Anti-Incretin Gut Features Induced by Feed Supplementation with Alpha-Amylase: Studies on EPI Pigs
Abstract
:1. Introduction
2. Results
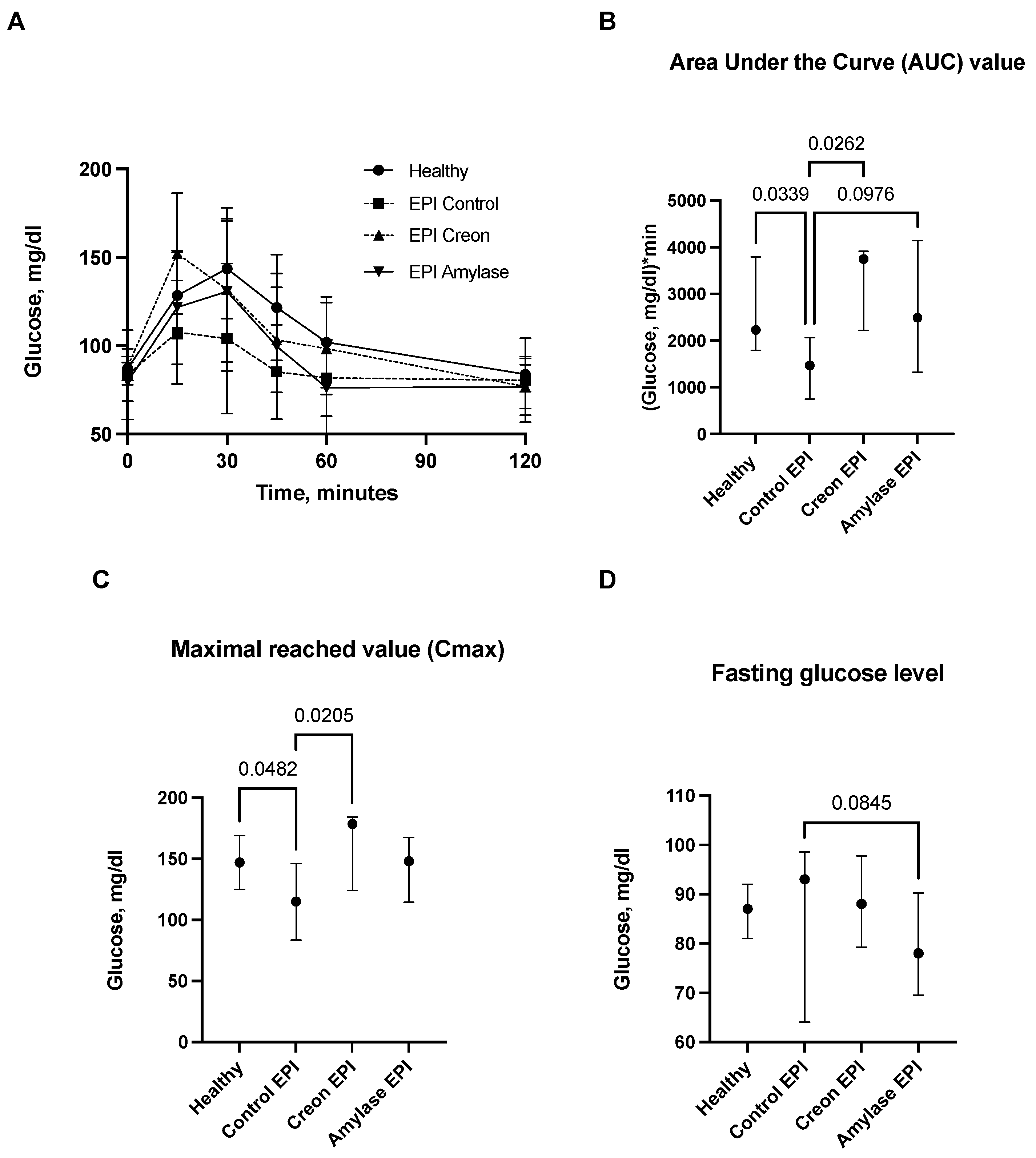
2.1. Glucose Absorption
2.2. Insulin Release and HOMA-IR Index
2.3. Glucagon-Like-Peptide 1 (GLP1) and Glucose-Dependent Insulinotropic Polypeptide/Gastric Inhibitory Polypeptide (GIP)
2.4. Body Weight Gain
3. Discussion
3.1. Study Limitations
3.2. Conclusions and Future Directions
4. Materials and Methods
4.1. Animals
4.2. Feed and Enzyme Administration
4.3. Enzymes
4.4. Study Flow
4.5. Blood Sampling
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnesjö, I.I.; Lundquist, I. Effects on Exocrine and Endocrine Rat Pancreas of Long-Term Administration of CCK-PZ (Cholecystokinin-Pancreozymin) or Synthetic Octapeptide—CCK-PZ. Scand J. Gastroenterol. 1976, 11, 529–535. [Google Scholar] [PubMed]
- Schneeman, B.O.; Inman, M.D.; Stern, J.S. Pancreatic Enzyme Activity in Obese and Lean Zucker Rats: A Developmental Study. J. Nutr. 1983, 113, 921–925. [Google Scholar] [CrossRef] [PubMed]
- Kondo, T.; Hayakawa, T.; Shibata, T.; Sato, Y.; Toda, Y. Serum Levels of Pancreatic Enzymes in Lean And Obese Subjects. Int. J. Pancreatol. 1988, 3, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, K.; Muneyuki, T.; Munakata, H.; Kakei, M. Revisiting the Cardiometabolic Relevance of Serum Amylase. BMC Res. Notes 2011, 4, 419. [Google Scholar] [CrossRef] [PubMed]
- Muneyuki, T.; Nakajima, K.; Aoki, A.; Yoshida, M.; Fuchigami, H.; Munakata, H.; Ishikawa, S.E.; Sugawara, H.; Kawakami, M.; Momomura, S.; et al. Latent Associations of Low Serum Amylase with Decreased Plasma Insulin Levels and Insulin Resistance in Asymptomatic Middle-Aged Adults. Cardiovasc. Diabetol. 2012, 11, 80. [Google Scholar] [CrossRef]
- Mandel, A.L.; Breslin, P.A. High Endogenous Salivary Amylase Activity is Associated with Improved Glycemic Homeostasis Following Starch Ingestion in Adults. J. Nutr. 2012, 142, 853–858. [Google Scholar] [CrossRef]
- Falchi, M.; El-Sayed Moustafa, J.S.; Takousis, P.; Pesce, F.; Bonnefond, A.; Andersson-Assarsson, J.C.; Sudmant, P.H.; Dorajoo, R.; Al-Shafai, M.N.; Bottolo, L.; et al. Low Copy Number of the Salivary Amylase Gene Predisposes to Obesity. Nat. Genet. 2014, 46, 492–497. [Google Scholar] [CrossRef]
- Choi, Y.J.; Nam, Y.S.; Yun, J.M.; Park, J.H.; Cho, B.L.; Son, H.Y.; Kim, J.I.; Yun, J.W. Association Between Salivary Amylase (AMY1) Gene Copy Numbers and Insulin Resistance in Asymptomatic Korean Men. Diabet. Med. 2015, 32, 1588–1595. [Google Scholar] [CrossRef]
- Elder, P.J.D.; Ramsden, D.B.; Burnett, D.; Weickert, M.O.; Barber, T.M. Human Amylase Gene Copy Number Variation as a Determinant of Metabolic State. Expert Rev. Endocrinol. Metab. 2018, 13, 193–205. [Google Scholar] [CrossRef]
- Ko, J.; Cho, J.; Petrov, M.S. Low Serum Amylase, Lipase, and Trypsin as Biomarkers of Metabolic Disorders: A Systematic Review and Meta-Analysis. Diabetes Res. Clin. Pract. 2020, 159, 107974. [Google Scholar] [CrossRef]
- Zhan, F.; Chen, J.; Yan, H.; Wang, S.; Zhao, M.; Zhang, S.; Lan, X.; Maekawa, M. Association of Serum Amylase Activity and the Copy Number Variation of AMY1/2A/2B with Metabolic Syndrome in Chinese Adults. Diabetes Metab. Syndr. Obes. 2021, 14, 4705–4714. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, K. Low Serum Amylase and Obesity, Diabetes and Metabolic Syndrome: A Novel Interpretation. World J. Diabetes 2016, 7, 112–121. [Google Scholar] [CrossRef]
- Williams, J.A.; Goldfine, I.D. The Insulin-Pancreatic Acinar Axis. Diabetes 1985, 34, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Pierzynowski, S.G.; Goncharova, K.; Woliński, J.; Prykhodko, O.; Weström, B.; Lozinska, L. Enteral Pancreatic-like Enzymes of Microbial Origin Affect Insulin Release during an Intravenous Glucose Tolerance Test. J. Diabetes Metab. 2016, 7, 681. [Google Scholar] [CrossRef]
- Pierzynowska, K.G.; Lozinska, L.; Woliński, J.; Pierzynowski, S. The Inverse Relationship between Blood Amylase and Insulin Levels in Pigs during Development, Bariatric Surgery, and Intravenous Infusion of Amylase. PLoS ONE 2018, 13, e0198672. [Google Scholar] [CrossRef]
- Asanuma-Date, K.; Hirano, Y.; Le, N.; Sano, K.; Kawasaki, N.; Hashii, N.; Hiruta, Y.; Nakayama, K.I.; Umemura, M.; Ishikawa, K.; et al. Functional Regulation of Sugar Assimilation by N-Glycan-Specific Interaction of Pancreatic α-Amylase with Glycoproteins of Duodenal Brush Border Membrane. J. Biol. Chem. 2012, 287, 23104–23118. [Google Scholar] [CrossRef]
- Date, K.; Satoh, A.; Iida, K.; Ogawa, H. Pancreatic α-Amylase Controls Glucose Assimilation by Duodenal Retrieval through N-Glycan-specific Binding, Endocytosis, and Degradation. J. Biol. Chem. 2015, 290, 17439–17450. [Google Scholar] [CrossRef]
- Zhou, H.; Wu, Y.; Sun, X.; Yin, D.; Wang, Y.; Mahmood, T.; Yuan, J. Effects of Exogenous α-(1,4)-Amylase on the Utilisation of Corn Starch and Glucose Metabolism in Broiler Chickens. Animal 2021, 15, 100396. [Google Scholar] [CrossRef]
- Pierzynowski, S.G.; Stier, C.; Pierzynowska, K. Hypothesis That Alpha-Amylase Evokes Regulatory Mechanisms Originating in the Pancreas, Gut and Circulation, Which Govern Glucose/Insulin Homeostasis. World J. Diabetes 2023, 14, 1341–1348. [Google Scholar] [CrossRef]
- Pierzynowski, S.G.; Gregory, P.C.; Filip, R.; Woliński, J.; Pierzynowska, K.G. Glucose Homeostasis Dependency on Acini–Islet–Acinar (AIA) Axis Communication: A New Possible Pathophysiological Hypothesis Regarding Diabetes Mellitus. Nutr. Diabetes 2018, 8, 55. [Google Scholar] [CrossRef]
- Date, K.; Yamazaki, T.; Toyoda, Y.; Hoshi, K.; Ogawa, H. A-Amylase Expressed in Human Small Intestinal Epithelial Cells is Essential for Cell Proliferation and Differentiation. J. Cell Biochem. 2020, 121, 1238–1249. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Abe, Y.; Nishise, S.; Yagi, M.; Mizumoto, N.; Kon, T.; Onozato, Y.; Sakai, T.; Umehara, M.; Ito, M.; et al. Low Serum Pancreatic Amylase Levels as a Novel Latent Risk Factor for Colorectal Adenoma in Non-Alcohol Drinkers. J. Gastroenterol. Hepatol. 2022, 37, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Byman, E.; Schultz, N.; Fex, M.; Wennström, M.; Netherlands Brain Bank. Brain Alpha-Amylase: A Novel Energy Regulator Important in Alzheimer Disease? Brain Pathol. 2018, 28, 920–932. [Google Scholar] [CrossRef] [PubMed]
- Byman, E.; Martinsson, I.; Haukedal, H.; Netherlands Brain Bank Gouras, G.; Freude, K.K.; Wennström, M. Neuronal A-Amylase is Important for Neuronal Activity and Glycogenolysis and Reduces in Presence of Amyloid Beta Pathology. Aging Cell 2021, 20, e13433. [Google Scholar] [CrossRef] [PubMed]
- Pierzynowska, K.; Thomasson, S.; Oredsson, S. Alpha-Amylase Inhibits Cell Proliferation and Glucose Uptake in Human Neuroblastoma Cell Lines. Biomed. Res. Int. 2022, 2022, 4271358. [Google Scholar] [CrossRef]
- April-Sanders, A.K.; Rodriguez, C.J. Metabolically Healthy Obesity Redefined. JAMA Netw. Open 2021, 4, e218860. [Google Scholar] [CrossRef]
- Mendrick, D.L.; Diehl, A.M.; Topor, L.S.; Dietert, R.R.; Will, Y.; La Merrill, M.A.; Bouret, S.; Varma, V.; Hastings, K.L.; Schug, T.T.; et al. Metabolic Syndrome and Associated Diseases: From the Bench to the Clinic. Toxicol. Sci. 2018, 162, 36–42. [Google Scholar] [CrossRef]
- Rubino, F.; Gagner, M. Potential of Surgery for Curing Type 2 Diabetes Mellitus. Ann. Surg. 2002, 236, 554–559. [Google Scholar] [CrossRef]
- Rubino, F. Is Type 2 Diabetes an Operable Intestinal Disease? Diabetes Care 2008, 31, S290–S296. [Google Scholar] [CrossRef]
- Rubino, F.; Amiel, S.A. Is the Gut the “Sweet Spot” for the Treatment of Diabetes? Diabetes 2014, 63, 2225–2228. [Google Scholar] [CrossRef]
- Lindqvist, A.; Spégel, P.; Ekelund, M.; Garcia Vaz, E.; Pierzynowski, S.; Gomez, M.F.; Mulder, H.; Hedenbro, J.; Groop, L.; Wierup, N. Gastric Bypass Improves Β-Cell Function and Increases Β-Cell Mass in A Porcine Model. Diabetes 2014, 63, 1665–1671. [Google Scholar] [CrossRef] [PubMed]
- Salinari, S.; le Roux, C.W.; Bertuzzi, A.; Rubino, F.; Mingrone, G. Duodenal-Jejunal Bypass and Jejunectomy Improve Insulin Sensitivity in Goto-Kakizaki Diabetic Rats without Changes in Incretins or Insulin Secretion. Diabetes 2014, 63, 1069–1078. [Google Scholar] [CrossRef] [PubMed]
- Salinari, S.; Mingrone, G.; Bertuzzi, A.; Previti, E.; Capristo, E.; Rubino, F. Downregulation of Insulin Sensitivity After Oral Glucose Administration: Evidence for the Anti-Incretin Effect. Diabetes 2017, 66, 2756–2763. [Google Scholar] [CrossRef] [PubMed]
- Rehfeld, J.F. The Origin and Understanding of the Incretin Concept. Front. Endocrinol. 2018, 9, 387. [Google Scholar] [CrossRef]
- Drucker, D.J.; Holst, J.J. The Expanding Incretin Universe: From Basic Biology to Clinical Translation. Diabetologia 2023, 66, 1765–1779. [Google Scholar] [CrossRef]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pierzynowska, K.; Wychowański, P.; Zaworski, K.; Woliński, J.; Donaldson, J.; Pierzynowski, S. Anti-Incretin Gut Features Induced by Feed Supplementation with Alpha-Amylase: Studies on EPI Pigs. Int. J. Mol. Sci. 2023, 24, 16177. https://doi.org/10.3390/ijms242216177
Pierzynowska K, Wychowański P, Zaworski K, Woliński J, Donaldson J, Pierzynowski S. Anti-Incretin Gut Features Induced by Feed Supplementation with Alpha-Amylase: Studies on EPI Pigs. International Journal of Molecular Sciences. 2023; 24(22):16177. https://doi.org/10.3390/ijms242216177
Chicago/Turabian StylePierzynowska, Kateryna, Piotr Wychowański, Kamil Zaworski, Jarosław Woliński, Janine Donaldson, and Stefan Pierzynowski. 2023. "Anti-Incretin Gut Features Induced by Feed Supplementation with Alpha-Amylase: Studies on EPI Pigs" International Journal of Molecular Sciences 24, no. 22: 16177. https://doi.org/10.3390/ijms242216177




