PD-L1 Expression in Non-Small Cell Lung Cancer Specimens: Association with Clinicopathological Factors and Molecular Alterations
Abstract
:1. Introduction
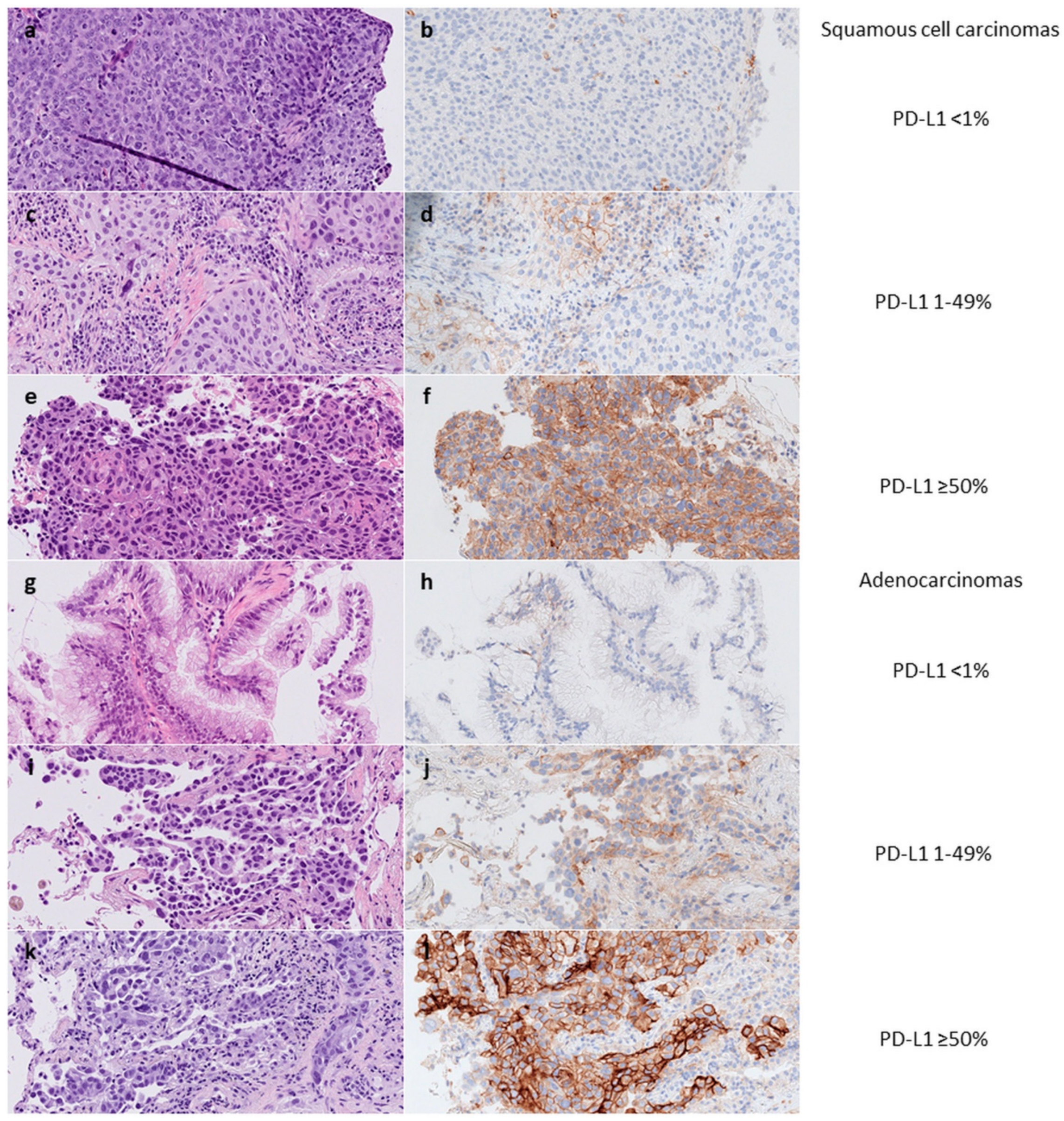
2. Results
2.1. Characteristics of the Cases
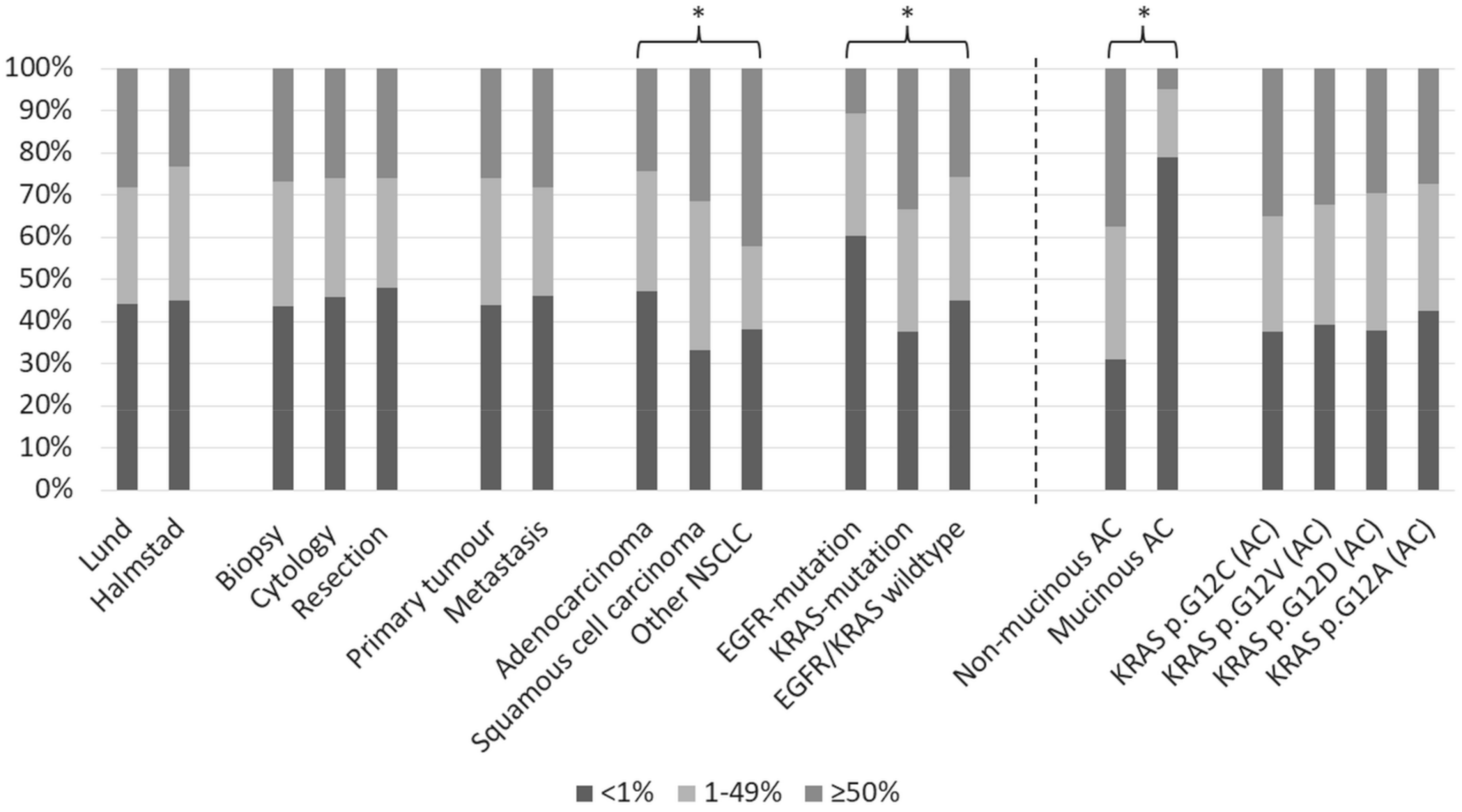
2.2. Correlation between PD-L1 Expression and Clinicopathological and Molecular Features
2.3. PD-L1 Expression in EGFR-Mutated Lung Cancers
2.4. PD-L1 Expression in KRAS-Mutated Adenocarcinomas
| Parameter | All Cases | PD-L1 < 1% | PD-L1 1–49% | PD-L1 ≥ 50% |
|---|---|---|---|---|
| Growth pattern | ||||
| Non-mucinous | 338 | 105 (31%) | 106 (31%) | 127 (38%) |
| Mucinous | 62 | 49 (79%) | 10 (16%) | 3 (5%) |
| Undetermined | 3 | 2 (67%) | 0 (0%) | 1 (33%) |
| Mutation | ||||
| p.G12C | 154 | 58 (38%) | 42 (27%) | 54 (35%) |
| p.G12V | 74 | 29 (39%) | 21 (28%) | 24 (32%) |
| p.G12D | 61 | 23 (38%) | 20 (33%) | 18 (30%) |
| p.G12A | 33 | 14 (42%) | 10 (30%) | 9 (27%) |
| p.G13C | 17 | 7 (41%) | 4 (24%) | 6 (35%) |
| p.Q61H | 16 | 7 (44%) | 4 (25%) | 5 (31%) |
| p.G13D | 12 | 4 (33%) | 4 (33%) | 4 (33%) |
| p.G12S | 10 | 5 (50%) | 3 (30%) | 2 (20%) |
| p.G12R | 8 | 3 (38%) | 2 (25%) | 3 (38%) |
| p.Q61L | 5 | 1 (20%) | 3 (60%) | 1 (20%) |
| p.G12F | 4 | 0 (0%) | 2 (50%) | 2 (50%) |
| p.G13V | 3 | 2 (67%) | 1 (33%) | 0 (0%) |
| p.A146V | 2 | 2 (100%) | 0 (0%) | 0 (0%) |
| p.G21C | 1 | 0 (0%) | 0 (0%) | 1 (100%) |
| p.Q61R | 1 | 1 (100%) | 0 (0%) | 0 (0%) |
| p.L19F | 1 | 0 (0%) | 0 (0%) | 1 (100%) |
| p.Q61K | 1 | 0 (0%) | 0 (0%) | 1 (100%) |
3. Discussion
4. Materials and Methods
4.1. The Lund Cohort
4.2. PD-L1 Testing in Lund
4.3. Molecular Testing in Lund
4.4. The Halmstad Cohort
4.5. PD-L1 Testing in Halmstad
4.6. Molecular Testing in Halmstad
4.7. Data Collection and Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raju, S.; Joseph, R.; Sehgal, S. Review of checkpoint immunotherapy for the management of non-small cell lung cancer. Immunotargets Ther. 2018, 7, 63–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Five-Year Outcomes With Pembrolizumab Versus Chemotherapy for Metastatic Non-Small-Cell Lung Cancer with PD-L1 Tumor Proportion Score ≥ 50. J. Clin. Oncol. 2021, 39, 2339–2349. [Google Scholar] [CrossRef]
- Herbst, R.S.; Garon, E.B.; Kim, D.W.; Cho, B.C.; Gervais, R.; Perez-Gracia, J.L.; Han, J.Y.; Majem, M.; Forster, M.D.; Monnet, I.; et al. Five Year Survival Update From KEYNOTE-010: Pembrolizumab Versus Docetaxel for Previously Treated, Programmed Death-Ligand 1-Positive Advanced NSCLC. J. Thorac. Oncol. 2021, 16, 1718–1732. [Google Scholar] [CrossRef]
- Waterhouse, D.; Lam, J.; Betts, K.A.; Yin, L.; Gao, S.; Yuan, Y.; Hartman, J.; Rao, S.; Lubinga, S.; Stenehjem, D. Real-world outcomes of immunotherapy–based regimens in first-line advanced non-small cell lung cancer. Lung Cancer 2021, 156, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Lantuejoul, S.; Sound-Tsao, M.; Cooper, W.A.; Girard, N.; Hirsch, F.R.; Roden, A.C.; Lopez-Rios, F.; Jain, D.; Chou, T.Y.; Motoi, N.; et al. PD-L1 Testing for Lung Cancer in 2019: Perspective From the IASLC Pathology Committee. J. Thorac. Oncol. 2020, 15, 499–519. [Google Scholar] [CrossRef] [PubMed]
- Torous, V.F.; Rangachari, D.; Gallant, B.P.; Shea, M.; Costa, D.B.; VanderLaan, P.A. PD-L1 testing using the clone 22C3 pharmDx kit for selection of patients with non–small cell lung cancer to receive immune checkpoint inhibitor therapy: Are cytology cell blocks a viable option? J. Am. Soc. Cytopathol. 2018, 7, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.S.; Lindquist, K.E.; Seidal, T.; Mager, U.; Mohlin, R.; Tran, L.; Hejny, K.; Holmgren, B.; Violidaki, D.; Dobra, K.; et al. PD-L1 Testing in Cytological Non-Small Cell Lung Cancer Specimens: A Comparison with Biopsies and Review of the Literature. Acta Cytol. 2021, 65, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Gosney, J.R.; Boothman, A.M.; Ratcliffe, M.; Kerr, K.M. Cytology for PD-L1 testing: A systematic review. Lung Cancer 2020, 141, 101–106. [Google Scholar] [CrossRef] [Green Version]
- Mansour, M.S.; Hejny, K.; Johansson, F.; Mufti, J.; Vidis, A.; Mager, U.; Dejmek, A.; Seidal, T.; Brunnström, H. Factors Influencing Concordance of PD-L1 Expression between Biopsies and Cytological Specimens in Non-Small Cell Lung Cancer. Diagnostics 2021, 11, 1927. [Google Scholar] [CrossRef]
- Brody, R.; Zhang, Y.; Ballas, M.; Siddiqui, M.K.; Gupta, P.; Barker, C.; Midha, A.; Walker, J. PD-L1 expression in advanced NSCLC: Insights into risk stratification and treatment selection from a systematic literature review. Lung Cancer 2017, 112, 200–215. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Xu, Y.; Wan, B.; Song, Y.; Zhan, P.; Hu, Y.; Zhang, Q.; Zhang, F.; Liu, H.; Li, T.; et al. The clinicopathological and prognostic significance of PD-L1 expression assessed by immunohistochemistry in lung cancer: A meta-analysis of 50 studies with 11,383 patients. Transl. Lung Cancer Res. 2019, 8, 429–449. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.; O’Sullivan, B.; Hughes, F.; Mullis, T.; Smith, M.; Trim, N.; Taniere, P. The Clinicopathological and Molecular Associations of PD-L1 Expression in Non-small Cell Lung Cancer: Analysis of a Series of 10,005 Cases Tested with the 22C3 Assay. Pathol. Oncol. Res. 2018, 26, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Noordhof, A.; Damhuis, R.; Hendriks, L.; de Langen, A.; Timens, W.; Venmans, B.; van Geffen, W. Prognostic impact of KRAS mutation status for patients with stage IV adenocarcinoma of the lung treated with first-line pembrolizumab monotherapy. Lung Cancer 2021, 155, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Velcheti, V.; Hu, X.; Li, Y.; El-Osta, H.; Pietanza, M.C.; Burke, T. Real-World Time on Treatment with First-Line Pembrolizumab Monotherapy for Advanced NSCLC with PD-L1 Expression ≥ 50%: 3-Year Follow-Up Data. Cancers 2022, 14, 1041. [Google Scholar] [CrossRef]
- Kadota, K.; Yeh, Y.-C.; D’Angelo, S.P.; Moreira, A.L.; Kuk, D.; Sima, C.S.; Riely, G.J.; Arcila, M.E.; Kris, M.; Rusch, V.; et al. Associations Between Mutations and Histologic Patterns of Mucin in Lung Adenocarcinoma. Am. J. Surg. Pathol. 2014, 38, 1118–1127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velcheti, V.; Patwardhan, P.D.; Liu, F.X.; Chen, X.; Cao, X.; Burke, T. Real-world PD-L1 testing and distribution of PD-L1 tumor expression by immunohistochemistry assay type among patients with metastatic non-small cell lung cancer in the United States. PLoS ONE 2018, 13, e0206370. [Google Scholar] [CrossRef] [PubMed]
- Dietel, M.; Savelov, N.; Salanova, R.; Micke, P.; Bigras, G.; Hida, T.; Antunez, J.; Skov, B.G.; Hutarew, G.; Sua, L.F.; et al. Real-world prevalence of programmed death ligand 1 expression in locally advanced or metastatic non-small-cell lung cancer: The global, multicenter EXPRESS study. Lung Cancer 2019, 134, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.M.; Albaqer, T.; Santiago, R.C.; Weiss, J.; Tanguay, J.; Cabanero, M.; Leung, Y.; Pal, P.; Khan, Z.; Lau, S.C.; et al. Prevalence and Heterogeneity of PD-L1 Expression by 22C3 Assay in Routine Population-Based and Reflexive Clinical Testing in Lung Cancer. J. Thorac. Oncol. 2021, 16, 1490–1500. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Q.; Huang, Y.; Zeng, X.; Chen, X.; Shao, S.; Jin, Y.; Xue, Q.; Wang, Y.; Guo, Y.; Gu, B.; et al. Clinicopathological and molecular characteristics associated with PD-L1 expression in non-small cell lung cancer: A large-scale, multi-center, real-world study in China. J. Cancer Res. Clin. Oncol. 2020, 147, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Agulnik, J.; Kasymjanova, G.; Wang, A.; Jiménez, P.; Cohen, V.; Small, D.; Pepe, C.; Sakr, L.; Fiset, P.; et al. Cytology cell blocks are suitable for immunohistochemical testing for PD-L1 in lung cancer. Ann. Oncol. 2018, 29, 1417–1422. [Google Scholar] [CrossRef]
- Kerr, K.M.; Thunnissen, E.; Dafni, U.; Finn, S.P.; Bubendorf, L.; Soltermann, A.; Verbeken, E.; Biernat, W.; Warth, A.; Marchetti, A.; et al. A retrospective cohort study of PD-L1 prevalence, molecular associations and clinical outcomes in patients with NSCLC: Results from the European Thoracic Oncology Platform (ETOP) Lungscape Project. Lung Cancer 2019, 131, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.S.P.; Severson, E.; Haberberger, J.; Duncan, D.L.; Hemmerich, A.; Edgerly, C.; Ferguson, N.L.; Frampton, G.; Owens, C.; Williams, E.; et al. Landscape of Biomarkers in Non-small Cell Lung Cancer Using Comprehensive Genomic Profiling and PD-L1 Immunohistochemistry. Pathol. Oncol. Res. 2021, 27, 592997. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Maltese, M.; Tomasello, G.; Conti, B.; Borgonovo, K.; Cabiddu, M.; Ghilardi, M.; Ghidini, M.; Passalacqua, R.; Barni, S.; et al. Clinical and Molecular Predictors of PD-L1 Expression in Non–Small-Cell Lung Cancer: Systematic Review and Meta-analysis. Clin. Lung Cancer 2018, 19, 315–322. [Google Scholar] [CrossRef]
- Schoenfeld, A.J.; Rizvi, H.; Bandlamudi, C.; Sauter, J.L.; Travis, W.D.; Rekhtman, N.; Plodkowski, A.J.; Perez-Johnston, R.; Sawan, P.; Beras, A.; et al. Clinical and molecular correlates of PD-L1 expression in patients with lung adenocarcinomas. Ann. Oncol. 2020, 31, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Gainor, J.F.; Shaw, A.T.; Sequist, L.V.; Fu, X.; Azzoli, C.G.; Piotrowska, Z.; Huynh, T.G.; Zhao, L.; Fulton, L.; Schultz, K.R.; et al. EGFR Mutations and ALK Rearrangements Are Associated with Low Response Rates to PD-1 Pathway Blockade in Non–Small Cell Lung Cancer: A Retrospective Analysis. Clin. Cancer Res. 2016, 22, 4585–4593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Offin, M.; Rizvi, H.; Tenet, M.; Ni, A.; Sanchez-Vega, F.; Li, B.T.; Drilon, A.; Kris, M.G.; Rudin, C.M.; Schultz, N.; et al. Tumor Mutation Burden and Efficacy of EGFR-Tyrosine Kinase Inhibitors in Patients with EGFR-Mutant Lung Cancers. Clin. Cancer Res. 2018, 25, 1063–1069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, R.; Liu, C.; Zheng, S.; Wang, X.; Feng, X.; Li, H.; Sun, N.; He, J. Molecular heterogeneity of anti-PD-1/PD-L1 immunotherapy efficacy is correlated with tumor immune microenvironment in East Asian patients with non-small cell lung cancer. Cancer Biol. Med. 2020, 17, 768–781. [Google Scholar] [CrossRef] [PubMed]
- To, K.K.W.; Fong, W.; Cho, W.C.S. Immunotherapy in Treating EGFR-Mutant Lung Cancer: Current Challenges and New Strategies. Front. Oncol. 2021, 11, 635007. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.; Wang, R.; Zhang, X.; Ma, Y.; Zhong, L.; Li, K.; Nishiyama, A.; Arai, S.; Yano, S.; Wang, W. EGFR-TKI resistance promotes immune escape in lung cancer via increased PD-L1 expression. Mol. Cancer 2019, 18, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.C.; Manandhar, A.; Carrasco, M.A.; Gurbani, D.; Gondi, S.; Westover, K.D. Biochemical and Structural Analysis of Common Cancer-Associated KRAS Mutations. Mol. Cancer Res. 2015, 13, 1325–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, Y.J.; Hyun, D.-G.; Choi, C.-M.; Lee, D.H.; Kim, S.-W.; Yoon, S.; Kim, W.S.; Ji, W.; Lee, J.C. Optimizing palliative chemotherapy for advanced invasive mucinous adenocarcinoma of the lung. BMC Cancer 2021, 21, 731. [Google Scholar] [CrossRef] [PubMed]
- Tuminello, S.; Sikavi, D.; Veluswamy, R.; Gamarra, C.; Lieberman-Cribbin, W.; Flores, R.; Taioli, E. PD-L1 as a prognostic biomarker in surgically resectable non- small cell lung cancer: A meta-analysis. Transl. Lung Cancer Res. 2020, 9, 1343–1360. [Google Scholar] [CrossRef] [PubMed]
- Sholl, L.M. Biomarkers of response to checkpoint inhibitors beyond PD-L1 in lung cancer. Mod. Pathol. 2021, 35, 66–74. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Lund Cohort | PD-L1 <1% | PD-L1 1–49% | PD-L1 ≥50% | Halmstad Cohort | PD-L1 <1% | PD-L1 1–49% | PD-L1 ≥50% |
|---|---|---|---|---|---|---|---|---|
| All cases | 1094 | 492 (45%) | 303 (28%) | 299 (27%) | 527 | 239 (45%) | 174 (33%) | 114 (22%) |
| Sample type * | ||||||||
| Biopsy | 845 | 364 (43%) | 238 (28%) | 243 (29%) | 469 | 212 (45%) | 160 (35%) | 97 (21%) |
| Cytology | 176 | 85 (48%) | 50 (28%) | 41 (23%) | 180 | 86 (48%) | 46 (26%) | 48 (27%) |
| Resection | 110 | 55 (50%) | 29 (26%) | 26 (24%) | 2 ** | 0 (0%) | 1 (50%) | 1 (50%) |
| Locality | ||||||||
| Primary tumor | 785 | 340 (43%) | 226 (29%) | 219 (28%) | 469 | 211 (45%) | 161 (34%) | 97 (21%) |
| Metastasis | 305 | 151 (50%) | 75 (25%) | 79 (26%) | 58 | 28 (48%) | 13 (22%) | 17 (29%) |
| Unclear/mixed | 4 | 1 (25%) | 2 (50%) | 1 (25%) | 0 | |||
| Diagnosis | ||||||||
| Adenocarcinoma | 776 | 380 (49%) | 208 (27%) | 188 (24%) | 384 | 173 (45%) | 121 (32%) | 90 (23%) |
| Squamous cell carcinoma | 237 | 80 (34%) | 79 (33%) | 78 (33%) | 137 | 63 (46%) | 51 (37%) | 23 (18%) |
| Sarcomatoid carcinoma/features | 15 | 4 (27%) | 2 (13%) | 9 (60%) | 0 | |||
| Adenosquamous carcinoma | 3 | 2 (67%) | 1 (33%) | 0 (0%) | 0 | |||
| NSCLC not otherwise specified | 63 | 26 (41%) | 13 (21%) | 24 (38%) | 6 | 3 (50%) | 2 (33%) | 1 (17%) |
| Mutations *** | ||||||||
| EGFR | 109 (of 1075) | 68 (62%) | 28 (26%) | 13 (12%) | 54 (of 387) | 32 (59%) | 18 (33%) | 4 (7%) |
| KRAS | 304 (of 901) | 120 (39%) | 79 (26%) | 105 (34%) | 139 (of 354) | 47 (34%) | 46 (33%) | 46 (33%) |
| NRAS | 7 (of 901) | 3 (43%) | 3 (43%) | 1 (14%) | 4 (of 289) | 0 (0%) | 0 (0%) | 4 (100%) |
| BRAF (V600) | 11 (of 901) | 3 (27%) | 2 (18%) | 6 (55%) | 6 (of 289) | 4 (67%) | 1 (17%) | 1 (17%) |
| ERBB2 | 16 (of 901) | 8 (50%) | 4 (25%) | 4 (25%) | 4 (of 289) | 3 (75%) | 1 (25%) | 0 (0%) |
| PIK3CA | 65 (of 901) | 19 (29%) | 20 (31%) | 26 (40%) | 8 (of 289) | 3 (38%) | 3 (38%) | 2 (25%) |
| MET exon 14 | 13 | 4 (31%) | 3 (23%) | 6 (46%) | not analyzed | |||
| TP53 | not analyzed | 100 (of 289) | 45 (45%) | 29 (29%) | 26 (26%) | |||
| Fusions *** | ||||||||
| ALK | 20 (of 981) | 6 (30%) | 7 (35%) | 7 (35%) | 9 (of 369) | 3 (33%) | 4 (44%) | 2 (22%) |
| ROS1 | 1 (of 976) | 1 (100%) | 0 (0%) | 0 (0%) | 4 (of 239) | 1 (25%) | 1 (25%) | 2 (50%) |
| RET | 4 | 1 (25%) | 3 (75%) | 0 (0%) | not analyzed | |||
| NTRK | 1 | 0 (0%) | 1 (100%) | 0 (0%) | not analyzed |
| Characteristics | PD-L1 <1% | PD-L1 1–49% | PD-L1 ≥50% | Student’s t-Test | Chi2 | Multiple Regression (Coefficient) |
|---|---|---|---|---|---|---|
| Cohort | p = 0.010 | p = 0.12 | p = 0.81 (−0.012) | |||
| Lund | 419 (44%) | 265 (28%) | 267 (28%) | |||
| Halmstad | 193 (45%) | 137 (32%) | 100 (23%) | |||
| Sample type | p = 0.75 * | p = 0.88 | p = 0.28 (−0.041) | |||
| Biopsy | 446 (44%) | 304 (30%) | 274 (27%) | p = 0.61 vs. cytology | ||
| Cytology | 116 (46%) | 71 (28%) | 66 (26%) | p = 0.81 vs. resection | ||
| Resection | 50 (48%) | 27 (26%) | 27 (26%) | p = 0.53 vs. biopsy | ||
| Locality | p = 0.98 | p = 0.30 | p = 0.37 (0.049) | |||
| Primary tumor | 452 (44%) | 312 (30%) | 269 (26%) | |||
| Metastasis | 160 (46%) | 90 (26%) | 98 (28%) | |||
| Diagnosis | p < 0.001 * | p < 0.0001 | p < 0.0001 (0.17) | |||
| Adenocarcinoma | 505 (47%) | 304 (28%) | 261 (24%) | p = 0.0003 vs. squamous | ||
| Squamous cell carcinoma | 78 (33%) | 83 (35%) | 74 (31%) | p = 0.61 vs. “other” | ||
| Other NSCLC | 29 (38%) | 15 (20%) | 32 (42%) | p = 0.0062 vs. adeno | ||
| Molecular profile | p < 0.001 * | p < 0.0001 | p < 0.0001 (0.22) | |||
| EGFR-mutation | 106 (60%) | 51 (29%) | 19 (11%) | p < 0.0001 vs. KRAS | ||
| KRAS-mutation | 179 (38%) | 138 (29%) | 160 (34%) | p = 0.0020 vs. wild-type | ||
| EGFR/KRAS wild-type | 327 (45%) | 213 (29%) | 188 (26%) | p < 0.0001 vs. EGFR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansour, M.S.I.; Malmros, K.; Mager, U.; Ericson Lindquist, K.; Hejny, K.; Holmgren, B.; Seidal, T.; Dejmek, A.; Dobra, K.; Planck, M.; et al. PD-L1 Expression in Non-Small Cell Lung Cancer Specimens: Association with Clinicopathological Factors and Molecular Alterations. Int. J. Mol. Sci. 2022, 23, 4517. https://doi.org/10.3390/ijms23094517
Mansour MSI, Malmros K, Mager U, Ericson Lindquist K, Hejny K, Holmgren B, Seidal T, Dejmek A, Dobra K, Planck M, et al. PD-L1 Expression in Non-Small Cell Lung Cancer Specimens: Association with Clinicopathological Factors and Molecular Alterations. International Journal of Molecular Sciences. 2022; 23(9):4517. https://doi.org/10.3390/ijms23094517
Chicago/Turabian StyleMansour, Mohammed S. I., Karina Malmros, Ulrich Mager, Kajsa Ericson Lindquist, Kim Hejny, Benjamin Holmgren, Tomas Seidal, Annika Dejmek, Katalin Dobra, Maria Planck, and et al. 2022. "PD-L1 Expression in Non-Small Cell Lung Cancer Specimens: Association with Clinicopathological Factors and Molecular Alterations" International Journal of Molecular Sciences 23, no. 9: 4517. https://doi.org/10.3390/ijms23094517
APA StyleMansour, M. S. I., Malmros, K., Mager, U., Ericson Lindquist, K., Hejny, K., Holmgren, B., Seidal, T., Dejmek, A., Dobra, K., Planck, M., & Brunnström, H. (2022). PD-L1 Expression in Non-Small Cell Lung Cancer Specimens: Association with Clinicopathological Factors and Molecular Alterations. International Journal of Molecular Sciences, 23(9), 4517. https://doi.org/10.3390/ijms23094517









