A Review on Stimuli-Actuated 3D Micro/Nanostructures for Tissue Engineering and the Potential of Laser-Direct Writing via Two-Photon Polymerization for Structure Fabrication
Abstract
:1. Introduction
2. Laser Assisted Fabrication Methods
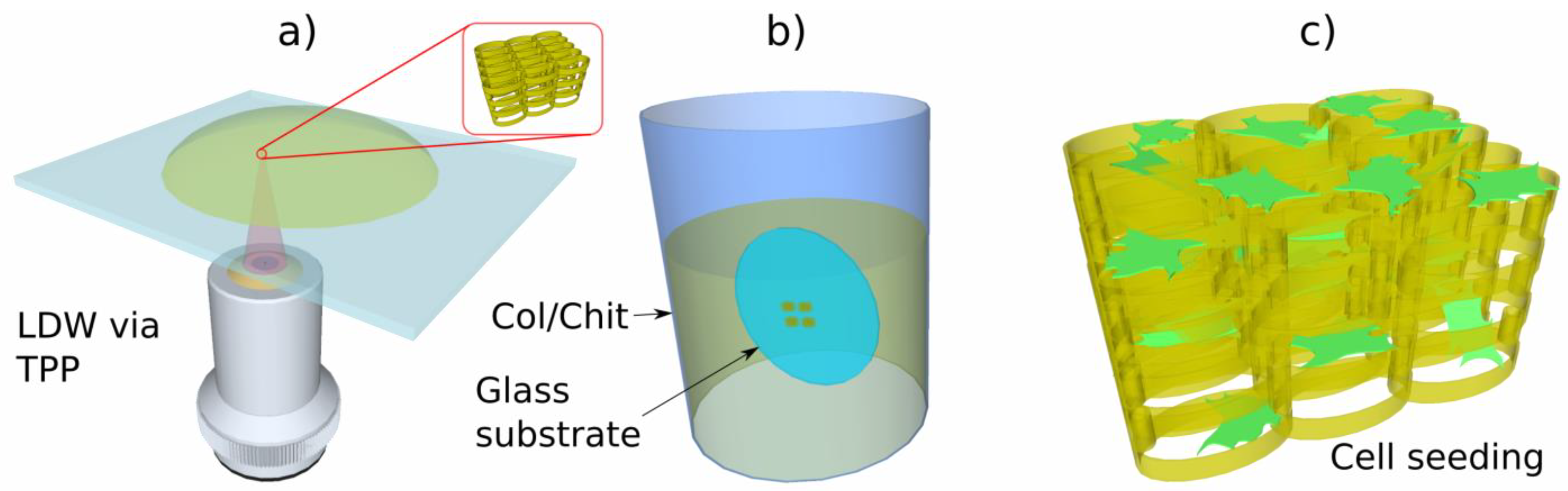
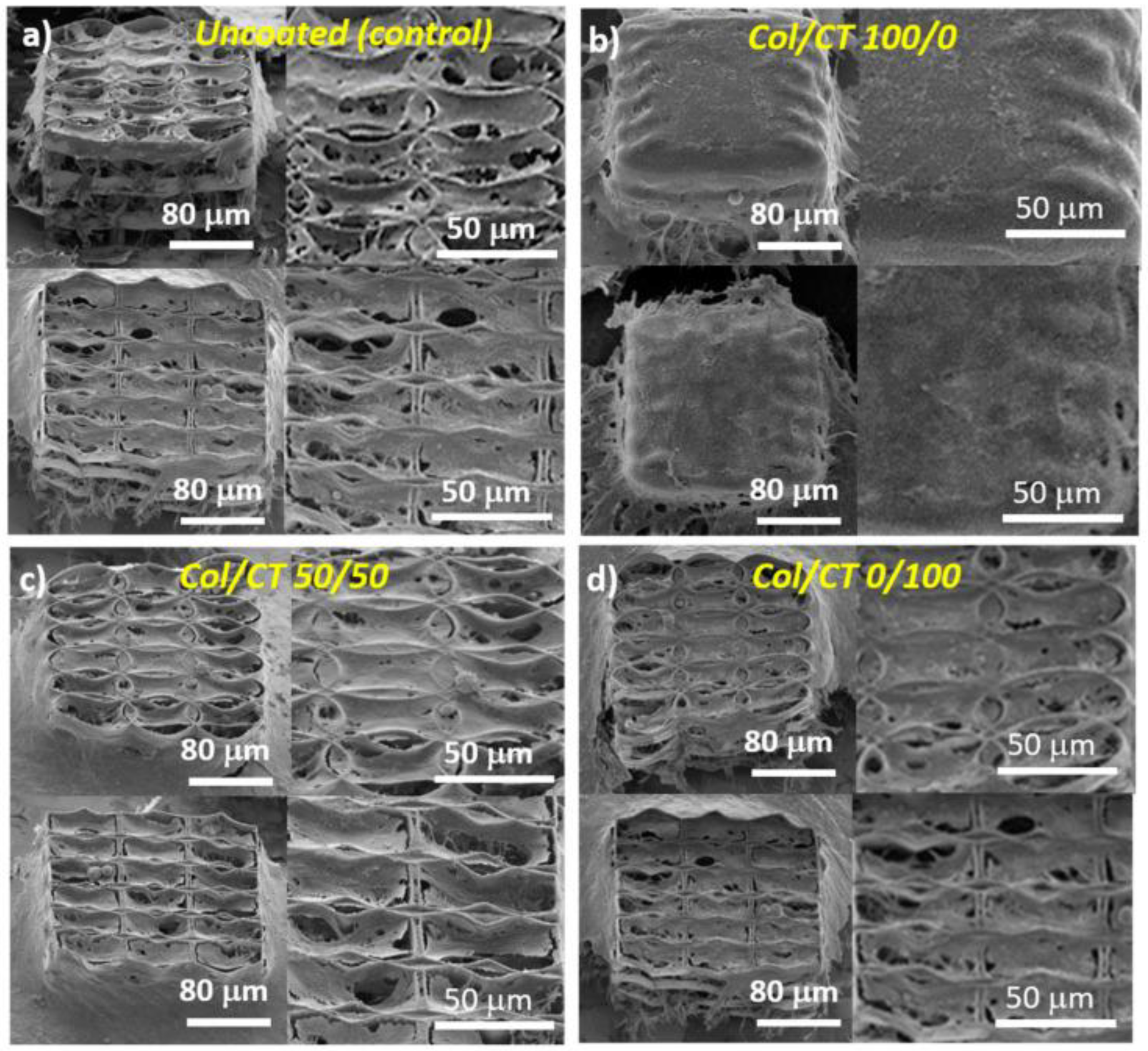
3. Laser-direct Writing via Two Photon Polymerization
4. Actuation of 3D Micro/Nanostructures Using Different Types of Stimuli, for Tissue Engineering Applications
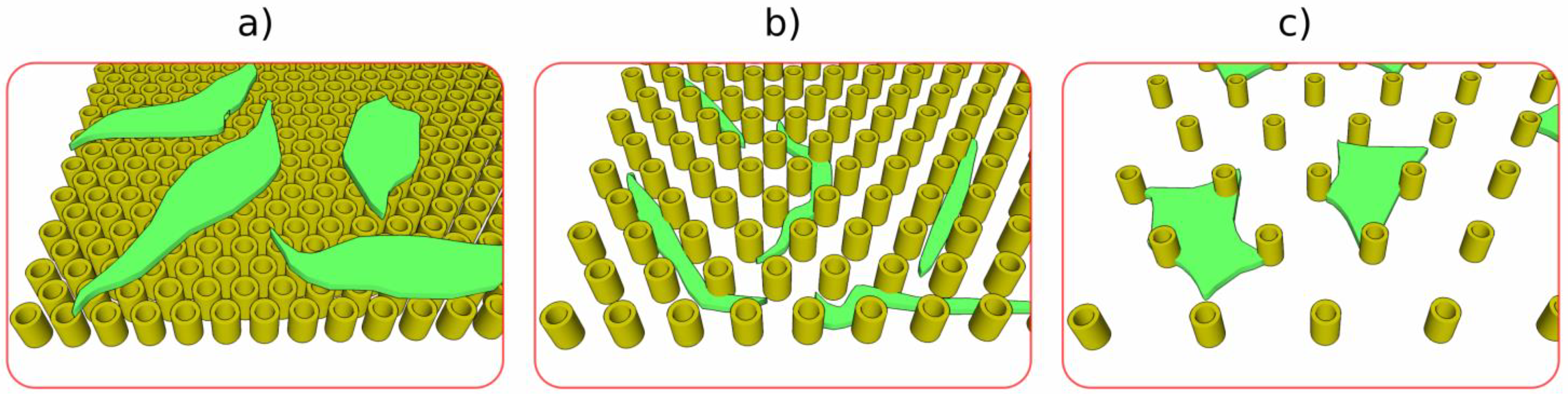
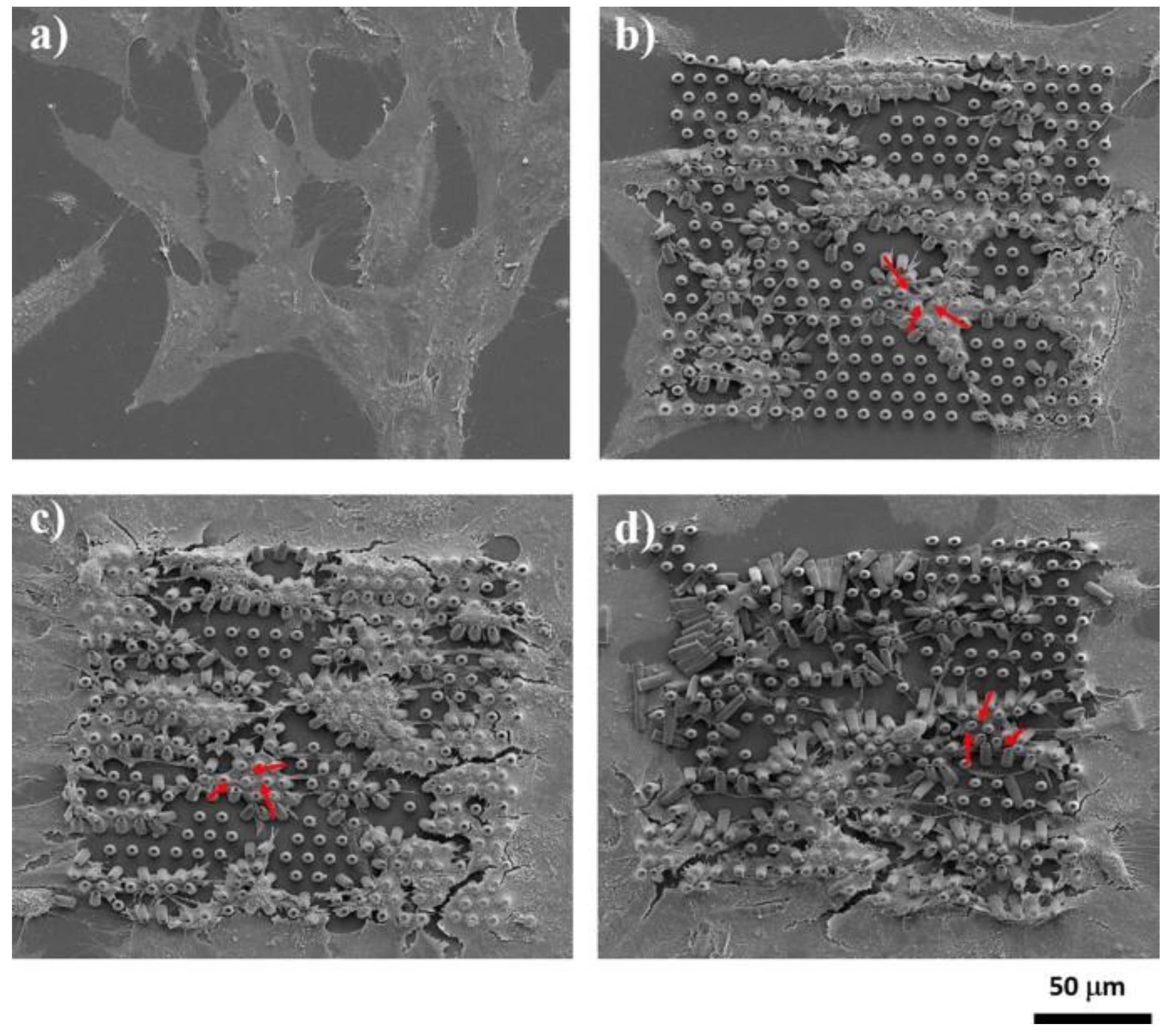
4.1. 3D Structures Actuated through MicroTopographies
4.2. 3D Structures Actuated through Hierarchic Micro/Nano-Topographies
4.3. 3D Structures Actuated through Mechanical Stimuli
4.4. 3D Structures Actuated through Chemical Stimuli
4.5. 3D Structures Actuated by Electric Fields
4.6. 3D Structures Actuated by Magnetic Fields
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bahraminasab, M. Challenges on optimization of 3D-printed bone scaffolds. Biomed. Eng. Online 2020, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Ikada, Y. Challenges in tissue engineering. J. R. Soc. Interface 2006, 3, 589–601. [Google Scholar] [CrossRef]
- Pogorielov, M.; Oleshko, O.; Hapchenko, A. Tissue Engineering: Challenges and Selected Application. Adv. Tissue Eng. Regen. Med. Open Access 2017, 3, 330–334. [Google Scholar] [CrossRef]
- Bácskay, I.; Ujhelyi, Z.; Fehér, P.; Arany, P. The Evolution of the 3D-Printed Drug Delivery Systems: A Review. Pharmaceutics 2022, 14, 1312. [Google Scholar] [CrossRef]
- Tricinci, O.; Pasquale, D.D.; Marino, A.; Battaglini, M.; Pucci, C.; Ciofani, G. A 3D Biohybrid Real-Scale Model of the Brain Cancer Microenvironment for Advanced In Vitro Testing. Adv. Mater. Technol. 2020, 5, 2000540. [Google Scholar] [CrossRef]
- Ho, B.; Mishra, A.; Hu, K.; An, J.; Kim, Y.-J.; Yoon, Y. Femtosecond-Laser-Based 3D Printing for Tissue Engineering and Cell Biology Applications. ACS Biomater. Sci. Eng. 2017, 3, 2198. [Google Scholar] [CrossRef]
- Nava, M.M.; Zandrini, T.; Cerullo, G.; Osellame, R.; Raimondi, M.T. 3D Cell Culture—Methods and Protocols; Koledova, Z., Ed.; Springer: New York, NY, USA, 2017; pp. 253–266. [Google Scholar]
- Raimondi, M.T.; Eaton, S.M.; Nava, M.M.; Laganà, M.; Cerullo, G.; Osellame, R. Two-Photon Laser Polymerization: From Fundamentals to Biomedical Application in Tissue Engineering and Regenerative Medicine. J. Appl Biomater. Funct. Mater. 2012, 10, 55. [Google Scholar] [CrossRef]
- Meloni, G.; Tricinci, O.; Degl’Innocenti, A.; Mazzolai, B. A protein-coated micro-sucker patch inspired by octopus for adhesion in wet conditions. Sci. Rep. 2020, 10, 15480. [Google Scholar] [CrossRef]
- Tricinci, O.; Eason, E.V.; Filippeschi, C.; Mondini, A.; Mazzolai, B.; Pugno, N.M.; Cutkosky, M.R.; Greco, F.; Mattoli, V. Approximating gecko setae via direct laser lithography. Smart Mater. Struct. 2018, 27, 075009. [Google Scholar] [CrossRef] [Green Version]
- Hasan, R.M.M.; Luo, X. Promising Lithography Techniques for Next-Generation Logic Devices. Nanomanuf. Metrol. 2018, 1, 67. [Google Scholar] [CrossRef]
- Chen, Y. Nanofabrication by electron beam lithography and its applications: A review. Microelectron. Eng. 2015, 135, 57. [Google Scholar] [CrossRef]
- Kim, S.-S.; Chalykh, R.; Kim, H.; Lee, S.; Park, C.; Hwang, M.; Park, J.; Jinhong, P.; Kim, H.; Jeon, J.; et al. Progress in EUV Lithography toward Manufacturing; SPIE, Ed.; The International Society for Optical Engineering: San Jose, CA, USA, 2017. [Google Scholar]
- Gauvin, R.; Chen, Y.-C.; Lee, J.W.; Soman, P.; Zorlutuna, P.; Nichol, J.W.; Bae, H.; Chen, S.; Khademhosseini, A. Microfabrication of complex porous tissue engineering scaffolds using 3D projection stereolithography. Biomaterials 2012, 33, 15. [Google Scholar] [CrossRef] [Green Version]
- Liu, K.; Li, W.; Chen, S.; Wen, W.; Lu, L.; Liu, M.; Zhou, C.; Luo, B. The design, fabrication and evaluation of 3D printed gHNTs/gMgO whiskers/PLLA composite scaffold with honeycomb microstructure for bone tissue engineering. Compos. Part B Eng. 2020, 192, 108001. [Google Scholar] [CrossRef]
- Fendler, C.; Denker, C.; Harberts, J.; Bayat, P.; Zierold, R.; Loers, G.; Münzenberg, M.; Blick, R.H. Microscaffolds by Direct Laser Writing for Neurite Guidance Leading to Tailor-Made Neuronal Networks. Adv. Biosyst. 2019, 3, 1800329. [Google Scholar] [CrossRef]
- Gonçalves, J.L.M.; Lopes, A.B.C.; Baleizao, C.; Farinha, J.P. Mesoporous Silica Nanoparticles Modified inside and out for ON: OFF pH-Modulated Cargo Release. Pharmaceutics 2021, 13, 716. [Google Scholar] [CrossRef]
- Califano, V.; Bloisi, F.; Vicari, L.R.M.; Yunos, D.M.; Chatzistavrou, X.; Boccaccini, A.R. Matrix Assisted Pulsed Laser Evaporation (MAPLE) of Poly(D,L lactide) (PDLLA) on Three Dimensional Bioglass® Structures. Adv. Eng. Mater. 2009, 11, 685–689. [Google Scholar] [CrossRef]
- Rodrigo, K.; Czuba, P.; Toftmann, B.; Schou, J.; Pedrys, R. Surface morphology of polyethylene glycol films produced by matrix-assisted pulsed laser evaporation (MAPLE): Dependence on substrate temperature. Appl. Surf. Sci. 2006, 252, 4824. [Google Scholar] [CrossRef]
- Bernardeschi, I.; Ilyas, M.; Beccai, L. A Review on Active 3D Microstructures via Direct Laser Lithography. Adv. Intell. Syst. 2021, 3, 2100051. [Google Scholar] [CrossRef]
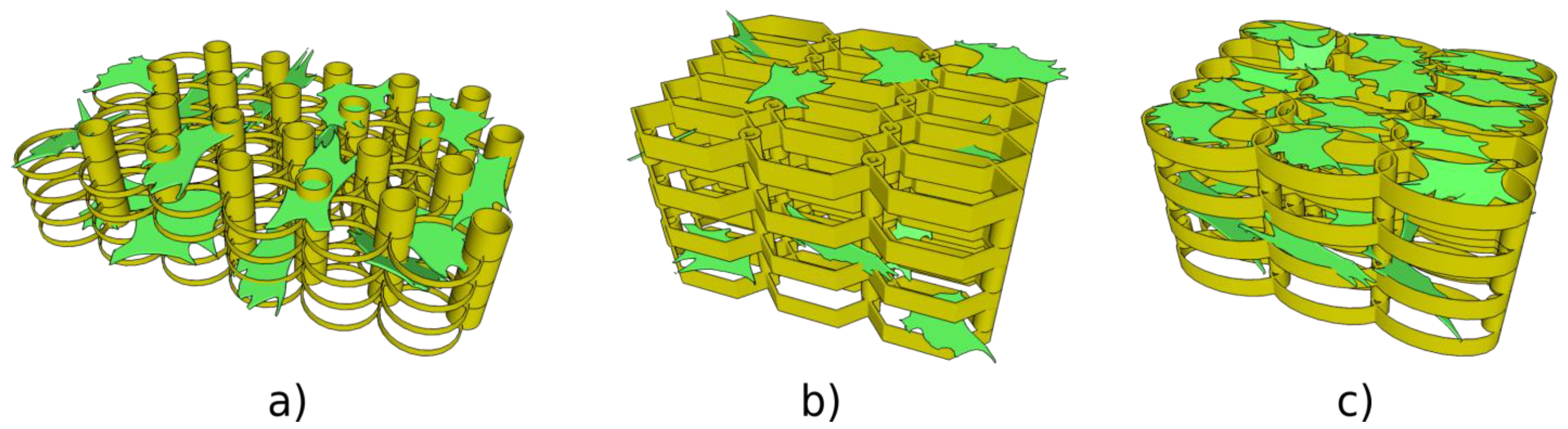
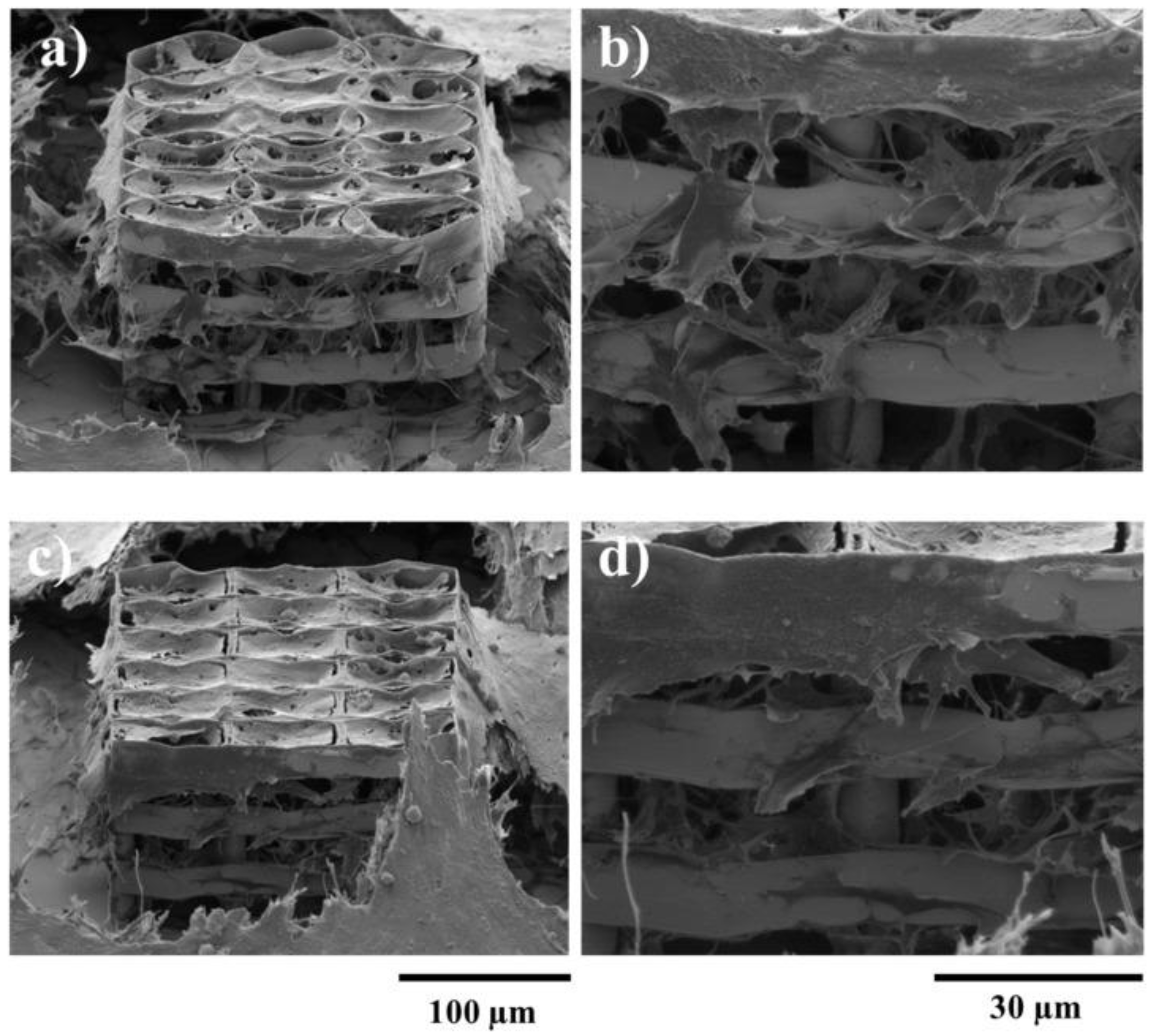
- Paun, I.A.; Popescu, R.C.; Mustaciosu, C.C.; Zamfirescu, M.; Calin, B.S.; Mihailescu, M.; Dinescu, M.; Popescu, A.; Chioibasu, D.G.; Soproniy, M.; et al. Laser-direct writing by two-photon polymerization of 3D honeycomb-like structures for bone regeneration. Biofabrication 2018, 10, 025009. [Google Scholar] [CrossRef]
- Mansouri, N.; Bagheri, S. The influence of topography on tissue engineering perspective. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 61, 906–921. [Google Scholar] [CrossRef]
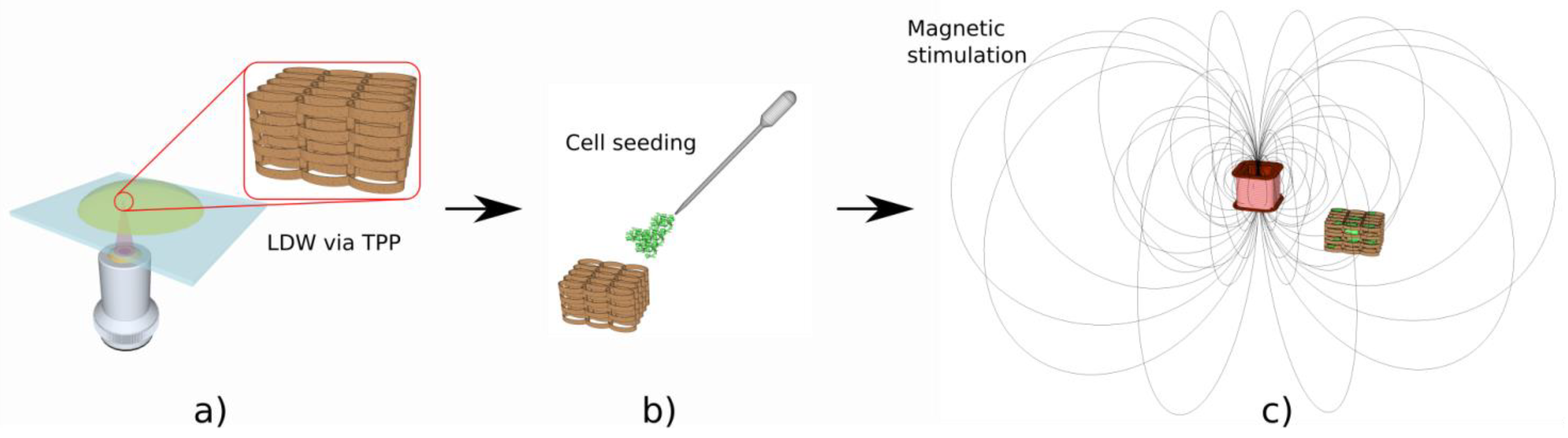
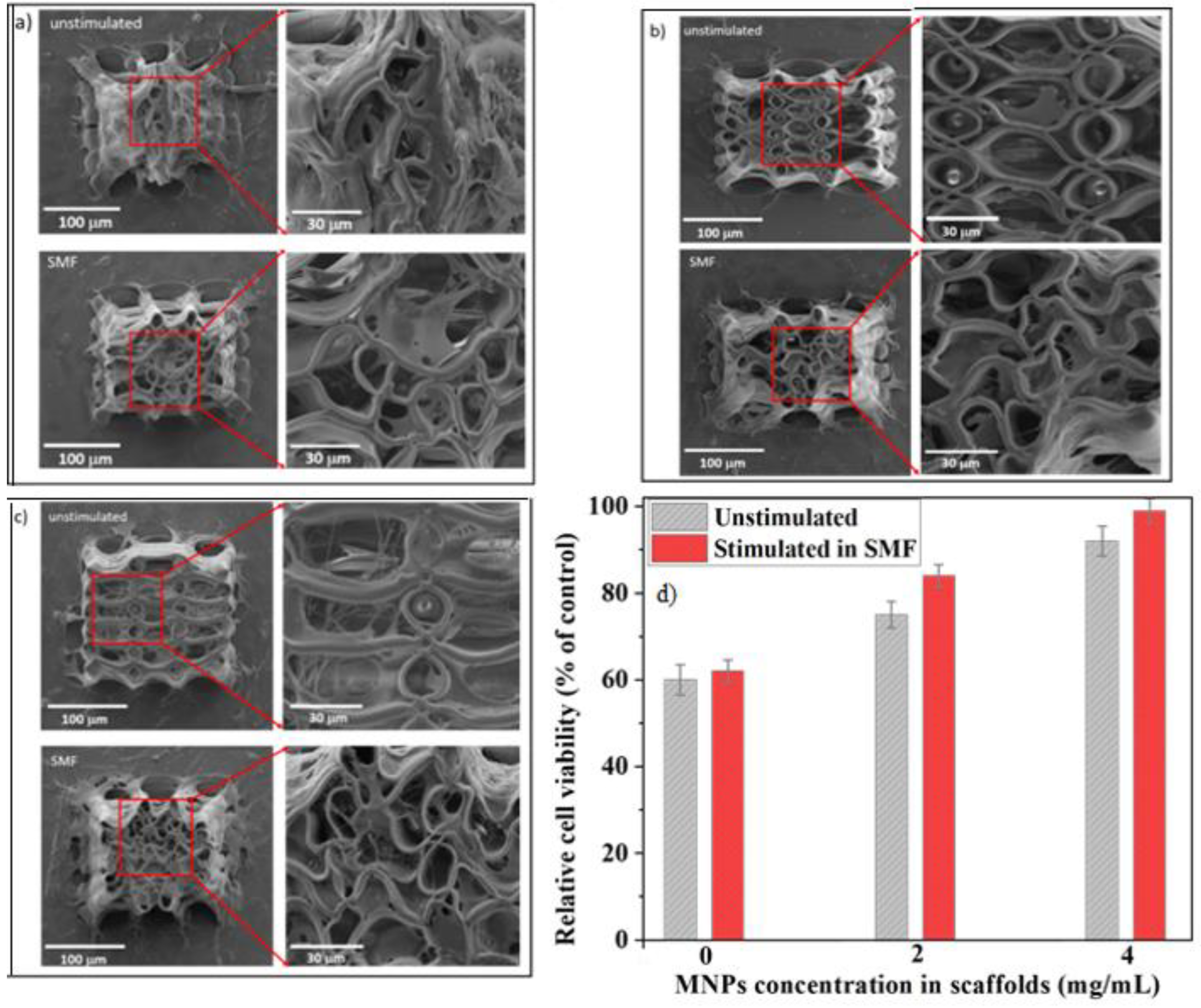
- Paun, I.A.; Popescu, R.C.; Calin, B.S.; Mustaciosu, C.C.; Dinescu, M.; Luculescu, C.R. 3D Biomimetic Magnetic Structures for Static Magnetic Field Stimulation of Osteogenesis. Int. J. Mol. Sci. 2018, 19, 495. [Google Scholar] [CrossRef] [Green Version]
- Efimenko, K.; Finlay, J.; Callow, M.E.; Callow, J.A.; Genzer, J. Development and Testing of Hierarchically Wrinkled Coatings for Marine Antifouling. ACS Appl. Mater. Interfaces 2009, 1, 1031–1040. [Google Scholar] [CrossRef]
- John, P.S.; Poulose, C.S.; George, B. Therapeutic ultrasound in fracture healing: The mechanism of osteoinduction. Indian J. Orthop. 2008, 42, 444–447. [Google Scholar] [CrossRef]
- Mundi, R.; Petis, S.; Kaloty, R.; Shetty, V.; Bhandari, M. Low-intensity pulsed ultrasound: Fracture healing. Indian J. Orthop. 2009, 43, 132–140. [Google Scholar] [CrossRef]
- Paun, I.A.; Calin, B.S.; Mustaciosu, C.C.; Mihailescu, M.; Popovici, C.S.; Luculescu, C.R. Osteogenic cells differentiation on topological surfaces under ultrasound stimulation. J. Mater. Sci. 2019, 54, 11213–11230. [Google Scholar] [CrossRef]
- Cheng, C.; Gupta, M. Surface functionalization of 3D-printed plastics via initiated chemical vapor deposition. Beilstein J. Nanotechnol. 2017, 8, 1629–1636. [Google Scholar] [CrossRef]
- Păun, I.A.; Mustăciosu, C.C.; Popescu, R.C.; Călin, B.; Mihăilescu, M. Collagen/Chitosan Functionalization of Complex 3D Structures Fabricated by Laser Direct Writing via Two-Photon Polymerization for Enhanced Osteogenesis. Int. J. Mol. Sci. 2020, 21, 6426. [Google Scholar] [CrossRef]
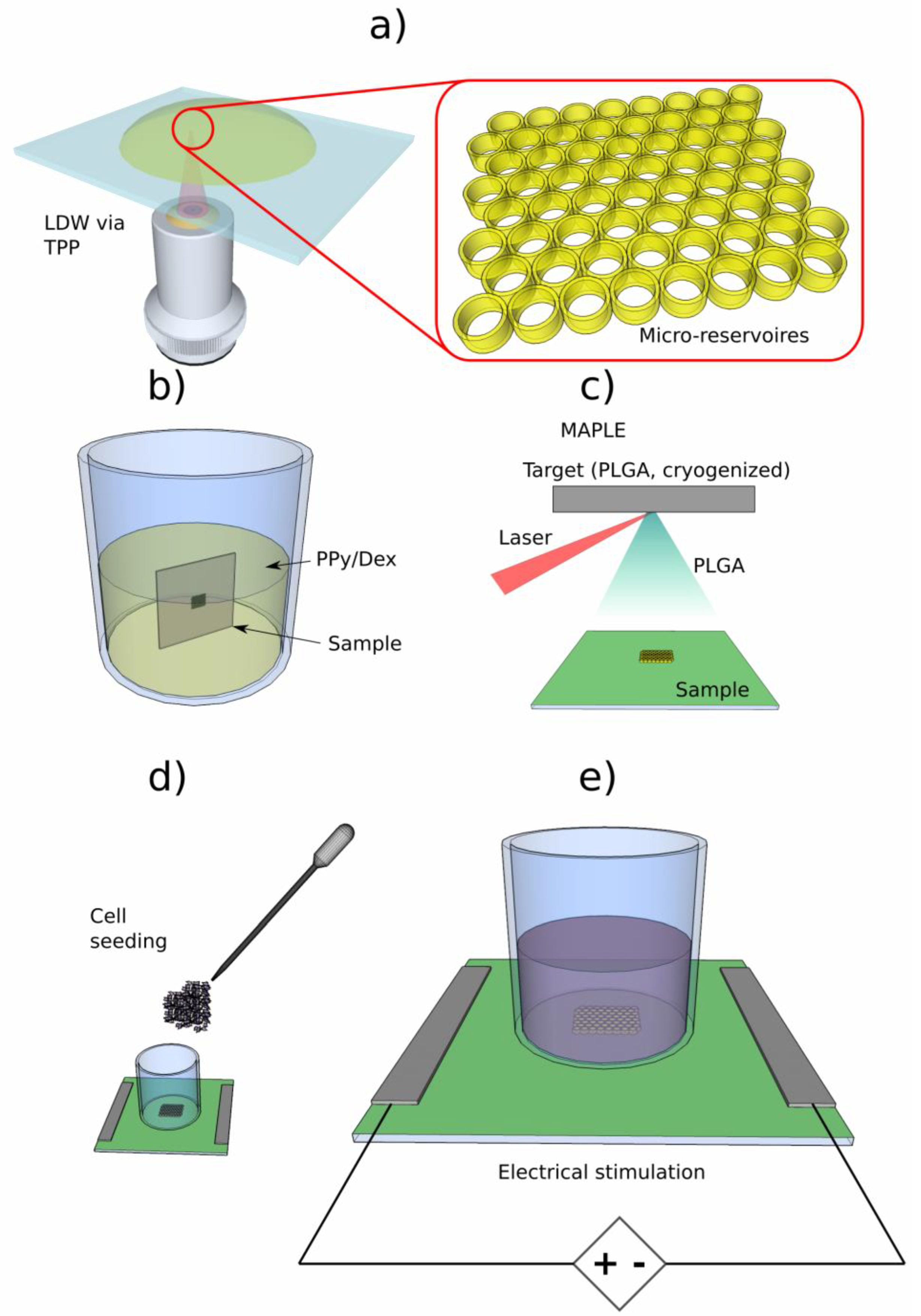
- Paun, I.A.; Zamfirescu, M.; Luculescu, C.R.; Acasandrei, A.M.; Mustaciosu, C.C.; Mihailescu, M.; Dinescu, M. Electrically responsive microreservoires for controllable delivery of dexamethasone in bone tissue engineering. Appl. Surf. Sci. 2017, 392, 321–331. [Google Scholar] [CrossRef]
- Schäfer, R.; Bantleon, R.; Kehlbach, R.; Siegel, G.; Wiskirchen, J.; Wolburg, H.; Kluba, T.; Eibofner, F.; Northoff, H.; Claussen, C.D.; et al. Functional investigations on human mesenchymal stem cells exposed to magnetic fields and labeled with clinically approved iron nanoparticles. BMC Cell Biol. 2010, 11, 22. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.-C.; Leesungbok, R.; Lee, S.-W.; Lee, H.-W.; Park, S.H.; Mah, S.-J.; Ahn, S.-J. Effects of moderate intensity static magnetic fields on human bone marrow-derived mesenchymal stem cells. Bioelectromagnetics 2015, 36, 267–276. [Google Scholar] [CrossRef]
- Dvir, T.; Timko, B.P.; Kohane, D.S.; Langer, R. Nanotechnological strategies for engineering complex tissues. Nat. Nanotechnol. 2011, 6, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Webster, T.J. Nanotechnology and nanomaterials: Promises for improved tissue regeneration. Nano Today 2009, 4, 66–80. [Google Scholar] [CrossRef]
- Aubin, J.; Liu, F.; Malaval, L.; Gupta, A. Osteoblast and chondroblast differentiation. Bone 1995, 17, S77–S83. [Google Scholar] [CrossRef]
- Zhang, J.; Ding, C.; Ren, L.; Zhou, Y.; Shang, P. The effects of static magnetic fields on bone. Prog. Biophys. Mol. Biol. 2014, 114, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Panseri, S.; Russo, A.; Giavaresi, G.; Sartori, M.; Veronesi, F.; Fini, M.; Salter, D.M.; Ortolani, A.; Strazzari, A.; Visani, A.; et al. Inovative magnetic scaffolds for orthopedic tissue engineering. J. Biomed. Mater. Res. 2012, 100, 2278–2286. [Google Scholar]
- Zablotskii, V.; Polyakova, T.; Lunov, O.; Dejneka, A. How a High-Gradient Magnetic Field Could Affect Cell Life. Sci. Rep. 2016, 6, 37407. [Google Scholar] [CrossRef] [Green Version]
- Zablotskii, V.; Dejneka, A.; Kubinová, Š.; Le-Roy, D.; Dumas-Bouchiat, F.; Givord, D.; Dempsey, N.M.; Syková, E. Life on Magnets: Stem Cell Networking on Micro-Magnet Arrays. PLoS ONE 2013, 8, e70416. [Google Scholar] [CrossRef] [Green Version]
- Yun, H.-M.; Ahn, S.-J.; Park, K.-R.; Kim, M.-J.; Kim, J.-J.; Jin, G.-Z.; Kim, H.-W.; Kim, E.-C. Magnetic nanocomposite scaffolds combined with static magnetic field in the stimulation of osteoblastic differentiation and bone formation. Biomaterials 2016, 85, 88–98. [Google Scholar] [CrossRef]
- Zhao, Y.; Fan, T.; Chen, J.; Su, J.; Zhi, X.; Pan, P.; Zou, L.; Zhang, Q. Magnetic bioinspired micro/nanostructured composite scaffold for bone regeneration. Colloids Surfaces B Biointerfaces 2019, 174, 70–79. [Google Scholar] [CrossRef]
- Huang, J.; Wang, D.; Chen, J.; Liu, W.; Duan, L.; You, W.; Xiong, J.; Wang, D. Osteogenic differentiation of bone marrow mesenchymal stem cells by magnetic nanoparticle composite scaffolds under a pulsed electromagnetic field. Saudi Pharm. J. 2017, 25, 575–579. [Google Scholar] [CrossRef]
- Mazidi, Z.; Javanmardi, S.; Naghib, S.M.; Mohammadpour, Z. Smart stimuli-responsive implantable drug delivery systems for programmed and on-demand cancer treatment: An overview on emerging materials. Chem. Eng. J. 2022, 433, 134569. [Google Scholar] [CrossRef]
- Sedghi, R.; Ashrafzadeh, S.; Heidari, B. pH-sensitive molecularly imprinted polymer based on grapheme oxide for stimuli actuated controlled release of curcumin. J. Alloys Compd. 2021, 857, 157603. [Google Scholar] [CrossRef]
- Lim, A.E.; Lam, Y.C. Numerical investigation of nanostructure orientation on electroosmotic flow. Micromachines 2020, 11, 971. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.E.; Lam, Y.C. Electroosmotic Flow Hysteresis for Fluids with Dissimilar pH and Ionic Species. Micromachines 2021, 12, 1031. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Ma, X.; Gou, M.; Mei, D.; Zhang, K.; Chen, S. 3D printing of functional biomaterials for tissue engineering. Curr. Opin. Biotechnol. 2016, 40, 103–112. [Google Scholar] [CrossRef] [Green Version]
- Wu, P.K.; Ringeisen, B.R.; Krizman, D.B.; Frondoza, C.G.; Brooks, M.; Bubb, D.M.; Auyeung, R.C.Y.; Pique, A.; Spargo, B.; McGill, R.A.; et al. Laser transfer of biomaterials: Matrix-assisted pulsed laser evaporation (MAPLE) and MAPLE Direct Write. Rev. Sci. Instrum. 2003, 74, 2546–2557. [Google Scholar] [CrossRef]
- Schwodiauer, R.; Gogonea, S.B.; Bauer, S.; Heitz, J.; Arenholz, E.; Bauerle, D. Pyroelectricity in Polycrystalline Ferroelectrics. Appl. Phys. Lett. 1998, 73, 2941. [Google Scholar]
- Chrisey, D.B.; PiquØ, A.; McGill, R.A.; Horwitz, J.S.; Ringeisen, B.R.; Bubb, D.M.; Wu, P.K. Laser deposition of polymer and biomaterial films. Chem. Rev. 2003, 103, 553. [Google Scholar] [CrossRef]
- Stamatin, L.; Cristescu, R.; Socol, G.; Moldovan, A.; Mihaiescu, D.; Stamatin, I.; Mihailescu, I.N.; Chrisey, D.B. Laser deposition of fibrinogen blood proteins thin films by matrix assisted pulsed laser evaporation. Appl. Surf. Sci. 2005, 248, 422. [Google Scholar] [CrossRef]
- Cristescu, R.; Mihaiescu, D.; Socol, G.; Stamatin, I.; Mihailescu, I.N.; Chrisey, D.B. Deposition of biopolymer thin films by matrix assisted pulsed laser evaporation. Appl. Phys. A 2004, 79, 1023. [Google Scholar] [CrossRef]
- Ringeisen, B.R.; Callahan, J.; Wu, P.K.; PiquØ, A.; Spargo, B.; McGill, R.A.; Bucaro, M.; Kim, H.; Bubb, D.M.; Chrisey, D.B. Novel Laser-Based Deposition of Active Protein Thin Films. Langmuir 2001, 17, 3472. [Google Scholar] [CrossRef]
- Khan, T.T.; Sreerunothai, P.; Hert, L.M.; Banach, M.J.; Kohler, A. Morphology-dependent energy transfer within polyfluorene thin films. Phys. Rev. B 2004, 69, 085201. [Google Scholar] [CrossRef]
- Grigorescu, S.; Carradò, A.; Ulhaq, C.; Faerber, J.; Ristoscu, C.; Dorcioman, G.; Axente, E.; Werckmann, J.; Mihailescu, I.N. Study of the gradual interface between hydroxyapatite thin films PLD grown onto Ti-controlled sublayers. Appl. Surf. Sci. 2007, 254, 1150. [Google Scholar] [CrossRef]
- Do, A.-V.; Smith, R.; Acri, T.M.; Geary, S.M.; Salem, A.K. 3D printing technologies for 3D scaffolds engineering. In Functional 3D Tissue Engineering Scaffolds. Materials, Technologies and Applications; Deng, Y., Kuiper, J., Eds.; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar] [CrossRef]
- Yusupov, V.; Churbanov, S.; Churbanova, E.; Bardakova, K.; Antoshin, A.; Evlashin, S.; Timashev, P.; Minaev, N. Laser-induced Forward Transfer Hydrogel Printing: A Defined Route for Highly Controlled Process. Int. J. Bioprint. 2020, 6, 271. [Google Scholar] [CrossRef]
- Cristescu, R.; Negut, I.; Visan, A.I.; Nguyen, A.K.; Sachan, A.; Goering, P.L.; Chrisey, D.B.; Narayan, R.J. Matrix-Assisted Pulsed laser Evaporation-deposited Rapamycin Thin Films Maintain Antiproliferative Activity. Int. J. Bioprint. 2020, 6, 188, Erratum in Int. J. Bioprint. 2020, 6, 309. [Google Scholar] [CrossRef]
- Serra, P.; Piqué, A. Laser-Induced Forward Transfer: Fundamentals and Applications. Adv. Mater. Technol. 2019, 4, 1800099. [Google Scholar] [CrossRef] [Green Version]
- Guillemot, F.; Souquet, A.; Catros, S.; Guillotin, B. Laser-assisted cell printing: Principle, physical parameters versus cell fate and perspectives in tissue engineering. Nanomedicine 2010, 5, 507–515, Erratum in Nanomedicine 2010, 5, 831–832. [Google Scholar] [CrossRef]
- Barron, J.; Spargo, B.; Ringeisen, B. Biological laser printing of three dimensional cellular structures. Appl. Phys. A 2004, 79, 1027–1030. [Google Scholar] [CrossRef]
- Kim, K.; Yeatts, A.; Dean, D.; Fisher, J.P. Stereolithographic Bone Scaffold Design Parameters: Osteogenic Differentiation and Signal Expression. Tissue Eng. Part B Rev. 2010, 16, 523–539. [Google Scholar] [CrossRef] [Green Version]
- Derakhshanfar, S.; Mbeleck, R.; Xu, K.; Zhang, X.; Zhong, W.; Xing, M. 3D bioprinting for biomedical devices and tissue engineering: A review of recent trends and advances. Bioact. Mater. 2018, 3, 2. [Google Scholar] [CrossRef]
- Pan, Y.-Q.; Zheng, R.; Liu, F.-B.; Jing, W.; Yong, C.; Liang, X.-Y.; Bing, W. The use of CT scan and stereo lithography apparatus technologies in a canine individualized rib prosthesis. Int. J. Surg. 2014, 12, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Melchels, F.P.W.; Feijen, J.; Grijpma, D.W. A review on stereolithography and its applications in biomedical engineering. Biomaterials 2010, 31, 6121–6130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skoog, S.A.; Goering, P.L.; Narayan, R.J. Stereolithography in tissue engineering. J. Mater. Sci. Mater. Med. 2014, 25, 845–856. [Google Scholar] [CrossRef] [PubMed]
- Brandi, F.; Anjum, F.; Ceseracciu, L.; Barone, A.C.; Athanassiou, A. Rigid biodegradable photopolymer structures of high resolution using deep-UV laser photocuring. J. Micromech. Microeng. 2011, 21, 054007. [Google Scholar] [CrossRef]
- Rad, Z.F.; Prewett, P.D.; Davies, G.J. High-resolution two-photon polymerization: The most versatile technique for the fabrication of microneedle arrays. Microsyst. Nanoeng. 2021, 7, 71. [Google Scholar] [CrossRef]
- Hribar, K.C.; Soman, P.; Warner, J.; Chung, P.; Chen, S. Light-assisted direct-write of 3D functional biomaterials. Lab Chip 2013, 14, 268–275. [Google Scholar] [CrossRef] [Green Version]
- Huang, Z.; Tsui, G.C.-P.; Deng, Y.; Tang, C.-Y. Two-photon polymerization nanolithography technology for fabrication of stimulus-responsive micro/nano-structures for biomedical applications. Nanotechnol. Rev. 2020, 9, 1118–1136. [Google Scholar] [CrossRef]
- Do, A.-V.; Worthington, K.; Tucker, B.; Salem, A.K. Controlled drug delivery from 3D printed two-photon polymerized poly(ethylene glycol) dimethacrylate devices. Int. J. Pharm. 2018, 552, 217–224. [Google Scholar] [CrossRef]
- Kurselis, K.; Kiyan, R.; Bagratashvili, V.N.; Popov, V.K.; Chichkov, B.N. 3D fabrication of all-polymer conductive microstructures by two photon polymerization. Opt. Express 2013, 21, 31029–31035. [Google Scholar] [CrossRef]
- Wang, C.; Hu, Z.; Yang, L.; Zhang, C.; Zhang, L.; Ji, S.; Xu, L.; Li, J.; Hu, Y.; Wu, D.; et al. Magnetically driven rotary microfilter fabricated by two-photon polymerization for multimode filtering of particles. Opt. Lett. 2021, 46, 2968–2971. [Google Scholar] [CrossRef]
- Dong, M.; Wang, X.; Chen, X.; Mushtaq, F.; Deng, S.; Zhu, C.; Torlakcik, H.; Terzopoulou, A.; Qin, X.; Xiao, X.; et al. Micro/nanoscale magnetic robots for biomedical applications. Adv. Funct. Mater. 2020, 30, 1910323. [Google Scholar] [CrossRef]
- Giltinan, J.; Katsamba, P.; Wang, W.; Lauga, E.; Sitti, M. Selectively controlled magnetic microrobots with opposing helices. Appl. Phys. Lett. 2020, 116, 134101. [Google Scholar] [CrossRef]
- Li, B.; Gil, B.; Power, M.; Gao, A.; Treratanakulchai, S.; Anastasova, S.; Yang, G.-Z. Carbon-Nanotube-Coated 3D Microspring Force Sensor for Medical Applications. ACS Appl. Mater. Interfaces 2019, 11, 35577. [Google Scholar] [CrossRef]
- Xia, X.; Afshar, A.; Yang, H.; Portela, C.M.; Kochmann, D.M.; di Leo, C.V.; Greer, J.R. Electrochemically reconfigurable architected materials. Nature 2019, 573, 205. [Google Scholar] [CrossRef] [PubMed]
- Tottori, S.; Zhang, L.; Qiu, F.; Krawczyk, K.K.; Franco-Obregón, A.; Nelson, B.J. Micromachines: Magnetic Helical Micromachines: Fabrication, Controlled Swimming, and Cargo Transport. Adv. Mater. 2012, 24, 811. [Google Scholar] [CrossRef]
- Park, J.; Jin, C.; Lee, S.; Kim, J.-Y.; Choi, H. Magnetically Actuated Degradable Microrobots for Actively Controlled Drug Release and Hyperthermia Therapy. Adv. Healthc. Mater. 2019, 8, 1900213. [Google Scholar] [CrossRef]
- Yamanaka, T.; Arai, F. Miniaturization effect of electroosmotic self-propulsive microswimmer powered by biofuel cell. Robomech. J. 2019, 6, 22. [Google Scholar] [CrossRef]
- Soreni-Harari, M.; Pierre, R.S.; McCue, C.; Moreno, K.; Bergbreiter, S. Multimaterial 3D Printing for Microrobotic Mechanisms. Soft Robot. 2019, 7, 59. [Google Scholar] [CrossRef]
- Bakhtina, N.A.; Loeffelmann, U.; MacKinnon, N.; Korvink, J.G. Two-Photon Nanolithography Enhances the Performance of an Ionic Liquid-Polymer Composite Sensor. Adv. Funct. Mater. 2015, 25, 1682. [Google Scholar] [CrossRef]
- Bunea, A.-I.; Iniesta, N.D.C.; Droumpali, A.; Wetzel, A.E.; Engay, E.; Taboryski, R. Micro 3D Printing by Two-Photon Polymerization: Configurations and Parameters for the Nanoscribe System. Micro 2021, 1, 164–180. [Google Scholar] [CrossRef]
- Otuka, A.; Tomazio, N.; Paula, K.; Mendonça, C. Two-Photon Polymerization: Functionalized Microstructures, Micro-Resonators, and Bio-Scaffolds. Polymers 2021, 13, 1994. [Google Scholar] [CrossRef] [PubMed]
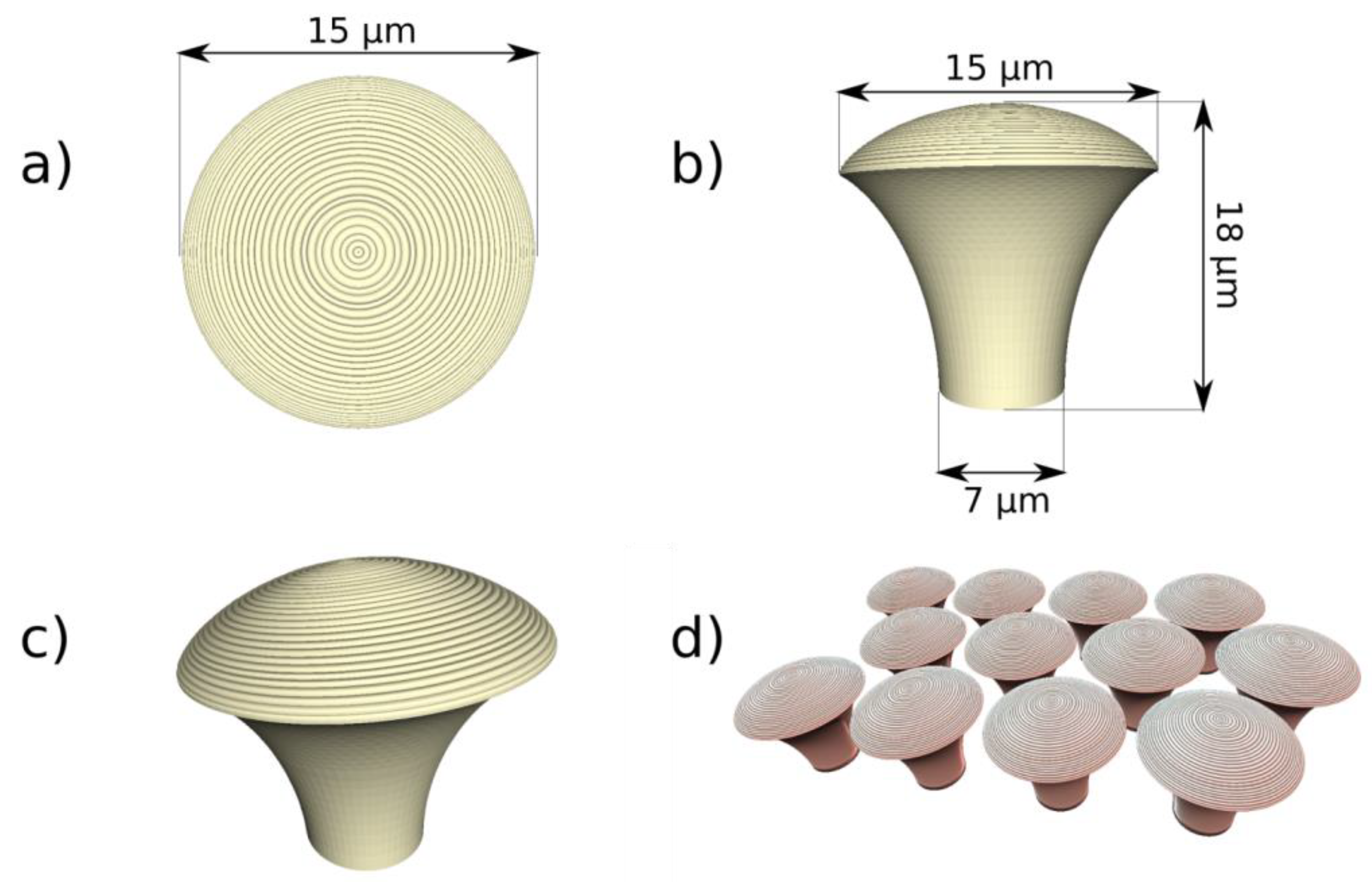
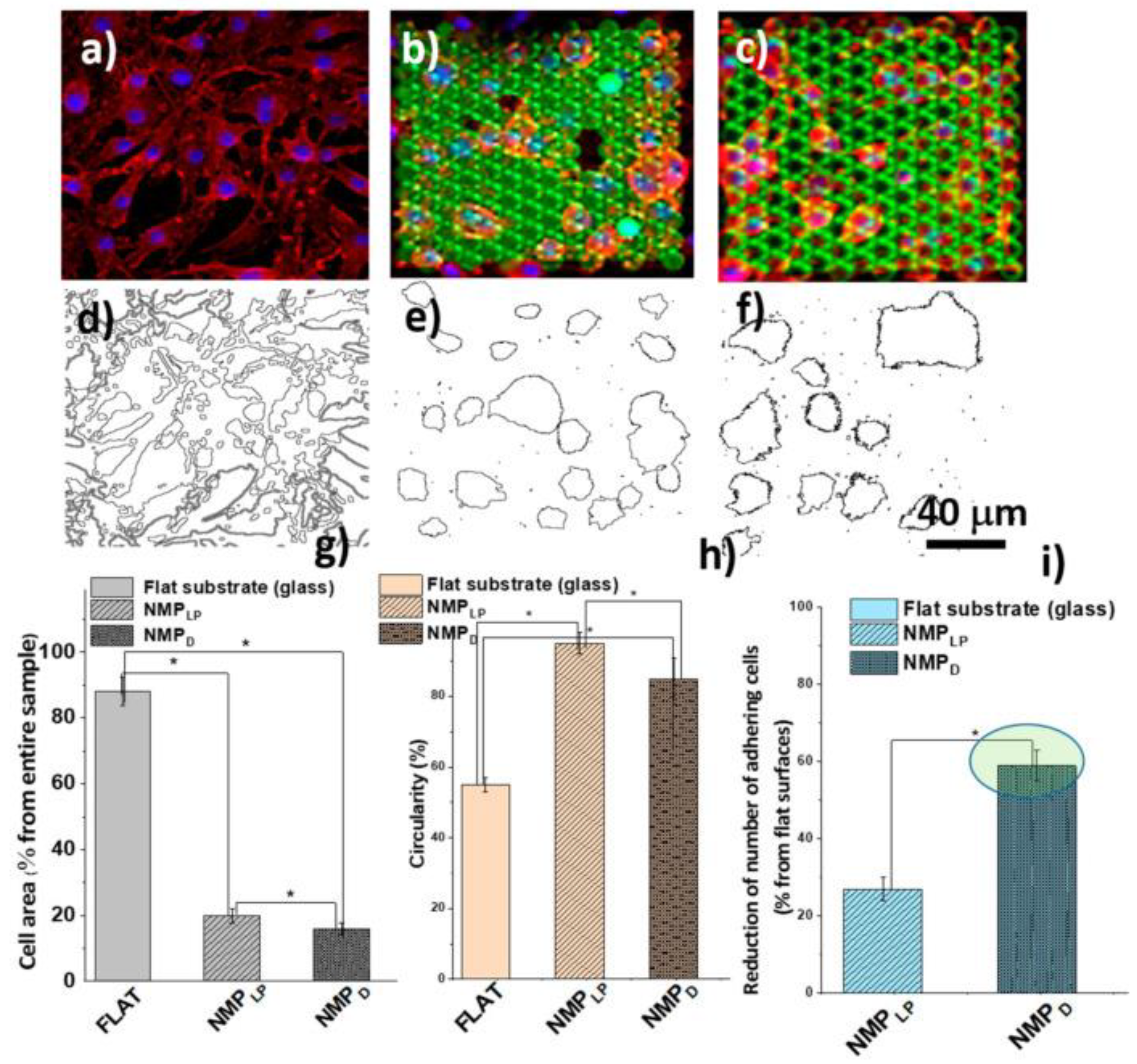
- Paun, I.; Calin, B.; Mustaciosu, C.; Tanasa, E.; Moldovan, A.; Niemczyk, A.; Dinescu, M. Laser Direct Writing via Two-Photon Polymerization of 3D Hierarchical Structures with Cells-Antiadhesive Properties. Int. J. Mol. Sci. 2021, 22, 5653. [Google Scholar] [CrossRef]
- Peidaee, P.; Almansour, N.; Shukla, R.; Pirogova, E. The cytotoxic effects of low intensity visible and infrared light on human breast cancer (mcf7) cells. Comput. Struct. Biotechnol. J. 2013, 6, e201303015. [Google Scholar] [CrossRef] [Green Version]
- Bassen, H.; Czerski, P.; Monahan, J. Biological effects of electromagnetic radiation. IEEE Antennas Propag. Soc. Newsl. 1984, 26, 17–19. [Google Scholar] [CrossRef]
- Eells, J.T.; Wong-Riley, M.T.; VerHoeve, J.; Henry, M.; Buchman, E.V.; Kane, M.P.; Gould, L.J.; Das, R.; Jett, M.; Hodgson, B.D.; et al. Mitochondrial signal transduction in accelerated wound and retinal healing by near-infrared light therapy. Mitochondrion 2004, 4, 559–567. [Google Scholar] [CrossRef]
- Lourenço, B.N.; Marchioli, G.; Song, W.; Reis, R.L.; van Blitterswijk, C.A.; Karperien, M.; van Apeldoorn, A.; Mano, J.F. Wettability Influences Cell Behavior on Superhydrophobic Surfaces with Different Topographies. Biointerphases 2012, 7, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denchai, A.; Tartarini, D.; Mele, E. Cellular Response to Surface Morphology: Electrospinning and Computational Modeling. Front. Bioeng. Biotechnol. 2018, 6, 155. [Google Scholar] [CrossRef] [Green Version]
- Kamath, S.; Bhattacharyya, D.; Padukudru, C.; Timmons, R.B.; Tang, L. Surface chemistry influences implant-mediated host tissue responses. J. Biomed. Mater. Res. Part A 2008, 86A, 617–626. [Google Scholar] [CrossRef] [Green Version]
- Vazquez, K.; Saraswathibhatla, A.; Notbohm, J. Effect of substrate stiffness on friction in collective cell migration. Sci. Rep. 2022, 12, 2474. [Google Scholar] [CrossRef]
- Majhy, B.; Priyadarshini, P.; Sen, A.K. Effect of surface energy and roughness on cell adhesion and growth—Facile surface modification for enhanced cell culture. RSC Adv. 2021, 11, 15467–15476. [Google Scholar] [CrossRef]
- Paun, I.A.; Calin, B.S.; Popescu, R.C.; Tanasa, E.; Moldovan, A. Laser Direct Writing of Dual-Scale 3D Structures for Cell Repelling at High Cellular Density. Int. J. Mol. Sci. 2022, 23, 3247. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Connell, S.; Shi, R. Biomimetic Architectures for Tissue Engineering. In Biomimetics Learning from Nature; IntechOpen: London, UK, 2010. [Google Scholar] [CrossRef] [Green Version]
- Ock, G.; Li, W. Fabrication of a three-dimensional tissue model microarray using laser foaming of a gas-impregnated biodegradable polymer. Biofabrication 2014, 6, 024110. [Google Scholar] [CrossRef] [PubMed]
- Zieber, L.; Or, S.; Ruvinov ECohen, S. Microfabrication of channel arrays promotes vessel-like network formation in cardiac cell construct and vascularization in vivo. Biofabrication 2014, 6, 024102. [Google Scholar] [CrossRef] [PubMed]
- Bian, W.; Jackman, C.P.; Bursac, N. Controlling structural and functional anisotropy of engineering cardiac tissues. Biofabrication 2014, 6, 024109. [Google Scholar] [CrossRef]
- Senevirathne, S.W.M.A.I.; Hasan, J.; Mathew, A.; Woodruff, M.; Yarlagadda, P.K.D.V. Bactericidal efficiency of micro- and nanostructured surfaces: A critical perspective. RSC Adv. 2021, 11, 1883–1900. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Lei, Z.; Chen, Y.; Chen, C.; Zhang, R.; Chen, X.; Bi, J.; Sun, H. Inhibition Effectiveness of Laser-Cleaned Nanostructured Aluminum Alloys to Sulfate-reducing Bacteria Based on Superwetting and Ultraslippery Surfaces. ACS Appl. Bio. Mater. 2020, 3, 6131–6144. [Google Scholar] [CrossRef]
- Joya, Y.F.; Wang, T.; Liu, Z. Formation and antibacterial activities of nanostructured TiO2 based thin films by sol-gel/laser-induced technique. ICALEO 2011, 2011, 1152–1160. [Google Scholar] [CrossRef]
- Loh, Q.L.; Choong, C. Three-Dimensional Scaffolds for Tissue Engineering Applications: Role of Porosity and Pore Size. Tissue Eng. Part B Rev. 2013, 19, 485–502. [Google Scholar] [CrossRef] [Green Version]
- Ma, T.; Li, Y.; Yang, S.-T.; Kniss, D.A. Effects of pore size in 3-D fibrous matrix on human trophoblast tissue development. Biotechnol. Bioeng. 2000, 70, 606–618. [Google Scholar] [CrossRef]
- Mandal, B.B.; Kundu, S.C. Cell proliferation and migration in silk fibroin 3D scaffolds. Biomaterials 2009, 30, 2956–2965. [Google Scholar] [CrossRef]
- Mata, A.; Kim, E.J.; Boehm, C.A.; Fleischman, A.J.; Muschler, G.F.; Roy, S. A three-dimensional scaffold with precise micro-architecture and surface micro-textures. Biomaterials 2009, 30, 4610–4617. [Google Scholar] [CrossRef] [Green Version]
- Mohanty, S.; Larsen, L.B.; Trifol, J.; Szabo, P.; Burri, H.V.R.; Canali, C.; Dufva, M.; Emnéus, J.; Wolff, A. Fabrication of scalable and structured tissue engineering scaffolds using water dissolvable sacrificial 3D printed moulds. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 55, 569–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, D.; Meredith, J.C. Influence of Topography on Adhesion and Bioadhesion. In Contamination Mitigating Polymeric Coatings for Extreme Environments; Advances in Polymer Science; Springer: Berlin/Heidelberg, Germany, 2019; Volume 284, pp. 19–50. [Google Scholar]
- Yiannakou, C.; Simitzi, C.; Manousaki, A.; Fotakis, C.; Ranella, A.; Stratakis, E. Cell patterning via laser micro/nano structured silicon surfaces. Biofabrication 2017, 9, 025024. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.; Meredith, J.C. Contamination Mitigating Polymeric Coatings for Extreme Environments; Advances in Polymer Science; Wohl, C.J., Berry, D.H., Eds.; Springer: Cham, Switzerland, 2017; Volume 284. [Google Scholar]
- Du, Y.; Guo, J.L.; Wang, J.; Mikos, A.G.; Zhang, S. Hierarchically designed bone scaffolds: From internal cues to external stimuli. Biomaterials 2019, 218, 119334. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.; Koo, S.; Reese, W.M.; Loskill, P.; Grigoropoulos, C.P.; Healy, K.E. Directing cell migration and organization via nanocrater-patterned cell-repellent interfaces. Nat. Mater. 2015, 14, 918–923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinhardt, H.; Kroll, M.; Karstens, S.L.; Schlabach, S.; Hampp, N.A.; Tallarek, U. Nanoscaled Fractal Superstructures via Laser Patterning—A Versatile Route to Metallic Hierarchical Porous Materials. Adv. Mater. Interfaces 2021, 8, 2000253. [Google Scholar] [CrossRef] [Green Version]
- Paci, J.T.; Chapman, C.T.; Lee, W.-K.; Odom, T.W.; Schatz, G.C. Wrinkles in Polytetrafluoroethylene on Polystyrene: Persistence Lengths and the Effect of Nanoinclusions. ACS Appl. Mater. Interfaces 2017, 9, 9079–9088. [Google Scholar] [CrossRef]
- Gatto, M.; Groppo, R.; Bloise, N.; Fassina, L.; Visai, L.; Galati, M.; Iuliano, L.; Mengucci, P. Topological, Mechanical and Biological Properties of Ti6Al4V Scaffolds for Bone Tissue Regeneration Fabricated with Reused Powders via Electron Beam Melting. Materials 2021, 14, 224. [Google Scholar] [CrossRef]
- Sun, Y.; Wan, B.; Wang, R.; Zhang, B.; Luo, P.; Wang, D.; Nie, J.-J.; Chen, D.; Wu, X. Mechanical Stimulation on Mesenchymal Stem Cells and Surrounding Microenvironments in Bone Regeneration: Regulations and Applications. Front. Cell Dev. Biol. 2022, 10, 808303. [Google Scholar] [CrossRef]
- Hung, B.P.; Hutton, D.L.; Grayson, W.L. Mechanical control of tissue-engineered bone. Stem Cell Res. Ther. 2013, 4, 10. [Google Scholar] [CrossRef]
- Levin, M.; Spiro, R.C.; Jain, H.; Falk, M.M. Effects of Titanium Implant Surface Topology on Bone Cell Attachment and Proliferation in vitro. Med. Devices Évid. Res. 2022, 15, 103–119. [Google Scholar] [CrossRef] [PubMed]
- Mihailescu, M.; Paun, I.A.; Zamfirescu, M.; Luculescu, C.R.; Acasandrei, M.A.; Dinescu, M. Laser-assisted fabrication and non-invasive imaging of 3D cell-seeding constructs for bone tissue engineering. J. Mater. Sci. 2016, 51, 4262–4273. [Google Scholar] [CrossRef]
- Salinas, E.; Hu, J.C.; Athanasiou, K. A Guide for Using Mechanical Stimulation to Enhance Tissue-Engineered Articular Cartilage Properties. Tissue Eng. Part B Rev. 2018, 24, 345–358. [Google Scholar] [CrossRef]
- Jahed, Z.; Zareian, R.; Chau, Y.Y.; Seo, B.B.; West, M.; Tsui, T.Y.; Wen, W.; Mofrad, M.R.K. Differential Collective- and Single-Cell Behaviors on Silicon Micropillar Arrays. ACS Appl. Mater. Interfaces 2016, 8, 23604–23613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Wan, Y.; Liu, Y. Effects of nanopillar array diameter and spacing on cancer cell capture and cell behaviors. Nanoscale 2014, 6, 12482–12489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koch, B.; Sanchez, S.; Schmidt, C.; Swiersy, A.; Jackson, S.P.; Schmidt, O.G. Confinement and Deformation of Single Cells and Their Nuclei Inside Size-Adapted Microtubes. Adv. Healthc. Mater. 2014, 3, 1753–1758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, C.; Hanson, L.; Xie, W.; Lin, Z.; Cui, B.; Cui, Y. Noninvasive Neuron Pinning with Nanopillar Arrays. Nano Lett. 2010, 10, 4020–4024. [Google Scholar] [CrossRef] [Green Version]
- Fu, J.; Wang, Y.-K.; Yang, M.T.; Desai, R.; Yu, X.; Liu, Z.; Chen, C. Mechanical regulation of cell function with geometrically modulated elastomeric substrates. Nat. Methods 2010, 7, 733–736. [Google Scholar] [CrossRef]
- Henriks-Eckerman, M.-L.; Suuronen, K.; Jolanki, R.; Alanko, K. Methacrylates in dental restorative materials. Contact Dermat. 2004, 50, 233–237. [Google Scholar] [CrossRef]
- Huang, Y.; Onyeri, S.; Siewe, M.; Moshfeghian, A.; Madihally, S.V. In vitro characterization of chitosan–gelatin scaffolds for tissue engineering. Biomaterials 2005, 26, 36. [Google Scholar] [CrossRef]
- Noè, C.; Zanon, M.; Arencibia, A.; López-Muñoz, M.-J.; de Paz, N.F.; Calza, P.; Sangermano, M. UV-Cured Chitosan and Gelatin Hydrogels for the Removal of As(V) and Pb(II) from Water. Polymers 2022, 14, 1268. [Google Scholar] [CrossRef] [PubMed]
- Mano, J.F.; Silva, G.A.; Azevedo, H.S.; Malafaya, P.B.; Sousa, R.A.; Silva, S.S.; Boesel, L.F.; Oliveira, J.M.; Santos, T.C.; Marques, A.P.; et al. Natural origin biodegradable systems in tissue engineering and regenerative medicine: Present status and some moving trends. J. R. Soc. Interface 2007, 4, 999–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Guo, Q.; Cai, X.; Zhou, S.; Kobe, B.; Yang, J. Initiator-Integrated 3D Printing Enables the Formation of Complex Metallic Architectures. ACS Appl. Mater. Interfaces 2014, 6, 2583–2587. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, C.B.; Bell, E. A blood vessel model constructed from collagen and cultured vascular cells. Science 1986, 231, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.T.; McCanless, J.D.; Mecwan, M.M.; Noblett, A.P.; Haggard, W.O.; Smith, R.A.; Bumgardner, J.D. Balancing mechanical strength with bioactivity in chitosan-calcium phosphate 3D microsphere scaffolds for bone tissue engineering: Air- vs. freeze-drying processes. J. Biomater. Sci. Polym. Ed. 2013, 24, 1071–1083. [Google Scholar] [CrossRef]
- Miller, L.L.; Smith, G.A.; Chang, A.-C.; Zhou, Q.-X. Electrochemically controlled release. J. Control. Release 1987, 6, 293–296. [Google Scholar] [CrossRef]
- Pyo, M.; Maeder, G.; Kennedy, R.T.; Reynolds, J.R. Controlled release of biological molecules from conducting polymer modified electrodes: The potential dependent release of adenosine 5′-triphosphate from poly(pyrrole adenosine 5′-triphosphate) films. J. Electroanal. Chem. 1994, 368, 329–332. [Google Scholar] [CrossRef]
- Hepel, M.; Mahdavi, F. Application of the Electrochemical Quartz Crystal Microbalance for Electrochemically Controlled Binding and Release of Chlorpromazine from Conductive Polymer Matrix. Microchem. J. 1997, 56, 54–64. [Google Scholar] [CrossRef]
- Sirivisoot, S.; Pareta, R.; Webster, T.J. Electrically controlled drug release from nanostructured polypyrrole coated on titanium. Nanotechnology 2011, 22, 085101. [Google Scholar] [CrossRef]
- Walsh, S.; Jordan, G.R.; Jefferiss, C.; Stewart, K.; Beresford, J.N. High concentrations of dexamethasone suppress the proliferation but not the differentiation or further maturation of human osteoblast precursors in vitro: Relevance to glucocorticoid-induced osteoporosis. Rheumatology 2001, 40, 74–83. [Google Scholar] [CrossRef]
- Pernaut, J.-M.; Reynolds, J.R. Use of Conducting Electroactive Polymers for Drug Delivery and Sensing of Bioactive Molecules. A Redox Chemistry Approach. J. Phys. Chem. B 2000, 104, 4080–4090. [Google Scholar] [CrossRef]
- Davey, J.M.; Ralph, S.F.; Too, C.O.; Wallace, G.G.; Partridge, A.C. Electrochemically controlled transport of metal ions across polypyrrole membranes using a flow-through cell. React. Funct. Polym. 2001, 49, 87–98. [Google Scholar] [CrossRef]
- Miller, L.L. Electrochemically Controlled Release of Drug Ions from Conducting Polymers. Mol. Cryst. Liq. Cryst. 1988, 160, 297–301. [Google Scholar] [CrossRef]
- Paun, I.A.; Calin, B.S.; Mustaciosu, C.C.; Mihailescu, M.; Moldovan, A.; Crisan, O.; Leca, A.; Luculescu, C.R. 3D Superparamagnetic Scaffolds for Bone Mineralization under Static Magnetic Field Stimulation. Materials 2019, 12, 2834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paun, I.A.; Mustaciosu, C.C.; Mihailescu, M.; Calin, B.S.; Sandu, A.M. Magnetically-driven 2D cells organization on superparamagnetic micromagnets fabricated by laser direct writing. Sci. Rep. 2020, 10, 16418. [Google Scholar] [CrossRef]
- Meng, J.; Xiao, B.; Zhang, Y.; Liu, J.; Xue, H.; Lei, J.; Kong, H.; Huang, Y.; Jin, Z.; Gu, N.; et al. Super-paramagnetic responsive nanofibrous scaffolds under static magnetic field enhance osteogenesis for bone repair in vivo. Sci. Rep. 2013, 3, 2655. [Google Scholar] [CrossRef] [Green Version]
- Bock, N.; Riminucci, A.; Dionigi, C.; Russo, A.; Tampieri, A.; Landi, E.; Goranov, V.A.; Marcacci, M.; Dediu, V. A novel route in bone tissue engineering: Magnetic biomimetic scaffolds. Acta Biomater. 2010, 6, 786–796. [Google Scholar] [CrossRef]
- Bañobre-López, M.; Piñeiro-Redondo, Y.; De Santis, R.; Gloria, A.; Ambrosio, L.; Tampieri, A.; Dediu, V.; Rivas, J. Poly(caprolactone) based magnetic scaffolds for bone tissue engineering. J. Appl. Phys. 2011, 109, 07B313. [Google Scholar] [CrossRef]
- Gloria, A.; Russo, T.; D’Amora, U.; Zeppetelli, S.; D’Alessandro, T.; Sandri, M.; Bañobre-López, M.; Piñeiro-Redondo, Y.; Uhlarz, M.; Tampieri, A.; et al. Magnetic poly(ε-caprolactone)/iron-doped hydroxyapatite nanocomposite substrates for advanced bone tissue engineering. J. R. Soc. Interface 2013, 10, 20120833. [Google Scholar] [CrossRef]
- De Santis, R.; Gloria, A.; Russo, T.; D’Amora, U.; Zeppetelli, S.; Dionigi, C.; Sytcheva, A.; Herrmannsdörfer, T.; Dediu, V.; Ambrosio, L. A basic approach toward the development of nanocomposite magnetic scaffolds for advanced bone tissue engineering. J. Appl. Polym. Sci. 2011, 122, 3599–3605. [Google Scholar] [CrossRef]
- Tampieri, A.; Landi, E.; Valentini, F.; Sandri, M.; D’Alessandro, T.; Dediu, V.; Marcacci, M. A conceptually new type of bio-hybrid scaffold for bone regeneration. Nanotechnology 2011, 22, 015104. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Patel, K.D.; Lee, J.H.; Lee, E.-J.; Kim, J.-H.; Kim, T.-H.; Kim, H.-W. Potential of Magnetic Nanofiber Scaffolds with Mechanical and Biological Properties Applicable for Bone Regeneration. PLoS ONE 2014, 9, e91584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tampieri, A.; D’Alessandro, T.; Sandri, M.; Sprio, S.; Landi, E.; Bertinetti, L.; Panseri, S.; Pepponi, G.; Goettlicher, J.; Bañobre-López, M.; et al. Intrinsic magnetism and hyperthermia in bioactive Fe-doped hydroxyapatite. Acta Biomater. 2012, 8, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Ba, X.; Hadjiargyrou, M.; DiMasi, E.; Meng, Y.; Simon, M.; Tan, Z.; Rafailovich, M.H. The role of moderate static magnetic fields on biomineralization of osteoblasts on suflonated polystyrene films. Biomaterials 2011, 32, 7831–7838. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Wang, J.; Tian, Y.; Chen, Q.-D.; Du, X.-B.; Zhang, Y.-L.; He, Y.; Sun, H.-B. Ferrofluids for Fabrication of Remotely Controllable Micro-Nanomachines by Two-Photon Polymerization. Adv. Mater. 2010, 22, 3204–3207. [Google Scholar] [CrossRef] [PubMed]
- Zandrini, T.; Taniguchi, S.; Maruo, S. Magnetically Driven Micromachines Created by Two-Photon Microfabrication and Selective Electroless Magnetite Plating for Lab-on-a-Chip Applications. Micromachines 2017, 8, 35. [Google Scholar] [CrossRef] [Green Version]
- Williams, G.; Hunt, M.; Boehm, B.; May, A.; Taverne, M.; Ho, Y.-L.D.; Giblin, S.; Read, D.; Rarity, J.; Allenspach, R.; et al. Two-photon lithography for 3D magnetic nanostructure fabrication. Nano Res. 2018, 11, 845–854. [Google Scholar] [CrossRef]









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calin, B.S.; Paun, I.A. A Review on Stimuli-Actuated 3D Micro/Nanostructures for Tissue Engineering and the Potential of Laser-Direct Writing via Two-Photon Polymerization for Structure Fabrication. Int. J. Mol. Sci. 2022, 23, 14270. https://doi.org/10.3390/ijms232214270
Calin BS, Paun IA. A Review on Stimuli-Actuated 3D Micro/Nanostructures for Tissue Engineering and the Potential of Laser-Direct Writing via Two-Photon Polymerization for Structure Fabrication. International Journal of Molecular Sciences. 2022; 23(22):14270. https://doi.org/10.3390/ijms232214270
Chicago/Turabian StyleCalin, Bogdan Stefanita, and Irina Alexandra Paun. 2022. "A Review on Stimuli-Actuated 3D Micro/Nanostructures for Tissue Engineering and the Potential of Laser-Direct Writing via Two-Photon Polymerization for Structure Fabrication" International Journal of Molecular Sciences 23, no. 22: 14270. https://doi.org/10.3390/ijms232214270
APA StyleCalin, B. S., & Paun, I. A. (2022). A Review on Stimuli-Actuated 3D Micro/Nanostructures for Tissue Engineering and the Potential of Laser-Direct Writing via Two-Photon Polymerization for Structure Fabrication. International Journal of Molecular Sciences, 23(22), 14270. https://doi.org/10.3390/ijms232214270





