A Novel Aniline Derivative from Peganum harmala L. Promoted Apoptosis via Activating PI3K/AKT/mTOR-Mediated Autophagy in Non-Small Cell Lung Cancer Cells
Abstract
:1. Introduction
2. Results
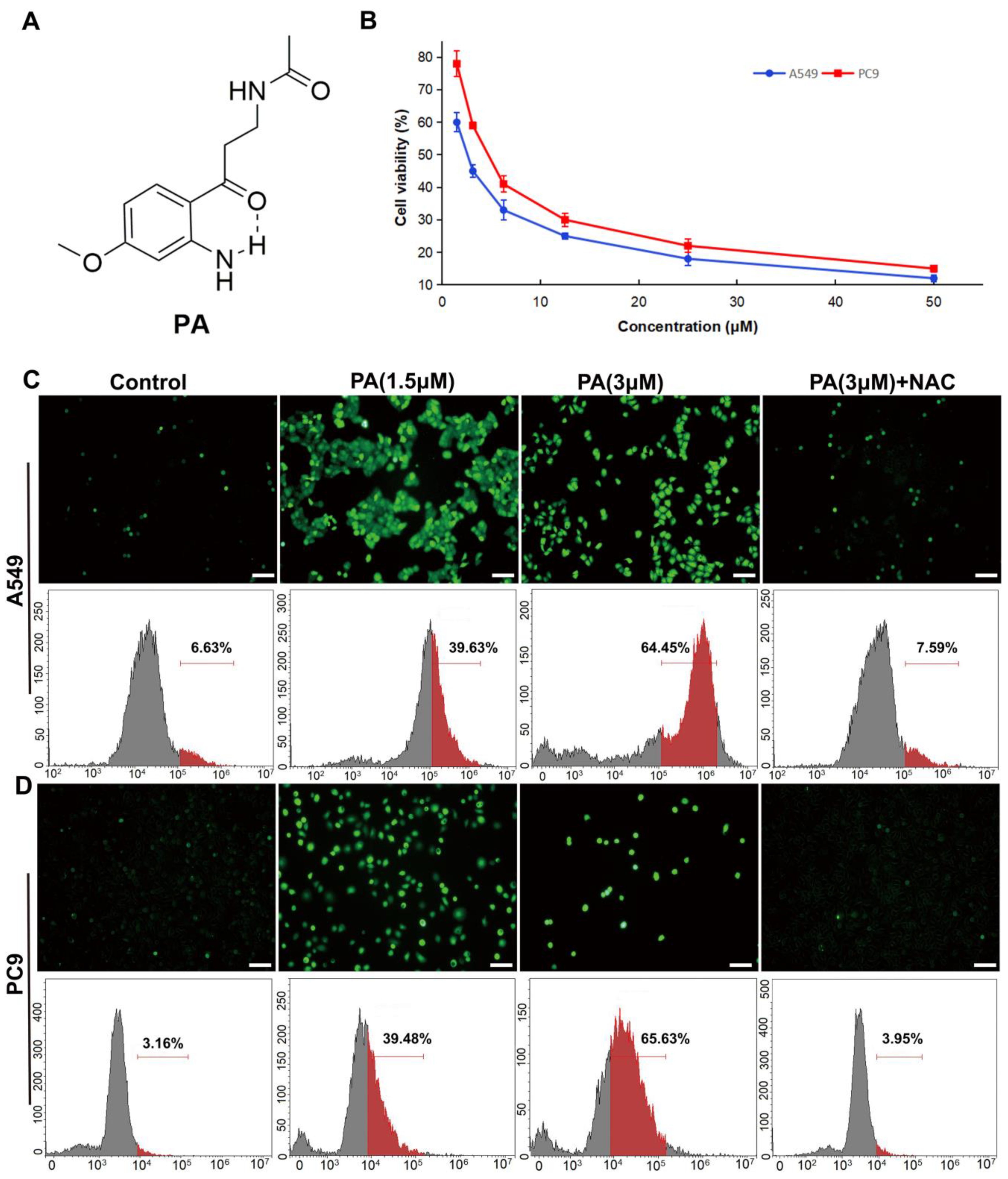
2.1. Structural Elucidation of Pegaharoline A (PA)
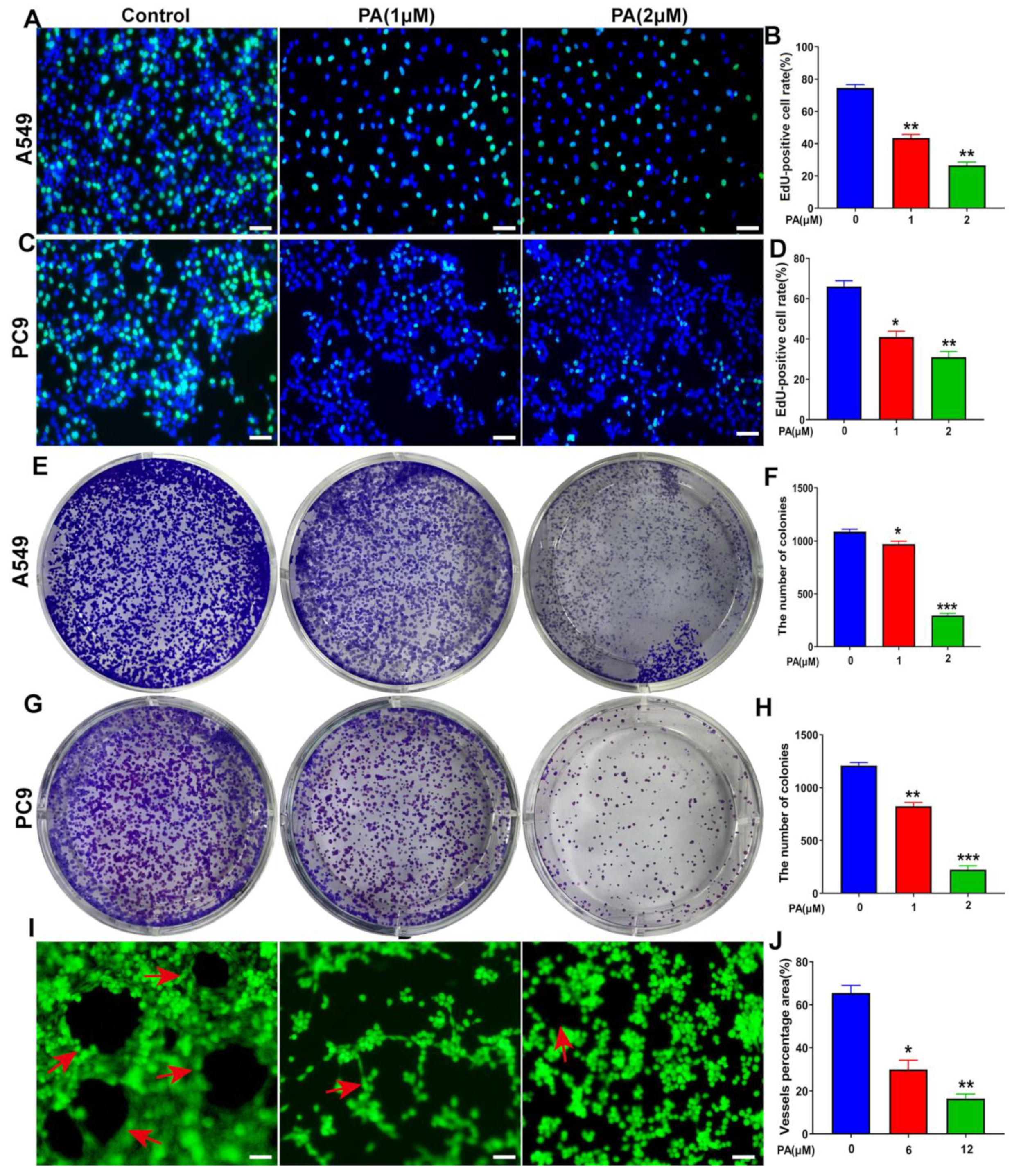
2.2. Pegaharoline A (PA) Inhibited the Proliferation of NSCLC Cells
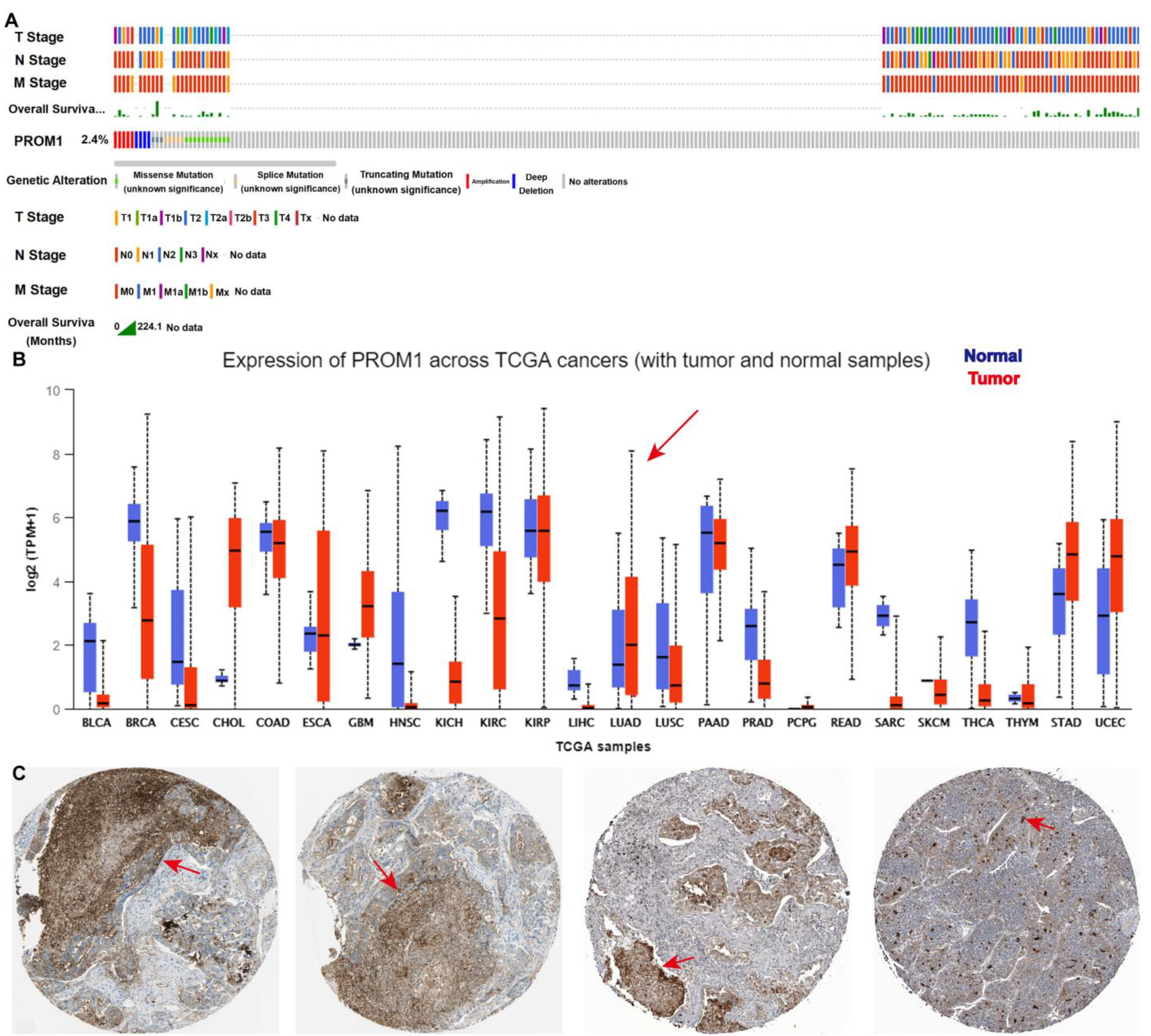
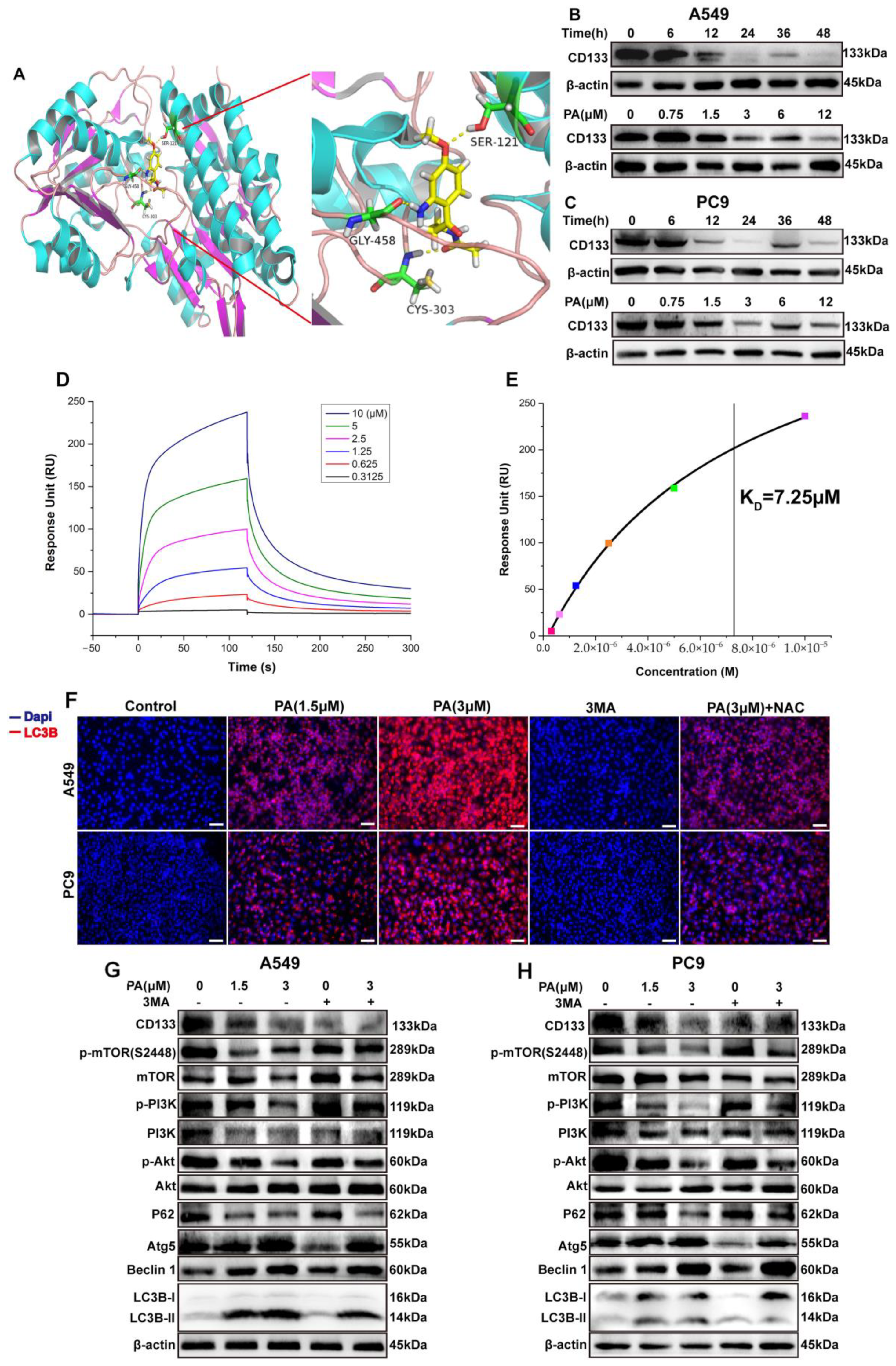
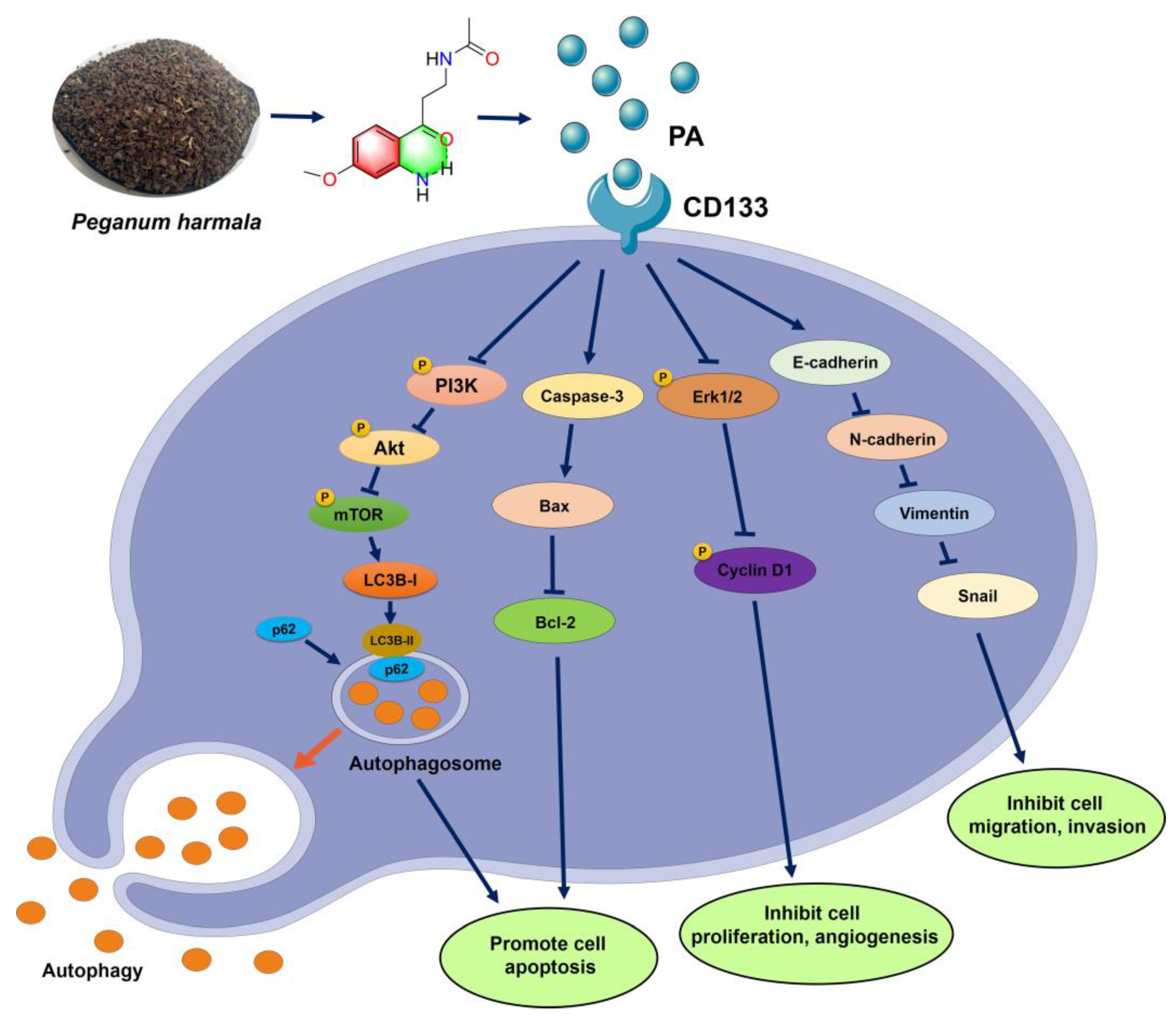
2.3. Pegaharoline A (PA) Inhibited the Expression of CD133 to Activate Autophagy through Blocking the PI3K/AKT/mTOR Pathway
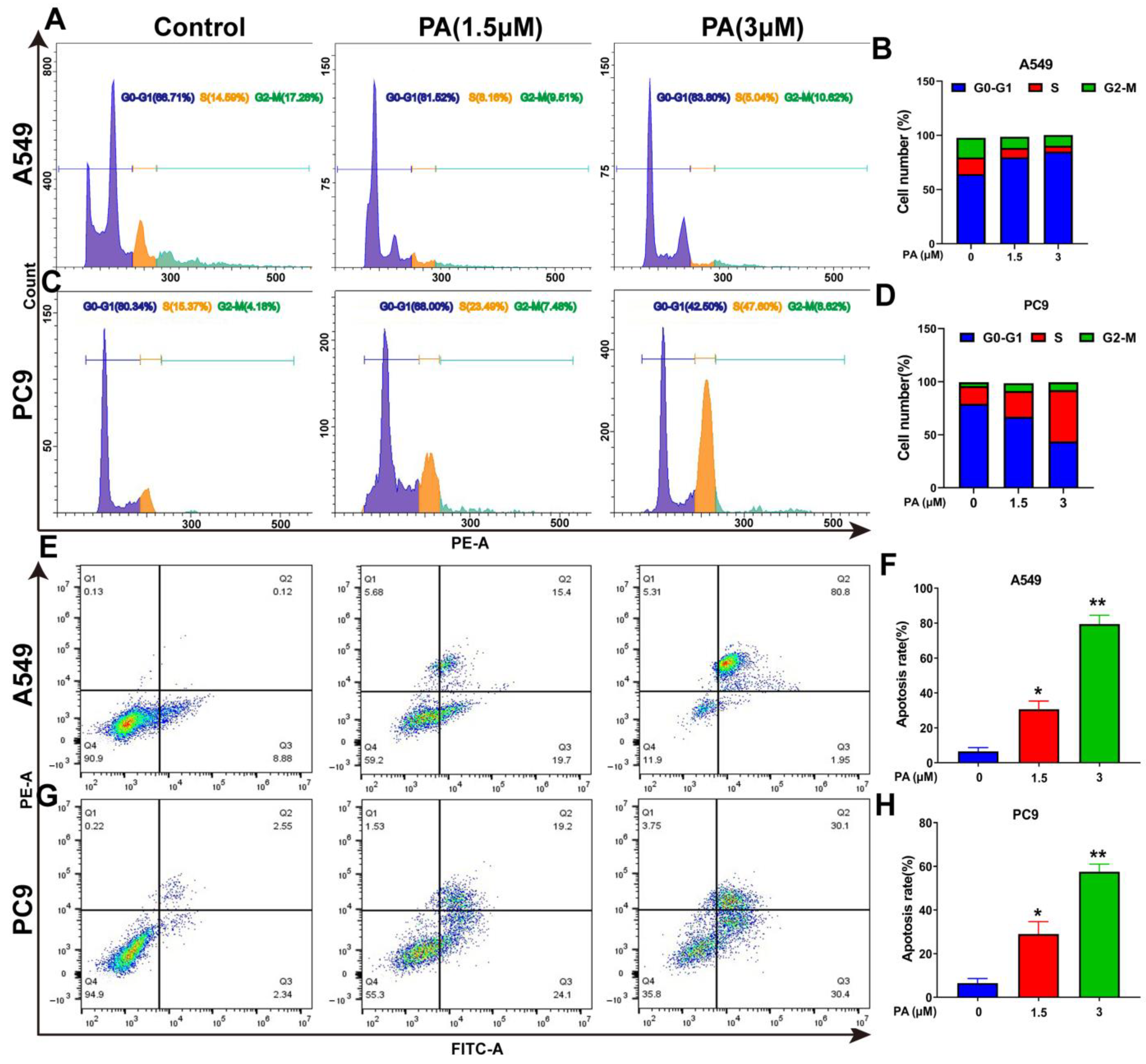
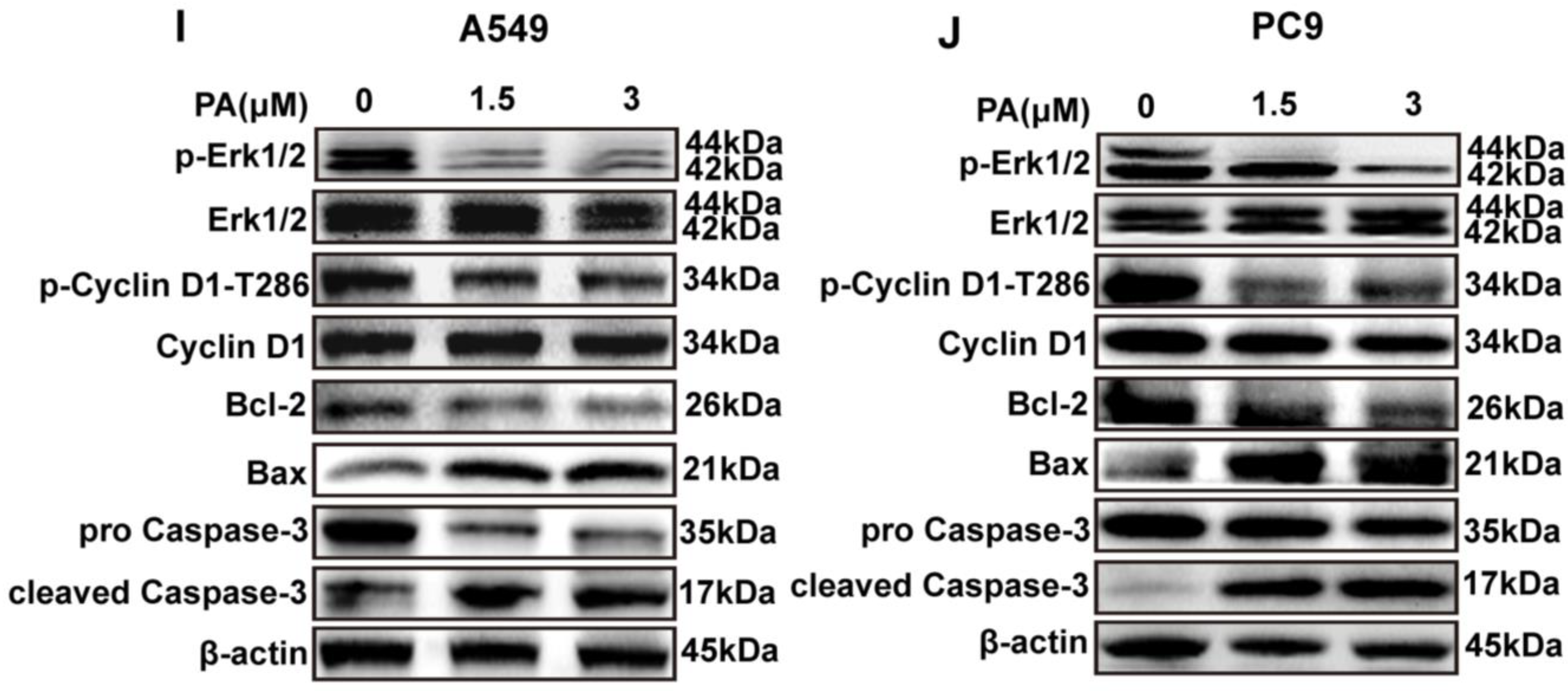
2.4. Pegaharoline A (PA) Arrested the Cell Cycle and Promoted Apoptosis of NSCLC Cells
2.5. Pegaharoline A (PA) Inhibits DNA Synthesis, Clone Formation, and Angiogenesis of HUVECs
2.6. Pegaharoline A (PA) Inhibited the Invasion and Migration Abilities of NSCLC Cells through Inhibiting the EMT Signal Pathway
3. Discussion
4. Materials and Methods
4.1. Experimental Instruments and Chemicals
4.2. Plant Material
4.3. Extraction and Isolation
4.4. Cell Culture
4.5. MTT Assay
4.6. Measurement of ROS
4.7. Molecular Docking Studies
4.8. Immunofluorescence Assay
4.9. Western Blotting
4.10. Apoptosis Assay
4.11. Cell Cycle Assay
4.12. EdU Staining
4.13. Colony Formation Assay
4.14. Transwell Test
4.15. Angiogenesis of HUVEC Assay
4.16. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, W.Q.; Li, H.; Sun, K.X.; Zheng, R.S.; He, J. Report of cancer incidence and mortality in China, 2014. Chin. J. Oncol. 2018, 40, 5–13. [Google Scholar] [CrossRef]
- Torre, L.A.; Siegel, R.L.; Jemal, A. Lung cancer statistics. In Lung Cancer and Personalized Medicine; Part of Advances in Experimental Medicine and Biology Book Series (AEMB); Springer: Cham, Switzerland, 2016; Volume 893, pp. 1–19. [Google Scholar] [CrossRef]
- Rossi, A.; La-Salvia, A.; Di-Maio, M. Chemotherapy and intercalated gefitinib or erlotinib in the treatment of advanced non-small-cell lung cancer. Expert Rev. Respir. Med. 2017, 11, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Ding, P.N.; Lord, S.J.; Gebski, V.; Links, M.; Bray, V.; Gralla, R.J.; Yang, J.C.; Lee, C.K. Risk of treatment-related toxicities from EGFR tyrosine kinase inhibitors: A meta-analysis of clinical trials of gefitinib, erlotinib, and afatinib in advanced EGFR-mutated non-small cell lung cancer. J. Thorac. Oncol. 2017, 12, 633–643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.N.; Chen, P.C.; Wu, Q.S.; Gio, L.B.; Leong, K.W.; Chan, K.L.; Kwok, H.F. A novel combination treatment of antiADAM17 antibody and erlotinib to overcome acquired drug resistance in non-small cell lung cancer through the FOXO3a/FOXM1 axis. Cell. Mol. Life Sci. 2022, 79, 614. [Google Scholar] [CrossRef]
- Li, J.N.; Kwok, H.F. Current strategies for treating NSCLC: From biological mechanisms to clinical treatment. Cancers 2020, 12, 1587. [Google Scholar] [CrossRef]
- Xia, J.B.; Dai, L.J.; Wang, L.S.; Zhu, J. Ganoderic acid DM induces autophagic apoptosis in non-small cell lung cancer cells by inhibiting the PI3K/Akt/mTOR activity. Chem.-Biol. Interact. 2020, 316, 108932. [Google Scholar] [CrossRef]
- Zhang, R.R.; Meng, N.N.; Liu, C.; Li, K.L.; Wang, M.X.; Lv, Z.B.; Chen, S.Y.; Guo, X.; Wang, X.K.; Wang, Q.; et al. PDB-1 from Potentilla discolor Bunge induces apoptosis and autophagy by downregulating the PI3K/Akt/mTOR signaling pathway in A549 cells. Biomed. Pharmacother. 2020, 129, 110378. [Google Scholar] [CrossRef]
- Agliano, A.; Calvo, A.; Box, C. The challenge of targeting cancer stem cells to halt metastasis. Semin. Cancer Biol. 2017, 44, 25–42. [Google Scholar] [CrossRef]
- Hardavella, G.; George, R.; Sethi, T. Lung cancer stem cells-characteristics, phenotype. Transl. Lung. Cancer Res. 2016, 5, 272–279. [Google Scholar] [CrossRef] [Green Version]
- Kim, W.T.; Ryu, C.J. Cancer stem cell surface markers on normal stem cells. BMB Rep. 2017, 50, 285–298. [Google Scholar] [CrossRef] [Green Version]
- Behrooz, A.B.; Syahir, A.; Ahmad, S. CD133: Beyond a cancer stem cell biomarker. J. Drug Target. 2019, 27, 257–269. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Wen, G.M.; Hou, W.; Xia, P. The roles of CD133 expression in the patients with non-small cell lung cancer. Cancer Biomark. 2018, 22, 385–394. [Google Scholar] [CrossRef]
- Huang, X.; Wan, J.; Leng, D.; Zhang, Y.; Yang, S. Dual-targeting nanomicelles with CD133 and CD44 aptamers for enhanced delivery of gefitinib to two populations of lung cancer-initiating cells. Exp. Ther. Med. 2020, 19, 192–204. [Google Scholar] [CrossRef]
- Galluzzi, L.; Pietrocola, F.; Bravo-San Pedro, J.M.; Amaravadi, R.K.; Baehrecke, E.H.; Cecconi, F.; Codogno, P.; Debnath, J.; Gewirtz, D.A.; Karantza, V.; et al. Autophagy in malignant transformation and cancer progression. EMBO. J. 2015, 34, 856–880. [Google Scholar] [CrossRef] [Green Version]
- Russell, R.C.; Yuan, H.X.; Guan, K.L. Autophagy regulation by nutrient signaling. Cell Res. 2014, 24, 42–57. [Google Scholar] [CrossRef] [Green Version]
- Marino, G.; Niso-Santano, M.; Baehrecke, E.H.; Kroemer, G. Self-consumption: The interplay of autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 2014, 15, 81–94. [Google Scholar] [CrossRef] [Green Version]
- Liang, J.; Zhou, J.; Xu, Y.; Huang, X.; Wang, X.; Huang, W.; Li, H. Osthole inhibits ovarian carcinoma cells through LC3-mediated autophagy and GSDME-dependent pyroptosis except for apoptosis. Eur. J. Pharmacol. 2020, 874, 172990. [Google Scholar] [CrossRef]
- Editorial Committee of the Desert Flora of China. Desert Flora of China (II); Science Press: Beijing, China, 1987; pp. 306–308. [Google Scholar]
- Ma, J.; Wang, X.L. The species and distribution of genus Peganum L. in the desert area of China. J. Desert Res. 1998, 2, 131–136. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD9899&filename=ZGSS802.005&uniplatform=NZKPT&v=kdHSjebEMGOeNkH7-6MFvW_2JgNlDY1EWaNt8IdbYnBKfL_Kv6wTRtVHG2i7M64V (accessed on 1 January 2020).
- Li, S.G.; Wang, K.B.; Gong, Q.; Bao, Y.; Qin, N.B.; Li, D.H.; Li, Z.L.; Bai, J.; Hua, H.M. Cytotoxic quinazoline alkaloids from the seeds of Peganum harmala. Bioorg. Med. Chem. Lett. 2018, 28, 103–106. [Google Scholar] [CrossRef]
- Wang, K.B.; Hu, X.; Li, S.G.; Li, X.Y.; Li, D.H.; Bai, J.; Pei, Y.H.; Li, Z.L.; Hua, H.M. Racemic indole alkaloids from the seeds of Peganum harmala. Fitoterapia 2018, 125, 155–160. [Google Scholar] [CrossRef]
- Liu, X.; Li, M.X.; Tan, S.; Wang, C.H.; Fan, S.J.; Huang, C. Harmine is an inflammatory inhibitor through the suppression of NF-κB signaling. Biochem. Biophys. Res. Commun. 2017, 489, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Niu, X.F.; Yao, Q.; Li, W.F.; Zang, L.L.; Li, W.Q.; Zhao, J.M.; Liu, F.; Zhi, W.B. Harmine mitigates LPS-induced acute kidney injury through inhibition of the TLR4-NF-κB/NLRP3 inflammasome signalling pathway in mice. Eur. J. Pharmacol. 2019, 849, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Benzekri, R.; Bouslama, L.; Papetti, A.; Hammami, M.; Smaoui, A.; Limam, F. Anti HSV-2 activity of Peganum harmala (L.) and isolation of the active compound. Microb. Pathog. 2018, 114, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.Y.; Su, A.R.; Fu, Y.X.; Wang, X.H.; Lv, X.W.; Xu, W.T.; Xu, S.J.; Wang, H.R.; Wu, Z.W. Harmine blocks herpes simplex virus infection through downregulating cellular NF-κB and MAPK pathways induced by oxidative stress. Antiviral Res. 2015, 123, 27–38. [Google Scholar] [CrossRef]
- Wu, Z.N.; Chen, N.H.; Tang, Q.; Chen, S.; Zhan, Z.C.; Zhang, Y.B.; Wang, G.C.; Li, Y.L.; Ye, W.C. β-Carboline alkaloids from the seeds of Peganum harmala and their anti-HSV-2 virus activities. Org. Lett. 2020, 22, 7310–7314. [Google Scholar] [CrossRef]
- Herraiz, T.; Guilln, H. Monoamine oxidase-A inhibition and associated antioxidant activity in plant extracts with potential antidepressant actions. Biomed Res. Int. 2018, 2018, 4810394. [Google Scholar] [CrossRef] [Green Version]
- Herraiz, T.; Guilln, H.; Arn, V.J.; Salgado, A. Identification, occurrence and activity of quinazoline alkaloids in Peganum harmala. Food Chem. Toxicol. 2017, 103, 261–269. [Google Scholar] [CrossRef]
- Zhou, J.; Zhang, L.; Wang, M.; Zhou, L.; Feng, X.P.; Yu, L.L.; Lan, J.; Gao, W.; Zhang, C.D.; Bu, Y.Q.; et al. CPX targeting DJ-1 triggers ROS-induced cell death and protective autophagy in colorectal cancer. Theranostics 2019, 9, 5577–5594. [Google Scholar] [CrossRef]
- Alexandre, J.; Hu, Y.; Lu, W.; Pelicano, H.; Huang, P. Novel action of paclitaxel against cancer cells: Bystander effect mediated by reactive oxygen species. Cancer Res. 2007, 67, 3512–3517. [Google Scholar] [CrossRef] [Green Version]
- Gao, N.; Rahmani, M.; Dent, P.; Grant, S. 2-Methoxyestradiol-induced apoptosis in human leukemia cells proceeds through a reactive oxygen species and Akt-dependent process. Oncogene 2005, 24, 3797–3809. [Google Scholar] [CrossRef] [Green Version]
- Bertolini, G.; D′Amico, L.; Moro, M.; Landoni, E.; Perego, P.; Miceli, R.; Gatti, L.; Andriani, F.; Wong, D.; Caserini, R.; et al. Microenvironment-modulated metastatic CD133+/CXCR4+/EpCAM-lung cancer-initiating cells sustain tumor dissemination and correlate with poor prognosis. Cancer Res. 2015, 75, 3636–3649. [Google Scholar] [CrossRef] [Green Version]
- Huddle, B.C.; Grimley, E.; Buchman, C.D.; Chtcherbinine, M.; Debnath, B.; Mehta, P.; Yang, K.; Morgan, C.A.; Li, S.; Felton, J.; et al. Structure-based optimization of a novel class of aldehyde dehydrogenase 1A (ALDH1A) subfamily-selective inhibitors as potential adjuncts to ovarian cancer chemotherapy. J. Med. Chem. 2018, 61, 8754–8773. [Google Scholar] [CrossRef]
- Hsin, I.L.; Chiu, L.Y.; Ou, C.C.; Wu, W.J.; Sheu, G.T.; Ko, J.L. CD133 inhibition via autophagic degradation in pemetrexed-resistant lung cancer cells by GMI, a fungal immunomodulatory protein from Ganoderma microsporum. Br. J. Cancer 2020, 123, 449–458. [Google Scholar] [CrossRef]
- Wu, Q.S.; Chen, P.C.; Li, J.N.; Lin, Z.Q.; Zhang, Q.W.; Kwok, H.F. Inhibition of bladder cancer growth with homoharringtonine by inactivating integrin α5/β1-FAK/Src axis: A novel strategy for drug application. Pharmacol. Res. 2023, 188, 106654. [Google Scholar] [CrossRef]
- Goel, S.; DeCristo, M.J.; McAllister, S.S.; Zhao, J.J. CDK4/6 inhibition in cancer: Beyond cell cycle arrest. Trends Cell Biol. 2018, 28, 911–925. [Google Scholar] [CrossRef]
- Roskoski, R.J. Targeting ERK1/2 protein-serine/threonine kinases in human cancers. Pharmacol. Res. 2019, 142, 151–168. [Google Scholar] [CrossRef]
- Montalto, F.I.; De Amicis, F. Cyclin D1 in cancer: A molecular connection for cell cycle control, adhesion and invasion in tumor and stroma. Cells 2020, 9, 2648. [Google Scholar] [CrossRef]
- Asadi, M.; Taghizadeh, S.; Kaviani, E.; Vakili, O.; Taheri-Anganeh, M.; Tahamtan, M.; Savardashtaki, A. Caspase-3: Structure, function, and biotechnological aspects. Biotechnol. Appl. Biochem. 2022, 69, 1633–1645. [Google Scholar] [CrossRef]
- Liu, E.Y.; Ryan, K.M. Autophagy and cancer-issues we need to digest. J. Cell Sci. 2012, 125, 2349–2358. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.C.; Guan, K.L. mTOR: A pharmacologic target for autophagy regulation. J. Clin. Investig. 2015, 125, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Nazio, F.; Bordi, M.; Cianfanelli, V.; Locatelli, F.; Cecconi, F. Autophagy and cancer stem cells: Molecular mechanisms and therapeutic applications. Cell Death Differ. 2019, 26, 690–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheel, C.; Weinberg, R.A. Cancer stem cells and epithelial-mesenchymal transition: Concepts and molecular links. Semin. Cancer Biol. 2012, 22, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Derynck, R.; Weinberg, R.A. EMT and cancer: More than meets the eye. Dev. Cell 2019, 49, 313–316. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Z.C.; Dong, X.L.; Dai, Y.; Xiao, G.K.; Wang, X.L.; Wong, K.C.; Wong, M.S.; Yao, X.S. Discovery of a new class of Cathepsin K inhibitors in Rhizoma drynariae as potential candidates for the treatment of osteoporosis. Int. J. Mol. Sci. 2016, 17, 2116. [Google Scholar] [CrossRef] [Green Version]
- Malik, Y.A.; Awad, T.A.; Abdalla, M.; Yagi, S.; Alhazmi, H.A.; Ahsan, W.; Albratty, M.; Najmi, A.; Muhammad, S.; Khalid, A. Chalcone scaffolds exhibiting acetylcholinesterase enzyme inhibition: Mechanistic and computational investigations. Molecules 2022, 27, 3181. [Google Scholar] [CrossRef]
- Alquraini, A. Potency of hexaconazole to disrupt endocrine function with sex hormone-binding globulin. Int. J. Mol. Sci. 2023, 24, 3882. [Google Scholar] [CrossRef]
- Ghanem, A.; Al-Karmalawy, A.A.; Maksoud, A.I.A.E.; Hanafy, S.M.; Emara, H.A.; Saleh, R.M.; Elshal, M.F. Rumex Vesicarius L. extract improves the efficacy of doxorubicin in triple-negative breast cancer through inhibiting Bcl2, mTOR, JNK1 and augmenting p21 expression. Inform. Med. Unlocked 2022, 29, 100869. [Google Scholar] [CrossRef]
- ElMahdy, M.K.; Zaki, M.O.; Al-Karmalawy, A.A.; Abdo, W.; Alnasser, S.M.; Antar, S.A. Glimepiride ameliorates renal toxicity induced by cadmium in mice: Modulation of Jun N terminal kinase (JNK)/nuclear factor kappa B (NF-κB) and phosphatidylinositol 3-kinases (PI3K)/protein kinase (AKT) pathways. Life Sci. 2022, 311, 121184. [Google Scholar] [CrossRef]
- Alzokaky, A.A.; Al-Karmalawy, A.A.; Saleh, M.A.; Abdo, W.; Farage, A.E.; Belal, A.; Abourehab, M.A.S.; Antar, S.A. Metformin ameliorates doxorubicin-induced cardiotoxicity targeting HMGB1/TLR4/NLRP3 signaling pathway in mice. Life Sci. 2023, 316, 121390. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Z.; Li, W.; Tang, Q.; Huang, L.; Zhan, Z.; Li, Y.; Wang, G.; Dai, X.; Zhang, Y. A Novel Aniline Derivative from Peganum harmala L. Promoted Apoptosis via Activating PI3K/AKT/mTOR-Mediated Autophagy in Non-Small Cell Lung Cancer Cells. Int. J. Mol. Sci. 2023, 24, 12626. https://doi.org/10.3390/ijms241612626
Wu Z, Li W, Tang Q, Huang L, Zhan Z, Li Y, Wang G, Dai X, Zhang Y. A Novel Aniline Derivative from Peganum harmala L. Promoted Apoptosis via Activating PI3K/AKT/mTOR-Mediated Autophagy in Non-Small Cell Lung Cancer Cells. International Journal of Molecular Sciences. 2023; 24(16):12626. https://doi.org/10.3390/ijms241612626
Chicago/Turabian StyleWu, Zhongnan, Wen Li, Qing Tang, Laiqiang Huang, Zhaochun Zhan, Yaolan Li, Guocai Wang, Xiaoyong Dai, and Yubo Zhang. 2023. "A Novel Aniline Derivative from Peganum harmala L. Promoted Apoptosis via Activating PI3K/AKT/mTOR-Mediated Autophagy in Non-Small Cell Lung Cancer Cells" International Journal of Molecular Sciences 24, no. 16: 12626. https://doi.org/10.3390/ijms241612626




