Investigating the Efficacy of Saccharomyces boulardii in Metabolic Syndrome Treatment: A Narrative Review of What Is Known So Far
Abstract
:1. Introduction
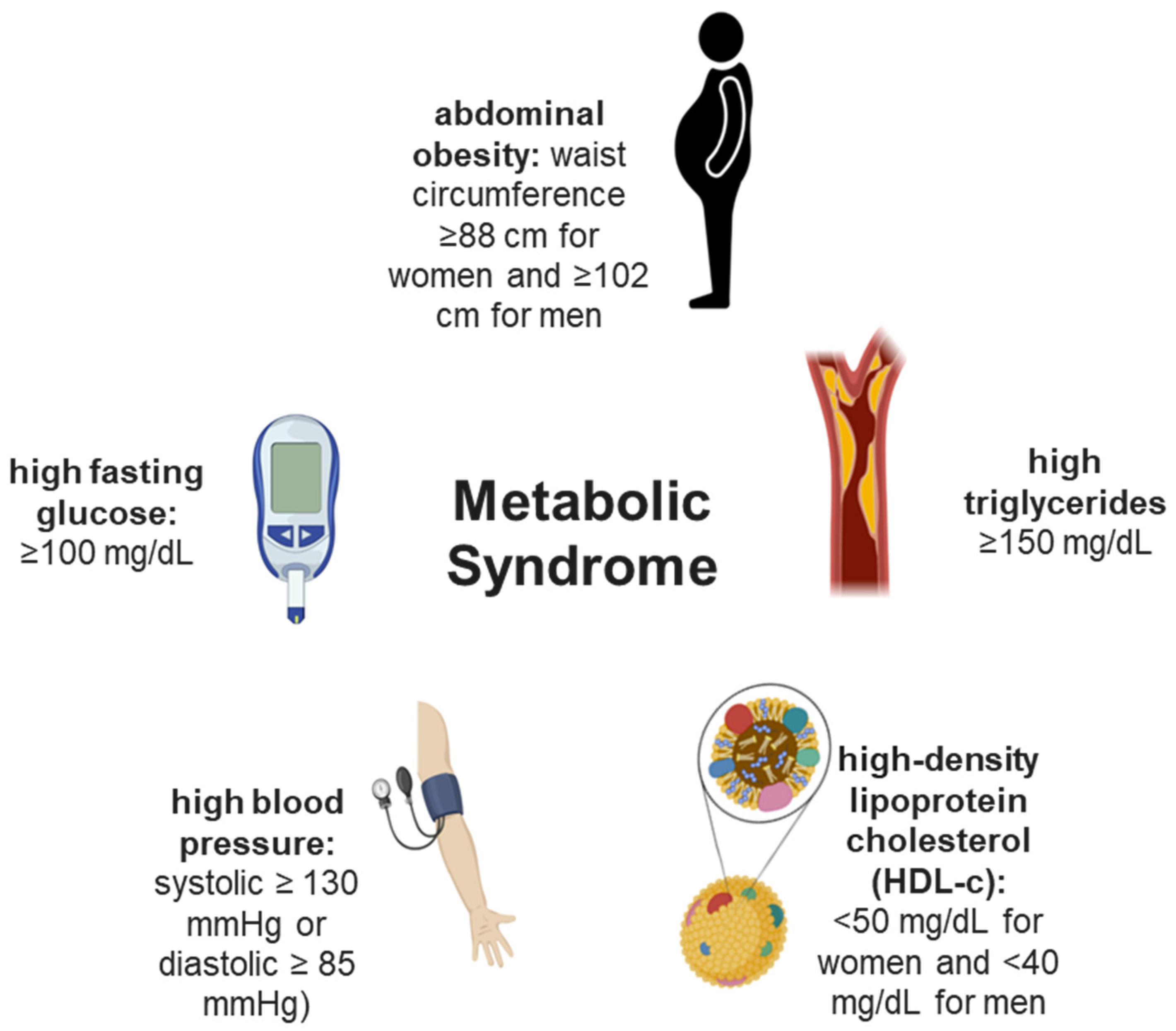
2. Metabolic Syndrome and Its Risk Factors
3. Probiotics
3.1. Saccharomyces boulardii
3.2. Understanding Possible Actions of Saccharomyces boulardii in Metabolic Syndrome and Its Risk Factors
4. Conclusions
5. Limitations of Our Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fahed, G.; Aoun, L.; Zerdan, M.B.; Allam, S.; Zerdan, M.B.; Bouferraa, Y.; Assi, H.I. Metabolic syndrome: Updates on pathophysiology and management in 2021. Int. J. Mol. Sci. 2022, 23, 786. [Google Scholar] [CrossRef]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G. Metabolic syndrome: Definitions and controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef] [Green Version]
- WHO (World Health Organization). Obesity and Overweight. 2016. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 9 December 2022).
- WHO. Raised Cholesterol. 2019. Available online: https://www.who.int/gho/ncd/riskfactors/cholesteroltext/en/ (accessed on 17 December 2022).
- WHO (World Health Organization). Hypertension. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 12 December 2022).
- Al-Zahrani, J.; Shubair, M.M.; Al-Ghamdi, S.; Alrasheed, A.A.; Alduraywish, A.A.; Alreshidi, F.S.; Alshahrani, S.M.; Alsalamah, M.; Al-Khateeb, B.F.; Ashathri, A.I.; et al. The prevalence of hypercholesterolemia and associated risk factors in Al-Kharj population, Saudi Arabia: A cross-sectional survey. BMC Cardiovasc. Disord 2021, 21, 22. [Google Scholar] [CrossRef]
- Upala, P.; Apidechkul, T.; Wongfu, C.; Khunthason, S.; Kullawong, N.; Keawdounglek, V.; Chomchoei, C.; Yeemard, F.; Tamornpark, R. Factors associated with hypertriglyceridemia among the hill tribe people aged 30 years and over, Thailand: A cross-sectional study. BMC Public Health 2021, 21, 581. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Ferran, M.; de la Guía-Galipienso, F.; Sanchis-Gomar, F.; Pareja-Galeano, H. Metabolic impacts of confinement during the COVID-19 pandemic due to modified diet and physical activity habits. Nutrients 2020, 12, 1549. [Google Scholar] [CrossRef] [PubMed]
- Corb Aron, R.A.; Abid, A.; Vesa, C.M.; Nechifor, A.C.; Behl, T.; Ghitea, T.C.; Munteanu, M.A.; Fratila, O.; Andronie-Cioara, F.L.; Toma, M.M.; et al. Recognizing the benefits of pre-/probiotics in metabolic syndrome and type 2 diabetes mellitus considering the influence of akkermansia muciniphila as a key gut bacterium. Microorganisms 2021, 9, 618. [Google Scholar] [CrossRef]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liong, M.-T. Probiotics: Biology, Genetics and Health Aspects; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Sirchak, Y.S.; Patskun, S.V.; Bedey, N.V. Dynamics of gastrin level in patients with diabetes Mellitus 2 type and chronic gastritis after Helicobateer pylori eradication therapy. Wiad. Lek. 2020, 73, 2512–2514. [Google Scholar] [CrossRef] [PubMed]
- Bohora, A.A.; Kokate, S.R.; Khedkar, S.; Vankudre, A. Antimicrobial activity of probiotics against endodontic pathogens: A preliminary study. Indian J. Med. Microbiol. 2019, 37, 5–11. [Google Scholar] [CrossRef] [PubMed]
- McFarland, L. Common organisms and probiotics: Saccharomyces boulardii. In The Microbiota in Gastrointestinal Pathophysiology; Elsevier: Amsterdam, The Netherlands, 2017; pp. 145–164. [Google Scholar]
- Samah, S.; Ramasamy, K.; Lim, S.M.; Neoh, C.F. Probiotics for the management of type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Res. Clin. Pract 2016, 118, 172–182. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, L.; Guo, C.; Mu, D.; Feng, B.; Zuo, X.; Li, Y. Effects of probiotic type, dose and treatment duration on irritable bowel syndrome diagnosed by Rome III criteria: A meta-analysis. BMC Gastroenterol. 2016, 16, 62. [Google Scholar] [CrossRef] [Green Version]
- Tenorio-Jiménez, C.; Martínez-Ramírez, M.J.; Gil, Á.; Gómez-Llorente, C. Effects of probiotics on metabolic syndrome: A systematic review of randomized clinical trials. Nutrients 2020, 12, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McFarland, L.V.; Dublin, S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J. Gastroenterol. WJG 2008, 14, 2650. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Liu, J.; Wen, X.; Zhang, G.; Cai, J.; Qiao, Z.; An, Z.; Zheng, J.; Li, L. Unique Probiotic Properties and Bioactive Metabolites of Saccharomyces boulardii. Probiotics Antimicrob. Proteins 2022, 1–16. [Google Scholar] [CrossRef]
- Bagherpour, G.; Ghasemi, H.; Zand, B.; Zarei, N.; Roohvand, F.; Ardakani, E.M.; Azizi, M.; Khalaj, V. Oral administration of recombinant Saccharomyces boulardii expressing ovalbumin-CPE fusion protein induces antibody response in mice. Front. Microbiol. 2018, 9, 723. [Google Scholar] [CrossRef] [Green Version]
- Cleeman, J.I.; Lenfant, C. The national cholesterol education program: Progress and prospects. JAMA 1998, 280, 2099–2104. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, J.V.; Mark, H.E.; Anstee, Q.M.; Arab, J.P.; Batterham, R.L.; Castera, L.; Cortez-Pinto, H.; Crespo, J.; Cusi, K.; Dirac, M.A.; et al. Advancing the global public health agenda for NAFLD: A consensus statement. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 60–78. [Google Scholar] [CrossRef]
- de Carvalho Vidigal, F.; Ribeiro, A.Q.; Babio, N.; Salas-Salvadó, J.; Bressan, J. Prevalence of metabolic syndrome and pre-metabolic syndrome in health professionals: LATINMETS Brazil study. Diabetol. Metab. Syndr. 2015, 7, 6. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, J.B.; dos Santos, A.M.; Barbosa, M.M.; Barbosa, M.M.; de Carvalho, C.A.; Fonseca, P.C.; Fonseca, J.M.; Barbosa Mdo, C.; Bogea, E.G.; da Silva, A.A.M.; et al. Metabolic syndrome, insulin resistance and other cardiovascular risk factors in university students. Ciência Saúde Coletiva 2016, 21, 1123–1136. [Google Scholar] [CrossRef] [Green Version]
- Ramires, E.K.N.M.; Menezes, R.C.E.d.; Longo-Silva, G.; Santos, T.G.d.; Marinho, P.d.M.; Silveira, J.A.C.d. Prevalência e fatores associados com a Síndrome Metabólica na população adulta brasileira: Pesquisa nacional de saúde-2013. Arq. Bras. Cardiol. 2018, 110, 455–466. [Google Scholar] [PubMed]
- Yi, Y.; An, J. Sex differences in risk factors for metabolic syndrome in the Korean population. Int. J. Environ. Res. Public Health 2020, 17, 9513. [Google Scholar] [CrossRef]
- Mozumdar, A.; Liguori, G. Persistent increase of prevalence of metabolic syndrome among US adults: NHANES III to NHANES 1999–2006. Diabetes Care 2011, 34, 216–219. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.J.; Hwang, J.-Y.; Kim, H.; Park, S.; Kwon, O. Diet quality, physical activity, and their association with metabolic syndrome in Korean adults. Nutrition 2019, 59, 138–144. [Google Scholar] [CrossRef]
- Golbidi, S.; Mesdaghinia, A.; Laher, I. Exercise in the metabolic syndrome. Oxidative Med. Cell. Longev. 2012, 2012, 349710. [Google Scholar] [CrossRef] [Green Version]
- Soliman, S.F. Metabolic Syndrome: Impact of Dietary Therapy. In Cellular Metabolism and Related Disorders; IntechOpen: London, UK, 2020. [Google Scholar]
- Ejtahed, H.-S.; Angoorani, P.; Soroush, A.-R.; Atlasi, R.; Hasani-Ranjbar, S.; Mortazavian, A.M.; Larijani, B. Probiotics supplementation for the obesity management; A systematic review of animal studies and clinical trials. J. Funct. Foods 2019, 52, 228–242. [Google Scholar] [CrossRef]
- Godoy-Matos, A.; Júnior, W.; Valerio, C. NAFLD as a continuum: From obesity to metabolic syndrome and diabetes. Diabetol. Metab. Syndr. 2020, 12, 60. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Lee, S.-G.; Jee, S.H.; Kim, J.-H. Hypertriglyceridemia is a major factor associated with elevated levels of small dense LDL cholesterol in patients with metabolic syndrome. Ann. Lab. Med. 2015, 35, 586–594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chait, A.; Subramanian, S. Hypertriglyceridemia: Pathophysiology, Role of Genetics, Consequences, and Treatment. 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK326743/ (accessed on 17 December 2022).
- Yanai, H.; Tomono, Y.; Ito, K.; Furutani, N.; Yoshida, H.; Tada, N. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr. J. 2008, 7, 10. [Google Scholar] [CrossRef] [Green Version]
- WHO. Cardiovascular Diseases (CVDs). 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 15 December 2022).
- Berg, A.; Scherer, P. Adipose tissue, inflammation, and cardiovascular disease. Circ. Res. 2005, 96, 939–949. [Google Scholar] [CrossRef]
- Rochlani, Y.; Pothineni, N.V.; Kovelamudi, S.; Mehta, J.L. Metabolic syndrome: Pathophysiology, management, and modulation by natural compounds. Ther. Adv. Cardiovasc. Dis. 2017, 11, 215–225. [Google Scholar] [CrossRef] [Green Version]
- IDF. Diabetes Around the World in 2021. 2021. Available online: https://diabetesatlas.org/#:~:text=1%20in%208%20adults%20(206,caused%20by%20diabetes%20in%202021 (accessed on 11 December 2022).
- Pirola, L.; Ferraz, J. Role of pro-and anti-inflammatory phenomena in the physiopathology of type 2 diabetes and obesity. World J. Biol. Chem. 2017, 8, 120. [Google Scholar] [CrossRef] [PubMed]
- Emanuela, F.; Grazia, M.; Marco, D.R.; Maria Paola, L.; Giorgio, F.; Marco, B. Inflammation as a link between obesity and metabolic syndrome. J. Nutr. Metab. 2012, 2012, 476380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallappa, R.H.; Rokana, N.; Duary, R.K.; Panwar, H.; Batish, V.K.; Grover, S. Management of metabolic syndrome through probiotic and prebiotic interventions. Indian J. Endocrinol. Metab. 2012, 16, 20. [Google Scholar]
- Fujioka, K. Metabolic syndrome treatment strategies. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2006, 26, 222S–226S. [Google Scholar] [CrossRef] [PubMed]
- Lilly, D.M.; Stillwell, R.H. Probiotics: Growth-promoting factors produced by microorganisms. Science 1965, 147, 747–748. [Google Scholar] [CrossRef]
- WHO. Food and Agricultural Organization of the United Nations and World Health Organization. Health and Nutritional Properties of Probiotics in Food including Powder Milk with Live Lactic Acid Bacteria. 2001. Available online: http://www.who.int/foodsafety/publications/fs_management/en/probiotics.pdf (accessed on 10 December 2022).
- Andersson, H.; Asp, N.-G.; Bruce, Å.; Roos, S.; Wadström, T.; Wold, A.E. Health effects of probiotics and prebiotics A literature review on human studies. Näringsforskning 2001, 45, 58–75. [Google Scholar] [CrossRef]
- Zendeboodi, F.; Khorshidian, N.; Mortazavian, A.M.; da Cruz, A.G. Probiotic: Conceptualization from a new approach. Curr. Opin. Food Sci. 2020, 32, 103–123. [Google Scholar] [CrossRef]
- Lim, P.; Loke, C.; Ho, Y.; Tan, H. Cholesterol homeostasis associated with probiotic supplementation in vivo. J. Appl. Microbiol. 2020, 129, 1374–1388. [Google Scholar] [CrossRef]
- Galdeano, C.M.; Cazorla, S.I.; Dumit, J.M.L.; Vélez, E.; Perdigón, G. Beneficial effects of probiotic consumption on the immune system. Ann. Nutr. Metab. 2019, 74, 115–124. [Google Scholar]
- Mekonnen, S.A.; Merenstein, D.; Fraser, C.M.; Marco, M.L. Molecular mechanisms of probiotic prevention of antibiotic-associated diarrhea. Curr. Opin. Biotechnol. 2020, 61, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, S.A.; Gyawali, R.; Awaisheh, S.S.; Ayivi, R.D.; Silva, R.C.; Subedi, K.; Aljaloud, S.O.; Siddiqui, S.A.; Krastanov, A. Fermented foods and probiotics: An approach to lactose intolerance. J. Dairy Res. 2021, 88, 357–365. [Google Scholar] [CrossRef]
- Drago, L. Probiotics and colon cancer. Microorganisms 2019, 7, 66. [Google Scholar] [CrossRef] [Green Version]
- Pecora, F.; Persico, F.; Gismondi, P.; Fornaroli, F.; Iuliano, S.; de’Angelis, G.L.; Esposito, S. Gut microbiota in celiac disease: Is there any role for probiotics? Front. Immunol. 2020, 11, 957. [Google Scholar] [CrossRef]
- Dallal, M.M.S.; Yazdi, M.H.; Holakuyee, M.; Hassan, Z.M.; Abolhassani, M.; Mahdavi, M. Lactobacillus casei ssp. casei induced Th1 cytokine profile and natural killer cells activity in invasive ductal carcinoma bearing mice. Iran. J. Allergy Asthma Immunol. 2012, 11, 183–189. [Google Scholar]
- Blaak, E.E.; Canfora, E.E.; Theis, S.; Frost, G.; Groen, A.K.; Mithieux, G.; Nauta, A.; Scott, K.; Stahl, B.; Van Harsselaar, J.; et al. Short chain fatty acids in human gut and metabolic health. Benef. Microbes 2020, 11, 411–455. [Google Scholar] [CrossRef] [PubMed]
- Saad, N.; Delattre, C.; Urdaci, M.; Schmitter, J.-M.; Bressollier, P. An overview of the last advances in probiotic and prebiotic field. LWT-Food Sci. Technol. 2013, 50, 1–16. [Google Scholar] [CrossRef]
- Han, S.; Lu, Y.; Xie, J.; Fei, Y.; Zheng, G.; Wang, Z.; Liu, J.; Lv, L.; Ling, Z.; Berglund, B.; et al. Probiotic gastrointestinal transit and colonization after oral administration: A long journey. Front. Cell. Infect. Microbiol. 2021, 11, 609722. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, B.; De Los Reyes-Gavilán, C.G.; Margolles, A.; Gueimonde, M. Probiotic fermented milks: Present and future. Int. J. Dairy Technol. 2009, 62, 472–483. [Google Scholar] [CrossRef]
- Staniszewski, A.; Kordowska-Wiater, M. Probiotic and potentially probiotic yeasts—Characteristics and food application. Foods 2021, 10, 1306. [Google Scholar] [CrossRef]
- Pandey, K.; Naik, S.; Vakil, B. Probiotics, prebiotics and synbiotics-a review. J. Food Sci. Technol. 2015, 52, 7577–7587. [Google Scholar] [CrossRef] [Green Version]
- Agarbati, A.; Canonico, L.; Marini, E.; Zannini, E.; Ciani, M.; Comitini, F. Potential probiotic yeasts sourced from natural environmental and spontaneous processed foods. Foods 2020, 9, 287. [Google Scholar] [CrossRef] [Green Version]
- Hossain, M.N.; Afrin, S.; Humayun, S.; Ahmed, M.M.; Saha, B.K. Identification and growth characterization of a novel strain of Saccharomyces boulardii isolated from soya paste. Front. Nutr. 2020, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Souza HFd Carosia, M.F.; Pinheiro, C.; Carvalho MVd Oliveira CAFd Kamimura, E.S. On probiotic yeasts in food development: Saccharomyces boulardii, a trend. Food Sci. Technol. 2022, 42, e92321. [Google Scholar] [CrossRef]
- Hudson, L.E.; McDermott, C.D.; Stewart, T.P.; Hudson, W.H.; Rios, D.; Fasken, M.B.; Corbett, A.H.; Lamb, T.J. Characterization of the probiotic yeast Saccharomyces boulardii in the healthy mucosal immune system. PLoS ONE 2016, 11, e0153351. [Google Scholar] [CrossRef] [Green Version]
- Mousa, A.H.; Wang, G.; Zhang, H. Morphological and molecular tools for identification of Saccharomyces boulardii isolated from active dry yeast. Int. J. Agric. Innov. Res. 2019, 7. ISSN 2319-1473. [Google Scholar]
- Nayebhashemi, M.; Enayati, S.; Zahmatkesh, M.; Madanchi, H.; Saberi, S.; Mostafavi, E.; Ardakani, E.M.; Azizi, M.; Khalaj, V. Surface display of pancreatic lipase inhibitor peptides by engineered Saccharomyces boulardii: Potential as an anti-obesity probiotic. J. Funct. Foods 2023, 102, 105458. [Google Scholar]
- Moré, M.I.; Swidsinski, A. Saccharomyces boulardii CNCM I-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis—A review. Clin. Exp. Gastroenterol. 2015, 8, 237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Sá Del Fiol, F.; Tardelli Ferreira, A.C.M.; Marciano, J.J.; Marques, M.C.; Sant’Ana, L.L. Obesity and the use of antibiotics and probiotics in rats. Chemotherapy 2014, 60, 162–167. [Google Scholar] [CrossRef]
- Abreu, I.C.M.E.; Albuquerque, R.C.M.F.; Brandão, A.B.P.; Barssotti, L.; de Souza, L.B.; Ferreira, F.G.; Oliveira, L.C.G.; Yokota, R.; Sparvoli, L.G.; Dias, D.D.S.; et al. Saccharomyces boulardii exerts renoprotection by modulating oxidative stress, renin angiotensin system and uropathogenic microbiota in a murine model of diabetes. Life Sci. 2022, 301, 120616. [Google Scholar] [CrossRef]
- Barssotti, L.; Abreu, I.C.M.E.; Brandão, A.B.P.; Albuquerque, R.C.M.F.; Ferreira, F.G.; Salgado, M.A.C.; Dias, D.D.S.; De Angelis, K.; Yokota, R.; Casarini, D.E.; et al. Saccharomyces boulardii modulates oxidative stress and renin angiotensin system attenuating diabetes-induced liver injury in mice. Sci. Rep. 2021, 11, 9189. [Google Scholar] [CrossRef]
- Castagliuolo, I.; Riegler, M.F.; Valenick, L.; LaMont, J.T.; Pothoulakis, C. Saccharomyces boulardii protease inhibits the effects of Clostridium difficile toxins A and B in human colonic mucosa. Infect. Immun. 1999, 67, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Buts, J.-P.; Dekeyser, N.; Stilmant, C.; Delem, E.; Smets, F.; Sokal, E. Saccharomyces boulardii produces in rat small intestine a novel protein phosphatase that inhibits Escherichia coli endotoxin by dephosphorylation. Pediatr. Res. 2006, 60, 24–29. [Google Scholar] [CrossRef]
- Czerucka, D.; Roux, I.; Rampal, P. Saccharomyces boulardii inhibits secretagogue-mediated adenosine 3′, 5′-cyclic monophosphate induction in intestinal cells. Gastroenterology 1994, 106, 65–72. [Google Scholar] [CrossRef]
- Fakruddin, M.; Hossain, M.; Ahmed, M.M. Antimicrobial and antioxidant activities of Saccharomyces cerevisiae IFST062013, a potential probiotic. BMC Complement. Altern. Med. 2017, 17, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Generoso, S.V.; Viana, M.L.; Santos, R.G.; Arantes, R.M.; Martins, F.S.; Nicoli, J.R.; Machado, J.A.; Correia, M.I.; Cardoso, V.N. Protection against increased intestinal permeability and bacterial translocation induced by intestinal obstruction in mice treated with viable and heat-killed Saccharomyces boulardii. Eur. J. Nutr. 2011, 50, 261–269. [Google Scholar] [CrossRef]
- Moré, M.I.; Vandenplas, Y. Saccharomyces boulardii CNCM I-745 improves intestinal enzyme function: A trophic effects review. Clin. Med. Insights Gastroenterol. 2018, 11, 1179552217752679. [Google Scholar] [PubMed] [Green Version]
- Hennequin, C.; Kauffmann-Lacroix, C.; Jobert, A.; Viard, J.P.; Ricour, C.; Jacquemin, J.L.; Berche, P. Possible role of catheters in Saccharomyces boulardii fungemia. Eur. J. Clin. Microbiol. Infect. Dis. 2000, 19, 16–20. [Google Scholar] [CrossRef]
- Perapoch, J.; Planes, A.M.; Querol, A.; López, V.; Martínez-Bendayán, I.; Tormo, R.; Fernández, F.; Peguero, G.; Salcedo, S. Fungemia with Saccharomyces cerevisiae in two newborns, only one of whom had been treated with ultra-levura. Eur. J. Clin. Microbiol. Infect. Dis. 2000, 19, 468–470. [Google Scholar] [CrossRef]
- McFarland, L. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J. Gastroenterol. WJG 2010, 16, 2202. [Google Scholar] [CrossRef]
- Santos, D.C.D.; de Oliveira Filho, J.G.; de Sousa, T.L.; Ribeiro, C.B. Quality parameters and sensorial profile of clarified “Cerrado” cashew juice supplemented with Sacharomyces boulardii and different sweeteners. LWT 2020, 128, 109319. [Google Scholar]
- Chan, M.Z.A.; Liu, S.-Q. Fortifying foods with synbiotic and postbiotic preparations of the probiotic yeast, Saccharomyces boulardii. Curr. Opin. Food Sci. 2022, 43, 216–224. [Google Scholar] [CrossRef]
- Briand, F.; Sulpice, T.; Giammarinaro, P.; Roux, X. Saccharomyces boulardii CNCM I-745 changes lipidemic profile and gut microbiota in a hamster hypercholesterolemic model. Benef. Microbes 2019, 10, 555–567. [Google Scholar] [CrossRef]
- Everard, A.; Matamoros, S.; Geurts, L.; Delzenne, N.M.; Cani, P.D. Saccharomyces boulardii administration changes gut microbiota and reduces hepatic steatosis, low-grade inflammation, and fat mass in obese and type 2 diabetic db/db mice. mBio 2014, 5, e01011-14. [Google Scholar] [CrossRef] [Green Version]
- Girard, P.; Pansart, Y.; Verleye, M. Anti-Hypercholesterolemic Effect of Saccharomyces boulardii in the Hamster. Pharmacology 2014, 94, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Saikia, D.; Manhar, A.K.; Deka, B.; Roy, R.; Gupta, K.; Namsa, N.D.; Chattopadhyay, P.; Doley, R.; Mandal, M. Hypocholesterolemic activity of indigenous probiotic isolate Saccharomyces cerevisiae ARDMC1 in a rat model. J. Food Drug Anal. 2018, 26, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.J.; Hanes, D.A.; Schafer, M.B.; Mikolai, J.; Zwickey, H. Effect of the Probiotic Saccharomyces boulardii on Cholesterol and Lipoprotein Particles in Hypercholesterolemic Adults: A Single-Arm, Open-Label Pilot Study. J. Altern. Complement. Med. 2015, 21, 288–293. [Google Scholar] [CrossRef] [Green Version]
- Awoyemi, A.; Mayerhofer, C.; Felix, A.S.; Hov, J.R.; Moscavitch, S.D.; Lappegård, K.T.; Hovland, A.; Halvorsen, S.; Halvorsen, B.; Gregersen, I.; et al. Rifaximin or Saccharomyces boulardii in heart failure with reduced ejection fraction: Results from the randomized GutHeart trial. EBioMedicine 2021, 70, 103511. [Google Scholar] [CrossRef] [PubMed]
- Costanza, A.C.; Moscavitch, S.D.; Neto, H.C.F.; Mesquita, E.T. Probiotic therapy with Saccharomyces boulardii for heart failure patients: A randomized, double-blind, placebo-controlled pilot trial. Int. J. Cardiol. 2015, 179, 348–350. [Google Scholar] [CrossRef] [Green Version]
- Albuquerque, R.C.M.F.; Brandão, A.B.P.; De Abreu, I.C.M.E.; Ferreira, F.G.; Santos, L.B.; Moreira, L.N.; Taddei, C.R.; Aimbire, F.; Cunha, T.S. Saccharomyces boulardii Tht 500101 changes gut microbiota and ameliorates hyperglycaemia, dyslipidaemia, and liver inflammation in streptozotocin-diabetic mice. Benef. Microbes 2019, 10, 901–912. [Google Scholar] [CrossRef]
- Hoadley, J. US regulation of functional foods. In Functional Foods; Elsevier: Amsterdam, The Netherlands, 2011; pp. 41–63. [Google Scholar]
- Smith, I.M.; Baker, A.; Christensen, J.E.; Boekhout, T.; Frøkiær, H.; Arneborg, N.; Jespersen, L. Kluyveromyces marxianus and Saccharomyces boulardii Induce Distinct Levels of Dendritic Cell Cytokine Secretion and Significantly Different T Cell Responses In Vitro. PLoS ONE 2016, 11, e0167410. [Google Scholar] [CrossRef] [Green Version]
- Fortin, O.; Aguilar-Uscanga, B.R.; Vu, K.D.; Salmieri, S.; Lacroix, M. Effect of Saccharomyces Boulardii Cell Wall Extracts on Colon Cancer Prevention in Male F344 Rats Treated with 1,2-Dimethylhydrazine. Nutr. Cancer 2018, 70, 632–642. [Google Scholar] [CrossRef]
- Gautério, G.V.; Silvério, S.I.d.C.; Egea, M.B.; Lemes, A.C. β-glucan from brewer’s spent yeast as a techno-functional food ingredient. Front. Food Sci. Technol. 2022, 2, 1074505. [Google Scholar] [CrossRef]
- Salminen, S.; Collado, M.C.; Endo, A.; Hill, C.; Lebeer, S.; Quigley, E.M.M.; Sanders, M.E.; Shamir, R.; Swann, J.R.; Szajewska, H.; et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 649–667. [Google Scholar] [CrossRef]
- Eren, Z.; Gurol, Y.; Sonmezoglu, M.; Eren, H.S.; Celik, G.; Kantarci, G. Saccharomyces cerevisiae fungemia in an elderly patient following probiotic treatment. Mikrobiyoloji Bul. 2014, 48, 351–355. [Google Scholar] [CrossRef]
- Gupta, P.; Singh, Y.P.; Taneja, A. Saccharomyces: A Friend or Foe in ICU (A Case Report with Solution). Indian J. Crit. Care Med. 2019, 23, 430–431. [Google Scholar]
- Al-Assal, K.; Martinez, A.C.; Torrinhas, R.S.; Cardinelli, C.; Waitzberg, D. Gut microbiota and obesity. Clin. Nutr. Exp. 2018, 20, 60–64. [Google Scholar] [CrossRef] [Green Version]
- Walker, W.A. Chapter 25—Dysbiosis. In The Microbiota in Gastrointestinal Pathophysiology; Floch, M.H., Ringel, Y., Allan Walker, W., Eds.; Academic Press: Boston, MA, USA, 2017; pp. 227–232. [Google Scholar]
- De la Cuesta-Zuluaga, J.; Mueller, N.T.; Álvarez-Quintero, R.; Velásquez-Mejía, E.P.; Sierra, J.A.; Corrales-Agudelo, V.; Carmona, J.A.; Abad, J.M.; Escobar, J.S. Higher fecal short-chain fatty acid levels are associated with gut microbiome dysbiosis, obesity, hypertension and cardiometabolic disease risk factors. Nutrients 2018, 11, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, C.J.; Zheng, L.; Campbell, E.L.; Saeedi, B.; Scholz, C.C.; Bayless, A.J.; Wilson, K.E.; Glover, L.E.; Kominsky, D.J.; Magnuson, A.; et al. Crosstalk between microbiota-derived short-chain fatty acids and intestinal epithelial HIF augments tissue barrier function. Cell Host Microbe 2015, 17, 662–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baothman, O.A.; Zamzami, M.A.; Taher, I.; Abubaker, J.; Abu-Farha, M. The role of gut microbiota in the development of obesity and diabetes. Lipids Health Dis. 2016, 15, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campagnoli, L.I.M.; Marchesi, N.; Vairetti, M.; Pascale, A.; Ferrigno, A.; Barbieri, A. Age-related NAFLD: The use of probiotics as a supportive therapeutic intervention. Cells 2022, 11, 2827. [Google Scholar] [CrossRef] [PubMed]
- Perumpail, B.J.; Li, A.A.; John, N.; Sallam, S.; Shah, N.D.; Kwong, W.; Cholankeril, G.; Kim, D.; Ahmed, A. The Therapeutic Implications of the Gut Microbiome and Probiotics in Patients with NAFLD. Diseases 2019, 7, 27. [Google Scholar] [CrossRef] [Green Version]
- Carpino, G.; Del Ben, M.; Pastori, D.; Carnevale, R.; Baratta, F.; Overi, D.; Francis, H.; Cardinale, V.; Onori, P.; Safarikia, S.; et al. Increased Liver Localization of Lipopolysaccharides in Human and Experimental NAFLD. Hepatology 2020, 72, 470–485. [Google Scholar] [CrossRef]
- Xue, L.; He, J.; Gao, N.; Lu, X.; Li, M.; Wu, X.; Liu, Z.; Jin, Y.; Liu, J.; Xu, J.; et al. Probiotics may delay the progression of nonalcoholic fatty liver disease by restoring the gut microbiota structure and improving intestinal endotoxemia. Sci. Rep. 2017, 7, 45176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maciejewska, D.; Łukomska, A.; Dec, K.; Skonieczna-Żydecka, K.; Gutowska, I.; Skórka-Majewicz, M.; Styburski, D.; Misiakiewicz-Has, K.; Pilutin, A.; Palma, J.; et al. Diet-Induced Rat Model of Gradual Development of Non-Alcoholic Fatty Liver Disease (NAFLD) with Lipopolysaccharides (LPS) Secretion. Diagnostics 2019, 9, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hegazy, M.A.; Mogawer, S.M.; Alnaggar, A.R.L.R.; Ghoniem, O.A.; Samie, R.M.A. Serum LPS and CD163 Biomarkers Confirming the Role of Gut Dysbiosis in Overweight Patients with NASH. Diabetes Metab. Syndr. Obes. 2020, 13, 3861–3872. [Google Scholar] [CrossRef] [PubMed]
- Ferro, D.; Baratta, F.; Pastori, D.; Cocomello, N.; Colantoni, A.; Angelico, F.; Del Ben, M. New Insights into the Pathogenesis of Non-Alcoholic Fatty Liver Disease: Gut-Derived Lipopolysaccharides and Oxidative Stress. Nutrients 2020, 12, 2762. [Google Scholar]
- Del Ben, M.; Polimeni, L.; Baratta, F.; Bartimoccia, S.; Carnevale, R.; Loffredo, L.; Pignatelli, P.; Violi, F.; Angelico, F. Serum cytokeratin-18 is associated with NOX2-generated oxidative stress in patients with nonalcoholic fatty liver. Int. J. Hepatol. 2014, 2014, 784985. [Google Scholar] [CrossRef]
- Sabirin, F.; Lim, S.M.; Neoh, C.F.; Ramasamy, K. Hepatoprotection of Probiotics Against Non-Alcoholic Fatty Liver Disease in vivo: A Systematic Review. Front. Nutr. 2022, 9, 844374. [Google Scholar]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef]
- Wang, T.; He, C. Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Cytokine Growth Factor Rev. 2018, 44, 38–50. [Google Scholar]
- Egea, M.B.; Pierce, G.; Becraft, A.; Sturm, M.; Yu, W.; Shay, N. Intake of Watermelon and Watermelon Byproducts Male Mice Fed a Western-style Obesigenic Diet Alters Hepatic Gene Expression Patterns as Determined by RNA Sequencing. Curr. Dev. Nutr. 2020, 4, nzaa122. [Google Scholar] [CrossRef] [PubMed]
- Egea, M.B.; Pierce, G.; Park, S.-H.; Lee, S.-I.; Heger, F.; Shay, N. Consumption of Antioxidant-Rich “Cerrado” Cashew Pseudofruit Affects Hepatic Gene Expression in Obese C57BL/6J High Fat-Fed Mice. Foods 2022, 11, 2543. [Google Scholar] [CrossRef] [PubMed]
- Wilund, K.R.; Yu, L.; Xu, F.; Hobbs, H.H.; Cohen, J.C. High-level expression of ABCG5 and ABCG8 attenuates diet-induced hypercholesterolemia and atherosclerosis in Ldlr−/− mice. J. Lipid Res. 2004, 45, 1429–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rondanelli, M.; Miraglia, N.; Putignano, P.; Castagliuolo, I.; Brun, P.; Dall’Acqua, S.; Peroni, G.; Faliva, M.A.; Naso, M.; Nichetti, M.; et al. Effects of 60-day saccharomyces boulardii and superoxide dismutase supplementation on body composition, hunger sensation, pro/antioxidant ratio, inflammation and hormonal lipo-metabolic biomarkers in obese adults: A double-blind, placebo-controlled trial. Nutrients 2021, 13, 2512. [Google Scholar] [CrossRef]
- Palacios, T.; Vitetta, L.; Coulson, S.; Madigan, C.D.; Lam, Y.Y.; Manuel, R.; Briskey, D.; Hendy, C.; Kim, J.-N.; Ishoey, T.; et al. Targeting the intestinal microbiota to prevent type 2 diabetes and enhance the effect of metformin on glycaemia: A randomised controlled pilot study. Nutrients 2020, 12, 2041. [Google Scholar] [CrossRef]

| Administration (Dose/Duration) | Model | Principally Observed Results | References |
|---|---|---|---|
| Administration of S. boulardii CNCM I-745 (3 g/kg) by oral gavage (twice a week) for 21 or 39 days | Six-week-old hypercholesterolemic male Golden Syrian hamsters (0.3% cholesterol diet) (n = 40) | ↑ 23 and 36% of total cholesterol in feces at 21 (p < 0.05) and 39 (p < 0.01) days, respectively; HMGCoA-R gene expression at 21 and 39 days (p < 0.05); and the presence of the phyla Pseudomonadota (former Proteobacteria) and Lentispharerae (p < 0.05). ↓ plasma total cholesterol (p < 0.001); 31% HDL-c in 21 days; 25% hepatic triglycerides (p < 0.05) in 39 days; 43% of the total mass of bile excreted in feces in 21 days; ABCG5 gene expression at 21 and 39 days (p < 0.05); ABCG8 gene expression in 39 days (p < 0.05); and the presence of phyla Bacillota, Tenericutes, and TM7 (p < 0.05). | Briand et al. [82] |
| Daily administration of S. boulardii Biocodex (120 mg) by oral gavage for 4 weeks | Six-week-old mice with leptin resistant obesity and type 2 diabetes (db/db) (n = 30) | ↑ mass of cecum and cecum tissue; 160 times total Saccharomyces and 40 times total yeast cells; 37% phylum Bacteroidota; 6 times the Bacteroidaceae family; and 40 times the genus Bacteroides. ↓ 15% mass gain; fat mass; liver mass; adipose index; visceral, epididymal, and subcutaneous fat; total fat content in the liver; markers of hepatic macrophage infiltration (50% for CD11c, 40% for MCP-1, and 37% for IL-1B); plasma concentrations of cytokines (IL-6 and IL-4 twice); 57, 55, and 30% the phyla Tenericutes, Proteobacteria, and Bacillota; 8 times the Porphyromonadaceae family; and genera Anaeroplasma (92%), Anaerotruncus (47%), Dorea (77%), Odoribacter (82%), Oscillospira (38%), Parabacteroides (91%), Prevotella (76%), and Ruminococcus (44%). | Everard et al. [83] |
| Oral administration of S. boulardii at 12 × 1010 CFU/kg (3 g/kg) twice a day in two experimental designs, being (1) a preventive protocol for 14 days from the beginning of the diet and (2) a curative protocol after a 14-day curative protocol with S. boulardii starting after 14 days of cholesterolemic diet | Male Golden Syrian hamsters (weighed 80–90 g, 0.1% cholesterol) | ↓ (1) 14% increased cholesterolemia and 26% increased liver cholesterol; and (2) 12% increase in cholesterolemia and 39% increase in total plasma triglycerides. | Girard et al. [84] |
| S. boulardii (Lupin Laboratories, India) was administered at a concentration of 108 CFU/g along with the diet (0.5% cholesterol, 30% dalda, 10% refined oil and 50% wheat flour) with high lipid concentration for 21 (1) and 42 (2) days | Adult male Wistar rats (mean body weight 150 g, n = 12) | ↓ (1) total triglycerides (108.12 to 85.63 mg/dL) and total cholesterol (98.88 to 74.70 mg/dL); (2) total triglycerides (260.20 to 108.73 mg/dL), total cholesterol (173.70 to 65.63 mg/dL), LDL-c (110.37 to 27.55 mg/dL), atherogenic index (9.67 to 3.05), LDL/HDL (6.82 to 1.64), and body mass (314.16 to 300.83 g). | Saikia et al. [85] |
| Saccharomyces boulardii CNCM I-745 (Yomogi®) (Ardeypharm GmbH, Herdecke, Germany) was administered at a concentration of 109 yeast cell/rat daily by oral gavage for 2 weeks (14 d) | Male Sprague-Dawley rats (8-week-aged and body weight to 150–180) assigned a high-fat diet for 8 weeks (body weight to 350–400 g) | After two weeks of treatment with S. boulardii, there was no significant change in triglyceride and total cholesterol levels, as well as body weight of the rats. | Nayebhashemi et al. [66] |
| Two capsules of 250 mg of the S. boulardii (CNMI-745) twice a day for 3-month oral daily therapy | Heart failure patients (n = 46, phase II, multicenter, randomized, open-label, controlled trial) | ↑ N-terminal-pro-B-type-natriuretic peptide level. No significant difference these was demonstrate for C-reactive protein, trimethyl-mine N-oxide (TMAO), and global microbiota composition (beta diversity) and bacterial richness (a diversity) from baseline to the end of the intervention group. | Awoyemi et al. [87] |
| S. boulardii (1000 mg) per day for 3-month oral daily therapy | Heart failure patients (n = 7, randomized, double-blind, placebo-controlled pilot trial) | ↓ total cholesterol (150.8 to 143.2 mg/dL); uric acid (6.15 to 5.1 mg/dL); creatinine (1.12 to 0.9 mg/dL); high-sensitivity C reactive protein (0.65 to 0.22 mg/dL); and left atrial diameter (4.5 to 4.2 cm). | Costanza et al. [88] |
| S. boulardii CNCM I-1079 (5.6 × 1010 CFU/g) per capsule twice daily for a period of 8 weeks | Participants (n = 11) hypercholesterolemic (200–275 mg/dL and BMI of 20–45 kg/m2) aged 21–69 years | ↓ remnant lipoprotein particles (p = 0.03).Nonsignificant results in the variables measured related to the MetS. | Ryan et al. [86] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Egea, M.B.; Oliveira Filho, J.G.d.; Lemes, A.C. Investigating the Efficacy of Saccharomyces boulardii in Metabolic Syndrome Treatment: A Narrative Review of What Is Known So Far. Int. J. Mol. Sci. 2023, 24, 12015. https://doi.org/10.3390/ijms241512015
Egea MB, Oliveira Filho JGd, Lemes AC. Investigating the Efficacy of Saccharomyces boulardii in Metabolic Syndrome Treatment: A Narrative Review of What Is Known So Far. International Journal of Molecular Sciences. 2023; 24(15):12015. https://doi.org/10.3390/ijms241512015
Chicago/Turabian StyleEgea, Mariana Buranelo, Josemar Gonçalves de Oliveira Filho, and Ailton Cesar Lemes. 2023. "Investigating the Efficacy of Saccharomyces boulardii in Metabolic Syndrome Treatment: A Narrative Review of What Is Known So Far" International Journal of Molecular Sciences 24, no. 15: 12015. https://doi.org/10.3390/ijms241512015
APA StyleEgea, M. B., Oliveira Filho, J. G. d., & Lemes, A. C. (2023). Investigating the Efficacy of Saccharomyces boulardii in Metabolic Syndrome Treatment: A Narrative Review of What Is Known So Far. International Journal of Molecular Sciences, 24(15), 12015. https://doi.org/10.3390/ijms241512015








