Should Degenerated Intervertebral Discs of Patients with Modic Type 1 Changes Be Treated with Mesenchymal Stem Cells?
Abstract
:1. Introduction
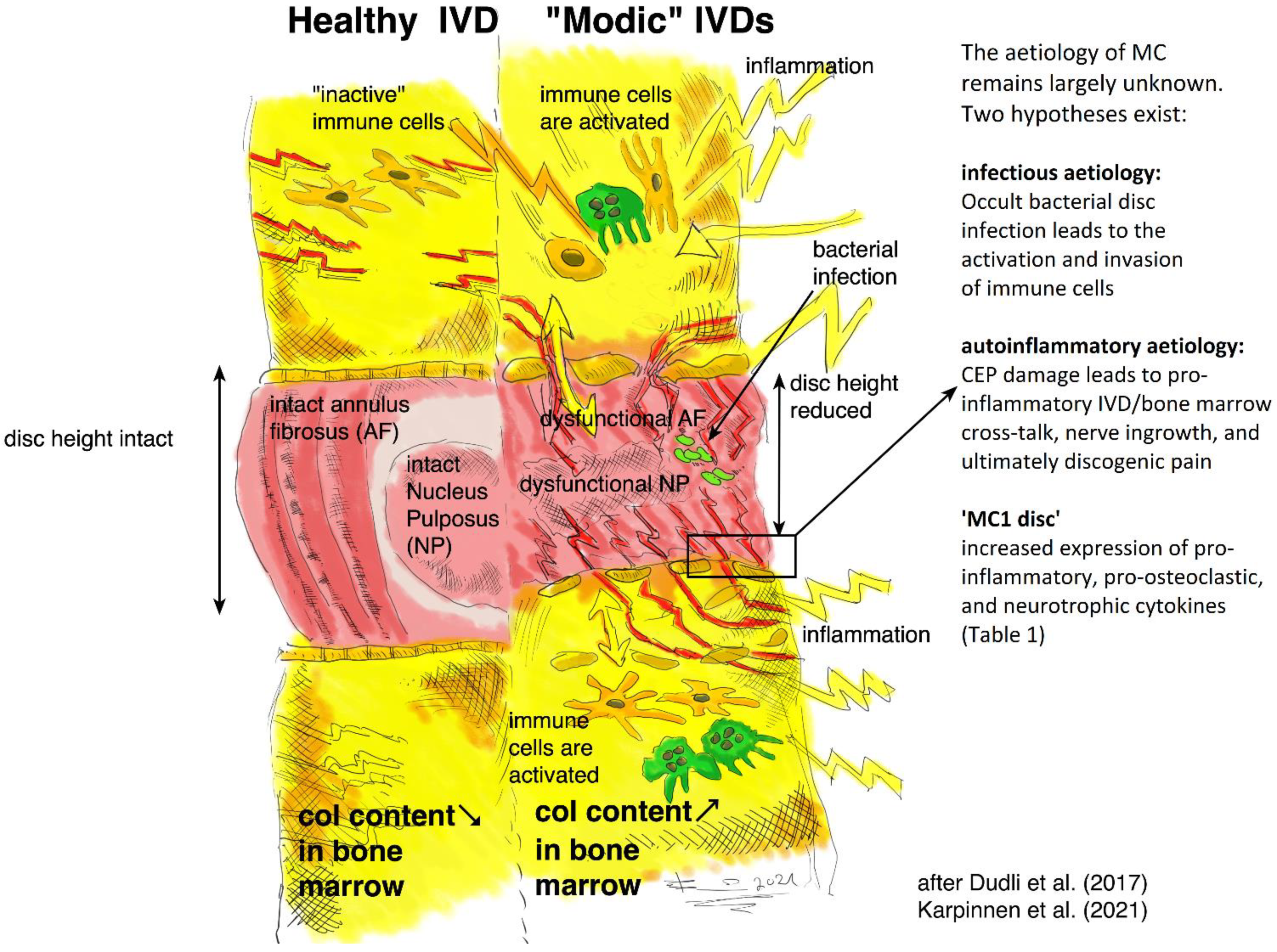
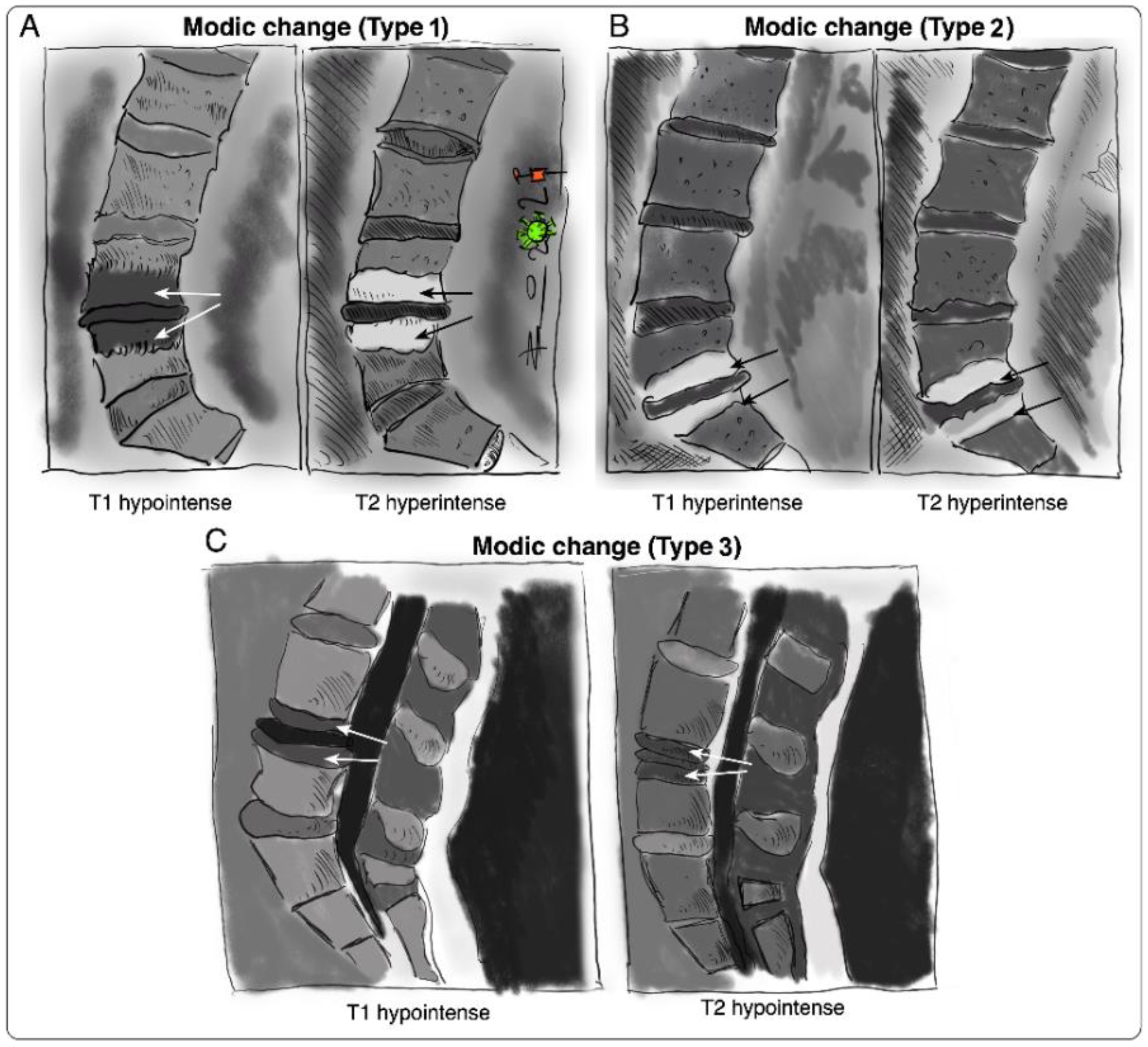
Modic Changes
2. Clinical Trials for MC
| Clinical Trial/Study | Year | Aim | Treatment | Phase and Design | Inclusion Criteria | Number of Patients | Status and Outcome | Outcome Measures | References |
|---|---|---|---|---|---|---|---|---|---|
| Antibiotics in Modic changes (AIM) NCT02323412 | 2015 2018 | Effects of amoxicillin in CLBP patients with MC at the disc herniation level | Amoxicillin 750 mg three times a day for three months | Phase III. Double-blind, multicenter, randomized, placebo-controlled | CLBP patients with disc herniation and MC1 and/or MC2 at the same level | 180 | Completed Without clinically important benefit |
| [47,48] |
| Antibiotic treatment of patients with low back pain NCT00302796 | 2006 2010 | Effect of antibiotics in CLBP patients with MC1 | Amoxicillin-clavulanate (500/125 mg) three times a day for 100 days | Phase IV. Double-blind, randomized, placebo-controlled | CLBP patients with disc herniation and MC1 | 162 | Completed Clinically important benefit |
| [49] |
| Antibiotic treatment for the management of CLBP ACTRN12615000958583 | 2015 | Efficacy of antibiotics in a broader subgroup of CLBP patients with disc herniation | Amoxicillin-clavulanate (500/125 mg) two times per day for 90 days | Double-blind, randomized, placebo-controlled | CLBP patients with disc herniation—with and without MC1 and MC2 | 170 | Recruiting |
| [71] |
| Antibiotic treatment of CLBP patients with MC1 | 2016 | Efficacy of antibiotic treatment of CLBP patients with MC1 | Amoxicillin-clavulanate (500/125 mg) three times a day for 100 days | Prospective, open-label | CLBP patients with MC1 | 28 | Completed No clinically important benefit |
| [51] |
| Antibiotics in CLBP patients with MC1 | 2014 | Efficacy of antibiotics in CLBP patients with MC1 | Amoxicillin-clavulanate (500/125 mg) two times per day for 100 days | Randomized, placebo-controlled | CLBP patients with disc herniation and MC1 | 71 | Completed Clinically important benefit |
| [50] |
| PP353 for CLBP patients with MC1 NCT04238676 | 2020 | Safety, tolerability, and efficacy of PP353 | Intradiscal injection of the antibiotic PP353 | Phase I/II. Randomized, placebo-controlled | CLBP patients with MC1 | 43 | Recruiting |
| - |
| The efficacy of Zoledronic Acid in MC-related LBP NCT01330238 | 2008 2011 | Efficacy of Zoledronic Acid in patients with CLBP and MC | Single infusion of 5 mg zoledronic acid | Phase II. Double-blind, randomized, placebo-controlled | CLBP patients with MC1 or MC2 | 40 | Completed Reduced LBP and faster MC1 conversion to MC2 |
| [42,43] |
| Intradiscal steroid injection in CLBP with inflammatory MC | 2007 | Association between MC severity and response to intradiscal steroid injection | Intradiscal injection of 25 mg prednisolone acetate | Retrospective | CLBP patients with MC1, MC1/2, or MC2 | 74 | Completed Significant short-term benefit |
| [39] |
| Intradiscal steroid therapy for CLBP patients with MC | 2011 | Efficacy of various intradiscal steroid injection regimens for CLBP patients with MC | Intradiscal injection of normal saline, disprospan, or disprospan and songmeile | Double-blinded, randomized, placebo-controlled, prospective | CLBP patients with MC and positive discography | 120 | Completed Significant short-term benefit |
| [40] |
| Intradiscal steroid injection in CLBP patients with MC1 | 2012 | Efficacy of intradiscal steroid injection on CLBP patients with MC1 | Intradiscal injection of methylprednisolone | Retrospective | CLBP patients with and without MC1 | 97 | Completed Significant short-term benefit |
| [41] |
| Intradiscal glucocorticoid injection for CLBP patients with active discopathy NCT00804531 | 2017 | Efficacy of single intradiscal glucocorticoid injection in CLBP patients and active discopathy | Single intradiscal injection of 25 mg prednisolone acetate | Phase IV. Prospective, parallel-group, double-blind, randomized, placebo-controlled | CLBP patients with active discopathy | 135 | Completed Significant short-term benefit with no long-term benefit |
| [54] |
| Epidural steroid injections in discogenic LBP NCT04930211 | 2020 | Effectiveness of epidural steroid injections in DDD patients with/without MC1 | Transforaminal epidural steroid injection of dexamethasone-lidocaine | Non-randomized without placebo | CLBP patients with/without MC1 | 40 | Recruiting |
| - |
| BackToBasic: Infliximab in CLBP and MCs NCT03704363 | 2018 | Efficacy of Infliximab in CLBP with MCs | Four intravenous Infliximab infusions (5 mg/kg) | Phase III. Double-blind, multicenter, randomized, placebo-controlled | CLBP patients with MC1 | 126 | Recruiting |
| [58] |
| Intradiscal injection of PRP for CLBP patients with MC1 NCT03712527 | 2018 | Efficacy of intradiscal PRP injection at 3 months | Single intradiscal PRP injection versus normal saline | Randomized, placebo-controlled | Patients with at least 3 months LBP with MC1 | 126 | Recruiting |
| - |
3. MSC Therapy for DDD
3.1. Regenerative Mode of Action
3.1.1. Nutrient and Oxygen Deficiency
3.1.2. Acidity
3.1.3. Hyperosmolarity
3.2. Immunomodulatory Mode of Action
3.3. Immunomodulatory vs. Regenerative Mode of Action in DDD
4. Patient Stratification: MSC Therapy for DDD Patients with MC1
5. Possible Mode of Action of MSCs in MC1
6. PRO—MSCs for Patients with MC1
7. CONTRA—MSCs for Patients with MC1
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AF | annulus fibrosus |
| BDNF | brain-derived neurotrophic factor |
| CCL2 | C-C motif chemokine ligand 2 |
| CEP | cartilage endplate |
| CLBP | chronic low back pain |
| CXCL5 | C-X-C motif chemokine ligand 5 |
| DD | disc degeneration |
| DDD | degenerative disc disease |
| ECM | extracellular matrix |
| EGF | epidermal growth factor |
| GDF-7 | growth differentiation factor-7 |
| GM-CSF | granulocyte-macrophage colony-stimulating factor |
| ICAM-1 | intercellular adhesion molecule-1 |
| IDO | indoleamine 2,3 dioxygenase |
| IFN-γ | interferon-gamma |
| IGF-1 | insulin-like growth factor-1 |
| IL-1α | interleukin-1 alpha |
| IL-1β | interleukin-1 beta |
| IL-6 | interleukin-6 |
| IL-8 | interleukin-8 |
| IL-17 | interleukin-17 |
| IVD | intervertebral disc |
| IVDC | intervertebral disc cell |
| LBP | low back pain |
| MC | Modic changes |
| MC1 | Modic type 1 changes |
| MC2 | Modic type 2 changes |
| MC3 | Modic type 3 changes |
| M-CSF | macrophage colony-stimulating factor |
| MRI | magnetic resonance imaging |
| MSC | mesenchymal stem cell |
| NGF | nerve growth factor |
| NO | nitric oxide |
| NP | nucleus pulposus |
| NPC | nucleus pulposus cell |
| NTRK1 | neurotrophic receptor tyrosine kinase 1 |
| OPG | osteoprotegerin |
| OP-1 | osteogenic protein-1 |
| OSCAR | osteoclast associated Ig-like receptor |
| PGE2 | prostaglandin E2 |
| PRP | platelet-rich plasma |
| RANKL | tumor necrosis superfamily member 11 |
| RUNX1 | runt-related transcription factor 1 |
| RUNX2 | runt-related transcription factor 2 |
| TGF-β | transforming growth factor-beta |
| TNF-α | tumor necrosis factor-alpha |
| TrkA | neurotrophic receptor tyrosine kinase 1 |
| TSG-6 | tumor necrosis factor-alpha-inducible protein 6 |
| VEGF | vascular endothelial growth factor |
| ZA | zoledronic acid |
References
- Binch, A.L.A.; Fitzgerald, J.C.; Growney, E.A.; Barry, F. Cell-based strategies for IVD repair: Clinical progress and translational obstacles. Nat. Rev. Rheumatol. 2021, 17, 158–175. [Google Scholar] [CrossRef]
- Cheung, K.M.C.; Karppinen, J.; Chan, D.; Ho, D.W.H.; Song, Y.-Q.; Sham, P.; Cheah, K.S.E.; Leong, J.C.Y.; Luk, K.D.K. Prevalence and Pattern of Lumbar Magnetic Resonance Imaging Changes in a Population Study of One Thousand Forty-Three Individuals. Spine 2009, 34, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Brinjikji, W.; Diehn, F.E.; Jarvik, J.G.; Carr, C.M.; Kallmes, D.F.; Murad, M.H.; Luetmer, P.H. MRI Findings of Disc Degeneration are More Prevalent in Adults with Low Back Pain than in Asymptomatic Controls: A Systematic Review and Meta-Analysis. Am. J. Neuroradiol. 2015, 36, 2394–2399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, T.S.; Karppinen, J.; Sorensen, J.S.; Niinimäki, J.; Leboeuf-Yde, C. Vertebral endplate signal changes (Modic change): A systematic literature review of prevalence and association with non-specific low back pain. Eur. Spine J. 2008, 17, 1407–1422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarukado, K.; Ono, T.; Tono, O.; Tanaka, H.; Ikuta, K.; Harimaya, K.; Doi, T. Does Modic Change Progresss with Age? Spine 2017, 42, 1805–1809. [Google Scholar] [CrossRef] [PubMed]
- Kjaer, P.; Korsholm, L.; Bendix, T.; Sorensen, J.S.; Leboeuf-Yde, C. Modic changes and their associations with clinical findings. Eur. Spine J. 2006, 15, 1312–1319. [Google Scholar] [CrossRef] [Green Version]
- Sørlie, A.; Moholdt, V.; Kvistad, K.A.; Nygaard, P.; Ingebrigtsen, T.; Iversen, T.; Kloster, R.; Solberg, T.K. Modic type I changes and recovery of back pain after lumbar microdiscectomy. Eur. Spine J. 2012, 21, 2252–2258. [Google Scholar] [CrossRef] [Green Version]
- Jensen, O.K.; Nielsen, C.V.; Sørensen, J.S.; Stengaard-Pedersen, K. Type 1 Modic changes was a significant risk factor for 1-year outcome in sick-listed low back pain patients: A nested cohort study using magnetic resonance imaging of the lumbar spine. Spine J. 2014, 14, 2568–2581. [Google Scholar] [CrossRef]
- Schistad, E.I.; Espeland, A.; Rygh, L.J.; Røe, C.; Gjerstad, J.; Schistad, E.I.; Espeland, A.; Rygh, L.J.; Røe, C.; Gjerstad, J. The association between Modic changes and pain during 1-year follow-up in patients with lumbar radicular pain. Skelet. Radiol. 2014, 43, 1271–1279. [Google Scholar] [CrossRef]
- Chung, C.B.; Berg, B.C.V.; Tavernier, T.; Cotten, A.; Laredo, J.-D.; Vallee, C.; Malghem, J. End plate marrow changes in the asymptomatic lumbosacral spine: Frequency, distribution and correlation with age and degenerative changes. Skelet. Radiol. 2004, 33, 399–404. [Google Scholar] [CrossRef]
- Bailly, F.; Maigne, J.-Y.; Genevay, S.; Marty, M.; Gandjbakhch, F.; Rozenberg, S.; Foltz, V. Inflammatory pain pattern and pain with lumbar extension associated with Modic 1 changes on MRI: A prospective case–control study of 120 patients. Eur. Spine J. 2013, 23, 493–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Järvinen, J.; Karppinen, J.; Niinimäki, J.; Haapea, M.; Grönblad, M.; Luoma, K.; Rinne, E. Association between changes in lumbar Modic changes and low back symptoms over a two-year period. BMC Musculoskelet. Disord. 2015, 16, 98. [Google Scholar] [CrossRef] [PubMed]
- Weishaupt, D.; Zanetti, M.; Hodler, J.; Min, K.; Fuchs, B.; Pfirrmann, C.W.; Boos, N. Painful Lumbar Disk Derangement: Relevance of Endplate Abnormalities at MR Imaging. Radiology 2001, 218, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Assheuer, J.; Lenz, G.; Lenz, W.; Gottschlich, K.W.; Schulitz, K.P. Fat/Water Separation in the NMR Tomogram. The Imaging of Bone Marrow Reactions in Degenerative Intervertebral Disk Changes. Rofo 1987, 147, 58–63. [Google Scholar] [CrossRef]
- Modic, M.T.; Steinberg, P.M.; Ross, J.S.; Masaryk, T.J.; Carter, J.R. Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging. Radiology 1988, 166, 193–199. [Google Scholar] [CrossRef]
- Jensen, T.S.; Bendix, T.; Sorensen, J.S.; Manniche, C.; Korsholm, L.; Kjaer, P. Characteristics and natural course of vertebral endplate signal (Modic) changes in the Danish general population. BMC Musculoskelet. Disord. 2009, 10, 81. [Google Scholar] [CrossRef] [Green Version]
- Perilli, E.; Parkinson, I.H.; Truong, L.-H.; Chong, K.C.; Fazzalari, N.L.; Osti, O.L. Modic (endplate) changes in the lumbar spine: Bone micro-architecture and remodelling. Eur. Spine J. 2015, 24, 1926–1934. [Google Scholar] [CrossRef] [Green Version]
- Fields, A.J.; Liebenberg, E.C.; Lotz, J.C. Innervation of pathologies in the lumbar vertebral end plate and intervertebral disc. Spine J. 2014, 14, 513–521. [Google Scholar] [CrossRef] [Green Version]
- Dudli, S.; Sing, D.C.; Hu, S.S.; Berven, S.H.; Burch, S.; Deviren, V.; Cheng, I.; Tay, B.K.B.; Alamin, T.F.; Ith, M.A.M.; et al. ISSLS PRIZE IN BASIC SCIENCE 2017: Intervertebral disc/bone marrow cross-talk with Modic changes. Eur. Spine J. 2017, 26, 1362–1373. [Google Scholar] [CrossRef]
- Lotz, J.C.; Fields, A.; Liebenberg, E.C. The Role of the Vertebral End Plate in Low Back Pain. Glob. Spine J. 2013, 3, 153–163. [Google Scholar] [CrossRef] [Green Version]
- Ohtori, S.; Inoue, G.; Ito, T.; Koshi, T.; Ozawa, T.; Doya, H.; Saito, T.; Moriya, H.; Takahashi, K. Tumor Necrosis Factor-Immunoreactive Cells and PGP 9.5-Immunoreactive Nerve Fibers in Vertebral Endplates of Patients With Discogenic Low Back Pain and Modic Type 1 or Type 2 Changes on MRI. Spine 2006, 31, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Farshad-Amacker, N.A.; Hughes, A.; Herzog, R.J.; Seifert, B.; Farshad, M. The intervertebral disc, the endplates and the vertebral bone marrow as a unit in the process of degeneration. Eur. Radiol. 2017, 27, 2507–2520. [Google Scholar] [CrossRef] [PubMed]
- Määttä, J.H.; Rade, M.; Freidin, M.B.; Airaksinen, O.; Karppinen, J.; Williams, F.M.K. Strong association between vertebral endplate defect and Modic change in the general population. Sci. Rep. 2018, 8, 16630. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, S.J.; Ito, K.; Nolte, L.-P. Fluid flow and convective transport of solutes within the intervertebral disc. J. Biomech. 2003, 37, 213–221. [Google Scholar] [CrossRef]
- Rajasekaran, S.; Babu, J.N.; Arun, R.; Armstrong, B.R.W.; Shetty, A.; Murugan, S. ISSLS Prize Winner: A Study of Diffusion in Human Lumbar Discs: A Serial Magnetic Resonance Imaging Study Documenting the Influence of the Endplate on Diffusion in Normal and Degenerate Discs. Spine 2004, 29, 2654–2667. [Google Scholar] [CrossRef] [PubMed]
- Malinin, T.; Brown, M.D. Changes in Vertebral Bodies Adjacent to Acutely Narrowed Intervertebral Discs: Observations in Baboons. Spine 2007, 32, E603–E607. [Google Scholar] [CrossRef]
- Ulrich, J.A.; Liebenberg, E.C.; Thuillier, D.U.; Lotz, J.C. ISSLS Prize Winner: Repeated Disc Injury Causes Persistent Inflammation. Spine 2007, 32, 2812–2819. [Google Scholar] [CrossRef]
- Papuga, M.O.; Proulx, S.; Kwok, E.; You, Z.; Rubery, P.T.; Dougherty, P.E.; Hilton, M.; Awad, H.; Schwarz, E.M. Chronic axial compression of the mouse tail segment induces MRI bone marrow edema changes that correlate with increased marrow vasculature and cellularity. J. Orthop. Res. 2010, 28, 1220–1228. [Google Scholar] [CrossRef] [Green Version]
- Moore, R.J.; Vernon-Roberts, B.; Osti, O.L.; Fraser, R.D. Remodeling of Vertebral Bone After Outer Anular Injury in Sheep. Spine 1996, 21, 936–940. [Google Scholar] [CrossRef]
- Torkki, M.; Majuri, M.-L.; Wolff, H.; Koskelainen, T.; Haapea, M.; Niinimäki, J.; Alenius, H.; Lotz, J.; Karppinen, J. Osteoclast activators are elevated in intervertebral disks with Modic changes among patients operated for herniated nucleus pulposus. Eur. Spine J. 2016, 25, 207–216. [Google Scholar] [CrossRef]
- Burke, J.; Watson, R.; McCormack, D.; Fitzpatrick, J.M.; Stack, J.; Walsh, M. Modic changes are associated with increased disc inflammatory mediator production. Spine J. 2002, 2, 3–4. [Google Scholar] [CrossRef]
- Dudli, S.; Liebenberg, E.; Magnitsky, S.; Lu, B.; Lauricella, M.; Lotz, J.C. Modic type 1 change is an autoimmune response that requires a proinflammatory milieu provided by the ‘Modic disc’. Spine J. 2018, 18, 831–844. [Google Scholar] [CrossRef] [PubMed]
- Dudli, S.; Liebenberg, E.; Magnitsky, S.; Miller, S.; Demir-Deviren, S.; Lotz, J.C. Propionibacterium acnesinfected intervertebral discs cause vertebral bone marrow lesions consistent with Modic changes. J. Orthop. Res. 2016, 34, 1447–1455. [Google Scholar] [CrossRef] [Green Version]
- Geiss, A.; Larsson, K.; Junevik, K.; Rydevik, B.; Olmarker, K. Autologous nucleus pulposus primes T cells to develop into interleukin-4-producing effector cells: An experimental study on the autoimmune properties of nucleus pulposus. J. Orthop. Res. 2008, 27, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Gertzbein, S.D.; Tait, J.H.; Devlin, S.R. The stimulation of lymphocytes by nucleus pulposus in patients with degenerative disk disease of the lumbar spine. Clin. Orthop. Relat. Res. 1976, 123, 149–154. [Google Scholar] [CrossRef]
- Capossela, S.; Schläfli, P.; Bertolo, A.; Janner, T.; Stadler, B.M.; Pötzel, T.; Baur, M.; Stoyanov, J.V. Degenerated human intervertebral discs contain autoantibodies against extracellular matrix proteins. Eur. Cells Mater. 2014, 27, 251–263. [Google Scholar] [CrossRef]
- Capoor, M.N.; Ruzicka, F.; Schmitz, J.E.; James, G.A.; Machackova, T.; Jancalek, R.; Smrcka, M.; Lipina, R.; Ahmed, F.S.; Alamin, T.F.; et al. Propionibacterium acnes biofilm is present in intervertebral discs of patients undergoing microdiscectomy. PLoS ONE 2017, 12, e0174518. [Google Scholar] [CrossRef] [Green Version]
- Gilligan, C.J.; Cohen, S.P.; Fischetti, V.A.; Hirsch, J.A.; Czaplewski, L.G. Chronic low back pain, bacterial infection and treatment with antibiotics. Spine J. 2021, 21, 903–914. [Google Scholar] [CrossRef]
- Manniche, C.; Hall, G.M. Chronic low back pain, Modic changes and low-grade virulent infection: Efficacy of antibiotic treatment. Futur. Sci. OA 2021, 7, FSO703. [Google Scholar] [CrossRef]
- Annen, M.; Peterson, C.; Leemann, S.; Schmid, C.; Anklin, B.; Humphreys, B.K. Comparison of Outcomes in MRI Confirmed Lumbar Disc Herniation Patients With and Without Modic Changes Treated With High Velocity, Low Amplitude Spinal Manipulation. J. Manip. Physiol. Ther. 2016, 39, 200–209. [Google Scholar] [CrossRef] [Green Version]
- Fayad, F.; Lefevre-Colau, M.-M.; Rannou, F.; Quintero, N.; Nys, A.; Macé, Y.; Poiraudeau, S.; Drapé, J.L.; Revel, M. Relation of inflammatory modic changes to intradiscal steroid injection outcome in chronic low back pain. Eur. Spine J. 2007, 16, 925–931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, P.; Jiang, L.; Zhuang, C.; Yang, Y.; Zhang, Z.; Chen, W.; Zheng, T. Intradiscal injection therapy for degenerative chronic discogenic low back pain with end plate Modic changes. Spine J. 2011, 11, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Beaudreuil, J.; Dieude, P.; Poiraudeau, S.; Revel, M. Disabling chronic low back pain with Modic type 1 MRI signal: Acute reduction in pain with intradiscal corticotherapy. Ann. Phys. Rehabil. Med. 2012, 55, 139–147. [Google Scholar] [CrossRef] [Green Version]
- Koivisto, K.; Järvinen, J.; Karppinen, J.; Haapea, M.; Paananen, M.; Kyllönen, E.; Tervonen, O.; Niinimäki, J. The effect of zoledronic acid on type and volume of Modic changes among patients with low back pain. BMC Musculoskelet. Disord. 2017, 18, 274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koivisto, K.; Kyllönen, E.; Haapea, M.; Niinimäki, J.; Sundqvist, K.; Pehkonen, T.; Seitsalo, S.; Tervonen, O.; Karppinen, J. Efficacy of zoledronic acid for chronic low back pain associated with Modic changes in magnetic resonance imaging. BMC Musculoskelet. Disord. 2014, 15, 64. [Google Scholar] [CrossRef] [Green Version]
- Korhonen, T.; Karppinen, J.; Paimela, L.; Malmivaara, A.; Lindgren, K.-A.; Bowman, C.; Hammond, A.; Kirkham, B.; Järvinen, S.; Niinimäki, J.; et al. The Treatment of Disc Herniation-Induced Sciatica With Infliximab: One-Year Follow-up Results of FIRST II, a Randomized Controlled Trial. Spine 2006, 31, 2759–2766. [Google Scholar] [CrossRef] [PubMed]
- Esposito, P.; Pinheiro-Franco, J.; Froelich, S.; Maitrot, D. Predictive value of MRI vertebral end-plate signal changes (MODIC) on outcome of surgically treated degenerative disc disease: Results of a cohort study including 60 patients. Neurochirurgie 2006, 52, 315–322. [Google Scholar] [CrossRef]
- Storheim, K.; Espeland, A.; Grøvle, L.; Skouen, J.S.; Aßmus, J.; Anke, A.; Froholdt, A.; Pedersen, L.M.; Haugen, A.J.; Fors, T.; et al. Antibiotic treatment In patients with chronic low back pain and Modic changes (the AIM study): Study protocol for a randomised controlled trial. Trials 2017, 18, 596. [Google Scholar] [CrossRef] [Green Version]
- Bråten, L.C.H.; Rolfsen, M.P.; Espeland, A.; Wigemyr, M.; Aßmus, J.; Froholdt, A.; Haugen, A.J.; Marchand, G.H.; Kristoffersen, P.M.; Lutro, O.; et al. Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): Double blind, randomised, placebo controlled, multicentre trial. BMJ 2019, 367, l5654. [Google Scholar] [CrossRef] [Green Version]
- Albert, H.B.; Sorensen, J.S.; Christensen, B.S.; Manniche, C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): A double-blind randomized clinical controlled trial of efficacy. Eur. Spine J. 2013, 22, 697–707. [Google Scholar] [CrossRef] [Green Version]
- Al-Falahi, M.A.; Salal, M.H.; Abdul-Wahab, D.M. Antibiotic Treatment in Patients with Chronic Low Back Pain and Vertebral Bone Edema (Modic Type I Changes): A Randomized Clinical Controlled Trial of Efficacy. Iraqi Postgrad. Med. J. 2014, 13, 390–398. [Google Scholar]
- Palazzo, C.; Ferrari, M.; Lefevre-Colau, M.-M.; Nguyen, C.; Rannou, F.; Poiraudeau, S. Lack of effectiveness of antibiotics in chronic low back pain with Modic 1 changes. Jt. Bone Spine 2017, 84, 507–508. [Google Scholar] [CrossRef] [PubMed]
- Simmons, J.W.; McMillin, J.N.; Emery, S.F.; Kimmich, S.J. Intradiscal Steroids. A Prospective Double-Blind Clinical Trial. Spine 1992, 17, S172–S175. [Google Scholar] [CrossRef] [PubMed]
- Khot, A.; Bowditch, M.; Powell, J.; Sharp, D. The Use of Intradiscal Steroid Therapy for Lumbar Spinal Discogenic Pain: A Randomized Controlled Trial. Spine 2004, 29, 833–836. [Google Scholar] [CrossRef]
- Nguyen, C.; Boutron, I.; Baron, G.; Sanchez, K.; Palazzo, C.; Benchimol, R.; Paris, G.; James-Belin, É.; Lefevre-Colau, M.-M.; Beaudreuil, J.; et al. Intradiscal Glucocorticoid Injection for Patients With Chronic Low Back Pain Associated With Active Discopathy: A Randomized Trial. Ann. Intern. Med. 2017, 166, 547–556. [Google Scholar] [CrossRef]
- Buttermann, G.R. The effect of spinal steroid injections for degenerative disc disease. Spine J. 2004, 4, 495–505. [Google Scholar] [CrossRef]
- Nguyen, C.; Bénichou, M.; Revel, M.; Poiraudeau, S.; Rannou, F. Association of accelerated switch from vertebral end-plate Modic I to Modic 0 signal changes with clinical benefit of intradiscal corticosteroid injection for chronic low back pain. Arthritis Care Res. 2011, 63, 2828–2831. [Google Scholar] [CrossRef]
- Mineta, K.; Higashino, K.; Sakai, T.; Fukui, Y.; Sairyo, K. Recurrence of type I Modic inflammatory changes in the lumbar spine: Effectiveness of intradiscal therapy. Skelet. Radiol. 2014, 43, 1645–1649. [Google Scholar] [CrossRef]
- Gjefsen, E.; Bråten, L.C.H.; Goll, G.L.; Wigemyr, M.; Bolstad, N.; Valberg, M.; Schistad, E.I.; Marchand, G.H.; Granviken, F.; Selmer, K.K.; et al. The effect of infliximab in patients with chronic low back pain and Modic changes (the BackToBasic study): Study protocol of a randomized, double blind, placebo-controlled, multicenter trial. BMC Musculoskelet. Disord. 2020, 21, 698. [Google Scholar] [CrossRef]
- Lyu, F.-J.; Cui, H.; Pan, H.; Cheung, K.M.C.; Cao, X.; Iatridis, J.C.; Zheng, Z. Painful intervertebral disc degeneration and inflammation: From laboratory evidence to clinical interventions. Bone Res. 2021, 9, 7. [Google Scholar] [CrossRef]
- Cohen, S.P.; Bogduk, N.; Dragovich, A.; Buckenmaier, C.C.; Griffith, S.; Kurihara, C.; Raymond, J.; Richter, P.J.; Williams, N.; Yaksh, T.L. Randomized, Double-blind, Placebo-controlled, Dose-response, and Preclinical Safety Study of Transforaminal Epidural Etanercept for the Treatment of Sciatica. Anesthesiology 2009, 110, 1116–1126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karppinen, J.; Korhonen, T.; Malmivaara, A.; Paimela, L.; Kyllönen, E.; Lindgren, K.-A.; Rantanen, P.; Tervonen, O.; Niinimäki, J.; Seitsalo, S.; et al. Tumor Necrosis Factor-α Monoclonal Antibody, Infliximab, Used to Manage Severe Sciatica. Spine 2003, 28, 750–753. [Google Scholar] [CrossRef] [PubMed]
- Korhonen, T.; Karppinen, J.; Malmivaara, A.; Autio, R.; Niinimäki, J.; Paimela, L.; Kyllönen, E.; Lindgren, K.-A.; Tervonen, O.; Seitsalo, S.; et al. Efficacy of Infliximab for Disc Herniation-Induced Sciatica. Spine 2004, 29, 2115–2119. [Google Scholar] [CrossRef] [PubMed]
- Autio, R.A.; Karppinen, J.; Niinimäki, J.; Ojala, R.; Veeger, N.; Korhonen, T.; Hurri, H.; Tervonen, O. The Effect of Infliximab, a Monoclonal Antibody Against TNF-α, on Disc Herniation Resorption: A Randomized Controlled Study. Spine 2006, 31, 2641–2645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katz, N.; Borenstein, D.G.; Birbara, C.; Bramson, C.; Nemeth, M.A.; Smith, M.D.; Brown, M.T. Efficacy and safety of tanezumab in the treatment of chronic low back pain. Pain 2011, 152, 2248–2258. [Google Scholar] [CrossRef]
- Kivitz, A.J.; Gimbel, J.S.; Bramson, C.; Nemeth, M.A.; Keller, D.S.; Brown, M.T.; West, C.R.; Verburg, K.M. Efficacy and safety of tanezumab versus naproxen in the treatment of chronic low back pain. Pain 2013, 154, 1009–1021. [Google Scholar] [CrossRef]
- Gimbel, J.S.; Kivitz, A.J.; Bramson, C.; Nemeth, M.A.; Keller, D.S.; Brown, M.T.; West, C.R.; Verburg, K.M. Long-term safety and effectiveness of tanezumab as treatment for chronic low back pain. Pain 2014, 155, 1793–1801. [Google Scholar] [CrossRef]
- Hochberg, M.C.; Tive, L.A.; Abramson, S.; Vignon, E.; Verburg, K.M.; West, C.R.; Smith, M.D.; Hungerford, D.S. When Is Osteonecrosis Not Osteonecrosis?: Adjudication of Reported Serious Adverse Joint Events in the Tanezumab Clinical Development Program. Arthritis Rheumatol. 2015, 68, 382–391. [Google Scholar] [CrossRef] [Green Version]
- Tuakli-Wosornu, Y.A.; Terry, A.; Boachie-Adjei, K.; Harrison, J.R.; Gribbin, C.K.; LaSalle, E.E.; Nguyen, J.T.; Solomon, J.L.; Lutz, G.E. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R 2015, 8, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Levi, D.; Horn, D.S.; Tyszko, P.S.; Levin, J.; Hecht-Leavitt, C.; Walko, D.E. Intradiscal Platelet-Rich Plasma Injection for Chronic Discogenic Low Back Pain: Preliminary Results from a Prospective Trial. Pain Med. 2015, 17, 1010–1022. [Google Scholar] [CrossRef] [Green Version]
- Séguin, C.A.; Pilliar, R.M.; Roughley, P.J.; Kandel, R.A. Tumor Necrosis Factorα Modulates Matrix Production and Catabolism in Nucleus Pulposus Tissue. Spine 2005, 30, 1940–1948. [Google Scholar] [CrossRef] [PubMed]
- Elabd, C.; Centeno, C.J.; Schultz, J.R.; Lutz, G.; Ichim, T.; Silva, F.J. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: A long-term safety and feasibility study. J. Transl. Med. 2016, 14, 253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comella, K.; Silbert, R.; Parlo, M. Effects of the intradiscal implantation of stromal vascular fraction plus platelet rich plasma in patients with degenerative disc disease. J. Transl. Med. 2017, 15, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryan, J.M.; Barry, F.P.; Murphy, J.M.; Mahon, B.P. Mesenchymal stem cells avoid allogeneic rejection. J. Inflamm. 2005, 2, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noriega, D.C.; Ardura, F.; Hernández-Ramajo, R.; Martín-Ferrero, M.Á.; Sánchez-Lite, I.; Toribio, B.; Alberca, M.; García, V.; Moraleda, J.M.; Sánchez, A.; et al. Intervertebral Disc Repair by Allogeneic Mesenchymal Bone Marrow Cells: A Randomized Controlled Trial. Transplantation 2017, 101, 1945–1951. [Google Scholar] [CrossRef]
- Akeda, K.; Ohishi, K.; Masuda, K.; Bae, W.C.; Takegami, N.; Yamada, J.; Nakamura, T.; Sakakibara, T.; Kasai, Y.; Sudo, A. Intradiscal Injection of Autologous Platelet-Rich Plasma Releasate to Treat Discogenic Low Back Pain: A Preliminary Clinical Trial. Asian Spine J. 2017, 11, 380–389. [Google Scholar] [CrossRef]
- Fujii, K.; Yamazaki, M.; Kang, J.D.; Risbud, M.V.; Cho, S.K.; Qureshi, S.A.; Hecht, A.C.; Iatridis, J.C. Discogenic Back Pain: Literature Review of Definition, Diagnosis, and Treatment. JBMR Plus 2019, 3, e10180. [Google Scholar] [CrossRef] [Green Version]
- Sakai, D.; Andersson, G.B.J. Stem cell therapy for intervertebral disc regeneration: Obstacles and solutions. Nat. Rev. Rheumatol. 2015, 11, 243–256. [Google Scholar] [CrossRef]
- Roughley, P.J. Biology of Intervertebral Disc Aging and Degeneration. Spine 2004, 29, 2691–2699. [Google Scholar] [CrossRef]
- Sakai, D. Future perspectives of cell-based therapy for intervertebral disc disease. Eur. Spine J. 2008, 17, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Lai, A.; Moon, A.; Purmessur, D.; Skovrlj, B.; Laudier, D.M.; Winkelstein, B.A.; Cho, S.K.; Hecht, A.C.; Iatridis, J.C. Annular puncture with tumor necrosis factor-alpha injection enhances painful behavior with disc degeneration in vivo. Spine J. 2015, 16, 420–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aoki, Y.; Ohtori, S.; Ino, H.; Douya, H.; Ozawa, T.; Saito, T.; Moriya, H.; Takahashi, K. Disc Inflammation Potentially Promotes Axonal Regeneration of Dorsal Root Ganglion Neurons Innervating Lumbar Intervertebral Disc in Rats. Spine 2004, 29, 2621–2626. [Google Scholar] [CrossRef] [PubMed]
- Krock, E.; Rosenzweig, D.H.; Chabot-Doré, A.-J.; Jarzem, P.; Weber, M.H.; Ouellet, J.A.; Stone, L.S.; Haglund, L. Painful, degenerating intervertebral discs up-regulate neurite sprouting and CGRP through nociceptive factors. J. Cell. Mol. Med. 2014, 18, 1213–1225. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Lv, F.-J. Symptomatic versus Asymptomatic Intervertebral Disc Degeneration: Is Inflammation the Key? Crit. Rev. Eukaryot. Gene Expr. 2015, 25, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Loibl, M.; Wuertz-Kozak, K.; Vadala, G.; Lang, S.; Fairbank, J.; Urban, J.P. Controversies in regenerative medicine: Should intervertebral disc degeneration be treated with mesenchymal stem cells? JOR Spine 2019, 2, e1043. [Google Scholar] [CrossRef]
- Saukkonen, J.; Määttä, J.; Oura, P.; Kyllönen, E.; Tervonen, O.; Niinimäki, J.; Auvinen, J.; Karppinen, J. Association Between Modic Changes and Low Back Pain in Middle Age: A Northern Finland Birth Cohort Study. Spine 2020, 45, 1360–1367. [Google Scholar] [CrossRef]
- Spees, J.L.; Lee, R.H.; Gregory, C.A. Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Res. Ther. 2016, 7, 125. [Google Scholar] [CrossRef] [Green Version]
- Mukhamedshina, Y.O.; Gracheva, O.A.; Mukhutdinova, D.M.; Chelyshev, Y.A.; Rizvanov, A. Mesenchymal stem cells and the neuronal microenvironment in the area of spinal cord injury. Neural Regen. Res. 2019, 14, 227–237. [Google Scholar] [CrossRef]
- Frauchiger, D.A.; Heeb, S.R.; May, R.D.; Wöltje, M.; Benneker, L.M.; Gantenbein, B. Differentiation of MSC and annulus fibrosus cells on genetically engineered silk fleece-membrane-composites enriched for GDF-6 or TGF-β3. J. Orthop. Res. 2017, 36, 1324–1333. [Google Scholar] [CrossRef]
- Clarke, L.; McConnell, J.C.; Sherratt, M.J.; Derby, B.; Richardson, S.M.; Hoyland, J. Growth differentiation factor 6 and transforming growth factor-beta differentially mediate mesenchymal stem cell differentiation, composition, and micromechanical properties of nucleus pulposus constructs. Arthritis Res. Ther. 2014, 16, R67. [Google Scholar] [CrossRef] [Green Version]
- Dai, J.; Wang, H.; Liu, G.; Xu, Z.; Li, F.; Fang, H. Dynamic compression and co-culture with nucleus pulposus cells promotes proliferation and differentiation of adipose-derived mesenchymal stem cells. J. Biomech. 2014, 47, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Peroglio, M.; Eglin, D.; Benneker, L.M.; Alini, M.; Grad, S. Thermoreversible hyaluronan-based hydrogel supports in vitro and ex vivo disc-like differentiation of human mesenchymal stem cells. Spine J. 2013, 13, 1627–1639. [Google Scholar] [CrossRef] [PubMed]
- Le Maitre, C.L.; Baird, P.; Freemont, A.J.; A Hoyland, J. An in vitro study investigating the survival and phenotype of mesenchymal stem cells following injection into nucleus pulposus tissue. Arthritis Res. Ther. 2009, 11, R20. [Google Scholar] [CrossRef] [Green Version]
- Zha, K.; Li, X.; Yang, Z.; Tian, G.; Sun, Z.; Sui, X.; Dai, Y.; Liu, S.; Guo, Q. Heterogeneity of mesenchymal stem cells in cartilage regeneration: From characterization to application. NPJ Regen. Med. 2021, 6, 14. [Google Scholar] [CrossRef]
- Richardson, S.M.; Kalamegam, G.; Pushparaj, P.N.; Matta, C.; Memic, A.; Khademhosseini, A.; Mobasheri, R.; Poletti, F.L.; Hoyland, J.A.; Mobasheri, A. Mesenchymal stem cells in regenerative medicine: Focus on articular cartilage and intervertebral disc regeneration. Methods 2016, 99, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Vadalà, G.; Ambrosio, L.; Russo, F.; Papalia, R.; Denaro, V. Interaction between Mesenchymal Stem Cells and Intervertebral Disc Microenvironment: From Cell Therapy to Tissue Engineering. Stem Cells Int. 2019, 2019, 2376172. [Google Scholar] [CrossRef]
- Baumgartner, L.; Arnhold, S.; Brixius, K.; Addicks, K.; Bloch, W. Human mesenchymal stem cells: Influence of oxygen pressure on proliferation and chondrogenic differentiation in fibrin gluein vitro. J. Biomed. Mater. Res. Part A 2009, 9999A, 930–940. [Google Scholar] [CrossRef]
- Richardson, S.M.; Hoyland, J.A.; Mobasheri, R.; Csaki, C.; Shakibaei, M.; Mobasheri, A. Mesenchymal stem cells in regenerative medicine: Opportunities and challenges for articular cartilage and intervertebral disc tissue engineering. J. Cell. Physiol. 2010, 222, 23–32. [Google Scholar] [CrossRef]
- Shim, E.-K.; Lee, J.-S.; Kim, D.-E.; Kim, S.K.; Jung, B.-J.; Choi, E.-Y.; Kim, C.-S. Autogenous Mesenchymal Stem Cells from the Vertebral Body Enhance Intervertebral Disc Regeneration via Paracrine Interaction: An in Vitro Pilot Study. Cell Transplant. 2016, 25, 1819–1832. [Google Scholar] [CrossRef]
- Stoyanov, J.; Gantenbein-Ritter, B.; Bertolo, A.; Aebli, N.; Baur, M.; Alini, M.; Grad, S. Role of hypoxia and growth and differentiation factor-5 on differentiation of human mesenchymal stem cells towards intervertebral nucleus pulposus-like cells. Eur. Cells Mater. 2011, 21, 533–547. [Google Scholar] [CrossRef]
- Gantenbein-Ritter, B.; Benneker, L.M.; Alini, M.; Grad, S. Differential response of human bone marrow stromal cells to either TGF-β1 or rhGDF-5. Eur. Spine J. 2010, 20, 962–971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Zhao, L.; Deng, X.; Shi, D.; Wu, F.; Liang, H.; Huang, D.; Shao, Z. Mesenchymal Stem Cells Protect Nucleus Pulposus Cells from Compression-Induced Apoptosis by Inhibiting the Mitochondrial Pathway. Stem Cells Int. 2017, 2017, 9843120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.-C.; Leung, V.Y.; Lu, W.W.; Luk, K.D. The effects of microenvironment in mesenchymal stem cell–based regeneration of intervertebral disc. Spine J. 2013, 13, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Chiang, E.; Ma, H.; Wang, J.; Chang, M.; Liu, C.; Chen, T.; Hung, S. Use of Allogeneic Hypoxic Mesenchymal Stem Cells For Treating Disc Degeneration in Rabbits. J. Orthop. Res. 2019, 37, 1440–1450. [Google Scholar] [CrossRef]
- Tsai, C.-C.; Chen, Y.-J.; Yew, T.-L.; Chen, L.-L.; Wang, J.-Y.; Chiu, C.-H.; Hung, S.-C. Hypoxia inhibits senescence and maintains mesenchymal stem cell properties through down-regulation of E2A-p21 by HIF-TWIST. Blood 2011, 117, 459–469. [Google Scholar] [CrossRef] [Green Version]
- Basciano, L.; Nemos, C.; Foliguet, B.; de Isla, N.; de Carvalho, M.; Tran, N.; Dalloul, A. Long term culture of mesenchymal stem cells in hypoxia promotes a genetic program maintaining their undifferentiated and multipotent status. BMC Cell Biol. 2011, 12, 12. [Google Scholar] [CrossRef] [Green Version]
- Grayson, W.L.; Zhao, F.; Bunnell, B.; Ma, T. Hypoxia enhances proliferation and tissue formation of human mesenchymal stem cells. Biochem. Biophys. Res. Commun. 2007, 358, 948–953. [Google Scholar] [CrossRef]
- Liang, C.; Li, H.; Tao, Y.; Zhou, X.; Li, F.; Chen, G.; Chen, Q. Responses of human adipose-derived mesenchymal stem cells to chemical microenvironment of the intervertebral disc. J. Transl. Med. 2012, 10, 49. [Google Scholar] [CrossRef] [Green Version]
- Wuertz, K.; Godburn, K.; Neidlinger-Wilke, C.; Urban, J.; Iatridis, J. Behavior of Mesenchymal Stem Cells in the Chemical Microenvironment of the Intervertebral Disc. Spine 2008, 33, 1843–1849. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, H.T.J.; Hodson, N.; Baird, P.; Richardson, S.; Hoyland, J.A. Acidic pH promotes intervertebral disc degeneration: Acid-sensing ion channel -3 as a potential therapeutic target. Sci. Rep. 2016, 6, 37360. [Google Scholar] [CrossRef] [Green Version]
- Bischof, M.; Häckel, S.; Oberli, A.; Croft, A.; Oswald, K.; Albers, C.; Gantenbein, B.; Guerrero, J. Influence of Angiopoietin Treatment with Hypoxia and Normoxia on Human Intervertebral Disc Progenitor Cell’s Proliferation, Metabolic Activity, and Phenotype. Appl. Sci. 2021, 11, 7144. [Google Scholar] [CrossRef]
- Chen, J.-W.; Li, B.; Yang, Y.-H.; Jiang, S.-D.; Jiang, L.-S. Significance of hypoxia in the physiological function of intervertebral disc cells. Crit. Rev. Eukaryot. Gene Expr. 2014, 24, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Feng, G.; Li, L.; Liu, H.; Song, Y.; Huang, F.; Tu, C.; Shen, B.; Gong, Q.; Li, T.; Zeng, J.; et al. Hypoxia differentially regulates human nucleus pulposus and annulus fibrosus cell extracellular matrix production in 3D scaffolds. Osteoarthr. Cartil. 2013, 21, 582–588. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Tao, H.; Wang, H.; Dong, F.; Zhang, R.; Li, J.; Ge, P.; Song, P.; Zhang, H.; Xu, P.; et al. Biological Behavior of Human Nucleus Pulposus Mesenchymal Stem Cells in Response to Changes in the Acidic Environment During Intervertebral Disc Degeneration. Stem Cells Dev. 2017, 26, 901–911. [Google Scholar] [CrossRef]
- Su, Y.-S.; Sun, W.-H.; Chen, C.-C. Molecular mechanism of inflammatory pain. World J. Anesthesiol. 2014, 3, 71–81. [Google Scholar] [CrossRef]
- Urban, J.P.G. The role of the physicochemical environment in determining disc cell behaviour. Biochem. Soc. Trans. 2002, 30, 858–863. [Google Scholar] [CrossRef]
- Mwale, F.; Ciobanu, I.; Giannitsios, D.; Roughley, P.; Steffen, T.; Antoniou, J. Effect of Oxygen Levels on Proteoglycan Synthesis by Intervertebral Disc Cells. Spine 2011, 36, E131–E138. [Google Scholar] [CrossRef] [PubMed]
- Grunhagen, T.; Shirazi-Adl, A.; Fairbank, J.C.; Urban, J.P. Intervertebral Disk Nutrition: A Review of Factors Influencing Concentrations of Nutrients and Metabolites. Orthop. Clin. N. Am. 2011, 42, 465–477. [Google Scholar] [CrossRef]
- Vo, N.V.; Hartman, R.A.; Patil, P.R.; Risbud, M.V.; Kletsas, D.; Iatridis, J.; Hoyland, J.A.; Le Maitre, C.; Sowa, G.A.; Kang, J.D. Molecular mechanisms of biological aging in intervertebral discs. J. Orthop. Res. 2016, 34, 1289–1306. [Google Scholar] [CrossRef] [Green Version]
- Wuertz, K.; Godburn, K.; Iatridis, J. MSC response to pH levels found in degenerating intervertebral discs. Biochem. Biophys. Res. Commun. 2009, 379, 824–829. [Google Scholar] [CrossRef] [Green Version]
- Tsai, T.-T.; Danielson, K.G.; Guttapalli, A.; Oguz, E.; Albert, T.J.; Shapiro, I.M.; Risbud, M.V. TonEBP/OREBP Is a Regulator of Nucleus Pulposus Cell Function and Survival in the Intervertebral Disc. J. Biol. Chem. 2006, 281, 25416–25424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Risbud, M.V.; Shapiro, I.M. Role of cytokines in intervertebral disc degeneration: Pain and disc content. Nat. Rev. Rheumatol. 2013, 10, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.; Tunger, A.; Wobus, M.; von Bonin, M.; Towers, R.; Bornhäuser, M.; Dazzi, F.; Wehner, R.; Schmitz, M. Immunomodulatory Properties of Mesenchymal Stromal Cells: An Update. Front. Cell Dev. Biol. 2021, 9, 637725. [Google Scholar] [CrossRef] [PubMed]
- Joel, M.D.M.; Yuan, J.; Wang, J.; Yan, Y.; Qian, H.; Zhang, X.; Xu, W.; Mao, F. MSC: Immunoregulatory effects, roles on neutrophils and evolving clinical potentials. Am. J. Transl. Res. 2019, 11, 3890–3904. [Google Scholar]
- Yang, H.; Liu, B.; Liu, Y.; He, D.; Xing, Y.; An, Y.; Tian, W. Secreted Factors From Intervertebral Disc Cells and Infiltrating Macrophages Promote Degenerated Intervertebral Disc Catabolism. Spine 2019, 44, E520–E529. [Google Scholar] [CrossRef]
- Shamji, M.F.; Setton, L.A.; Jarvis, W.; So, S.; Chen, J.; Jing, L.; Bullock, R.; Isaacs, R.E.; Brown, C.; Richardson, W. Pro-inflammatory cytokine expression profile in degenerative and herniated human intervertebral disc tissues. Arthritis Care Res. 2010, 62, 1974–1982. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.; Jiang, J.; Gu, Z.; Zhang, J.; Chen, Y.; Liu, X. Mesenchymal stromal cell therapies: Immunomodulatory properties and clinical progress. Stem Cell Res. Ther. 2020, 11, 345. [Google Scholar] [CrossRef]
- De Castro, L.L.; Lopes-Pacheco, M.; Weiss, D.J.; Cruz, F.F.; Rocco, P.R.M. Current understanding of the immunosuppressive properties of mesenchymal stromal cells. Klin. Wochenschr. 2019, 97, 605–618. [Google Scholar] [CrossRef]
- Wang, M.; Yuan, Q.; Xie, L. Mesenchymal Stem Cell-Based Immunomodulation: Properties and Clinical Application. Stem Cells Int. 2018, 2018, 3057624. [Google Scholar] [CrossRef]
- Le Maitre, C.L.; Freemont, A.J.; Hoyland, J.A. The role of interleukin-1 in the pathogenesis of human Intervertebral disc degeneration. Arthritis Res. Ther. 2005, 7, R732–R745. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Wang, H.; Yang, H.; Li, J.; Cai, Q.; Shapiro, I.M.; Risbud, M.V. Tumor Necrosis Factor-α– and Interleukin-1β–Dependent Matrix Metalloproteinase-3 Expression in Nucleus Pulposus Cells Requires Cooperative Signaling via Syndecan 4 and Mitogen-Activated Protein Kinase–NF-κB Axis: Implications in Inflammatory Disc Disease. Am. J. Pathol. 2014, 184, 2560–2572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Markova, D.; Anderson, D.G.; Zheng, Z.; Shapiro, I.M.; Risbud, M.V. TNF-α and IL-1β Promote a Disintegrin-like and Metalloprotease with Thrombospondin Type I Motif-5-mediated Aggrecan Degradation through Syndecan-4 in Intervertebral Disc. J. Biol. Chem. 2011, 286, 39738–39749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orozco, L.; Soler, R.; Morera, C.; Alberca, M.; Sánchez, A.; Garcia-Sancho, J. Intervertebral Disc Repair by Autologous Mesenchymal Bone Marrow Cells: A Pilot Study. Transplantation 2011, 92, 822–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahme, R.; Moussa, R. The Modic Vertebral Endplate and Marrow Changes: Pathologic Significance and Relation to Low Back Pain and Segmental Instability of the Lumbar Spine. Am. J. Neuroradiol. 2008, 29, 838–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montoya, J.E.M.; Cataño, C.P.; Cuellar, A.M.T.; Osorio, M.P.V.; Cano, J.R.; Suarez, J.C.L.; Lopez, M.L.C. Utility of the claw sign in spine magnetic nuclear resonance with diffusion to differentiate Modic type I changes for degenerative disease versus infection. J. Spine Surg. 2018, 4, 616–623. [Google Scholar] [CrossRef]
- Ding, H.; Wei, J.; Zhao, Y.; Liu, Y.; Liu, L.; Cheng, L. Progranulin derived engineered protein Atsttrin suppresses TNF-α-mediated inflammation in intervertebral disc degenerative disease. Oncotarget 2017, 8, 109692–109702. [Google Scholar] [CrossRef] [Green Version]
- Deng, X.; Zhao, F.; Kang, B.; Zhang, X. Elevated interleukin-6 expression levels are associated with intervertebral disc degeneration. Exp. Ther. Med. 2016, 11, 1425–1432. [Google Scholar] [CrossRef] [Green Version]
- Gruber, H.E.; Hoelscher, G.L.; A Ingram, J.; Norton, H.J.; Hanley, E.N. Increased IL-17 expression in degenerated human discs and increased production in cultured annulus cells exposed to IL-1ß and TNF-α. Biotech. Histochem. 2013, 88, 302–310. [Google Scholar] [CrossRef]
- Gabr, M.A.; Jing, L.; Helbling, A.R.; Sinclair, S.M.; Allen, K.D.; Shamji, M.F.; Richardson, W.J.; Fitch, R.D.; Setton, L.A.; Chen, J. Interleukin-17 synergizes with IFNγ or TNFα to promote inflammatory mediator release and intercellular adhesion molecule-1 (ICAM-1) expression in human intervertebral disc cells. J. Orthop. Res. 2010, 29, 1–7. [Google Scholar] [CrossRef]
- Urquhart, D.M.; Rosenfeld, J.V.; van Tulder, M.; Wluka, A.E.; Leder, K.; Cheng, A.C.; Forbes, A.B.; Chan, P.; O’Sullivan, R.; Liew, S.; et al. Is antibiotic treatment effective in the management of chronic low back pain with disc herniation? Study protocol for a randomised controlled trial. Trials 2021, 22, 759. [Google Scholar] [CrossRef]
- Teixeira, G.Q.; Pereira, C.L.; Ferreira, J.R.; Maia, A.F.; Gomez-Lazaro, M.; Barbosa, M.A.; Neidlinger-Wilke, C.; Goncalves, R.M. Immunomodulation of Human Mesenchymal Stem/Stromal Cells in Intervertebral Disc Degeneration. Spine 2018, 43, E673–E682. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, A.A.; Bach, F.C.; Tryfonidou, M.A.; Le Maitre, C.L.; Mwale, F.; Diwan, A.D.; Ito, K. Leaping the hurdles in developing regenerative treatments for the intervertebral disc from preclinical to clinical. JOR Spine 2018, 1, e1027. [Google Scholar] [CrossRef]
- Boisson, M.; Lefèvre-Colau, M.-M.; Rannou, F.; Nguyen, C. Active discopathy: A clinical reality. RMD Open 2018, 4, e000660. [Google Scholar] [CrossRef] [PubMed]
- Gruber, H.E.; Chow, Y.; Hoelscher, G.L.; Ingram, J.A.; Zinchenko, N.; Norton, H.J.; Sun, Y.; Hanley, E.N. Micromass Culture of Human Anulus Cells: Morphology and Extracellular Matrix Production. Spine 2010, 35, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.B.; Poplawski, M.M.; Pawha, P.S.; Naidich, T.P.; Tanenbaum, L.N. Diffusion-Weighted MRI “Claw Sign” Improves Differentiation of Infectious from Degenerative Modic Type 1 Signal Changes of the Spine. Am. J. Neuroradiol. 2014, 35, 1647–1652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daghighi, M.H.; Poureisa, M.; Safarpour, M.; Behzadmehr, R.; Fouladi, D.F.; Meshkini, A.; Varshochi, M.; Nazarlou, A.K. Diffusion-weighted magnetic resonance imaging in differentiating acute infectious spondylitis from degenerative Modic type 1 change; the role of b-value, apparent diffusion coefficient, claw sign and amorphous increased signal. Br. J. Radiol. 2016, 89, 20150152. [Google Scholar] [CrossRef] [Green Version]
- Magnitsky, S.; Dudli, S.; Tang, X.; Kaur, J.; Diaz, J.; Miller, S.; Lotz, J.C. Quantification of Propionic Acid in the Bovine Spinal Disk After Infection of the Tissue With Propionibacteria acnes Bacteria. Spine 2018, 43, E634–E638. [Google Scholar] [CrossRef] [Green Version]
- Gornet, M.G.; Peacock, J.; Claude, J.; Schranck, F.W.; Copay, A.G.; Eastlack, R.K.; Benz, R.; Olshen, A.; Lotz, J.C. Magnetic resonance spectroscopy (MRS) can identify painful lumbar discs and may facilitate improved clinical outcomes of lumbar surgeries for discogenic pain. Eur. Spine J. 2019, 28, 674–687. [Google Scholar] [CrossRef] [Green Version]
- Heggli, I.; Schüpbach, R.; Herger, N.; Schweizer, T.A.; Juengel, A.; Farshad-Amacker, N.; Betz, M.; Spirig, J.M.; Wanivenhaus, F.; Ulrich, N.H.; et al. OP0083 Infectious and Autoinflammatory Modic Type 1 Changes Have Different Pathomechanisms. Ann. Rheum. Dis. 2021, 80, 45. [Google Scholar] [CrossRef]
- Heggli, I.; Epprecht, S.; Juengel, A.; Schuepbach, R.; Farshad-Amacker, N.; German, C.; Mengis, T.; Herger, N.; Straumann, L.; Baumgartner, S.; et al. Pro-fibrotic phenotype of bone marrow stromal cells in Modic type 1 changes. Eur. Cells Mater. 2021, 41, 648–667. [Google Scholar] [CrossRef]
- Yang, H.; Tian, W.; Wang, S.; Liu, X.; Wang, Z.; Hou, L.; Ge, J.; Zhang, X.; He, Z.; Wang, X. TSG-6 secreted by bone marrow mesenchymal stem cells attenuates intervertebral disc degeneration by inhibiting the TLR2/NF-κB signaling pathway. Lab. Investig. 2018, 98, 755–772. [Google Scholar] [CrossRef] [PubMed]
- De Luca, P.; Galeazzi, O.B.L.I.O.; De Girolamo, L.; Kouroupis, D.; Castagnetta, M.; Orfei, C.P.; Coviello, D.; Coco, S.; Correa, D.; Brayda-Bruno, M.; et al. Intervertebral disc and endplate cells response to IL-1β inflammatory cell priming and identification of molecular targets of tissue degeneration. Eur. Cells Mater. 2020, 39, 227–248. [Google Scholar] [CrossRef] [PubMed]
- Ge, J.; Yan, Q.; Wang, Y.; Cheng, X.; Song, D.; Wu, C.; Yu, H.; Yang, H.; Zou, J. IL-10 delays the degeneration of intervertebral discs by suppressing the p38 MAPK signaling pathway. Free Radic. Biol. Med. 2019, 147, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Yoon, Y.; Park, H.; Kuh, S. Molecular response of human cervical and lumbar nucleus pulposus cells from degenerated discs following cytokine treatment. Genet. Mol. Res. 2013, 12, 838–851. [Google Scholar] [CrossRef]
- Abbott, R.D.; Purmessur, D.; Monsey, R.D.; Iatridis, J.C. Regenerative potential of TGFβ3 + Dex and notochordal cell conditioned media on degenerated human intervertebral disc cells. J. Orthop. Res. 2011, 30, 482–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.M.; Song, J.Y.; Baek, M.; Jung, H.-Y.; Kang, H.; Han, I.B.; Kwon, Y.D.; Shin, D.E. Interleukin-1β induces angiogenesis and innervation in human intervertebral disc degeneration. J. Orthop. Res. 2010, 29, 265–269. [Google Scholar] [CrossRef]
- Freemont, A.J.; Watkins, A.; Le Maitre, C.; Baird, P.; Jeziorska, M.; Knight, M.T.N.; Ross, E.R.S.; O’Brien, J.P.; Hoyland, J.A. Nerve growth factor expression and innervation of the painful intervertebral disc. J. Pathol. 2002, 197, 286–292. [Google Scholar] [CrossRef]
- Kumar, H.; Ha, D.-H.; Lee, E.-J.; Park, J.H.; Shim, J.H.; Ahn, T.-K.; Kim, K.-T.; Ropper, A.E.; Sohn, S.; Kim, C.-H.; et al. Safety and tolerability of intradiscal implantation of combined autologous adipose-derived mesenchymal stem cells and hyaluronic acid in patients with chronic discogenic low back pain: 1-year follow-up of a phase I study. Stem Cell Res. Ther. 2017, 8, 262. [Google Scholar] [CrossRef] [Green Version]
- Lam, A.T.; Reuveny, S.; Oh, S.K.-W. Human mesenchymal stem cell therapy for cartilage repair: Review on isolation, expansion, and constructs. Stem Cell Res. 2020, 44, 101738. [Google Scholar] [CrossRef]

| MC Type | Pro-Inflammatory | Pro-Osteoclastic | Neurotrophic |
|---|---|---|---|
| MC1 | CCL2, IL-6, IL-8, PGE2 | OSCAR | NTRK1 |
| MC2 | CCL2, CXCL5, GM-CSF, IL-1β, M-CSF | RANKL, RUNX1, RUNX2 | NTRK1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herger, N.; Bermudez-Lekerika, P.; Farshad, M.; Albers, C.E.; Distler, O.; Gantenbein, B.; Dudli, S. Should Degenerated Intervertebral Discs of Patients with Modic Type 1 Changes Be Treated with Mesenchymal Stem Cells? Int. J. Mol. Sci. 2022, 23, 2721. https://doi.org/10.3390/ijms23052721
Herger N, Bermudez-Lekerika P, Farshad M, Albers CE, Distler O, Gantenbein B, Dudli S. Should Degenerated Intervertebral Discs of Patients with Modic Type 1 Changes Be Treated with Mesenchymal Stem Cells? International Journal of Molecular Sciences. 2022; 23(5):2721. https://doi.org/10.3390/ijms23052721
Chicago/Turabian StyleHerger, Nick, Paola Bermudez-Lekerika, Mazda Farshad, Christoph E. Albers, Oliver Distler, Benjamin Gantenbein, and Stefan Dudli. 2022. "Should Degenerated Intervertebral Discs of Patients with Modic Type 1 Changes Be Treated with Mesenchymal Stem Cells?" International Journal of Molecular Sciences 23, no. 5: 2721. https://doi.org/10.3390/ijms23052721






