Testosterone and Prolactin Perturbations Possibly Associated with Reduced Levels of β-Arrestin1 in Mononuclear Leukocytes of Women with Premenstrual Dysphoric Disorder
Abstract
:1. Introduction
2. Results
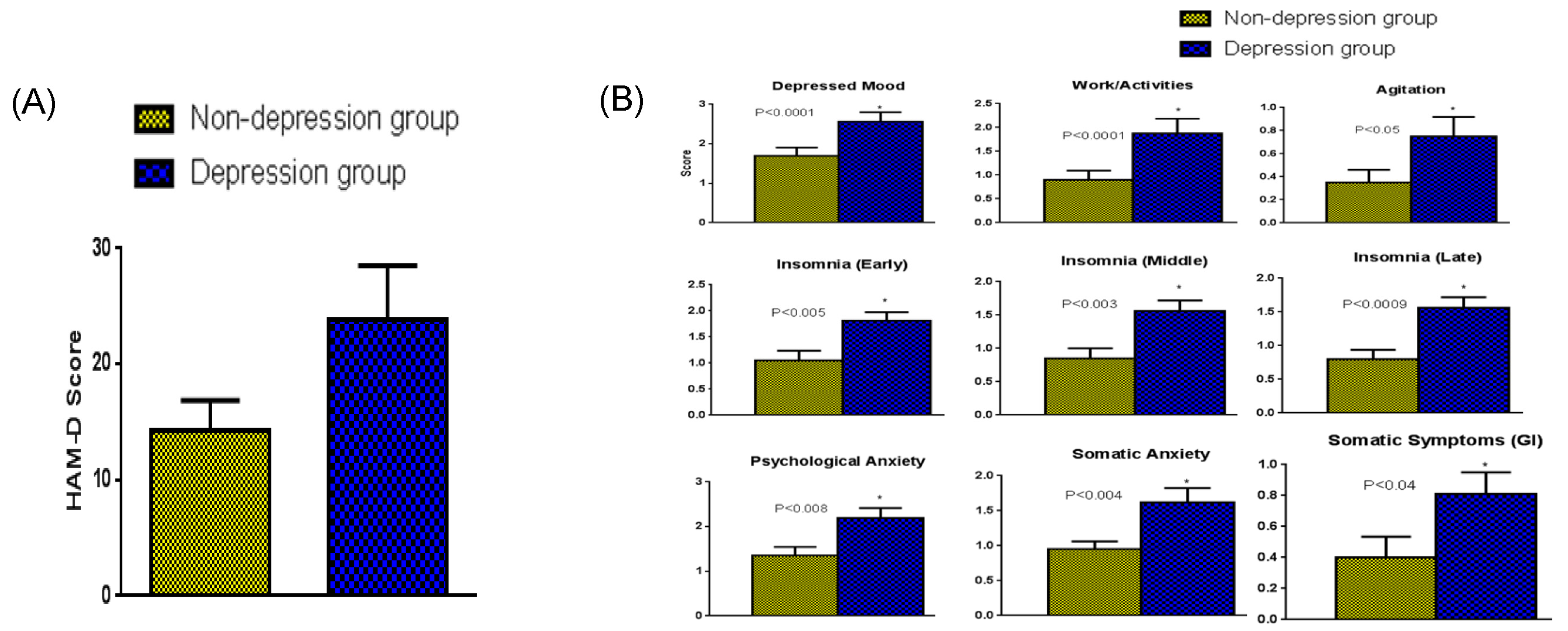
2.1. Analysis of Different Parameters on the Hamilton Rating Scale for Depression (HAM-D)
2.2. Change in β-Arrestin1 Protein Concentrations Due to Depression
2.3. Correlation between β-Arrestin1 Protein Concentrations and HAM-D
2.4. Depression-Associated Changes in Hormones That Regulate Steroidogenesis at the Perimenstrual Stage of the Menstrual Cycle Studied
2.5. Correlation between Testosterone Concentrations and β-Arrestin1
3. Discussion
Limitations
4. Materials and Methods
4.1. Subject Recruitment
4.2. HAM-D Scores
4.3. Blood collection and Isolation of Mononuclear Leukocytes
4.4. Enzyme-Linked Immunosorbent Assay (ELISA)
4.5. Radioimmunoassay (RIA)
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Biro, F.M.; Greenspan, L.C.; Galvez, M.P. Puberty in girls of the 21st century. J. Pediatr. Adolesc. Gynecol. 2012, 25, 289–294. [Google Scholar] [CrossRef]
- Ceylan, B.; Özerdoğan, N. Factors affecting age of onset of menopause and determination of quality of life in menopause. Turk. J. Obstet. Gynecol. 2015, 12, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Hofmeister, S.; Bodden, S. Premenstrual Syndrome and Premenstrual Dysphoric Disorder. Am. Fam. Physician. 2016, 94, 236–240. [Google Scholar] [PubMed]
- Hardy, C.; Hunter, M.S. Premenstrual Symptoms and Work: Exploring Female Staff Experiences and Recommendations for Workplaces. Int. J. Environ. Res. Public Health 2021, 18, 3647. [Google Scholar] [CrossRef]
- Yesildere Saglam, H.; Orsal, O. Effect of exercise on premenstrual symptoms: A systematic review. Complement. Ther. Med. 2020, 48, 102272. [Google Scholar] [CrossRef]
- Kwan, I.; Onwude, J.L. Premenstrual syndrome. BMJ Clin. Evid. 2015, 2015, 0806. [Google Scholar]
- Choi, D.S. Premenstrual syndrome. J. Women Med. 2009, 2, 141–146. [Google Scholar]
- Jang, S.H.; Kim, D.I.; Choi, M.S. Effects and treatment methods of acupuncture and herbal medicine for premenstrual syndrome/premenstrual dysphoric disorder: Systematic review. BMC Complement. Altern. Med. 2014, 14, 11. [Google Scholar] [CrossRef]
- Yonkers, K.A.; O’Brien, P.M.; Eriksson, E. Premenstrual syndrome. Lancet 2008, 371, 1200–1210. [Google Scholar] [CrossRef] [PubMed]
- Yen, J.Y.; Lin, H.C.; Lin, P.C.; Liu, T.L.; Long, C.Y.; Ko, C.H. Early- and Late-Luteal-Phase Estrogen and Progesterone Levels of Women with Premenstrual Dysphoric Disorder. Int. J. Environ. Res. Public Health 2019, 16, 4352. [Google Scholar] [CrossRef] [PubMed]
- Landén, M.; Erlandsson, H.; Bengtsson, F.; Andersch, B.; Eriksson, E. Short onset of action of a serotonin reuptake inhibitor when used to reduce premenstrual irritability. Neuropsychopharmacology 2009, 34, 585–592. [Google Scholar] [CrossRef]
- Schweizer-Schubert, S.; Gordon, J.L.; Eisenlohr-Moul, T.A.; Meltzer-Brody, S.; Schmalenberger, K.M.; Slopien, R.; Zietlow, A.-L.; Ehlert, U.; Ditzen, B. Steroid hormone sensitivity in reproductive mood disorders: On the role of the GABAA receptors complex and stress during hormonal transition. Front. Med. 2021, 7, 479646. [Google Scholar] [CrossRef] [PubMed]
- Studd, J.; Nappi, R.E. Reproductive depression. Gynecol. Endocrinol. 2012, 28 (Suppl. S1), 42–45. [Google Scholar] [CrossRef]
- Hall, K.S.; Steinberg, J.R.; Cwiak, C.A.; Allen, R.H.; Marcus, S.M. Contraception and mental health: A commentary on the evidence and principles for practice. Am. J. Obstet. Gynecol. 2015, 212, 740–746. [Google Scholar] [CrossRef]
- Mu, E.; Kulkarni, J. Hormonal contraception and mood disorders. Aust. Prescr. 2022, 45, 75–79. [Google Scholar] [CrossRef]
- Westhoff, C.L.; Heartwell, S.; Edwards, S.; Zieman, M.; Stuart, G.; Cwiak, C.; Davis, A.; Robilotto, T.; Cushman, L.; Kalmuss, D. Oral contraceptive discontinuation: Do side effects matter? Am. J. Obstet. Gynecol. 2007, 196, 412.e1–412.e6. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.S.; White, K.O.C.; Rickert, V.I.; Reame, N.; Carolyn Westhoff, C. Influence of depressed mood and psychological stress symptoms on perceived oral contraceptive side effects and discontinuation in young minority women. Contraception 2012, 86, 518–525. [Google Scholar] [CrossRef]
- Toffol, E.; Heikinheimo, O.; Koponen, P.; Luoto, R.; Partonen, T. Further evidence for lack of negative associations between hormonal contraception and mental health. Contraception 2012, 86, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Keyes, K.M.; Cheslack-Postava, K.; Westhoff, C.; Heim, C.M.; Haloossim, M.; Walsh, K.; Koenen, K. Association of hormonal contraceptive use with reduced levels of depressive symptoms: A national study of sexually active women in the United States. Am. J. Epidemiol. 2013, 178, 1378–1388. [Google Scholar] [CrossRef]
- Lundin, C.; Wikman, A.; Lampa, E.; Bixo, M.; Gemzell-Danielsson, K.; Wikman, P.; Ljung, R.; Sundström Poromaa, I. There is no association between combined oral hormonal contraceptives and depression: A Swedish register-based cohort study. BJOG 2022, 129, 917–925. [Google Scholar] [CrossRef]
- Hasler, G. Pathophysiology of depression: Do we have any solid evidence of interest to clinicians? World Psychiatry 2010, 9, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Dfarhud, D.; Malmir, M.; Khanahmadi, M. Happiness & Health: The Biological Factors—Systematic Review Article. Iran J. Public Health 2014, 43, 1468–1477. [Google Scholar] [PubMed]
- Rybaczyk, L.A.; Bashaw, M.J.; Pathak, D.R.; Moody, S.M.; Gilders, R.M.; Holzschu, D.L. An overlooked connection: Serotonergic mediation of estrogen-related physiology and pathology. BMC Womens Health 2005, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Del Río, J.P.; Alliende, M.I.; Molina, N.; Serrano, F.G.; Molina, S.; Vigil, P. Steroid hormones and their action in women’s brain: The importance of hormonal balance. Front. Public Health 2018, 6, 141. [Google Scholar] [CrossRef] [PubMed]
- Rapkin, A.J.; Akopians, A.L. Pathophysiology of premenstrual syndrome and premenstrual dysphoric disorder. Menopause Int. 2012, 18, 52–59. [Google Scholar] [CrossRef]
- Jiang, D.; Xie, T.; Liang, J.; Noble, P.W. β-Arrestins in the immune system. Prog. Mol. Biol. Transl. Sci. 2013, 118, 359–393. [Google Scholar]
- Smith, K.; Nayyar, S.; Rana, T.; Archibong, A.E.; Looney, K.R.; Nayyar, T. Do Progestin-Only Contraceptives Contribute to the Risk of Developing Depression as Implied by Beta-Arrestin 1 Levels in Leukocytes? A Pilot Study. Int. J. Environ. Res. Public Health 2018, 15, 1966. [Google Scholar] [CrossRef]
- Hughes, G.C. Progesterone and autoimmune disease. Autoimmun. Rev. 2012, 11, A502–A514. [Google Scholar] [CrossRef]
- Hall, O.; Klein, S. Progesterone-based compounds affect immune responses and susceptibility to infections at diverse mucosal sites. Mucosal Immunol. 2017, 10, 1097–1107. [Google Scholar] [CrossRef]
- Guennoun, R. Progesterone in the Brain: Hormone, Neurosteroid and Neuroprotectant. Int. J. Mol. Sci. 2020, 21, 5271. [Google Scholar] [CrossRef]
- Yu, K.; Huang, Z.Y.; Xu, X.L.; Li, J.; Fu, X.W.; Deng, S.L. Estrogen Receptor Function: Impact on the Human Endometrium. Front. Endocrinol. 2022, 13, 827724. [Google Scholar] [CrossRef]
- Mastorakos, G.; Pavlatou, M.; Diamanti-Kandarakis, E.; Chrousos, G.P. Exercise and the stress system. Hormones 2005, 4, 73–89. [Google Scholar]
- Alam, F.; Nayyar, S.; Richie, W.; Archibong, A.; Nayyar, T. Beta-Arrestin1 Levels in Mononuclear Leukocytes Support Depression Scores for Women with Premenstrual Dysphoric Disorder. Int. J. Environ. Res. Public Health 2016, 13, 0043. [Google Scholar] [CrossRef]
- Zwahlen, M.; Stute, P. Impact of progesterone on the immune system in women: A systematic literature review. Arch. Gynecol. Obstet. 2023, 18, 1–10. [Google Scholar] [CrossRef]
- Su, L.; Sun, Y.; Ma, F.; Lü, P.; Huang, H.; Zhou, J. Progesterone inhibits Toll-like receptor 4-mediated innate immune response in macrophages by suppressing NF-kappa B activation and enhancing SOCS1 expression. Immunol. Lett. 2009, 125, 151–155. [Google Scholar] [CrossRef]
- Lombardi, I.; Luisi, S.; Quirici, B.; Monteleone, P.; Bernardi, F.; Liut, M.; Casarosa, E.; Palumbo, M.; Petraglia, F.; Genazzani, A.R. Adrenal response to adrenocorticotropic hormone stimulation in patients with premenstrual syndrome. Gynecol. Endocrinol. 2004, 18, 79–87. [Google Scholar] [CrossRef]
- Ekholm, U.-B.; Turkmen, S.; Hammarb€ack, S.; B€ackstr€om, T. Sexuality and androgens in women with cyclical mood changes and pre-menstrual syndrome. Acta Obstet. Gynecol. Scand. 2014, 93, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Elgellaiea, A.; Larkina, T.; Kaelleb, J.; Mills JThomasa, S. Plasma prolactin is higher in major depressive disorder and females, and associated with anxiety, hostility, somatization, psychotic symptoms and heartrate. Compr. Psychoneuroendocrinol. 2021, 6, 100049. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Mukherjee, A.; Biswas, S.; Bose, S.; Nath, S.; Das, H.N. Evaluation of endocrine parameters as predictor of major depressive disorder. Indian J. Psychol. Med. 2017, 39, 766–769. [Google Scholar] [CrossRef] [PubMed]
- Kimball, A.; Dichtel, L.E.N.; Mischoulon, D.; Fisher, L.B.; Cusin, C.; Dording, C.M.; Trinh, N.-H.; Yeung, A.; Haines, M.S.; Joshua, C.; et al. The Allopregnanolone to Progesterone Ratio Across the Menstrual Cycle and in Menopause. Psychoneuroendocrinology 2020, 112, 104512. [Google Scholar] [CrossRef] [PubMed]
- King, S.R. Neurosteroids and the Nervous System; Springer: New York, NY, USA, 2013. [Google Scholar]
- Schüle, C.; Nothdurfter, C.; Rupprecht, R. The role of allopregnanolone in depression and anxiety. Prog. Neurobiol. 2014, 113, 79–87. [Google Scholar] [CrossRef]
- Rasmusson, A.M.; Lipschitz, D.S.; Wang, S.; Hu, S.; Vojvoda, D.; Bremner, J.D.; Southwick, S.M.; Charney, D.S. Increased pituitary and adrenal reactivity in premenopausal women with posttraumatic stress disorder. Biol. Psychiatry. 2001, 50, 965–977. [Google Scholar] [CrossRef]
- Mody, I.; Maguire, J. The reciprocal regulation of stress hormones and GABA(A) receptors. Front. Cell. Neurosci. 2011, 6, 4. [Google Scholar] [PubMed]
- Almeida, F.B.; Pinna, G.; Barros, H.M.T. The Role of HPA Axis and Allopregnanolone on the Neurobiology of Major Depressive Disorders and PTSD. Int. J. Mol. Sci. 2021, 22, 5495. [Google Scholar] [CrossRef] [PubMed]
- Rabi, A.; Khader, Y.; Alkafajei, A.; Aqoulah, A.A. Sanitary Conditions of Public Swimming Pools in Amman, Jordan. Int. J. Environ. Res. Public Health 2007, 4, 301–306. [Google Scholar] [CrossRef]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nayyar, S.; Archibong, A.; Nayyar, T. Testosterone and Prolactin Perturbations Possibly Associated with Reduced Levels of β-Arrestin1 in Mononuclear Leukocytes of Women with Premenstrual Dysphoric Disorder. Int. J. Mol. Sci. 2023, 24, 15449. https://doi.org/10.3390/ijms242015449
Nayyar S, Archibong A, Nayyar T. Testosterone and Prolactin Perturbations Possibly Associated with Reduced Levels of β-Arrestin1 in Mononuclear Leukocytes of Women with Premenstrual Dysphoric Disorder. International Journal of Molecular Sciences. 2023; 24(20):15449. https://doi.org/10.3390/ijms242015449
Chicago/Turabian StyleNayyar, Sanket, Anthony Archibong, and Tultul Nayyar. 2023. "Testosterone and Prolactin Perturbations Possibly Associated with Reduced Levels of β-Arrestin1 in Mononuclear Leukocytes of Women with Premenstrual Dysphoric Disorder" International Journal of Molecular Sciences 24, no. 20: 15449. https://doi.org/10.3390/ijms242015449
APA StyleNayyar, S., Archibong, A., & Nayyar, T. (2023). Testosterone and Prolactin Perturbations Possibly Associated with Reduced Levels of β-Arrestin1 in Mononuclear Leukocytes of Women with Premenstrual Dysphoric Disorder. International Journal of Molecular Sciences, 24(20), 15449. https://doi.org/10.3390/ijms242015449




