Exploring the mRNA and Plasma Protein Levels of BDNF, NT4, SIRT1, HSP27, and HSP70 in Multiple Sclerosis Patients and Healthy Controls
Abstract
:1. Introduction
2. Results
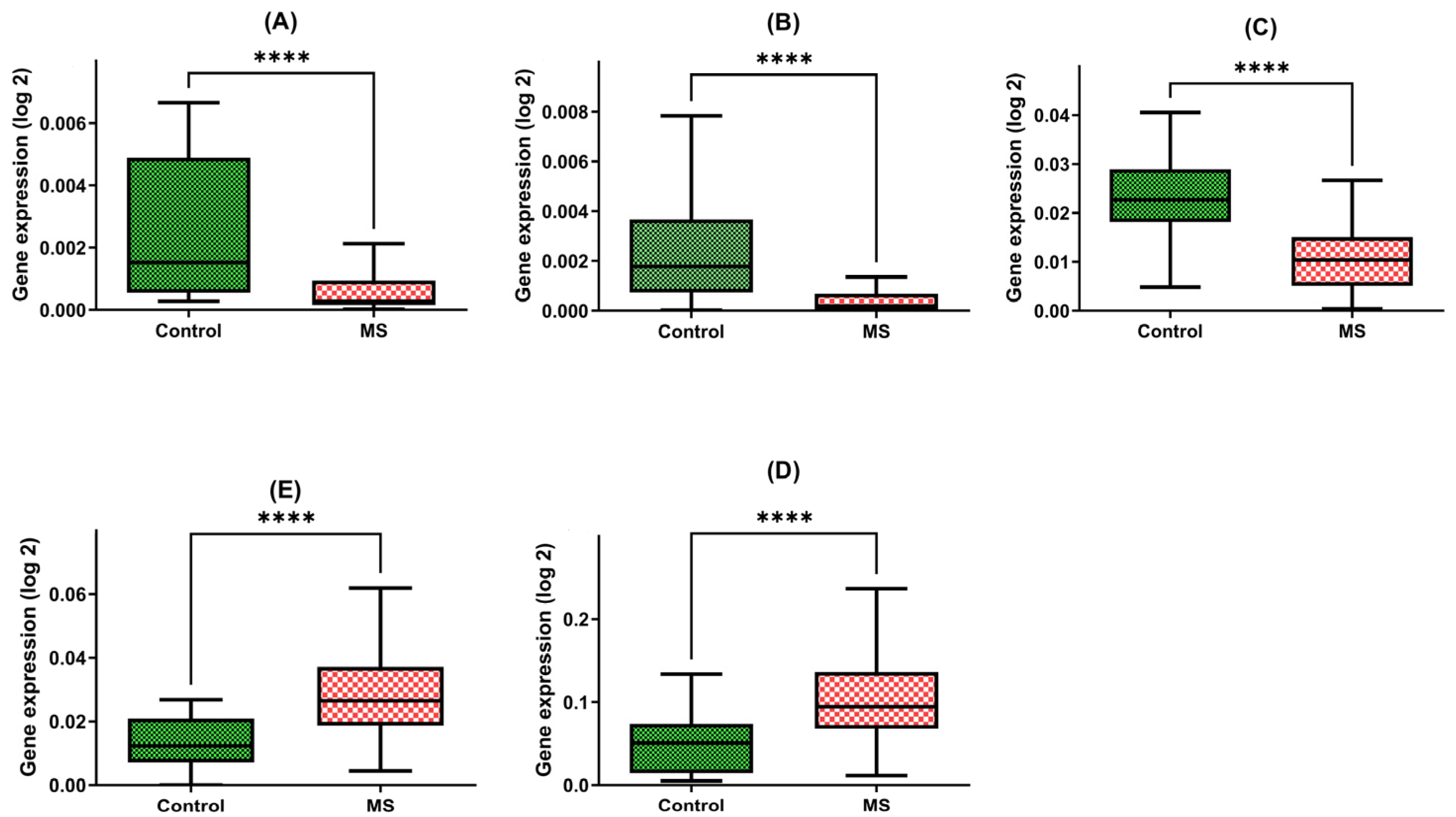
2.1. Gene Expression Levels of Neurotrophins (BDNF and NT4/5), Heat Shock Proteins (HSP70 and HSP27), and Sirtuin-1 (SIRT1) in PBMCs in Patients with Multiple Sclerosis
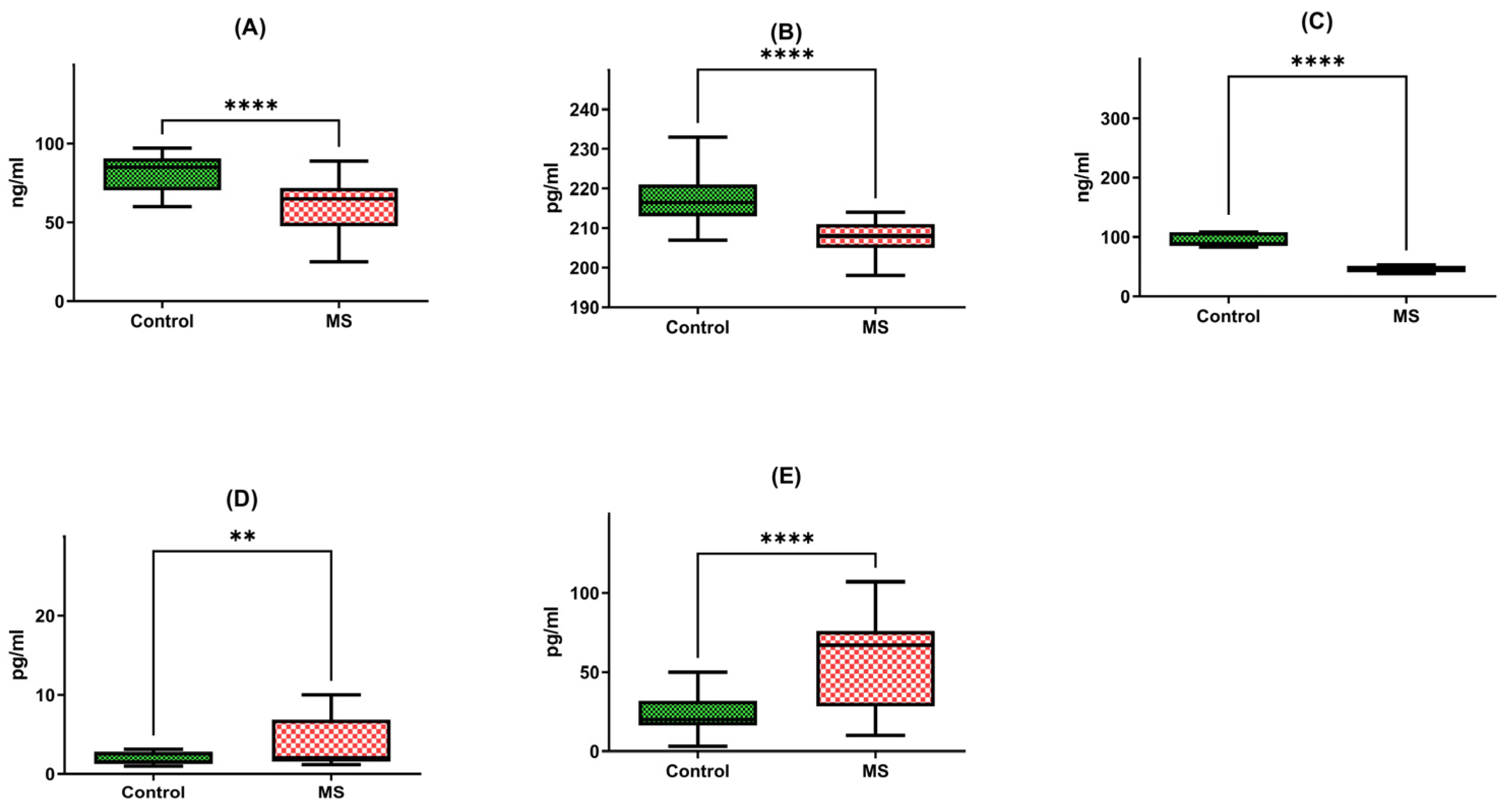
2.2. Plasma Protein Levels Assessed through ELISA Testing
2.3. Correlation of the Gene Expression Level and Protein Concentration
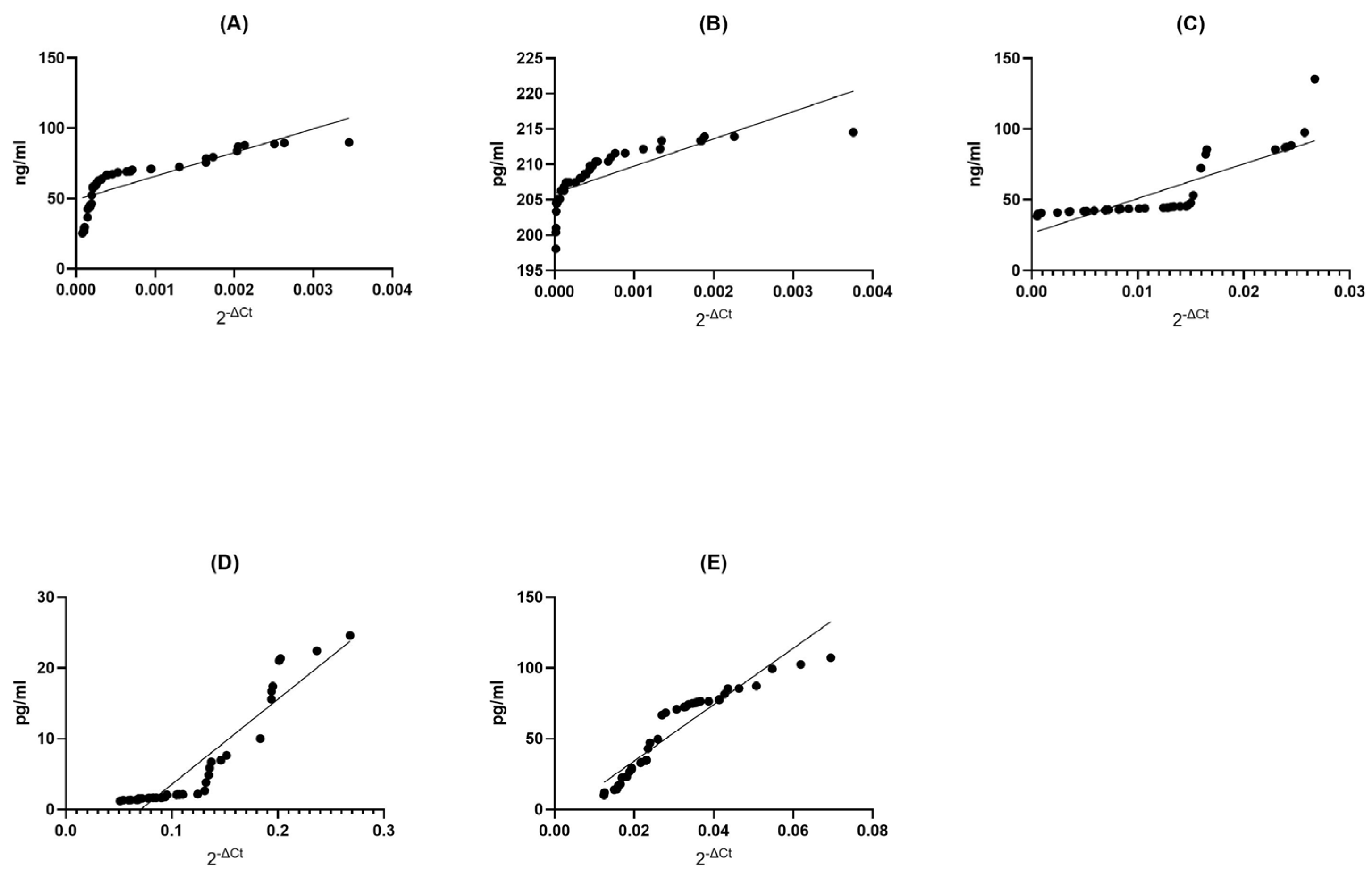
2.3.1. Correlation between Gene Expression and Protein Concentration in Multiple Sclerosis Groups
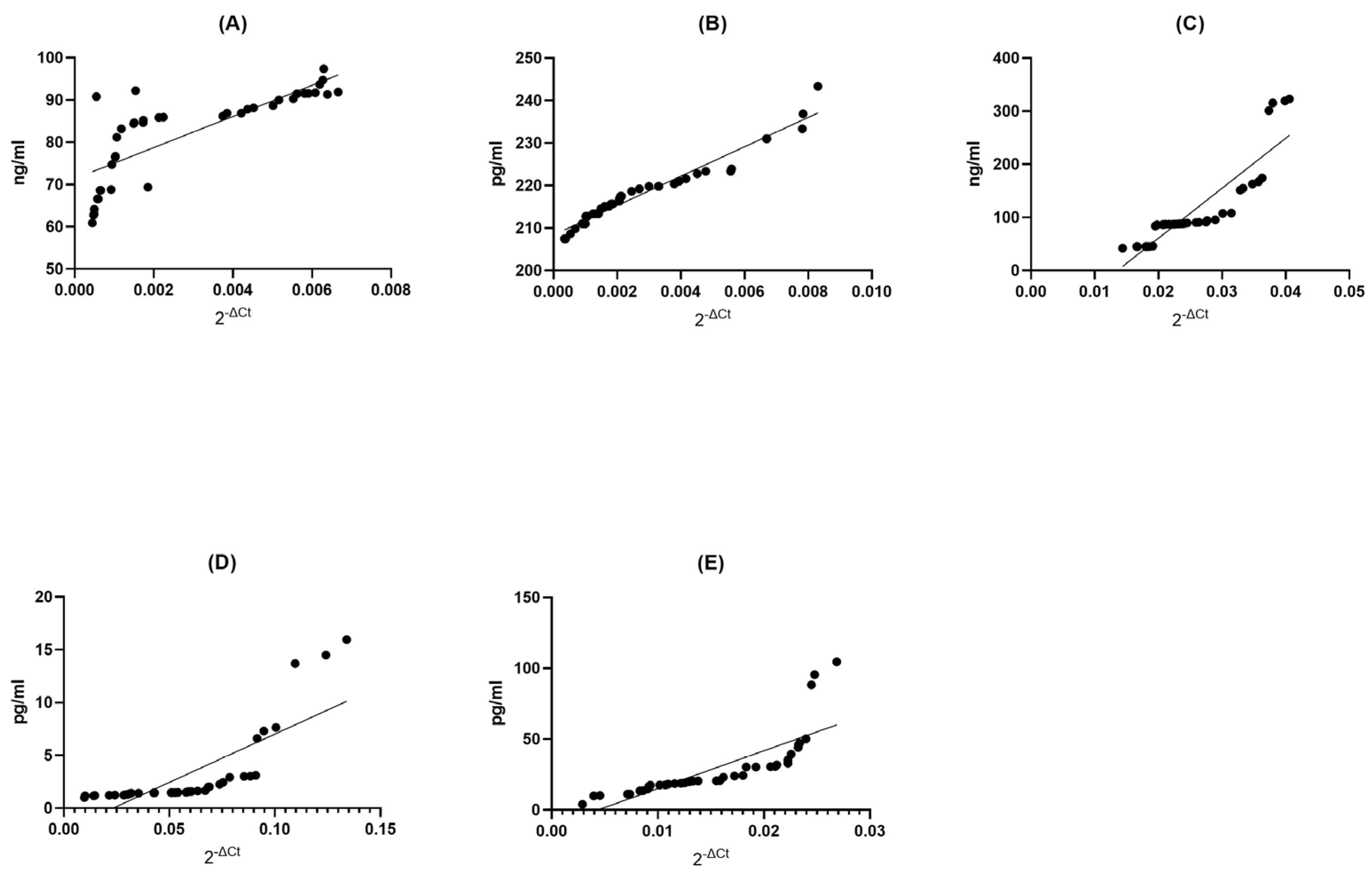
2.3.2. Correlation between Gene Expression and Protein Concentration in Healthy Donors Groups
2.3.3. Summary of Correlation Analysis
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Methods
4.2.1. Blood Sample Collection, RNA Preparation, and Reverse Transcription Quantitative Real-Time PCR RNA: Isolation and cDNA Synthesis
4.2.2. Plasma Sample Collection, ELISA Test
4.2.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wallin, M.T.; Culpepper, W.J.; Campbell, J.D.; Nelson, L.M.; Langer-Gould, A.; Marrie, R.A.; Cutter, G.R.; Kaye, W.E.; Wagner, L.; Tremlett, H.; et al. The prevalence of MS in the United States. Neurology 2019, 92, e1029–e1040. [Google Scholar] [CrossRef] [PubMed]
- Dutta, R.; Trapp, B.D. Relapsing and progressive forms of multiple sclerosis: Insights from pathology. Curr. Opin. Neurol. 2014, 27, 271–278. Available online: https://www.ncbi.nlm.nih.gov/pubmed/24722325 (accessed on 6 November 2023).
- Reich, D.S.; Lucchinetti, C.F.; Calabresi, P.A. Multiple Sclerosis. N. Engl. J. Med. 2018, 378, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Sawcer, S.; Hellenthal, G.; Pirinen, M.; Spencer, C.C.A.; Patsopoulos, N.A.; Moutsianas, L.; Dilthey, A.; Su, Z.; Freeman, C.; Hunt, S. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature 2011, 476, 214–219. [Google Scholar]
- Mortazavi, M.; Hizarci, Ö; Gerdes, L.A.; Havla, J.; Kümpfel, T.; Hohlfeld, R.; Stöcklein, S.; Keeser, D.; Ertl-Wagner, B. Multiple sclerosis and subclinical neuropathology in healthy individuals with familial risk: A scoping review of MRI studies. NeuroImage Clin. 2021, 31, 102734. [Google Scholar]
- Patsopoulos, N.A. Genetics of multiple sclerosis: An overview and new directions. Cold Spring Harb. Perspect. Med. 2018, 8, a028951. [Google Scholar]
- International Multiple Sclerosis Genetics Consortium. Multiple sclerosis genomic map implicates peripheral immune cells and microglia in susceptibility. Science 2019, 365, eaav7188. [Google Scholar]
- Oksenberg, J.R.; Baranzini, S.E. Multiple sclerosis geneticsĝ€″is the glass half full, or half empty? Nat. Rev. Neurol. 2010, 6, 429–439. [Google Scholar]
- Simpson, S.; Blizzard, L.; Otahal, P.; Van Der Mei, I.; Taylor, B. Latitude is significantly associated with the prevalence of multiple sclerosis: A meta-analysis. J. Neurol. Neurosurg. Psychiatry 2011, 82, 1132–1141. [Google Scholar] [CrossRef]
- Sintzel, M.B.; Rametta, M.; Reder, A.T. Vitamin D and Multiple Sclerosis: A Comprehensive Review. Neurol. Ther. 2018, 7, 59–85. [Google Scholar]
- Simpson, S.; Taylor, B.V.; Van Der Mei, I. The role of epidemiology in MS research: Past successes, current challenges and future potential. Mult. Scler. J. 2015, 21, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.; Jakimovski, D.; Ramanathan, M.; Weinstock-Guttman, B.; Zivadinov, R. The role of Epstein-Barr virus in multiple sclerosis: From molecular pathophysiology to in vivo imaging. Neural Regen. Res. 2019, 14, 373–386. [Google Scholar] [PubMed]
- Didonna, A.; Oksenberg, J.R. Genetic determinants of risk and progression in multiple sclerosis. Clin. Chim. Acta 2015, 449, 16–22. [Google Scholar]
- James, T.; Lindén, M.; Morikawa, H.; Fernandes, S.J.; Ruhrmann, S.; Huss, M.; Brandi, M.; Piehl, F.; Jagodic, M.; Tegnér, J.; et al. Impact of genetic risk loci for multiple sclerosis on expression of proximal genes in patients. Hum. Mol. Genet. 2018, 27, 912–928. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Poo, M.M. Neurotrophin regulation of neural circuit development and function. Nat. Rev. Neurosci. 2013, 14, 7–23. [Google Scholar] [PubMed]
- Lu, B.; Nagappan, G.; Guan, X.; Nathan, P.J.; Wren, P. BDNF-based synaptic repair as a disease-modifying strategy for neurodegenerative diseases. Nat. Rev. Neurosci. 2013, 14, 401–416. [Google Scholar] [PubMed]
- Minichiello, L. TrkB signalling pathways in LTP and learning. Nat. Rev. Neurosci. 2009, 10, 850–860. [Google Scholar]
- Bekinschtein, P.; Cammarota, M.; Medina, J.H. BDNF and memory processing. Neuropharmacology 2014, 76, 677–683. [Google Scholar] [CrossRef]
- Chen, Z.Y.; Jing, D.; Bath, K.G.; Ieraci, A.; Khan, T.; Siao, C.J.; Herrera, D.G.; Toth, M.; Yang, C.; McEwen, B.S.; et al. Genetic Variant BDNF (Val66Met) Polymorphism Alters Anxiety-Related Behavior. Science 2006, 314, 140–143. Available online: http://www.sciencemag.org (accessed on 6 November 2023). [CrossRef]
- Nieto, R.; Kukuljan, M.; Silva, H. BDNF and schizophrenia: From neurodevelopment to neuronal plasticity, learning, and memory. Front. Psychiatry 2013, 4, 45. [Google Scholar] [CrossRef]
- Gao, L.; Zhang, Y.; Sterling, K.; Song, W. Brain-derived neurotrophic factor in Alzheimer’s disease and its pharmaceutical potential. Transl. Neurodegener. 2022, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.L.; Spinhoven, P.; Polak, M.; Bus, B.A.A.; Penninx, B.W.J.H.; Elzinga, B.M. Serum BDNF concentrations as peripheral manifestations of depression: Evidence from a systematic review and meta-analyses on 179 associations (N = 9484). Mol. Psychiatry 2014, 19, 791–800. [Google Scholar] [PubMed]
- Kalinowska-Lyszczarz, A.; Losy, J. The role of neurotrophins in multiple sclerosis-pathological and clinical implications. Int. J. Mol. Sci. 2012, 13, 13713–13725. [Google Scholar]
- Torres-Cruz, F.M.; César Vivar-Cortés, I.; Moran, I.; Mendoza, E.; Gómez-Pineda, V.; García-Sierra, F.; Hernández-Echeagaray, E. NT-4/5 antagonizes the BDNF modulation of corticostriatal transmission: Role of the TrkB.T1 receptor. CNS Neurosci. Ther. 2019, 25, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Haigis, M.C.; Sinclair, D.A. Mammalian sirtuins: Biological insights and disease relevance. Annu. Rev. Pathol. Mech. Dis. 2010, 5, 253–295. [Google Scholar] [CrossRef]
- Herskovits, A.Z.; Guarente, L. Sirtuin deacetylases in neurodegenerative diseases of aging. Cell Res. 2013, 23, 746–758. [Google Scholar]
- Guarente, L.; Picard, F. Calorie restriction—The SIR2 connection. Cell 2005, 120, 473–482. [Google Scholar] [CrossRef]
- Beretta, G.; Shala, A.L. Impact of Heat Shock Proteins in Neurodegeneration: Possible Therapeutical Targets. Ann. Neurosci. 2022, 29, 71–82. [Google Scholar] [CrossRef]
- Mymrikov, E.V.; Seit-Nebi, A.S.; Gusev, N.B. Large Potentials of Small Heat Shock Proteins. Physiol. Rev. 2011, 91, 1123–1159. Available online: http://www.prv.org (accessed on 6 November 2023).
- Foster, J.A.; Brown, I.R. Differential induction of heat shock mRNA in oligodendrocytes, microglia, and astrocytes following hyperthermia. Mol. Brain Res. 1997, 45, 207–218. [Google Scholar] [CrossRef]
- Turturici, G.; Tinnirello, R.; Sconzo, G.; Asea, A.; Savettieri, G.; Ragonese, P.; Geraci, F. Positive or Negative Involvement of Heat Shock Proteins in Multiple Sclerosis Pathogenesis: An Overview. J. Neuropathol. Exp. Neurol. 2014, 73, 1092–1106. [Google Scholar]
- Nociti, V. What is the role of Brain derived neurotrophic factor in Multiple Sclerosis neuroinflammation? Neuroimmunol. Neuroinflammation 2020, 7, 291–299. [Google Scholar] [CrossRef]
- Islas-Hernandez, A.; Aguilar-Talamantes, H.S.; Bertado-Cortes, B.; Mejia-Delcastillo, G.d.J.; Carrera-Pineda, R.; Cuevas-Garcia, C.F.; Garcia-Delatorre, P. BDNF and Tau as biomarkers of severity in multiple sclerosis. Biomark. Med. 2018, 12, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Karimi, N.; Ashourizadeh, H.; Pasha, B.A.; Haghshomar, M.; Jouzdani, T.; Shobeiri, P.; Teixeira, A.L.; Rezaei, N. Blood levels of brain-derived neurotrophic factor (BDNF) in people with multiple sclerosis (MS): A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2022, 65, 103984. [Google Scholar] [CrossRef] [PubMed]
- Wens, I.; Keytsman, C.; Deckx, N.; Cools, N.; Dalgas, U.; Eijnde, B.O. Brain derived neurotrophic factor in multiple sclerosis: Effect of 24 weeks endurance and resistance training. Eur. J. Neurol. 2016, 23, 1028–1035. [Google Scholar] [CrossRef]
- Azoulay, D.; Vachapova, V.; Shihman, B.; Miler, A.; Karni, A. Lower brain-derived neurotrophic factor in serum of relapsing remitting MS: Reversal by glatiramer acetate. J. Neuroimmunol. 2005, 167, 215–218. [Google Scholar] [CrossRef]
- Azoulay, D.; Urshansky, N.; Karni, A. Low and dysregulated BDNF secretion from immune cells of MS patients is related to reduced neuroprotection. J. Neuroimmunol. 2008, 195, 186–193. [Google Scholar] [CrossRef]
- Comini-Frota, E.R.; Rodrigues, D.H.; Miranda, E.C.; Brum, D.G.; Kaimen-Maciel, D.R.; Donadi, E.A.; Teixeira, A.L. Serum levels of brain-derived neurotrophic factor correlate with the number of T2 MRI lesions in multiple sclerosis. Braz. J. Med. Biol. Res. 2012, 45, 68–71. [Google Scholar] [CrossRef]
- Nagahara, A.H.; Merrill, D.A.; Coppola, G.; Tsukada, S.; Schroeder, B.E.; Shaked, G.M.; Wang, L.; Blesch, A.; Kim, A.; Conner, J.M.; et al. Neuroprotective effects of brain-derived neurotrophic factor in rodent and primate models of Alzheimer’s disease. Nat. Med. 2009, 15, 331–337. [Google Scholar] [CrossRef]
- Zuccato, C.; Ciammola, A.; Rigamonti, D.; Leavitt, B.R.; Goffredo, D.; Conti, L.; MacDonald, M.E.; Friedlander, R.M.; Silani, V.; Hayden, M.R.; et al. Loss of Huntingtin-Mediated BDNF Gene Transcription in Huntington’s Disease. Science 2001, 293, 493–498. [Google Scholar] [CrossRef]
- Petereit, H.F.; Lindemann, H.; Schoppe, S. Effect of immunomodulatory drugs on in vitro production of brain-derived neurotrophic factor. Mult. Scler. 2003, 9, 16–20. [Google Scholar] [CrossRef]
- Liguori, M.; Fera, F.; Patitucci, A.; Manna, I.; Condino, F.; Valentino, P.; Telarico, P.; Cerasa, A.; Gioia, M.C.; di Palma, G.; et al. A longitudinal observation of Brain-Derived Neurotrophic Factor mRNA levels in patients with Relapsing-Remitting Multiple Sclerosis. Brain Res. 2009, 1256, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Frota, E.R.C.; Rodrigues, D.H.; Donadi, E.A.; Brum, D.G.; Maciel, D.R.K.; Teixeira, A.L. Increased plasma levels of brain derived neurotrophic factor (BDNF) after multiple sclerosis relapse. Neurosci. Lett. 2009, 460, 130–132. [Google Scholar] [CrossRef] [PubMed]
- Oraby, M.I.; El Masry, H.A.; Abd El Shafy, S.S.; Abdul Galil, E.M. Serum level of brain-derived neurotrophic factor in patients with relapsing–remitting multiple sclerosis: A potential biomarker for disease activity. Egypt. J. Neurol. Psychiatry Neurosurg. 2021, 57, 40. [Google Scholar] [CrossRef]
- Caggiula, M.; Batocchi, A.P.; Frisullo, G.; Angelucci, F.; Patanella, A.K.; Sancricca, C.; Nociti, V.; Tonali, P.A.; Mirabella, M. Neurotrophic Factors and Clinical Recovery in Relapsing-Remitting Multiple Sclerosis. Scand. J. Immunol. 2005, 62, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, S.; Ochi, H.; Matsushita, T. Altered Production of Brain-derived neurotrophic factor by peripheral blood immune cells in multiple sclerosis. Mult. Scler. J. 2010, 16, 1178–1188. Available online: https://hdl.handle.net/2324/26026 (accessed on 6 November 2023). [CrossRef]
- Trushnikova, T.N.; Medvedeva, E.L.; Baĭdina, T.V.; Danilova, M.A. Brain-derived and ciliary neurotrophic factors in patients with multiple sclerosis. Zhurnal Nevrol. I Psikhiatrii Im. SS Korsakova 2014, 114 Pt 2, 33–36. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25591532 (accessed on 6 November 2023).
- Sarchielli, P.; Zaffaroni, M.; Floridi, A.; Greco, L.; Candeliere, A.; Mattioni, A.; Tenaglia, S.; Di Filippo, M.; Calabresi, P. Production of brain-derived neurotrophic factor by mononuclear cells of patients with multiple sclerosis treated with glatiramer acetate, interferon-β 1a, and high doses of immunoglobulins. Mult. Scler. J. 2007, 13, 313–331. [Google Scholar] [CrossRef]
- Damasceno, A.; Damasceno, B.P.; Cendes, F.; Moraes, A.S.; Farias, A.; Dos Santos, L.M.B. Serum BDNF levels are not reliable correlates of neurodegeneration in MS patients. Mult. Scler. Relat. Disord. 2015, 4, 65–66. [Google Scholar] [CrossRef]
- Lalive, P.H.; Kantengwa, S.; Benkhoucha, M.; Juillard, C.; Chofflon, M. Interferon-β induces brain-derived neurotrophic factor in peripheral blood mononuclear cells of multiple sclerosis patients. J. Neuroimmunol. 2008, 197, 147–151. [Google Scholar] [CrossRef]
- Gold, S.M.; Schulz, K.-H.; Hartmann, S.; Mladek, M.; Lang, U.E.; Hellweg, R.; Reer, R.; Braumann, K.-M.; Heesen, C. Basal serum levels and reactivity of nerve growth factor and brain-derived neurotrophic factor to standardized acute exercise in multiple sclerosis and controls. J. Neuroimmunol. 2003, 138, 99–105. [Google Scholar] [CrossRef]
- Emamgholipour, S.; Hossein-Nezhad, A.; Sahraian, M.A.; Askarisadr, F.; Ansari, M. Evidence for possible role of melatonin in reducing oxidative stress in multiple sclerosis through its effect on SIRT1 and antioxidant enzymes. Life Sci. 2016, 145, 34–41. [Google Scholar] [CrossRef]
- Hewes, D.; Tatomir, A.; Kruszewski, A.M.; Rao, G.; Tegla, C.A.; Ciriello, J.; Nguyen, V.; Royal, W., III; Bever, C.; Rus, V.; et al. SIRT1 as a potential biomarker of response to treatment with glatiramer acetate in multiple sclerosis. Exp. Mol. Pathol. 2017, 102, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Tegla, C.A.; Azimzadeh, P.; Andrian-Albescu, M.; Martin, A.; Cudrici, C.D.; Trippe, R.; Sugarman, A.; Chen, H.; Boodhoo, D.; Vlaicu, S.I.; et al. SIRT1 is decreased during relapses in patients with multiple sclerosis. Exp. Mol. Pathol. 2014, 96, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Ciriello, J.; Tatomir, A.; Hewes, D.; Boodhoo, D.; Anselmo, F.; Rus, V.; Rus, H. Phosphorylated SIRT1 as a biomarker of relapse and response to treatment with glatiramer acetate in multiple sclerosis. Exp. Mol. Pathol. 2018, 105, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Pennisi, G.; Cornelius, C.; Cavallaro, M.; Salinaro, A.T.; Cambria, M.; Pennisi, M.; Bella, R.; Milone, P.; Ventimiglia, B.; Migliore, M.; et al. Redox regulation of cellular stress response in multiple sclerosis. Biochem. Pharmacol. 2011, 82, 1490–1499. [Google Scholar] [CrossRef]
- Kubiliute, A.; Gedvilaite, G.; Vilkeviciute, A.; Kriauciuniene, L.; Bruzaite, A.; Zaliuniene, D.; Liutkeviciene, R. The role of SIRT1 level and SIRT1 gene polymorphisms in optic neuritis patients with multiple sclerosis. Orphanet J. Rare Dis. 2023, 18, 64. [Google Scholar] [CrossRef]
- Kalinowska-Łyszczarz, A.; Pawlak, M.A.; Wyciszkiewicz, A.; Osztynowicz, K.; Kozubski, W.; Michalak, S. Immune-cell BDNF expression in treatment-naïve relapsing-remitting multiple sclerosis patients and following one year of immunomodulation therapy. Neurol. I Neurochir. Pol. 2018, 52, 483–489. [Google Scholar] [CrossRef]
- Piotrzkowska, D.; Miller, E.; Kucharska, E.; Niwald, M.; Majsterek, I. Association of mirna and mrna levels of the clinical onset of multiple sclerosis patients. Biology 2021, 10, 554. [Google Scholar] [CrossRef]
- Ce, P.; Erkizan, O.; Gedizlioglu, M. Elevated HSP27 levels during attacks in patients with multiple sclerosis. Acta Neurol. Scand. 2011, 124, 317–320. [Google Scholar] [CrossRef]
- Hecker, J.G.; Sundram, H.; Zou, S.; Praestgaard, A.; Bavaria, J.E.; Ramchandren, S.; McGarvey, M. Heat shock proteins HSP70 and HSP27 in the cerebral spinal fluid of patients undergoing thoracic aneurysm repair correlate with the probability of postoperative paralysis. Cell Stress Chaperones 2008, 13, 435–446. [Google Scholar] [CrossRef]
- Lechner, P.; Buck, D.; Sick, L.; Hemmer, B.; Multhoff, G. Serum heat shock protein 70 levels as a biomarker for inflammatory processes in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2018, 4. [Google Scholar] [CrossRef] [PubMed]
- Koren, J.; Jinwal, U.K.; Lee, D.C.; Jones, J.R.; Shults, C.L.; Johnson, A.G.; Anderson, L.J.; Dickey, C.A. Chaperone signalling complexes in Alzheimer’s disease. J. Cell. Mol. Medicine. 2009, 13, 619–630. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.B.; Huang, G.X.; Lu, J.J.; Ma, J.; Yuan, Q.J.; Cao, Y.; Zhu, L. Up-regulation of heat shock protein 27 inhibits apoptosis in lumbosacral nerve root avulsion-induced neurons. Sci. Rep. 2019, 9, 11468. [Google Scholar] [CrossRef]
- Bartelt-Kirbach, B.; Golenhofen, N. Reaction of small heat-shock proteins to different kinds of cellular stress in cultured rat hippocampal neurons. Cell Stress Chaperones 2014, 19, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Li, H.F.; Zhang, H.L. Elevated HSP27 levels during attacks in patients with multiple sclerosis. Acta Neurol. Scand. 2012, 126, e8–e9. [Google Scholar] [CrossRef] [PubMed]
- Nova, A.; Fazia, T.; Beecham, A.; Saddi, V.; Piras, M.; McCauley, J.L.; Berzuini, C.; Bernardinelli, L. Plasma Protein Levels Analysis in Multiple Sclerosis Sardinian Families Identified C9 and CYP24A1 as Candidate Biomarkers. Life 2022, 12, 151. [Google Scholar] [CrossRef]
| MS Group | Control Group | |
|---|---|---|
| Number of subjects | 45 | 48 |
| Females/males | 27/18 | 28/20 |
| Age (years, mean +/−SD) | 56/4.5 | 54/5.5 |
| Expanded disability status scale (EDSS) at the stable phase (range) | 5.5 ± 1.0 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sokolowski, I.; Kucharska-Lusina, A.; Miller, E.; Majsterek, I. Exploring the mRNA and Plasma Protein Levels of BDNF, NT4, SIRT1, HSP27, and HSP70 in Multiple Sclerosis Patients and Healthy Controls. Int. J. Mol. Sci. 2023, 24, 16176. https://doi.org/10.3390/ijms242216176
Sokolowski I, Kucharska-Lusina A, Miller E, Majsterek I. Exploring the mRNA and Plasma Protein Levels of BDNF, NT4, SIRT1, HSP27, and HSP70 in Multiple Sclerosis Patients and Healthy Controls. International Journal of Molecular Sciences. 2023; 24(22):16176. https://doi.org/10.3390/ijms242216176
Chicago/Turabian StyleSokolowski, Igor, Aleksandra Kucharska-Lusina, Elzbieta Miller, and Ireneusz Majsterek. 2023. "Exploring the mRNA and Plasma Protein Levels of BDNF, NT4, SIRT1, HSP27, and HSP70 in Multiple Sclerosis Patients and Healthy Controls" International Journal of Molecular Sciences 24, no. 22: 16176. https://doi.org/10.3390/ijms242216176





