Diagnostic Value of MAML2 Rearrangements in Mucoepidermoid Carcinoma
Abstract
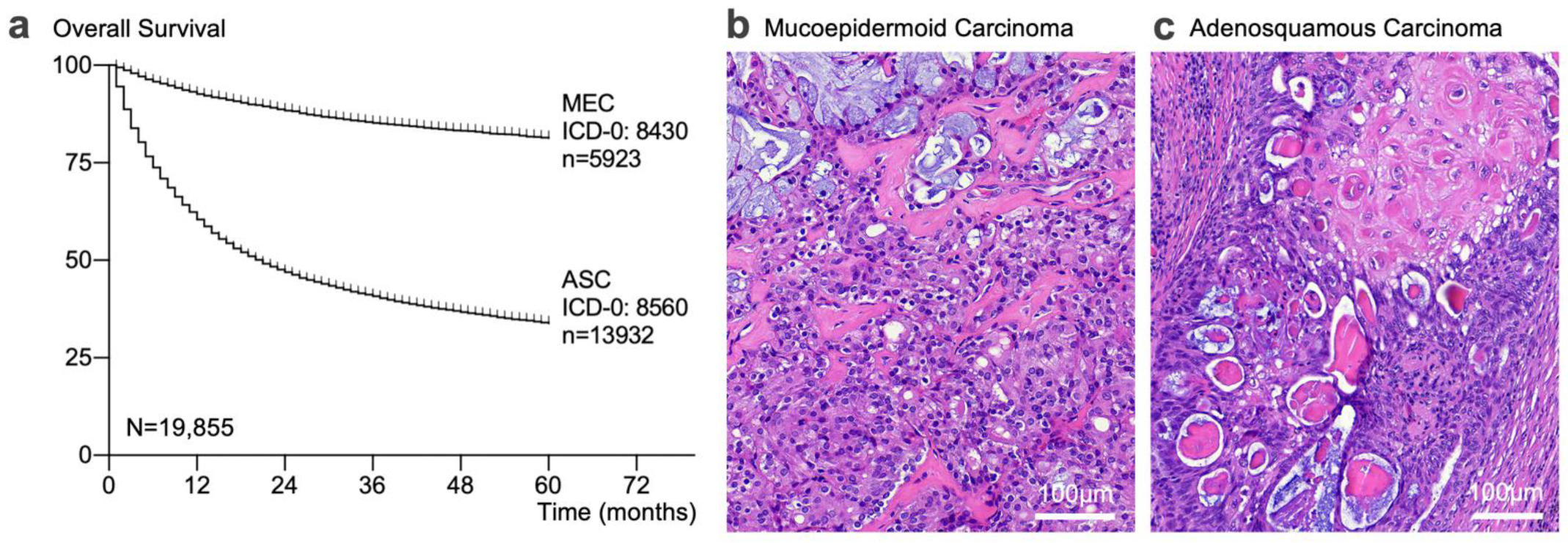
1. Introduction
2. Results
2.1. MAML2 Fusions Were Rare Outside of Major Salivary Gland Tumors
2.2. Test Order Analysis of MAML2 in Diagnostic Practice
2.3. Diagnostic Performance Assessment
2.4. Added Value of MAML2 Testing and Economic Impact Analysis
2.5. A Markov Model for MAML2-Related Diagnostic State Transition Probabilities
2.6. Specifying the Relative Diagnostic Value of MAML2 via an Expert Survey
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Clinical Genotyping
4.3. Data Sources and Queries
4.4. Test Order Analysis
4.5. Markov Model
4.6. Expert Opinion
4.7. Statistical, Economic Impact, and Survey Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pan, F.; Cui, S.; Wang, W.; Gu, A.; Jiang, L. Survival analysis for lung adenosquamous carcinoma patients with brain metastasis. J. Cancer 2018, 9, 3707–3712. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.C.; Sun, Y.H.; Lin, S.W.; Yeh, Y.C.; Chan, M.L. Surgical outcomes of pulmonary mucoepidermoid carcinoma: A review of 41 cases. PLoS ONE 2017, 12, e0176918. [Google Scholar] [CrossRef] [PubMed]
- Nance, M.A.; Seethala, R.R.; Wang, Y.; Chiosea, S.I.; Myers, E.N.; Johnson, J.T.; Lai, S.Y. Treatment and survival outcomes based on histologic grading in patients with head and neck mucoepidermoid carcinoma. Cancer 2008, 113, 2082–2089. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.Y.; Choi, N.; Ko, Y.H.; Chung, M.K.; Son, Y.I.; Baek, C.H.; Baek, K.H.; Jeong, H.S. Treatment outcomes in metastatic and localized high-grade salivary gland cancer: High chance of cure with surgery and post-operative radiation in T1-2 N0 high-grade salivary gland cancer. BMC Cancer 2018, 18, 672. [Google Scholar] [CrossRef]
- Zhu, L.; Jiang, L.; Yang, J.; Gu, W.; He, J. Clinical characteristics and prognosis of patients with lung adenosquamous carcinoma after surgical resection: Results from two institutes. J. Thorac. Dis. 2018, 10, 2397–2402. [Google Scholar] [CrossRef]
- Wang, J.; Lian, B.; Ye, L.; Hu, J.; Song, Y. Clinicopathological characteristics and survival outcomes in adenosquamous carcinoma of the lung: A population-based study from the SEER database. Oncotarget 2018, 9, 8133–8146. [Google Scholar] [CrossRef][Green Version]
- Fu, J.Y.; Wu, C.X.; Shen, S.K.; Zheng, Y.; Zhang, C.P.; Zhang, Z.Y. Salivary gland carcinoma in Shanghai (2003-2012): An epidemiological study of incidence, site and pathology. BMC Cancer 2019, 19, 350. [Google Scholar] [CrossRef]
- Jee, K.J.; Persson, M.; Heikinheimo, K.; Passador-Santos, F.; Aro, K.; Knuutila, S.; Odell, E.W.; Mäkitie, A.; Sundelin, K.; Stenman, G.; et al. Genomic profiles and CRTC1–MAML2 fusion distinguish different subtypes of mucoepidermoid carcinoma. Mod. Pathol. 2013, 26, 213–222. [Google Scholar] [CrossRef]
- Boahene, D.K.O.; Olsen, K.D.; Lewis, J.E.; Pinheiro, A.D.; Pankratz, V.S.; Bagniewski, S.M. Mucoepidermoid carcinoma of the parotid gland: The Mayo Clinic experience. Arch. Otolaryngol.-Head Neck Surg. 2004, 130, 849–856. [Google Scholar] [CrossRef]
- El-Naggar, A.K.; Chan, J.K.C.; Grandis, J.R.; Takata, T.S.P. WHO Classification of Head and Neck Tumours, 4th ed.; IARC: Lyon, France, 2017. [Google Scholar]
- Kusafuka, K.; Miki, T.; Nakajima, T. Adenosquamous carcinoma of the parotid gland. Histopathology 2013, 63, 593–595. [Google Scholar] [CrossRef]
- Brambilla, E. 2 Histopathological classification phenotype and molecular pathology of lung tumors. In Handbook of Immunohistochemistry and In Situ Hybridization of Human Carcinomas; Elsevier Inc.: Amsterdam, The Netherlands, 2002; Volume 1, pp. 105–114. ISBN 9780123339416. [Google Scholar]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef]
- Chenevert, J.; Barnes, L.E.; Chiosea, S.I. Mucoepidermoid carcinoma: A five-decade journey. Virchows Arch. 2011, 458, 133–140. [Google Scholar] [CrossRef]
- Damiani, J.; Damiani, K.K.; Hauck, K.; Hyams, V.J. Mucoepidermoid-adenosquamous carcinoma of the larynx and hypopharynx: A report of 21 cases and a review of the literature. Otolaryngol.-Head Neck Surg. 1981, 89, 235–243. [Google Scholar] [CrossRef]
- Hyams, V.; Batsakis, J.; Michaels, L. Tumors of the Upper Respira-Tory Tract and Ear. Atlas of Tumor Pathology, 2nd Series, Fascicle25, 2nd ed.; Armed Forces Institute of Pathology: Washington, DC, USA, 1986. [Google Scholar]
- Kitagawa, M. Notch signalling in the nucleus: Roles of Mastermind-like (MAML) transcriptional coactivators. J. Biochem. 2016, 159, 287–294. [Google Scholar] [CrossRef]
- Achcar, R.D.O.D.; Nikiforova, M.N.; Dacic, S.; Nicholson, A.G.; Yousem, S.A. Mammalian mastermind like 2 11q21 gene rearrangement in bronchopulmonary mucoepidermoid carcinoma. Hum. Pathol. 2009, 40, 854–860. [Google Scholar] [CrossRef]
- Lennerz, J.K.M.; Perry, A.; Mills, J.C.; Huettner, P.C.; Pfeifer, J.D. Mucoepidermoid carcinoma of the cervix: Another tumor with the t(11;19)-associated CRTC1-MAML2 gene fusion. Am. J. Surg. Pathol. 2009, 33, 835–843. [Google Scholar] [CrossRef]
- Zhu, F.; Wang, W.; Hou, Y.; Shi, J.; Liu, Z.; He, D.; Bai, C.; Li, S.; Jiang, L. MAML2 rearrangement in primary pulmonary mucoepidermoid carcinoma and the correlation with FLT1 expression. PLoS ONE 2014, 9, e94399. [Google Scholar] [CrossRef]
- Tochigi, N.; Dacic, S.; Nikiforova, M.; Cieply, K.M.; Yousem, S.A. Adenosquamous Carcinoma of the Lung. Am. J. Clin. Pathol. 2011, 135, 783–789. [Google Scholar] [CrossRef]
- Roden, A.C.; Erickson-Johnson, M.R.; Yi, E.S.; García, J.J. Analysis of MAML2 rearrangement in mucoepidermoid carcinoma of the thymus. Hum. Pathol. 2013, 44, 2799–2805. [Google Scholar] [CrossRef]
- Saeki, K.; Ohishi, Y.; Matsuda, R.; Mochidome, N.; Miyasaka, Y.; Yamamoto, H.; Koga, Y.; Maehara, Y.; Nakamura, M.; Oda, Y. “Pancreatic Mucoepidermoid Carcinoma” Is not a Pancreatic Counterpart of CRTC1/3-MAML2 Fusion Gene-related Mucoepidermoid Carcinoma of the Salivary Gland, and May More Appropriately be Termed Pancreatic Adenosquamous Carcinoma with Mucoepidermoid Carcinoma-like Features. Am. J. Surg. Pathol. 2018, 42, 1419–1428. [Google Scholar] [CrossRef]
- White, V.A.; Hyrcza, M.D.; Lennerz, J.; Thierauf, J.; Lokuhetty, D.; Cree, I.A.; Indave, B.I. Mucoepidermoid carcinoma (MEC) and adenosquamous carcinoma (ADSC): The same or different? A systematic review of molecular pathology to aid in classification. 2021. [Google Scholar]
- Chiosea, S.I.; Dacic, S.; Nikiforova, M.N.; Seethala, R.R. Prospective testing of mucoepidermoid carcinoma for the MAML2 translocation: Clinical implications. Laryngoscope 2012, 122, 1690–1694. [Google Scholar] [CrossRef]
- Kass, J.I.; Lee, S.C.; Abberbock, S.; Seethala, R.R.; Duvvuri, U. Adenosquamous carcinoma of the head and neck: Molecular analysis using CRTC-MAML FISH and survival comparison with paired conventional squamous cell carcinoma. Laryngoscope 2015, 125, E371–E376. [Google Scholar] [CrossRef]
- Birkeland, A.C.; Foltin, S.K.; Michmerhuizen, N.L.; Hoesli, R.C.; Rosko, A.J.; Byrd, S.; Yanik, M.; Nor, J.E.; Bradford, C.R.; Prince, M.E.; et al. Correlation of Crtc1/3-Maml2 fusion status, grade and survival in mucoepidermoid carcinoma. Oral Oncol. 2017, 68, 5–8. [Google Scholar] [CrossRef]
- Bishop, J.A.; Cowan, M.L.; Shum, C.H.; Westra, W.H. MAML2 Rearrangements in Variant Forms of Mucoepidermoid Carcinoma: Ancillary Diagnostic Testing for the Ciliated and Warthin-like Variants. Am. J. Surg. Pathol. 2018, 42, 130–136. [Google Scholar] [CrossRef]
- Clauditz, T.S.; Gontarewicz, A.; Wang, C.J.; Münscher, A.; Laban, S.; Tsourlakis, M.C.; Knecht, R.; Sauter, G.; Wilczak, W. 11q21 rearrangement is a frequent and highly specific genetic alteration in mucoepidermoid carcinoma. Diagnostic Mol. Pathol. 2012, 21, 134–137. [Google Scholar] [CrossRef]
- Šimundić, A.-M. Measures of Diagnostic Accuracy: Basic Definitions. EJIFCC 2009, 19, 203–211. [Google Scholar]
- Gladwell, M. Outliers: The Story of Success; Little, Brown and Company: Boston, MA, USA, 2011. [Google Scholar]
- Cree, I.A.; Indave Ruiz, B.I.; Zavadil, J.; McKay, J.; Olivier, M.; Kozlakidis, Z.; Lazar, A.J.; Hyde, C.; Holdenrieder, S.; Hastings, R.; et al. The International Collaboration for Cancer Classification and Research. Int. J. Cancer 2021, 148, 560–571. [Google Scholar] [CrossRef]
- Chow, Z.L.; Indave, B.I.; Lokuhetty, M.D.S.; Ochiai, A.; Cree, I.A.; White, V.A. Misleading terminology in pathology: Lack of definitions hampers communication. Virchows Arch. 2021, 479, 425–430. [Google Scholar] [CrossRef]
- Uttley, L.; Indave, B.I.; Hyde, C.; White, V.; Lokuhetty, D.; Cree, I. Invited commentary—WHO Classification of Tumours: How should tumors be classified? Expert consensus, systematic reviews or both? Int. J. Cancer 2020, 146, 3516–3521. [Google Scholar] [CrossRef]
- Cree, I.A.; Indave, B.I. Commentary: Cancer research quality and tumour classification. Tumor Biol. 2020, 42, 7544. [Google Scholar] [CrossRef]
- Zheng, Z.; Liebers, M.; Zhelyazkova, B.; Cao, Y.; Panditi, D.; Lynch, K.D.; Chen, J.; Robinson, H.E.; Shim, H.S.; Chmielecki, J.; et al. Anchored multiplex PCR for targeted next-generation sequencing. Nat. Med. 2014, 20, 1479–1484. [Google Scholar] [CrossRef] [PubMed]
- Dias-Santagata, D.; Akhavanfard, S.; David, S.S.; Vernovsky, K.; Kuhlmann, G.; Boisvert, S.L.; Stubbs, H.; McDermott, U.; Settleman, J.; Kwak, E.L.; et al. Rapid targeted mutational analysis of human tumours: A clinical platform to guide personalized cancer medicine. EMBO Mol. Med. 2010, 2, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Chabner, B.A.; Ellisen, L.W.; Iafrate, A.J. Personalized Medicine: Hype or Reality. Oncologist 2013, 18, 640–643. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thierauf, J.; Ramamurthy, N.; Jo, V.Y.; Robinson, H.; Frazier, R.P.; Gonzalez, J.; Pacula, M.; Dominguez Meneses, E.; Nose, V.; Nardi, V.; et al. Clinically Integrated Molecular Diagnostics in Adenoid Cystic Carcinoma. Oncologist 2019, 24, 1356–1367. [Google Scholar] [CrossRef]
- Chan, S.A.; Van Abel, K.M.; Lewis, J.E.; Routman, D.M.; Garcia, J.J.; Karp, E.E.; Price, D.L.; Janus, J.R.; Kasperbauer, J.L.; Moore, E.J. Mucoepidermoid carcinoma of the parotid gland: Twenty-year experience in treatment and outcomes. Head Neck 2021, 43, 2663–2671. [Google Scholar] [CrossRef]
- Cipriani, N.A.; Lusardi, J.J.; McElherne, J.; Pearson, A.T.; Olivas, A.D.; Fitzpatrick, C.; Lingen, M.W.; Blair, E.A. Mucoepidermoid Carcinoma. Am. J. Surg. Pathol. 2019, 43, 885–897. [Google Scholar] [CrossRef]
- Seethala, R.R.; Dacic, S.; Cieply, K.; Kelly, L.M.; Nikiforova, M.N. A reappraisal of the MECT1/MAML2 translocation in salivary mucoepidermoid carcinomas. Am. J. Surg. Pathol. 2010, 34, 1106–1121. [Google Scholar] [CrossRef]
- Nakayama, T.; Miyabe, S.; Okabe, M.; Sakuma, H.; Ijichi, K.; Hasegawa, Y.; Nagatsuka, H.; Shimozato, K.; Inagaki, H. Clinicopathological significance of the CRTC3-MAML2 fusion transcript in mucoepidermoid carcinoma. Mod. Pathol. 2009, 22, 1575–1581. [Google Scholar] [CrossRef]
- Freiberger, S.N.; Brada, M.; Fritz, C.; Höller, S.; Vogetseder, A.; Horcic, M.; Bihl, M.; Michal, M.; Lanzer, M.; Wartenberg, M.; et al. SalvGlandDx—A comprehensive salivary gland neoplasm specific next generation sequencing panel to facilitate diagnosis and identify therapeutic targets. Neoplasia 2021, 23, 473–487. [Google Scholar] [CrossRef]
- Skálová, A.; Stenman, G.; Simpson, R.H.W.; Hellquist, H.; Slouka, D.; Svoboda, T.; Bishop, J.A.; Hunt, J.L.; Nibu, K.I.; Rinaldo, A.; et al. The role of molecular testing in the differential diagnosis of salivary gland carcinomas. Am. J. Surg. Pathol. 2018, 42, e11–e27. [Google Scholar] [CrossRef]
- Bishop, J.A.; Koduru, P.; Veremis, B.M.; Oliai, B.R.; Weinreb, I.; Rooper, L.M.; Dickson, B.C.; Demicco, E.G. SS18 Break-Apart Fluorescence In Situ Hybridization is a Practical and Effective Method for Diagnosing Microsecretory Adenocarcinoma of Salivary Glands. Head Neck Pathol. 2021, 15, 723–726. [Google Scholar] [CrossRef]
- Yan, M.; Gilmore, H.; Harbhajanka, A. Mucoepidermoid Carcinoma of the Breast With MAML2 Rearrangement: A Case Report and Literature Review. Int. J. Surg. Pathol. 2020, 28, 787–792. [Google Scholar] [CrossRef]
- Robinson, L.; van Heerden, M.B.; Ker-Fox, J.G.; Hunter, K.D.; van Heerden, W.F.P. Expression of Mucins in Salivary Gland Mucoepidermoid Carcinoma. Head Neck Pathol. 2021, 15, 491–502. [Google Scholar] [CrossRef]
- Toper, M.H.; Sarioglu, S. Molecular Pathology of Salivary Gland Neoplasms: Diagnostic, Prognostic, and Predictive Perspective. Adv. Anat. Pathol. 2021, 28, 81–93. [Google Scholar] [CrossRef]
- Ni, W.; Chen, Z.; Zhou, X.; Yang, R.; Yu, M.; Lu, J.; Kaye, F.J.; Wu, L. Targeting Notch and EGFR signaling in human mucoepidermoid carcinoma. Signal Transduct. Target. Ther. 2021, 6, 27. [Google Scholar] [CrossRef]
- Chen, Z.; Ni, W.; Li, J.L.; Lin, S.; Zhou, X.; Sun, Y.; Li, J.W.; Leon, M.E.; Hurtado, M.D.; Zolotukhin, S.; et al. The CRTC1-MAML2 fusion is the major oncogenic driver in mucoepidermoid carcinoma. JCI Insight 2021, 6, e139497. [Google Scholar] [CrossRef]
- Fehr, A.; Röser, K.; Belge, G.; Löning, T.; Bullerdiek, J. A closer look at Warthin tumors and the t(11;19). Cancer Genet. Cytogenet. 2008, 180, 135–139. [Google Scholar] [CrossRef]
- Winnes, M.; Enlund, F.; Mark, J.; Stenman, G. The MECT1-MAML2 gene fusion and benign Warthin’s tumor. J. Mol. Diagn. 2006, 8, 394–396. [Google Scholar] [CrossRef]
- Memon, R.A.; Prieto Granada, C.N.; Wei, S. Clear cell papillary neoplasm of the breast with MAML2 gene rearrangement: Clear cell hidradenoma or low-grade mucoepidermoid carcinoma? Pathol. Res. Pract. 2020, 216, 153140. [Google Scholar] [CrossRef]
- Tirado, Y.; Williams, M.D.; Hanna, E.Y.; Kaye, F.J.; Batsakis, J.G.; El-Naggar, A.K. CRTC1/MAML2 fusion transcript in high grade mucoepidermoid carcinomas of salivary and thyroid glands and Warthin’s tumors: Implications for histogenesis and biologic behavior. Genes Chromosom. Cancer 2007, 46, 708–715. [Google Scholar] [CrossRef]
- Enlund, F.; Behboudi, A.; Andrén, Y.; Öberg, C.; Lendahl, U.; Mark, J.; Stenman, G. Altered Notch signaling resulting from expression of a WAMTP1-MAML2 gene fusion in mucoepidermoid carcinomas and benign Warthin’s tumors. Exp. Cell Res. 2004, 292, 21–28. [Google Scholar] [CrossRef]
- Zhang, C.; Gu, T.; Hu, Y.; Sun, J.; Xia, R.; Tian, Z.; Wang, L.; Li, J. Reevaluation of Salivary Lymphadenoma: A Subgroup Identified as Warthin-like Mucoepidermoid Carcinoma Following Molecular Investigation for MAML2 Rearrangement. Arch. Pathol. Lab. Med. 2021, 145, 744–752. [Google Scholar] [CrossRef]
- Nakano, S.; Okumura, Y.; Murase, T.; Nagao, T.; Kusafuka, K.; Urano, M.; Yamamoto, H.; Kano, S.; Tsukahara, K.; Okami, K.; et al. Salivary mucoepidermoid carcinoma: Histological variants, grading systems, CRTC1/3-MAML2 fusions, and clinicopathological features. Histopathology 2022, 80, 729–735. [Google Scholar] [CrossRef]
- Ishibashi, K.; Ito, Y.; Masaki, A.; Fujii, K.; Beppu, S.; Sakakibara, T.; Takino, H.; Takase, H.; Ijichi, K.; Shimozato, K.; et al. Warthin-like Mucoepidermoid Carcinoma: A Combined Study of Fluorescence In Situ Hybridization and Whole-slide Imaging. Am. J. Surg. Pathol. 2015, 39, 1479–1487. [Google Scholar] [CrossRef]
- Bieńkowski, M.; Kunc, M.; Iliszko, M.; Kuźniacka, A.; Studniarek, M.; Biernat, W. MAML2 rearrangement as a useful diagnostic marker discriminating between Warthin tumour and Warthin-like mucoepidermoid carcinoma. Virchows Arch. 2020, 477, 393–400. [Google Scholar] [CrossRef]
- Stanford University–UCSF Evidence-Based Practice Center. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies Volume 7—Care Coordination; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2007; Volume 7. [Google Scholar]
- Silverman, J.F.; Fletcher, C.D.M.; Frable, W.J.; Goldblum, J.R.; Pereira, T.C.; Swanson, P.E. Critical diagnoses (critical values) in anatomic pathology. Hum. Pathol. 2006, 37, 982–984. [Google Scholar] [CrossRef]
- Pereira, T.C.; Silverman, J.F.; LiVolsi, V.; Fletcher, C.D.M.; Frable, W.J.; Goldblum, J.R.; Swanson, P.E. A multi-institutional survey of critical diagnoses (critical values) in surgical pathology and cytology. Am. J. Clin. Pathol. 2008, 130, 731–735. [Google Scholar] [CrossRef]
- Cretara, A.D.; Otis, C.N. Perspectives and perceptions of urgent and alert values in surgical pathology and cytopathology: A survey of clinical practitioners and pathologists. Cancer Cytopathol. 2018, 126, 970–979. [Google Scholar] [CrossRef]
- Baskovich, B.W.; Allan, R.W. Web-based synoptic reporting for cancer checklists. J. Pathol. Inform. 2011, 2, 16. [Google Scholar] [CrossRef]
- Słodkowska, J.; Cierniak, S.; Patera, J.; Kopik, J.; Baranowski, W.; Markiewicz, T.; Murawski, P.; Buda, I.; Kozłowski, W. Functional Assessment of Synoptic Pathology Reporting for Ovarian Cancer. Pathobiology 2016, 83, 70–78. [Google Scholar] [CrossRef]
- Renshaw, M.A.; Renshaw, S.A.; Mena-Allauca, M.; Carrion, P.P.; Mei, X.; Narciandi, A.; Gould, E.W.; Renshaw, A.A. Performance of a web-based method for generating synoptic reports. J. Pathol. Inform. 2017, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Campbell, W.S.; Karlsson, D.; Vreeman, D.J.; Lazenby, A.J.; Talmon, G.A.; Campbell, J.R. A computable pathology report for precision medicine: Extending an observables ontology unifying SNOMED CT and LOINC. J. Am. Med. Inform. Assoc. 2018, 25, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Sluijter, C.E.; van Workum, F.; Wiggers, T.; van de Water, C.; Visser, O.; van Slooten, H.-J.; Overbeek, L.I.H.; Nagtegaal, I.D. Improvement of Care in Patients With Colorectal Cancer: Influence of the Introduction of Standardized Structured Reporting for Pathology. JCO Clin. Cancer Inform. 2019, 3, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Messenger, D.E.; McLeod, R.S.; Kirsch, R. What impact has the introduction of a synoptic report for rectal cancer had on reporting outcomes for specialist gastrointestinal and nongastrointestinal pathologists? Arch. Pathol. Lab. Med. 2011, 135, 1471–1475. [Google Scholar] [CrossRef]
- Renshaw, A.A.; Mena-Allauca, M.; Gould, E.W.; Sirintrapun, S.J. Synoptic Reporting: Evidence-Based Review and Future Directions. JCO Clin. Cancer Inform. 2018, 2, 1–9. [Google Scholar] [CrossRef]
- Schmidt, H.G.; Norman, G.R.; Boshuizen, H.P.A. A cognitive perspective on medical expertise: Theory and implications. Acad. Med. 1990, 65, 611–621. [Google Scholar] [CrossRef]
- Bartels, P.H. The diagnostic pattern in histopathology. Am. J. Clin. Pathol. 1989, 91, S7–S13. [Google Scholar]
- van Ginneken, A.M.; van der Lei, J. Understanding differential diagnostic disagreement in pathology. Proc. Annu. Symp. Comput. Appl. Med. Care 1991, 1991, 99–103. [Google Scholar]
- Crowley, R.S.; Naus, G.J.; Stewart, J.; Friedman, C.P. Development of visual diagnostic expertise in pathology: An information-processing study. J. Am. Med. Inform. Assoc. 2003, 10, 39–51. [Google Scholar] [CrossRef]
- Nogichi, K.; Kanda, S.; Yoshida KFunaoka, Y.; Yamanegi, K.; Yoshikawa, K.; Takaoka, K.; Kishimoto, H.; Nakano, Y. Establishment of a patient-derived mucoepidermoid carcinoma cell line with the CRTC1-MAML2 fusion gene. Mol. Clin. Oncol. 2022, 16, 75. [Google Scholar] [CrossRef]
- Bishop, J.A.; Rooper, L.M.; Chiosea, S.I.; Westra, W.H. Clear Cell Carcinoma of Salivary Glands Is Frequently p16 Positive. Am. J. Surg. Pathol. 2018, 42, 367–371. [Google Scholar] [CrossRef]
- Tian, S.; Switchenko, J.M.; Jhaveri, J.; Cassidy, R.J.; Ferris, M.J.; Press, R.H.; Pfister, N.T.; Patel, M.R.; Saba, N.F.; McDonald, M.W.; et al. Survival outcomes by high-risk human papillomavirus status in nonoropharyngeal head and neck squamous cell carcinomas: A propensity-scored analysis of the National Cancer Data Base. Cancer 2019, 125, 2782–2793. [Google Scholar] [CrossRef]
- Barragán-Montero, A.; Javaid, U.; Valdés, G.; Nguyen, D.; Desbordes, P.; Macq, B.; Willems, S.; Vandewinckele, L.; Holmström, M.; Löfman, F.; et al. Artificial intelligence and machine learning for medical imaging: A technology review. Phys. Med. 2021, 83, 242–256. [Google Scholar] [CrossRef]
- Försch, S.; Klauschen, F.; Hufnagl, P.; Roth, W. Artificial intelligence in pathology. Dtsch. Aerzteblatt Online 2021, 118, 199–204. [Google Scholar] [CrossRef]




| Cases | Total | MAML2+/Total | % | Fusion |
|---|---|---|---|---|
| All | 8106 | 23/8106 | 0.28% | |
| Head and neck | 307 | 18/307 | 5.86% | |
| Head and neck/all MAML2+ | - | 18/23 | 78.3% | MAML2 (exon2)–CRTC1 (exon1), n = 17 |
| MAML2 (exon2)–CRTC3 (exon1), n = 1 | ||||
| Other than head and neck | 7799 | 5/7799 | 0.06% | |
| Brain | 742 | 1/742 | 0.13% | MAML2 (exon2)–YAP1 (exon5), n = 1 |
| Breast | 414 | 2/414 | 0.48% | MAML2 (exon2)–CRTC1 (exon1), n = 2 |
| Thymus | 16 | 1/16 | 6.25% | MAML2 (exon2)–KMT2A (exon10), n = 1 |
| Lung | 2364 | 1/2364 | 0.04% | MAML2 (exon3)–SAMSN1 (exon2), n = 1 |
| Setting | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Youden’s J-Index |
|---|---|---|---|---|---|
| Literature | 62 | 100 | 100 | 18 | 0.62 |
| Salivary gland | 60 | 100 | 100 | 73 | 0.60 |
| Test order analysis | |||||
| Confirmatory testing * | 70 | 100 | 100 | 67 | 0.70 |
| Confirmatory testing | 62 | 100 | 100 | 81 | 0.62 |
| Diagnostic testing | 33 | 100 | 100 | 67 | 0.33 |
| Scenario Working Dx > MDx > Final Dx | RII | RII Rank | SRO | SRO Rank | Description | RWE% | Markov |
|---|---|---|---|---|---|---|---|
| MEC MAML2+ MEC | 0.80 | 1 | 25 | 1 | Molecular confirmation | 12.7 | 0.3 |
| ASC MAML2− ASC | 0.65 | 3 | 40 | 2 | Molecular confirmation * | 43.6 | 0.96 |
| ASC MAML2+ MEC | 0.68 | 2 | 47 | 3 | Re-classified via molecular | 0 | 0 |
| Other MAML2+ MEC | 0.59 | 4 | 51 | 4 | Re-classified via molecular | 3.5 | 0.29 |
| MEC MAML2− MEC | 0.39 | 7 | 59 | 5 | “Molecularly unchanged” | 10.9 | 0.26 |
| Other MAML2− Other | 0.51 | 5 | 68 | 6 | Molecular confirmation * | 7.2 | 0.57 |
| Other MAML2+ Other | 0.43 | 6 | 74 | 7 | Molecularly unchanged | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thierauf, J.C.; Farahani, A.A.; Indave, B.I.; Bard, A.Z.; White, V.A.; Smith, C.R.; Marble, H.; Hyrcza, M.D.; Chan, J.K.C.; Bishop, J.; et al. Diagnostic Value of MAML2 Rearrangements in Mucoepidermoid Carcinoma. Int. J. Mol. Sci. 2022, 23, 4322. https://doi.org/10.3390/ijms23084322
Thierauf JC, Farahani AA, Indave BI, Bard AZ, White VA, Smith CR, Marble H, Hyrcza MD, Chan JKC, Bishop J, et al. Diagnostic Value of MAML2 Rearrangements in Mucoepidermoid Carcinoma. International Journal of Molecular Sciences. 2022; 23(8):4322. https://doi.org/10.3390/ijms23084322
Chicago/Turabian StyleThierauf, Julia C., Alex A. Farahani, B. Iciar Indave, Adam Z. Bard, Valerie A. White, Cameron R. Smith, Hetal Marble, Martin D. Hyrcza, John K. C. Chan, Justin Bishop, and et al. 2022. "Diagnostic Value of MAML2 Rearrangements in Mucoepidermoid Carcinoma" International Journal of Molecular Sciences 23, no. 8: 4322. https://doi.org/10.3390/ijms23084322
APA StyleThierauf, J. C., Farahani, A. A., Indave, B. I., Bard, A. Z., White, V. A., Smith, C. R., Marble, H., Hyrcza, M. D., Chan, J. K. C., Bishop, J., Shi, Q., Ely, K., Agaimy, A., Martinez-Lage, M., Nose, V., Rivera, M., Nardi, V., Dias-Santagata, D., Garg, S., ... Lennerz, J. K. (2022). Diagnostic Value of MAML2 Rearrangements in Mucoepidermoid Carcinoma. International Journal of Molecular Sciences, 23(8), 4322. https://doi.org/10.3390/ijms23084322







