Applications of Metal-Organic Frameworks as Drug Delivery Systems
Abstract
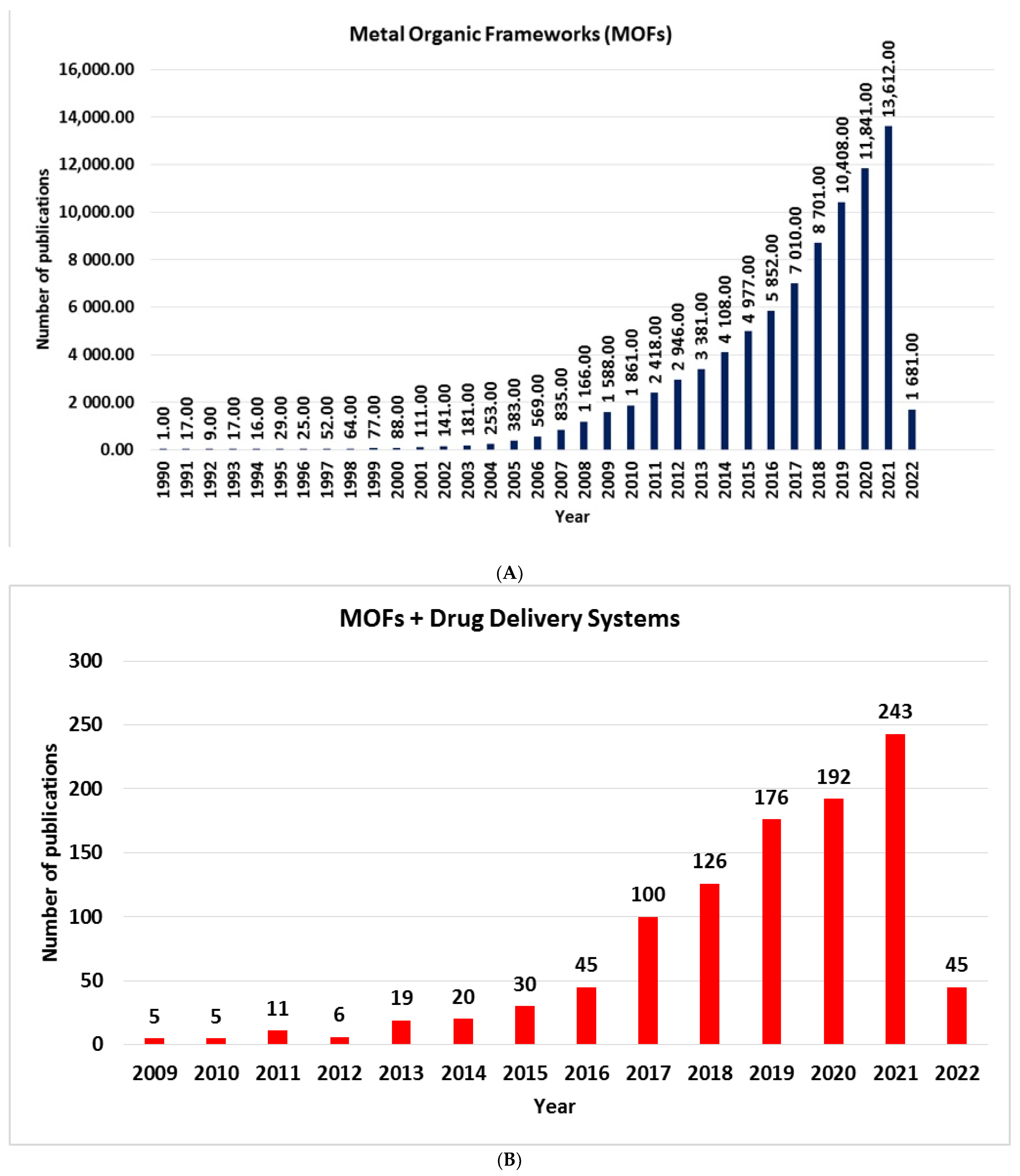
:1. Introduction
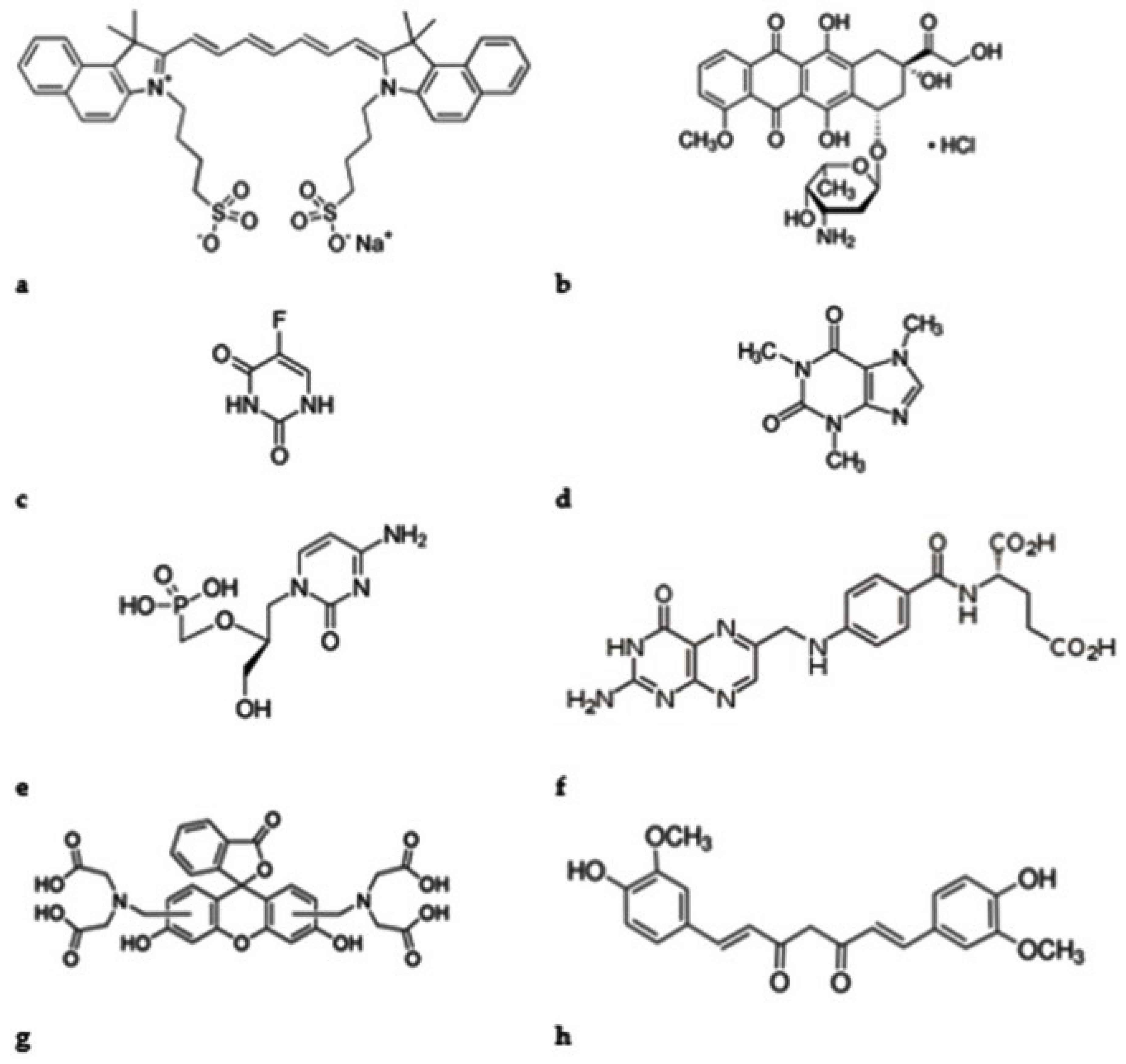
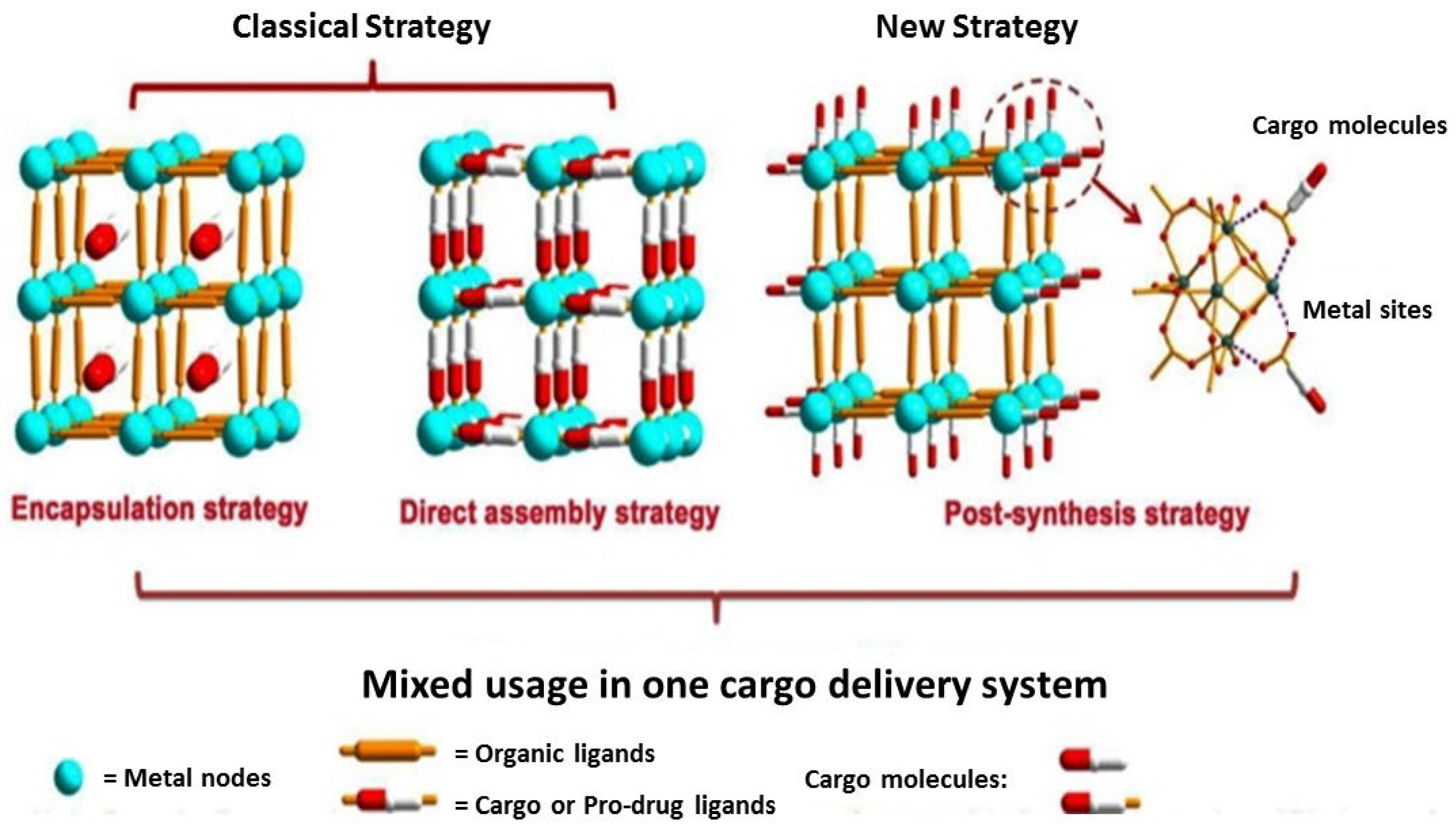
2. Modification of MOFs—Cargo Loading Strategies
- Encapsulation strategy: Cargo is situated inside of the MOFs pores or channels by noncovalent bonding interaction. This type of strategy does not alter the MOF framework structures.
- Direct assembly strategy: The interaction between MOFs and cargo is coordination bonds. The cargo participate in the synthetic reaction as ligands to partly contribute to the construction of MOFs.
- Post-synthesis strategy: The cargo molecules are located in MOFs surfaces. These molecules serve as linkers for pre-synthesized MOFs. The chemical interactions implied by this strategy are coordination bonds and covalent bonds between metal nodes/organic linkers and used cargo. This type of strategy does not alter the MOF framework structures. The second possibility as a post-synthesis strategy is adsorption on MOF surfaces. In general, the main forces in adsorption are weak interactions, such as π–π and Van der Waals interactions, and hydrogen bonding.
2.1. Encapsulation Strategy
2.2. Direct Assembly Strategy
2.3. Post-Synthesis Strategy
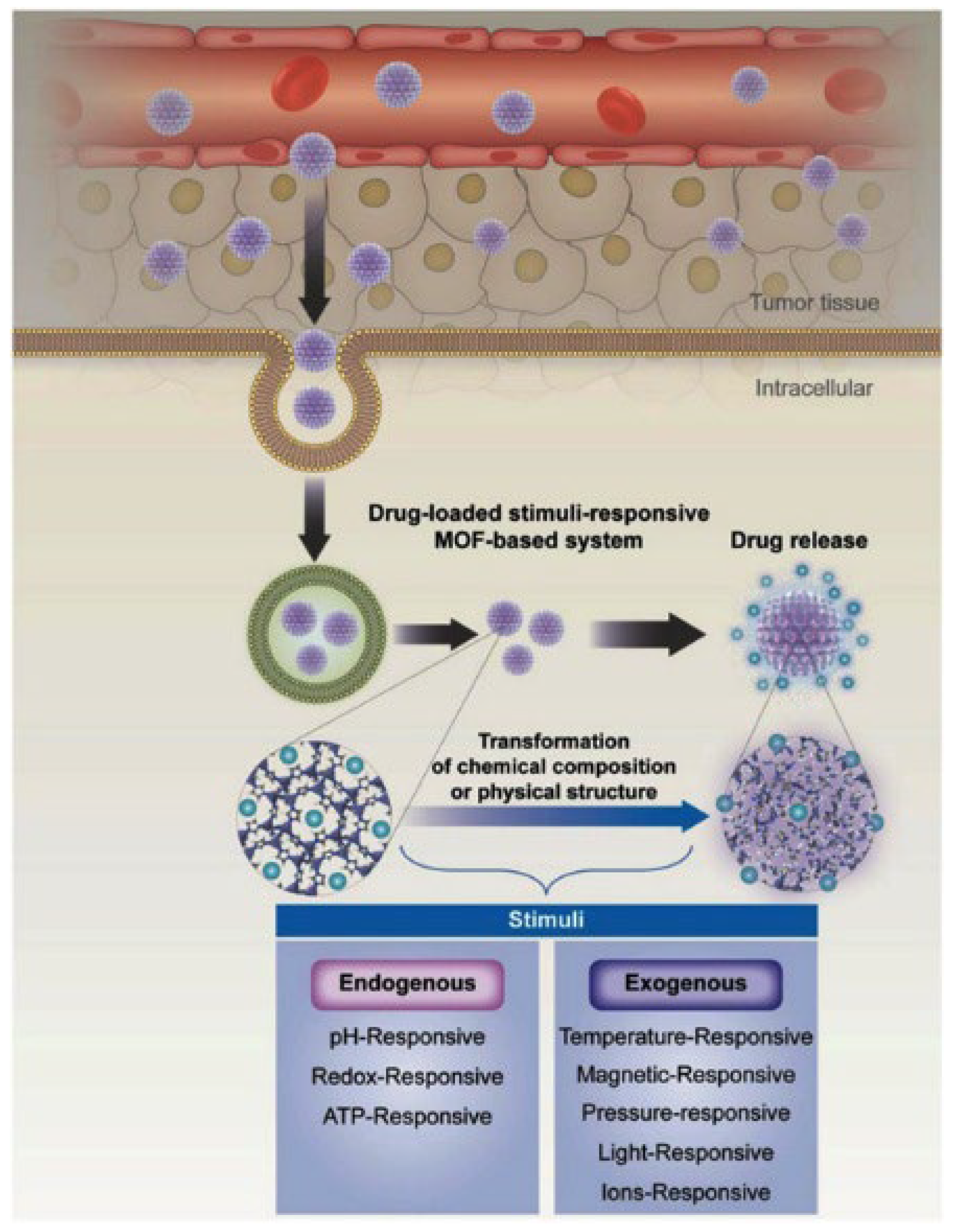
3. Stimuli Responsive for MOFs as DDSs
4. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 5-Fu | 5-Fluorouracil |
| Cal | Calcein |
| CpG ODN | Cytosine-phosphate-guanine sequence–oligo nucleotides |
| Cur | Curcumin |
| DDSs | Drug delivery systems |
| DNA | Deoxyribonucleic acid |
| HKUST | Hong Kong University of Science and Technology |
| HEPES | 4-(2-hydroxyethyl) piperazine-1-ethane sulfonic acid |
| ICG | Indocianine green |
| MOFs | Metal Organic Frameworks |
| US FDA | US Food and Drug Administration |
| NIR | Near-infrared |
| MIL | Materials of Institute Lavoisier |
| NEM | N-ethylmorpholine |
| DOX | Doxorubicin hydrochloride |
| FA | Folic acid |
| HSAB | Hard–Soft Acid–Base |
| H-PMOF | Porphyrinic MOF nanoplatform |
| PDT | Photodynamic therapy |
| PDA | Polydopamine |
| PEG | Polyethylene glycol |
| PB | Phosphate buffer |
| RBC | Red blood cell |
| RNA | Ribonucleic acid |
| TRIS | 2-Amino-2-(hydroxymethyl)-1:3-propanediol |
| UiO | Universitetet I Oslo |
| ZIF | Zeolitic imidazole framework |
References
- Dzhardimalieva, G.I.; Rabinskiy, L.N.; Kydralieva, K.A.; Uflyand, I.E. Recent advances in metallopolymer-based drug delivery systems. RSC Adv. 2019, 9, 37009–37051. [Google Scholar] [CrossRef] [Green Version]
- Adepu, S.; Ramakrishna, S. Controlled Drug Delivery Systems: Current Status and Future Directions. Molecules 2021, 26, 5905. [Google Scholar] [CrossRef]
- Zhang, W.; Zhang, Z.; Zhang, Y. The application of carbon nanotubes in target drug delivery systems for cancer therapies. Nanoscale Res. Lett. 2011, 6, 555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahamathulla, M.; Bhosale, R.R.; Osmani, R.A.M.; Mahima, C.K.; Johnson, P.A.; Hani, U.; Ghazwani, M.; Begum, M.Y.; Alshehri, S.; Ghoneim, M.M.; et al. Carbon nanotubes: Current perspectives on diverse applications in targeted drug delivery and therapies. Materials 2021, 14, 6707. [Google Scholar] [CrossRef] [PubMed]
- Jampilek, J.; Kralova, K. Advances in drug delivery nanosystems using graphene-based materials and carbon nanotubes. Materials 2021, 14, 1059. [Google Scholar] [CrossRef]
- Aslam, H.; Shukrullah, S.; Naz, M.Y.; Fatima, H.; Hussain, H.; Ullah, S.; Assiri, M.A. Current and future perspectives of multifunctional magnetic nanoparticles based controlled drug delivery systems. J. Drug Deliv. Sci. Technol. 2021, 67, 102946. [Google Scholar] [CrossRef]
- Kalubowilage, M.; Janik, K.; Bossmann, S.H. Magnetic Nanomaterials for Magnetically-Aided Drug Delivery and Hyperthermia. Appl. Sci. 2019, 9, 2927. [Google Scholar] [CrossRef] [Green Version]
- Twana, M.; Keng, W.; Wing, M.L.; Vitaliy, V.K. Silica nanoparticles in transmucosal drug delivery. Pharmaceutics 2020, 12, 751. [Google Scholar]
- Vallet-Regí, M.; Colilla, M.; Izquierdo-Barba, I.; Manzano, M. Mesoporous silica nanoparticles for drug delivery: Current insights. Molecules 2018, 23, 47. [Google Scholar] [CrossRef] [Green Version]
- Zhu, F.; Tan, G.; Zhong, Y.; Jiang, Y.; Cai, L.; You, Z.; Liu, S.; Ren, F. Smart nanoplatform for sequential drug release and enhanced chemo-thermal effect of dual drug loaded gold nanorod vesicles for cancer therapy. J. Nanobiotechnol. 2019, 17, 44. [Google Scholar] [CrossRef]
- Zhang, H.; Gao, Z.; Li, X.; Li, L.; Ye, S.; Tang, B. Multiple-mRNA-controlled and heat-driven drug release from gold nanocages in targeted chemo-photothermal therapy for tumors. Chem. Sci. 2021, 12, 12429–12436. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Li, X.; Tang, K.; Song, Z.; Luo, X.A. AuNP-capped cage fluorescent biosensor based on controlled-release and cyclic enzymatic amplification for ultrasensitive detection of ATP. J. Mater. Chem. B 2020, 8, 5945. [Google Scholar] [CrossRef] [PubMed]
- Maranescu, B.; Visa, A.; Mracec, M.; Ilia, G.; Maranescu, V.; Simon, Z.; Mracec, M. Lamellar Co2+ vinylphosphonate metal organic framework.PM3 semi-empirical analysis of structural properties. Rev. Roum. Chim. 2011, 56, 473–482. [Google Scholar]
- Visa, A.; Mracec, M.; Maranescu, B.; Maranescu, V.; Ilia, G.; Popa, A.; Mracec, M. Structure simulation into a lamellar supramolecular network and calculation of the metal ions/ligands ratio. Chem. Cent. J. 2012, 6, 91. [Google Scholar] [CrossRef] [Green Version]
- Visa, A.; Maranescu, B.; Bucur, A.; Iliescu, S.; Demadis, K. Synthesis and characterization of a novel phosphonate metal organic framework starting from copper salts. Phosphorus Sulfur Silicon Relat. Elem. 2014, 189, 630–639. [Google Scholar] [CrossRef]
- Maranescu, B.; Visa, A.; Ilia, G.; Simon, Z.; Demadis, K.; Colodrero, R.M.P.; Cabeza, A.; Vallcorba, O.; Rius, J.; Choquesillo-Lazarte, D. Synthesis and characterization of styryl phosphonic acid and its use as new ligand for phosphonate metal organic framework. J. Coord. Chem. 2014, 67, 1562–1572. [Google Scholar] [CrossRef]
- Li, H.; Li, L.; Lin, R.B.; Zhou, W.; Zhang, Z.; Xiang, S.; Chen, B. Porous metal-organic frameworks for gas storage and separation: Status and challenges. Energy Chem. 2019, 1, 100006. [Google Scholar] [CrossRef]
- Dolgopolova, E.A.; Rice, A.M.; Martina, C.R.; Shustova, N.B. Photochemistry and photophysics of MOFs: Steps towards MOF-based sensing enhancements. Chem. Soc. Rev. 2018, 47, 4710–4728. [Google Scholar] [CrossRef]
- Bazaga-García, M.; Vílchez-Cózar, Á.; Maranescu, B.; Olivera-Pastor, P.; Marganovici, M.; Ilia, G.; Cabeza Díaz, A.; Visa, A.; Colodrero, R.M.P. Synthesis and electrochemical properties of metal(II)-carboxyethylphenylphosphinates. Dalton. Trans. 2021, 50, 6539–6548. [Google Scholar] [CrossRef]
- Song, J.; Hua, M.; Huang, X.; Visa, A.; Wu, T.; Hou, M.; Zhang, Z.; Han, B. Highly Efficient Meerwein-Ponndorf-Verley Reductions Over a Robust Zirconium-Organoboronic Acid Hybrid. Green Chem. 2021, 23, 1259–1265. [Google Scholar] [CrossRef]
- Iliescu, S.; Ilia, G.; Pascariu, A.; Popa, A.; Plesu, N. Novel synthesis of phosphorus containing polymers under inverse phase transfer catalysis. Polymer 2006, 47, 6509–6512. [Google Scholar] [CrossRef]
- Nabipour, H.; Wang, X.; Song, L.; Hu, Y. Metal-organic frameworks for flame retardant polymers application: A critical review. Compos. Part A Appl. Sci. 2020, 139, 106113. [Google Scholar] [CrossRef]
- Drehe, M.; Simulescu, V.; Ilia, G. Progress in the development of flame retardants. Rev. Chem. Eng. 2006, 24, 263–302. [Google Scholar]
- Macarie, L.; Simulescu, V.; Ilia, G. Ultrasonic irradiation used in synthesis of aminophosphonates. Monatsh Chem. 2019, 150, 163–171. [Google Scholar] [CrossRef]
- Maranescu, B.; Lupa, L.; Tara Lunga Mihali, M.; Plesu, N.; Maranescu, V.; Visa, A. The corrosion inhibitor behavior of iron in saline solution by the action of magnesium carboxyphosphonate. Pure Appl. Chem. 2018, 90, 1713–1722. [Google Scholar] [CrossRef]
- Maranescu, B.; Plesu, N.; Visa, A. Phosphonic acid vs phosphonate metal organic framework influence on mild steel corrosion protection. Appl. Surface Sci. 2019, 497, 143734. [Google Scholar] [CrossRef]
- Li, H.; Wang, K.; Sun, Y.; Lollar, C.T.; Li, J.; Zhou, H.-C. Recent advances in gas storage and separation using metal–organic frameworks. Mater. Today 2018, 21, 108–121. [Google Scholar] [CrossRef]
- Lupa, L.; Maranescu, B.; Visa, A. Equilibrium and kinetic studies of chromium ions adsorption on Co(II) based phosphonate metal organic frameworks. Sep. Sci. Technol. 2018, 53, 1017–1026. [Google Scholar] [CrossRef]
- Nistor, M.A.; Muntean, S.G.; Maranescu, B.; Visa, A. Phosphonate metal organic frameworks used as dyes removal materials from wastewaters. Appl. Organomet. Chem. 2020, 34, e5939. [Google Scholar] [CrossRef]
- Maranescu, B.; Lupa, L.; Visa, A. Synthesis, characterization and rare earth elements adsorption properties of phosphonate metal organic frameworks. Appl. Surface Sci. 2019, 481, 83–91. [Google Scholar] [CrossRef]
- Baby, R.; Hussein, M.Z.; Abdullah, A.H.; Zainal, Z. Nanomaterials for the treatment of heavy metal contaminated water. Polymers 2022, 14, 583. [Google Scholar] [CrossRef] [PubMed]
- Visa, A.; Maranescu, B.; Lupa, L.; Crisan, L.; Borota, A. New efficient adsorbent materials in the removal process of Cd(II) from aqueous solutions. Nanomaterials 2020, 10, 899. [Google Scholar] [CrossRef] [PubMed]
- Maranescu, B.; Lupa, L.; Visa, A. Synthesis, characterizations and Pb(II) sorption properties of cobalt phosphonate materials. Pure Appl. Chem. 2016, 88, 979–992. [Google Scholar] [CrossRef] [Green Version]
- Maranescu, B.; Popa, A.; Lupa, L.; Maranescu, V.; Visa, A. Use of chitosan complex with aminophosphonic groups and cobalt for the removal of Sr2+ ions. Sep. Sci. Technol. 2018, 53, 1058–1064. [Google Scholar]
- Al Sharabati, M.; Sabouni, R.; Ghaleb, A.; Husseini, G.A. Biomedical applications of metal–organic frameworks for disease diagnosis and drug delivery: A review. Nanomaterials 2022, 12, 277. [Google Scholar] [CrossRef]
- Popa, A.; Ilia, G.; Iliescu, S.; Dehelean, G.; Pascariu, A.; Bora, A.; Pacureanu, L. Mixed quaternary ammonium and phosphonium salts bound to macromolecular supports for removal bacteria from water. Mol. Cryst. Liq. Cryst. 2004, 418, 195–203. [Google Scholar] [CrossRef]
- Pettinari, C.; Pettinari, R.; Di Nicola, C.; Tombesi, A.; Scuri, S.; Marchetti, F. Antimicrobial MOFs. Coord. Chem. Rev. 2021, 446, 214121. [Google Scholar] [CrossRef]
- Popa, A.; Ilia, G.; Pascariu, A.; Iliescu, S.; Plesu, N. Grafted styrene-divinylbenzene copolymers containing benzaldehyde and their Wittig reactions with various phosphonium salts. Chin. J. Polym. Sci. 2005, 23, 651–656. [Google Scholar] [CrossRef]
- Quijia, C.R.; Lima, R.; Silva, C.; Alves, C.R.; Frem, R.; Chorilli, M. Application of MIL-100(Fe) in drug delivery and biomedicine. J. Drug. Deliv. Sci. Technol. 2021, 61, 102217. [Google Scholar] [CrossRef]
- Vassaki, M.; Kotoula, C.; Turhanen, P.; Choquesillo-Lazarte, D.; Demadis, K.D. Calcium and strontium coordination polymers as controlled delivery systems of the anti-osteoporosis drug risedronate and the augmenting effect of solubilizers. Appl. Sci. 2021, 11, 11383. [Google Scholar] [CrossRef]
- Vaughn, J.; Wu, H.; Efremovska, B.; Olson, D.H.; Mattai, J.; Ortiz, C.; Puchalski, A.; Li, J.; Pan, L. Encapsulated recyclable porous materials: An effective moisture-triggered fragrance release system. Chem. Comm. 2013, 49, 5724–5726. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Lepoitevin, M.; Serre, C. Metal–organic frameworks towards bio-medical applications. Mater. Chem. Front. 2021, 5, 5573–5594. [Google Scholar] [CrossRef]
- Sun, Y.; Zheng, L.; Yang, Y.; Fu, F.; Li, X.; Yang, Z.; Yan, H.; Cui, C.; Tan, W.N. Metal–organic framework nanocarriers for drug delivery in biomedical applications. Nano-Micro Lett. 2020, 12, 103. [Google Scholar] [CrossRef] [PubMed]
- Mallakpour, S.; Nikkhoo, E.; Hussain, C.M. Application of MOF materials as drug delivery systems for cancer therapy and dermal treatment. Coord. Chem. Rev. 2022, 451, 214262. [Google Scholar] [CrossRef]
- Jeyaseelan, C.; Jain, P.; Soin, D.; Gupta, G. Metal organic frameworks: An effective application in drug delivery systems. Inorg. Nano-Met. Chem. 2021. [Google Scholar] [CrossRef]
- Martí-Rujas, J. Structural elucidation of microcrystalline MOFs from powder X-ray diffraction. Dalton Trans. 2020, 49, 13897. [Google Scholar] [CrossRef]
- Torresi, S.; Famulari, A.; Martí-Rujas, J. Kinetically Controlled Fast Crystallization of M12L8 Poly-[n]-catenanes Using the 2,4,6-Tris(4-pyridyl)benzene Ligand and ZnCl2 in an Aromatic Environment. J. Am. Chem. Soc. 2020, 142, 9537–9543. [Google Scholar] [CrossRef]
- Guo, F.; Wang, H.-C.; Famulari, A.; Lu, H.-D.; Martí-Rujas, J. Dynamic behaviour in nonporous hybrid metal–organic materials via mechanochemical and gas–solid reactions. CrystEngComm 2018, 20, 6721–6726. [Google Scholar] [CrossRef]
- Silva, P.; Vilela, S.M.F.; João, P.C.; Tome, J.P.C.; Almeida Paz, F.A. Multifunctional metal–organic frameworks: From academia to industrial applications. Chem. Soc. Rev. 2015, 44, 6774–6803. [Google Scholar] [CrossRef] [Green Version]
- Sun, C.-Y.; Qin, C.; Wang, X.-L.; Suet, Z.M. Metal–organic frameworks as potential drug delivery systems. Expert Opin. Drug Deliv. 2013, 10, 89–101. [Google Scholar] [CrossRef]
- Wang, L.; Zheng, M.; Xie, Z. Nanoscale metal–organic frameworks for drug delivery: A conventional platform with new promise. J. Mater. Chem. B 2018, 6, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Petric, M.; Crisan, L.; Crisan, M.; Micle, A.; Maranescu, B.; Ilia, G. Synthesis and QSRR Study for a Series of Phosphoramidic Acid Derivatives. Heteroatom Chem. 2013, 24, 138–145. [Google Scholar] [CrossRef]
- Gheonea, R.; Mak, C.; Crasmareanu, E.C.; Simulescu, V.; Plesu, N.; Ilia, G. Surface modification of SnO2 with phosphonic acids. J. Chem. 2017, 2017, 2105938. [Google Scholar] [CrossRef] [Green Version]
- Mohammed, L.; Gomaa, H.G.; Ragab, D.; Zhu, J. Magnetic nanoparticles for environmental and biomedical applications: A review. Particuology 2017, 30, 1–14. [Google Scholar] [CrossRef]
- Bunzen, H. Chemical stability of metal-organic frameworks for applications in drug delivery. ChemNanoMat 2021, 7, 998–1007. [Google Scholar] [CrossRef]
- Bůžek, D.; Adamec, S.; Lang, K.; Demel, J. Metal–organic frameworks vs. buffers: Case study of UiO-66 stability. Inorg. Chem. Front. 2021, 8, 720–734. [Google Scholar] [CrossRef]
- Velásquez-Hernández, M.J.; Linares-Moreau, M.; Astria, E.; Carraro, F.; Alyami, M.Z.; Khashab, N.M.; Sumby, C.J.; Doonan, C.J.; Falcaro, P. Towards applications of bioentities@MOFs in biomedicine. Coord. Chem. Rev. 2021, 429, 213651. [Google Scholar] [CrossRef]
- Raliya, R.; Chadha, T.S.; Hadad, K.; Biswas, P. Perspective on nanoparticle technology for biomedical use. Curr. Pharm. Des. 2016, 22, 2481–2490. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Q.; Zhang, L.; Wu, H. Nanomaterials for cancer therapies. Nanotechnol. Rev. 2017, 6, 473–496. [Google Scholar] [CrossRef]
- Lai, S.K.; Wang, Y.-Y.; Hida, K.; Cone, R.; Hanes, J. Nanoparticles reveal that human cervicovaginal mucus is riddled with pores larger than viruses. Proc. Natl. Acad. Sci. USA 2010, 107, 598–603. [Google Scholar] [CrossRef] [Green Version]
- Li, B.; Chrzanowski, M.; Zhang, Y.; Ma, S. Applications of metal-organic frameworks featuring multi-functional sites. Coord. Chem. Rev. 2016, 307, 106–129. [Google Scholar] [CrossRef] [Green Version]
- Hannah, A.; Wilson, K.; Homan, K.; Emelianov, S. Indocyanine green-loaded photoacoustic nanodroplets: Dual contrast nanoconstructs for enhanced photoacoustic and ultrasound imaging. ACS Nano 2014, 8, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Dai, Q.; Ren, E.; Xu, D.; Zeng, Y.; Chen, C.; Liu, G. Indocyanine green-based nanodrugs: A portfolio strategy for precision medicine. Prog. Nat. Sci. 2020, 30, 577–588. [Google Scholar] [CrossRef]
- Jung, H.S.; Verwilst, P.; Sharma, A.; Shin, J.; Sessler, J.L.; Kim, J.S. Organic molecule-based photothermal agents: An expanding photothermal therapy universe. Chem. Soc. Rev. 2018, 47, 2280–2297. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, A.; Mihir, G.S.; Purkait, K. Fe3O4 promoted metal organic framework MIL-100(Fe) for the controlled release of doxorubicin hydrochloride. Micropor. Mesopor. Mat. 2018, 259, 203–210. [Google Scholar] [CrossRef]
- Yang, C.; Xu, J.; Yang, D.; Wang, X.; Liu, B.; He, N.; Wang, Z. ICG@ZIF-8: One-step encapsulation of Indocyanine Green in ZIF-8 and use as a therapeutic nanoplatform. Chin. Chem. Lett. 2018, 29, 1421–1424. [Google Scholar] [CrossRef]
- Bhattacharjee, A.; Purkaita, M.K.; Gumma, S. Loading and release of doxorubicin hydrochloride from iron(III) trimesate MOF and zinc oxide nanoparticle composites. Dalton Trans. 2020, 49, 8755–8763. [Google Scholar] [CrossRef]
- Yao, L.; Tang, Y.; Cao, W.; Yuanjing Cui, Y.; Qian, G. Highly efficient encapsulation of doxorubicin hydrochloride in metal–organic frameworks for synergistic chemotherapy and chemodynamic therapy. ACS Biomater. Sci. Eng. 2021, 7, 4999–5006. [Google Scholar] [CrossRef]
- Mojardin, L.; Botet, J.; Quintales, L.; Moreno, S.; Salas, M. New Insights into the RNA based mechanism of action of the anticancer drug 5′-fluorouracil in eukaryotic cells. PLoS ONE 2013, 8, e78172. [Google Scholar] [CrossRef] [Green Version]
- Stefaniak, K.R.; Epley, C.C.; Novak, J.J.; McAndrew, M.L.; Cornell, H.D.; Zhu, J.; McDaniel, D.K.; Davis, J.L.; Allen, I.C.; Morris, A.J.; et al. Photo-triggered release of 5-fluorouracil from a MOF drug delivery vehicle. Chem. Commun. 2018, 54, 7617–7620. [Google Scholar] [CrossRef]
- Sun, X.Y.; Zhang, H.J.; Zhao, X.Y.; Sun, Q.; Yuan-Yuan Wanga, Y.-Y.; Gao, E.Y. Dual functions of pH-sensitive cation Zr-MOF for 5-Fu: Large drug-loading capacity and high-sensitivity fluorescence detection. Dalton Trans. 2021, 50, 10524–10532. [Google Scholar] [CrossRef] [PubMed]
- Márquez, A.G.; Hidalgo, T.; Lana, H.; Cunha, D.; Blanco-Prieto, M.J.; Álvarez-Lorenzo, C.; Boissière, C.; Sánchez, C.; Serrea, C.; Horcajada, P. Biocompatible polymer–metal–organic framework composite patches for cutaneous administration of cosmetic molecules. J. Mater. Chem. B 2016, 4, 7031–7040. [Google Scholar] [CrossRef] [PubMed]
- Liédana, N.; Galve, A.; Rubio, C.; Téllez, C.; Coronas, J. CAF@ZIF-8: One-step encapsulation of caffeine in MOF. ACS Appl. Mater. Interfaces 2012, 4, 5016–5021. [Google Scholar] [CrossRef] [PubMed]
- Gaudin, C.; Cunha, D.; Ivanoff, E.; Horcajada, P.; Chevé, G.; Yasri, A.; Loget, O.; Serre, C.; Maurin, G. A Quantitative Structure Activity Relationship Approach to Probe the Influence of the Functionalization on the Drug Encapsulation of Porous Metal-organic Frameworks. Microporous Mesoporous Mater. 2012, 157, 124–130. [Google Scholar] [CrossRef]
- Xu, W.; Lou, Y.; Chen, W.; Kang, Y. Folic acid decorated metal-organic frameworks loaded with doxorubicin for tumor-targeted chemotherapy of osteosarcoma. Biomed Technol. 2020, 65, 229–236. [Google Scholar] [CrossRef]
- Prabaharan, M.; Grailer, J.J.; Pilla, S.; Steeber, D.A.; Gong, S.Q. Folate-conjugated Amphiphilic Hyperbranched Block Copolymers based on Boltorn®H40, Poly(l-lactide) and Poly(ethylene glycol) for Tumor-targeted Drug Delivery. Biomaterials 2009, 30, 3009–3019. [Google Scholar] [CrossRef]
- Mansoori, G.A.; Brandenburg, K.S.; Shakeri-Zadeh, A. A Comparative study of two folate-conjugated gold nanoparticles for cancer nanotechnology applications. Cancers 2010, 2, 1911–1928. [Google Scholar] [CrossRef] [Green Version]
- Orellana-Tavra, C.; Baxter, E.F.; Tian, T.; Bennett, T.D.; Slater, N.K.H.; Cheetham, A.K.; Fairen-Jimenez, D. Amorphous metal–organic frameworks for drug delivery. Chem. Commun. 2015, 51, 13878–13881. [Google Scholar] [CrossRef] [Green Version]
- Yalamandala, B.N.; Shen, W.T.; Min, S.-H.; Chiang, W.-H.; Chang, S.J.; Hu, S.-H. Advances in functional metal-organic frameworks based on-demand drug delivery systems for tumor therapeutics. Adv. NanoBiomed Res. 2021, 1, 2100014. [Google Scholar] [CrossRef]
- Tomeh, M.A.; Hadianamrei, R.; Zhao, X. A review of curcumin and its derivatives as anticancer agents. Int. J. Mol. Sci. 2019, 20, 1033. [Google Scholar] [CrossRef] [Green Version]
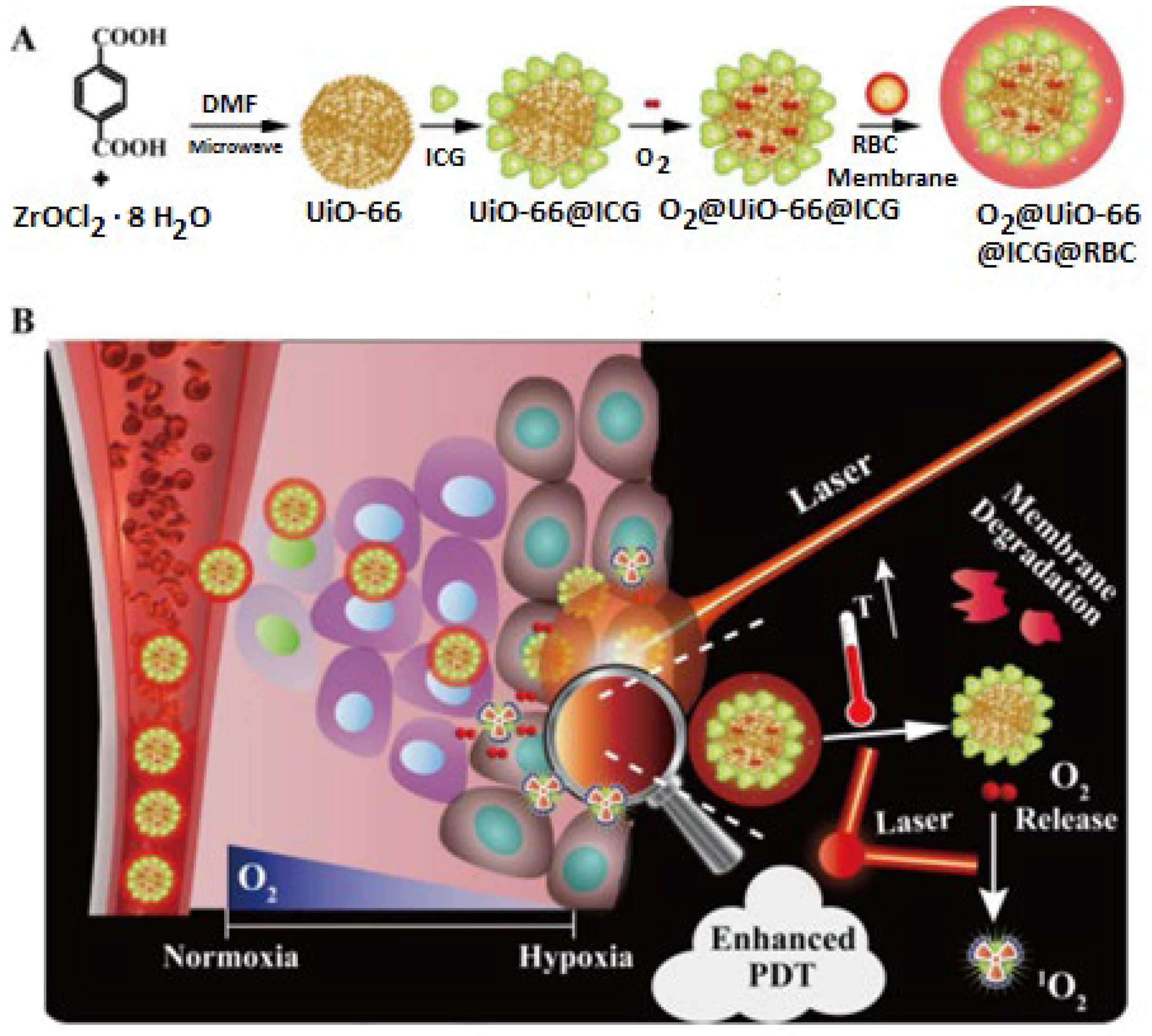
- Gao, S.; Zheng, P.; Li, Z.; Feng, X.; Yan, W.; Chen, S.; Guo, W.; Liu, D.; Yang, X.; Wang, S.; et al. Biomimetic O2- evolving metal-organic framework nanoplatform for highly efficient photodynamic therapy against hypoxic tumor. Biomaterials 2018, 178, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.C.; Ren, E.; Zhang, Y.M.; Yu, J.W.; Lin, H.R.; Pang, X.; Zhang, Y.; Liu, H.; Qin, Z.N.; Cheng, Y.; et al. Zinc(II)-dipicolylamine coordination nanotheranostics: Toward synergistic nanomedicine by combined photo/gene therapy. Angew. Chem. Int. Ed. 2019, 58, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Cen, D.; Wang, Y.F.; Wu, Y.J.; Cai, X.J.; Li, X.; Han, G.R. ZnS@ZIF-8 core-shell nanoparticles incorporated with ICG and TPZ to enable H2S-amplified synergistic therapy. Theranostics 2020, 10, 7671–7682. [Google Scholar] [CrossRef]
- You, Q.; Zhang, K.Y.; Liu, J.Y.; Liu, C.L.; Wang, H.Y.; Wang, M.T.; Ye, S.Y.; Gao, H.Q.; Lv, L.T.; Wang, C.; et al. Persistent regulation of tumor hypoxia microenvironment via a bioinspired Pt-based oxygen nanogenerator for multimodal imaging-guided synergistic phototherapy. Adv. Sci. 2020, 7, 1903341. [Google Scholar] [CrossRef] [PubMed]
- Fan, Z.; Liu, H.; Xue, Y.; Lin, J.; Fu, Y.; Xia, Z.; Pan, D.; Zhang, J.; Qiao, K.; Zhang, Z.; et al. Reversing cold tumors to hot: An immunoadjuvant-functionalized metal-organic framework for multimodal imaging-guided synergistic photoimmunotherapy. Bioact. Mater. 2021, 6, 312–325. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Fu, J.; Zhou, Y.; Luo, S.; Zhao, Y.; Quan, G.; Pan, X.; Wu, C. Tailored core-shell dual metal-organic frameworks as a versatile nanomotor for effective synergistic antitumor therapy. Acta Pharm. Sin. B 2020, 10, 2198–2211. [Google Scholar] [CrossRef]
- Su, Y.; Ni, W.; Zhang, H.; Jiang, K.; Wen, F. One-pot synthesis of ICG&Cur@ZIF-8 nanocomposites with pH-controlled drug delivery and good photothermal performance. Z. Anorg. Allg. Chem. 2021. [Google Scholar] [CrossRef]
- Gautam, S.; Singhal, J.; Lee, H.K.; Chae, K.H. Drug delivery of paracetamol by metal-organic frameworks (HKUST-1): Improvised synthesis and investigations. Mater. Today Chem. 2022, 23, 100647. [Google Scholar] [CrossRef]
- Yang, Y.; Liu, J.; Liang, C.; Feng, L.; Fu, T.; Dong, Z.; Chao, Y.; Li, Y.; Lu, G.; Chen, M.; et al. Nanoscale metal-organic particles with rapid clearance for magnetic resonance imaging-guided photothermal therapy. ACS Nano 2016, 23, 2774–2781. [Google Scholar] [CrossRef]
- Lu, K.; He, C.; Lin, W. A Chlorin-Based Nanoscale metal–organic framework for photodynamic therapy of colon cancers. J. Am. Chem. Soc. 2015, 137, 7600–7603. [Google Scholar] [CrossRef] [Green Version]
- Rabiee, N.; Bagherzadeh, M.; Jouyandeh, M.; Zarrintaj, P.; Saeb, M.R.; Mozafari, M.; Shokouhimehr, M.; Varma, R.S. Natural Polymers Decorated MOF-MXene nanocarriers for Co-delivery of doxorubicin/pCRISPR. ACS Appl. Bio Mater. 2021, 4, 5106–5121. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; He, G.; Xiong, C.; Wang, C.; Lian, X.; Hu, L.; Li, Z.; Dalgarno, S.J.; Yang, Y.-W.; Tian, J. One-pot fabrication of hollow porphyrinic MOF nanoparticles with ultrahigh drug loading toward controlled delivery and synergistic cancer therapy. ACS Appl. Mater. Interfaces 2021, 13, 3679–3693. [Google Scholar] [CrossRef] [PubMed]
- Alves, R.C.; Schulte, Z.M.; Luiz, M.T.; da Silva, P.B.; Frem, R.C.G.; Rosi, N.L.; Chorilli, M. Breast Cancer targeting of a drug delivery system through postsynthetic modification of curcumin@N3-bio-MOF-100 via Click Chemistry. Inorg. Chem. 2021, 60, 11739–11744. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Shen, M.; Liu, J.; Ren, F. Post-Synthetic Modification nanoscale metal-organic frameworks for targeted drug delivery in cancer cells. Pharm. Res. 2017, 34, 2440–2450. [Google Scholar] [CrossRef] [PubMed]
- Horcajada, P.; Chalati, T.; Serre, C.; Gillet, B.; Sebrie, C.; Baati, T.; Eubank, J.F.; Heurtaux, D.; Clayette, P.; Kreuz, C.; et al. Porous metal-organic-framework nanoscale carriers as a potential platform for drug delivery and imaging. Nat. Mater. 2010, 9, 172–178. [Google Scholar] [CrossRef]
- Gao, X.; Zhai, M.; Guan, W.; Liu, J.; Liu, Z.; Damirin, A. Controllable Synthesis of a Smart Multifunctional Nanoscale Metal–Organic Framework for Magnetic Resonance/Optical Imaging and Targeted Drug Delivery. ACS Appl. Mater. Interfaces 2017, 9, 3455–3462. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Yu, J.; Liu, M.; Liu, A.; Dou, Z.; Yang, Y. A low cytotoxic cationic metal-organic framework carrier for controllable drug release. J. Med. Chem. 2014, 57, 5679–5685. [Google Scholar] [CrossRef]
- Lawson, S.; Newport, K.; Schueddig, K.; Rownaghi, A.A.; Rezaei, F. Optimizing ibuprofen concentration for rapid pharmacokinetics on biocompatible zinc-based MOF-74 and UTSA-74. Mater. Sci. Eng. C 2020, 117, 111336. [Google Scholar] [CrossRef]
- Taylor-Pashow, K.M.L.; Della Rocca, J.; Xie, Z.; Tran, S.; Lin, L. Postsynthetic Modifications of iron-carboxylate nanoscale metal-organic frameworks for imaging and drug delivery. J. Am. Chem. Soc. 2009, 131, 14261–142632. [Google Scholar] [CrossRef] [Green Version]
- Han, L.; Qi, H.; Zhang, D.; Ye, G.; Zhou, W.; Hou, C.; Xud, W.; Sun, Y. A facile and green synthesis of MIL-100(Fe) with high-yield and its catalytic performance. New J. Chem. 2017, 41, 13504–13509. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, L.; Liu, L.; Lin, L.; Liu, F.; Xie, Z.; Tian, H.; Chen, X. Engineering metal–organic frameworks for photoacoustic imaging-guided chemo-/photothermal combinational tumor therapy. ACS Appl. Mater. Interfaces 2018, 10, 41035–41045. [Google Scholar] [CrossRef] [PubMed]
- Xue, T.; Xu, C.; Wang, Y.; Wang, Y.; Tian, H.; Zhang, Y. Doxorubicin-loaded nanoscale metal–organic framework for tumor-targeting combined chemotherapy and chemodynamic therapy. Biomater. Sci. 2019, 7, 4615–4623. [Google Scholar] [CrossRef] [PubMed]
- Devautour-Vinot, S.; Martineau, C.; Diaby, S.; Ben-Yahia, M.; Miller, S.; Serre, C.; Horcajada, P.; Cunha, D.; Taulelle, F.; Maurin, G. Caffeine confinement into a series of functionalized porous zirconium MOFs: A joint experimental/modeling exploration. J. Phys. Chem. C 2013, 117, 11694–11704. [Google Scholar] [CrossRef]
- Chen, X.; Zhuang, Y.; Rampal, N.; Hewitt, R.; Divitini, G.; O’Keefe, C.A.; Liu, X.; Whitaker, D.J.; Wills, J.W.; Jugdaohsingh, R.; et al. Formulation of metal–organic framework-based drug carriers by controlled coordination of methoxy PEG phosphate: Boosting colloidal stability and redispersibility. J. Am. Chem. Soc. 2021, 143, 13557–13572. [Google Scholar] [CrossRef]
- Cunha, D.; Mouna, B.Y.; Hall, S.; Miller, R.S.; Chevreau, H.; Elkaïm, E.; Maurin, G.; Horcajada, P.; Serre, C. Rationale of drug encapsulation and release from biocompatible porous metal–organic frameworks. Chem. Mater. 2013, 25, 2767–2776. [Google Scholar] [CrossRef]
- Ye, X.; Liu, D. Metal–Organic Framework UiO-68 and Its Derivatives with sufficiently good properties and performance show promising prospects in potential industrial applications. Cryst. Growth Des. 2021, 21, 4780–4804. [Google Scholar] [CrossRef]
- Li, S.; Wang, K.; Shi, Y.; Cui, Y.; Chen, B.; He, B.; Dai, W.; Zhang, H.; Wang, X.; Zhong, C.; et al. Novel biological functions of ZIF-NP as a delivery vehicle: High pulmonary accumulation, favorable biocompatibility, and improved therapeutic outcome. Adv. Funct. Mater. 2016, 26, 2715. [Google Scholar] [CrossRef]
- Tan, L.-L.; Song, N.; Zhang, S.X.-A.; Li, H.; Wang, B.; Yang, Y.-W. Ca2+, pH and thermo triple-responsive mechanized Zr-based MOFs for on-command drug release in bone diseases. J. Mater. Chem. B 2016, 4, 135. [Google Scholar] [CrossRef]
- He, S.; Wu, L.; Li, X.; Sun, H.; Xiong, T.; Liu, J.; Chengxi Huang, C.; Xu, H.; Sun, H.; Chen, W.; et al. Metal-organic frameworks for advanced drug delivery. Acta Pharm. Sin. B 2021, 11, 2362–2395. [Google Scholar] [CrossRef]
- Cai, W.; Wang, J.; Chu, C.; Chen, W.; Wu, C.; Liu, G. Metal–organic framework-based stimuli-responsive systems for drug delivery. Adv. Sci. 2018, 6, 1801526. [Google Scholar] [CrossRef] [Green Version]
- Luo, Z.; Jiang, L.; Yang, S.; Li, Z.; Soh, W.M.W.; Zheng, L.; Loh, X.J.; Wu, Y.L. Light-induced redox-responsive smart drug delivery system by using selenium-containing polymer@MOF Shell/Core nanocomposite. Adv. Healthc. Mater. 2019, 8, 1900406. [Google Scholar] [CrossRef] [PubMed]
- Diring, S.; Carne-Sanchez, A.; Zhang, J.; Ikemura, S.; Kim, C.; Inaba, H.; Kitagawa, S.; Furukawa, S. Light responsive metal–organic frameworks as controllable CO-releasing cell culture substrates. Chem. Sci. 2017, 8, 2381–2386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, Z.; Zhao, P.; Zhang, J.; Yang, T.; Zhou, G.; Zhang, D.; Wang, T.; He, Q. Intelligent metal carbonyl metal–organic framework nanocomplex for fluorescent traceable H2O2-triggered CO delivery. Chem. Eur. J. 2018, 24, 11667–11674. [Google Scholar] [CrossRef] [PubMed]
- Pobłocki, K.; Drzeżdżon, J.; Kostrzewa, T.; Jacewicz, D. Coordination Complexes as a New Generation Photosensitizer for Photodynamic Anticancer Therapy. Int. J. Mol. Sci. 2021, 22, 8052. [Google Scholar] [CrossRef]
- Cabrera-García, A.; Checa-Chavarria, E.; Rivero-Buceta, E.; Moreno, V.; Fernández, E.; Botella, P. Amino modified metal-organic frameworks as pH-responsive nanoplatforms for safe delivery of camptothecin. J. Colloid Interface Sci. 2019, 541, 163–174. [Google Scholar] [CrossRef]
- Tan, L.L.; Li, H.; Qiu, Y.C.; Chen, D.X.; Wang, X.; Pan, R.Y.; Wang, Y.; Zhang, S.X.; Wang, B.; Yang, Y.W. Stimuli-responsive metal–organic frameworks gated by pillar[5]arene supramolecular switches. Chem. Sci. 2015, 6, 1640–1644. [Google Scholar] [CrossRef] [Green Version]
- Karimzadeh, S.; Javanbakht, S.; Baradaran, B.; Shahbazi, M.A.; Hashemzaei, M.; Mokhtarzadeh, A.; Santos, H.A. Synthesis and therapeutic potential of stimuli-responsive metal-organic frameworks. Chem. Eng. J. 2021, 408, 127233. [Google Scholar] [CrossRef]
- Zhu, Y.D.; Chen, S.P.; Zhao, H.; Yang, Y.; Chen, X.Q.; Sun, J.; Fan, H.S.; Zhang, X.D. PPy@MIL-100 Nanoparticles as a pH- and Near-IR-irradiation-responsive drug carrier for simultaneous photothermal therapy and chemotherapy of cancer cells. ACS Appl. Mater. Interfaces 2016, 8, 34209–34217. [Google Scholar] [CrossRef]
- Zou, Z.; Li, S.Q.; He, D.G.; He, X.X.; Wang, K.M.; Li, L.L.; Yang, X.; Li, H.F. A versatile stimulus-responsive metal–organic framework for size/morphology tunable hollow mesoporous silica and pH-triggered drug delivery. J. Mater. Chem. B 2017, 5, 2126–2132. [Google Scholar] [CrossRef]
- Tian, Z.F.; Yao, X.X.; Zhu, Y.F. Simple synthesis of multifunctional zeolitic imidazolate frameworks-8/graphene oxide nanocrystals with controlled drug release and photothermal effect. Microporous Mesoporous Mater. 2017, 237, 160–167. [Google Scholar] [CrossRef]
- Tang, L.; Shi, J.F.; Wang, X.L.; Zhang, S.H.; Wu, H.; Sun, H.F.; Jiang, Z.Y. Coordination polymer nanocapsules prepared using metal-organic framework templates for pH-responsive drug delivery. Nanotechnology 2017, 28, 275601. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Gu, J.; Wang, Y.; Li, B.; Li, Y.; Zhao, W.; Shi, J. Inherent anchorages in UiO-66 nanoparticles for efficient capture of alendronate and its mediated release. Chem. Commun. 2014, 50, 8779–8782. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Hu, Q.; Zhang, Q.; Jiang, K.; Lin, W.; Yang, Y.; Cui, Y.; Qian, G. A large capacity cationic metal–organic framework nanocarrier for physiological pH responsive drug delivery. Mol. Pharm. 2016, 13, 2782–2786. [Google Scholar] [CrossRef]
- Kundu, T.; Mitra, S.; Patra, P.; Goswami, A.; Diaz, D.; Banerjee, R. Mechanical Downsizing of a Gadolinium(III)-based Metal–Organic Framework for Anticancer Drug Delivery. Chem.-Eur. J. 2014, 20, 10514–10518. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.J.; Wang, H.R.; Yi, X.; Chao, Y.; Geng, Y.H.; Xu, L.G.; Yang, K.; Liu, Z. pH-sensitive dissociable nanoscale coordination polymers with drug loading for synergistically enhanced chemoradiotherapy. Adv. Funct. Mater. 2017, 27, 1703832. [Google Scholar] [CrossRef]
- Duan, F.; Feng, X.C.; Yang, X.J.; Sun, W.T.; Jin, Y.; Liu, H.F.; Ge, K.; Li, Z.H.; Zhang, J.C. A simple and powerful co-delivery system based on pH-responsive metal-organic frameworks for enhanced cancer immunotherapy. Biomaterials 2017, 122, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Hamisu, A.M.; Ariffin, A.; Wibowo, A.C. Cation Exchange in Metal-Organic Frameworks (MOFs): The Hard-Soft Acid-Base (HSAB) Principle Appraisal. Inorganica Chim. Acta 2020, 511, 119801. [Google Scholar] [CrossRef]
- Vardali, S.C.; Manousi, N.; Barczak, M.; Giannakoudakis, D.A. Novel Approaches Utilizing Metal-Organic Framework Composites for the Extraction of Organic Compounds and Metal Traces from Fish and Seafood. Molecules 2020, 25, 513. [Google Scholar] [CrossRef]
- Wang, C.; Liu, X.; Demir, N.K.; Chen, J.P.; Li, K. Applications of water stable metal–organic frameworks. Chem. Soc. Rev. 2016, 45, 5107–5134. [Google Scholar] [CrossRef]
- Park, K.S.; Ni, Z.; Côté, A.P.; Choi, J.Y.; Huang, R.; Uribe-Romo, F.J.; Chae, H.K.; O’Keeffe, M.; Yaghi, O.M. Exceptional chemical and thermal stability of zeolitic imidazolate frameworks. Proc. Natl. Acad. Sci. USA 2006, 103, 10186–10191. [Google Scholar] [CrossRef] [Green Version]
- Fei, H.; Cahill, J.F.; Prather, K.A.; Cohen, S.M. Tandem postsynthetic metal ion and ligand exchange in zeolitic imidazolate frameworks. Inorg. Chem. 2016, 52, 4011–4016. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.; Dou, W.; Caro, J.R. Steam-Stable Zeolitic Imidazolate Framework ZIF-90 Membrane with Hydrogen Selectivity through Covalent Functionalization. J. Am. Chem. Soc. 2010, 132, 15562–15564. [Google Scholar] [CrossRef] [PubMed]

| MOFs | Components | Pore Size or Volume/Particle Size | Therapeutic Agent | Drug Loading Percentage | Outcome | Ref. | |
|---|---|---|---|---|---|---|---|
| Organic | Inorganic | ||||||
| MIL-53(Fe) | Terephtalic acid | FeCl3·6H2O | 8.6 Å/ 350 nm | Ibuprofen Caffeine | 22 23.1 | antitumoral and retroviral drugs against cancer and AIDS | [95] |
| MIL-53-NH2 (Fe) | 2-Amino-terephtalic acid | FeCl3·6H2O | 120 nm | 5-Fu | 28 | magnetic resonance, optical imaging, targeted drug delivery | [96] |
| MOF-74-Fe | 1.4-Dihydroxy terephtalic acid | FeCl2·4H2O | -/200–800 nm × some μm | Ibuprofen | 15.9 | low cytotoxicity, efficient drug loading capacity, controllable drug release | [97] |
| MOF-74-Zn | 2.5-Dihydroxyterephthalic acid | Zn(NO3)2 6H2O | 12.7 A/20 nm | Ibuprofen | 50 | fast kinetics (k = 0.27 h−1/2), high drug conc. in first 10 h. | [98] |
| MIL-101 (Cr) | 1,4-benzenedicarboxylates, | trimeric chromium(III) octahedral clusters | 34 Å | Ibuprofen | - | can adsorb 138 wt% ibuprofen, release the total amount slowly in 6 days | [99] |
| MIL-100 (Fe) | Trimesic acid | Fe (NO3)3·9H2O or FeCl3·6H2O | 29 A/200 nm | Ibuprofen urcumin | 33 | antitumoural and retroviral drugs, photoacoustic imaging-guided chemo-photothermal combinational tumor therapy | [95,100,101] |
| MIL-89 (Fe) | Muconic acid | FeCl3·6H2O | 11A/50–100 nm | Cidofovir | 14 | antitumoral and retroviral drugs | [95] |
| MIL-101-NH2 (Fe) | Aminoterephtalic acid | FeCl3·6H2O | 34 A/120 nm | Cidofovir | 41.9 | [95] | |
| MIL-100 (Fe) | Trimesic acid | Fe (NO3)3·9H2O or FeCl3·6H2O | 1.2 cm3/g /102.8 nm | DOX Caffeine | 28 24.2 | released DOX in a pH-dependent manner, breast cancer treatment | [102] |
| UiO-66(Zr) | 1,4-Benzenedicarboxylic acid | ZrCl4 | 5–7 A | Caffeine DOX | 22.4 15.1 | caffeine molecules are preferentially located in the smaller cages, DOX-containing PEGylated nanoMOFs exhibit notable redispersibility | [103,104] |
| MIL-127 Fe | 3,3′,5,5′-Azobenzene tetracarboxylate | trimers of iron(III) octahedra | 4 A | Caffeine | 15.9 | carriers for topical administration of caffeine | [105] |
| MIL-100 (Fe) | Trimesic acid | {Fe3O} trimer | 200 nm | DOX | 9.1 | full release of drug in 5 days | [95] |
| Mi-UiO-68 | maleimide-attached H2L ligand | ZrCl4 | 25.6 A | DOX FA (acid folic) | 4.84 | multifunctional cancer treatment system | [106] |
| MIL-88@ZIF-8 | BDC-NH2, 2-Me-IM | FeCl3·6H2O Zn(NO3)2·6H2O | -/1.3 nm | ICG DOX | 3.58% 21.69% | MIL-88-ICG@ZIF-8-DOX core-shell dual MOF for synergistic cancer, photothermal and photodynamic therapy | [86] |
| ZIF-8 | Me-IM | Zn(NO3)2·6H2O | 200 nm | 5-Fu | 21.2 | biological purposes: bio–nano interaction, pulmonary accumulation, antitumor therapy | [107] |
| UiO-66-NH2 | NH2-BDC | {Zr6O8} cluster | 100 nm | 5-Fu | 3.1 | multistimuli responsive in bone diseases: increasing Ca2+ concentration, decreasing pH, thermal therapy | [108] |
| MIL-88A (Fe) | Fumaric acid | FeCl3·6H2O | 6 A/150 nm | Cidofovir | 2.6 | [109] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maranescu, B.; Visa, A. Applications of Metal-Organic Frameworks as Drug Delivery Systems. Int. J. Mol. Sci. 2022, 23, 4458. https://doi.org/10.3390/ijms23084458
Maranescu B, Visa A. Applications of Metal-Organic Frameworks as Drug Delivery Systems. International Journal of Molecular Sciences. 2022; 23(8):4458. https://doi.org/10.3390/ijms23084458
Chicago/Turabian StyleMaranescu, Bianca, and Aurelia Visa. 2022. "Applications of Metal-Organic Frameworks as Drug Delivery Systems" International Journal of Molecular Sciences 23, no. 8: 4458. https://doi.org/10.3390/ijms23084458
APA StyleMaranescu, B., & Visa, A. (2022). Applications of Metal-Organic Frameworks as Drug Delivery Systems. International Journal of Molecular Sciences, 23(8), 4458. https://doi.org/10.3390/ijms23084458







