. Structural hybridization as a facile approach to new drug candidates. Bioorg. Med. Chem. Lett. 2020, 30, 127514. [Google Scholar] [CrossRef] [PubMed]





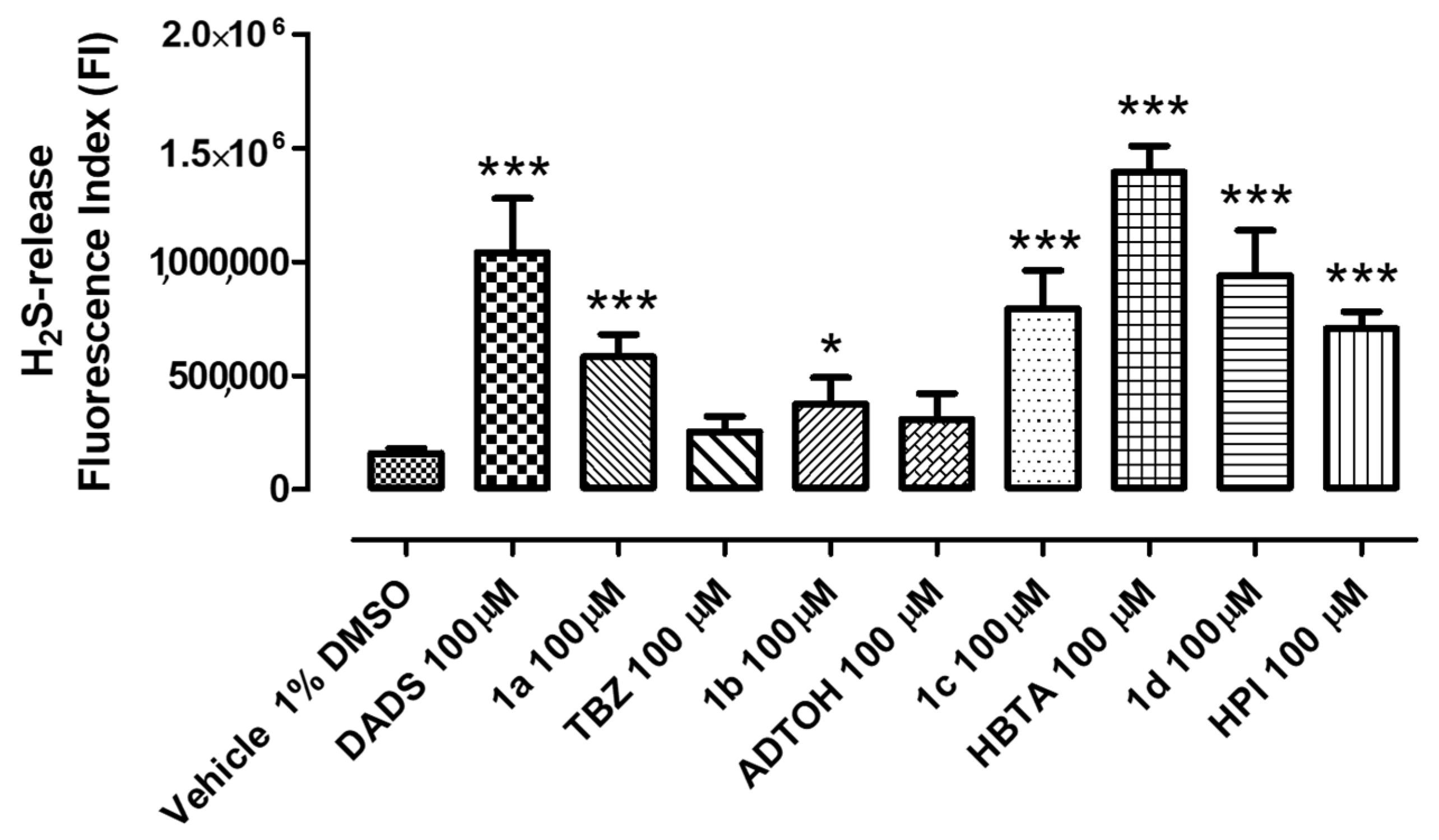

Brinzolamide Derivatives 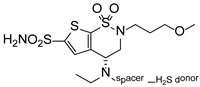 | |||||
|---|---|---|---|---|---|
| Cmpd | Spacer | H2S Donor | H2S Release (μM) | ||
| + L-Cys | − L-Cys | ||||
| 1a |  | 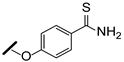 | 0.4 ± 0.2 | n.d. | |
| 1b |  | 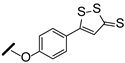 | 0.9 ± 0.3 | 0.4 ± 0.1 | |
| 1c |  | 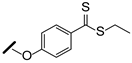 | 3.5 ± 0.3 | n.d. | |
| 1d |  | 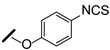 | 2.1 ± 0.4 | 0.4 ± 0.1 | |
Betaxolol derivatives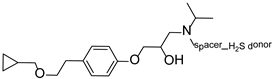 | |||||
| 2a |  | 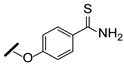 | 0.5 ± 0.2 | n.d. | |
| 2b |  | 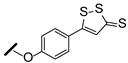 | n.d. | n.d. | |
| 2c |  | 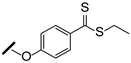 | 0.5 ± 0.1 | n.d. | |
| 2d | 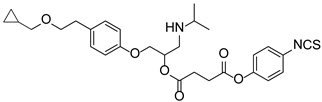 | 0.5 ± 0.1 | n.d. | ||
Brimonidine derivatives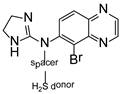 | |||||
| 3a |  | 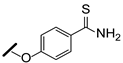 | 1.2 ± 0.5 | n.d. | |
| 3b |  | 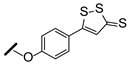 | 0.9 ± 0.4 | n.d. | |
| 3c |  | 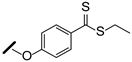 | 1.7 ± 0.5 | n.d. | |
| 3d |  | 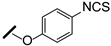 | 6.2 ± 0.5 | 0.8 ± 0.1 | |
| H2S release (μM) | |||||
| + L-Cys | − L-Cys | ||||
| TBZ (7) | 1.6 ± 0.3 | n.d. | |||
| ADT-OH (8) | 1.8 ± 0.5 | 1.1 ± 0.3 | |||
| HBTA (9) | 3.5 ± 0.5 | n.d. | |||
| HPI (10) | 15 ± 0.2 | 3.4 ± 0.7 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sparaco, R.; Citi, V.; Magli, E.; Martelli, A.; Piragine, E.; Calderone, V.; Andreozzi, G.; Perissutti, E.; Frecentese, F.; Santagada, V.; et al. Design, Synthesis and Evaluation of Novel Molecular Hybrids between Antiglaucoma Drugs and H2S Donors. Int. J. Mol. Sci. 2022, 23, 13804. https://doi.org/10.3390/ijms232213804
Sparaco R, Citi V, Magli E, Martelli A, Piragine E, Calderone V, Andreozzi G, Perissutti E, Frecentese F, Santagada V, et al. Design, Synthesis and Evaluation of Novel Molecular Hybrids between Antiglaucoma Drugs and H2S Donors. International Journal of Molecular Sciences. 2022; 23(22):13804. https://doi.org/10.3390/ijms232213804
Chicago/Turabian StyleSparaco, Rosa, Valentina Citi, Elisa Magli, Alma Martelli, Eugenia Piragine, Vincenzo Calderone, Giorgia Andreozzi, Elisa Perissutti, Francesco Frecentese, Vincenzo Santagada, and et al. 2022. "Design, Synthesis and Evaluation of Novel Molecular Hybrids between Antiglaucoma Drugs and H2S Donors" International Journal of Molecular Sciences 23, no. 22: 13804. https://doi.org/10.3390/ijms232213804
APA StyleSparaco, R., Citi, V., Magli, E., Martelli, A., Piragine, E., Calderone, V., Andreozzi, G., Perissutti, E., Frecentese, F., Santagada, V., Caliendo, G., Severino, B., Corvino, A., & Fiorino, F. (2022). Design, Synthesis and Evaluation of Novel Molecular Hybrids between Antiglaucoma Drugs and H2S Donors. International Journal of Molecular Sciences, 23(22), 13804. https://doi.org/10.3390/ijms232213804













