Free Light Chains κ and λ as New Biomarkers of Selected Diseases
Abstract
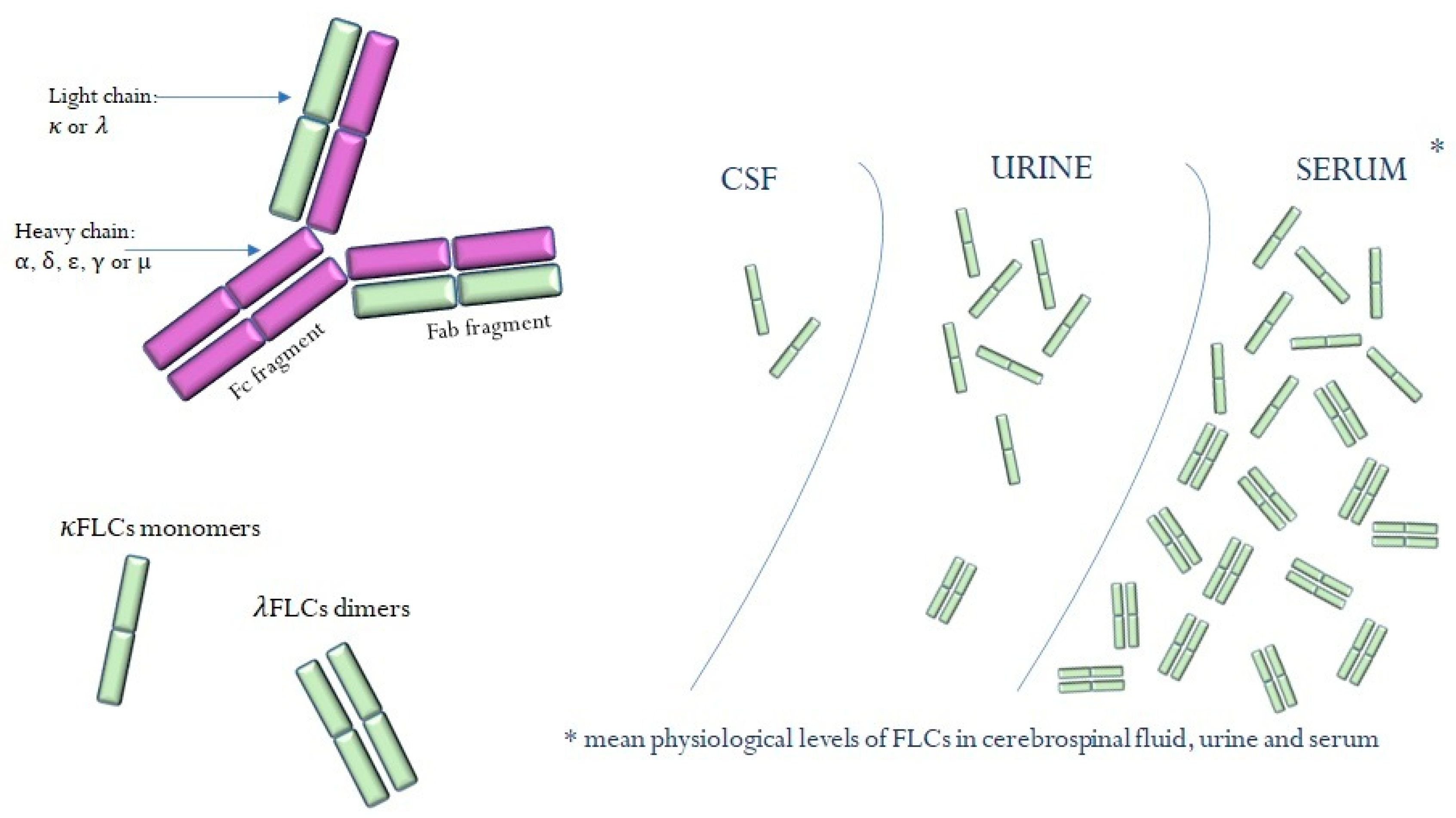
:1. Introduction
2. Material and Methods
3. Results
3.1. Monoclonal Gammopathy
3.2. Multiple Sclerosis
3.3. Viral Infections
3.3.1. COVID-19
3.3.2. Hepatitis C
3.3.3. Hepatitis B
3.3.4. AIDS
3.4. Tick-Borne Diseases
3.4.1. Lyme Disease
3.4.2. Tick-Borne Encephalitis
3.5. Diabetes
3.6. Cardiovascular Disorders
3.7. Rheumatic Diseases
3.8. Cancers
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Schroeder, H.W., Jr.; Cavacini, L. Structure and function of immunoglobulins. J. Allergy Clin. Immunol. 2010, 125 (Suppl. 2), S41–S52. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Huang, T.; Hammarström, L.; Zhao, Y. The Immunoglobulins: New Insights, Implications, and Applications. Annu. Rev. Anim. Biosci. 2020, 8, 145–169. [Google Scholar] [CrossRef] [PubMed]
- Mix, E.; Goertsches, R.; Zett, U.K. Immunoglobulins—Basic considerations. J. Neurol. 2006, 253 (Suppl. 5), V9–V17. [Google Scholar] [CrossRef] [PubMed]
- Tosi, P.; Tomassetti, S.; Merli, A.; Polli, V. Serum free light-chain assay for the detection and monitoring of multiple myeloma and related conditions. Ther. Adv. Hematol. 2013, 4, 37–41. [Google Scholar] [CrossRef]
- Vani, B.; Ritu, A.; Praveen, S.; Pankaj, M.; Minz, R. Excess Free Light Chains in Serum Immunofixation Electrophoresis: Attributes of a Distinctive Pattern. Indian J. Hematol. Blood Transfus. 2018, 34, 632–635. [Google Scholar] [CrossRef]
- Katzmann, J.A.; Clark, R.J.; Abraham, R.S.; Bryant, S.; Lymp, J.F.; Bradwell, A.R.; Kyle, R.A. Serum reference intervals and diagnostic ranges for free kappa and free lambda immunoglobulin light chains: Relative sensitivity for detection of monoclonal light chains. Clin. Chem. 2002, 48, 1437–1444. [Google Scholar] [CrossRef]
- Redegeld, F.A.; Thio, M.; Kormelink, T.G. Polyclonal immunoglobulin free light chain and chronic inflammation. Mayo Clin. Proc. 2012, 87, 1032–1033. [Google Scholar] [CrossRef]
- Brebner, J.A.; Stockley, R.A. Polyclonal free light chains: A biomarker of inflammatory disease or treatment target? F1000 Med. Rep. 2013, 5, 4. [Google Scholar] [CrossRef]
- Bhole, M.V.; Sadler, R.; Ramasamy, K. Serum-free light-chain assay: Clinical utility and limitations. Ann. Clin. Biochem. 2014, 51, 528–542. [Google Scholar] [CrossRef]
- Xu, Z.L.; Wu, C.; Teng, W.-H.; Wan, K.; Jia, W.J.; Li, H.J.; Meng, L.; Zhou, J.F.; Tang, Y. Exploring the Relationship Between Serum and Urinary Free Light Chain Levels During the Different Phases of Renal Damage in Multiple Myeloma Patients. Indian J. Hematol. Blood Transfus. Off. J. Indian Soc. Hematol. Blood Transfus. 2015, 31, 352–355. [Google Scholar] [CrossRef]
- Ferraro, D.; Trovati, A.; Bedin, R.; Natali, P.; Franciotta, D.; Santangelo, M.; Camera, V.; Vitetta, F.; Varani, M.; Trenti, T.; et al. Cerebrospinal fluid kappa and lambda free light chains in oligoclonal band-negative patients with suspected multiple sclerosis. Eur. J. Neurol. 2020, 27, 461–467. [Google Scholar] [CrossRef]
- Aggarwal, R.; Sequeira, W.; Kokebie, R.; Mikolaitis, R.A.; Fogg, L.; Finnegan, A.; Plaas, A.; Block, J.A.; Jolly, M. Serum free light chains as biomarkers for systemic lupus erythematosus disease activity. Arthritis Care Res. 2011, 63, 891–898. [Google Scholar] [CrossRef]
- Glavey, S.V.; Leung, N. Monoclonal gammopathy: The good, the bad and the ugly. Blood Rev. 2016, 30, 223–231. [Google Scholar] [CrossRef]
- Kyle, R.A. The monoclonal gammopathies. Clin. Chem. 1994, 40, 2154–2161. [Google Scholar] [CrossRef]
- Ríos-Tamayo, R.; Paiva, B.; Lahuerta, J.J.; López, J.M.; Duarte, R.F. Monoclonal Gammopathies of Clinical Significance: A Critical Appraisal. Cancers 2022, 14, 5247. [Google Scholar] [CrossRef]
- Dimopoulos, M.; Kyle, R.; Fermand, J.-P.; Rajkumar, S.V.; Miguel, J.S.; Chanan-Khan, A.; Ludwig, H.; Joshua, D.; Mehta, J.; Gertz, M.; et al. Consensus recommendations for standard investigative workup: Report of the International Myeloma Workshop Consensus Panel 3. Blood 2011, 117, 4701–4705. [Google Scholar] [CrossRef]
- Milani, P.; Merlini, G.; Palladini, G. Light Chain Amyloidosis. Hematol. Infect. Dis. 2018, 10, e2018022. [Google Scholar] [CrossRef]
- Phull, P.; Sanchorawala, V.; Connors, L.H.; Doros, G.; Ruberg, F.L.; Berk, J.L.; Sarosiek, S. Monoclonal gammopathy of undetermined significance in systemic transthyretin amyloidosis (ATTR). Amyloid 2018, 25, 62–67. [Google Scholar] [CrossRef]
- Mankad, A.K.; Sesay, I.; Shah, K.B. Light-chain cardiac amyloidosis. Curr. Probl. Cancer 2017, 41, 144–156. [Google Scholar] [CrossRef]
- Deng, X.; Crowson, C.S.; Rajkumar, S.V.; Dispenzieri, A.; Larson, D.R.; Therneau, T.M.; Matteson, E.L.; Kyle, R.A.; Katzmann, J.A.; Gabriel, S.E.; et al. Elevation of serum immunoglobulin free light chains during the preclinical period of rheumatoid arthritis. J. Rheumatol. 2015, 42, 181–187. [Google Scholar] [CrossRef]
- Czyżewska, E.; Wiśniewska, A.; Waszczuk-Gajda, A.; Ciepiela, O. The Role of Light Kappa and Lambda Chains in Heart Function Assessment in Patients with AL Amyloidosis. J. Clin. Med. 2021, 10, 1274. [Google Scholar] [CrossRef] [PubMed]
- Muchtar, E.; Gertz, M.A.; Lacy, M.Q.; Go, R.S.; Buadi, F.K.; Dingli, D.; Grogan, M.; AbouEzzeddine, O.F.; Hayman, S.R.; Kapoor, P.; et al. Ten-year survivors in AL amyloidosis: Characteristics and treatment pattern. Br. J. Haematol. 2019, 187, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Gertz, M.A. Immunoglobulin Light Chain Amyloidosis: 2020 Update on Diagnosis, Prognosis, and Treatment. Am. J. Hematol. 2020, 95, 848–860. [Google Scholar] [CrossRef] [PubMed]
- Posadas-Martinez, M.L.; Aguirre, M.A.; Brulc, E.; Saez, M.S.; Sorroche, P.; Machnicki, G.; Fernandez, M.; Nucifora, E.M. Treatment patterns and outcomes in light chain amyloidosis: An institutional registry of amyloidosis report in Argentina. PLoS ONE 2022, 17, e0274578. [Google Scholar] [CrossRef]
- Kumar, S.; Larson, D.R.; Dispenzieri, A.; Therneau, T.M.; Murray, D.L.; Bergsagel, P.L.; Kyle, R.A.; Rajkumar, S.V. Polyclonal serum free light chain elevation is associated with increased risk of monoclonal gammopathies. Blood Cancer J. 2019, 9, 49. [Google Scholar] [CrossRef]
- Mead, G.P.; Carr-Smith, H.D.; Drayson, M.T.; Morgan, G.J.; Child, J.A.; Bradwell, A.R. Serum free light chains for monitoring multiple myeloma. Br. J. Haematol. 2004, 126, 348–354. [Google Scholar] [CrossRef]
- Milani, P.; Palladini, G.; Merlini, G. Serum-free light-chain analysis in diagnosis and management of multiple myeloma and related conditions. Scand. J. Clin. Lab. Investig. 2016, 76 (Suppl. 245), S113–S118. [Google Scholar] [CrossRef]
- El Naggar, A.A.; El-Naggar, M.; Mokhamer, E.-H.; Avad, M.W. Prognostic Value of Serum Free Light Chain in Multiple Myeloma. Egypt. J. Immunol. 2015, 22, 69–78. [Google Scholar]
- Zhang, S.-S.; Wu, S.; Qu, X.-Y.; Xu, J.; Liu, P.; Lü, H.; Wu, H.-X.; Xu, J.-R.; Li, J.-Y.; Chen, L.-J. Clinical significance of serum free light chain in patients with multiple myeloma. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2013, 21, 930–935. [Google Scholar] [CrossRef]
- Bracco, F.; Gallo, P.; Menna, R.; Battistin, L.; Tavolato, B. Free light chains in the CSF in multiple sclerosis. J. Neurol. 1987, 234, 303–307. [Google Scholar] [CrossRef]
- Vecchio, D.; Bellomo, G.; Serino, R.; Virgilio, E.; Lamonaca, M.; Dianzani, U.; Cantello, R.; Comi, C.; Crespi, I. Intrathecal kappa free light chains as markers for multiple sclerosis. Sci. Rep. 2020, 10, 20329. [Google Scholar] [CrossRef]
- Rosenstein, I.; Rasch, S.; Axelsson, M.; Novakova, L.; Blennow, K.; Zetterberg, H.; Lycke, J. Kappa free light chain index as a diagnostic biomarker in multiple sclerosis: A real-world investigation. J. Neurochem. 2021, 159, 618–628. [Google Scholar] [CrossRef]
- Martins, D.A.; Lopes, J.; da Silva, A.M.; Morais, C.I.; Vasconcelos, J.; Lima, I.; Carneiro, C.; Neves, E. Kappa free light chains: Diagnostic performance in multiple sclerosis and utility in a clinical laboratory. Clin. Chim. Acta 2022, 528, 56–64. [Google Scholar] [CrossRef]
- Berek, K.; Bsteh, G.; Auer, M.; Di Pauli, F.; Grams, A.; Milosavljevic, D.; Poskaite, P.; Schnabl, C.; Wurth, S.; Zinganell, A.; et al. Kappa-Free Light Chains in CSF Predict Early Multiple Sclerosis Disease Activity. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1005. [Google Scholar] [CrossRef]
- Cavalla, P.; Caropreso, P.; Limoncelli, S.; Bosa, C.; Pasanisi, M.; Schillaci, V.; Alteno, A.; Costantini, G.; Giordana, M.; Mengozzi, G.; et al. Kappa free light chains index in the differential diagnosis of Multiple Sclerosis from Neuromyelitis optica spectrum disorders and other immune-mediated central nervous system disorders. J. Neuroimmunol. 2020, 339, 577122. [Google Scholar] [CrossRef]
- Gudowska-Sawczuk, M.; Tarasiuk, J.; Kułakowska, A.; Kochanowicz, J.; Mroczko, B. Kappa Free Light Chains and IgG Combined in a Novel Algorithm for the Detection of Multiple Sclerosis. Brain Sci. 2020, 10, 324. [Google Scholar] [CrossRef]
- Presslauer, S.; Milosavljevic, D.; Brücke, T.; Bayer, P.; Hübl, W. Elevated levels of kappa free light chains in CSF support the diagnosis of multiple sclerosis. J. Neurol. 2008, 255, 1508–1514. [Google Scholar] [CrossRef]
- Presslauer, S.; Milosavljevic, D.; Huebl, W.; Parigger, S.; Schneider-Koch, G.; Bruecke, T. Kappa free light chains: Diagnostic and prognostic relevance in MS and CIS. PLoS ONE 2014, 9, e89945. [Google Scholar] [CrossRef]
- Cutellè, C.; Balducci, C.; Cereda, D.; Fusco, M.L.; Iacobucci, D.; Perugini, J.; Pirro, F.; Brivio, R.; Bernasconi, D.P.; Ferrarese, C.; et al. K index utility as diagnostic and prognostic biomarker in the assessment of patients with suspected Multiple Sclerosis. J. Neuroimmunol. 2022, 373, 577992. [Google Scholar] [CrossRef]
- Voortman, M.M.; Stojakovic, T.; Pirpamer, L.; Jehna, M.; Langkammer, C.; Scharnagl, H.; Reindl, M.; Ropele, S.; Seifert-Held, T.; Archelos, J.-J.; et al. Prognostic value of free light chains lambda and kappa in early multiple sclerosis. Mult. Scler. 2017, 23, 1496–1505. [Google Scholar] [CrossRef]
- Menéndez-Valladares, P.; García-Sánchez, M.I.; Benítez, P.C.; Lucas, M.; Martínez, M.A.; Galán, V.C.; De Veas Silva, J.L.G.; Guitarte, C.B.; Ayuso, G.I. Free kappa light chains in cerebrospinal fluid as a biomarker to assess risk conversion to multiple sclerosis. Mult. Scler. J.-Exp. Transl. Clin. 2015, 1, 2055217315620935. [Google Scholar] [CrossRef] [PubMed]
- Hegen, H.; Arrambide, G.; Gnanapavan, S.; Kaplan, B.; Khalil, M.; Saadeh, R.; Teunissen, C.; Tumani, H.; Villar, L.M.; Willrich, M.A.V.; et al. Cerebrospinal fluid kappa free light chains for the diagnosis of multiple sclerosis: A consensus statement. Mult. Scler. 2023, 29, 182–195. [Google Scholar] [CrossRef] [PubMed]
- Małecka-Giełdowska, M.; Fołta, M.; Wiśniewska, A.; Czyżewska, E.; Ciepiela, O. Cell Population Data and Serum Polyclonal Immunoglobulin Free Light Chains in the Assessment of COVID-19 Severity. Viruses 2021, 13, 1381. [Google Scholar] [CrossRef] [PubMed]
- Gudowska-Sawczuk, M.; Moniuszko-Malinowska, A.; Pączek, S.; Guziejko, K.; Chorąży, M.; Mroczko, B. Evaluation of Free Light Chains (FLCs) Synthesis in Response to Exposure to SARS-CoV-2. Int. J. Mol. Sci. 2022, 23, 11589. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, I.S.; Cabral, M.S.; Jesus, L.S.; Paraná, R.; Atta, A.M.; Atta, M.L.B.S. Serum levels of immunoglobulin free light chains in patients with chronic hepatitis C presenting cryoglobulinemia. Braz. J. Infect. Dis. Off. Publ. Braz. Soc. Infect. Dis. 2014, 18, 638–642. [Google Scholar] [CrossRef]
- Basile, U.; Napodano, C.; Pocino, K.; Gulli, F.; Santini, S.A.; Todi, L.; Marino, M.; Rapaccini, G.L. Serological profile of asymptomatic HCV positive patients with low level of cryoglobulins. BioFactors 2019, 45, 318–325. [Google Scholar] [CrossRef]
- Basile, U.; Marino, M.; Gragnani, L.; Napodano, C.; Gulli, F.; Pocino, K.; Lorini, S.; Santini, S.A.; Basile, V.; Miele, L.; et al. Sentinel biomarkers in HCV positive patients with mixed cryoglobulinemia. J. Immunol. Methods 2020, 476, 112687. [Google Scholar] [CrossRef]
- Terrier, B.; Sène, D.; Saadoun, D.; Ghillani-Dalbin, P.; Thibault, V.; Delluc, A.; Piette, J.-C.; Cacoub, P. Serum-free light chain assessment in hepatitis C virus-related lymphoproliferative disorders. Ann. Rheum. Dis. 2009, 68, 89–93. [Google Scholar] [CrossRef]
- Terrier, B.; Chaara, W.; Dufat, L.; Geri, G.; Rosenzwajg, M.; Musset, L.; Sène, D.; Saadoun, D.; Six, A.; Klatzmann, D.; et al. Serum biomarker signature identifies patients with B-cell non-Hodgkin lymphoma associated with cryoglobulinemia vasculitis in chronic HCV infection. Autoimmun. Rev. 2014, 13, 319–326. [Google Scholar] [CrossRef]
- Gragnani, L.; Lorini, S.; Marri, S.; Basile, U.; Santarlasci, V.; Monti, M.; Madia, F.; Petraccia, L.; Stasi, C.; Marello, N.; et al. Hematological and Genetic Markers in the Rational Approach to Patients with HCV Sustained Virological Response with or without Persisting Cryoglobulinemic Vasculitis. Hepatology 2021, 74, 1164–1173. [Google Scholar] [CrossRef]
- Basile, U.; Gragnani, L.; Piluso, A.; Gulli, F.; Urraro, T.; Dell’Abate, M.T.; Torti, E.; Stasi, C.; Monti, M.; Rapaccini, G.L.; et al. Assessment of free light chains in HCV-positive patients with mixed cryoglobulinaemia vasculitis undergoing rituximab treatment. Liver Int. Off. J. Int. Assoc. Study Liver 2015, 35, 2100–2107. [Google Scholar] [CrossRef]
- Basile, U.; Napodano, C.; Pocino, K.; Marino, M.; A Santini, S.; Barini, A.; Stefanile, A.; Basile, V.; A Callà, C.; Cattani, P.; et al. Lack of association between Vitamin D status and free light chains profile with different chronic HCV-related liver and extrahepatic disorders. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 8506–8514. [Google Scholar] [CrossRef]
- Chen, B.; Wang, W.; Xu, W.; Ying, L.; Zhou, C.; Zheng, M. Serum free light chain is associated with histological activity and cirrhosis in patients with chronic hepatitis B. Int. Immunopharmacol. 2021, 99, 107881. [Google Scholar] [CrossRef]
- Klimas, N.; Koneru, A.O.; Fletcher, M.A. Overview of HIV. Psychosom. Med. 2008, 70, 523–530. [Google Scholar] [CrossRef]
- Nunnari, G.; A Smith, J.; Daniel, R. HIV-1 Tat and AIDS-associated cancer: Targeting the cellular anti-cancer barrier? J. Exp. Clin. Cancer Res. 2008, 27, 3. [Google Scholar] [CrossRef]
- Zemlin, A.E.; Ipp, H.; Rensburg, M.A.; Germishuys, J.J.; Esser, M.M.; Olivier, M.; Erasmus, R.T. Serum free light chains in patients with HIV infection: Their association with markers of disease severity and antiretroviral use. J. Clin. Pathol. 2015, 68, 148–153. [Google Scholar] [CrossRef]
- Gallo, P.; Piccinno, M.; De Rossi, A.; Pagni, S.; Amadori, A.; Chiecobianchi, L.; Tavolato, B. Free light chains of immunoglobulins in the cerebrospinal fluid of human immunodeficiency virus type 1-infected patients. J. Neuroimmunol. 1990, 26, 229–238. [Google Scholar] [CrossRef]
- Elovaara, I.; Seppälä, I.; Kinnunen, E.; Laaksovirta, H. Increased occurrence of free immunoglobulin light chains in cerebrospinal fluid and serum in human immunodeficiency virus-1 infection. J. Neuroimmunol. 1991, 35, 65–77. [Google Scholar] [CrossRef]
- Gallo, P.; Laverda, A.M.; DE Rossi, A.; Pagni, S.; DEL Mistro, A.; Cogo, P.; Piccinno, M.G.; Plebani, A.; Tavolato, B.; Chieco-Bianchi, L. Immunological markers in the cerebrospinal fluid of HIV-1-infected children. Acta Paediatr. 1991, 80, 659–666. [Google Scholar] [CrossRef]
- Shiels, M.S.; Landgren, O.; Costello, R.; Zingone, A.; Goedert, J.J.; Engels, E.A. Free light chains and the risk of AIDS-defining opportunistic infections in HIV-infected individuals. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2012, 55, e103–e108. [Google Scholar] [CrossRef]
- Landgren, O.; Goedert, J.J.; Rabkin, C.S.; Wilson, W.H.; Dunleavy, K.; Kyle, R.A.; Katzmann, J.A.; Rajkumar, S.V.; Engels, E.A. Circulating serum free light chains as predictive markers of AIDS-related lymphoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Bibas, M.; Trotta, M.P.; Cozzi-Lepri, A.; Lorenzini, P.; Pinnetti, C.; Rizzardini, G.; Angarano, G.; Caramello, P.; Sighinolfi, L.; Mastroianni, C.M.; et al. Role of serum free light chains in predicting HIV-associated non-Hodgkin lymphoma and Hodgkin’s lymphoma and its correlation with antiretroviral therapy. Am. J. Hematol. 2012, 87, 749–753. [Google Scholar] [CrossRef] [PubMed]
- Tittle, V.; Rayment, M.; Keeling, E.; Gabriel, I.; Yarranton, H.; Bower, M. Serum-free light chains in HIV-associated lymphoma: No correlation with histology or prognosis. AIDS 2015, 29, 1201–1204. [Google Scholar] [CrossRef]
- Hegen, H.; Milosavljevic, D.; Schnabl, C.; Manowiecka, A.; Walde, J.; Deisenhammer, F.; Presslauer, S. Cerebrospinal fluid free light chains as diagnostic biomarker in neuroborreliosis. Clin. Chem. Lab. Med. 2018, 56, 1383–1391. [Google Scholar] [CrossRef] [PubMed]
- Gudowska-Sawczuk, M.; Czupryna, P.; Moniuszko-Malinowska, A.; Pancewicz, S.; Mroczko, B. Free Immunoglobulin Light Chains in Patients with Tick-Borne Encephalitis: Before and after Treatment. J. Clin. Med. 2021, 10, 2922. [Google Scholar] [CrossRef]
- Banday, M.Z.; Sameer, A.S.; Nissar, S. Pathophysiology of diabetes: An overview. Avicenna J. Med. 2020, 10, 174. [Google Scholar] [CrossRef]
- Tsalamandris, S.; Antonopoulos, A.S.; Oikonomou, E.; Papamikroulis, G.-A.; Vogiatzi, G.; Papaioannou, S.; Deftereos, S.; Tousoulis, D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur. Cardiol. Rev. 2019, 14, 50–59. [Google Scholar] [CrossRef]
- Matsumori, A.; Shimada, T.; Shimada, M.; Drayson, M.T. Immunoglobulin free light chains: An inflammatory biomarker of diabetes. Inflamm. Res. Off. J. Eur. Histamine Res. Soc. 2020, 69, 715–718. [Google Scholar] [CrossRef]
- Aberer, F.; Tripolt, N.J.; Scharnagl, H.; Zedler, J.; Eder, M.; Oulhaj, A.; Stojakovic, T.; Sourij, H. Combined serum free light chain levels are associated with carotid atherosclerosis in type 2 diabetes mellitus. Diabetes Vasc. Dis. Res. 2018, 15, 162–164. [Google Scholar] [CrossRef]
- Bellary, S.; Faint, J.M.; Assi, L.K.; Hutchison, C.A.; Harding, S.J.; Raymond, N.T.; Barnett, A.H. Elevated serum free light chains predict cardiovascular events in type 2 diabetes. Diabetes Care 2014, 37, 2028–2030. [Google Scholar] [CrossRef]
- Tziomalos, K.; Weerasinghe, C.N.; Mikhailidis, D.P.; Seifalian, A.M. Vascular risk factors in South Asians. Int. J. Cardiol. 2008, 128, 5–16. [Google Scholar] [CrossRef]
- Hutchison, C.A.; Cockwell, P.; Harding, S.; Mead, G.P.; Bradwell, A.R.; Barnett, A.H. Quantitative assessment of serum and urinary polyclonal free light chains in patients with type II diabetes: An early marker of diabetic kidney disease? Expert Opin. Ther. Targets 2008, 12, 667–676. [Google Scholar] [CrossRef]
- Basile, U.; La Rosa, G.; Napodano, C.; Pocino, K.; Cappannoli, L.; Gulli, F.; Cianfrocca, C.; Di Stasio, E.; Biasucci, L.M. Free light chains a novel biomarker of cardiovascular disease. A pilot study. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 2563–2569. [Google Scholar] [CrossRef]
- Jackson, C.E.; Haig, C.; Welsh, P.; Dalzell, J.R.; Tsorlalis, I.K.; McConnachie, A.; Preiss, D.; McInnes, I.B.; Sattar, N.; Petrie, M.C.; et al. Combined Free Light Chains Are Novel Predictors of Prognosis in Heart Failure. JACC Heart Fail. 2015, 3, 618–625. [Google Scholar] [CrossRef]
- Perrone, M.A.; Pieri, M.; Marchei, M.; Sergi, D.; Bernardini, S.; Romeo, F. Serum free light chains in patients with ST elevation myocardial infarction (STEMI): A possible correlation with left ventricle dysfunction. Int. J. Cardiol. 2019, 292, 32–34. [Google Scholar] [CrossRef]
- Shantsila, E.; Wrigley, B.; Lip, G.Y.H. Free light chains in patients with acute heart failure secondary to atherosclerotic coronary artery disease. Am. J. Cardiol. 2014, 114, 1243–1248. [Google Scholar] [CrossRef]
- Goldblatt, F.; O′Neill, S.G. Clinical aspects of autoimmune rheumatic diseases. Lancet 2013, 382, 797–808. [Google Scholar] [CrossRef]
- Gottenberg, J.-E.; Aucouturier, F.; Goetz, J.; Sordet, C.; Jahn, I.; Busson, M.; Cayuela, J.-M.; Sibilia, J.; Mariette, X. Serum immunoglobulin free light chain assessment in rheumatoid arthritis and primary Sjogren’s syndrome. Ann. Rheum. Dis. 2007, 66, 23–27. [Google Scholar] [CrossRef]
- Ye, Y.; Li, S.-L.; Xie, M.; Jiang, P.; Liu, K.-G.; Li, Y.-J. Judging disease activity in rheumatoid arthritis by serum free kappa and lambda light chain levels. Kaohsiung J. Med Sci. 2013, 29, 547–553. [Google Scholar] [CrossRef]
- Gulli, F.; Napodano, C.; Marino, M.; Ciasca, G.; Pocino, K.; Basile, V.; Visentini, M.; Stefanile, A.; Todi, L.; De Spirito, M.; et al. Serum immunoglobulin free light chain levels in systemic autoimmune rheumatic diseases. Clin. Exp. Immunol. 2020, 199, 163–171. [Google Scholar] [CrossRef]
- Kormelink, T.G.; Tekstra, J.; Thurlings, R.M.; Boumans, M.H.J.; Vos, K.; Tak, P.P.; Bijlsma, J.W.J.; Lafeber, F.P.J.G.; Redegeld, F.A.; van Roon, J.A.G. Decrease in immunoglobulin free light chains in patients with rheumatoid arthritis upon rituximab (anti-CD20) treatment correlates with decrease in disease activity. Ann. Rheum. Dis. 2010, 69, 2137–2144. [Google Scholar] [CrossRef] [PubMed]
- Verstappen, G.M.; Moerman, R.V.; Van Nimwegen, J.F.; Van Ginkel, M.S.; Bijzet, J.; Mossel, E.; Vissink, A.; Hazenberg, B.P.C.; Arends, S.; Kroese, F.G.M.; et al. Serum immunoglobulin free light chains are sensitive biomarkers for monitoring disease activity and treatment response in primary Sjögren’s syndrome. Rheumatology 2018, 57, 1812–1821. [Google Scholar] [CrossRef] [PubMed]
- Konen, F.F.; Seeliger, T.; Schwenkenbecher, P.; Gingele, S.; Jendretzky, K.F.; Sühs, K.-W.; Ernst, D.; Witte, T.; Skripuletz, T. Saliva Free Light Chains in Patients with Neuro-Sjögren. Biomedicines 2022, 10, 2470. [Google Scholar] [CrossRef] [PubMed]
- Chiche, L.; Cournac, J.; Mancini, J.; Bardin, N.; Thomas, G.; Jean, R.; Schleinitz, N.; Kaplanski, G.; Durand, J.; Boucraut, J.; et al. Normalization of serum-free light chains in patients with systemic lupus erythematosus upon rituximab treatment and correlation with biological disease activity. Clin. Rheumatol. 2011, 30, 685–689. [Google Scholar] [CrossRef]
- Rodríguez-Cambrón, A.B.; Jiménez-Jiménez, J.; Blázquez-Cañamero, M.; Pazos, F.R.; Macía-Villa, C.; Alcalde-Villar, M.; Collado-Ramos, P.; Del Pozo, F.M.C.; Álvarez-Andrés, E.; Cruz-Valenciano, A. Determination of serum free light chains as a marker of systemic lupus flare. Clin. Rheumatol. 2020, 39, 449–454. [Google Scholar] [CrossRef]
- Bettacchioli, E.; Le Gaffric, C.; Mazeas, M.; Borghi, M.O.; Frostegard, J.; Barturen, G.; Makowska, Z.; Babei, S.; Lesche, R.; Meroni, P.L.; et al. An elevated polyclonal free light chain level reflects a strong interferon signature in patients with systemic autoimmune diseases. J. Transl. Autoimmun. 2021, 4, 100090. [Google Scholar] [CrossRef]
- Draborg, A.H.; Lydolph, M.C.; Westergaard, M.; Larsen, S.O.; Nielsen, C.T.; Duus, K.; Jacobsen, S.; Houen, G. Elevated Concentrations of Serum Immunoglobulin Free Light Chains in Systemic Lupus Erythematosus Patients in Relation to Disease Activity, Inflammatory Status, B Cell Activity and Epstein-Barr Virus Antibodies. PLoS ONE 2015, 10, e0138753. [Google Scholar] [CrossRef]
- Jolly, M.; Francis, S.; Aggarwal, R.; Mikolaitis, R.; Niewold, T.; Chubinskaya, S.; Block, J.; Scanzello, C.; Sequeira, W. Serum free light chains, interferon-alpha, and interleukins in systemic lupus erythematosus. Lupus 2014, 23, 881–888. [Google Scholar] [CrossRef]
- Diakos, C.I.; Charles, K.A.; McMillan, D.C.; Clarke, S.J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014, 15, e493–e503. [Google Scholar] [CrossRef]
- Kormelink, T.G.; Pardo, A.; Knipping, K.; Buendía-Roldán, I.; de Alba, C.G.; Blokhuis, B.R.; Selman, M.; Redegeld, F.A. Immunoglobulin free light chains are increased in hypersensitivity pneumonitis and idiopathic pulmonary fibrosis. PLoS ONE 2011, 6, e25392. [Google Scholar] [CrossRef]
- Groot Kormelink, T.; Powe, D.G.; Kuijpers, S.A.; Abudukelimu, A.; Fens, M.H.; Pieters, E.H.; Kassing van der Ven, W.W.; Habashy, H.O.; Ellis, I.O.; Blokhuis, B.R.; et al. Immunoglobulin free light chains are biomarkers of poor prognosis in basal-like breast cancer and are potential targets in tumor-associated inflammation. Oncotarget 2014, 5, 3159–3167. [Google Scholar] [CrossRef] [PubMed]
- Whiteside, T.L.; Ferrone, S. For breast cancer prognosis, immunoglobulin kappa chain surfaces to the top. Clin. Cancer Res. 2012, 18, 2417–2419. [Google Scholar] [CrossRef]
- Mastroianni, A.; Panella, R.; Morelli, D. Differential diagnosis between bone relapse of breast cancer and lambda light chain multiple myeloma: Role of the clinical biochemist. Tumori J. 2019, 105, NP17–NP19. [Google Scholar] [CrossRef]
- Ma, J.; Jiang, D.; Gong, X.; Shao, W.; Zhu, Z.; Xu, W.; Qiu, X. Free immunoglobulin light chain (FLC) promotes murine colitis and colitis-associated colon carcinogenesis by activating the inflammasome. Sci. Rep. 2017, 7, 5165. [Google Scholar] [CrossRef]
- Rijnierse, A.; Redegeld, F.A.; Blokhuis, B.R.; Van der Heijden, M.W.; Velde, A.A.T.; Pronk, I.; Hommes, D.W.; Nijkamp, F.P.; Koster, A.S.; Kraneveld, A.D. Ig-free light chains play a crucial role in murine mast cell-dependent colitis and are associated with human inflammatory bowel diseases. J. Immunol. 2010, 185, 653–659. [Google Scholar] [CrossRef]
- Wang, Q.; Jiang, D.; Ye, Q.; Zhou, W.; Ma, J.; Wang, C.; Geng, Z.; Chu, M.; Zheng, J.; Chen, H.; et al. A widely expressed free immunoglobulin κ chain with a unique Vκ4-1/Jκ3 pattern promotes colon cancer invasion and metastasis by activating the integrin β1/FAK pathway. Cancer Lett. 2022, 540, 215720. [Google Scholar] [CrossRef]
| Disease | Level of FLCs | Application | References |
|---|---|---|---|
| Monoclonal gammopathies | ↑ in serum, urine abnormal ratio |
| [4,25,26,27,28,29] |
| Multiple sclerosis | ↑ in serum, CSF ↑ values of κFLC index and λFLC index |
| [31,32,33,34,35,36,37,38,39] |
| SARS-CoV-2 infection | ↑ in serum abnormal ratio |
| [43,44] |
| HCV | ↑ in serum abnormal ratio |
| [45,46,47,48,49,50,51,52] |
| HBV | ↑ in serum |
| [53] |
| HIV | ↑ in serum, CSF |
| [56,57,58,59,60,61,62,63] |
| Lyme disease | ↑ in serum, CSF ↑ values of κFLC index and λFLC index |
| [64] |
| Tick-borne encephalitis | ↑ λFLCs in serum (pre-treatment) ↑ λFLCs in CSF (post-treatment) |
| [65] |
| Diabetes | ↓ κFLCs in serum and ratio in T2B ↑ in serum |
| [68,69,70,71,72] |
| Cardiovascular disorders | ↑ in serum |
| [19,20,21,73,74,75,76] |
| Rheumatoid arthritis | ↑ in serum |
| [78,79,80,81] |
| Sjogren’s syndrome | ↑ in serum abnormal ratio |
| [82,83,86] |
| Systemic lupus erythematosus | ↑ λFLCs |
| [63,84,87] |
| Lung cancer | ↑ in serum and bronchoalveolar fluid ↑ expression |
| [90] |
| Breast cancer |
| [91,93] | |
| Bowel diseases | ↑ in serum ↑ expression |
| [95,96] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gudowska-Sawczuk, M.; Mroczko, B. Free Light Chains κ and λ as New Biomarkers of Selected Diseases. Int. J. Mol. Sci. 2023, 24, 9531. https://doi.org/10.3390/ijms24119531
Gudowska-Sawczuk M, Mroczko B. Free Light Chains κ and λ as New Biomarkers of Selected Diseases. International Journal of Molecular Sciences. 2023; 24(11):9531. https://doi.org/10.3390/ijms24119531
Chicago/Turabian StyleGudowska-Sawczuk, Monika, and Barbara Mroczko. 2023. "Free Light Chains κ and λ as New Biomarkers of Selected Diseases" International Journal of Molecular Sciences 24, no. 11: 9531. https://doi.org/10.3390/ijms24119531







