MTARC1 and HSD17B13 Variants Have Protective Effects on Non-Alcoholic Fatty Liver Disease in Patients Undergoing Bariatric Surgery
Abstract
1. Introduction
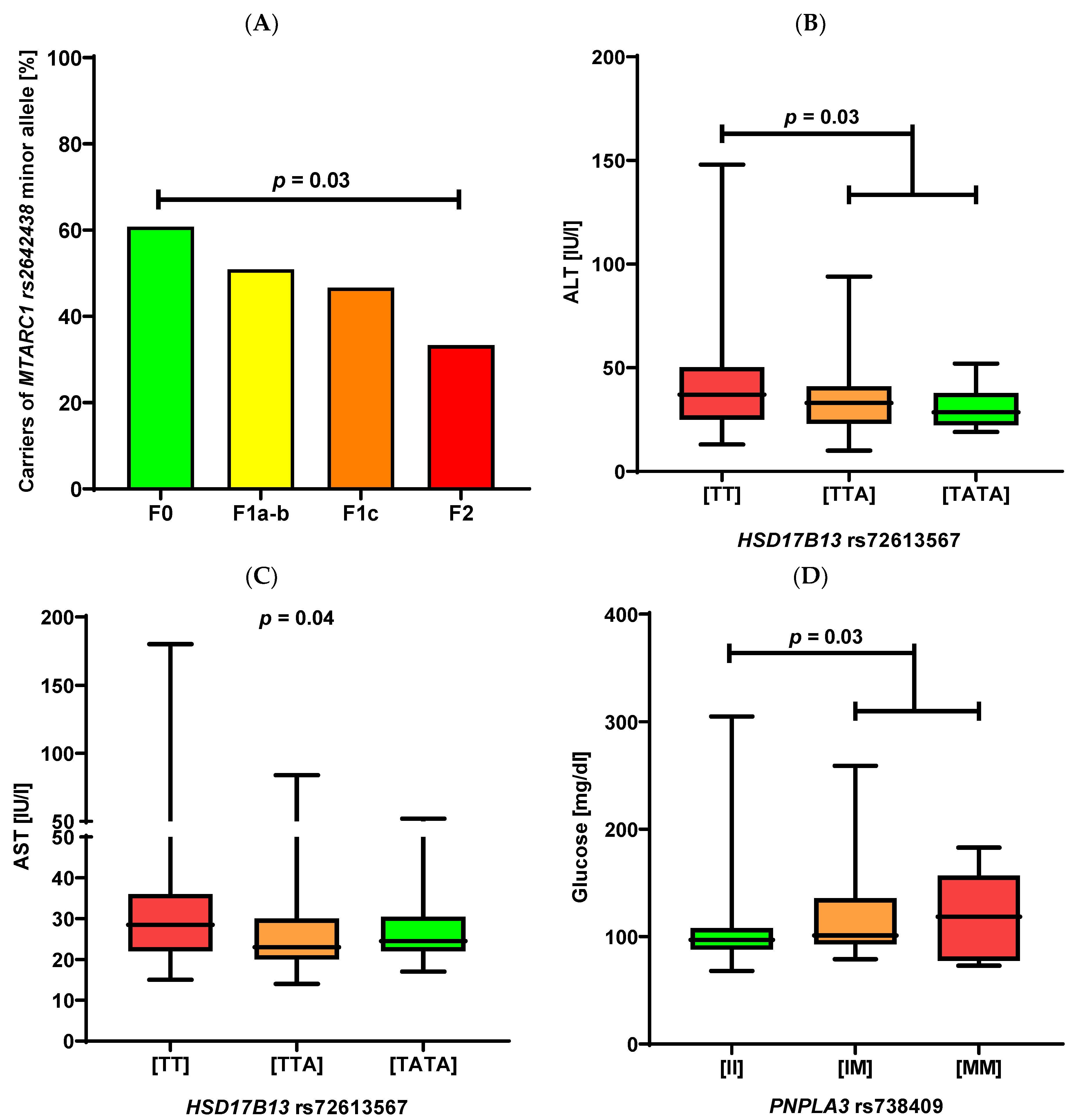
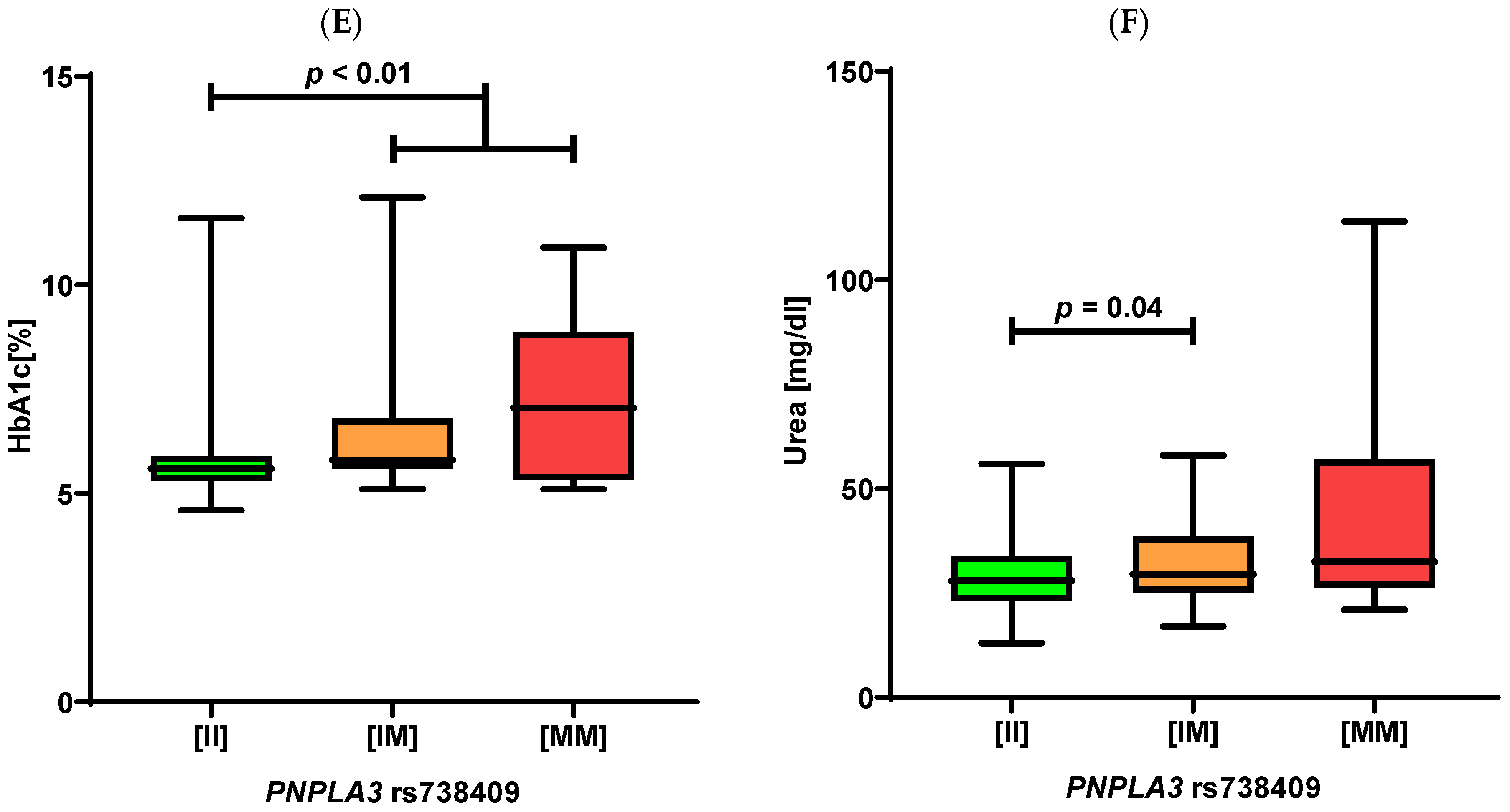
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Cohort and Clinical Data
4.2. Genotyping
4.3. Statistical Analyses
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Estes, C.; Anstee, Q.M.; Arias-Loste, M.T.; Bantel, H.; Bellentani, S.; Caballeria, J.; Colombo, M.; Craxi, A.; Crespo, J.; Day, C.P.; et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018, 69, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Sarwar, R.; Pierce, N.; Koppe, S. Obesity and nonalcoholic fatty liver disease: Current perspectives. Diabetes Metab. Syndr. Obes. Targets Ther. 2018, 11, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Lefere, S.; Onghena, L.; Vanlander, A.; van Nieuwenhove, Y.; Devisscher, L.; Geerts, A. Bariatric surgery and the liver—Mechanisms, benefits, and risks. Obes. Rev. 2021, 22, e13294. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.; Friedman, S.L.; Shulman, G.I. Mechanisms and disease consequences of nonalcoholic fatty liver disease. Cell 2021, 184, 2537–2564. [Google Scholar] [CrossRef] [PubMed]
- Krawczyk, M.; Liebe, R.; Lammert, F. Toward Genetic Prediction of Nonalcoholic Fatty Liver Disease Trajectories: PNPLA3 and Beyond. Gastroenterology 2020, 158, 1865–1880.e1861. [Google Scholar] [CrossRef]
- Dubuquoy, C.; Burnol, A.-F.; Moldes, M. PNPLA3, a genetic marker of progressive liver disease, still hiding its metabolic function? Clin. Res. Hepatol. Gastroenterol. 2013, 37, 30–35. [Google Scholar] [CrossRef]
- Kozlitina, J.; Smagris, E.; Stender, S.; Nordestgaard, B.G.; Zhou, H.H.; Tybjærg-Hansen, A.; Vogt, T.F.; Hobbs, H.H.; Cohen, J.C. Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2014, 46, 352–356. [Google Scholar] [CrossRef]
- Teo, K.; Abeysekera, K.W.; Adams, L.; Aigner, E.; Anstee, Q.M.; Banales, J.M.; Banerjee, R.; Basu, P.; Berg, T.; Bhatnagar, P.; et al. rs641738C>T near MBOAT7 is associated with liver fat, ALT and fibrosis in NAFLD: A meta-analysis. J. Hepatol. 2021, 74, 20–30. [Google Scholar] [CrossRef]
- Gijón, M.A.; Riekhof, W.R.; Zarini, S.; Murphy, R.C.; Voelker, D.R. Lysophospholipid Acyltransferases and Arachidonate Recycling in Human Neutrophils. J. Biol. Chem. 2008, 283, 30235–30245. [Google Scholar] [CrossRef]
- Li, T.-T.; Li, T.-H.; Peng, J.; He, B.; Liu, L.-S.; Wei, D.-H.; Jiang, Z.-S.; Zheng, X.-L.; Tang, Z.-H. TM6SF2: A novel target for plasma lipid regulation. Atherosclerosis 2018, 268, 170–176. [Google Scholar] [CrossRef]
- Abul-Husn, N.S.; Cheng, X.; Li, A.H.; Xin, Y.; Schurmann, C.; Stevis, P.; Liu, Y.; Kozlitina, J.; Stender, S.; Wood, G.C.; et al. A Protein-Truncating HSD17B13 Variant and Protection from Chronic Liver Disease. N. Engl. J. Med. 2018, 378, 1096–1106. [Google Scholar] [CrossRef]
- Emdin, C.A.; Haas, M.E.; Khera, A.V.; Aragam, K.; Chaffin, M.; Klarin, D.; Hindy, G.; Jiang, L.; Wei, W.-Q.; Feng, Q.; et al. A missense variant in Mitochondrial Amidoxime Reducing Component 1 gene and protection against liver disease. PLoS Genet. 2020, 16, e1008629. [Google Scholar] [CrossRef]
- Janik, M.K.; Smyk, W.; Kruk, B.; Szczepankiewicz, B.; Górnicka, B.; Lebiedzińska-Arciszewska, M.; Potes, Y.; Simões, I.C.M.; Weber, S.N.; Lammert, F.; et al. MARC1 p.A165T variant is associated with decreased markers of liver injury and enhanced antioxidant capacity in autoimmune hepatitis. Sci. Rep. 2021, 11, 24407. [Google Scholar] [CrossRef]
- Luukkonen, P.K.; Juuti, A.; Sammalkorpi, H.; Penttilä, A.K.; Orešič, M.; Hyötyläinen, T.; Arola, J.; Orho-Melander, M.; Yki-Järvinen, H. MARC1 variant rs2642438 increases hepatic phosphatidylcholines and decreases severity of non-alcoholic fatty liver disease in humans. J. Hepatol. 2020, 73, 725–726. [Google Scholar] [CrossRef]
- Innes, H.; Buch, S.; Hutchinson, S.; Guha, I.N.; Morling, J.R.; Barnes, E.; Irving, W.; Forrest, E.; Pedergnana, V.; Goldberg, D.; et al. Genome-Wide Association Study for Alcohol-Related Cirrhosis Identifies Risk Loci in MARC1 and HNRNPUL1. Gastroenterology 2020, 159, 1276–1289.e1277. [Google Scholar] [CrossRef]
- Schneider, C.V.; Schneider, K.M.; Conlon, D.M.; Park, J.; Vujkovic, M.; Zandvakili, I.; Ko, Y.-A.; Trautwein, C.; Carr, R.M.; Strnad, P.; et al. A genome-first approach to mortality and metabolic phenotypes in MTARC1 p.Ala165Thr (rs2642438) heterozygotes and homozygotes. Med 2021, 2, 851–863.e853. [Google Scholar] [CrossRef]
- Parisinos, C.A.; Wilman, H.R.; Thomas, E.L.; Kelly, M.; Nicholls, R.C.; McGonigle, J.; Neubauer, S.; Hingorani, A.D.; Patel, R.S.; Hemingway, H.; et al. Genome-wide and Mendelian randomisation studies of liver MRI yield insights into the pathogenesis of steatohepatitis. J. Hepatol. 2020, 73, 241–251. [Google Scholar] [CrossRef]
- Sveinbjornsson, G.; Ulfarsson, M.O.; Thorolfsdottir, R.B.; Jonsson, B.A.; Einarsson, E.; Gunnlaugsson, G.; Rognvaldsson, S.; Arnar, D.O.; Baldvinsson, M.; Bjarnason, R.G.; et al. Multiomics study of nonalcoholic fatty liver disease. Nat. Genet. 2022, 54, 1652–1663. [Google Scholar] [CrossRef]
- Gruenewald, S.; Wahl, B.; Bittner, F.; Hungeling, H.; Kanzow, S.; Kotthaus, J.; Schwering, U.; Mendel, R.R.; Clement, B. The Fourth Molybdenum Containing Enzyme mARC: Cloning and Involvement in the Activation of N-Hydroxylated Prodrugs. J. Med. Chem. 2008, 51, 8173–8177. [Google Scholar] [CrossRef]
- Kotthaus, J.; Wahl, B.; Havemeyer, A.; Kotthaus, J.; Schade, D.; Garbe-Schönberg, D.; Mendel, R.; Bittner, F.; Clement, B. Reduction of Nω-hydroxy-L-arginine by the mitochondrial amidoxime reducing component (mARC). Biochem. J. 2011, 433, 383–391. [Google Scholar] [CrossRef]
- Ma, Y.; Belyaeva, O.V.; Brown, P.M.; Fujita, K.; Valles, K.; Karki, S.; De Boer, Y.S.; Koh, C.; Chen, Y.; Du, X.; et al. 17-Beta Hydroxysteroid Dehydrogenase 13 Is a Hepatic Retinol Dehydrogenase Associated With Histological Features of Nonalcoholic Fatty Liver Disease. Hepatology 2019, 69, 1504–1519. [Google Scholar] [CrossRef] [PubMed]
- Gao, C.; Marcketta, A.; Backman, J.D.; O’Dushlaine, C.; Staples, J.; Ferreira, M.A.R.; Lotta, L.A.; Overton, J.D.; Reid, J.G.; Mirshahi, T.; et al. Genome-wide association analysis of serum alanine and aspartate aminotransferase, and the modifying effects of BMI in 388k European individuals. Genet. Epidemiol. 2021, 45, 664–681. [Google Scholar] [CrossRef] [PubMed]
- Anstee, Q.M.; Darlay, R.; Cockell, S.; Meroni, M.; Govaere, O.; Tiniakos, D.; Burt, A.D.; Bedossa, P.; Palmer, J.; Liu, Y.-L.; et al. Genome-wide association study of non-alcoholic fatty liver and steatohepatitis in a histologically characterised cohort. J. Hepatol. 2020, 73, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Romeo, S.; Kozlitina, J.; Xing, C.; Pertsemlidis, A.; Cox, D.; Pennacchio, L.A.; Boerwinkle, E.; Cohen, J.C.; Hobbs, H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008, 40, 1461–1465. [Google Scholar] [CrossRef] [PubMed]
- Namjou, B.; Lingren, T.; Huang, Y.; Parameswaran, S.; Cobb1, B.L.; Stanaway, I.B.; Connolly, J.J.; Mentch, F.D.; Benoit, B.; Niu, X.; et al. GWAS and enrichment analyses of non-alcoholic fatty liver disease identify new trait-associated genes and pathways across eMERGE Network. BMC Med. 2019, 17, 135. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, B.; Lindén, D.; Brolén, G.; Liljeblad, M.; Bjursell, M.; Romeo, S.; Loomba, R. Review article: The emerging role of genetics in precision medicine for patients with non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2020, 51, 1305–1320. [Google Scholar] [CrossRef]
- Zechner, R.; Zimmermann, R.; Eichmann, T.O.; Kohlwein, S.D.; Haemmerle, G.; Lass, A.; Madeo, F. FAT SIGNALS—Lipases and Lipolysis in Lipid Metabolism and Signaling. Cell Metab. 2012, 15, 279–291. [Google Scholar] [CrossRef]
- Pirazzi, C.; Valenti, L.; Motta, B.M.; Pingitore, P.; Hedfalk, K.; Mancina, R.M.; Burza, M.A.; Indiveri, C.; Ferro, Y.; Montalcini, T.; et al. PNPLA3 has retinyl-palmitate lipase activity in human hepatic stellate cells. Hum. Mol. Genet. 2014, 23, 4077–4085. [Google Scholar] [CrossRef]
- Krawczyk, M.; Rau, M.; Schattenberg, J.M.; Bantel, H.; Pathil, A.; Demir, M.; Kluwe, J.; Boettler, T.; Lammert, F.; Geier, A. Combined effects of the PNPLA3 rs738409, TM6SF2 rs58542926, and MBOAT7 rs641738 variants on NAFLD severity: A multicenter biopsy-based study. J. Lipid Res. 2017, 58, 247–255. [Google Scholar] [CrossRef]
- Krawczyk, M.; Stachowska, E.; Milkiewicz, P.; Lammert, F.; Milkiewicz, M. Reduction of Caloric Intake Might Override the Prosteatotic Effects of the PNPLA3 p.I148M and TM6SF2 p.E167K Variants in Patients with Fatty Liver: Ultrasound-Based Prospective Study. Digestion 2016, 93, 139–148. [Google Scholar] [CrossRef]
- Stender, S.; Kozlitina, J.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Hobbs, H.H.; Cohen, J.C. Adiposity amplifies the genetic risk of fatty liver disease conferred by multiple loci. Nat. Genet. 2017, 49, 842–847. [Google Scholar] [CrossRef]
- Krawczyk, M.; Jiménez-Agüero, R.; Alustiza, J.M.; Emparanza, J.I.; Perugorria, M.J.; Bujanda, L.; Lammert, F.; Banales, J.M. PNPLA3 p.I148M variant is associated with greater reduction of liver fat content after bariatric surgery. Surg. Obes. Relat. Dis. 2016, 12, 1838–1846. [Google Scholar] [CrossRef]
- Shen, J.; Wong, G.L.-H.; Chan, H.L.-Y.; Chan, R.S.; Chan, H.-Y.; Chu, W.C.; Cheung, B.H.-K.; Yeung, D.K.-W.; Li, L.S.; Sea, M.M.-M.; et al. PNPLA3 gene polymorphism and response to lifestyle modification in patients with nonalcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2015, 30, 139–146. [Google Scholar] [CrossRef]
- Delpero, M.; Arends, D.; Freiberg, A.; Brockmann, G.A.; Hesse, D. QTL-mapping in the obese Berlin Fat Mouse identifies additional candidate genes for obesity and fatty liver disease. Sci. Rep. 2022, 12, 10471. [Google Scholar] [CrossRef]
- Fried, M.; Yumuk, V.; Oppert, J.-M.; Scopinaro, N.; Torres, A.J.; Weiner, R.; Yashkov, Y.; Frühbeck, G. Interdisciplinary European Guidelines on Metabolic and Bariatric Surgery. Obes. Facts 2013, 6, 449–468. [Google Scholar] [CrossRef]
- Kleiner, D.E.; Brunt, E.M.; Van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.-C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef]
| Entire Cohort | Patients without NAFLD | Patients with NAFLD | |
|---|---|---|---|
| Total participants, n | 165 | 49 (29.7%) | 116 (70.3%) |
| Female, n [%] | 110 (66.7%) | 39 (79.6%) | 71 (61.2%) |
| Age [years] | 42 (19–65) | 39 (19–63) | 42 (21–65) |
| BMI [kg/m2] | 43.8 (34.2–64.3) | 43.8 (34.2–56.0) | 43.7 (34.3–64.3) |
| Hypertension | 107 (64.8%) | 25 (51.0%) | 82 (70.7%) |
| Type 2 diabetes mellitus | 48 (29.1%) | 4 (8.2%) | 44 (37.9%) |
| Hyperlipidaemia | 109 (66.1%) | 23 (46.9%) | 86 (74.1%) |
| Haemoglobin [g/dL] | 14.1 (10.2–18.3) | 13.6 (10.2–18.3) | 14.2 (10.6–18.0) |
| Platelets [G/L] | 258.0 (122.0–426.0) | 266.0 (122.0–426.0) | 253.0 (131.0–425.0) |
| Creatinine [mg/dL] | 0.8 (0.5–3.6) | 0.8 (0.6–3.6) | 0.8 (0.5–2.1) |
| Urea [mg/dL] | 29.0 (13.0–114.0) | 28.0 (13.0–114.0) | 29.0 (14.0–58.0) |
| ALT [IU/L] | 34.0 (10.0–148.0) | 25.0 (13.0–94.0) | 38.0 (10.0–148.0) |
| AST [IU/L] | 26.0 (14.0–180.0) | 22.0 (15.0–108.0) | 29.0 (14.0–180.0) |
| ALP [IU/L] | 72.0 (25.0–133.0) | 73.0 (40.0–116.0) | 71.0 (25.0–133.0) |
| GGT [IU/L] | 31.0 (12.0–296.0) | 23.0 (12.0–192.0) | 35.5 (12.0–296.0) |
| Bilirubin [mg/dL] | 0.6 (0.1–1.9) | 0.5 (0.2–1.7) | 0.6 (0.1–1.9) |
| Amylase [IU/L] | 38.5 (17.0–144.0) | 37.0 (18.0–144.0) | 39.0 (17.0–89.0) |
| Lipase [IU/L] | 26.0 (13.0–180.0) | 25.0 (14.0–86.0) | 29.0 (13.0–180.0) |
| Total cholesterol [mg/dL] | 185.0 (97.0–273.0) | 176.0 (97.0–270.0) | 187.0 (115.0–273.0) |
| Triglycerides [mg/dL] | 151.0 (58.0–779.0) | 117.0 (58.0–263.0) | 163.5 (63.0–779.0) |
| HDL [mg/dL] | 44.0 (18.0–88.0) | 47.5 (29.0–88.0) | 42.0 (18.0–84.0) |
| LDL [mg/dL] | 105.0 (27.4–213.0) | 104.0 (29.0–213.0) | 105.0 (27.4–181.0) |
| FIB-4 [points] | 0.7 (0.2–5.0) | 0.7 (0.2–2.1) | 0.8 (0.3–5.0) |
| NFS [points] | −0.85 (−4.0–4.8) | −1.1 (−3.0–2.7) | −0.7 (−4.0–4.8) |
| Glycaemia [mg/dL] | 97.0 (68.0–305.0) | 92.0 (73.0–126.0) | 101.0 (68.0–305.0) |
| HbA1c [%] | 5.7 (4.6–12.1) | 5.4 (4.9–7.1) | 5.8 (4.6–12.1) |
| C-peptide [ng/mL] | 3.8 (0.7–11.8) | 3.1 (2.0–5.5) | 3.9 (0.7–11.8) |
| Insulin [IU/mL] | 19.7 (4.8–177.0) | 14.5 (6.1–79.4) | 21.7 (4.8–177.0) |
| HOMA-IR [points] | 4.7 (1.0–74.0) | 3.4 (1.2–14.3) | 5.5 (1.0–74.0) |
| Histology | Score | Number of Patients | % |
|---|---|---|---|
| Steatosis | |||
| 0 | 49 | 29.7 |
| 1 | 64 | 38.8 |
| 2 | 36 | 21.8 |
| 3 | 16 | 9.7 |
| Lobular inflammation | |||
| 0 | 15 | 9.1 |
| 1 | 69 | 41.8 |
| 2 | 71 | 43.0 |
| 3 | 10 | 6.1 |
| Hepatocyte ballooning | |||
| 0 | 48 | 29.1 |
| 1 | 77 | 46.7 |
| 2 | 40 | 24.2 |
| NAS | |||
| 0–2 | 51 | 30.9 |
| 3–4 | 67 | 40.6 |
| ≥5 | 47 | 28.5 |
| Fibrosis | |||
| 0 | 51 | 30.9 |
| 1a | 57 | 34.6 |
| 1b | 2 | 1.2 |
| 1c | 30 | 18.2 |
| 2 | 21 | 12.7 |
| 3 | 4 | 2.4 |
| 4 | 0 | 0 |
| Cases | |||||
|---|---|---|---|---|---|
| MTARC1 (rs2642438) | PNPLA3 (rs738409) | TM6SF2 (rs58542926) | MBOAT7 (rs641738) | HSD17B13 (rs72613567) | |
| Wild-type | 80 (48.5%) | 117 (70.9%) | 149 (90.3%) | 56 (33.9%) | 102 (61.8%) |
| Heterozygous variant | 75 (45.4%) | 42 (25.5%) | 14 (8.5%) | 81 (49.1%) | 51 (30.9%) |
| Homozygous variant | 10 (6.1%) | 6 (3.6%) | 2 (1.2%) | 28 (17.0%) | 12 (7.3%) |
| Controls | |||||
| Wild-type | 144 (45.9%) | 181 (57.6%) | 278 (88.5%) | 90 (28.6%) | 176 (56.1%) |
| Heterozygous variant | 142 (45.2%) | 114 (36.3%) | 35 (11.2%) | 166 (52.9%) | 110 (35.0%) |
| Homozygous variant | 28 (8.9%) | 19 (6.1%) | 1 (0.3%) | 58 (18.5%) | 28 (8.9%) |
| p | 0.37 | <0.01 | 0.79 | 0.30 | 0.23 |
| OR | 0.85 | 0.64 | 1.06 | 0.87 | 0.84 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Factor | Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p |
| Fibrosis Grade ≥ 1a | ||||
| MTARC1 (rs2642438) | 0.56 (0.32–0.96) | 0.04 | NA | |
| PNPLA3 (rs738409) | 1.65 (0.84–3.23) | 0.15 | NA | |
| TM6SF2 (rs58542926) | 1.50 (0.52–4.35) | 0.45 | NA | |
| MBOAT7 (rs641738) | 0.96 (0.60–1.55) | 0.87 | NA | |
| HSD17B13 (rs72613567) | 1.37 (0.79–2.39) | 0.26 | NA | |
| BMI (kg/m2) | 1.01 (0.95–1.07) | 0.74 | NA | |
| Age (years) | 1.00 (0.97–1.04) | 0.95 | NA | |
| Gender | 0.77 (0.37–1.58) | 0.48 | NA | |
| Fibrosis Grade ≥ 1b | ||||
| MTARC1 (rs2642438) | 0.55 (0.31–0.96) | 0.04 | 0.52 (0.29–0.92) | 0.03 |
| PNPLA3 (rs738409) | 1.75 (0.98–3.13) | 0.06 | NA | |
| TM6SF2 (rs58542926) | 1.79 (0.73–4.35) | 0.20 | NA | |
| MBOAT7 (rs641738) | 1.16 (0.73–1.84) | 0.53 | NA | |
| HSD17B13 (rs72613567) | 1.08 (0.65–1.79) | 0.78 | NA | |
| BMI (kg/m2) | 1.03 (0.98–1.09) | 0.25 | NA | |
| Age (years) | 1.04 (1.00–1.08) | 0.03 | 1.04 (1.01–1.08) | 0.02 |
| Gender | 0.70 (0.36–1.37) | 0.30 | NA | |
| Fibrosis Grade ≥ 1c | ||||
| MTARC1 (rs2642438) | 0.55 (0.31–0.97) | 0.04 | 0.51 (0.28–0.92) | 0.04 |
| PNPLA3 (rs738409) | 1.87 (1.04–3.35) | 0.04 | 1.79 (0.98–3.30) | 0.06 |
| TM6SF2 (rs58542926) | 1.88 (0.77–4.58) | 0.17 | NA | |
| MBOAT7 (rs641738) | 1.14 (0.72–1.82) | 0.58 | NA | |
| HSD17B13 (rs72613567) | 1.07 (0.64–1.79) | 0.79 | NA | |
| BMI (kg/m2) | 1.04 (0.98–1.10) | 0.18 | NA | |
| Age (years) | 1.04 (1.00–1.07) | 0.04 | 1.04 (1.00–1.08) | 0.06 |
| Gender | 0.72 (0.37–1.43) | 0.35 | NA | |
| Fibrosis Grade ≥ 2 | ||||
| MTARC1 (rs2642438) | 0.54 (0.25–1.17) | 0.12 | NA | |
| PNPLA3 (rs738409) | 2.86 (1.43–5.72) | 0.003 | 3.09 (1.49–6.40) | 0.002 |
| TM6SF2 (rs58542926) | 2.56 (0.97–6.72) | 0.06 | NA | |
| MBOAT7 (rs641738) | 1.13 (0.61–2.08) | 0.70 | NA | |
| HSD17B13 (rs72613567) | 0.64 (0.29–1.38) | 0.25 | NA | |
| BMI (kg/m2) | 1.11 (1.04–1.20) | 0.003 | 1.12 (1.04–1.21) | 0.003 |
| Age (years) | 1.02 (0.97–1.06) | 0.46 | NA | |
| Gender | 0.58 (0.25–1.39) | 0.22 | NA | |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Factor | Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p |
| Steatosis grade ≥ S1 | ||||
| MTARC1 (rs2642438) | 1.20 (0.68–2.09) | 0.53 | NA | |
| PNPLA3 (rs738409) | 1.38 (0.71–2.65) | 0.34 | NA | |
| TM6SF2 (rs58542926) | 1.98 (0.60–6.58) | 0.26 | NA | |
| MBOAT7 (rs641738) | 1.25 (0.77–2.04) | 0.37 | NA | |
| HSD17B13 (rs72613567) | 0.77 (0.46–1.29) | 0.31 | NA | |
| BMI (kg/m2) | 1.01 (0.95–1.07) | 0.81 | NA | |
| Age (years) | 1.02 (0.98–1.05) | 0.35 | NA | |
| Gender | 0.41 (0.18–0.89) | 0.03 | NA | |
| Steatosis grade ≥ S2 | ||||
| MTARC1 (rs2642438) | 0.68 (0.38–1.19) | 0.17 | NA | |
| PNPLA3 (rs738409) | 2.27 (1.25–4.12) | 0.007 | 2.27 (1.24–4.15) | 0.008 |
| TM6SF2 (rs58542926) | 2.51 (1.00–6.28) | 0.049 | 2.51 (0.98–6.46) | 0.056 |
| MBOAT7 (rs641738) | 1.25 (0.78–2.01) | 0.36 | NA | |
| HSD17B13 (rs72613567) | 0.89 (0.52–1.51) | 0.66 | NA | |
| BMI (kg/m2) | 1.01 (0.95–1.07) | 0.82 | NA | |
| Age (years) | 1.02 (0.98–1.05) | 0.33 | NA | NA |
| Gender | 0.72 (0.36–1.43) | 0.34 | NA | |
| Steatosis grade = S3 | ||||
| MTARC1 (rs2642438) | 1.65 (0.73–3.75) | 0.23 | NA | |
| PNPLA3 (rs738409) | 3.46 (1.55–7.72) | 0.002 | 3.69 (1.56–8.70) | 0.003 |
| TM6SF2 (rs58542926) | 5.66 (1.99–16.11) | 0.001 | 6.19 (2.00–19.17) | 0.001 |
| MBOAT7 (rs641738) | 1.28 (0.61–2.67) | 0.52 | NA | |
| HSD17B13 (rs72613567) | 0.95 (0.41–2.19) | 0.91 | NA | |
| BMI (kg/m2) | 1.07 (0.99–1.17) | 0.11 | NA | |
| Age (years) | 1.00 (0.95–1.05) | 0.96 | NA | |
| Gender | 0.82 (0.28–2.38) | 0.71 | NA | |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Factor | Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p |
| MTARC1 (rs2642438) | 0.60 (0.33–1.08) | 0.08 | NA | |
| PNPLA3 (rs738409) | 2.26 (1.24–4.13) | 0.008 | 2.22 (1.03–4.80) | 0.04 |
| TM6SF2 (rs58542926) | 2.32 (0.94–5.75) | 0.07 | NA | |
| MBOAT7 (rs641738) | 1.06 (0.65–1.72) | 0.81 | NA | |
| HSD17B13 (rs72613567) | 1.05 (0.61–1.79) | 0.86 | NA | |
| Type 2 diabetes mellitus | 8.94 (3.94–20.28) | <0.001 | 7.91 (3.32–18.86) | <0.001 |
| Hyperlipidemia | 2.68 (1.14–6.30) | 0.02 | 2.93 (0.97–8.89) | 0.06 |
| BMI (kg/m2) | 1.01 (0.95–1.07) | 0.75 | NA | |
| Age (years) | 1.01 (0.98–1.05) | 0.57 | NA | |
| Gender | 1.09 (0.53–2.25) | 0.81 | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalinowski, P.; Smyk, W.; Nowosad, M.; Paluszkiewicz, R.; Michałowski, Ł.; Ziarkiewicz-Wróblewska, B.; Weber, S.N.; Milkiewicz, P.; Lammert, F.; Zieniewicz, K.; et al. MTARC1 and HSD17B13 Variants Have Protective Effects on Non-Alcoholic Fatty Liver Disease in Patients Undergoing Bariatric Surgery. Int. J. Mol. Sci. 2022, 23, 15825. https://doi.org/10.3390/ijms232415825
Kalinowski P, Smyk W, Nowosad M, Paluszkiewicz R, Michałowski Ł, Ziarkiewicz-Wróblewska B, Weber SN, Milkiewicz P, Lammert F, Zieniewicz K, et al. MTARC1 and HSD17B13 Variants Have Protective Effects on Non-Alcoholic Fatty Liver Disease in Patients Undergoing Bariatric Surgery. International Journal of Molecular Sciences. 2022; 23(24):15825. https://doi.org/10.3390/ijms232415825
Chicago/Turabian StyleKalinowski, Piotr, Wiktor Smyk, Małgorzata Nowosad, Rafał Paluszkiewicz, Łukasz Michałowski, Bogna Ziarkiewicz-Wróblewska, Susanne N. Weber, Piotr Milkiewicz, Frank Lammert, Krzysztof Zieniewicz, and et al. 2022. "MTARC1 and HSD17B13 Variants Have Protective Effects on Non-Alcoholic Fatty Liver Disease in Patients Undergoing Bariatric Surgery" International Journal of Molecular Sciences 23, no. 24: 15825. https://doi.org/10.3390/ijms232415825
APA StyleKalinowski, P., Smyk, W., Nowosad, M., Paluszkiewicz, R., Michałowski, Ł., Ziarkiewicz-Wróblewska, B., Weber, S. N., Milkiewicz, P., Lammert, F., Zieniewicz, K., & Krawczyk, M. (2022). MTARC1 and HSD17B13 Variants Have Protective Effects on Non-Alcoholic Fatty Liver Disease in Patients Undergoing Bariatric Surgery. International Journal of Molecular Sciences, 23(24), 15825. https://doi.org/10.3390/ijms232415825






