Mechanisms Underlying Antiarrhythmic Properties of Cardioprotective Agents Impacting Inflammation and Oxidative Stress
Abstract
:1. Introduction
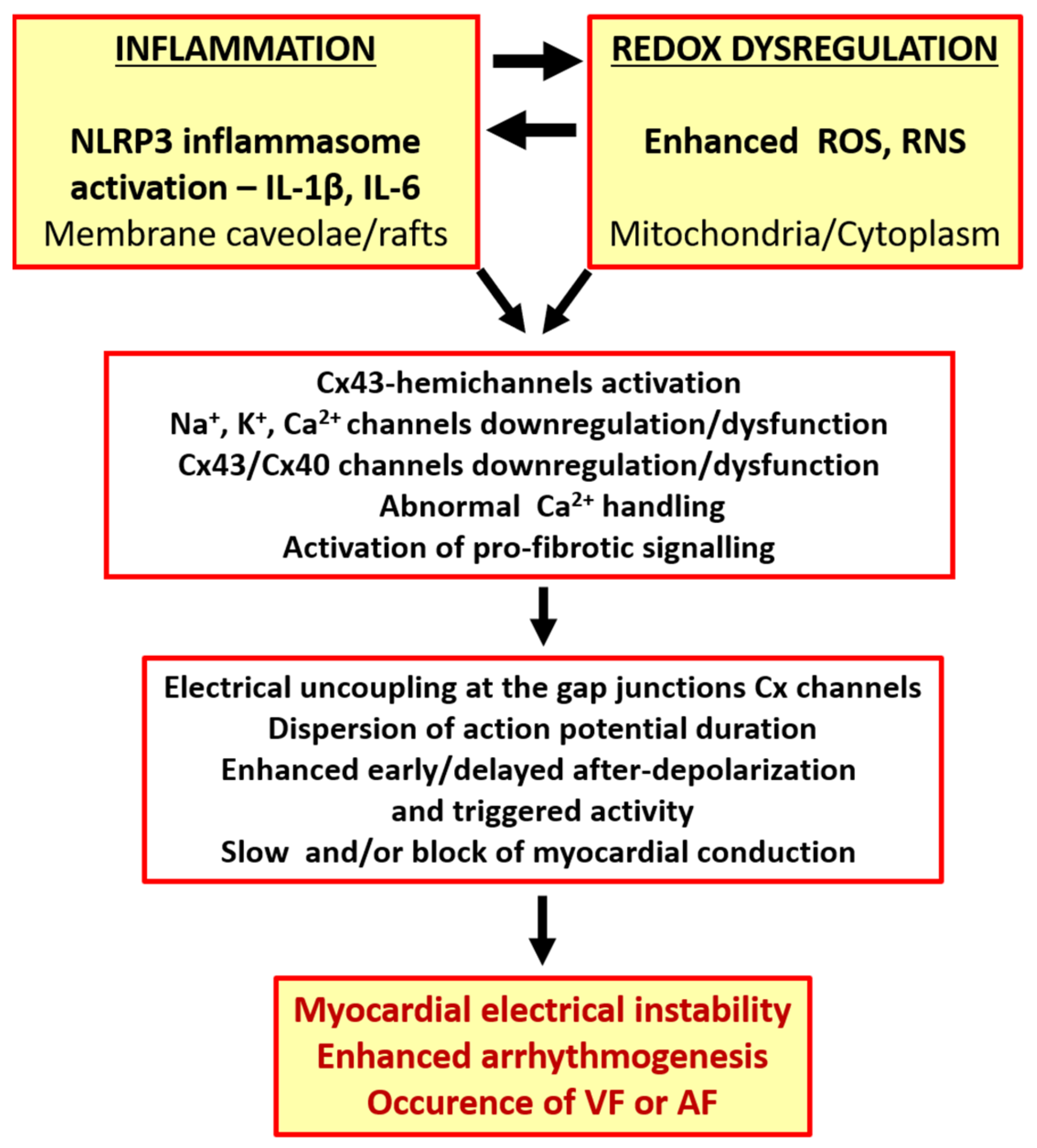
2. Inflammation and Redox Disorders Linked with Cardiac Arrhythmia Burden
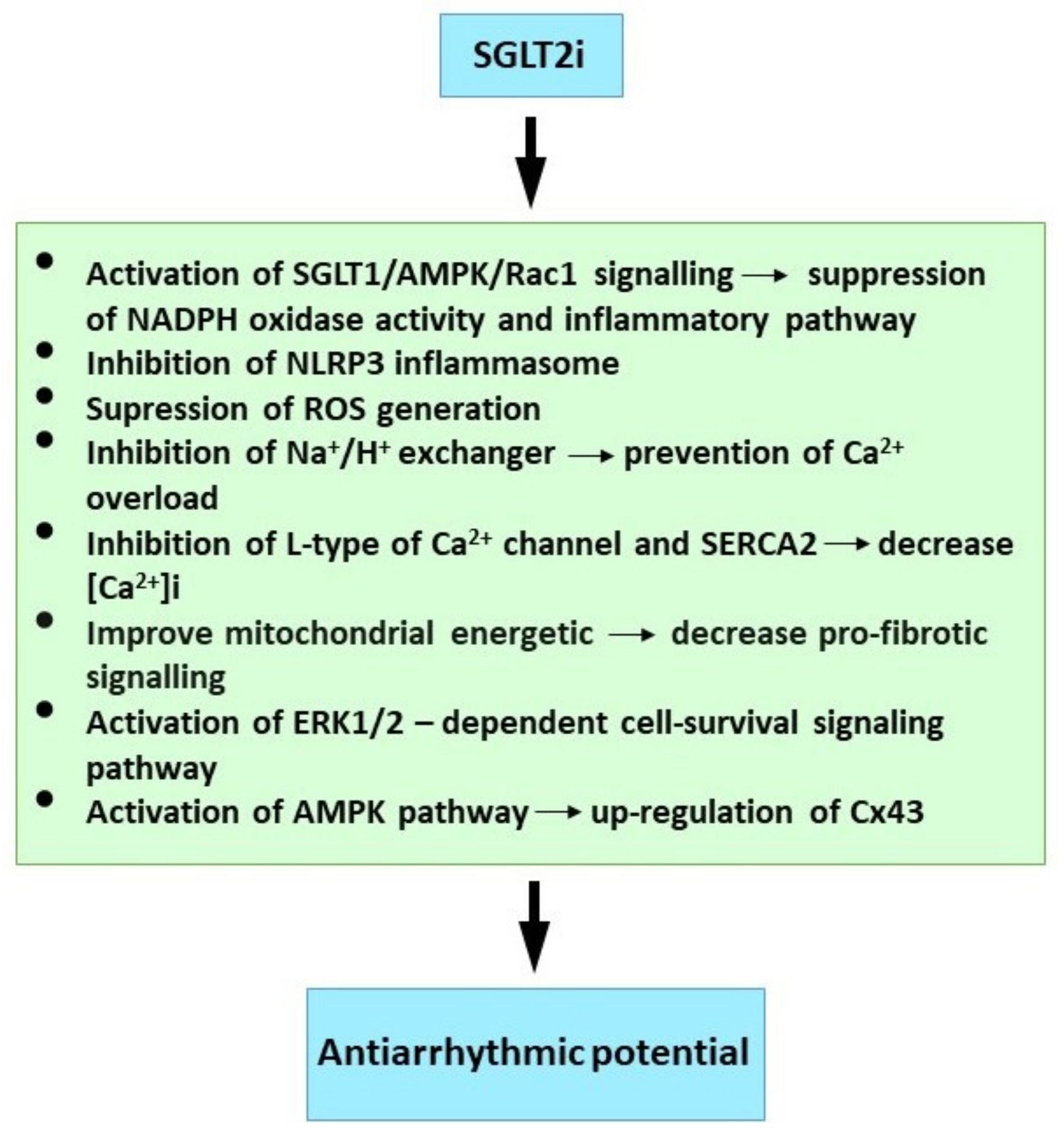
3. Antiarrhythmic Efficacy of SGLT2 Inhibitors
Mechanisms Relevant to Antiarrhythmic Properties of SGLT2 Inhibitors
4. Antiarrhythmic Efficacy of Statins
Mechanims Relevant to Statins Antiarrhythmic Properties
5. Antiarrhythmic Efficacy of Omega-3 Fatty Acids
Mechanisms Relevant to Antiarrhythmic Properties Omega-3 Fatty Acids
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zipes, D.P. Antiarrhythmic therapy in 2014: Contemporary approaches to treating arrhythmias. Nat. Rev. Cardiol. 2015, 12, 68–69. [Google Scholar] [CrossRef]
- Heijman, J.; Voigt, N.; Nattel, S.; Dobrev, D. Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ. Res. 2014, 114, 1483–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tribulova, N.; Szeiffova Bacova, B.; Benova, T.; Viczenczova, C. Can we protect from malignant arrhythmias by modulation of cardiac cell-to-cell coupling? J. Electrocardiol. 2015, 48, 434–440. [Google Scholar] [CrossRef]
- Tribulova, N.; Egan Benova, T.; Szeiffova Bacova, B.; Viczenczova, C.; Barancik, M. New aspects of pathogenesis of atrial fibrillation: Remodeling of intercalated discs. J. Physiol. Pharmacol. 2015, 66, 625–634. [Google Scholar] [PubMed]
- Tribulova, N.; Bacova, B.S.; Benova, T.E.; Knezl, V.; Barancik, M.; Slezak, J. Omega-3 index and anti-arrhythmic potential of omega-3 PUFAs. Nutrients 2017, 9, 1191. [Google Scholar] [CrossRef] [Green Version]
- Nattel, S.; Heijman, J.; Zhou, L.; Dobrev, D. Molecular Basis of Atrial Fibrillation Pathophysiology and Therapy: A Translational Perspective. Circ. Res. 2020, 127, 51–72. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, K.A.; Giotaki, S.G.; Vrachatis, D.A.; Siasos, G.; Lambadiari, V.; Iliodromitis, K.E.; Kossyvakis, C.; Kaoukis, A.; Raisakis, K.; Deftereos, G.; et al. Molecular insights in atrial fibrillation pathogenesis and therapeutics: A narrative review. Diagnostics 2021, 11, 1584. [Google Scholar] [CrossRef]
- Thomas, D.; Christ, T.; Fabritz, L.; Goette, A.; Hammwöhner, M.; Heijman, J.; Kockskämper, J.; Linz, D.; Odening, K.E.; Schweizer, P.A.; et al. German Cardiac Society Working Group on Cellular Electrophysiology state-of-the-art paper: Impact of molecular mechanisms on clinical arrhythmia management. Clin. Res. Cardiol. 2019, 108, 577–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campana, C.; Dariolli, R.; Boutjdir, M.; Sobie, E.A. Inflammation as a Risk Factor in Cardiotoxicity: An Important Consideration for Screening During Drug Development. Front. Pharmacol. 2021, 12, 598549. [Google Scholar] [CrossRef]
- Tretter, V.; Hochreiter, B.; Zach, M.L.; Krenn, K.; Klein, K.U. Understanding Cellular Redox Homeostasis: A Challenge for Precision Medicine. Int. J. Mol. Sci. 2022, 23, 106. [Google Scholar] [CrossRef] [PubMed]
- Lawler, P.R.; Bhatt, D.L.; Godoy, L.C.; Lüscher, T.F.; Bonow, R.O.; Verma, S.; Ridker, P.M. Targeting cardiovascular inflammation: Next steps in clinical translation. Eur. Heart J. 2021, 42, 113–131. [Google Scholar] [CrossRef]
- Liberale, L.; Montecucco, F.; Schwarz, L.; Lüscher, T.F.; Camici, G.G. Inflammation and cardiovascular diseases: Lessons from seminal clinical trials. Cardiovasc. Res. 2021, 117, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Sagris, M.; Theofilis, P.; Antonopoulos, A.S.; Oikonomou, E. Inflammation in Coronary Microvascular Dysfunction. Int. J. Mol. Sci. 2021, 22, 13471. [Google Scholar] [CrossRef] [PubMed]
- Santangeli, P.; Di Biase, L.; Pelargonio, G.; Burkhardt, J.D.; Natale, A. The pharmaceutical pipeline for atrial fibrillation. Ann. Med. 2011, 43, 13–32. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Korantzopoulos, P.; Li, G. Antioxidant therapies for the management of atrial fibrillation. Cardiovasc. Diagn. Ther. 2012, 2, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Barančík, M.; Grešová, L.; Barteková, M.; Dovinová, I. Nrf2 as a key player of redox regulation in cardiovascular diseases. Physiol. Res. 2016, 65, S1–S10. [Google Scholar] [CrossRef]
- Andelova, K.; Benova, T.E.; Bacova, B.S.; Sykora, M.; Prado, N.J.; Diez, E.R.; Hlivak, P.; Tribulova, N. Cardiac connexin-43 hemichannels and pannexin1 channels: Provocative antiarrhythmic targets. Int. J. Mol. Sci. 2021, 22, 260. [Google Scholar] [CrossRef] [PubMed]
- Vilela, E.M.; Fontes-Carvalho, R. Inflammation and ischemic heart disease: The next therapeutic target? Rev. Port. Cardiol. 2021, 40, 785–796. [Google Scholar] [CrossRef]
- Li, N.; Brundel, B.J.J.M. Inflammasomes and Proteostasis Novel Molecular Mechanisms Associated with Atrial Fibrillation. Circ. Res. 2020, 127, 73–90. [Google Scholar] [CrossRef]
- Lopaschuk, G.D.; Verma, S. Mechanisms of Cardiovascular Benefits of Sodium Glucose Co-Transporter 2 (SGLT2) Inhibitors: A State-of-the-Art Review. JACC Basic Transl. Sci. 2020, 5, 632–644. [Google Scholar] [CrossRef]
- Kondo, H.; Akoumianakis, I.; Badi, I.; Akawi, N.; Kotanidis, C.P.; Polkinghorne, M.; Stadiotti, I.; Sommariva, E.; Antonopoulos, A.S.; Carena, M.C.; et al. Effects of canagliflozin on human myocardial redox signalling: Clinical implications. Eur. Heart J. 2021, 42, 4947–4960. [Google Scholar] [CrossRef]
- Jayaram, R.; Jones, M.; Reilly, S.; Crabtree, M.J.; Pal, N.; Goodfellow, N.; Nahar, K.; Simon, J.; Carnicer, R.; DeSilva, R.; et al. Atrial nitroso-redox balance and refractoriness following on-pump cardiac surgery: A randomized trial of atorvastatin. Cardiovasc. Res. 2022, 118, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Huang, C.; Sin, J.; Germano, J.D.F.; Taylor, D.J.R.; Thakur, R.; Gottlieb, R.A.; Mentzer, R.M.; Andres, A.M. Attenuation of Adverse Postinfarction Left Ventricular Remodeling with Empagliflozin Enhances Mitochondria-Linked Cellular Energetics and Mitochondrial Biogenesis. Int. J. Mol. Sci. 2022, 23, 437. [Google Scholar] [CrossRef]
- Lendeckel, U.; Dobrev, D.; Goette, A. Aldosterone-receptor antagonism as a potential therapeutic option for atrial fibrillation. Br. J. Pharmacol. 2010, 159, 1581–1583. [Google Scholar] [CrossRef] [PubMed]
- Akar, F.G. Mitochondrial targets for arrhythmia suppression: Is there a role for pharmacological intervention? J. Interv. Card. Electrophysiol. 2013, 37, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Orenes-Piñero, E.; Valdés, M.; Lip, G.Y.H.; Maŕn, F. A comprehensive insight of novel antioxidant therapies for atrial fibrillation management. Drug Metab. Rev. 2015, 47, 388–400. [Google Scholar] [CrossRef]
- Tribulova, N.; Knezl, V.; Szeiffova Bacova, B.; Egan Benova, T.; Viczenczova, C.; Gonçalvesova, E.; Slezak, J. Disordered myocardial Ca2+ homeostasis results in substructural alterations that may promote occurrence of malignant arrhythmias. Physiol. Res. 2016, 65, S139–S148. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.A.; Russo, V.; Ceraso, S.; Gupta, D.; Barrett-Jolley, R. Anti-arrhythmic properties of non-antiarrhythmic medications. Pharmacol. Res. 2020, 156, 104762. [Google Scholar] [CrossRef] [PubMed]
- Savelieva, I.; Camm, J. Anti-arrhythmic drug therapy for atrial fibrillation: Current anti-arrhythmic drugs, investigational agents, and innovative approaches. Europace 2008, 10, 647–665. [Google Scholar] [CrossRef]
- Savelieva, I.; Kakouros, N.; Kourliouros, A.; Camm, A.J. Upstream therapies for management of atrial fibrillation: Review of clinical evidence and implications for European Society of Cardiology guidelines. Part I: Primary prevention. Europace 2011, 13, 308–328. [Google Scholar] [CrossRef]
- Varghese, B.; Feldman, D.I.; Chew, C.; Valilis, E.; Blumenthal, R.S.; Sharma, G.; Calkins, H. Inflammation, atrial fibrillation, and the potential role for colchicine therapy. Heart Rhythm O2 2021, 2, 298–303. [Google Scholar] [CrossRef]
- Groslambert, M.; Py, B.F. Spotlight on the NLRP3 inflammasome pathway. J. Inflamm. Res. 2018, 11, 359–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, J.; Lv, Z.; Zhang, Y.; Wang, Y.; Qiao, X.; Sun, C.; Chen, Y.; Guo, M.; Han, W.; Ye, A.; et al. Precision Redox: The Key for Antioxidant Pharmacology. Antioxid. Redox Signal. 2021, 34, 1069–1082. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Mallat, Z.; Weyand, C. Immune and inflammatory mechanisms mediate cardiovascular diseases from head to toe. Cardiovasc. Res. 2021, 117, 2503–2505. [Google Scholar] [CrossRef] [PubMed]
- Cas, M.D.; Roda, G.; Li, F.; Secundo, F. Functional lipids in autoimmune inflammatory diseases. Int. J. Mol. Sci. 2020, 21, 3074. [Google Scholar] [CrossRef]
- De Miguel, C.; Pelegrín, P.; Baroja-Mazo, A.; Cuevas, S. Emerging role of the inflammasome and pyroptosis in hypertension. Int. J. Mol. Sci. 2021, 22, 1064. [Google Scholar] [CrossRef] [PubMed]
- Onódi, Z.; Ruppert, M.; Kucsera, D.; Sayour, A.A.; Tóth, V.E.; Koncsos, G.; Novák, J.; Brenner, G.B.; Makkos, A.; Baranyai, T.; et al. AIM2-driven inflammasome activation in heart failure. Cardiovasc. Res. 2021, 117, 2639–2651. [Google Scholar] [CrossRef]
- Scott, L.; Fender, A.C.; Saljic, A.; Li, L.; Chen, X.; Wang, X.; Linz, D.; Lang, J.; Hohl, M.; Twomey, D.; et al. NLRP3 inflammasome is a key driver of obesity-induced atrial arrhythmias. Cardiovasc. Res. 2021, 117, 1746–1759. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.H.K.; Hwang, T.; Se Liebers, C.; Ng, F.S. Epicardial adipose tissue as a mediator of cardiac arrhythmias. Am. J. Physiol. Circ. Physiol. 2021, 322, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Christ, A.; Günther, P.; Lauterbach, M.A.R.; Duewell, P.; Biswas, D.; Pelka, K.; Scholz, C.J.; Oosting, M.; Haendler, K.; Baßler, K.; et al. Western Diet Triggers NLRP3-Dependent Innate Immune Reprogramming. Cell 2018, 172, 162–175.e14. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Zhang, S.; Li, B.; Luo, Y.; Gong, Y.; Jin, X.; Zhang, J.; Zhou, Y.; Zhuo, X.; Wang, Z.; et al. Gut microbiota dysbiosis promotes age-related atrial fibrillation by lipopolysaccharide and glucose-induced activation of NLRP3-inflammasome. Cardiovasc. Res. 2021, cvab114. [Google Scholar] [CrossRef] [PubMed]
- Linz, D.; Gawałko, M.; Sanders, P.; Penders, J.; Li, N.; Nattel, S.; Dobrev, D. Does gut microbiota affect atrial rhythm? Causalities and speculations. Eur. Heart J. 2021, 42, 3521–3525. [Google Scholar] [CrossRef] [PubMed]
- Münzel, T.; Hahad, O.; Sørensen, M.; Lelieveld, J.; Duerr, G.D.; Nieuwenhuijsen, M.; Daiber, A. Environmental risk factors and cardiovascular diseases: A comprehensive expert review. Cardiovasc. Res. 2021, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Egan Benova, T.; Viczenczova, C.; Szeiffova Bacova, B.; Zurmanova, J.; Knezl, V.; Andelova, K.; Tribulova, N. Omacor Protects Normotensive and Hypertensive Rats Exposed to Continuous Light from Increased Risk to Malignant Cardiac Arrhythmias. Mar. Drugs 2021, 19, 659. [Google Scholar] [CrossRef]
- Grune, J.; Yamazoe, M.; Nahrendorf, M. Electroimmunology and cardiac arrhythmia. Nat. Rev. Cardiol. 2021, 18, 547–564. [Google Scholar] [CrossRef]
- Ziegler, K.A.; Ahles, A.; Wille, T.; Kerler, J.; Ramanujam, D.; Engelhardt, S. Local sympathetic denervation attenuates myocardial inflammation and improves cardiac function after myocardial infarction in mice. Cardiovasc. Res. 2018, 114, 291–299. [Google Scholar] [CrossRef] [Green Version]
- Clemente-Moragón, A.; Gómez, M.; Villena-Gutiérrez, R.; Lalama, D.V.; García-Prieto, J.; Martínez, F.; Sánchez-Cabo, F.; Fuster, V.; Oliver, E.; Ibáñez, B. Metoprolol exerts a non-class effect against ischaemia-reperfusion injury by abrogating exacerbated inflammation. Eur. Heart J. 2020, 41, 4425–4440. [Google Scholar] [CrossRef] [PubMed]
- Schiattarella, G.G.; Rodolico, D.; Hill, J.A. Metabolic inflammation in heart failure with preserved ejection fraction. Cardiovasc. Res. 2021, 117, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Schunk, S.J.; Kleber, M.E.; März, W.; Pang, S.; Zewinger, S.; Triem, S.; Ege, P.; Reichert, M.C.; Krawczyk, M.; Weber, S.N.; et al. Genetically determined NLRP3 inflammasome activation associates with systemic inflammation and cardiovascular mortality. Eur. Heart J. 2021, 42, 1742–1756. [Google Scholar] [CrossRef]
- Heijman, J.; Muna, A.P.; Veleva, T.; Molina, C.E.; Sutanto, H.; Tekook, M.; Wang, Q.; Abu-Taha, I.H.; Gorka, M.; Künzel, S.; et al. Atrial myocyte NLRP3/CaMKII nexus forms a substrate for postoperative atrial fibrillation. Circ. Res. 2020, 127, 1036–1055. [Google Scholar] [CrossRef]
- Forrester, S.J.; Kikuchi, D.S.; Hernandes, M.S.; Xu, Q.; Griendling, K.K. Reactive oxygen species in metabolic and inflammatory signaling. Circ. Res. 2018, 122, 877–902. [Google Scholar] [CrossRef] [PubMed]
- Hernansanz-Agustín, P.; Enríquez, J.A. Generation of reactive oxygen species by mitochondria. Antioxidants 2021, 10, 415. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.; Veleva, T.; Scott, L.; Cao, S.; Li, L.; Chen, G.; Jeyabal, P.; Pan, X.; Alsina, K.M.; Abu-Taha, I.; et al. Enhanced Cardiomyocyte NLRP3 Inflammasome Signaling Promotes Atrial Fibrillation. Circulation 2018, 138, 2227–2242. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Liu, W.; Lan, T.; Pan, W.; Chen, X.; Wu, H.; Xu, D. Salvianolate reduces atrial fibrillation through suppressing atrial interstitial fibrosis by inhibiting TGF-β1/Smad2/3 and TXNIP/NLRP3 inflammasome signaling pathways in post-MI rats. Phytomedicine 2018, 51, 255–265. [Google Scholar] [CrossRef]
- Akar, F.G.; O’Rourke, B. Mitochondria are sources of metabolic sink and arrhythmias. Pharmacol. Ther. 2011, 131, 287–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghosh, A.; Shcherbik, N. Effects of oxidative stress on protein translation: Implications for cardiovascular diseases. Int. J. Mol. Sci. 2020, 21, 2661. [Google Scholar] [CrossRef] [Green Version]
- Bubb, K.J.; Drummond, G.R.; Figtree, G.A. New opportunities for targeting redox dysregulation in cardiovascular disease. Cardiovasc. Res. 2020, 116, 532–544. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Shi, Q.; Liu, X.; Li, Y.; Li, X. Attenuation of Myocardial Fibrosis Using Molecular Hydrogen by Inhibiting the TGF-β Signaling Pathway in Spontaneous Hypertensive Rats. Am. J. Hypertens. 2021, 1–8. [Google Scholar] [CrossRef]
- Lüscher, T.F. The sooner, the better: Anti-inflammation in acute myocardial infarction. Eur. Heart J. 2020, 41, 4100–4102. [Google Scholar] [CrossRef]
- Van Wagoner, D.R. Oxidative stress and inflammation in atrial fibrillation: Role in pathogenesis and potential as a therapeutic target. J. Cardiovasc. Pharmacol. 2008, 52, 306–313. [Google Scholar] [CrossRef]
- Lewek, J.; Kaczmarek, K.; Cygankiewicz, I.; Wranicz, J.K.; Ptaszynski, P. Inflammation and arrhythmias: Potential mechanisms and clinical implications. Expert Rev. Cardiovasc. Ther. 2014, 12, 1077–1085. [Google Scholar] [CrossRef]
- Van Wagoner, D.R.; Chung, M.K. Inflammation, Inflammasome Activation, and Atrial Fibrillation: Evidence for Causation and New Therapeutic Targets. Circulation 2018, 138, 2243–2246. [Google Scholar] [CrossRef]
- Tsalamandris, S.; Antonopoulos, A.S.; Oikonomou, E.; Papamikroulis, G.A.; Vogiatzi, G.; Papaioannou, S.; Deftereos, S.; Tousoulis, D. The role of inflammation in diabetes: Current concepts and future perspectives. Eur. Cardiol. Rev. 2019, 14, 50–59. [Google Scholar] [CrossRef] [Green Version]
- Antonopoulos, A.S.; Goliopoulou, A.; Oikonomou, E.; Tsalamandris, S.; Papamikroulis, G.-A.; Lazaros, G.; Tsiamis, E.; Latsios, G.; Brili, S.; Papaioannou, S.; et al. Redox State in Atrial Fibrillation Pathogenesis and Relevant Therapeutic Approaches. Curr. Med. Chem. 2017, 26, 765–779. [Google Scholar] [CrossRef] [PubMed]
- Azam, M.A.; Chakraborty, P.; Si, D.; Du, B.B.; Massé, S.; Lai, P.F.H.; Ha, A.C.T.; Nanthakumar, K. Anti-arrhythmic and inotropic effects of empagliflozin following myocardial ischemia. Life Sci. 2021, 276, 119440. [Google Scholar] [CrossRef]
- Zhang, Y.; Qi, Y.; Li, J.J.; He, W.J.; Gao, X.H.; Zhang, Y.; Sun, X.; Tong, J.; Zhang, J.; Deng, X.L.; et al. Stretch-induced sarcoplasmic reticulum calcium leak is causatively associated with atrial fibrillation in pressure-overloaded hearts. Cardiovasc. Res. 2021, 117, 1091–1102. [Google Scholar] [CrossRef] [PubMed]
- Aviles, R.J.; Martin, D.O.; Apperson-Hansen, C.; Houghtaling, P.L.; Rautaharju, P.; Kronmal, R.A.; Tracy, R.P.; Van Wagoner, D.R.; Psaty, B.M.; Lauer, M.S.; et al. Inflammation as a Risk Factor for Atrial Fibrillation. Circulation 2003, 108, 3006–3010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nattel, S.; Maguy, A.; Le Bouter, S.; Yeh, Y.H. Arrhythmogenic ion-channel remodeling in the heart: Heart failure, myocardial infarction, and atrial fibrillation. Physiol. Rev. 2007, 87, 425–456. [Google Scholar] [CrossRef]
- Calcaterra, V.; Regalbuto, C.; Porri, D.; Pelizzo, G.; Mazzon, E.; Vinci, F.; Zuccotti, G.; Fabiano, V.; Cena, H. Inflammation in obesity-related complications in children: The protective effect of diet and its potential role as a therapeutic agent. Biomolecules 2020, 10, 1324. [Google Scholar] [CrossRef]
- Madhur, M.S.; Elijovich, F.; Alexander, M.R.; Pitzer, A.; Ishimwe, J.; Van Beusecum, J.P.; Patrick, D.M.; Smart, C.D.; Kleyman, T.R.; Kingery, J.; et al. Hypertension: Do Inflammation and Immunity Hold the Key to Solving this Epidemic? Circ. Res. 2021, 128, 908–933. [Google Scholar] [CrossRef]
- Bernardi, J.; Aromolaran, K.A.; Aromolaran, A.S. Neurological disorders and risk of arrhythmia. Int. J. Mol. Sci. 2021, 22, 188. [Google Scholar] [CrossRef]
- Marín-Aguilar, F.; Lechuga-Vieco, A.V.; Alcocer-Gómez, E.; Castejón-Vega, B.; Lucas, J.; Garrido, C.; Peralta-Garcia, A.; Pérez-Pulido, A.J.; Varela-López, A.; Quiles, J.L.; et al. NLRP3 inflammasome suppression improves longevity and prevents cardiac aging in male mice. Aging Cell 2020, 19, e13050. [Google Scholar] [CrossRef] [Green Version]
- Segovia-Roldan, M.; Diez, E.R.; Pueyo, E. Melatonin to Rescue the Aged Heart: Antiarrhythmic and Antioxidant Benefits. Oxid. Med. Cell. Longev. 2021, 2021, 8876792. [Google Scholar] [CrossRef]
- Murray, E.C.; Nosalski, R.; MacRitchie, N.; Tomaszewski, M.; Maffia, P.; Harrison, D.G.; Guzik, T.J. Therapeutic targeting of inflammation in hypertension: From novelmechanisms to translational perspective. Cardiovasc. Res. 2021, 117, 2589–2609. [Google Scholar] [CrossRef] [PubMed]
- Egan Benova, T.; Szeiffova Bacova, B.; Viczenczova, C.; Diez, E.; Barancik, M.; Tribulova, N. Protection of cardiac cell-to-cell coupling attenuate myocardial remodeling and proarrhythmia induced by hypertension. Physiol. Res. 2016, 65, S29–S42. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.H.; Nattel, S.; Kalman, J.M.; Sanders, P. Modifiable Risk Factors and Atrial Fibrillation. Circulation 2017, 136, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Yalta, T.; Yalta, K. Systemic Inflammation and Arrhythmogenesis: A Review of Mechanistic and Clinical Perspectives. Angiology 2018, 69, 288–296. [Google Scholar] [CrossRef]
- Whayne, T.F.; Morales, G.X.; Darrat, Y.H. Clinical Aspects of Systemic Inflammation and Arrhythmogenesis, Especially Atrial Fibrillation. Angiology 2018, 69, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Bartekova, M.; Radosinska, J.; Jelemensky, M.; Dhalla, N.S. Role of cytokines and inflammation in heart function during health and disease. Heart Fail. Rev. 2018, 23, 733–758. [Google Scholar] [CrossRef] [PubMed]
- Zuo, L.; Prather, E.R.; Stetskiv, M.; Garrison, D.E.; Meade, J.R.; Peace, T.I.; Zhou, T. Inflammaging and oxidative stress in human diseases: From molecular mechanisms to novel treatments. Int. J. Mol. Sci. 2019, 20, 4472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fiordelisi, A.; Iaccarino, G.; Morisco, C.; Coscioni, E.; Sorriento, D. NfkappaB is a key player in the crosstalk between inflammation and cardiovascular diseases. Int. J. Mol. Sci. 2019, 20, 1599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García, I.E.; Sánchez, H.A.; Martínez, A.D.; Retamal, M.A. Redox-mediated regulation of connexin proteins; focus on nitric oxide. Biochim. Biophys. Acta-Biomembr. 2018, 1860, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Fakuade, F.E.; Tomsits, P.; Voigt, N. Connexin hemichannels in atrial fibrillation: Orphaned and irrelevant? Cardiovasc. Res. 2021, 117, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, A.D.; Joca, H.C.; Boyman, L.; Greiser, M. Calcium signaling silencing in atrial fibrillation: Implications for atrial sodium homeostasis. Int. J. Mol. Sci. 2021, 22, 513. [Google Scholar] [CrossRef]
- Lissoni, A.; Hulpiau, P.; Martins-Marques, T.; Wang, N.; Bultynck, G.; Schulz, R.; Witschas, K.; Girao, H.; De Smet, M.; Leybaert, L. RyR2 regulates Cx43 hemichannel intracellular Ca2+-dependent activation in cardiomyocytes. Cardiovasc. Res. 2021, 117, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Curcio, A.; Torella, D.; Iaconetti, C.; Pasceri, E.; Sabatino, J.; Sorrentino, S.; Giampà, S.; Micieli, M.; Polimeni, A.; Henning, B.J.; et al. MicroRNA-1 Downregulation Increases Connexin 43 Displacement and Induces Ventricular Tachyarrhythmias in Rodent Hypertrophic Hearts. PLoS ONE 2013, 8, e70158. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.J.; Tao, P.; Wang, Y. Attenuated Structural Transformation of Aconitine during Sand Frying Process and Antiarrhythmic Effect of Its Converted Products. Evid.-Based Complement. Altern. Med. 2021, 2021, e7243052. [Google Scholar] [CrossRef]
- Zima, A.V.; Blatter, L.A. Redox regulation of cardiac calcium channels and transporters. Cardiovasc. Res. 2006, 71, 310–321. [Google Scholar] [CrossRef]
- Tribulova, N.; Seki, S.; Radosinska, J.; Kaplan, P.; Babusikova, E.; Knezl, V.; Mochizuki, S. Myocardial Ca2+ handling and cell-to-cell coupling, key factors in prevention of sudden cardiac death1. Can. J. Physiol. Pharmacol. 2009, 87, 1120–1129. [Google Scholar] [CrossRef]
- Landstrom, A.P.; Dobrev, D.; Wehrens, X.H.T. Calcium Signaling and Cardiac Arrhythmias. Circ. Res. 2017, 120, 1969–1993. [Google Scholar] [CrossRef]
- Denham, N.C.; Pearman, C.M.; Caldwell, J.L.; Madders, G.W.P.; Eisner, D.A.; Trafford, A.W.; Dibb, K.M. Calcium in the pathophysiology of atrial fibrillation and heart failure. Front. Physiol. 2018, 9, 1380. [Google Scholar] [CrossRef] [Green Version]
- Parahuleva, M.S.; Kockskämper, J.; Heger, J.; Grimm, W.; Scherer, A.; Bühler, S.; Kreutz, J.; Schulz, R.; Euler, G. Structural, pro-inflammatory and calcium handling remodeling underlies spontaneous onset of paroxysmal atrial fibrillation in JDP2-overexpressing mice. Int. J. Mol. Sci. 2020, 21, 9095. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Cobo, M.; Gingalewski, C.; Drujan, D.; De Maio, A. Downregulation of connexin 43 gene expression in rat heart during inflammation. The role of tumour necrosis factor. Cytokine 1999, 11, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Gutstein, D.E. The cardiac gap junction: A potential therapeutic target in the treatment of heart disease. Mt. Sinai J. Med. 2002, 69, 421–424. [Google Scholar] [PubMed]
- Smyth, J.W.; Hong, T.T.; Gao, D.; Vogan, J.M.; Jensen, B.C.; Fong, T.S.; Simpson, P.C.; Stainier, D.Y.R.; Chi, N.C.; Shaw, R.M. Limited forward trafficking of connexin 43 reduces cell-cell coupling in stressed human and mouse myocardium. J. Clin. Investig. 2010, 120, 266–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cabo, C.; Yao, J.; Boyden, P.A.; Chen, S.; Hussain, W.; Duffy, H.S.; Ciaccio, E.J.; Peters, N.S.; Wit, A.L. Heterogeneous gap junction remodeling in reentrant circuits in the epicardial border zone of the healing canine infarct. Cardiovasc. Res. 2006, 72, 241–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danik, S.B.; Rosner, G.; Lader, J.; Gutstein, D.E.; Fishman, G.I.; Morley, G.E. Electrical remodeling contributes to complex tachyarrhythmias in connexin43-deficient mouse hearts. FASEB J. 2008, 22, 1204–1212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, J.H.; Huang, C.L.H.; Fraser, J.A. Determinants of myocardial conduction velocity: Implications for arrhythmogenesis. Front. Physiol. 2013, 4, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirubakaran, S.; Chowdhury, R.A.; Hall, M.C.S.; Patel, P.M.; Garratt, C.J.; Peters, N.S. Fractionation of electrograms is caused by colocalized conduction block and connexin disorganization in the absence of fibrosis as AF becomes persistent in the goat model. Heart Rhythm 2015, 12, 397–408. [Google Scholar] [CrossRef] [Green Version]
- Dhillon, P.S.; Chowdhury, R.A.; Patel, P.M.; Jabr, R.; Momin, A.U.; Vecht, J.; Gray, R.; Shipolini, A.; Fry, C.H.; Peters, N.S. Relationship between connexin expression and gap-junction resistivity in human atrial myocardium. Circ. Arrhythmia Electrophysiol. 2014, 7, 321–329. [Google Scholar] [CrossRef] [Green Version]
- Handa, B.S.; Li, X.; Baxan, N.; Roney, C.H.; Shchendrygina, A.; Mansfield, C.A.; Jabbour, R.J.; Pitcher, D.S.; Chowdhury, R.A.; Peters, N.S.; et al. Ventricular fibrillation mechanism and global fibrillatory organization are determined by gap junction coupling and fibrosis pattern. Cardiovasc. Res. 2021, 117, 1078–1090. [Google Scholar] [CrossRef]
- Bezzerides, V.J.; Pu, W.T. Two sides of the same coin: New insights into mechanisms of ventricular fibrillation. Cardiovasc. Res. 2021, 117, 983–984. [Google Scholar] [CrossRef] [PubMed]
- Peracchia, C. Gap junction channelopathies and calmodulinopathies. Do disease-causing calmodulin mutants affect direct cell–cell communication? Int. J. Mol. Sci. 2021, 22, 15–18. [Google Scholar] [CrossRef]
- Dhein, S.; Seidel, T.; Salameh, A.; Jozwiak, J.; Hagen, A.; Kostelka, M.; Hindricks, G.; Mohr, F.W. Remodeling of cardiac passive electrical properties and susceptibility to ventricular and atrial arrhythmias. Front. Physiol. 2014, 5, 424. [Google Scholar] [CrossRef] [PubMed]
- Zakkar, M.; Ascione, R.; James, A.F.; Angelini, G.D.; Suleiman, M.S. Inflammation, oxidative stress and postoperative atrial fibrillation in cardiac surgery. Pharmacol. Ther. 2015, 154, 13–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dhein, S.; Salameh, A. Remodeling of cardiac gap junctional cell–cell coupling. Cells 2021, 10, 2422. [Google Scholar] [CrossRef]
- Chatterjee, N.A.; Singh, J.P. Autonomic modulation and cardiac arrhythmias: Old insights and novel strategies. EP Eur. 2021, 23, 1708–1721. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [Green Version]
- Costard-Jäckle, A.; Tschöpe, D.; Meinertz, T. Cardiovascular outcome in type 2 diabetes and atrial fibrillation. Herz 2019, 44, 522–525. [Google Scholar] [CrossRef]
- Chan, Y.H.; Chen, S.W.; Chao, T.F.; Kao, Y.W.; Huang, C.Y.; Chu, P.H. The impact of weight loss related to risk of new-onset atrial fibrillation in patients with type 2 diabetes mellitus treated with sodium–glucose cotransporter 2 inhibitor. Cardiovasc. Diabetol. 2021, 20, 93. [Google Scholar] [CrossRef]
- Masson, W.; Lavalle-Cobo, A.; Nogueira, J.P. Effect of sglt2-inhibitors on epicardial adipose tissue: A meta-analysis. Cells 2021, 10, 2150. [Google Scholar] [CrossRef] [PubMed]
- Soucek, F.; Covassin, N.; Singh, P.; Ruzek, L.; Kara, T.; Suleiman, M.; Lerman, A.; Koestler, C.; Friedman, P.A.; Lopez-Jimenez, F.; et al. Effects of Atorvastatin (80 mg) Therapy on Quantity of Epicardial Adipose Tissue in Patients Undergoing Pulmonary Vein Isolation for Atrial Fibrillation. Am. J. Cardiol. 2015, 116, 1443–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, T.W.; Lee, T.I.; Lin, Y.K.; Chen, Y.C.; Kao, Y.H.; Chen, Y.J. Effect of antidiabetic drugs on the risk of atrial fibrillation: Mechanistic insights from clinical evidence and translational studies. Cell. Mol. Life Sci. 2021, 78, 923–934. [Google Scholar] [CrossRef]
- Böhm, M.; Slawik, J.; Brueckmann, M.; Mattheus, M.; George, J.T.; Ofstad, A.P.; Inzucchi, S.E.; Fitchett, D.; Anker, S.D.; Marx, N.; et al. Efficacy of empagliflozin on heart failure and renal outcomes in patients with atrial fibrillation: Data from the EMPA-REG OUTCOME trial. Eur. J. Heart Fail. 2020, 22, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Ling, A.W.C.; Chan, C.C.; Chen, S.W.; Kao, Y.W.; Huang, C.Y.; Chan, Y.H.; Chu, P.H. The risk of new-onset atrial fibrillation in patients with type 2 diabetes mellitus treated with sodium glucose cotransporter 2 inhibitors versus dipeptidyl peptidase-4 inhibitors. Cardiovasc. Diabetol. 2020, 19, 188. [Google Scholar] [CrossRef]
- Bonora, B.M.; Raschi, E.; Avogaro, A.; Fadini, G.P. SGLT-2 inhibitors and atrial fibrillation in the Food and Drug Administration adverse event reporting system. Cardiovasc. Diabetol. 2021, 20, 39. [Google Scholar] [CrossRef]
- Li, W.J.; Chen, X.Q.; Xu, L.L.; Li, Y.Q.; Luo, B.H. SGLT2 inhibitors and atrial fibrillation in type 2 diabetes: A systematic review with meta-analysis of 16 randomized controlled trials. Cardiovasc. Diabetol. 2020, 19, 130. [Google Scholar] [CrossRef]
- Okunrintemi, V.; Mishriky, B.M.; Powell, J.R.; Cummings, D.M. Sodium-glucose co-transporter-2 inhibitors and atrial fibrillation in the cardiovascular and renal outcome trials. Diabetes Obes. Metab. 2021, 23, 276–280. [Google Scholar] [CrossRef]
- Tanaka, H.; Tatsumi, K.; Matsuzoe, H.; Soga, F.; Matsumoto, K.; Hirata, K. ichi Association of type 2 diabetes mellitus with the development of new-onset atrial fibrillation in patients with non-ischemic dilated cardiomyopathy: Impact of SGLT2 inhibitors. Int. J. Cardiovasc. Imaging 2021, 37, 1333–1341. [Google Scholar] [CrossRef]
- Fitchett, D.; Inzucchi, S.E.; Cannon, C.P.; McGuire, D.K.; Scirica, B.M.; Johansen, O.E.; Sambevski, S.; Kaspers, S.; Pfarr, E.; George, J.T.; et al. Empagliflozin Reduced Mortality and Hospitalization for Heart Failure across the Spectrum of Cardiovascular Risk in the EMPA-REG OUTCOME Trial. Circulation 2019, 139, 1384–1395. [Google Scholar] [CrossRef]
- Zelniker, T.A.; Bonaca, M.P.; Furtado, R.H.M.; Mosenzon, O.; Kuder, J.F.; Murphy, S.A.; Bhatt, D.L.; Leiter, L.A.; McGuire, D.K.; Wilding, J.P.H.; et al. Effect of dapagliflozin on atrial fibrillation in patients with type 2 diabetes mellitus: Insights from the DECLARE-TIMI 58 Trial. Circulation 2020, 141, 1227–1234. [Google Scholar] [CrossRef]
- Li, H.L.; Lip, G.Y.H.; Feng, Q.; Fei, Y.; Tse, Y.K.; Wu, M.Z.; Ren, Q.W.; Tse, H.F.; Cheung, B.M.Y.; Yiu, K.H. Sodium-glucose cotransporter 2 inhibitors (SGLT2i) and cardiac arrhythmias: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2021, 20, 100. [Google Scholar] [CrossRef]
- Zhou, L.; Yang, Y.; Han, W. Sodium-glucose cotransporter-2 inhibitors protect against atrial fibrillation in patients with heart failure. Ann. Palliat. Med. 2021, 10, 10887–10895. [Google Scholar] [CrossRef] [PubMed]
- Curtain, J.P.; Docherty, K.F.; Jhund, P.S.; Petrie, M.C.; Inzucchi, S.E.; Kober, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; et al. Effect of dapagliflozin on ventricular arrhythmias, resuscitated cardiac arrest, or sudden death in DAPA-HF. Eur. Heart J. 2021, 42, 3727–3738. [Google Scholar] [CrossRef] [PubMed]
- Sfairopoulos, D.; Zhang, N.; Wang, Y.; Chen, Z.; Letsas, K.P.; Tse, G.; Li, G.; Lip, G.Y.H.; Liu, T.; Korantzopoulos, P. Association between sodium–glucose cotransporter-2 inhibitors and risk of sudden cardiac death or ventricular arrhythmias: A meta-analysis of randomized controlled trials. EP Eur. 2022, 24, 20–30. [Google Scholar] [CrossRef]
- Ilyas, F.; Jones, L.; Tee, S.L.; Horsfall, M.; Swan, A.; Wollaston, F.; Hecker, T.; De Pasquale, C.; Thomas, S.; Chong, W.; et al. Acute pleiotropic effects of dapagliflozin in type 2 diabetic patients with heart failure with reduced ejection fraction: A crossover trial. ESC Heart Fail. 2021, 8, 4346–4352. [Google Scholar] [CrossRef] [PubMed]
- Light, P.E. Decoding the effects of SGLT2 inhibitors on cardiac arrhythmias in heart failure. Eur. Heart J. 2021, 42, 3739–3740. [Google Scholar] [CrossRef] [PubMed]
- Teo, Y.H.; Teo, Y.N.; Syn, N.L.; Kow, C.S.; Yoong, C.S.Y.; Tan, B.Y.Q.; Yeo, T.C.; Lee, C.H.; Lin, W.; Sia, C.H. Effects of sodium/glucose cotransporter 2 (Sglt2) inhibitors on cardiovascular and metabolic outcomes in patients without diabetes mellitus: A systematic review and meta-analysis of randomized-controlled trials. J. Am. Heart Assoc. 2021, 10, e019463. [Google Scholar] [CrossRef]
- Yu, Y.W.; Zhao, X.M.; Wang, Y.H.; Zhou, Q.; Huang, Y.; Zhai, M.; Zhang, J. Effect of sodium–glucose cotransporter 2 inhibitors on cardiac structure and function in type 2 diabetes mellitus patients with or without chronic heart failure: A meta-analysis. Cardiovasc. Diabetol. 2021, 20, 25. [Google Scholar] [CrossRef]
- Zhang, N.; Wang, Y.; Tse, G.; Korantzopoulos, P.; Letsas, K.P.; Zhang, Q.; Li, G.; Lip, G.Y.H.; Liu, T. Effect of sodium-glucose cotransporter-2 inhibitors on cardiac remodelling: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2021, zwab173. [Google Scholar] [CrossRef]
- Zhang, D.P.; Xu, L.; Wang, L.F.; Wang, H.J.; Jiang, F. Effects of antidiabetic drugs on left ventricular function/dysfunction: A systematic review and network meta-analysis. Cardiovasc. Diabetol. 2020, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Ring, A.; Brand, T.; Macha, S.; Breithaupt-Groegler, K.; Simons, G.; Walter, B.; Woerle, H.J.; Broedl, U.C. The sodium glucose cotransporter 2 inhibitor empagliflozin does not prolong QT interval in a thorough QT (TQT) study. Cardiovasc. Diabetol. 2013, 12, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bode, D.; Semmler, L.; Oeing, C.U.; Alogna, A.; Schiattarella, G.G.; Pieske, B.M.; Heinzel, F.R.; Hohendanner, F. Implications of sglt inhibition on redox signalling in atrial fibrillation. Int. J. Mol. Sci. 2021, 22, 5937. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Römer, G.; Kerindongo, R.P.; Hermanides, J.; Albrecht, M.; Hollmann, M.W.; Zuurbier, C.J.; Preckel, B.; Weber, N.C. Sodium glucose co-transporter 2 inhibitors ameliorate endothelium barrier dysfunction induced by cyclic stretch through inhibition of reactive oxygen species. Int. J. Mol. Sci. 2021, 22, 6044. [Google Scholar] [CrossRef]
- Koyani, C.N.; Plastira, I.; Sourij, H.; Hallström, S.; Schmidt, A.; Rainer, P.P.; Bugger, H.; Frank, S.; Malle, E.; von Lewinski, D. Empagliflozin protects heart from inflammation and energy depletion via AMPK activation. Pharmacol. Res. 2020, 158, 104870. [Google Scholar] [CrossRef]
- Prattichizzo, F.; De Nigris, V.; Micheloni, S.; La Sala, L.; Ceriello, A. Increases in circulating levels of ketone bodies and cardiovascular protection with SGLT2 inhibitors: Is low-grade inflammation the neglected component? Diabetes Obes. Metab. 2018, 20, 2515–2522. [Google Scholar] [CrossRef] [PubMed]
- Sardu, C.; Massetti, M.; Testa, N.; Di Martino, L.; Castellano, G.; Turriziani, F.; Sasso, F.C.; Torella, M.; De Feo, M.; Santulli, G.; et al. Effects of Sodium-Glucose Transporter 2 Inhibitors (SGLT2-I) in Patients With Ischemic Heart Disease (IHD) Treated by Coronary Artery Bypass Grafting via MiECC: Inflammatory Burden, and Clinical Outcomes at 5 Years of Follow-Up. Front. Pharmacol. 2021, 12, 777083. [Google Scholar] [CrossRef]
- Jespersen, N.; Lassen, T.; Hjortbak, M.; Stottrup, N.; Botker, H. Sodium Glucose Transporter 2 (SGLT2) Inhibition does not Protect the Myocardium from Acute Ischemic Reperfusion Injury but Modulates Post- Ischemic Mitochondrial Function. Cardiovasc. Pharmacol. Open Access 2017, 6, 2–4. [Google Scholar] [CrossRef]
- Hu, Z.; Ju, F.; Du, L.; Abbott, G.W. Empagliflozin protects the heart against ischemia/reperfusion-induced sudden cardiac death. Cardiovasc. Diabetol. 2021, 20, 199. [Google Scholar] [CrossRef]
- Lee, C.C.; Chen, W.T.; Chen, S.Y.; Lee, T.M. Dapagliflozin attenuates arrhythmic vulnerabilities by regulating connexin43 expression via the AMPK pathway in post-infarcted rat hearts. Biochem. Pharmacol. 2021, 192, 114674. [Google Scholar] [CrossRef]
- Heller, S.; Darpö, B.; Mitchell, M.I.; Linnebjerg, H.; Leishman, D.J.; Mehrotra, N.; Zhu, H.; Koerner, J.; Fiszman, M.L.; Balakrishnan, S.; et al. Considerations for assessing the potential effects of antidiabetes drugs on cardiac ventricular repolarization: A report from the Cardiac Safety Research Consortium. Am. Heart J. 2015, 170, 23–35. [Google Scholar] [CrossRef]
- Durak, A.; Olgar, Y.; Degirmenci, S.; Akkus, E.; Tuncay, E.; Turan, B. A SGLT2 inhibitor dapagliflozin suppresses prolonged ventricular-repolarization through augmentation of mitochondrial function in insulin-resistant metabolic syndrome rats. Cardiovasc. Diabetol. 2018, 17, 144. [Google Scholar] [CrossRef] [PubMed]
- Lahnwong, S.; Palee, S.; Apaijai, N.; Sriwichaiin, S.; Kerdphoo, S.; Jaiwongkam, T.; Chattipakorn, S.C.; Chattipakorn, N. Acute dapagliflozin administration exerts cardioprotective effects in rats with cardiac ischemia/reperfusion injury. Cardiovasc. Diabetol. 2020, 19, 91. [Google Scholar] [CrossRef]
- Lin, Y.W.; Chen, C.Y.; Shih, J.Y.; Cheng, B.C.; Chang, C.P.; Lin, M.T.; Ho, C.H.; Chen, Z.C.; Fisch, S.; Chang, W.T. Dapagliflozin improves cardiac hemodynamics and mitigates arrhythmogenesis in mitral regurgitation-induced myocardial dysfunction. J. Am. Heart Assoc. 2021, 10, e019274. [Google Scholar] [CrossRef]
- Bariş, V.Ö.; Dinçsoy, B.; Gedikli, E.; Erdem, A. Empagliflozin significantly attenuates sotalol-induced QTc prolongation in rats. Kardiol. Pol. 2021, 79, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Baartscheer, A.; Schumacher, C.A.; Wüst, R.C.I.; Fiolet, J.W.T.; Stienen, G.J.M.; Coronel, R.; Zuurbier, C.J. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 2017, 60, 568–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, T.I.; Chen, Y.C.; Lin, Y.K.; Chung, C.C.; Lu, Y.Y.; Kao, Y.H.; Chen, Y.J. Empagliflozin attenuates myocardial sodium and calcium dysregulation and reverses cardiac remodeling in streptozotocin-induced diabetic rats. Int. J. Mol. Sci. 2019, 20, 1680. [Google Scholar] [CrossRef] [Green Version]
- Zuurbier, C.J.; Baartscheer, A.; Schumacher, C.A.; Fiolet, J.W.T.; Coronel, R. Sodium-glucose co-transporter 2 inhibitor empagliflozin inhibits the cardiac Na+/H+ exchanger 1: Persistent inhibition under various experimental conditions. Cardiovasc. Res. 2021, 117, 2699–2701. [Google Scholar] [CrossRef]
- Trum, M.; Riechel, J.; Wagner, S. Cardioprotection by sglt2 inhibitors—does it all come down to Na+ ? Int. J. Mol. Sci. 2021, 22, 7976. [Google Scholar] [CrossRef]
- Jhuo, S.J.; Liu, I.H.; Tasi, W.C.; Chou, T.W.; Lin, Y.H.; Wu, B.N.; Lee, K.T.; Lai, W. Ter Characteristics of ventricular electrophysiological substrates in metabolic mice treated with empagliflozin. Int. J. Mol. Sci. 2021, 22, 6105. [Google Scholar] [CrossRef]
- Bode, D.; Semmler, L.; Wakula, P.; Hegemann, N.; Primessnig, U.; Beindorff, N.; Powell, D.; Dahmen, R.; Ruetten, H.; Oeing, C.; et al. Dual SGLT-1 and SGLT-2 inhibition improves left atrial dysfunction in HFpEF. Cardiovasc. Diabetol. 2021, 20, 7. [Google Scholar] [CrossRef]
- Mustroph, J.; Wagemann, O.; Lücht, C.M.; Trum, M.; Hammer, K.P.; Sag, C.M.; Lebek, S.; Tarnowski, D.; Reinders, J.; Perbellini, F.; et al. Empagliflozin reduces ca/calmodulin-dependent kinase ii activity in isolated ventricular cardiomyocytes. ESC Heart Fail. 2018, 5, 642–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishinarita, R.; Niwano, S.; Niwano, H.; Nakamura, H.; Saito, D.; Sato, T.; Matsuura, G.; Arakawa, Y.; Kobayashi, S.; Shirakawa, Y.; et al. Canagliflozin suppresses atrial remodeling in a canine atrial fibrillation model. J. Am. Heart Assoc. 2021, 10, e017483. [Google Scholar] [CrossRef] [PubMed]
- Shao, Q.; Meng, L.; Lee, S.; Tse, G.; Gong, M.; Zhang, Z.; Zhao, J.; Zhao, Y.; Li, G.; Liu, T. Empagliflozin, a sodium glucose co-transporter-2 inhibitor, alleviates atrial remodeling and improves mitochondrial function in high-fat diet/streptozotocin-induced diabetic rats. Cardiovasc. Diabetol. 2019, 18, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beri, A.; Contractor, T.; Khasnis, A.; Thakur, R. Statins and the reduction of sudden cardiac death: Antiarrhythmic or anti-ischemic effect? Am. J. Cardiovasc. Drugs 2010, 10, 155–164. [Google Scholar] [CrossRef]
- Ghaisas, M.M.; Dandawate, P.R.; Zawar, S.A.; Ahire, Y.S.; Gandhi, S.P. Antioxidant, antinociceptive and anti-inflammatory activities of atorvastatin and rosuvastatin in various experimental models. Inflammopharmacology 2010, 18, 169–177. [Google Scholar] [CrossRef]
- Niessner, A.; Steiner, S.; Speidl, W.S.; Pleiner, J.; Seidinger, D.; Maurer, G.; Goronzy, J.J.; Weyand, C.M.; Kopp, C.W.; Huber, K.; et al. Simvastatin suppresses endotoxin-induced upregulation of toll-like receptors 4 and 2 in vivo. Atherosclerosis 2006, 189, 408–413. [Google Scholar] [CrossRef]
- Ascer, E.; Bertolami, M.C.; Venturinelli, M.L.; Buccheri, V.; Souza, J.; Nicolau, J.C.; Ramires, J.A.F.; Serrano, C.V. Atorvastatin reduces proinflammatory markers in hypercholesterolemic patients. Atherosclerosis 2004, 177, 161–166. [Google Scholar] [CrossRef]
- Satoh, M.; Tabuchi, T.; Itoh, T.; Nakamura, M. NLRP3 inflammasome activation in coronary artery disease: Results from prospective and randomized study of treatment with atorvastatin or rosuvastatin. Clin. Sci. 2014, 126, 233–241. [Google Scholar] [CrossRef]
- Lu, T.; Yang, X.; Cai, Y.; Xie, C.; Zhang, B. Prestroke statins improve prognosis of atrial fibrillation-associated stroke through increasing suppressor of cytokine signaling-3 levels. Eur. Neurol. 2021, 84, 96–102. [Google Scholar] [CrossRef]
- Vieira-Silva, S.; Falony, G.; Belda, E.; Nielsen, T.; Aron-Wisnewsky, J.; Chakaroun, R.; Forslund, S.K.; Assmann, K.; Valles-Colomer, M.; Nguyen, T.T.D.; et al. Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature 2020, 581, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Buber, J.; Goldenberg, I.; Moss, A.J.; Wang, P.J.; McNitt, S.; Hall, W.J.; Eldar, M.; Barsheshet, A.; Shechter, M. Reduction in life-threatening ventricular tachyarrhythmias in statin-treated patients with nonischemic cardiomyopathy enrolled in the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy). J. Am. Coll. Cardiol. 2012, 60, 749–755. [Google Scholar] [CrossRef] [Green Version]
- Liao, Y.C.; Hsieh, Y.C.; Hung, C.Y.; Huang, J.L.; Lin, C.H.; Wang, K.Y.; Wu, T.J. Statin therapy reduces the risk of ventricular arrhythmias, sudden cardiac death, and mortality in heart failure patients: A nationwide population-based cohort study. Int. J. Cardiol. 2013, 168, 4805–4807. [Google Scholar] [CrossRef] [PubMed]
- Rusnak, J.; Behnes, M.; Schupp, T.; Lang, S.; Reiser, L.; Taton, G.; Bollow, A.; Reichelt, T.; Ellguth, D.; Engelke, N.; et al. Statin therapy is associated with improved survival in patients with ventricular tachyarrhythmias. Lipids Health Dis. 2019, 18, 119. [Google Scholar] [CrossRef] [Green Version]
- Rahimi, K.; Majoni, W.; Merhi, A.; Emberson, J. Effect of statins on ventricular tachyarrhythmia, cardiac arrest, and sudden cardiac death: A meta-analysis of published and unpublished evidence from randomized trials. Eur. Heart J. 2012, 33, 1571–1581. [Google Scholar] [CrossRef] [Green Version]
- Wanahita, N.; Chen, J.; Bangalore, S.; Shah, K.; Rachko, M.; Coleman, C.I.; Schweitzer, P. The effect of statin therapy on ventricular tachyarrhythmias: A meta-analysis. Am. J. Ther. 2012, 19, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Manickam, P.; Rathod, A.; Badheka, A.; Afonso, L.; Aravindhakshan, R. Statin therapy significantly reduces risk of ventricular tachyarrhythmias in patients with an implantable cardioverter defibrillator. Am. J. Ther. 2012, 19, 261–268. [Google Scholar] [CrossRef]
- Abuissa, H.; O’Keefe, J.H.; Bybee, K.A. Statins as antiarrhythmics: A systematic review part II: Effects on risk of ventricular arrhythmias. Clin. Cardiol. 2009, 32, 549–552. [Google Scholar] [CrossRef]
- Liu, Y.-B.; Lee, Y.-T.; Pak, H.-N.; Lin, S.-F.; Fishbein, M.C.; Chen, L.S.; Merz, C.N.B.; Chen, P.-S. Effects of simvastatin on cardiac neural and electrophysiologic remodeling in rabbits with hypercholesterolemia. Heart Rhythm 2009, 6, 69–75. [Google Scholar] [CrossRef] [Green Version]
- Park, J.S.; Kim, B.W.; Hong, T.J.; Choe, J.C.; Lee, H.W.; Oh, J.H.; Choi, J.H.; Lee, H.C.; Cha, K.S.; Jeong, M.H. Lower In-Hospital Ventricular Tachyarrhythmia in Patients With Acute Myocardial Infarction Receiving Prior Statin Therapy. Angiology 2018, 69, 892–899. [Google Scholar] [CrossRef]
- Chen, M.J.; Bala, A.; Huddleston, J.I.; Goodman, S.B.; Maloney, W.J.; Aaronson, A.J.; Amanatullah, D.F. Statin use is associated with less postoperative cardiac arrhythmia after total hip arthroplasty. HIP Int. 2019, 29, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Bonano, J.C.; Aratani, A.K.; Sambare, T.D.; Goodman, S.B.; Huddleston, J.I.; Maloney, W.J.; Burk, D.R.; Aaronson, A.J.; Finlay, A.K.; Amanatullah, D.F. Perioperative Statin Use May Reduce Postoperative Arrhythmia Rates After Total Joint Arthroplasty. J. Arthroplast. 2021, 36, 3401–3405. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.R.; Liu, H.B.; Sha, Y.; Shi, Y.; Wang, H.; Yin, D.W.; Chen, Y.D.; Shi, X.M. Effects of statin on arrhythmia and heart rate variability in healthy persons with 48-hour sleep deprivation. J. Am. Heart Assoc. 2016, 5, e003833. [Google Scholar] [CrossRef] [Green Version]
- Bastani, M.; Khosravi, M.; Shafa, M.; Azemati, S.; Maghsoodi, B.; Asadpour, E. Evaluation of high-dose atorvastatin pretreatment influence in patients preconditioning of post coronary artery bypass graft surgery: A prospective triple blind randomized clinical trial. Ann. Card. Anaesth. 2021, 24, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Zhen-Han, L.; Rui, S.; Dan, C.; Xiao-Li, Z.; Qing-Chen, W.; Bo, F. Perioperative statin administration with decreased risk of postoperative atrial fibrillation, but not acute kidney injury or myocardial infarction: A meta-analysis. Sci. Rep. 2017, 7, 10091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, Y.; Ji, Q.; Mei, Y.; Wang, X.; Feng, J.; Cai, J.; Chi, L. Role of preoperative atorvastatin administration in protection against postoperative atrial fibrillation following conventional coronary artery bypass grafting. Int. Heart J. 2011, 52, 7–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nomani, H.; Mohammadpour, A.H.; Reiner, Ž.; Jamialahmadi, T.; Sahebkar, A. Statin therapy in post-operative atrial fibrillation: Focus on the anti-inflammatory effects. J. Cardiovasc. Dev. Dis. 2021, 8, 24. [Google Scholar] [CrossRef]
- Reilly, S.N.; Jayaram, R.; Nahar, K.; Antoniades, C.; Verheule, S.; Channon, K.M.; Alp, N.J.; Schotten, U.; Casadei, B. Atrial sources of reactive oxygen species vary with the duration and substrate of atrial fibrillation: Implications for the antiarrhythmic effect of statins. Circulation 2011, 124, 1107–1117. [Google Scholar] [CrossRef] [Green Version]
- Acampa, M.; Lazzerini, P.E.; Guideri, F.; Tassi, R.; Lo Monaco, A.; Martini, G. Previous use of Statins and Atrial Electrical Remodeling in Patients with Cryptogenic Stroke. Cardiovasc. Hematol. Disord. Targets 2018, 17, 212–215. [Google Scholar] [CrossRef]
- Hou, X.; Zhang, Y.; Wang, X.; Zheng, S.; Hou, Y.; Gao, M. Effects of rosuvastatin on atrial nerve sprouting and electrical remodeling in rabbits with myocardial infarction. Int. J. Clin. Exp. Med. 2015, 8, 7553–7560. [Google Scholar] [PubMed]
- Peng, H.; Yang, Y.; Zhao, Y.; Xiao, H. The effect of statins on the recurrence rate of atrial fibrillation after catheter ablation: A meta-analysis. Pacing Clin. Electrophysiol. 2018, 41, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Jia, Q.; Han, W.; Shi, S.; Hu, Y. The effects of ACEI/ARB, aldosterone receptor antagonists and statins on preventing recurrence of atrial fibrillation: A protocol for systematic review and network meta-analysis. Medicine 2021, 100, e24280. [Google Scholar] [CrossRef] [PubMed]
- Santangeli, P.; Ferrante, G.; Pelargonio, G.; Dello Russo, A.; Casella, M.; Bartoletti, S.; Di Biase, L.; Crea, F.; Natale, A. Usefulness of statins in preventing atrial fibrillation in patients with permanent pacemaker: A systematic review. Europace 2010, 12, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Soliman, E.Z.; Howard, G.; Judd, S.; Bhave, P.D.; Howard, V.J.; Herrington, D.M. Factors Modifying the Risk of Atrial Fibrillation Associated With Atrial Premature Complexes in Patients with Hypertension. Am. J. Cardiol. 2020, 125, 1324–1331. [Google Scholar] [CrossRef]
- Tseng, C.H.; Chung, W.J.; Li, C.Y.; Tsai, T.H.; Lee, C.H.; Hsueh, S.K.; Wu, C.C.; Cheng, C.I. Statins reduce new-onset atrial fibrillation after acute myocardial infarction: A nationwide study. Medicine 2020, 99, e18517. [Google Scholar] [CrossRef]
- Tekin, A.; Tekin, G.; Sezgin, A.T.; Müderrisoğlu, H. Short- and long-term effect of simvastatin therapy on the heterogeneity of cardiac repolarization in diabetic patients. Pharmacol. Res. 2008, 57, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Munhoz, D.B.; Carvalho, L.S.F.; Venancio, F.N.C.; Rangel de Almeida, O.L.; Quinaglia e Silva, J.C.; Coelho-Filho, O.R.; Nadruz, W.; Sposito, A.C. Statin Use in the Early Phase of ST-Segment Elevation Myocardial Infarction Is Associated with Decreased QTc Dispersion. J. Cardiovasc. Pharmacol. Ther. 2020, 25, 226–231. [Google Scholar] [CrossRef]
- Mitchell, L.B.; Powell, J.L.; Gillis, A.M.; Kehl, V.; Hallstrom, A.P. Are lipid-lowering drugs also antiarrhythmic drugs? An analysis of the Antiarrhythmics Versus Implantable Defibrillators (AVID) trial. J. Am. Coll. Cardiol. 2003, 42, 81–87. [Google Scholar] [CrossRef] [Green Version]
- Mohammed, K.S.; Kowey, P.R.; Musco, S. Adjuvant therapy for atrial fibrillation. Future Cardiol. 2010, 6, 67–81. [Google Scholar] [CrossRef]
- Okumus, T.; Pala, A.A.; Taner, T.; Aydin, U. Effects of preoperative statin on the frequency of ventricular fibrillation and c-reactive protein level in patients undergoing isolated coronary artery bypass grafting. J. Coll. Physicians Surg. Pak. 2021, 31, 373–378. [Google Scholar] [CrossRef]
- Bacova, B.; Radosinska, J.; Knezl, V.; Kolenova, L.; Weismann, P.; Navarova, J.; Barancik, M.; Mitasikova, M.; Tribulova, N. Omega-3 fatty acids and atorvastatin suppress ventricular fibrillation inducibility in hypertriglyceridemic rat hearts: Implication of intercellular coupling protein, connexin-43. J. Physiol. Pharmacol. 2010, 61, 717–723. [Google Scholar]
- Benova, T.; Knezl, V.; Viczenczova, C.; Bacova, B.S.; Radosinska, J.; Tribulova, N. Acute anti-fibrillating and defibrillating potential of atorvastatin, melatonin, eicosapentaenoic acid and docosahexaenoic acid demonstrated in isolated heart model. J. Physiol. Pharmacol. 2015, 66, 83–89. [Google Scholar] [PubMed]
- Chou, C.-C.; Lee, H.-L.; Huang, Y.-C.; Wo, H.-T.; Wen, M.-S.; Chu, Y.; Chang, P.-C. Single Bolus Rosuvastatin Accelerates Calcium Uptake and Attenuates Conduction Inhomogeneity in Failing Rabbit Hearts With Regional Ischemia–Reperfusion Injury. J. Cardiovasc. Pharmacol. 2020, 75, 64–74. [Google Scholar] [CrossRef]
- Bian, B.; Yu, X.; Wang, Q.; Teng, T.; Nie, J. Atorvastatin protects myocardium against ischemia–reperfusion arrhythmia by increasing Connexin 43 expression: A rat model. Eur. J. Pharmacol. 2015, 768, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Liptak, B.; Knezl, V.; Gasparova, Z. Anti-arrhythmic and cardio-protective effects of atorvastatin and a potent pyridoindole derivative on isolated hearts from rats with metabolic syndrome. Bratisl. Med. J. 2019, 120, 200–206. [Google Scholar] [CrossRef]
- Yang, N.; Cheng, W.; Hu, H.; Xue, M.; Li, X.; Wang, Y.; Xuan, Y.; Li, X.; Yin, J.; Shi, Y.; et al. Atorvastatin attenuates sympathetic hyperinnervation together with the augmentation of M2 macrophages in rats postmyocardial infarction. Cardiovasc. Ther. 2016, 34, 234–244. [Google Scholar] [CrossRef]
- Najjari, M.; Vaezi, G.; Hojati, V.; Mousavi, Z.; Bakhtiarian, A.; Nikoui, V. Involvement of IL-1β and IL-6 in antiarrhythmic properties of atorvastatin in ouabain-induced arrhythmia in rats. Immunopharmacol. Immunotoxicol. 2018, 40, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, Y.T.; Shan, Z.L.; Guo, H.Y.; Guan, Y.; Yuan, H.T. Role of inflammation in the initiation and maintenance of atrial fibrillation and the protective effect of atorvastatin in a goat model of aseptic pericarditis. Mol. Med. Rep. 2015, 11, 2615–2623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maguy, A.; Hebert, T.E.; Nattel, S. Involvement of lipid rafts and caveolae in cardiac ion channel function. Cardiovasc. Res. 2006, 69, 798–807. [Google Scholar] [CrossRef] [Green Version]
- Balycheva, M.; Faggian, G.; Glukhov, A.V.; Gorelik, J. Microdomain–specific localization of functional ion channels in cardiomyocytes: An emerging concept of local regulation and remodelling. Biophys. Rev. 2015, 7, 43–62. [Google Scholar] [CrossRef] [Green Version]
- Redondo-Morata, L.; Lea Sanford, R.; Andersen, O.S.; Scheuring, S. Effect of Statins on the Nanomechanical Properties of Supported Lipid Bilayers. Biophys. J. 2016, 111, 363–372. [Google Scholar] [CrossRef] [Green Version]
- Ding, C.; Fu, X.H.; He, Z.S.; Chen, H.X.; Xue, L.; Li, J.X. Cardioprotective effects of simvastatin on reversing electrical remodeling induced by myocardial ischemia-reperfusion in normocholesterolemic rabbits. Chin. Med. J. 2008, 121, 551–556. [Google Scholar] [CrossRef]
- Oesterle, A.; Liao, J.K. The Pleiotropic Effects of Statins—From Coronary Artery Disease and Stroke to Atrial Fibrillation and Ventricular Tachyarrhythmia. Curr. Vasc. Pharmacol. 2018, 17, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Kong, L.; Qi, S.; Wang, D. Atorvastatin blocks increased l-type Ca2+ current and cell injury elicited by angiotensin II via inhibiting oxide stress. Acta Biochim. Biophys. Sin. 2016, 48, 378–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, Y.; Li, B.; Wang, J.; Li, X. Rosuvastatin Alleviates Type 2 Diabetic Atrial Structural and Calcium Channel Remodeling. J. Cardiovasc. Pharmacol. 2016, 67, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Venturi, E.; Lindsay, C.; Lotteau, S.; Yang, Z.; Steer, E.; Witschas, K.; Wilson, A.D.; Wickens, J.R.; Russell, A.J.; Steele, D.; et al. Simvastatin activates single skeletal RyR1 channels but exerts more complex regulation of the cardiac RyR2 isoform. Br. J. Pharmacol. 2018, 175, 938–952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haseeb, M.; Thompson, P.D. The effect of statins on RyR and RyR-associated disease. J. Appl. Physiol. 2021, 131, 661–671. [Google Scholar] [CrossRef]
- Cho, K.I.; Cha, T.J.; Lee, S.J.; Shim, I.K.; Zhang, Y.H.; Heo, J.H.; Kim, H.S.; Kim, S.J.; Kim, K.L.; Lee, J.W. Attenuation of acetylcholine activated potassium current (IKACh) by simvastatin, not pravastatin in mouse atrial cardiomyocyte: Possible atrial fibrillation preventing effects of statin. PLoS ONE 2014, 9, e106570. [Google Scholar] [CrossRef]
- Jin, H.; Welzig, C.M.; Aronovitz, M.; Noubary, F.; Blanton, R.; Wang, B.; Rajab, M.; Albano, A.; Link, M.S.; Noujaim, S.F.; et al. QRS/T-wave and calcium alternans in a type I diabetic mouse model for spontaneous postmyocardial infarction ventricular tachycardia: A mechanism for the antiarrhythmic effect of statins. Heart Rhythm 2017, 14, 1406–1416. [Google Scholar] [CrossRef]
- Kisvári, G.; Kovács, M.; Gardi, J.; Seprényi, G.; Kaszaki, J.; Végh, Á. The effect of acute simvastatin administration on the severity of arrhythmias resulting from ischaemia and reperfusion in the canine: Is there a role for nitric oxide? Eur. J. Pharmacol. 2014, 732, 96–104. [Google Scholar] [CrossRef] [Green Version]
- Kisvári, G.; Kovács, M.; Seprényi, G.; Végh, Á. The activation of PI 3-kinase/Akt pathway is involved in the acute effects of simvastatin against ischaemia and reperfusion-induced arrhythmias in anaesthetised dogs. Eur. J. Pharmacol. 2015, 769, 185–194. [Google Scholar] [CrossRef] [Green Version]
- Kura, B.; Kalocayova, B.; Bacova, B.S.; Fulop, M.; Sagatova, A.; Sykora, M.; Andelova, K.; Abuawad, Z.; Slezak, J. The effect of selected drugs on the mitigation of myocardial injury caused by gamma radiation. Can. J. Physiol. Pharmacol. 2021, 99, 80–88. [Google Scholar] [CrossRef]
- Li, H.; Wan, Z.; Li, X.; Teng, T.; Du, X.; Nie, J. Effects of atorvastatin on time-dependent change of fast sodium current in simulated acute ischaemic ventricular myocytes. Cardiovasc. J. Afr. 2019, 30, 268–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nie, J.; Wang, G.; Zhao, G.; Du, X.; Zhang, L.; Yang, Q. Effects of Atorvastatin on Transient Sodium Currents in Rat Normal, Simulated Ischemia, and Reperfusion Ventricular Myocytes. Pharmacology 2020, 105, 320–328. [Google Scholar] [CrossRef]
- Li, H.; Wang, Y.; Liu, J.; Chen, X.; Duan, Y.; Wang, X.; Shen, Y.; Kuang, Y.; Zhuang, T.; Tomlinson, B.; et al. Endothelial Klf2-Foxp1-TGFβ signal mediates the inhibitory effects of simvastatin on maladaptive cardiac remodeling. Theranostics 2021, 11, 1609–1625. [Google Scholar] [CrossRef]
- Yeh, Y.H.; Kuo, C.T.; Chang, G.J.; Chen, Y.H.; Lai, Y.J.; Cheng, M.L.; Chen, W.J. Rosuvastatin suppresses atrial tachycardia-induced cellular remodeling via Akt/Nrf2/heme oxygenase-1 pathway. J. Mol. Cell. Cardiol. 2015, 82, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Qi, X.; Dang, Y.; Li, Y.; Song, X.; Hao, X. Effects of atorvastatin on atrial remodeling in a rabbit model of atrial fibrillation produced by rapid atrial pacing. BMC Cardiovasc. Disord. 2016, 16, 142. [Google Scholar] [CrossRef] [Green Version]
- Roy, J.; Le Guennec, J.Y. Cardioprotective effects of omega 3 fatty acids: Origin of the variability. J. Muscle Res. Cell Motil. 2017, 38, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Allaire, J.; Couture, P.; Leclerc, M.; Charest, A.; Marin, J.; Lépine, M.C.; Talbot, D.; Tchernof, A.; Lamarche, B. A randomized, crossover, head-to-head comparison of eicosapentaenoic acid and docosahexaenoic acid supplementation to reduce inflammation markers in men and women: The Comparing EPA to DHA (ComparED) Study. Am. J. Clin. Nutr. 2016, 104, 280–287. [Google Scholar] [CrossRef]
- Nelson, J.R.; Budoff, M.J.; Wani, O.R.; Le, V.; Patel, D.K.; Nelson, A.; Nemiroff, R.L. EPA’s pleiotropic mechanisms of action: A narrative review. Postgrad. Med. 2021, 133, 651–664. [Google Scholar] [CrossRef]
- Miralles-Pérez, B.; Méndez, L.; Nogués, M.R.; Sánchez-Martos, V.; Fortuño-Mar, À.; Ramos-Romero, S.; Hereu, M.; Medina, I.; Romeu, M. Effects of a fish oil rich in docosahexaenoic acid on cardiometabolic risk factors and oxidative stress in healthy rats. Mar. Drugs 2021, 19, 555. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.T.; Chen, S.Y.; Wu, D.W.; Lee, C.C.; Lee, T.M. Effect of icosapent ethyl on susceptibility to ventricular arrhythmias in postinfarcted rat hearts: Role of GPR120-mediated connexin43 phosphorylation. J. Cell. Mol. Med. 2020, 24, 9267–9279. [Google Scholar] [CrossRef] [PubMed]
- Mauerhofer, C.; Grumet, L.; Schemmer, P.; Leber, B.; Stiegler, P. Combating ischemia-reperfusion injury with micronutrients and natural compounds during solid organ transplantation: Data of clinical trials and lessons of preclinical findings. Int. J. Mol. Sci. 2021, 22, 10675. [Google Scholar] [CrossRef] [PubMed]
- Bacova, B.S.; Radosinska, J.; Wallukat, G.; Barancik, M.; Wallukat, A.; Knezl, V.; Sykora, M.; Paulis, L.; Tribulova, N. Suppression of β1-adrenoceptor autoantibodies is involved in the antiarrhythmic effects of omega-3 fatty acids in male and female hypertensive rats. Int. J. Mol. Sci. 2020, 21, 526. [Google Scholar] [CrossRef] [Green Version]
- Bačová, B.; Seč, P.; Radošinská, J.; Čertík, M.; Vachulová, A.; Tribulová, N. Lower Omega-3 index is a marker of increased propensity of hypertensive rat heart to malignant arrhythmias. Physiol. Res. 2013, 62, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Bacova, B.S.; Viczenczova, C.; Andelova, K.; Sykora, M.; Chaudagar, K.; Barancik, M.; Adamcova, M.; Knezl, V.; Benova, T.E.; Weismann, P.; et al. Antiarrhythmic effects of melatonin and omega-3 are linked with protection of myocardial cx43 topology and suppression of fibrosis in catecholamine stressed normotensive and hypertensive rats. Antioxidants 2020, 9, 546. [Google Scholar] [CrossRef]
- Egan Benova, T.; Viczenczova, C.; Szeiffova Bacova, B.; Knezl, V.; Dosenko, V.; Rauchova, H.; Zeman, M.; Reiter, R.J.; Tribulova, N. Obesity-associated alterations in cardiac connexin-43 and PKC signaling are attenuated by melatonin and omega-3 fatty acids in female rats. Mol. Cell. Biochem. 2019, 454, 191–202. [Google Scholar] [CrossRef]
- Packer, M. Drugs That Ameliorate Epicardial Adipose Tissue Inflammation May Have Discordant Effects in Heart Failure With a Preserved Ejection Fraction as Compared With a Reduced Ejection Fraction. J. Card. Fail. 2019, 25, 986–1003. [Google Scholar] [CrossRef]
- Dinicolantonio, J.J.; Okeefe, J. The benefits of marine omega-3s for preventing arrhythmias. Open Heart 2020, 7, 3–7. [Google Scholar] [CrossRef] [Green Version]
- Asfaw, A.; Minhas, S.; Khouzam, A.R.; Khouzam, N.R.; Khouzam, R.N. Fish Oil Dilemma: Does It Increase the Risk of Ventricular Arrhythmias and Death? Can Fish Oil Kill You? Curr. Probl. Cardiol. 2021, 46, 100718. [Google Scholar] [CrossRef]
- Aarsetøy, H.; Pönitz, V.; Nilsen, O.B.; Grundt, H.; Harris, W.S.; Nilsen, D.W.T. Low levels of cellular omega-3 increase the risk of ventricular fibrillation during the acute ischaemic phase of a myocardial infarction. Resuscitation 2008, 78, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Rauch, B.; Senges, J. The effects of supplementation with omega-3 polyunsaturated fatty acids on cardiac rhythm: Anti-arrhythmic, pro-arrhythmic, both or neither? It depends. Front. Physiol. 2012, 3, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Schacky, C. Omega-3 fatty acids: Anti-arrhythmic, pro-arrhythmic, or both? Front. Physiol. 2008, 11, 94–99. [Google Scholar] [CrossRef] [Green Version]
- Albert, C.M.; Cook, N.R.; Pester, J.; Moorthy, M.V.; Ridge, C.; Danik, J.S.; Gencer, B.; Siddiqi, H.K.; Ng, C.; Gibson, H.; et al. Effect of Marine Omega-3 Fatty Acid and Vitamin D Supplementation on Incident Atrial Fibrillation: A Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2021, 325, 1061–1073. [Google Scholar] [CrossRef]
- Buchhorn, R.; Willaschek, C. Resolution of a therapy-resistant focal atrial tachycardia after omega-3 fatty acid supplementation. Cardiol. Young 2019, 29, 989–992. [Google Scholar] [CrossRef]
- Buchhorn, R.; Baumann, C.; Willaschek, C. Alleviation of arrhythmia burden in children with frequent idiopathic premature ventricular contractions by omega-3-fatty acid supplementation. Int. J. Cardiol. 2019, 291, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Oner, T.; Ozdemir, R.; Doksöz, O.; Genc, D.B.; Guven, B.; Demirpence, S.; Yilmazer, M.M.; Yozgat, Y.; Mese, T.; Tavli, V. Cardiac function in children with premature ventricular contractions: The effect of omega-3 polyunsaturated fatty acid supplementation. Cardiol. Young 2018, 28, 949–954. [Google Scholar] [CrossRef]
- Colussi, G.L.; Catena, C.; Fagotto, V.; Darsiè, D.; Brosolo, G.; Bertin, N.; Sechi, L.A. Atrial fibrillation and its complications in arterial hypertension: The potential preventive role of ω-3 polyunsaturated fatty acids. Crit. Rev. Food Sci. Nutr. 2019, 59, 1937–1948. [Google Scholar] [CrossRef] [PubMed]
- Feguri, G.R.; de Lima, P.R.L.; Franco, A.C.; De La Cruz, F.R.H.; Borges, D.C.; Toledo, L.R.; Segri, N.J.; Eduardo de Aguilar-Nascimento, J. Benefits of fasting abbreviation with carbohydrates and omega-3 infusion during CABG: A double-blind controlled randomized trial. Braz. J. Cardiovasc. Surg. 2019, 34, 125–135. [Google Scholar] [CrossRef]
- Hashimoto, T.; Ako, J.; Nakao, K.; Ozaki, Y.; Kimura, K.; Noguchi, T.; Yasuda, S.; Suwa, S.; Fujimoto, K.; Nakama, Y.; et al. A lower eicosapentaenoic acid/arachidonic acid ratio is associated with in-hospital fatal arrhythmic events in patients with acute myocardial infarction: A J-MINUET substudy. Heart Vessel. 2018, 33, 481–488. [Google Scholar] [CrossRef]
- Bäck, M.; Yurdagul, A.; Tabas, I.; Öörni, K.; Kovanen, P.T. Inflammation and its resolution in atherosclerosis: Mediators and therapeutic opportunities. Nat. Rev. Cardiol. 2019, 16, 389–406. [Google Scholar] [CrossRef] [PubMed]
- Demaison, L.; Leger, T.; Vergely, C.; Rochette, L.; Azarnoush, K. About the controversies of the cardioprotective effect of n-3 polyunsaturated fatty acids (PUFAs) between animal studies and clinical meta-analyses: A review with several strategies to enhance the beneficial effects of n-3 PUFAs. J. Physiol. Biochem. 2019, 75, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Billman, G.E. The effects of omega-3 polyunsaturated fatty acids on cardiac rhythm: A critical reassessment. Pharmacol. Ther. 2013, 140, 53–80. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Cook, N.R.; Lee, I.-M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Albert, C.M.; Gordon, D.; Copeland, T.; et al. Marine n−3 Fatty Acids and Prevention of Cardiovascular Disease and Cancer. N. Engl. J. Med. 2019, 380, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.U.; Lone, A.N.; Khan, M.S.; Virani, S.S.; Blumenthal, R.S.; Nasir, K.; Miller, M.; Michos, E.D.; Ballantyne, C.M.; Boden, W.E.; et al. Effect of omega-3 fatty acids on cardiovascular outcomes: A systematic review and meta-analysis. eClinicalMedicine 2021, 38, 100997. [Google Scholar] [CrossRef]
- Nodari, S.; Triggiani, M.; Campia, U.; Cas, L.D. Omega-3 polyunsaturated fatty acid supplementation: Mechanism and current evidence in atrial fibrillation. J. Atr. Fibrillation 2012, 5, 49–63. [Google Scholar] [CrossRef]
- Ruijter, H.M.D.; Berecki, G.; Verkerk, A.O.; Bakker, D.; Baartscheer, A.; Schumacher, C.A.; Belterman, C.N.W.; DeJonge, N.; Fiolet, J.W.T.; Brouwer, I.A.; et al. Acute administration of fish oil inhibits triggered activity in isolated myocytes from rabbits and patients with heart failure. Circulation 2008, 117, 536–544. [Google Scholar] [CrossRef] [Green Version]
- Mollace, V.; Gliozzi, M.; Carresi, C.; Musolino, V.; Oppedisano, F. Re-assessing the mechanism of action of n-3 PUFAs. Int. J. Cardiol. 2013, 170, S8. [Google Scholar] [CrossRef]
- Baum, J.R.; Dolmatova, E.; Tan, A.; Duffy, H.S. Omega 3 fatty acid inhibition of inflammatory cytokine-mediated Connexin43 regulation in the heart. Front. Physiol. 2012, 3, 272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calder, P.C. Mechanisms of action of (n-3) fatty acids. J. Nutr. 2012, 142, 592S–599S. [Google Scholar] [CrossRef] [Green Version]
- Song, Y.J.; Dong, P.S.; Wang, H.L.; Zhu, J.H.; Xing, S.Y.; Han, Y.H.; Wang, R.X.; Jiang, W.P. Regulatory functions of docosahexaenoic acid on ion channels in rat ventricular myocytes. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 2632–2638. [Google Scholar]
- McLennan, P.L. Cardiac physiology and clinical efficacy of dietary fish oil clarified through cellular mechanisms of omega-3 polyunsaturated fatty acids. Eur. J. Appl. Physiol. 2014, 114, 1333–1356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Endo, J.; Arita, M. Cardioprotective mechanism of omega-3 polyunsaturated fatty acids. J. Cardiol. 2016, 67, 22–27. [Google Scholar] [CrossRef] [Green Version]
- Den Ruijter, H.M.; Verkerk, A.O.; Coronel, R. Incorporated fish oil fatty acids prevent action potential shortening induced by circulating fish oil fatty acids. Front. Physiol. 2010, 1, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siddiqui, R.A.; Harvey, K.A.; Zaloga, G.P. Modulation of enzymatic activities by n-3 polyunsaturated fatty acids to support cardiovascular health. J. Nutr. Biochem. 2008, 19, 417–437. [Google Scholar] [CrossRef] [PubMed]
- Suenari, K.; Chen, Y.C.; Kao, Y.H.; Cheng, C.C.; Lin, Y.K.; Kihara, Y.; Chen, Y.J.; Chen, S.A. Eicosapentaenoic acid reduces the pulmonary vein arrhythmias through nitric oxide. Life Sci. 2011, 89, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Borghi, C.; Pareo, I. Omega-3 in antiarrhythmic therapy: Cons position. High. Blood Press. Cardiovasc. Prev. 2012, 19, 207–211. [Google Scholar] [CrossRef]
- Verkerk, A.O.; den Ruijter, H.M.; de Jonge, N.; Coronel, R. Fish oil curtails the human action potential dome in a heterogeneous manner: Implication for arrhythmogenesis. Int. J. Cardiol. 2009, 132, 138–140. [Google Scholar] [CrossRef]
- Wang, R.X.; Li, X.R.; Guo, T.; Sun, L.P.; Guo, S.X.; Yang, Z.Y.; Yang, X.J.; Jiang, W.P. Docosahexaenoic acid has influence on action potentials and transient outward potassium currents of ventricular myocytes. Lipids Health Dis. 2010, 9, 39. [Google Scholar] [CrossRef] [Green Version]
- van Borren, M.M.G.J.; den Ruijter, H.M.; Baartscheer, A.; Ravesloot, J.H.; Coronel, R.; Verkerk, A.O. Dietary omega-3 polyunsaturated fatty acids suppress NHE-1 upregulation in a rabbit model of volume-and pressure-overload. Front. Physiol. 2012, 3, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Pignier, C.; Revenaz, C.; Rauly-Lestienne, I.; Cussac, D.; Delhon, A.; Gardette, J.; Grand, B. Direct protective effects of poly-unsaturated fatty acids, DHA and EPA, against activation of cardiac late sodium current: A mechanism for ischemia selectivity. Basic Res. Cardiol. 2007, 102, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Moreno, C.; De La Cruz, A.; Oliveras, A.; Kharche, S.R.; Guizy, M.; Comes, N.; Starý, T.; Ronchi, C.; Rocchetti, M.; Baró, I.; et al. Marine n-3 PUFAs modulate IKs gating, channel expression, and location in membrane microdomains. Cardiovasc. Res. 2015, 105, 223–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohrbach, S. Effects of Dietary Polyunsaturated Fatty Acids on Mitochondria. Curr. Pharm. Des. 2009, 15, 4103–4116. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andelova, K.; Bacova, B.S.; Sykora, M.; Hlivak, P.; Barancik, M.; Tribulova, N. Mechanisms Underlying Antiarrhythmic Properties of Cardioprotective Agents Impacting Inflammation and Oxidative Stress. Int. J. Mol. Sci. 2022, 23, 1416. https://doi.org/10.3390/ijms23031416
Andelova K, Bacova BS, Sykora M, Hlivak P, Barancik M, Tribulova N. Mechanisms Underlying Antiarrhythmic Properties of Cardioprotective Agents Impacting Inflammation and Oxidative Stress. International Journal of Molecular Sciences. 2022; 23(3):1416. https://doi.org/10.3390/ijms23031416
Chicago/Turabian StyleAndelova, Katarina, Barbara Szeiffova Bacova, Matus Sykora, Peter Hlivak, Miroslav Barancik, and Narcis Tribulova. 2022. "Mechanisms Underlying Antiarrhythmic Properties of Cardioprotective Agents Impacting Inflammation and Oxidative Stress" International Journal of Molecular Sciences 23, no. 3: 1416. https://doi.org/10.3390/ijms23031416
APA StyleAndelova, K., Bacova, B. S., Sykora, M., Hlivak, P., Barancik, M., & Tribulova, N. (2022). Mechanisms Underlying Antiarrhythmic Properties of Cardioprotective Agents Impacting Inflammation and Oxidative Stress. International Journal of Molecular Sciences, 23(3), 1416. https://doi.org/10.3390/ijms23031416






