Effect of Dietary Geranylgeraniol and Green Tea Polyphenols on Glucose Homeostasis, Bone Turnover Biomarkers, and Bone Microstructure in Obese Mice
Abstract
:1. Introduction
2. Results
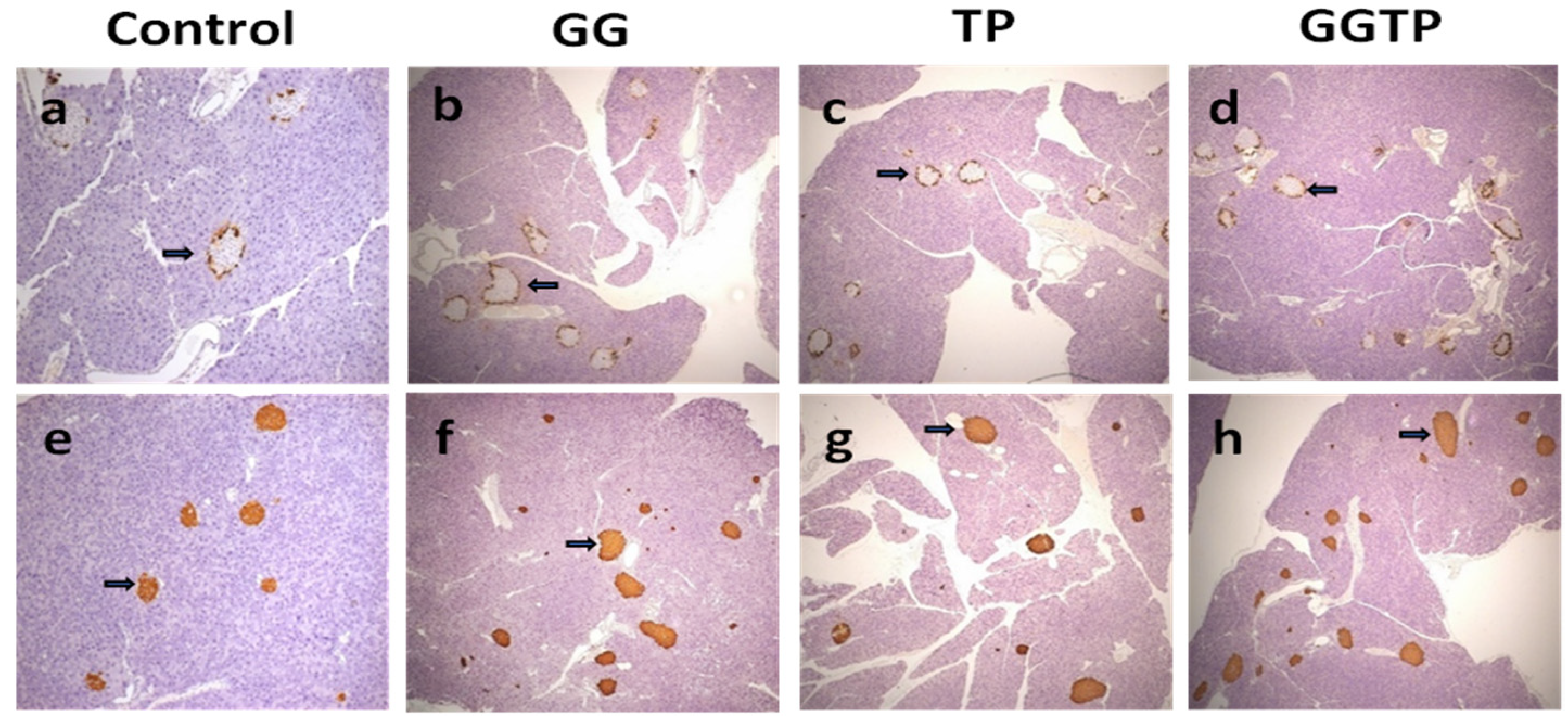
2.1. Glucose Homeostasis and Pancreatic Morphological Analysis
2.2. Serum Bone Turnover Biomarkers and Bone Microarchitectural Properties
2.3. Final Body Weights, White Adipose Tissue Weights, and Adipokine Concentrations
3. Discussion
4. Materials and Methods
4.1. Animals and Treatments
4.2. Glucose and Insulin Tolerance Tests
4.3. Sample Collection
4.4. Insulin and Histological Assessment of Pancreatic Tissue
4.5. Bone Biomarkers Analyses
4.6. Bone Microarchitecture Measurement with μ-CT
4.7. Adipokine Measurements
4.8. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes–Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef] [Green Version]
- Salari, N.; Ghasemi, H.; Mohammadi, L.; Behzadi, M.H.; Rabieenia, E.; Shohaimi, S.; Mohammadi, M. The global prevalence of osteoporosis in the world: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2021, 16, 609. [Google Scholar] [CrossRef] [PubMed]
- Gullberg, B.; Johnell, O.; Kanis, J. World-wide Projections for Hip Fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.J.; Sun, L.; Gao, H. Diet-induced obesity alters bone remodeling leading to decreased femoral trabecular bone mass in mice. Ann. New York Acad. Sci. USA 2010, 1192, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.J. Effects of obesity on bone metabolism. J. Orthop. Surg. Res. 2011, 6, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fehrendt, H.; Linn, T.; Hartmann, S.; Szalay, G.; Heiss, C.; Schnettler, R.; Lips, K.S. Negative Influence of a Long-Term High-Fat Diet on Murine Bone Architecture. Int. J. Endocrinol. 2014, 2014, 318924. [Google Scholar] [CrossRef] [Green Version]
- Murray, C.E.; Coleman, C.M. Impact of Diabetes Mellitus on Bone Health. Int. J. Mol. Sci. 2019, 20, 4873. [Google Scholar] [CrossRef] [Green Version]
- Gortler, H.; Rusyn, J.; Godbout, C.; Chahal, J.; Schemitsch, E.H.; Nauth, A. Diabetes and Healing Outcomes in Lower Extremity Fractures: A Systematic Review. Injury 2018, 49, 177–183. [Google Scholar] [CrossRef]
- Collins, K.H.; Herzog, W.; Macdonald, G.Z.; Reimer, R.A.; Rios, J.L.; Smith, I.C.; Zernicke, R.F.; Hart, D.A. Obesity, Metabolic Syndrome, and Musculoskeletal Disease: Common Inflammatory Pathways Suggest a Central Role for Loss of Muscle Integrity. Front. Physiol. 2018, 9, 112. [Google Scholar] [CrossRef]
- Hou, J.; He, C.; He, W.; Yang, M.; Luo, X.; Li, C. Obesity and Bone Health: A Complex Link. Front. Cell Dev. Biol. 2020, 8, 600181. [Google Scholar] [CrossRef]
- Okin, D.; Medzhitov, R. The Effect of Sustained Inflammation on Hepatic Mevalonate Pathway Results in Hyperglycemia. Cell 2016, 165, 343–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawai, M.; Rosen, C.J. PPARγ: A circadian transcription factor in adipogenesis and osteogenesis. Nat. Rev. Endocrinol. 2010, 6, 629–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, E.; Elmassry, M.M.; Cao, J.J.; Kaur, G.; Dufour, J.M.; Hamood, A.N.; Shen, C.-L. Beneficial effect of dietary geranylgeraniol on glucose homeostasis and bone microstructure in obese mice is associated with suppression of proinflammation and modification of gut microbiome. Nutr. Res. 2021, 93, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Tian, J.; Jiang, J.; Li, L.; Ying, X.; Tian, H.; Nie, M. Effects of green tea or green tea extract on insulin sensitivity and glycaemic control in populations at risk of type 2 diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials. J. Hum. Nutr. Diet. 2014, 27, 501–512. [Google Scholar] [CrossRef]
- Asbaghi, O.; Fouladvand, F.; Gonzalez, M.J.; Ashtary-Larky, D.; Choghakhori, R.; Abbasnezhad, A. Effect of green tea on glycemic control in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 23–31. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Kang, L.; Wang, C.-Z.; Huang, H.H.; Cheng, T.-L.; Huang, H.-T.; Lee, M.-J.; Lin, Y.-S.; Ho, M.-L.; Wang, G.-J.; et al. (−)-Epigallocatechin-3-Gallate (EGCG) Enhances Osteogenic Differentiation of Human Bone Marrow Mesenchymal Stem Cells. Molecules 2018, 23, 3221. [Google Scholar] [CrossRef] [Green Version]
- Shen, C.-L.; Chyu, M.-C.; Cao, J.J.; Yeh, J.K. Green Tea Polyphenols Improve Bone Microarchitecture in High-Fat-Diet–Induced Obese Female Rats Through Suppressing Bone Formation and Erosion. J. Med. Food 2013, 16, 421–427. [Google Scholar] [CrossRef]
- Dostal, A.M.; Arikawa, A.; Espejo, L.; Kurzer, M.S. Long-Term Supplementation of Green Tea Extract Does Not Modify Adiposity or Bone Mineral Density in a Randomized Trial of Overweight and Obese Postmenopausal Women. J. Nutr. 2016, 146, 256–264. [Google Scholar] [CrossRef] [Green Version]
- Shen, C.-L.; Chen, L.; Wang, S.; Chyu, M.-C. Effects of dietary fat levels and feeding durations on musculoskeletal health in female rats. Food Funct. 2014, 5, 598–604. [Google Scholar] [CrossRef]
- Fliefel, R.M.; Entekhabi, S.A.; Ehrenfeld, M.; Otto, S. Geranylgeraniol (GGOH) as a Mevalonate Pathway Activator in the Rescue of Bone Cells Treated with Zoledronic Acid: An In Vitro Study. Stem Cells Int. 2019, 2019, 4351327. [Google Scholar] [CrossRef]
- Giriwono, P.E.; Shirakawa, H.; Ohsaki, Y.; Sato, S.; Aoyama, Y.; Ho, H.-J.; Goto, T.; Komai, M. Geranylgeraniol Suppresses the Expression of IRAK1 and TRAF6 to Inhibit NFκB Activation in Lipopolysaccharide-Induced Inflammatory Responses in Human Macrophage-Like Cells. Int. J. Mol. Sci. 2019, 20, 2320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giriwono, P.E.; Shirakawa, H.; Ohsaki, Y.; Hata, S.; Kuriyama, H.; Sato, S.; Goto, T.; Komai, M. Dietary supplementation with geranylgeraniol suppresses lipopolysaccharide-induced inflammation via inhibition of nuclear factor-κB activation in rats. Eur. J. Nutr. 2013, 52, 1191–1199. [Google Scholar] [CrossRef] [PubMed]
- Tricarico, P.M.; Kleiner, G.; Valencic, E.; Campisciano, G.; Girardelli, M.; Crovella, S.; Knowles, A.; Marcuzzi, A. Block of the Mevalonate Pathway Triggers Oxidative and Inflammatory Molecular Mechanisms Modulated by Exogenous Isoprenoid Compounds. Int. J. Mol. Sci. 2014, 15, 6843–6856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heber, D.; Zhang, Y.; Yang, J.; Ma, J.E.; Henning, S.M.; Li, Z. Green Tea, Black Tea, and Oolong Tea Polyphenols Reduce Visceral Fat and Inflammation in Mice Fed High-Fat, High-Sucrose Obesogenic Diets. J. Nutr. 2014, 144, 1385–1393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, Y.; Zhang, M.; Wu, T.; Dai, S.; Xu, J.; Zhou, Z. The anti-obesity effect of green tea polysaccharides, polyphenols and caffeine in rats fed with a high-fat diet. Food Funct. 2015, 6, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Kinney, J.H.; Ladd, A.J.C. The Relationship Between Three-Dimensional Connectivity and the Elastic Properties of Trabecular Bone. J. Bone Miner. Res. 1998, 13, 839–845. [Google Scholar] [CrossRef]
- Shen, V.; Dempster, D.W.; Birchman, R.; Xu, R.; Lindsay, R. Loss of cancellous bone mass and connectivity in ovariectomized rats can be restored by combined treatment with parathyroid hormone and estradiol. J. Clin. Investig. 1993, 91, 2479–2487. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, S.A.; Goulet, R.W.; McCubbrey, D. Measurement and significance of three-dimensional architecture to the mechanical integrity of trabecular bone. Calcif. Tissue Int. 1993, 53 (Suppl. 1), S127–S132; [Google Scholar] [CrossRef] [Green Version]
- Hildebrand, T.; Rüegsegger, P. Quantification of Bone Microarchitecture with the Structure Model Index. Comput. Methods Biomech. Biomed. Eng. 1997, 1, 15–23. [Google Scholar] [CrossRef]
- Cheng, J.; Tan, Y.; Zhou, J.; Xiao, L.; Johnson, M.; Qu, X. Green tea polyphenols ameliorate metabolic abnormalities and insulin resistance by enhancing insulin signalling in skeletal muscle of Zucker fatty rats. Clin. Sci. 2020, 134, 1167–1180. [Google Scholar] [CrossRef]
- Li, X.; Li, S.; Chen, M.; Wang, J.; Xie, B.; Sun, Z. (−)-Epigallocatechin-3-gallate (EGCG) inhibits starch digestion and improves glucose homeostasis through direct or indirect activation of PXR/CAR-mediated phase II metabolism in diabetic mice. Food Funct. 2018, 9, 4651–4663. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.Y.; Friel, J.K.; Mackay, D.S. Effect of sucralose and aspartame on glucose metabolism and gut hormones. Nutr. Rev. 2020, 78, 725–746. [Google Scholar] [CrossRef]
- Qian, C.; Qi, Y.; Feng, R.; Yang, M.; Zhang, M.; Liu, W.; Rayner, C.K.; Ma, J. Sucralose can improve glucose tolerance and upregulate expression of sweet taste receptors and glucose transporters in an obese rat model. Eur. J. Nutr. 2021, 60, 1809–1817. [Google Scholar] [CrossRef] [PubMed]
- Orlando, G.; Leone, S.; Ferrante, C.; Chiavaroli, A.; Mollica, A.; Stefanucci, A.; Macedonio, G.; Dimmito, M.P.; Leporini, L.; Menghini, L.; et al. Effects of Kisspeptin-10 on Hypothalamic Neuropeptides and Neurotransmitters Involved in Appetite Control. Molecules 2018, 23, 3071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.-H.; Ho, M.-L.; Chang, J.-K.; Hung, S.-H.; Wang, G.-J. Green tea catechin enhances osteogenesis in a bone marrow mesenchymal stem cell line. Osteoporos. Int. 2005, 16, 2039–2045. [Google Scholar] [CrossRef] [PubMed]
- Singhatanadgit, W.; Hankamolsiri, W.; Janvikul, W. Geranylgeraniol prevents zoledronic acid-mediated reduction of viable mesenchymal stem cells via induction of Rho-dependent YAP activation. R. Soc. Open Sci. 2021, 8, 202066. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.J.; Gregoire, B.R.; Gao, H. High-fat diet decreases cancellous bone mass but has no effect on cortical bone mass in the tibia in mice. Bone 2009, 44, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Muraguchi, T.; Okamoto, K.; Mitake, M.; Ogawa, H.; Shidoji, Y. Polished rice as natural sources of cancer-preventing geranylgeranoic acid. J. Clin. Biochem. Nutr. 2011, 49, 8–15. [Google Scholar] [CrossRef] [Green Version]
- de Oliveira, G.J.P.L.; Basso, T.L.D.; Fontanari, L.A.; Faloni, A.P.D.S.; Marcantonio, E., Jr.; Orrico, S.R.P. Glycemic control protects against trabecular bone microarchitectural damage in a juvenile male rat model of streptozotocin-induced diabetes. Endocr. Res. 2017, 42, 171–179. [Google Scholar] [CrossRef]
- Bornstein, S.; Moschetta, M.; Kawano, Y.; Sacco, A.; Huynh, D.; Brooks, D.; Manier, S.; Fairfield, H.; Falank, C.; Roccaro, A.M.; et al. Metformin Affects Cortical Bone Mass and Marrow Adiposity in Diet-Induced Obesity in Male Mice. Endocrinology 2017, 158, 3369–3385. [Google Scholar] [CrossRef]
- Dufour, J.M.; Rajotte, R.V.; Zimmerman, M.; Rezania, A.; Kin, T.; Dixon, D.E.; Korbutt, G.S. Development of an Ectopic Site for Islet Transplantation, Using Biodegradable Scaffolds. Tissue Eng. 2005, 11, 1323–1331. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.J.; Gregoire, B.R.; Shen, C.-L. A High-Fat Diet Decreases Bone Mass in Growing Mice with Systemic Chronic Inflammation Induced by Low-Dose, Slow-Release Lipopolysaccharide Pellets. J. Nutr. 2017, 147, 1909–1916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouxsein, M.L.; Boyd, S.K.; Christiansen, B.A.; Guldberg, R.E.; Jepsen, K.J.; Müller, R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J. Bone Miner. Res. 2010, 25, 1468–1486. [Google Scholar] [CrossRef] [PubMed]
- Parfitt, A.M.; Drezner, M.K.; Glorieux, F.H.; Kanis, J.A.; Malluche, H.; Meunier, P.J.; Ott, S.M.; Recker, R.R. Bone histomorphometry: Standardization of nomenclature, symbols, and units: Report of the asbmr histomorphometry nomenclature committee. J. Bone Miner. Res. 1987, 2, 595–610. [Google Scholar] [CrossRef]
| Parameters | -GGOH | +GGOH | Two-Way ANOVA p-Value | ||||
|---|---|---|---|---|---|---|---|
| -GTP (Control) | +GTP (TP) | -GTP (GG) | +GTP (GGTP) | GGOH | GTP | GGOH×GTP | |
| Blood sugar (mg/dL) measured by ipGTT | |||||||
| 0 min | 186.3 ± 9.5 | 168.1 ± 9.5 | 166.6 ± 8.8 | 169.8 ± 9.5 | 0.343 | 0.433 | 0.263 |
| 15 min | 506.2 ± 24.6 | 492.3 ± 24.6 | 476.0 ± 22.8 | 483.0 ± 24.6 | 0.423 | 0.889 | 0.671 |
| 30 min | 542.0 ± 17.8 | 510.6 ± 17.8 | 553.1 ± 16.5 | 540.0 ± 17.8 | 0.260 | 0.218 | 0.609 |
| 60 min | 512.3 a ± 34.3 | 504.7 a ± 34.3 | 427.4 b ± 31.7 | 439.8 b ± 34.3 | 0.037 | 0.945 | 0.769 |
| 120 min | 369.3 ax ± 20.2 | 255.0 ay ± 20.2 | 243.6 bx ± 18.7 | 207.3 by ± 20.2 | <0.001 | 0.001 | 0.062 |
| AUC | 57125 ax ± 2009 | 49374 ay ± 1835 | 50496 bx ± 1835 | 46680 by ± 1834 | 0.023 | 0.006 | 0.308 |
| Blood glucose (mg/dL)measured by ipITT | |||||||
| 0 min | 171.1 ± 7.4 | 162.7 ± 7.4 | 161.1 ± 6.9 | 166.1 ± 6.9 | 0.651 | 0.809 | 0.354 |
| 15 min | 88.6 ± 7.9 | 93.1 ± 7.9 | 95.7 ± 7.3 | 85.7 ± 7.3 | 0.979 | 0.722 | 0.352 |
| 30 min | 81.8 ± 5.5 | 75.7 ± 5.5 | 81.0 ± 5.1 | 80.3 ± 5.1 | 0.724 | 0.523 | 0.612 |
| 60 min | 68.7x ± 6.3 | 53.0 y ± 6.3 | 63.9 x ± 5.8 | 53.3 y ± 5.8 | 0.713 | 0.042 | 0.679 |
| 120 min | 90.8 ax ± 6.5 | 74.0 ay ± 7.1 | 74.1 bx ± 6.5 | 58.9 by ± 6.0 | 0.025 | 0.024 | 0.909 |
| AUC | 9313 ± 464 | 8214 ± 430 | 8143 ± 464 | 7630 ± 430 | 0.063 | 0.085 | 0.519 |
| Serum insulin (ng/mL) | 13.2 y ± 1.8 | 37.0 x ± 1.9 | 14.0y ± 1.9 | 36.7x ± 1.8 | 0.897 | <0.001 | 0.762 |
| Pancreas insulin (μg/mL) | 341.4 ± 25.4 | 305.6 ± 27.1 | 341.0 ± 25.4 | 334.1 ± 25.4 | 0.591 | 0.415 | 0.579 |
| Parameters | -GGOH | +GGOH | Two-Way ANOVA p-Value | ||||
|---|---|---|---|---|---|---|---|
| -GTP (Control) | +GTP (TP) | -GTP (GG) | +GTP (GGTP) | GGOH | GTP | GGOH×GTP | |
| Serum bone biomarkers | |||||||
| P1NP (ng/mL) | 22.3 ± 0.9 | 20.5 ± 1.0 | 21.2 ± 0.9 | 20.6 ± 0.9 | 0.604 | 0.227 | 0.561 |
| CTX (ng/mL) | 21.3 A ± 1.6 | 14.0 B ± 1.7 | 14.2 B ± 1.6 | 13.8 B ± 1.5 | 0.031 | 0.022 | 0.041 |
| LV-4 (trabecular bone) | |||||||
| BV/TV (%) | 17.5 ± 0.9 | 18.1 ± 0.1 | 18.4 ± 0.1 | 16.7 ± 0.1 | 0.814 | 0.552 | 0.213 |
| Tb.N (mm−1) | 5.36 b ± 0.09 | 5.40 b ± 0.09 | 5.53 a ± 0.09 | 5.63 a ± 0.09 | 0.033 | 0.450 | 0.740 |
| Tb.Th (mm) | 0.044 y ± 0.001 | 0.044 x ± 0.001 | 0.041 y ± 0.001 | 0.046 x ± 0.001 | 0.280 | 0.038 | 0.110 |
| Tb.Sp (mm) | 0.185 a ± 0.003 | 0.185 a ± 0.003 | 0.176 b ± 0.003 | 0.177 b ± 0.003 | 0.019 | 0.990 | 0.948 |
| Conn.Dn (mm−3) | 167.7 C ± 10.4 | 179.4 B ± 10.9 | 221.1 A ± 10.9 | 186.8 B ± 10.4 | 0.006 | 0.295 | 0.036 |
| SMI | 1.702 A ± 0.115 | 1.622 A ± 0.120 | 1.242 B ± 0.120 | 1.639 A ± 0.115 | 0.067 | 0.186 | 0.049 |
| Distal femur (trabecular bone) | |||||||
| BV/TV (%) | 7.043 ± 0.924 | 7.255 ± 0.924 | 9.462 ± 0.850 | 7.255 ± 0.924 | 0.189 | 0.278 | 0.189 |
| Tb.N (mm−1) | 3.397 ± 0.146 | 3.543 ± 0.146 | 3.663 ± 0.134 | 3.543 ± 0.146 | 0.357 | 0.928 | 0.357 |
| Tb.Th (mm) | 0.048 ± 0.002 | 0.047 ± 0.002 | 0.051 ± 0.002 | 0.047 ± 0.002 | 0.422 | 0.199 | 0.422 |
| Tb.Sp (mm) | 0.300 ± 0.014 | 0.288 ± 0.014 | 0.270 ± 0.013 | 0.288 ± 0.013 | 0.268 | 0.821 | 0.268 |
| Conn.Dn (mm−3) | 28.23 ± 8.26 | 36.60 ± 8.26 | 50.43 ± 7.59 | 36.60 ± 8.26 | 0.178 | 0.737 | 0.178 |
| SMI | 2.983 A ± 0.113 | 2.911 A ± 0.113 | 2.588 B ± 0.104 | 2.911 A ± 0.113 | 0.080 | 0.260 | 0.080 |
| Femur mid-diaphysis (cortical bone) | |||||||
| B.Ar (mm2) | 0.990 ± 0.031 | 0.985 ± 0.029 | 0.981 ± 0.028 | 1.012 ± 0.029 | 0.753 | 0.660 | 0.556 |
| Me.Ar (%) | 51.71 ± 0.64 | 51.69 ± 0.62 | 51.83 ± 0.59 | 50.50 ± 0.61 | 0.385 | 0.280 | 0.297 |
| Ct.Th (mm) | 0.212 ± 0.004 | 0.210 ± 0.004 | 0.212 ± 0.004 | 0.216 ± 0.004 | 0.537 | 0.813 | 0.457 |
| Parameters | -GGOH | +GGOH | Two-Way ANOVA p-Value | ||||
|---|---|---|---|---|---|---|---|
| -GTP (Control) | +GTP (TP) | -GTP (GG) | +GTP (GGTP) | GGOH | GTP | GGOH×GTP | |
| Final BW | 37.9 ax ± 1.30 | 34.3 ay ± 1.40 | 35.3 bx ± 1.40 | 31.5 by ± 1.40 | 0.049 | 0.009 | 0.960 |
| WAT weight (g) | 2.23 ax ± 0.16 | 1.75 ay ± 0.16 | 1.90 bx ± 0.16 | 1.36 by ± 0.16 | 0.031 | 0.003 | 0.870 |
| Resistin (pg/mg protein) | 253.4 x ± 43.2 | 63.5 y ± 4.4 | 238.4 x ± 26.5 | 149.0 y ± 17.8 | 0.202 | <0.001 | 0.073 |
| Leptin (pg/mg protein) | 37.8 x ± 8.1 | 5.7 y ± 1.4 | 29.8 x ± 3.4 | 10.4 y ± 1.8 | 0.712 | <0.001 | 0.176 |
| IL-6 (pg/mg protein) | 0.662 x ± 0.106 | 0.194 y ± 0.021 | 0.839 x ± 0.176 | 0.321 y ± 0.040 | 0.141 | <0.001 | 0.701 |
| MCP-1 (pg/mg protein) | 0.413 x ± 0.067 | 0.023 y ± 0.007 | 0.327 x ± 0.066 | 0.140 y ± 0.077 | 0.836 | <0.001 | 0.174 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, C.-L.; Dufour, J.M.; Miranda, J.M.; Kaur, G.; Chung, E.; Ramalingam, L.; Moustaid-Moussa, N.; Cao, J.J. Effect of Dietary Geranylgeraniol and Green Tea Polyphenols on Glucose Homeostasis, Bone Turnover Biomarkers, and Bone Microstructure in Obese Mice. Int. J. Mol. Sci. 2023, 24, 979. https://doi.org/10.3390/ijms24020979
Shen C-L, Dufour JM, Miranda JM, Kaur G, Chung E, Ramalingam L, Moustaid-Moussa N, Cao JJ. Effect of Dietary Geranylgeraniol and Green Tea Polyphenols on Glucose Homeostasis, Bone Turnover Biomarkers, and Bone Microstructure in Obese Mice. International Journal of Molecular Sciences. 2023; 24(2):979. https://doi.org/10.3390/ijms24020979
Chicago/Turabian StyleShen, Chwan-Li, Jannette M. Dufour, Jonathan M. Miranda, Gurvinder Kaur, Eunhee Chung, Latha Ramalingam, Naima Moustaid-Moussa, and Jay J. Cao. 2023. "Effect of Dietary Geranylgeraniol and Green Tea Polyphenols on Glucose Homeostasis, Bone Turnover Biomarkers, and Bone Microstructure in Obese Mice" International Journal of Molecular Sciences 24, no. 2: 979. https://doi.org/10.3390/ijms24020979







