Encapsulation of Clofazimine by Cyclodextran: Preparation, Characterization, and In Vitro Release Properties
Abstract
1. Introduction
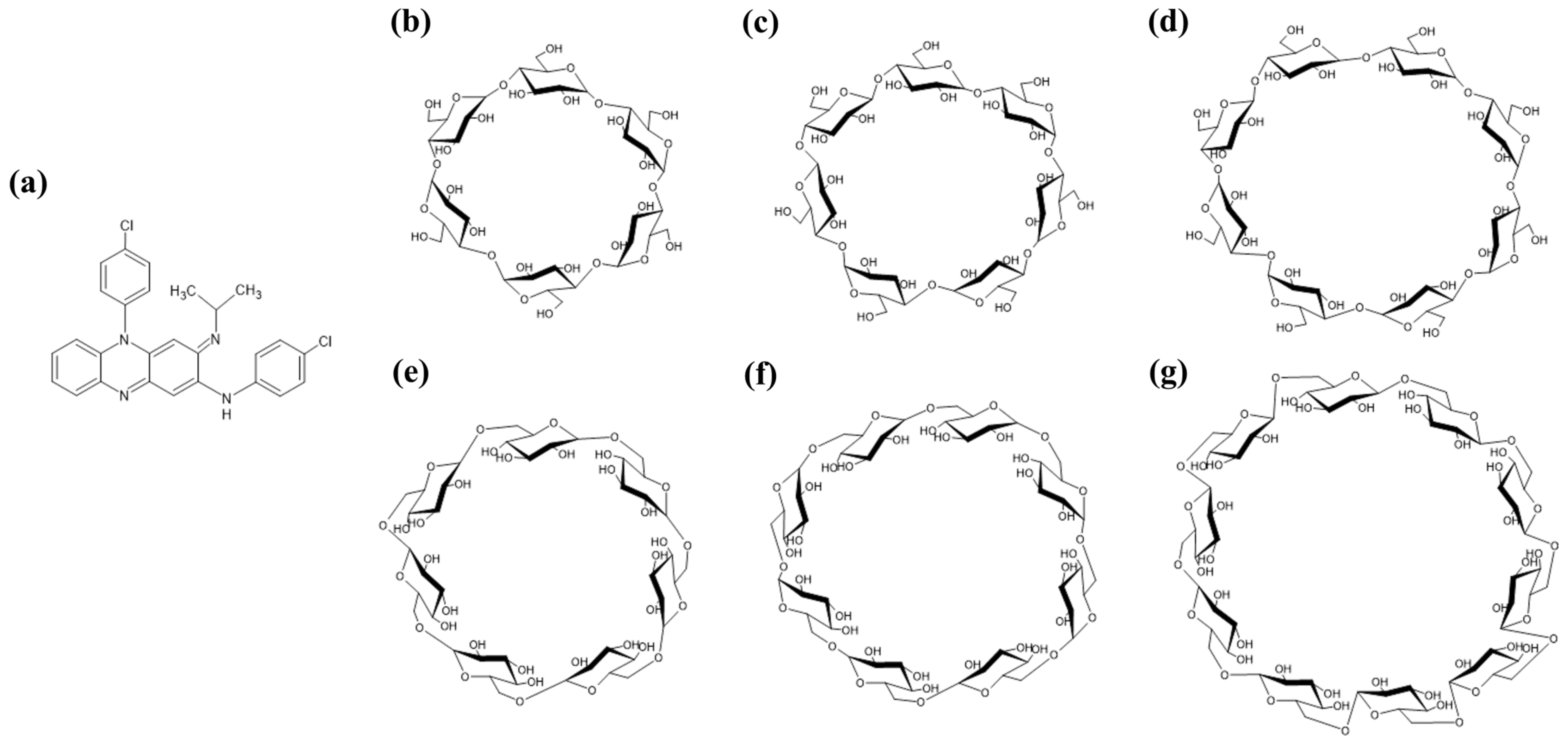
2. Results and Discussion
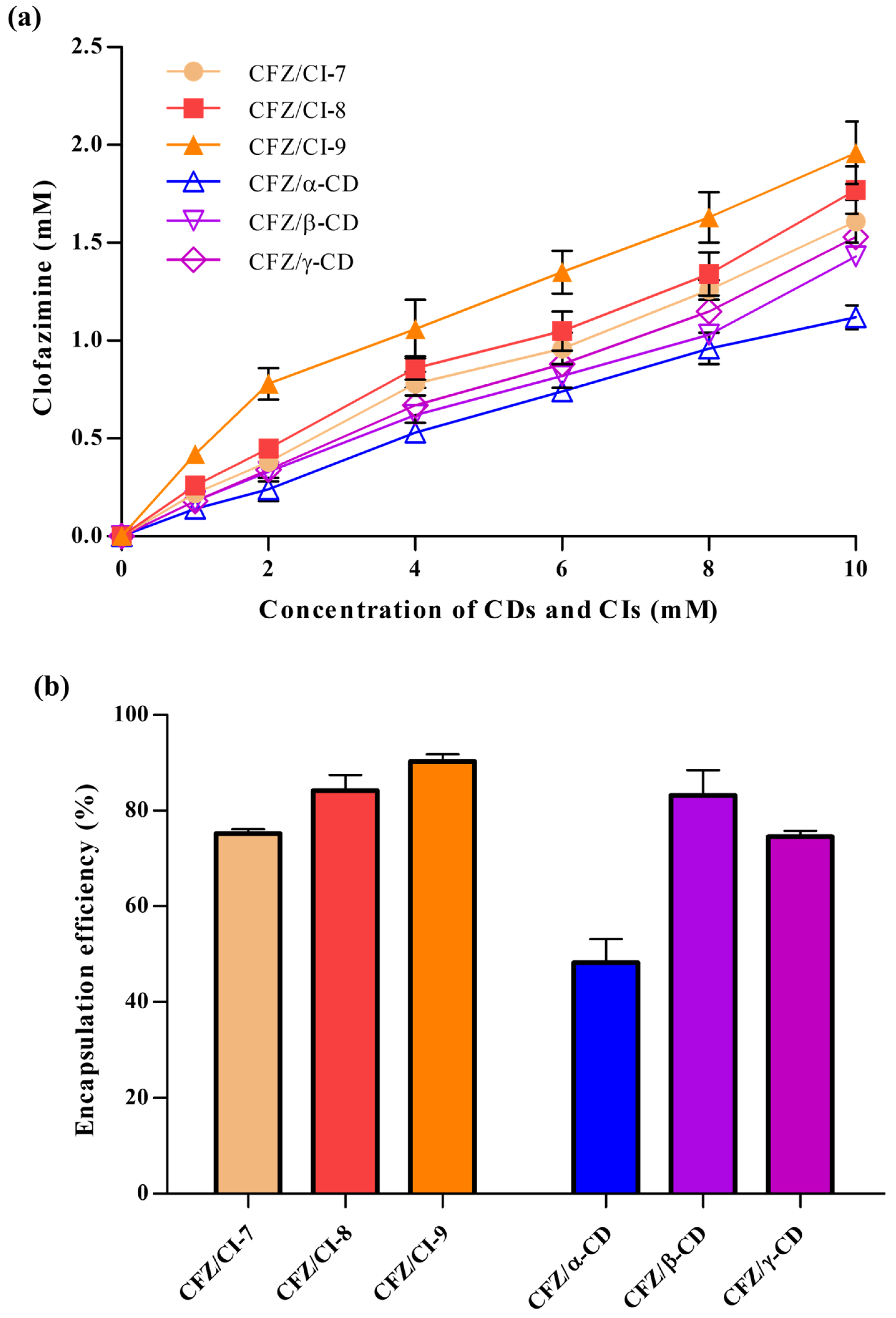
2.1. Phase Solubility Test
2.2. Encapsulation Efficiency
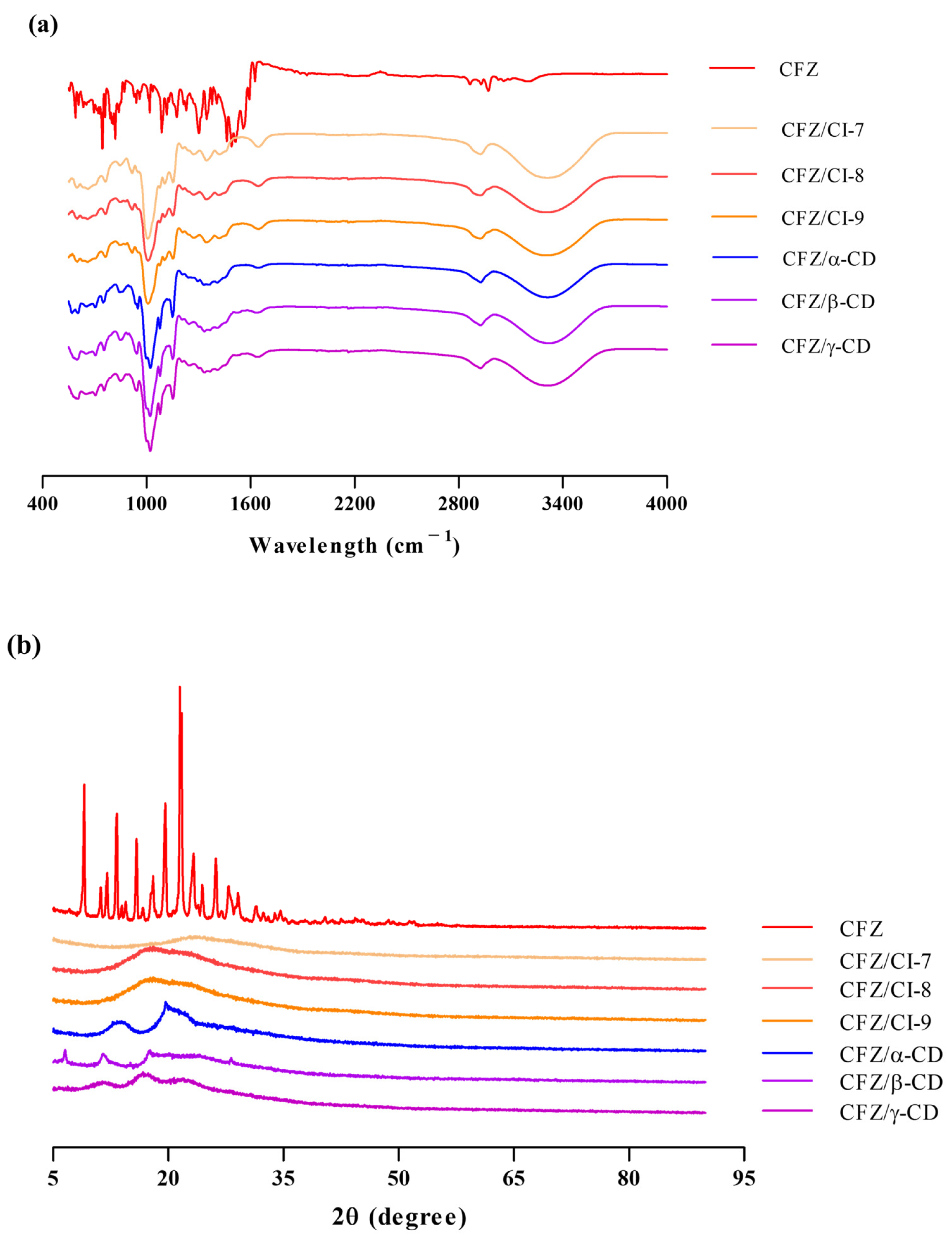
2.3. Physical Properties of CFZ/CI and CFZ/CD Complexes
2.3.1. FT-IR Analysis
2.3.2. X-ray Diffraction Analysis
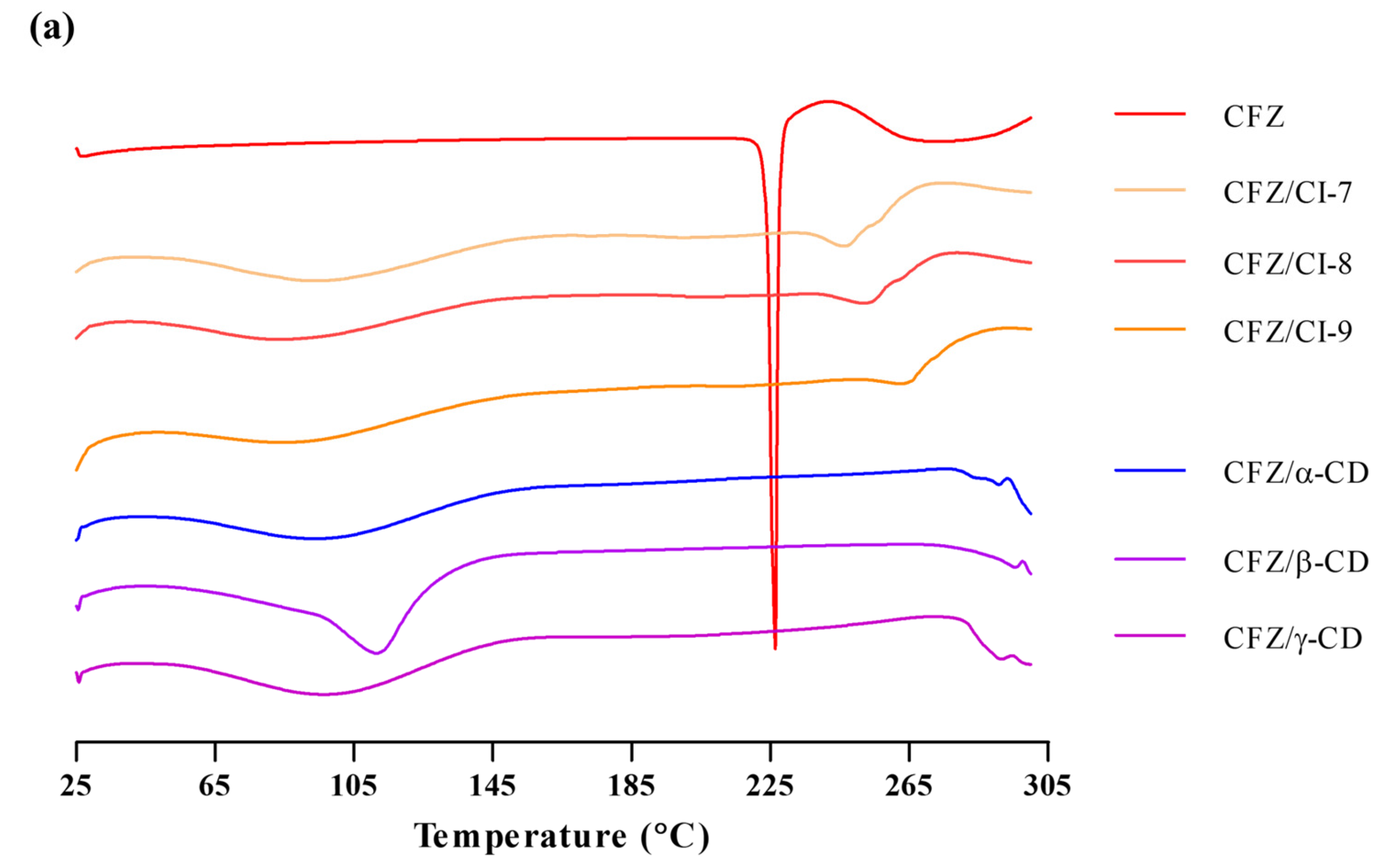
2.3.3. DSC Analysis
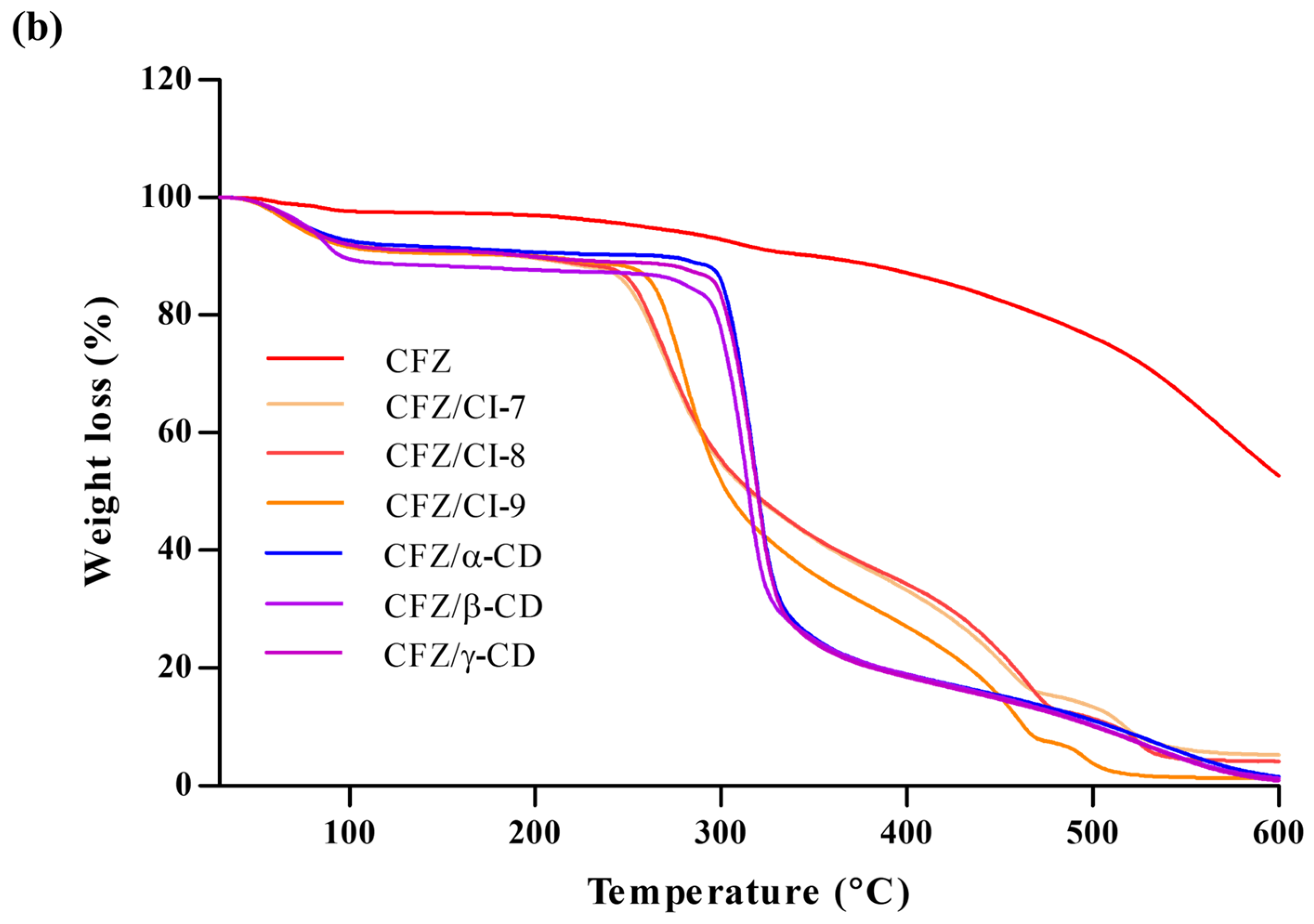
2.3.4. TGA
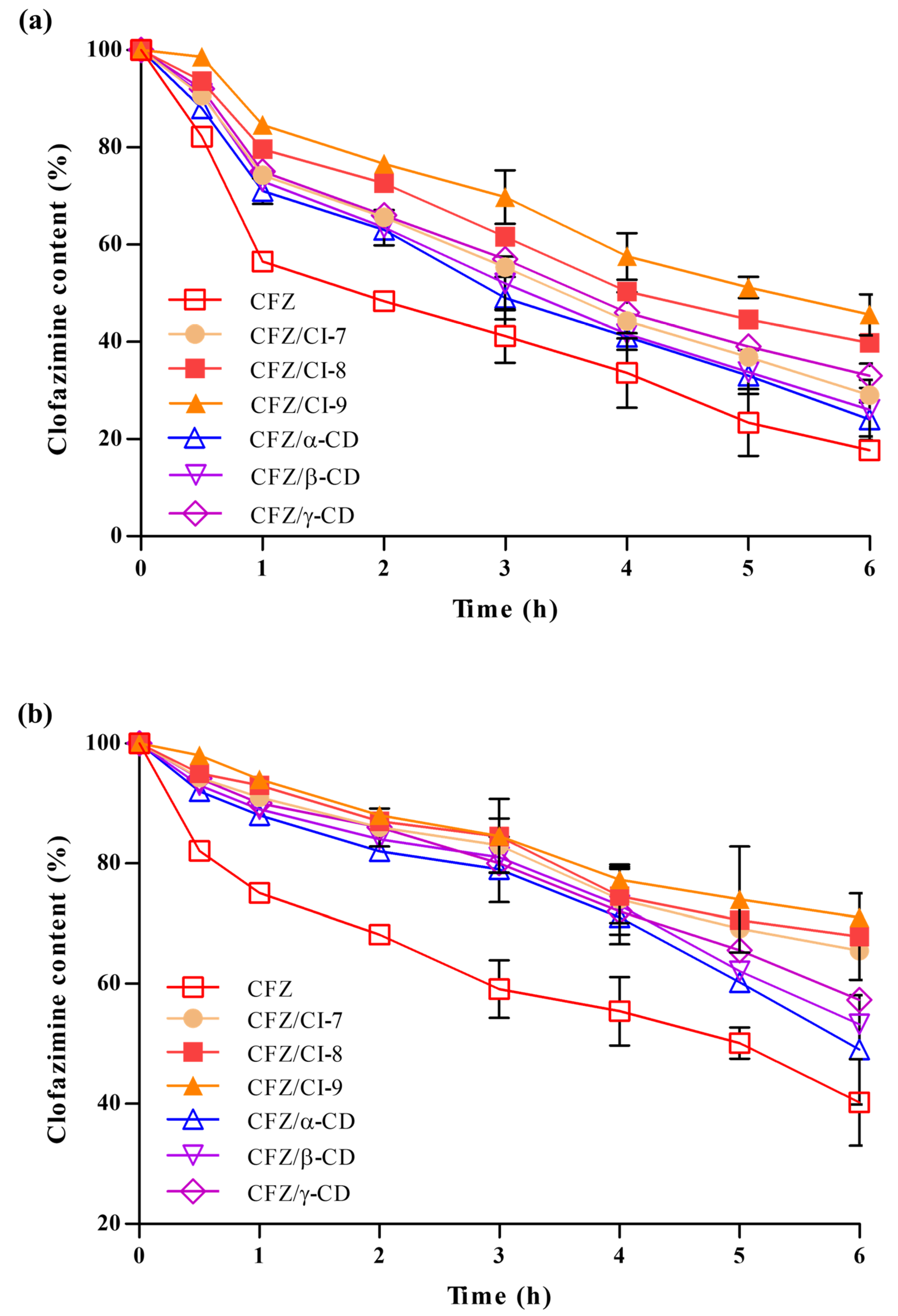
2.3.5. Stability Analysis
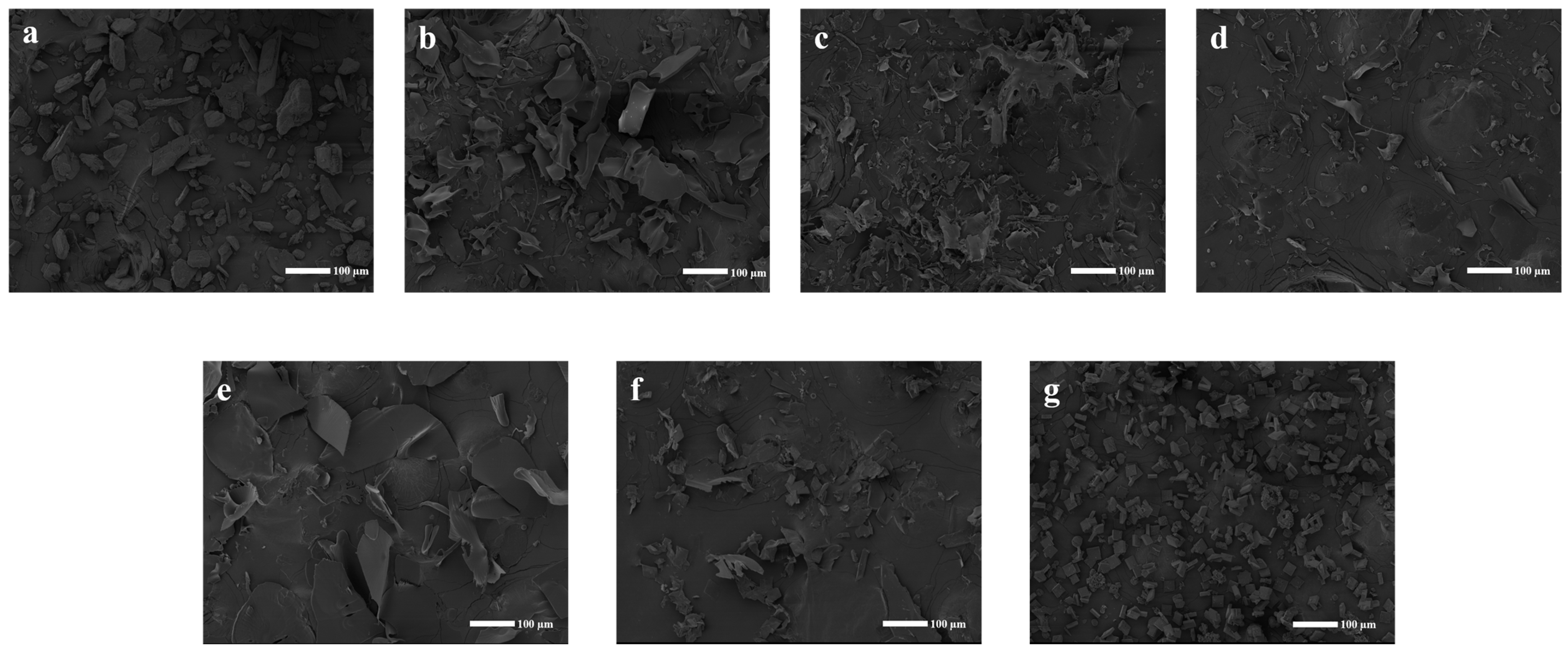
2.3.6. SEM Analysis
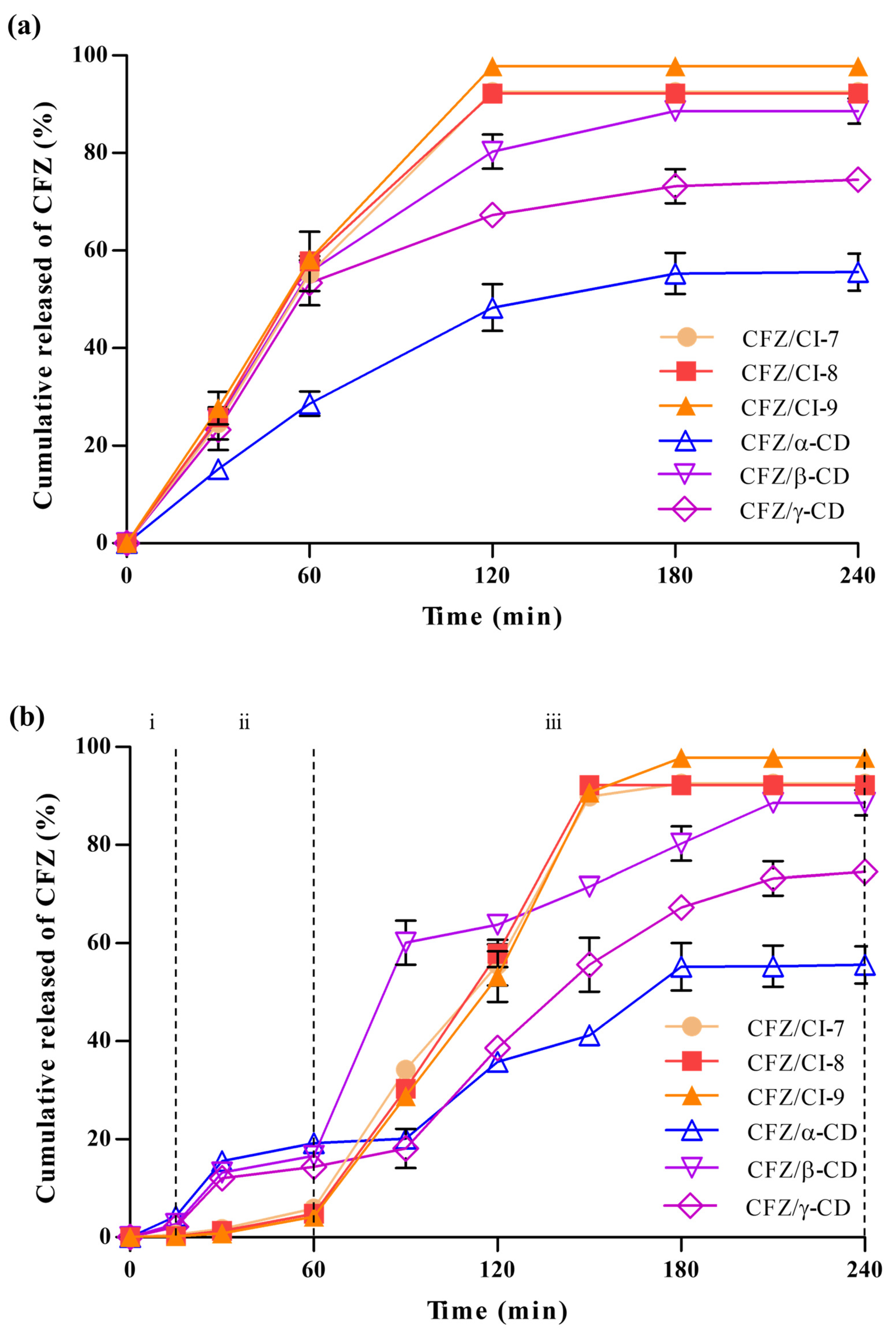
2.4. Drug Release Properties
2.4.1. Drug Release Analysis
2.4.2. In Vitro Simulated Drug Release Analysis
3. Materials and Methods
3.1. Materials and Chemicals
3.2. Preparation of the CFZ/CI and CFZ/CD Complexes
3.3. Phase Solubility Test
3.4. Encapsulation Efficiency (EE)
3.5. Physical Properties
3.5.1. FT-IR Analysis
3.5.2. X-ray Diffraction
3.5.3. Differential Scanning Calorimetry (DSC)
3.5.4. Thermogravimetric Analysis (TGA)
3.5.5. Stability Test
3.5.6. Scanning Electron Microscopy (SEM)
3.6. Drug Release Properties
3.6.1. Drug Release
3.6.2. In Vitro Simulated Digestion Release Analysis
3.7. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kornberg, H.L.; Krebs, H.A. A New Series of Phenazines (Rimino-Compounds) with High Antituberculosis Activity. Gr. Nat. Publ. 1957, 180, 756–757. [Google Scholar]
- Salem, I.I.; Steffan, G.; Düzgünes, N. Efficacy of Clofazimine-Modified Cyclodextrin against Mycobacterium avium Complex in Human Macrophages. Int. J. Pharm. 2003, 260, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Valetti, S.; Xia, X.; Costa-Gouveia, J.; Brodin, P.; Bernet-Camard, M.F.; Andersson, M.; Feiler, A. Clofazimine Encapsulation in Nanoporous Silica Particles for the Oral Treatment of Antibiotic-Resistant Mycobacterium tuberculosis Infections. Nanomedicine 2017, 12, 831–844. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, M.J.; Calcagno, T.; Hosseini, S.S.; Hematian, A. Role of Clofazimine in Treatment of Mycobacterium avium Complex. Front. Med. 2021, 8, 638306. [Google Scholar] [CrossRef] [PubMed]
- Ellard, G.A.; Pannikar, V.K.; Jesudasan, K.; Christian, M. Clofazimine and Dapsone Compliance in Leprosy. Lepr. Rev. 1988, 59, 205–213. [Google Scholar] [CrossRef]
- Medeiros Bezerra, E.L.; Pereira Vilar, M.J.; Da Trindade Neto, P.B.; Sato, E.I. Double-Blind, Randomized, Controlled Clinical Trial of Clofazimine Compared with Chloroquine in Patients with Systemic Lupus Erythematosus. Arthritis Rheum. 2005, 52, 3073–3078. [Google Scholar] [CrossRef]
- Salmaninejad, A.; Gowhari, A.; Hosseini, S.; Aslani, S.; Yousefi, M.; Bahrami, T.; Ebrahimi, M.; Nesaei, A.; Zal, M. Genetics and Immunodysfunction Underlying Behçet’s Disease and Immunomodulant Treatment Approaches. J. Immunotoxicol. 2017, 14, 137–151. [Google Scholar] [CrossRef]
- Gopal, M.; Padayatchi, N.; Metcalfe, J.Z.; O’Donnell, M.R. Systematic Review of Clofazimine for the Treatment of Drug-Resistant Tuberculosis. Int. J. Tuberc. Lung Dis. 2013, 17, 1001–1007. [Google Scholar] [CrossRef]
- Chen, W.; Cheng, C.; Lee, B.; Clemens, D.L.; Huang, W.; Horwitz, M.A.; Zink, I. Facile Strategy Enabling Both High Loading and High Release Amounts of the Water-Insoluble Drug Clofazimine Using Mesoporous Silica Nanoparticles. ACS Appl. Mater. Interfaces 2018, 10, 31870–31881. [Google Scholar] [CrossRef]
- De Castro, R.R.; Todaro, V.; da Silva, L.C.R.P.; Simon, A.; do Carmo, F.A.; de Sousa, V.P.; Rodrigues, C.R.; Sarmento, B.; Healy, A.M.; Cabral, L.M. Development of Inhaled Formulation of Modified Clofazimine as an Alternative to Treatment of Tuberculosis: Clofazimine Inhaled Formulation for Tuberculosis. J. Drug Deliv. Sci. Technol. 2020, 58, 101805. [Google Scholar] [CrossRef]
- Schwinté, P.; Ramphul, M.; Darcy, R.; O’Sullivan, J.F. Amphiphilic Cyclodextrin Complexation of Clofazimine. J. Incl. Phenom. 2003, 47, 109–112. [Google Scholar] [CrossRef]
- Poulson, B.G.; Alsulami, Q.A.; Sharfalddin, A.; El Agammy, E.F.; Mouffouk, F.; Emwas, A.-H.; Jaremko, L.; Jaremko, M. Cyclodextrins: Structural, Chemical, and Physical Properties, and Applications. Polysaccharides 2021, 3, 1. [Google Scholar] [CrossRef]
- Haimhoffer, Á.; Rusznyák, Á.; Réti-Nagy, K.; Vasvári, G.; Váradi, J.; Vecsernyés, M.; Bácskay, I.; Fehér, P.; Ujhelyi, Z.; Fenyvesi, F. Cyclodextrins in Drug Delivery Systems and Their Effects on Biological Barriers. Sci. Pharm. 2019, 87, 33. [Google Scholar] [CrossRef]
- Vyas, A.; Saraf, S.; Saraf, S. Cyclodextrin Based Novel Drug Delivery Systems. J. Incl. Phenom. Macrocycl. Chem. 2008, 62, 23–42. [Google Scholar] [CrossRef]
- Szejtli, J. Introduction and General Overview of Cyclodextrin Chemistry. Chem. Rev. 1998, 98, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Jansook, P.; Ogawa, N.; Loftsson, T. Cyclodextrins: Structure, Physicochemical Properties and Pharmaceutical Applications. Int. J. Pharm. 2018, 535, 272–284. [Google Scholar] [CrossRef]
- Harangi, J.; Béke, G.; Harangi, M.; Mótyán, J.A. The Digestable Parent Cyclodextrin. J. Incl. Phenom. Macrocycl. Chem. 2012, 73, 335–339. [Google Scholar] [CrossRef]
- Oguma, T.; Horiuchi, T.; Kobayashi, M. Novel Cyclic Dextrins, Cycloisomaltooligosaccharides, from Bacillus sp. T-3040 Culture. Biosci. Biotechnol. Biochem. 1993, 57, 1225–1227. [Google Scholar] [CrossRef]
- Oguma, T.; Kawamoto, H. Production of Cyclodextran and Its Application. Trends Glycosci. Glycotechnol. 2003, 15, 91–99. [Google Scholar] [CrossRef]
- Kobayashi, M.; Funane, K.; Oguma, T. Inhibition of Dextran and Mutan Synthesis by Cycloisomaltooligosaccharides. Biosci. Biotechnol. Biochem. 1995, 59, 1861–1865. [Google Scholar] [CrossRef]
- Salem, I.I.; Düzgünes, N. Efficacies of Cyclodextrin-Complexed and Liposome-Encapsulated Clarithromycin against Mycobacterium Avium Complex Infection in Human Macrophages. Int. J. Pharm. 2003, 250, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Groom, C.R.; Bruno, I.J.; Lightfoot, M.P.; Ward, S.C. The Cambridge Structural Database. Acta Crystallogr. Sect. B Struct. Sci. Cryst. Eng. Mater. 2016, 72, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-S. Study of Flavonoid/Hydroxypropyl-β-Cyclodextrin Inclusion Complexes by UV-Vis, FT-IR, DSC, and X-Ray Diffraction Analysis. Prev. Nutr. Food Sci. 2020, 25, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Catenacci, L.; Sorrenti, M.; Bonferoni, M.C.; Hunt, L.; Caira, M.R. Inclusion of the Phytoalexin Trans-Resveratrol in Native Cyclodextrins a Thermal, Spectroscopic, and X-ray Structural Study. Molecules 2020, 25, 998. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jin, Z.; Xu, X. Gamma-Cyclodextrin on Enhancement of Water Solubility and Store Stability of Nystatin. J. Incl. Phenom. Macrocycl. Chem. 2014, 78, 145–150. [Google Scholar] [CrossRef]
- Winkler, R.G.; Fioravanti, S.; Ciccotti, G.; Margheritis, C.; Villa, M. Hydration of β-Cyclodextrin: A Molecular Dynamics Simulation Study. J. Comput. Aided. Mol. Des. 2000, 14, 659–667. [Google Scholar] [CrossRef]
- Abarca, R.L.; Rodríguez, F.J.; Guarda, A.; Galotto, M.J.; Bruna, J.E. Characterization of Beta-Cyclodextrin Inclusion Complexes Containing an Essential Oil Component. Food Chem. 2016, 196, 968–975. [Google Scholar] [CrossRef]
- Hill, L.E.; Gomes, C.; Taylor, T.M. Characterization of Beta-Cyclodextrin Inclusion Complexes Containing Essential Oils (Trans-Cinnamaldehyde, Eugenol, Cinnamon Bark, and Clove Bud Extracts) for Antimicrobial Delivery Applications. LWT 2013, 51, 86–93. [Google Scholar] [CrossRef]
- Zhu, G.; Xiao, Z.; Zhou, R.; Zhu, Y. Study of Production and Pyrolysis Characteristics of Sweet Orange Flavor-β-Cyclodextrin Inclusion Complex. Carbohydr. Polym. 2014, 105, 75–80. [Google Scholar] [CrossRef]
- Giordano, F.; Novak, C.; Moyano, J.R. Thermal Analysis of Cyclodextrins and Their Inclusion Compounds. Thermochim. Acta 2001, 380, 123–151. [Google Scholar] [CrossRef]
- Trotta, F.; Zanetti, M.; Camino, G. Thermal Degradation of Cyclodextrins. Polym. Degrad. Stab. 2000, 69, 373–379. [Google Scholar] [CrossRef]
- Zarif, M.S.; Afidah, A.R.; Abdullah, J.M.; Shariza, A.R. Physicochemical Characterization of Vancomycin and Its Complexes with β-Cyclodextrin. Biomed. Res. 2012, 23, 513–520. [Google Scholar]
- Berkland, C.; King, M.; Cox, A.; Kim, K.; Pack, D.W. Precise Control of PLG Microsphere Size Provides Enhanced Control of Drug Release Rate. J. Control. Release 2002, 82, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.J.; Park, B.R.; Lee, H.N.; Jang, D.E.; Kang, H.J.; Ameer, K.; Kim, S.J.; Kim, Y.M. Carbohydrate-Binding Module of Cycloisomaltooligosaccharide Glucanotransferase from Thermoanaerobacter thermocopriae Improves Its Cyclodextran Production. Enzyme Microb. Technol. 2022, 157, 110023. [Google Scholar] [CrossRef] [PubMed]
- Mader, W.J.; Higuchi, T. Phase Solubility Analysis. CRC Crit. Rev. Anal. Chem. 1970, 1, 193–215. [Google Scholar] [CrossRef]
- Letona, C.A.M.; Luo, K.; Jeong, K.B.; Adra, H.J.; Park, C.S.; Kim, Y.R. Effect of Lecithin on the Spontaneous Crystallization of Enzymatically Synthesized Short-Chain Amylose Molecules into Spherical Microparticles. Polymers 2019, 11, 264. [Google Scholar] [CrossRef]
- Kim, J.Y.; Seo, T.R.; Lim, S.T. Preparation of Aqueous Dispersion of β-Carotene Nano-Composites through Complex Formation with Starch Dextrin. Food Hydrocoll. 2013, 33, 256–263. [Google Scholar] [CrossRef]
- Popat, A.; Karmakar, S.; Jambhrunkar, S.; Xu, C.; Yu, C. Curcumin-Cyclodextrin Encapsulated Chitosan Nanoconjugates with Enhanced Solubility and Cell Cytotoxicity. Colloids Surf. B Biointerfaces 2014, 117, 520–527. [Google Scholar] [CrossRef]
- Brodkorb, A.; Egger, L.; Alminger, M.; Alvito, P.; Assunção, R.; Ballance, S.; Bohn, T.; Bourlieu-Lacanal, C.; Boutrou, R.; Carrière, F.; et al. INFOGEST Static in vitro Simulation of Gastrointestinal Food Digestion. Nat. Protoc. 2019, 14, 991–1014. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, S.-J.; Kim, Y.-M. Encapsulation of Clofazimine by Cyclodextran: Preparation, Characterization, and In Vitro Release Properties. Int. J. Mol. Sci. 2023, 24, 8808. https://doi.org/10.3390/ijms24108808
Hong S-J, Kim Y-M. Encapsulation of Clofazimine by Cyclodextran: Preparation, Characterization, and In Vitro Release Properties. International Journal of Molecular Sciences. 2023; 24(10):8808. https://doi.org/10.3390/ijms24108808
Chicago/Turabian StyleHong, Seong-Jin, and Young-Min Kim. 2023. "Encapsulation of Clofazimine by Cyclodextran: Preparation, Characterization, and In Vitro Release Properties" International Journal of Molecular Sciences 24, no. 10: 8808. https://doi.org/10.3390/ijms24108808
APA StyleHong, S.-J., & Kim, Y.-M. (2023). Encapsulation of Clofazimine by Cyclodextran: Preparation, Characterization, and In Vitro Release Properties. International Journal of Molecular Sciences, 24(10), 8808. https://doi.org/10.3390/ijms24108808






