Epstein–Barr Virus Infection Is Associated with Elevated Hepcidin Levels
Abstract
:1. Introduction
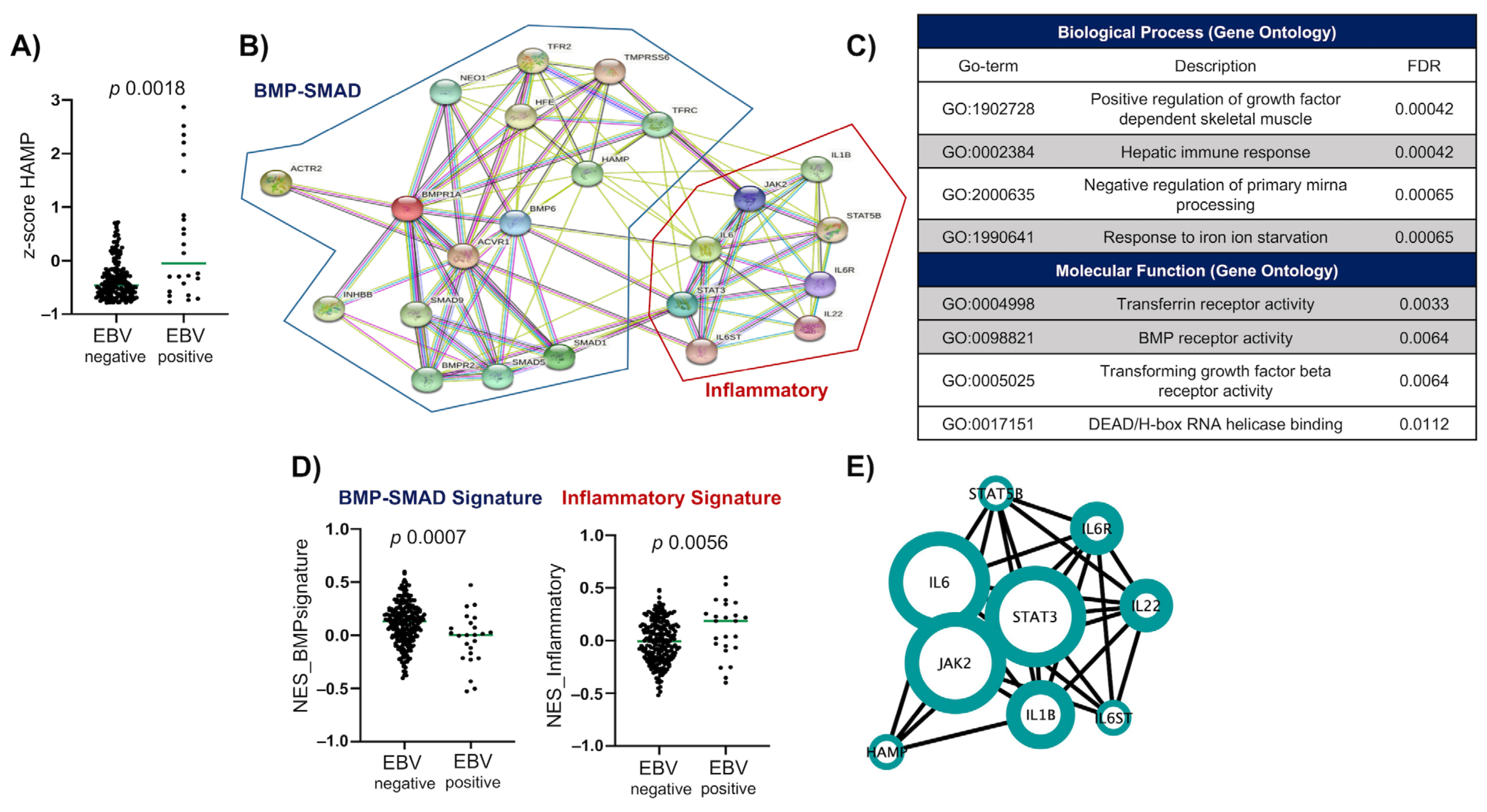
2. Results
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Study Population
4.2. Sample Collection
4.3. Determination of H. pylori Infection
4.4. Determination of Anti-EBV VCA Antibodies
4.5. Determination of Hematological Parameters
4.6. Anthropometric Indicators
4.7. TCGA Data Analysis
4.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| AGP | α-1 glycoprotein |
| A1GB | Gene that encodes to the α-1 glycoprotein |
| ATP | Adenosine 5′-triphosphate |
| BMI | Body mass index |
| BMP6 | Gene that encodes to the Bone morphogenetic protein 6 |
| BMPRII | Gene that encodes to the Bone morphogenetic protein receptor II |
| BMP–SMAD | Bone morphogenetic proteins and suppressor of mothers against decapentaplegic 2 signaling pathways |
| CagA | Cytotoxin-associated gene A |
| cBioportal | Tool for visualizing and analyzing cancer genomics data. |
| CRP | Gene that encodes to the C-reactive protein |
| CRP | C-reactive protein |
| DMT1 | Gene that encodes to the Divalent metal transporter 1 |
| EA | Early antigen of EBV |
| EA-IgG | IgG antibodies directed against the early antigen of EBV |
| EBNA1 | Epstein–Barr nuclear antigen1 |
| EBNA1-IgG | IgG antibodies directed against the Epstein–Barr nuclear antigen1 |
| EBV | Epstein–Barr virus |
| EBVaGC | Epstein–Barr virus associated gastric carcinoma |
| EBVnGC | Epstein–Barr virus negative gastric carcinoma |
| EDTA | Ethylenediamine tetraacetic acid |
| ELISA | Enzyme-linked immunosorbent assay |
| FDR | Fold discovery rate |
| GO | Gene ontology |
| GSVA | Gene set variation analysis |
| HAMP | Gene that encodes for Hepcidin |
| Hb | Hemoglobin |
| HBV | Hepatitis B virus. |
| HCMV | Human Cytomegalovirus |
| HCP1 | Gene that encodes for the Heme carrier protein 1 transporter |
| HFE | Gene that encodes for the Homeostatic iron regulator |
| HFE | Homeostatic iron regulator protein |
| HIF1A | Gene that encodes for the transcription factor Hypoxia-inducible factor 1 subunit alpha |
| HIV-1 | Human immunodeficiency virus 1 |
| HJV | Gene that encodes to the Hemojuvelin |
| H. pylori | Helicobacter pylori |
| IARC | International Agency for Research on Cancer |
| ID | Iron deficiency |
| IDA | Iron deficiency anemia |
| IgG | Immunoglobulin G |
| IgM | Immunoglobulin M |
| IL-1β | Interleukin 1 beta |
| IL-6 | Gene that encodes to the Interleukin 6 |
| IL-6 | Interleukin 6 |
| IL-6R | Interleukin 6 Receptor |
| IL-6ST | Interleukin 6 Cytokine Family Signal Transducer |
| IL-22 | Interleukin 22 |
| IRP-1 | Gene that encodes for the Iron-regulatory protein 1 |
| IRP-2 | Gene that encodes for the Iron-regulatory protein 2 |
| JAK2 | Janus kinase 2 |
| JAK/STAT | Janus kinases (JAK) and signal transducer and activator of transcription proteins (STAT) pathways |
| NES | Normalized enrichment score |
| NF-kB | Nuclear factor-kappa B |
| ODR | Optical density radio |
| PPI | Protein-protein interaction |
| RTA | Replication and transcription activator of EBV |
| ROUT | Robust regression and outlier removal test |
| SARS-CoV-2 | Severe acute respiratory syndrome Coronavirus 2 |
| SD | Standard deviation |
| SLC40A1 | Gene that encodes for the Iron exporter ferroportin 1 |
| SMAD4 | Gene that encodes for the SMAD family member 4 |
| STAT3 | Signal transducer and activator of transcription 3 |
| STAT5B | Signal transducer and activator of transcription 5B |
| STEAP1 | Gene that encodes to the Transmembrane epithelial antigen of the prostate protein 1 |
| STEAP2 | Gene that encodes for the transmembrane epithelial antigen of the prostate protein 2 |
| STEAP3 | Gene that encodes for the Transmembrane epithelial antigen of the prostate protein 3 |
| STEAP4 | Gene that encodes for the Transmembrane epithelial antigen of the prostate protein 4 |
| STRING | Search tool for the retrieval of interacting genes/proteins |
| ssGSEA | Single-sample gene set enrichment analysis |
| TCGA | The Cancer Genome Atlas |
| TFRC | Gene that encodes for the Transferrin receptor 1 |
| TFRC2 | Gene that encodes for the Transferrin receptor 2 |
| TLR4 | Toll like receptor 4 |
| TLR5 | Toll like receptor 5 |
| TMB | 3,3′,5,5′ Tetramethylbenzidin |
| TMPRSS6 | Gene that encodes for the Matriptase 2 |
| UBT | 13C-Urea breath test |
| US2 | Glycoprotein US2 from HCMV |
| VCA | Viral capsid antigen of EBV |
| VCA-IgG | IgG antibodies directed against Viral capsid antigen of EBV |
| VCA-IgM | IgM antibodies directed against Viral capsid antigen of EBV |
| WHO | World Health Organization |
References
- Zamani, M.; Ebrahimtabar, F.; Zamani, V.; Miller, W.H.; Alizadeh-Navaei, R.; Shokri-Shirvani, J.; Derakhshan, M.H. Systematic review with meta-analysis: The worldwide prevalence of Helicobacter pylori infection. Aliment. Pharmacol. Ther. 2018, 47, 868–876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dowd, J.B.; Palermo, T.; Brite, J.; McDade, T.W.; Aiello, A. Seroprevalence of Epstein-Barr Virus Infection in U.S. Children Ages 6–19, 2003–2010. PLoS ONE 2013, 8, e64921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IARC Working Group. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Biological Agents. IARC Monogr. Eval. Carcinog. Risks Hum. 2012, 100, 1–441. [Google Scholar]
- Wroblewski, L.E.; Peek, R.M., Jr.; Wilson, K.T. Helicobacter pylori and Gastric Cancer: Factors That Modulate Disease Risk. Clin. Microbiol. Rev. 2010, 23, 713–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Correa, P.; Piazuelo, M.B. The gastric precancerous cascade. J. Dig. Dis. 2012, 13, 2–9. [Google Scholar] [CrossRef] [Green Version]
- Bass, A.J.; Thorsson, V.; Shmulevich, I.; Reynolds, S.M.; Miller, M.; Bernard, B.; Hinoue, T.; Laird, P.W.; Curtis, C.; et al.; The Cancer Genome Atlas Research Network Comprehensive molecular characterization of gastric adenocarcinoma. Nature 2014, 513, 202–209. [Google Scholar]
- Yang, J.; Liu, Z.; Zeng, B.; Hu, G.; Gan, R. Epstein–Barr virus-associated gastric cancer: A distinct subtype. Cancer Lett. 2020, 495, 191–199. [Google Scholar] [CrossRef]
- Murata, T.; Sugimoto, A.; Inagaki, T.; Yanagi, Y.; Watanabe, T.; Sato, Y.; Kimura, H. Molecular Basis of Epstein–Barr Virus Latency Establishment and Lytic Reactivation. Viruses 2021, 13, 2344. [Google Scholar] [CrossRef]
- Murata, T.; Tsurumi, T. Switching of EBV cycles between latent and lytic states. Rev. Med. Virol. 2013, 24, 142–153. [Google Scholar] [CrossRef]
- Damania, B.; Kenney, S.C.; Raab-Traub, N. Epstein-Barr virus: Biology and clinical disease. Cell 2022, 185, 3652–3670. [Google Scholar] [CrossRef]
- Shannon-Lowe, C.; Rickinson, A. The Global Landscape of EBV-Associated Tumors. Front. Oncol. 2019, 9, 713. [Google Scholar] [CrossRef] [Green Version]
- McKenzie, J.; El-Guindy, A. Epstein-Barr Virus Lytic Cycle Reactivation. Poxviruses 2015, 391, 237–261. [Google Scholar] [CrossRef]
- Sinha, S.; Dickey, B.L.; Coghill, A.E. Utility of Epstein-Barr virus (EBV) antibodies as screening markers for nasopharyngeal carcinoma: A narrative review. Ann. Nasopharynx Cancer 2022, 6, 6. [Google Scholar] [CrossRef]
- Cárdenas-Mondragón, M.G.; Torres, J.; Flores-Luna, L.; Camorlinga-Ponce, M.; Carreón-Talavera, R.; Gomez-Delgado, A.; Kasamatsu, E.; Fuentes-Pananá, E.M. Case–control study of Epstein–Barr virus and Helicobacter pylori serology in Latin American patients with gastric disease. Br. J. Cancer 2015, 112, 1866–1873. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Ponce, Y.; Fuentes-Pananá, E. The Role of Coinfections in the EBV–Host Broken Equilibrium. Viruses 2021, 13, 1399. [Google Scholar] [CrossRef]
- Carabotti, M.; Annibale, B.; Lahner, E. Common Pitfalls in the Management of Patients with Micronutrient Deficiency: Keep in Mind the Stomach. Nutrients 2021, 13, 208. [Google Scholar] [CrossRef]
- Qu, X.; Huang, X.-L.; Xiong, P.; Zhu, C.-Y.; Huang, Y.-L.; Lu, L.-G.; Sun, X.; Rong, L.; Zhong, L.; Sun, D.-Y.; et al. Does Helicobacter pylori infection play a role in iron deficiency anemia? A meta-analysis. World J. Gastroenterol. 2010, 16, 886–896. [Google Scholar] [CrossRef]
- Wenzhen, Y.; Yumin, L.; Kehu, Y.; Bin, M.; Quanlin, G.; Donghai, W.; Lijuan, Y. Iron deficiency anemia in Helicobacter pylori infection: Meta-analysis of randomized controlled trials. Scand. J. Gastroenterol. 2010, 45, 665–676. [Google Scholar] [CrossRef]
- Annibale, B.; Marignani, M.; Monarca, B.; Antonelli, G.; Marcheggiano, A.; Martino, G.; Mandelli, F.; Caprilli, R.; Fave, G.D. Reversal of Iron Deficiency Anemia after Helicobacter pylori Eradication in Patients with Asymptomatic Gastritis. Ann. Intern. Med. 1999, 131, 668–672. [Google Scholar] [CrossRef]
- Burns, M.; Amaya, A.; Bodi, C.; Ge, Z.; Bakthavatchalu, V.; Ennis, K.; Wang, T.C.; Georgieff, M.; Fox, J.G. Helicobacter pylori infection and low dietary iron alter behavior, induce iron deficiency anemia, and modulate hippocampal gene expression in female C57BL/6 mice. PLoS ONE 2017, 12, e0173108. [Google Scholar] [CrossRef] [Green Version]
- Smolka, A.J.; Schubert, M.L. Helicobacter Pylori-Induced Changes in Gastric Acid Secretion and Upper Gastrointestinal Disease. In Molecular Pathogenesis and Signal Transduction by Helicobacter pylori; Tegtmeyer, N., Backert, S., Eds.; Current Topics in Microbiology and Immunology; Springer International Publishing: Cham, Switzerland, 2017; Volume 400, pp. 227–252. ISBN 978-3-319-50519-0. [Google Scholar]
- Sapmaz, F.; Basyigit, S.; Kısa; Kavak, E.E.; Guliter, S.; Kalkan, I.H. The impact of Helicobacter pylori eradication on serum hepcidin-25 level and iron parameters in patients with iron deficiency anemia. Wien. Klin. Wochenschr. 2016, 128, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Azab, S.F.A.; Esh, A.M.H. Serum hepcidin levels in Helicobacter pylori-infected children with iron-deficiency anemia: A case-control study. Ann. Hematol. 2013, 92, 1477–1483. [Google Scholar] [CrossRef] [PubMed]
- Nemeth, E.; Tuttle, M.S.; Powelson, J.; Vaughn, M.B.; Donovan, A.; Ward, D.M.V.; Ganz, T.; Kaplan, J. Hepcidin Regulates Cellular Iron Efflux by Binding to Ferroportin and Inducing Its Internalization. Science 2004, 306, 2090–2093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganz, T. Hepcidin and iron regulation, 10 years later. Blood 2011, 117, 4425–4433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nemeth, E.; Rivera, S.; Gabayan, V.; Keller, C.; Taudorf, S.; Pedersen, B.K.; Ganz, T. IL-6 mediates hypoferremia of in-flammation by inducing the synthesis of the iron regulatory hormone hepcidin. J. Clin. Invest. 2004, 113, 1271–1276. [Google Scholar] [CrossRef] [Green Version]
- Kanamori, Y.; Murakami, M.; Sugiyama, M.; Hashimoto, O.; Matsui, T.; Funaba, M. Interleukin-1β (IL-1β) transcriptionally activates hepcidin by inducing CCAAT enhancer-binding protein δ (C/EBPδ) expression in hepatocytes. J. Biol. Chem. 2017, 292, 10275–10287. [Google Scholar] [CrossRef] [Green Version]
- Wieringa, F.T.; Dijkhuizen, M.A.; West, C.E.; Northrop-Clewes, C.A. Muhilal Estimation of the Effect of the Acute Phase Response on Indicators of Micronutrient Status in Indonesian Infants. J. Nutr. 2002, 132, 3061–3066. [Google Scholar] [CrossRef] [Green Version]
- Münz, C. Latency and lytic replication in Epstein–Barr virus-associated oncogenesis. Nat. Rev. Genet. 2019, 17, 691–700. [Google Scholar] [CrossRef] [Green Version]
- Bánáti, F.; Koroknai, A.; Szenthe, K. Terminal Repeat Analysis of EBV Genomes. Methods Mol. Biol. 2016, 1532, 169–177. [Google Scholar] [CrossRef]
- Gulley, M.L.; Pulitzer, D.R.; A Eagan, P.; Schneider, B. Epstein-barr virus infection is an early event in gastric carcinogenesis and is independent of bcl-2 expression and p53 accumulation. Hum. Pathol. 1996, 27, 20–27. [Google Scholar] [CrossRef]
- Fan, H.; Gulley, M.L. Molecular Methods for Detecting Epstein-Barr Virus (Part II): Structural Analysis of Epstein-Barr Virus DNA as a Marker of Clonality. Methods Mol. Biol. 2001, 49, 313–319. [Google Scholar] [CrossRef]
- Cárdenas-Mondragón, M.G.; Carreón-Talavera, R.; Camorlinga-Ponce, M.; Gomez-Delgado, A.; Torres, J.; Fuentes-Pananá, E.M. Epstein Barr Virus and Helicobacter pylori Co-Infection Are Positively Associated with Severe Gastritis in Pediatric Patients. PLoS ONE 2013, 8, e62850. [Google Scholar] [CrossRef]
- Martínez-López, J.L.; Torres, J.; Camorlinga-Ponce, M.; Mantilla, A.; Leal, Y.A.; Fuentes-Pananá, E.M. Evidence of Epstein-Barr Virus Association with Gastric Cancer and Non-Atrophic Gastritis. Viruses 2014, 6, 301–318. [Google Scholar] [CrossRef] [Green Version]
- Dávila-Collado, R.; Jarquín-Durán, O.; Dong, L.T.; Espinoza, J.L. Epstein–Barr Virus and Helicobacter pylori Co-Infection in Non-Malignant Gastroduodenal Disorders. Pathogens 2020, 9, 104. [Google Scholar] [CrossRef] [Green Version]
- Cárdenas-Mondragón, M.G.; Torres, J.; Flores-Luna, L.; Carreón-Talavera, R.; Camorlinga-Ponce, M.; Fuentes-Pananá, E.M. Epstein-Barr Virus Association with Peptic Ulcer Disease. Anal. Cell. Pathol. 2015, 2015, 164840. [Google Scholar] [CrossRef] [Green Version]
- Saxena, A.; Prasad, K.N.; Ghoshal, U.C.; Krishnani, N.; Bhagat, M.R.; Husain, N. Association of Helicobacter pylori and Epstein-Barr virus with gastric cancer and peptic ulcer disease. Scand. J. Gastroenterol. 2008, 43, 669–674. [Google Scholar] [CrossRef]
- Saju, P.; Murata-Kamiya, N.; Hayashi, T.; Senda, Y.; Nagase, L.; Noda, S.; Matsusaka, K.; Funata, S.; Kunita, A.; Urabe, M.; et al. Host SHP1 phosphatase antagonizes Helicobacter pylori CagA and can be downregulated by Epstein–Barr virus. Nat. Microbiol. 2016, 1, 16026. [Google Scholar] [CrossRef]
- Zong, L.; Seto, Y. CpG Island Methylator Phenotype, Helicobacter pylori, Epstein-Barr Virus, and Microsatellite Instability and Prognosis in Gastric Cancer: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e86097. [Google Scholar] [CrossRef]
- Wu, W.K.; Yu, J.; Chan, M.T.; To, K.F.; Cheng, A.S. Combinatorial epigenetic deregulation by Helicobacter pylori and Epstein-Barr virus infections in gastric tumourigenesis. J. Pathol. 2016, 239, 245–249. [Google Scholar] [CrossRef] [Green Version]
- Shukla, S.K.; Prasad, K.N.; Tripathi, A.; Singh, A.; Saxena, A.; Ghoshal, U.C.; Krishnani, N.; Husain, N. Epstein-Barr Virus DNA Load and Its Association with Helicobacter pylori Infection in Gastroduodenal Diseases. Braz. J. Infect Dis. 2011, 15, 583–590. [Google Scholar] [CrossRef] [Green Version]
- Minoura-Etoh, J.; Gotoh, K.; Sato, R.; Ogata, M.; Kaku, N.; Fujioka, T.; Nishizono, A. Helicobacter pylori-associated oxidant monochloramine induces reactivation of Epstein–Barr virus (EBV) in gastric epithelial cells latently infected with EBV. J. Med Microbiol. 2006, 55, 905–911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pandey, S.; Jha, H.C.; Shukla, S.K.; Shirley, M.K.; Robertson, E.S. Epigenetic Regulation of Tumor Suppressors by Helicobacter pylori Enhances EBV-Induced Proliferation of Gastric Epithelial Cells. mBio 2018, 9, e00649-18. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas-Mondragón, M.G.; Torres, J.; Sánchez-Zauco, N.; Gómez-Delgado, A.; Camorlinga-Ponce, M.; Maldonado-Bernal, C.; Fuentes-Pananá, E.M. Elevated Levels of Interferon-γ Are Associated with High Levels of Epstein-Barr Virus Reactivation in Patients with the Intestinal Type of Gastric Cancer. J. Immunol. Res. 2017, 2017, 7069242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Growth Reference Data for School-Aged Children and Adolescents of 5–19 Years. Available online: http://www.who.int/growthref/en/ (accessed on 15 July 2022).
- Mendoza, E.; Duque, X.; Franco, J.I.H.; Maldonado, E.R.; Morán, S.; Martínez, G.; Rodríguez, A.S.; Martínez, H. Association between Active H. pylori Infection and Iron Deficiency Assessed by Serum Hepcidin Levels in School-Age Children. Nutrients 2019, 11, 2141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bille, B.B.E.; Mabeku, L.B.K. Relationship between active Helicobacter pylori infection and anemia, iron deficiency, iron deficiency anemia: A cross-sectional study in a sub-Saharan setting. JGH Open 2022, 6, 554–568. [Google Scholar] [CrossRef]
- Hudak, L.; Jaraisy, A.; Haj, S.; Muhsen, K. An updated systematic review and meta-analysis on the association between Helicobacter pylori infection and iron deficiency anemia. Helicobacter 2017, 22, e12330. [Google Scholar] [CrossRef]
- Chhabra, R.; Saha, A.; Chamani, A.; Schneider, N.; Shah, R.; Nanjundan, M. Iron Pathways and Iron Chelation Approaches in Viral, Microbial, and Fungal Infections. Pharmaceuticals 2020, 13, E275. [Google Scholar] [CrossRef]
- Lehmann, C.D.; Scott, C.R.; E Holbein, B. Iron should be restricted in acute infection. Front. Biosci. 2020, 25, 673–682. [Google Scholar] [CrossRef]
- Carver, P.L. The Battle for Iron between Humans and Microbes. Curr. Med. Chem. 2018, 25, 85–96. [Google Scholar] [CrossRef]
- Enko, D.; Wagner, H.; Kriegshäuser, G.; Wögerer, J.; Halwachs-Baumann, G.; Schnedl, W.J.; Zelzer, S.; Fauler, G.; Mangge, H.; Markus, H.; et al. Iron status determination in individuals with Helicobacter pylori infection: Conventional vs. new laboratory biomarkers. Clin. Chem. Lab. Med. (CCLM) 2019, 57, 982–989. [Google Scholar] [CrossRef]
- WHO. Global Anaemia Reduction Efforts among Women of Reproductive Age: Impact, Achievment of Targets and the Way Forward for Optimizing Efforts; World Healt Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-001220-2. [Google Scholar]
- Weiss, G. Modification of iron regulation by the inflammatory response. Best Pract. Res. Clin. Haematol. 2005, 18, 183–201. [Google Scholar] [CrossRef]
- Agarwal, N.; Prchal, J.T. Anemia of Chronic Disease (Anemia of Inflammation). Acta Haematol. 2009, 122, 103–108. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, S.; Nekhai, S.; Liu, S. Depriving Iron Supply to the Virus Represents a Promising Adjuvant Therapeutic Against Viral Survival. Curr. Clin. Microbiol. Rep. 2020, 7, 13–19. [Google Scholar] [CrossRef]
- Ben-Arieh, S.V.; Zimerman, B.; Smorodinsky, N.I.; Yaacubovicz, M.; Schechter, C.; Bacik, I.; Gibbs, J.; Bennink, J.R.; Yewdell, J.W.; Coligan, J.E.; et al. Human Cytomegalovirus Protein US2 Interferes with the Expression of Human HFE, a Nonclassical Class I Major Histocompatibility Complex Molecule That Regulates Iron Homeostasis. J. Virol. 2001, 75, 10557–10562. [Google Scholar] [CrossRef] [Green Version]
- Mao, W.; Hu, Y.; Lou, Y.; Chen, Y.; Zhang, J. Abnormal serum iron markers in chronic hepatitis B virus infection may be because of liver injury. Eur. J. Gastroenterol. Hepatol. 2015, 27, 130–136. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.-H.; Cheng, P.-P.; Jiang, F.; Jiao, X.-Y. The effect of hepatitis B virus infection on hepcidin expression in hepatitis B patients. Ann. Clin. Lab. Sci. 2013, 43, 126–134. [Google Scholar]
- Xu, M.; Kashanchi, F.; Foster, A.; Rotimi, J.; Turner, W.; Gordeuk, V.R.; Nekhai, S. Hepcidin induces HIV-1 transcription inhibited by ferroportin. Retrovirology 2010, 7, 104. [Google Scholar] [CrossRef] [Green Version]
- Drakesmith, A.; Prentice, A. Viral infection and iron metabolism. Nat. Rev. Genet. 2008, 6, 541–552. [Google Scholar] [CrossRef]
- Biasiotto, G.; Ferrari, F. Covidin, a possible new player between hepcidin and ferroportin in hypoxia and inflammation caused by COVID-19. J. Cell. Biochem. 2022, 123, 1701–1703. [Google Scholar] [CrossRef]
- Wang, Z.; Lv, Z.; Ding, H.; Xu, Q.; Sun, L.; Jing, J.; Yuan, Y. Role of serum EBV-VCA IgG detection in assessing gastric cancer risk and prognosis in Northern Chinese population. Cancer Med. 2018, 7, 5760–5774. [Google Scholar] [CrossRef] [Green Version]
- Shinkura, R.; Yamamoto, N.; Koriyama, C.; Shinmura, Y.; Eizuru, Y.; Tokunaga, M. Epstein-Barr virus-specific antibodies in Epstein-Barr virus-positive and -negative gastric carcinoma cases in Japan. J. Med. Virol. 2000, 60, 411–416. [Google Scholar] [CrossRef]
- Guo, J.; Cui, Z.; Zheng, Y.; Li, X.; Chen, Y. Comparison of Epstein-Barr Virus Serological Tools for the Screening and Risk Assessment of Nasopharyngeal Carcinoma: A Large Population-based Study. Pathol. Oncol. Res. 2020, 26, 2185–2190. [Google Scholar] [CrossRef] [PubMed]
- Yiu, S.P.T.; Hui, K.F.; Choi, C.K.; Kao, R.Y.T.; Ma, C.W.; Yang, D.; Chiang, A.K.S. Intracellular Iron Chelation by a Novel Compound, C7, Reactivates Epstein–Barr Virus (EBV) Lytic Cycle via the ERK-Autophagy Axis in EBV-Positive Epithelial Cancers. Cancers 2018, 10, 505. [Google Scholar] [CrossRef] [PubMed]
- Nairz, M.; Haschka, D.; Demetz, E.; Weiss, G. Iron at the interface of immunity and infection. Front. Pharmacol. 2014, 5, 152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nairz, M.; Weiss, G. Iron in infection and immunity. Mol. Asp. Med. 2020, 75, 100864. [Google Scholar] [CrossRef]
- Bode, J.G.; Albrecht, U.; Häussinger, D.; Heinrich, P.C.; Schaper, F. Hepatic acute phase proteins—Regulation by IL-6- and IL-1-type cytokines involving STAT3 and its crosstalk with NF-κB-dependent signaling. Eur. J. Cell Biol. 2012, 91, 496–505. [Google Scholar] [CrossRef]
- Gao, R.; Wang, L.; Bai, T.; Zhang, Y.; Bo, H.; Shu, Y. C-Reactive Protein Mediating Immunopathological Lesions: A Potential Treatment Option for Severe Influenza A Diseases. eBioMedicine 2017, 22, 133–142. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez, R.; Jung, C.-L.; Gabayan, V.; Deng, J.C.; Ganz, T.; Nemeth, E.; Bulut, Y. Hepcidin Induction by Pathogens and Pathogen-Derived Molecules Is Strongly Dependent on Interleukin-6. Infect. Immun. 2014, 82, 745–752. [Google Scholar] [CrossRef] [Green Version]
- Williams, A.M.; Ladva, C.N.; Leon, J.S.; A Lopman, B.; Tangpricha, V.; Whitehead, R.D.; E Armitage, A.; Wray, K.; Morovat, A.; Pasricha, S.-R.; et al. Changes in micronutrient and inflammation serum biomarker concentrations after a norovirus human challenge. Am. J. Clin. Nutr. 2019, 110, 1456–1464. [Google Scholar] [CrossRef] [Green Version]
- Peyssonnaux, C.; Zinkernagel, A.S.; Datta, V.; Lauth, X.; Johnson, R.S.; Nizet, V. TLR4-dependent hepcidin expression by myeloid cells in response to bacterial pathogens. Blood 2006, 107, 3727–3732. [Google Scholar] [CrossRef] [Green Version]
- Armitage, A.E.; Eddowes, L.A.; Gileadi, U.; Cole, S.; Spottiswoode, N.; Selvakumar, T.A.; Ho, L.-P.; Townsend, A.R.M.; Drakesmith, H. Hepcidin regulation by innate immune and infectious stimuli. Blood 2011, 118, 4129–4139. [Google Scholar] [CrossRef] [Green Version]
- Gupta, Y.; Maciorowski, D.; Medernach, B.; Becker, D.P.; Durvasula, R.; Libertin, C.R.; Kempaiah, P. Iron dysregulation in COVID-19 and reciprocal evolution of SARS-CoV-2: Natura nihil frustra facit. J. Cell. Biochem. 2022, 123, 601–619. [Google Scholar] [CrossRef]
- Gosselin, J.; Flamand, L.; D’Addario, M.; Hiscott, J.; Menezes, J. Infection of peripheral blood mononuclear cells by herpes simplex and Epstein-Barr viruses. Differential induction of interleukin 6 and tumor necrosis factor-alpha. J. Clin. Investig. 1992, 89, 1849–1856. [Google Scholar] [CrossRef]
- Wada, T.; Muraoka, M.; Yokoyama, T.; Toma, T.; Kanegane, H.; Yachie, A. Cytokine profiles in children with primary Epstein-Barr virus infection. Pediatr. Blood Cancer 2013, 60, E46–E48. [Google Scholar] [CrossRef] [Green Version]
- Rojas-Rechy, M.H.; Gaytán-Morales, F.; Sánchez-Ponce, Y.; Castorena-Villa, I.; López-Martínez, B.; Parra-Ortega, I.; Escamilla-Núñez, M.C.; Méndez-Tenorio, A.; Pompa-Mera, E.N.; Martinez-Ruiz, G.U.; et al. Herpesvirus Screening in Childhood Hematopoietic Transplant Reveals High Systemic Inflammation in Episodes of Multiple Viral Detection and an EBV Association with Elevated IL-1β, IL-8 and Graft-Versus-Host Disease. Microorganisms 2022, 10, 1685. [Google Scholar] [CrossRef]
- Mirowska-Guzel, D.; Gromadzka, G.; Mach, A.; Członkowski, A.; Czlonkowska, A. Association of IL1A, IL1B, ILRN, IL6, IL10 and TNF-α polymorphisms with risk and clinical course of multiple sclerosis in a Polish population. J. Neuroimmunol. 2011, 236, 87–92. [Google Scholar] [CrossRef]
- Costa, G.D.; Finardi, A.; Garzetti, L.; Carandini, T.; Comi, G.; Martinelli, V.; Furlan, R. Disease-modifying treatments modulate myeloid cells in multiple sclerosis patients. Neurol. Sci. 2017, 39, 373–376. [Google Scholar] [CrossRef]
- Kianfar, R.; Ravanshad, M.; Ghiass, M.A.; Rafiee, N.; Shayeghpour, A.; Maleki, A. Evaluation of IL-1β and IL-6 Expression following EBNA-1 and BRLF-1 Peptide Treatment in Epstein-Barr Virus-Positive Multiple Sclerosis Patients. Intervirology 2022, 65, 144–150. [Google Scholar] [CrossRef]
- Tung, K.-L.; Wu, Y.-T.; Liu, C.; Lin, S.-C.; Wu, C.-H.; Wu, S.-Y.; Chang, Y.; Lan, Y.-Y. EBV Rta-induced IL-6 Promotes Migration of Bystander Tumor Cells Through IL-6R/JAK/STAT3 Pathway In Vitro. Anticancer Res. 2020, 40, 3255–3264. [Google Scholar] [CrossRef]
- Huang, Y.-T.; Liu, M.-Y.; Tsai, C.-H.; Yeh, T.-H. Upregulation of interleukin-1 by Epstein-Barr virus latent membrane protein 1 and its possible role in nasopharyngeal carcinoma cell growth. Head Neck 2009, 32, 869–876. [Google Scholar] [CrossRef]
- Morales-Sánchez, A.; Torres, J.; Cardenas-Mondragón, M.G.; Romo-González, C.; Camorlinga-Ponce, M.; Flores-Luna, L.; Fuentes-Pananá, E.M. Detection of Epstein-Barr Virus DNA in Gastric Biopsies of Pediatric Patients with Dyspepsia. Pathogens 2020, 9, 623. [Google Scholar] [CrossRef] [PubMed]
- Drakesmith, H.; Prentice, A.M.; Parducci, L.; Edwards, M.E.; Bennett, K.D.; Alm, T.; Elverland, E.; Tollefsrud, M.M.; Jørgensen, T.; Houmark-Nielsen, M.; et al. Hepcidin and the Iron-Infection Axis. Science 2012, 338, 768–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vilchis, J.; Navarro, F.; Mera, R.; Torres, J.; Correa, P.; Kageyama-Escobar, M.D.L.L.; Duque, X.; Mendoza, E.; González-Cossío, T.; Morán, S.; et al. Association of Helicobacter pylori Infection and Height of Mexican Children of Low Socioeconomic Level Attending Boarding Schools. Am. J. Trop. Med. Hyg. 2009, 81, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Hino, B.; Eliakim, R.; Levine, A.; Sprecher, H.; Berkowitz, D.; Hartman, C.; Eshach-Adiv, O.; Shamir, R. Comparison of Invasive and Non-Invasive Tests Diagnosis and Monitoring of Helicobacter Pylori Infection in Children. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Goodman, K.J.; O’Rourke, K.; Day, R.S.; Wang, C.; Nurgalieva, Z.; Phillips, C.V.; Aragaki, C.; Campos, A.; de la Rosa, J.M. Dynamics of Helicobacter pylori infection in a US–Mexico cohort during the first two years of life. Leuk. Res. 2005, 34, 1348–1355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rowland, M.; Daly, L.; Vaughan, M.; Higgins, A.; Bourke, B.; Drumm, B. Age-Specific Incidence of Helicobacter pylori. Gastroenterology 2006, 130, 65–72. [Google Scholar] [CrossRef]
- Leal, Y.A.; Flores, L.L.; Fuentes-Pananá, E.M.; Cedillo-Rivera, R.; Torres, J. 13C-Urea Breath Test for the Diagnosis of Helicobacter pylori Infection in Children: A Systematic Review and Meta-Analysis. Helicobacter 2011, 16, 327–337. [Google Scholar] [CrossRef]
- Camorlinga-Ponce, M.; Torres, J.; Perez, G.P.; Leal-Herrera, Y.; Gonzalez-Ortiz, B.; A de la Garza, M.; Gomez, A.; Muñoz, O. Validation of a Serologic Test for the Diagnosis of Helicobacter pylori Infection and the Immune Response to Urease and CagA in Children. Am. J. Gastroenterol. 1998, 93, 1264–1270. [Google Scholar] [CrossRef]
- Cohen, J.H.; Haas, J.D. Hemoglobin correction factors for estimating the prevalence of iron deficiency anemia in pregnant women residing at high altitudes in Bolivia. Rev. Panam. Salud Pública 1999, 6, 392–399. [Google Scholar] [CrossRef] [Green Version]
- Lopez, A.; Cacoub, P.; Macdougall, I.C.; Peyrin-Biroulet, L. Iron deficiency anaemia. Lancet 2015, 387, 907–916. [Google Scholar] [CrossRef]
- Ganz, T.; Olbina, G.; Girelli, D.; Nemeth, E.; Westerman, M. Immunoassay for human serum hepcidin. Blood 2008, 112, 4292–4297. [Google Scholar] [CrossRef] [Green Version]
- Kroot, J.J.; Kemna, E.H.; Bansal, S.S.; Busbridge, M.; Campostrini, N.; Girelli, D.; Hider, R.C.; Koliaraki, V.; Mamalaki, A.; Olbina, G.; et al. Results of the first international round robin for the quantification of urinary and plasma hepcidin assays: Need for standardization. Haematologica 2009, 94, 1748–1752. [Google Scholar] [CrossRef] [Green Version]
- Van der Vorm, L.; Hendriks, J.C.; Laarakkers, C.M.; Klaver, S.; Armitage, A.E.; Bamberg, A.; Geurts-Moespot, A.J.; Girelli, D.; Herkert, M.; Itkonen, O.; et al. Toward Worldwide Hepcidin Assay Harmonization: Identification of a Commutable Secondary Reference Material. Clin. Chem. 2016, 62, 993–1001. [Google Scholar] [CrossRef]
- A Northrop-Clewes, C. Interpreting indicators of iron status during an acute phase response—Lessons from malaria and human immunodeficiency virus. Ann. Clin. Biochem. Int. J. Lab. Med. 2008, 45, 18–32. [Google Scholar] [CrossRef]
- WHO AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescents. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/application-tools (accessed on 15 July 2022).
- Ganz, T.; Nemeth, E. Hepcidin and iron homeostasis. Biochim. Biophys. Acta (BBA) Mol. Cell Res. 2012, 1823, 1434–1443. [Google Scholar] [CrossRef] [Green Version]
- Forciniti, S.; Greco, L.; Grizzi, F.; Malesci, A.; Laghi, L. Iron Metabolism in Cancer Progression. Int. J. Mol. Sci. 2020, 21, 2257. [Google Scholar] [CrossRef]


| Characteristics | N (145) | % |
|---|---|---|
| Age, years, mean ± SD | 9.3 ± 1.7 | |
| Sex Girls Boys | 70 75 | 48.3 51.7 |
| Socio-economic level High margination a Middle or lower margination | 86 56 | 60.6 39.4 |
| Overcrowding <3 persons/room ≥3 persons/room | 79 65 | 54.9 45.1 |
| Body Mass Index-for-age (Z-score), mean ± SD b | 0.65 ± 1.02 | |
| Thinness Normal BMI-for-age Overweight Obesity | 1 95 33 16 | 0.7 65.5 22.8 11.0 |
| Height-for-age (Z-score), mean ± SD c | −0.41 ± 0.96 | |
| Normal Stunting | 137 8 | 94.5 5.5 |
| Iron nutritional status and infectious/inflammation indicators | ||
| Hemoglobin (g/dL), mean ± SD d | 14.2 ± 0.8 | |
| Normal hemoglobin Anemia | 144 1 | 99.3 0.7 |
| Ferritin (ng/mL), median (p25–p75) | 27.3 (19.6–41.7) | |
| Normal ferritin (≥15 ng/mL) Low iron stores (ferritin < 15 ng/mL) | 122 23 | 84.1 15.9 |
| Hepcidin (ng/mL), (median, p25–p75) * | 7.6 (3.6–13.5) | |
| α-1 AGP (g/L) * median (p25–p75) | 0.66 (0.51–0.83) | |
| Normal (<1 g/L) High (≥1 g/L) | 93 13 | 87.7 12.3 |
| C-reactive protein (mg/L) * median (p25–p75) | 0.00 (0.00–1.84) | |
| Normal (<5 mg/L) High (≥5 mg/L) | 91 14 | 86.7 13.3 |
| Inflammatory process e Inflammatory process− Inflammatory process+ | 88 17 | 83.8 16.2 |
| Infection Type | N = 145 | |
|---|---|---|
| N | % | |
| H. pylori Positive (UBT+ or ELISA+) Negative (UBT− and ELISA−) | 50 95 | 34.5 65.5 |
| CagA pathogenicity island Positive Negative | 29 111 | 20.7 79.3 |
| EBV infection Positive Negative | 133 12 | 91.7 8.3 |
| H. pylori and EBV infection H. pylori+/EBV infection+ H. pylori+/EBV infection− H. pylori−/EBV infection+ H. pylori−/EBV infection− | 47 3 86 9 | 32.4 2.1 59.1 6.2 |
| With H. pylori or EBV infection or Inflammatory process Without H. pylori, EBV infection and Inflammatory process | 135 7 | 95.1 4.9 |
| Infection | Ferritin (ng/mL) | C-Reactive Protein (mg/dL) | α-1 Glycoprotein (g/L) | Hepcidin (ng/mL) | ||
|---|---|---|---|---|---|---|
| N | Median (p25–p75) | N | Median (p25–p75) | |||
| EBV infection b With infection Without infection p-value a | 131 12 | 28.5 (19.4–42.1) 26.8 (21.7–32.1) 0.730 | 96 9 | 0.16 (0.00–2.34) 0.00 (0.00–0.00) 0.005 | 0.66 (0.55–0.88) 0.46 (0.33–0.54) 0.002 | 8.6 (3.7–13.6) 2.0 (1.7–3.9) 0.002 |
| Coinfection H. pylori+/EBV infection+ * H. pylori+/EBV infection– H. pylori−/EBV infection+ H. pylori−/EBV infection– p-value b | 46 3 85 9 | 25.6 (20.1–37.9) 20.2 (5.8–26.5) 29.4 (19.4–45.9) 29.5 (26.0–34.1) 0.687 | 41 2 56 7 | 0.32 (0.00–2.30) 0.00 (0.00–0.00) 0.00 (0.00–3.10) 0.00 (0.00–0.00) 0.054 | 0.66 (0.53–0.84) 0.31 (0.30–0.32) 0.68 (0.55–0.89) 0.50 (0.43–0.68) 0.069 | 8.9 (4.2–13.5) c 1.5 (1.4–1.6) 8.6 (3.7–13.7) d 2.1 (1.9–5.7) e 0.030 |
| With H. pylori or EBV infection or Inflammatory process Without H. pylori or EBV infection or Inflammatory process p-value a | 133 7 | 28.3 (19.4–41.7) 29.5 (26.0–34.1) 0.660 | 98 7 | 0.07 (0.00–2.33) 0.00 (0.00–0.00) 0.014 | 0.66 (0.53–0.88) 0.50 (0.43–0.68) 0.036 | 8.6 (3.7–13.6) 2.1 (1.9–5.7) 0.016 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duque, X.; Mendoza, E.; Morán, S.; Suárez-Arriaga, M.C.; Morales-Sánchez, A.; Fontes-Lemus, J.I.; Domínguez-Martínez, D.A.; Fuentes-Pananá, E.M. Epstein–Barr Virus Infection Is Associated with Elevated Hepcidin Levels. Int. J. Mol. Sci. 2023, 24, 1630. https://doi.org/10.3390/ijms24021630
Duque X, Mendoza E, Morán S, Suárez-Arriaga MC, Morales-Sánchez A, Fontes-Lemus JI, Domínguez-Martínez DA, Fuentes-Pananá EM. Epstein–Barr Virus Infection Is Associated with Elevated Hepcidin Levels. International Journal of Molecular Sciences. 2023; 24(2):1630. https://doi.org/10.3390/ijms24021630
Chicago/Turabian StyleDuque, Ximena, Eugenia Mendoza, Segundo Morán, Mayra C. Suárez-Arriaga, Abigail Morales-Sánchez, José I. Fontes-Lemus, Diana A. Domínguez-Martínez, and Ezequiel M. Fuentes-Pananá. 2023. "Epstein–Barr Virus Infection Is Associated with Elevated Hepcidin Levels" International Journal of Molecular Sciences 24, no. 2: 1630. https://doi.org/10.3390/ijms24021630
APA StyleDuque, X., Mendoza, E., Morán, S., Suárez-Arriaga, M. C., Morales-Sánchez, A., Fontes-Lemus, J. I., Domínguez-Martínez, D. A., & Fuentes-Pananá, E. M. (2023). Epstein–Barr Virus Infection Is Associated with Elevated Hepcidin Levels. International Journal of Molecular Sciences, 24(2), 1630. https://doi.org/10.3390/ijms24021630





