The Role of Serum Calprotectin in Defining Disease Outcomes in Non-Systemic Juvenile Idiopathic Arthritis: A Pilot Study
Abstract
:1. Introduction
2. Results
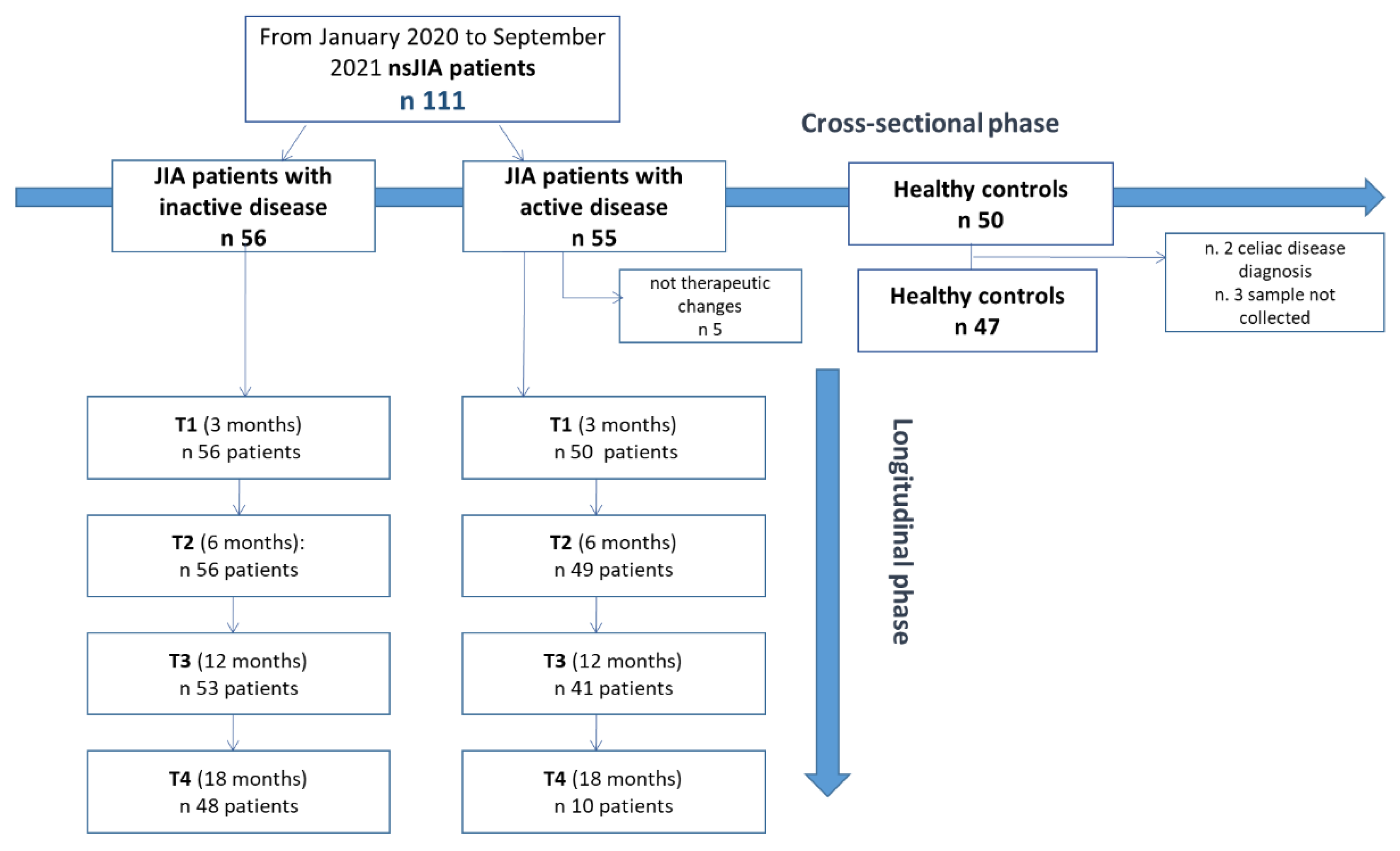
2.1. Study Design
2.2. Patient Characteristics at Baseline
2.3. Laboratory Characteristics and Calprotectin at Baseline
2.4. Survival Analysis and Cox Regression Model
3. Discussion
4. Materials and Method
4.1. Definitions
4.2. Clinical Assessment
4.3. Laboratory Examination
4.4. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eisenstein, E.M.; Berkun, Y. Diagnosis and classification of juvenile idiopathic arthritis. J. Autoimmun. 2014, 48–49, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Prakken, B.; Albani, S.; Martini, A. Juvenile idiopathic arthritis. Lancet 2011, 377, 2138–2149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinze, C.; Gohar, F.; Foell, D. Management of juvenile idiopathic arthritis: Hitting the target. Nat. Rev. Rheumatol. 2015, 11, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Guzman, J.; Oen, K.; Tucker, L.B.; Huber, A.M.; Shiff, N.; Boire, G.; Scuccimarri, R.; Berard, R.; Shirley, M.L.; Morishita, K.; et al. The outcomes of juvenile idiopathic arthritis in children managed with contemporary treatments: Results from the reacch-out cohort. Ann. Rheum. Dis. 2015, 74, 1854–1860. [Google Scholar] [CrossRef] [PubMed]
- Kearsley-Fleet, L.; Heaf, E.; Davies, R.; Baildam, E.; Beresford, M.W.; E Foster, H.; Southwood, T.R.; Thomson, W.; Hyrich, K.L. Frequency of biologic switching and the outcomes of switching in children and young people with juvenile idiopathic arthritis: A national cohort study. Lancet Rheumatol. 2020, 2, e217–e226. [Google Scholar] [CrossRef] [Green Version]
- Mourão, A.F.; Santos, M.J.; Gomes, J.A.M.; Martins, F.M.; Mendonça, S.C.; Ramos, F.O.; Fernandes, S.; Salgado, M.; Guedes, M.; Carvalho, S.; et al. Effectiveness and long-term retention of antitumour necrosis factor treatment in juvenile and adult patients with juvenile idiopathic arthritis: Data from Reuma.pt. Rheumatology 2016, 55, 697–703. [Google Scholar] [CrossRef] [Green Version]
- Wallace, C.A.; Giannini, E.H.; Huang, B.; Itert, L.; Ruperto, N. Childhood Arthritis Rheumatology Research Alliance; Pediatric Rheumatology Collaborative Study Group; Paediatric Rheumatology International Trials Organisation. American College of Rheumatology provisional criteria for defining clinical inactive disease in select categories of juvenile idiopathic arthritis. Arthritis Care Res. 2011, 63, 929–936. [Google Scholar]
- Thierry, S.; Fautrel, B.; Lemelle, I.; Guillemin, F. Prevalence and incidence of juvenile idiopathic arthritis: A systematic review. Jt. Bone Spine 2014, 81, 112–117. [Google Scholar] [CrossRef]
- Shoop-Worrall, S.J.W.; Wu, Q.; Davies, R.; Hyrich, K.L.; Wedderburn, L.R. Predicting disease outcomes in juvenile idiopathic arthritis: Challenges, evidence, and new directions. Lancet Child Adolesc. Health 2019, 3, 725–733. [Google Scholar] [CrossRef]
- Choida, V.; Hall-Craggs, M.; Jebson, B.R.; Fisher, C.; Leandro, M.; Wedderburn, L.R.; Ciurtin, C. Biomarkers of Response to Biologic Therapy in Juvenile Idiopathic Arthritis. Front. Pharmacol. 2021, 11, 635823. [Google Scholar] [CrossRef]
- Mariani, A.; Marsili, M.; Nozzi, M.; Faricelli, R.; Chiarelli, F.; Breda, L. Serum calprotectin: Review of its usefulness and validity in paediatric rheumatic diseases. Clin. Exp. Rheumatol. 2015, 33, 109–114. [Google Scholar] [PubMed]
- Heizmann, C.W.; Fritz, G.; Schäfer, B.W. S100 proteins: Structure, functions and pathology. Front. Biosci. 2002, 7, d1356–d1368. [Google Scholar] [PubMed]
- Kessel, C.; Holzinger, D.; Foell, A. Phagocyte-derived S100 proteins in autoinflammation: Putative role in pathogenesis and usefulness as biomarkers. Clin. Immunol. 2013, 147, 229–241. [Google Scholar] [CrossRef]
- Korndörfer, I.P.; Brueckner, F.; Skerra, A. The Crystal Structure of the Human (S100A8/S100A9)2 Heterotetramer, Calprotectin, Illustrates how Conformational Changes of Interacting α-Helices Can Determine Specific Association of Two EF-hand Proteins. J. Mol. Biol. 2007, 370, 887–898. [Google Scholar] [CrossRef] [PubMed]
- Viemann, D.; Strey, A.; Janning, A.; Jurk, K.; Klimmek, K.; Vogl, T.; Hirono, K.; Ichida, F.; Foell, D.; Kehrel, B.; et al. Myeloid-related proteins 8 and 14 induce a specific inflammatory response in human microvascular endothelial cells. Blood 2005, 105, 2955–2962. [Google Scholar] [CrossRef] [Green Version]
- Moncrieffe, H.; Ursu, S.; Holzinger, D.; Patrick, F.; Kassoumeri, L.; Wade, A.; Roth, J.; Wedderburn, L.R. A subgroup of juvenile idiopathic arthritis patients who respond well to methotrexate are identified by the serum biomarker MRP8/14 protein. Rheumatology 2013, 52, 1467–1476. [Google Scholar] [CrossRef] [Green Version]
- Anink, J.; van Suijlekom-Smit, L.W.; Otten, M.H.; Prince, F.H.; van Rossum, M.A.; Dolman, K.M.; Hoppenreijs, E.P.; ten Cate, R.; Ursu, S.; Wedderburn, L.R. MRP8/14 serum levels as a predictor of response to starting and stopping anti-TNF treatment in juvenile idiopathic arthritis. Arthritis Res. Ther. 2015, 17, 200. [Google Scholar] [CrossRef] [Green Version]
- La, C.; Lê, P.Q.; Ferster, A.; Goffin, L.; Spruyt, D.; Lauwerys, B.; Durez, P.; Boulanger, C.; Sokolova, T.; Rasschaert, J.; et al. Serum calprotectin (S100A8/A9): A promising biomarker in diagnosis and follow-up in different subgroups of juvenile idiopathic arthritis. RMD Open 2021, 7, e001646. [Google Scholar] [CrossRef]
- Barendregt, A.M.; Veldkamp, S.R.; Hissink Muller, P.C.; van de Geer, A.; Aarts, C.; van Gulik, E.C.; Schilham, M.W.; Kessel, C.; Keizer, M.P.; Hemke, R.; et al. MRP8/14 and neutrophil elastase for predicting treatment response and occurrence of flare in patients with juvenile idiopathic arthritis. Rheumatology 2020, 59, 2392–2401. [Google Scholar] [CrossRef]
- Schulze ZurWiesch, A.; Foell, D.; Frosch, M. Myeloid related proteins MRP8/MRP14 may predict disease flares in juvenile idiopathic arthritis. Clin. Exp. Rheumatol. 2004, 22, 368–373. [Google Scholar]
- Rothmund, F.; Gerss, J.; Ruperto, N.; Däbritz, J.; Wittkowski, H.; Frosch, M.; Wulffraat, N.M.; Wedderburn, L.R.; Holzinger, D.; Gohar, F.; et al. Validation of relapse risk biomarkers for routine use in patients with juvenile idiopathic arthritis. Arthritis Care Res. 2014, 66, 949–955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petty, R.E.; Southwood, T.R.; Manners, P.; Baum, J.; Glass, D.N.; Goldenberg, J.; He, X.; Maldonado-Cocco, J.; Orozco-Alcala, J.; Prieur, A.-M.; et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: Second revision, Edmonton, 2001. J. Rheumatol. 2004, 31, 390–392. [Google Scholar] [PubMed]
- Marzetti, V.; Breda, L.; Miulli, E.; Filippetti, F.; Mancini, C.; Chiarelli, F.; Altobelli, E. Clinical characteristics of juvenile idiopathic arthritis in an area of central Italy: A population-based study. Ann. Ig. 2017, 29, 281–292. [Google Scholar] [PubMed]
- Hinze, C.H.; Foell, D.; Johnson, A.L.; Spalding, S.J.; Gottlieb, B.S.; Morris, P.W.; Kimura, Y.; Onel, K.; Li, S.C.; Grom, A.A.; et al. Serum S100A8/A9 and S100A12 levels in children with polyarticular forms of juvenile idiopathic arthritis: Relationship to maintenance of clinically inactive disease during anti-tumor necrosis factor therapy and occurrence of disease flare after discontinuation of therapy. Arthritis Rheumatol. 2019, 71, 451–459. [Google Scholar]
- Ravelli, A.; Consolaro, A.; Horneff, G.; Laxer, R.M.; Lovell, D.J.; Wulffraat, N.M.; Akikusa, J.D.; Al-Mayouf, S.; Anton, J.; Avcin, T.; et al. Treating juvenile idiopathic arthritis to target: Recommendations of an international task force. Ann. Rheum. Dis. 2018, 77, 819–828. [Google Scholar] [CrossRef]
- Frosch, M.; Strey, A.; Vogl, T.; Wulffraat, N.M.; Kuis, W.; Sunderkötter, C.; Harms, E.; Sorg, C.; Roth, J. Myeloid-related proteins 8 and 14 are specifically secreted during interaction of phagocytes and activated endothelium and are useful markers for monitoring disease activity in pauciarticular-onset juvenile rheumatoid arthritis. Arthritis Rheum. 2000, 43, 628–637. [Google Scholar] [CrossRef]
- Altobelli, E.; Angeletti, P.M.; Petrocelli, R.; Lapergola, G.; Farello, G.; Cannataro, G.; Breda, L. Serum Calprotectin a Potential Biomarker in Juvenile Idiopathic Arthritis: A Meta-Analysis. J. Clin. Med. 2021, 10, 4861. [Google Scholar] [CrossRef]
- Hurnakova, J.; Zavada, J.; Hanova, P.; Hulejova, H.; Klein, M.; Mann, H.; Sleglova, O.; Olejarova, M.; Forejtova, S.; Ruzickova, O.; et al. Serum calprotectin (S100A8/A9): An independent predictor of ultrasounf synovitis in patients with rheumatoid arthritis. Arthritis Res. Ther. 2015, 17, 252. [Google Scholar] [CrossRef] [Green Version]
- Romano, M.; Gerloni, V.; De Lucia, O.; Piskin, D.; Giani, T.; Gattinara, M.; Borghi, M.O.; Bodio, C.; Mahler, M.; Meroni, P.L.; et al. Serum calprotectin (S100A8/9), clinical and ultrasound assessment in patients with juvenile idiopathic arthritis. Clin. Exp. Rheumatol. 2021, 39, 1132–1140. [Google Scholar] [CrossRef]
- Foell, D.; Wulffraat, N.; Wedderburn, L.R.; Wittkowski, H.; Frosch, M.; Gerß, J.; Stanevicha, V.; Mihaylova, D.; Ferriani, V.; Tsakalidou, F.K.; et al. Methotrexate withdrawal at 6 vs 12 months in juvenile idiopathic arthritis in remission: A randomized clinical trial. JAMA 2010, 303, 1266–1273. [Google Scholar] [CrossRef] [Green Version]
- Foell, D.; Frosch, M.; zur Wiesch, A.S.; Vogl, T.; Sorg, C.; Roth, J. Methotrexate treatment in juvenile idiopathic arthritis: When is the right time to stop? Ann. Rheum. Dis. 2004, 63, 206–208. [Google Scholar] [CrossRef] [PubMed]
- Gerss, J.; Roth, J.; Holzinger, D.; Ruperto, N.; Wittkowski, H.; Frosch, M.; Wulffraat, N.; Wedderburn, L.; Stanevicha, V.; Mihaylova, D.; et al. Phagocyte-specific S100 proteins and high-sensitivity C reactive protein as biomarkers for a risk-adapted treatment to maintain remission in juvenile idiopathic arthritis: A comparative study. Ann. Rheum. Dis. 2012, 71, 1991–1997. [Google Scholar] [CrossRef] [PubMed]
- Inciarte-Mundo, J.; Ramirez, J.; Hernández, M.V.; Ruiz-Esquide, V.; Cuervo, A.; Cabrera-Villalba, S.R.; Pascal, M.; Yagüe, J.; Cañete, J.D.; Sanmarti, R. Calprotectin strongly and independently predicts relapse in rheumatoid arthritis and polyarticular psoriatic arthritis patients treated with tumor necrosis factor inhibitors: A 1-year prospective cohort study. Arthritis Res. Ther. 2018, 20, 275. [Google Scholar] [CrossRef] [PubMed]
- Jit, M.; Henderson, B.; Stevens, M.; Seymour, R.M. TNF-alpha neutralization in cytokine- driven diseases: A mathematical model to account for therapeutic success in rheumatoid arthritis but therapeutic failure in systemic inflammatory response syndrome. Rheumatology 2005, 44, 323–331. [Google Scholar] [CrossRef] [Green Version]
- Sezer, M.; Aydın, F.; Kurt, T.; Tekgöz, N.; Tekin, Z.E.; Karagöl, C.; Çakar, N.; Acar, B. Prediction of inactive disease and relapse in oligoarticular juvenile idiopathic arthritis. ModRheumatol 2021, 31, 1025–1030. [Google Scholar] [CrossRef]
- Albarouni, M.; Becker, I.; Horneff, G. Predictors of response to methotrexate in juvenile idiopathic arthritis. PediatrRheumatol Online J. 2014, 12, 35. [Google Scholar] [CrossRef] [Green Version]
- Obry, A.; Lequerré, T.; Hardouin, J.; Boyer, O.; Fardellone, P.; Philippe, P.; Le Loët, X.; Cosette, P.; Vittecoq, O. Identification of S100A9 as biomarker of responsiveness to the methotrexate/etanerceptcombination in rheumatoid arthritis using a proteomic approach. PLoS ONE 2014, 9, e115800. [Google Scholar] [CrossRef]
- Consolaro, A.; Varnier, G.C.; Martini, A.; Ravelli, A. Advances in biomarkers for paediatric rheumatic diseases. NatRevRheumatol 2015, 11, 265–275. [Google Scholar] [CrossRef]
- Consolaro, A.; Ruperto, N.; Filocamo, G.; Lanni, S.; Bracciolini, G.; Garrone, M.; Scala, S.; Villa, L.; Silvestri, G.; Tani, D.; et al. Seeking insights into the EPidemiology, treatment and Outcome of Childhood Arthritis through a multinational collaborative effort: Introduction of the EPOCA study. PediatrRheumatol Online J. 2012, 10, 39. [Google Scholar]
- Consolaro, A.; Bracciolini, G.; Ruperto, N.; Pistorio, A.; Magni-Manzoni, S.; Malattia, C.; Pederzoli, S.; Davì, S.; Martini, A.; Ravelli, A.; et al. Remission, minimal disease activity and acceptable symptom state in juvenile idiopathic arthritis. Arthritis Rheum. 2012, 64, 2366–2374. [Google Scholar] [CrossRef]
- Ravelli, A.; Viola, S.; Ruperto, N.; Corsi, B.; Ballardini, G.; Martini, A. Correlation between conventional disease activity measures in juvenile chronic arthritis. Ann. Rheum. Dis. 1997, 56, 197–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filocamo, G.; Consolaro, A.; Ferrari, C.; Ravelli, A. Introducing new tools for assessment of parent- and child-reported outcomes in paediatric rheumatology practice: A work in progress. Clin. Exp. Rheumatol. 2013, 31, 964–968. [Google Scholar]
- Consolaro, A.; Negro, G.; Lanni, S.; Solari, N.; Martini, A.; Ravelli, A. Toward a treat-to-target approach in the management of juvenile idiopathic arthritis. Clin. Exp. Rheumatol. 2012, 30, S157–S162. [Google Scholar]
- Cacciari, E.; Milani, S.; Balsamo, A.; Spada, E.; Bona, G.; Cavallo, L.; Cerutti, F.; Gargantini, L.; Greggio, N.; Tonini, G.; et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J. Endocrinol. Invest. 2006, 29, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Holzinger, D.; Kessel, C.; Omenetti, A.; Gattorno, M. From bench to bedside and back again: Translational research in autoinflammation. Nat. Rev. Rheumatol. 2015, 11, 573–585. [Google Scholar] [CrossRef] [PubMed]
- Alexeeva, E.I.; Namazova-Baranova, L.; Bzarova, T.M.; Valieva, S.I.; Denisova, R.V.; Sleptsova, T.V.; Isaeva, K.B.; Chomahidze, A.M.; Taibulatov, N.I.; Fetisova, A.N.; et al. Predictors of the response to etanercept in patients with juvenile idiopathic arthritis without systemic manifestations within 12 months: Results of an open-label, prospective study conducted at the National Scientific and Practical Center of Children’s Health, Russia. PediatrRheumatol 2017, 15, 51. [Google Scholar]
- Geikowski, T.; Becker, I.; Horneff, G. German BIKER Registry Collaborative Study Group. Predictors of response to etanercept in polyarticular-course juvenile idiopathic arthritis. Rheumatology 2014, 53, 1245–1249. [Google Scholar] [CrossRef]
- Saccomanno, B.; Tibaldi, J.; Minoia, F.; Bagnasco, F.; Pistorio, A.; Guariento, A.; Caorsi, R.; Consolaro, A.; Gattorno, M.; Ravelli, A. Predictors of Effectiveness of Anakinra in Systemic Juvenile Idiopathic Arthritis. J. Rheumatol. 2019, 46, 416–421. [Google Scholar] [CrossRef]




| Inactive JIA (n = 56) | Active JIA (n = 55) | Controls (n = 47) | # p Value | |
| Sex, Female (%) | 48 (85.9) | 43 (78.0) | 31 (66.0) | 0.090 |
| Age at enrollment (ys) | 10.5 (3.20–17.18) | 11.9 (5.53–16.30) | 8.9 (2.27–15.3) | § 0.011 |
| BMI (Kg/m2) | 18.7 (14.00–28.50) | 19.1 (14.00–26.00) | 18.4 (13.00–24.00) | § 0.345 |
| BMI z-score | 0.0 (1.06) | 0.4 (0.23) | 0.4 (0.77) | * 0.130 |
| Previous uveitis (%) | 43 (76.8) | 44 (88.0) | N/A | 0.576 |
| JIA subgroup (%) Oligoarthritis Oligoarthritis-extended Polyarthritis Psoriasic arthritis Entesitis-arthritis | 31 (55.4) 11 (19.6) 11 (19.6) 3 (5.3) 0 (0.0) | 27 (54.0) 8 (14.0) 11 (20.0) 5 (10.1) 1 (2.0) | N/A | 0.486 |
| Ongoing therapy at baseline (%) MTX Etanercept Adalimumab MTX + adalimumab MTX + etanercept Infliximab NSAIDs No therapy | 29 (51.8) 4 (7.1) 6 (10.7) 7 (12.5) 1 (1.8) 1 (1.8) 0(0) 8 (14.3) | 28 (50.9) 2 (3.6) 2 (3.6) 0 (0) 0 (0) 0 (0) 6 (10.9) 12 (21.8) | N/A | N/A |
| New therapy at baseline (%) MTX Adalimumab Etanercept Infliximab | N/A | 20 (36.3) 15 (27.3) 11 (20) 4 (7.3) | N/A | N/A |
| N. of active joints at the onset of JIA | 3.1 (2.93–16.00) | 2.2 (1.76–12.00) | N/A | § 0.092 |
| Disease duration (ys) | 5.0 (0.00–12.00) | 4.9 (0.00–9.81) | N/A | § 0.387 |
| JADAS-27 | 0.0 (0.00–7.00) | 5.9 (2.50–18.00) | N/A | § <0.001 |
| Positive ANA (%) | 11 (24.4) | 15 (71.3) | N/A | 0.210 |
| TMj Inflammation (%) | 0 (0.0) | 13 (26.5) | N/A | <0.001 |
| Laboratory Data | ||||
| Laboratory value (normal range) | Inactive JIA n = 56 | Active JIA n = 55 | Controls n = 47 | § p value |
| Hb (g/dL) (12–16) | 13.25 (12.78–16.00) | 12.80 (10.60–15.00) | 13.40 (11.60–16.70) | 0.968 |
| PLT/µL (150,000–450,000) | 290,500 (188,000–410,000) | 325,000 (202,000–437,000) | 245,282 (202,000–437,000) | 0.053 |
| Leucocytes/µL (4000–10,000) | 6,845 (1240–5870) | 6,495 (4220–9400) | 5910 (1319–6210) | 0.360 |
| Neutrophils/µL (2000–7000) | 3054 (1,228–6980) | 3084 (1150–5420) | 3150 (1150–5380) | 0.764 |
| Lymphocytes/µL (1000–3500) | 2675 (1620–5870) | 2575 (1913–5320) | 2100 (319–6210) | 0.167 |
| Ferritin (ng/mL) (4.6–204) | 29.61 (18.70–64.80) | 26.50 (8.70–69.80) | 37.09 (12.30–65.74) | 0.069 |
| Calprotectin (ng/mL) | 3.30 (0.60–38.8) | 7.00 (1.20–34.00) | 4.00 (1.70–7.20) | 0.018 |
| Albumin (g/dL) (3.5–5.5) | 4.42 ± 0.21 | 4.39 ± 0.23 | 4.44 ± 0.17 | 0.230 |
| ESR (mm/h) (2–15) | 7.00 (3.00–9.00) | 7.50 (3.00–23.00) | 7.60 (2.00–10.00) | 0.050 |
| CRP (mg/dL) (0.00–10.00) | 0.29 (0.17–6.60) | 0.45 (0.10–9.50) | 1.35 (0.29–5.10) | 0.051 |
| Inactive JIA Patients (Relapse vs. Non-Relapse) | Relapse HR (95% CI) | Active JIA Patients (Remission vs. Non-Remission) | Remission HR (95% CI) |
|---|---|---|---|
| (cal. ≥ 3 vs. cal. < 3) | (cal. ≥ 3 vs. cal. < 3) | ||
| CRUDE MODEL p-value | 1.43 (0.86, 2.42)) 0.171 | CRUDE MODEL p-value | 0.75 (0.47, 1.21) 0.242 |
| * CONFOUNDER MODEL p-value | 2.19 (1.20, 4.10) 0.011 | CONFOUNDER MODEL p-value | 0.74 (0.43, 1.27) 0.271 |
| (cal. ≥ 10 vs. cal. < 10) | (cal. ≥ 10 vs. cal. < 10) | ||
| CRUDE MODEL p-value | 1.54 (0.92, 2.59) 0.104 | CRUDE MODEL p-value | 0.44 (0.26, 0.75) 0.002 |
| CONFOUNDER MODEL p-value | 1.86 (1.06, 3.26) 0.030 | CONFOUNDER MODEL p-value | 0.46 (0.26, 0.80) 0.006 |
| (cal. ≥ 12 vs. cal. < 12) | (cal. ≥ 12 vs. cal. < 12) | ||
| CRUDE MODEL p-value | 1.66 (0.96, 2.84) 0.068 | CRUDE MODEL p-value | 0.44 (0.26, 0.77) 0.004 |
| CONFOUNDER MODEL p-value | 1.99 (1.10, 3.62) 0.023 | CONFOUNDER MODEL p-value | 0.47(0.26, 0.84) 0.011 |
| (cal. ≥ 15 vs. cal. < 15) | (cal. ≥ 15 vs. cal. < 15) | ||
| CRUDE MODEL p-value | 1.75 (1.01, 3.03) 0.046 | CRUDE MODEL p-value | 0.44 (0.23, 0.86) 0.016 |
| CONFOUNDER MODEL p-value | 1.94 (1.08, 3.48) 0.028 | CONFOUNDER MODEL p-value | 0.45 (0.22, 0.94) 0.033 |
| (cal. ≥ 20 vs. cal. < 20) | (cal. ≥ 20 vs. cal. < 20) | ||
| CRUDE MODEL p-value | 2.01 (1.11, 3.66) 0.021 | CRUDE MODEL p-value | 0.50 (0.26, 0.98) 0.042 |
| CONFOUNDER MODEL p-value | 2.07 (1.07, 4.00) 0.031 | CONFOUNDER MODEL p-value | 0.54 (0.26, 1.29) 0.101 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
d’Angelo, D.M.; Attanasi, M.; Di Donato, G.; Lapergola, G.; Flacco, M.; Chiarelli, F.; Altobelli, E.; Breda, L. The Role of Serum Calprotectin in Defining Disease Outcomes in Non-Systemic Juvenile Idiopathic Arthritis: A Pilot Study. Int. J. Mol. Sci. 2023, 24, 1671. https://doi.org/10.3390/ijms24021671
d’Angelo DM, Attanasi M, Di Donato G, Lapergola G, Flacco M, Chiarelli F, Altobelli E, Breda L. The Role of Serum Calprotectin in Defining Disease Outcomes in Non-Systemic Juvenile Idiopathic Arthritis: A Pilot Study. International Journal of Molecular Sciences. 2023; 24(2):1671. https://doi.org/10.3390/ijms24021671
Chicago/Turabian Styled’Angelo, Debora Mariarita, Marina Attanasi, Giulia Di Donato, Giuseppe Lapergola, Mariarosaria Flacco, Francesco Chiarelli, Emma Altobelli, and Luciana Breda. 2023. "The Role of Serum Calprotectin in Defining Disease Outcomes in Non-Systemic Juvenile Idiopathic Arthritis: A Pilot Study" International Journal of Molecular Sciences 24, no. 2: 1671. https://doi.org/10.3390/ijms24021671
APA Styled’Angelo, D. M., Attanasi, M., Di Donato, G., Lapergola, G., Flacco, M., Chiarelli, F., Altobelli, E., & Breda, L. (2023). The Role of Serum Calprotectin in Defining Disease Outcomes in Non-Systemic Juvenile Idiopathic Arthritis: A Pilot Study. International Journal of Molecular Sciences, 24(2), 1671. https://doi.org/10.3390/ijms24021671









