Luteolin Enhances Transepithelial Sodium Transport in the Lung Alveolar Model: Integrating Network Pharmacology and Mechanism Study
Abstract
1. Introduction
2. Results
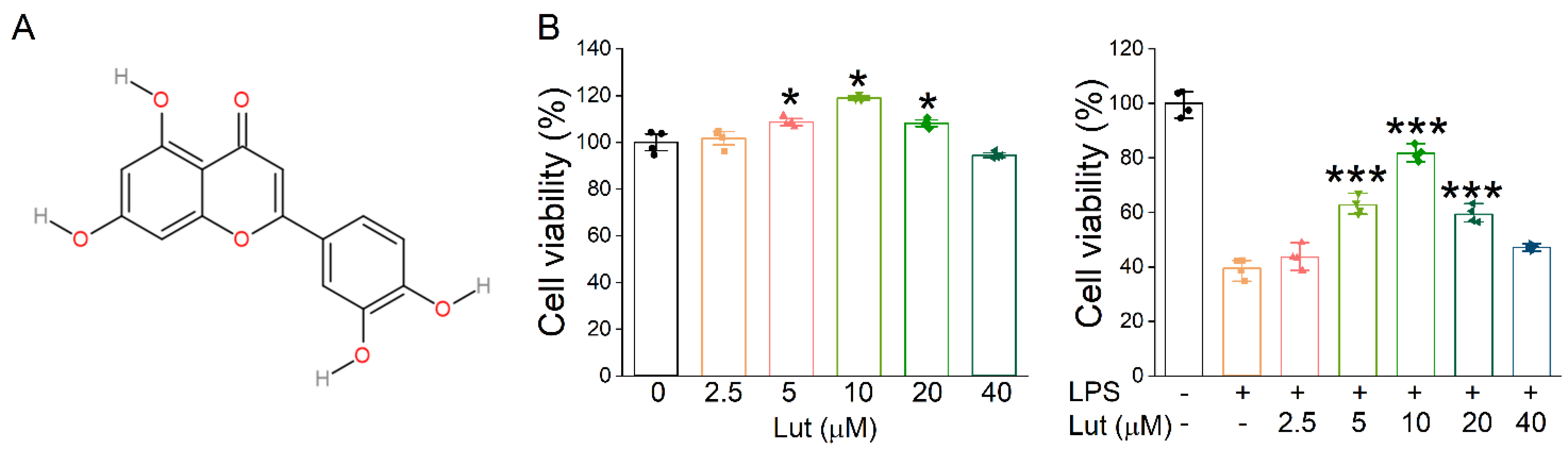
2.1. Lut Increased the Expression Level of ENaC in Primary AT2 Cells
2.2. Lut Suppressed Inflammatory Pulmonary Edema in ALI Mice
2.3. Establishment of the 3D Alveolar Epithelial Organoids
2.4. Lut Elevated the Expression of ENaC in the Lung Alveolar Model
2.5. Target Identification and Protein–Protein Interaction Analysis
2.6. Screening of the Hub Genes and Clusters in the PPI Network
2.7. Prediction of the Potential Signaling Pathways of Lut for ALI Treatment
2.8. Binding Activities of Lut to the JAK/STAT Pathway
2.9. Validation of the Pathways and Targets
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Animals
4.3. Primary Mouse AT2 Cell Culture and Cell Viability Analysis
4.4. Establishment of the ALI Mouse Model
4.5. Preparation for 3D Organoid Culture
4.6. Identification of 3D Alveolar Epithelial Organoid
4.7. Determination of Lung Wet/Dry Weight Ratio
4.8. Bronchoalveolar Lavage Fluid Analysis
4.9. Histological Studies
4.10. Real-Time PCR
4.11. Immunofluorescence Assay
4.12. Target Prediction
4.13. Constructing Protein–Protein Interaction Networks
4.14. Pathway Enrichment Analysis
4.15. Molecular Docking Analysis
4.16. Western Blot Assay
4.17. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xie, X.; Yu, T.; Hou, Y.; Han, A.; Ding, Y.; Nie, H.; Cui, Y. Ferulic acid ameliorates lipopolysaccharide-induced tracheal injury via cGMP/PKGII signaling pathway. Respir. Res. 2021, 22, 308. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xia, M.; Xu, J.; Huang, Q.; Dai, Z.; Zhang, X. Dexmedetomidine alleviates pulmonary edema through the epithelial sodium channel (ENaC) via the PI3K/Akt/Nedd4-2 pathway in LPS-induced acute lung injury. Immunol. Res. 2021, 69, 162–175. [Google Scholar] [CrossRef] [PubMed]
- Guillot, L.; Nathan, N.; Tabary, O.; Thouvenin, G.; Le Rouzic, P.; Corvol, H.; Amselem, S.; Clement, A. Alveolar epithelial cells: Master regulators of lung homeostasis. Int. J. Biochem. Cell Biol. 2013, 45, 2568–2573. [Google Scholar] [CrossRef] [PubMed]
- Ruaro, B.; Salton, F. The history and mystery of alveolar epithelial type II cells: Focus on their physiologic and pathologic role in lung. Int. J. Mol. Sci. 2021, 22, 2566–2582. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Song, H. Regulation of alveolar type 2 stem/progenitor cells in lung injury and regeneration. Acta Biochim. Biophys. Sin. 2020, 52, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Yu, T.; Hua, Y.; Hou, Y.; Ding, Y.; Nie, H. Effects of hypoxia on respiratory diseases: Perspective view of epithelial ion transport. Am. J. Physiol. Lung Cell. Mol. Physiol. 2022, 323, L240–L250. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Zhong, W.; Lin, Z.; Yan, J. Blockade of Indoleamine 2,3-Dioxygenase attenuates lipopolysaccharide-induced kidney injury by inhibiting TLR4/NF-κB signaling. Clin. Exp. Nephrol. 2023, 27, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.; Yang, F.; Qiu, C.; Yang, Y.; Lan, C. Rosmarinic acid protects against lipopolysaccharide-induced cardiac dysfunction via activating Sirt1/PGC-1α pathway to alleviate mitochondrial impairment. Clin. Exp. Pharmacol. Physiol. 2023, 50, 218–227. [Google Scholar] [CrossRef]
- Yang, T.; Zhao, S.; Sun, N.; Zhao, Y.; Wang, H.; Zhang, Y.; Hou, X.; Tang, Y.; Gao, X.; Fan, H. Network pharmacology and in vivo studies reveal the pharmacological effects and molecular mechanisms of Celastrol against acute hepatic injury induced by LPS. Int. Immunopharmacol. 2023, 117, 109898. [Google Scholar] [CrossRef]
- Zhang, H.; Cui, Y.; Zhou, Z.; Ding, Y.; Nie, H. Alveolar type 2 epithelial cells as potential therapeutics for acute lung injury/acute respiratory distress syndrome. Curr. Pharm. Des. 2019, 25, 4877–4882. [Google Scholar] [CrossRef]
- Zhang, M.; Ali, G.; Komatsu, S.; Zhao, R.; Ji, H.L. Prkg2 regulates alveolar type 2-mediated re-alveolarization. Stem Cell Res. Ther. 2022, 13, 111. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wu, Q.; Sun, X.; Shen, J.; Chen, H.Y. Organoids as a powerful model for respiratory diseases. Stem Cells Int. 2020, 2020, 5847876. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.M. Ethnomedicinal, phytochemical and pharmacological investigations of Perilla frutescens (L.) britt. Molecules 2018, 24, 102. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Qiu, J.F.; Ma, L.J.; Hu, Y.J.; Li, P.; Wan, J.B. Phytochemical and phytopharmacological review of Perilla frutescens L. (Labiatae), a traditional edible-medicinal herb in China. Food Chem. Toxicol. 2017, 108, 375–391. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Xu, X.; Lv, J.; Huang, J.; Lyu, L.; Liu, L. Potential mechanisms of perillae folium against COVID-19: A network pharmacology approach. J. Med. Food 2023. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; He, L.; Liu, J.; Zhou, L. Luteolin attenuates diabetic nephropathy through suppressing inflammatory response and oxidative stress by inhibiting STAT3 pathway. Exp. Clin. Endocrinol. Diabetes 2021, 129, 729–739. [Google Scholar] [CrossRef]
- Imran, M.; Rauf, A.; Abu-Izneid, T.; Nadeem, M.; Shariati, M.A.; Khan, I.A.; Imran, A.; Orhan, I.E.; Rizwan, M.; Atif, M.; et al. Luteolin, a flavonoid, as an anticancer agent: A review. Biomed. Pharmacother. 2019, 112, 108612–108621. [Google Scholar] [CrossRef]
- Ganai, S.A.; Sheikh, F.A.; Baba, Z.A.; Mir, M.A.; Mantoo, M.A.; Yatoo, M.A. Anticancer activity of the plant flavonoid luteolin against preclinical models of various cancers and insights on different signalling mechanisms modulated. Phytother. Res. 2021, 35, 3509–3532. [Google Scholar] [CrossRef]
- Park, E.J.; Kim, Y.M.; Kim, H.J.; Chang, K.C. Luteolin activates ERK1/2− and Ca2+-dependent HO−1 induction that reduces LPS-induced HMGB1, iNOS/NO, and COX−2 expression in RAW264.7 cells and mitigates acute lung injury of endotoxin mice. Inflamm. Res. 2018, 67, 445–453. [Google Scholar] [CrossRef]
- Xie, K.; Chai, Y.S.; Lin, S.H. Luteolin regulates the differentiation of regulatory T cells and activates IL-10 dependent macrophage polarization against acute lung injury. J. Immunol. Res. 2021, 2021, 8883962. [Google Scholar] [CrossRef]
- Hou, Y.; Li, J.; Ding, Y.; Cui, Y.; Nie, H. Luteolin attenuates lipopolysaccharide-induced acute lung injury/acute respiratory distress syndrome by activating alveolar epithelial sodium channels via cGMP/PI3K pathway. J. Ethnopharmacol. 2022, 282, 114654. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Yang, H.; Wei, J.; Li, W.; Yue, F.; Song, Y.; He, X.; Hu, K. Mechanisms underlying the effects of Lianhua Qingwen on sepsis-induced acute lung injury: A network pharmacology approach. Front. Pharmacol. 2021, 12, 717652. [Google Scholar] [CrossRef] [PubMed]
- Djeujo, F.M.; Stablum, V.; Pangrazzi, E.; Ragazzi, E. Luteolin and vernodalol as bioactive compounds of leaf and root vernonia amygdalina extracts: Effects on α-glucosidase, glycation, ROS, cell Viability, and in silico ADMET parameters. Pharmaceutics 2023, 15, 1541. [Google Scholar] [CrossRef] [PubMed]
- Mu, M.; Gao, P.; Yang, Q.; He, J.; Wu, F.; Han, X.; Guo, S.; Qian, Z.; Song, C. Alveolar epithelial cells promote IGF-1 production by alveolar macrophages through TGF-β to suppress endogenous inflammatory signals. Front. Immunol. 2020, 11, 1585–1598. [Google Scholar] [CrossRef]
- Gong, T.; Zhang, X.; Peng, Z.; Ye, Y.; Liu, R. Macrophage-derived exosomal aminopeptidase N aggravates sepsis-induced acute lung injury by regulating necroptosis of lung epithelial cell. Commun. Biol. 2022, 5, 543. [Google Scholar] [CrossRef]
- Li, J.; Bai, Y.; Tang, Y.; Wang, X.; Cavagnaro, M.J.; Li, L.; Li, Z.; Zhang, Y.; Shi, J. A 4-benzene-Indol derivative alleviates LPS-induced acute lung injury through inhibiting the NLRP3 inflammasome. Front. Immunol. 2022, 13, 812164. [Google Scholar] [CrossRef]
- Moore, P.J.; Tarran, R. The epithelial sodium channel as a therapeutic target for cystic fibrosis lung disease. Expert. Opin. Ther. Targets 2018, 22, 687–701. [Google Scholar] [CrossRef]
- Yang, Q.; Xu, H.R.; Xiang, S.Y.; Zhang, C.; Ye, Y.; Shen, C.X.; Mei, H.X.; Zhang, P.H.; Ma, H.Y.; Zheng, S.X.; et al. Resolvin conjugates in tissue regeneration 1 promote alveolar fluid clearance by activating alveolar epithelial sodium channels and Na, K-ATPase in lipopolysaccharide-induced acute lung injury. J. Pharmacol. Exp. Ther. 2021, 379, 156–165. [Google Scholar] [CrossRef]
- Han, J.; Li, H.; Bhandari, S.; Cao, F.; Wang, X.Y.; Tian, C.; Li, X.Y.; Zhang, P.H.; Liu, Y.J.; Wu, C.H.; et al. Maresin conjugates in tissue regeneration 1 improves alveolar fluid clearance by up-regulating alveolar ENaC, Na, K-ATPase in lipopolysaccharide-induced acute lung injury. J. Cell. Mol. Med. 2020, 24, 4736–4747. [Google Scholar] [CrossRef]
- Deng, W.; Qi, D.; Tang, X.M.; Deng, X.Y.; He, J.; Wang, D.X. The WNK4/SPAK pathway stimulates alveolar fluid clearance by up-regulation of epithelial sodium channel in mice with lipopolysaccharide-induced acute respiratory distress syndrome. Shock 2022, 58, 68–77. [Google Scholar] [CrossRef]
- Hua, Y.; Han, A.; Yu, T.; Hou, Y.; Ding, Y.; Nie, H. Small extracellular vesicles containing miR-34c derived from bone marrow mesenchymal stem cells regulates epithelial sodium channel via targeting MARCKS. Int. J. Mol. Sci. 2022, 23, 5196. [Google Scholar] [CrossRef] [PubMed]
- Lamers, M.M.; van der Vaart, J. An organoid-derived bronchioalveolar model for SARS-CoV-2 infection of human alveolar type II-like cells. EMBO J. 2021, 40, e105912. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.M.; Ji, R.; Chen, W.W.; Huang, S.W.; Zheng, Y.J.; Yang, Z.T. Paclitaxel alleviated sepsis-induced acute lung injury by activating MUC1 and suppressing TLR-4/NF-κB pathway. Drug. Des. Devel Ther. 2019, 13, 3391–3404. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, G.; Zhang, L.; Li, Y.; Zhao, Z. G9a promotes inflammation in Streptococcus pneumoniae induced pneumonia mice by stimulating M1 macrophage polarization and H3K9me2 methylation in FOXP1 promoter region. Ann. Transl. Med. 2022, 10, 583. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, L.; Althaus, M. Evolution of epithelial sodium channels: Current concepts and hypotheses. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2020, 319, R387–R400. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Wang, Y.; Lu, A.; Zhang, G. Systems pharmacology in small molecular drug discovery. Int. J. Mol. Sci. 2016, 17, 246. [Google Scholar] [CrossRef]
- Wang, Z.Y.; Li, M.Z.; Li, W.J.; Ouyang, J.F.; Gou, X.J.; Huang, Y. Mechanism of action of Daqinjiao decoction in treating cerebral small vessel disease explored using network pharmacology and molecular docking technology. Phytomedicine 2023, 108, 154538. [Google Scholar] [CrossRef]
- Zhu, W.; Li, Y.; Zhao, J.; Wang, Y.; Li, Y.; Wang, Y. The mechanism of triptolide in the treatment of connective tissue disease-related interstitial lung disease based on network pharmacology and molecular docking. Ann. Med. 2022, 54, 541–552. [Google Scholar] [CrossRef]
- Zhao, X.; Zhao, B.; Zhao, Y.; Zhang, Y.; Qian, M. Protective effect of anisodamine on bleomycin-induced acute lung injury in immature rats via modulating oxidative stress, inflammation, and cell apoptosis by inhibiting the JAK2/STAT3 pathway. Ann. Transl. Med. 2021, 9, 859. [Google Scholar] [CrossRef]
- Zhang, H.; Ding, Y.; Hou, Y.; Liu, Y.; Zhou, Z.; Nie, H. Bone marrow mesenchymal stem cells derived miRNA-130b enhances epithelial sodium channel by targeting PTEN. Respir. Res. 2020, 21, 329–343. [Google Scholar] [CrossRef]
- Liu, H.; Hou, Y.; Jin, R.; Zhou, Z.; Zhang, H.; Wang, L.; Ding, Y.; Nie, H. Luteolin affects lung epithelial ion transport by regulating epithelial sodium channels. Tradit. Chin. Drug Res. Clin. Pharmacol. 2020, 31, 402–408. [Google Scholar] [CrossRef]
- Kuo, M.Y.; Liao, M.F.; Chen, F.L.; Li, Y.C.; Yang, M.L.; Lin, R.H.; Kuan, Y.H. Luteolin attenuates the pulmonary inflammatory response involves abilities of antioxidation and inhibition of MAPK and NFκB pathways in mice with endotoxin-induced acute lung injury. Food Chem. Toxicol. 2011, 49, 2660–2666. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Hou, Y.; Liu, Y.; Yu, T.; Cui, Y.; Nie, H. MiR-130a-3p alleviates inflammatory and fibrotic phases of pulmonary fibrosis through proinflammatory factor TNF-α and profibrogenic receptor TGF-βRII. Front. Pharmacol. 2022, 13, 863646. [Google Scholar] [CrossRef]
- Hu, A.; Chen, W.; Wu, S.; Pan, B.; Zhu, A.; Yu, X.; Huang, Y. An animal model of transfusion-related acute lung injury and the role of soluble CD40 ligand. Vox Sang. 2020, 115, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Liu, T.; Duan, J.X.; Li, P.; Sun, G.Y.; Liu, Y.P.; Zhang, J.; Dong, L.; Lee, K.S.S.; Hammock, B.D.; et al. Soluble epoxide hydrolase inhibitor attenuates lipopolysaccharide-induced acute lung injury and improves survival in mice. Shock 2017, 47, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, H.; Fang, F.; Fang, C. Danggui buxue tang ameliorates bleomycin-induced pulmonary fibrosis by suppressing the TLR4/NLRP3 signaling pathway in rats. Evid. Based Complement. Altern. Med. 2021, 2021, 8030143. [Google Scholar] [CrossRef] [PubMed]








| Antibody | Manufacture | WB | IF | FCM |
|---|---|---|---|---|
| SP-C | Bioss (Beijing, China) | 1:100 | 1:100 | |
| PDPN | Santa Cruz (Dallas, TX, USA) | 1:100 | ||
| p-STAT3 | Affinity (Cincinnati, OH, USA) | 1:1000 | ||
| p-JAK2 | Affinity (Cincinnati, OH, USA) | 1:1000 | ||
| STAT3 | Affinity (Cincinnati, OH, USA) | 1:1000 | ||
| JAK2 | Affinity (Cincinnati, OH, USA) | 1:1000 | ||
| SOCS3 | Affinity (Cincinnati, OH, USA) | 1:1000 | ||
| α-ENaC | Santa Cruz (Dallas, TX, USA) | 1:2000 | 1:200 | |
| γ-ENaC | Santa Cruz (Dallas, TX, USA) | 1:2000 | 1:200 | |
| β-actin | Santa Cruz (Dallas, TX, USA) | 1:1000 | ||
| goat anti-mouse | ZSGB-BIO (Beijing, China) | 1:5000 | ||
| goat anti-rabbit | ZSGB-BIO (Beijing, China) | 1:5000 | ||
| FITC goat anti-rabbit | ZSGB-BIO (Beijing, China) | 1:100 | 1:200 | |
| TRITC goat anti-mouse | ZSGB-BIO (Beijing, China) | 1:100 |
| Primer Name | Forward (5′–3′) | Reverse (5′–3′) |
|---|---|---|
| α-ENaC | AAC AAA TCG GACTGC TTC TAC | AGC CAC CAT CAT CCA TAA A |
| β-ENaC | GGG ACC AAA GCA CCA AT | CAG ACG CAG GGA GTC ATAG |
| γ-ENaC | GCACCG TTC GCC ACC TTC TA | AGG TCA CCA GCA GCT CCT CA |
| IL-1β | AGA AGC TGT GGC AGC TAC CTG | GGA AAA GAA GGT GCT CAT GTC C |
| IL-6 | GCT ACC AAA CTG GAT ATA ATC AGG A | CCA GGT AGC TAT GGT ACT CCA GAA |
| TNF-α | TCT TCT CAT TCC TGC TTG TGG | GGT CTG GGG CCA TAG AAC TGA |
| GAPDH | AGA AGG CTG GGG CTC ATT TG | AGG GGC CAT CCA CAG TCT TC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, L.; Yu, T.; Zhai, Y.; Nie, H.; Li, X.; Ding, Y. Luteolin Enhances Transepithelial Sodium Transport in the Lung Alveolar Model: Integrating Network Pharmacology and Mechanism Study. Int. J. Mol. Sci. 2023, 24, 10122. https://doi.org/10.3390/ijms241210122
Chen L, Yu T, Zhai Y, Nie H, Li X, Ding Y. Luteolin Enhances Transepithelial Sodium Transport in the Lung Alveolar Model: Integrating Network Pharmacology and Mechanism Study. International Journal of Molecular Sciences. 2023; 24(12):10122. https://doi.org/10.3390/ijms241210122
Chicago/Turabian StyleChen, Lei, Tong Yu, Yiman Zhai, Hongguang Nie, Xin Li, and Yan Ding. 2023. "Luteolin Enhances Transepithelial Sodium Transport in the Lung Alveolar Model: Integrating Network Pharmacology and Mechanism Study" International Journal of Molecular Sciences 24, no. 12: 10122. https://doi.org/10.3390/ijms241210122
APA StyleChen, L., Yu, T., Zhai, Y., Nie, H., Li, X., & Ding, Y. (2023). Luteolin Enhances Transepithelial Sodium Transport in the Lung Alveolar Model: Integrating Network Pharmacology and Mechanism Study. International Journal of Molecular Sciences, 24(12), 10122. https://doi.org/10.3390/ijms241210122





