DNA Methylation of α-Synuclein Intron 1 Is Significantly Decreased in the Frontal Cortex of Parkinson’s Individuals with GBA1 Mutations
Abstract
1. Introduction
2. Results
2.1. Significant DNA Hypomethylation of Five CpG Sites of SNCA Intron 1 Located Further from the Transcription Start Site (TSS) in the Frontal Cortex of PD-GBA1
2.2. A Trend towards a Decrease in DNA Methylation of CpG Sites in SNCA Intron 1 Further from the TSS in the Putamen of Idiopathic PD and PD-GBA1
2.3. A Trend towards a Decrease in the DNA Methylation of CpG Sites in SNCA Intron 1 Further from the TSS in the Substantia Nigra of Idiopathic PD
2.4. No Significant DNA Methylation Differences within the SNCA Promoter in Either the Frontal Cortex or the Putamen
2.5. Significantly Lower DNA Methylation of CpG Site in the SNCA Promoter in the Substantia Nigra in Idiopathic PD but Not in PD-GBA1
3. Discussion
4. Materials and Methods
4.1. Subjects and Samples
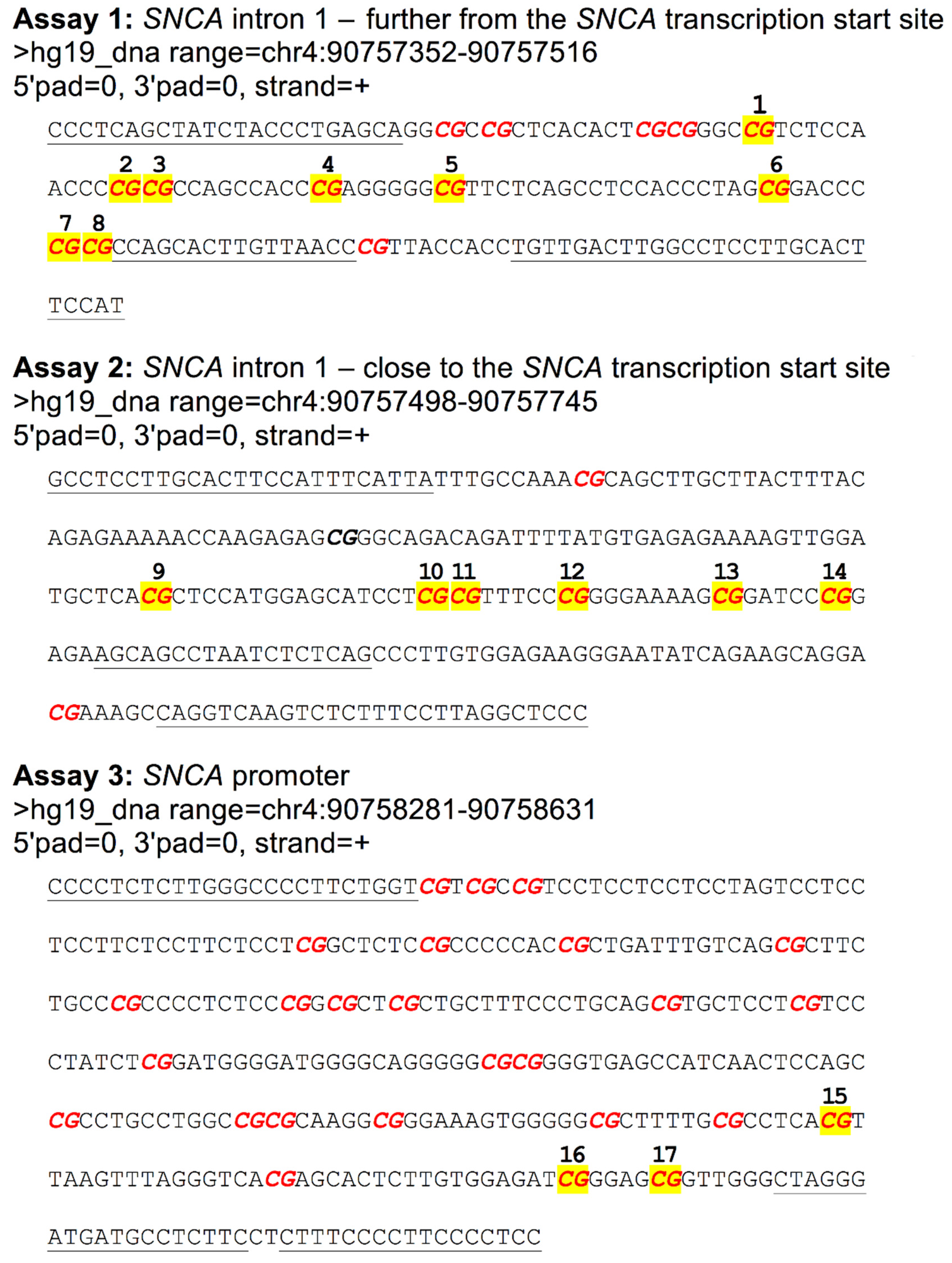
4.2. SNCA Bisulfite Pyrosequencing
4.3. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rana, H.Q.; Balwani, M.; Bier, L.; Alcalay, R.N. Age-specific Parkinson disease risk in GBA mutation carriers: Information for genetic counseling. Genet. Med. 2013, 15, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Alcalay, R.N.; Dinur, T.; Quinn, T.; Sakanaka, K.; Levy, O.; Waters, C.; Fahn, S.; Dorovski, T.; Chung, W.K.; Pauciulo, M.; et al. Comparison of Parkinson risk in Ashkenazi Jewish patients with Gaucher disease and GBA heterozygotes. JAMA Neurol. 2014, 71, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Migdalska-Richards, A.; Schapira, A.H.V. The relationship between glucocerebrosidase mutations and Parkinson disease. J. Neurochem. 2016, 139, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Rogers, G.; Davies, D.; Pink, J.; Cooper, P. Parkinson’s disease: Summary of updated NICE guidance. BMJ 2017, 358, j1951. [Google Scholar] [CrossRef] [PubMed]
- Frank, C.; Pari, G.; Rossiter, J.P. Approach to diagnosis of Parkinson disease. Can. Fam. Physician 2006, 52, 862–868. [Google Scholar]
- Beutler, E. Gaucher disease: New molecular approaches to diagnosis and treatment. Science 1992, 256, 794–799. [Google Scholar] [CrossRef]
- Sidransky, E.; Nalls, M.A.; Aasly, J.; Aharon-Peretz, J.; Annesi, G.; Barbosa, E.R.; Bar-Shira, A.; Berg, D.; Bras, J.; Brice, A.; et al. Multicenter Analysis of Glucocerebrosidase Mutations in Parkinson’s Disease. N. Engl. J. Med. 2009, 361, 1651–1661. [Google Scholar] [CrossRef]
- Neumann, J.; Bras, J.; Deas, E.; O’Sullivan, S.S.; Parkkinen, L.; Lachmann, R.H.; Li, A.; Holton, J.; Guerreiro, R.; Paudel, R.; et al. Glucocerebrosidase mutations in clinical and pathologically proven Parkinson’s disease. Brain 2009, 132, 1783–1794. [Google Scholar] [CrossRef]
- Brockmann, K.; Srulijes, K.; Hauser, A.K.; Schulte, C.; Csoti, I.; Gasser, T.; Berg, D. GBA-associated PD presents with nonmotor characteristics. Neurology 2011, 77, 276–280. [Google Scholar] [CrossRef]
- Westbroek, W.; Gustafson, A.M.; Sidransky, E. Exploring the link between glucocerebrosidase mutations and parkinsonism. Trends Mol. Med. 2011, 17, 485–493. [Google Scholar] [CrossRef]
- Manning-Boğ, A.B.; Schüle, B.; Langston, J.W. Alpha-synuclein-glucocerebrosidase interactions in pharmacological Gaucher models: A biological link between Gaucher disease and parkinsonism. Neurotoxicology 2009, 30, 1127–1132. [Google Scholar] [CrossRef] [PubMed]
- Cullen, V.; Sardi, S.P.; Ng, J.; Xu, Y.H.; Sun, Y.; Tomlinson, J.J.; Kolodziej, P.; Kahn, I.; Saftig, P.; Woulfe, J.; et al. Acid b-glucosidase mutants linked to Gaucher disease, Parkinson disease, and Lewy body dementia alter a-synuclein processing. Ann. Neurol. 2011, 69, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Mazzulli, J.R.; Xu, Y.H.; Sun, Y.; Knight, A.L.; McLean, P.J.; Caldwell, G.; Sidransky, E.; Grabowski, G.A.; Krainc, D. Gaucher disease glucocerebrosidase and a-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell 2011, 146, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Cleeter, M.W.; Chau, K.; Gluck, C.; Mehta, A.; Hughes, D.A.; Duchen, M.; Wood, N.; Hardy, J.; Cooper, J.M.; Schapira, A.H. Glucocerebrosidase inhibition causes mitochondrial dysfunction and free radical damage. Neurochem. Int. 2013, 62, 1–7. [Google Scholar] [CrossRef]
- Osellame, L.D.; Rahim, A.A.; Hargreaves, I.P.; Gegg, M.E.; Richard-Londt, A.; Brandner, S.; Waddington, S.N.; Schapira, A.H.; Duchen, M.R. Mitochondria and Quality Control Defects in a Mouse Model of Gaucher Disease—Links to Parkinson’s Disease. Cell Metab. 2013, 17, 941–953. [Google Scholar] [CrossRef]
- Sardi, S.P.; Clarke, J.; Viel, C.; Chan, M.; Tamsett, T.J.; Treleaven, C.M.; Bu, J.; Sweet, L.; Passini, M.A.; Dodge, J.C.; et al. Augmenting CNS glucocerebrosidase activity as a therapeutic strategy for parkinsonism and other Gaucher-related synucleinopathies. Proc. Natl. Acad. Sci. USA 2013, 110, 3537–3542. [Google Scholar] [CrossRef]
- Magalhaes, J.; Gegg, M.E.; Migdalska-Richards, A.; Doherty, M.K.; Whitfield, P.D.; Schapira, A.H.V. Autophagic lysosome reformation dysfunction in glucocerebrosidase deficient cells: Relevance to Parkinson disease. Hum. Mol. Genet. 2016, 25, 3432–3445. [Google Scholar] [CrossRef]
- Migdalska-Richards, A.M.; Wegrzynowicz, M.; Rusconi, R.; Deangelli, G.; Di Monte, D.A.; Spillantini, M.G.; Schapira, A.H.V. The L444P Gba1 mutation enhances α-synuclein induced loss of nigral dopaminergic neurons in mice. Brain 2017, 140, 2706–2721. [Google Scholar] [CrossRef]
- Magalhaes, J.; Gegg, M.E.; Migdalska-Richards, A.; Schapira, A.H. Effects of ambroxol on the autophagy-lysosome pathway and mitochondria in primary cortical neurons. Sci. Rep. 2018, 8, 1385. [Google Scholar] [CrossRef]
- Migdalska-Richards, A.; Węgrzynowicz, M.; Harrison, I.F.; Verona, G.; Bellotti, V.; Spillantini, M.G.; Schapira, A.H.V. L444P Gba1 mutation increases formation and spread of α-synuclein deposits in mice injected with mouse α-synuclein pre-formed fibrils. PLoS ONE 2020, 15, e0238075. [Google Scholar] [CrossRef]
- Gegg, M.E.; Burke, D.; Heales, S.J.R.; Cooper, J.M.; Hardy, J.; Wood, N.W.; Schapira, A.H.V. Glucocerebrosidase deficiency in substantia nigra of parkinson disease brains. Ann. Neurol. 2012, 72, 455–463. [Google Scholar] [CrossRef]
- Migdalska-Richards, A.; Daly, L.; Bezard, E.; Schapira, A.H. Ambroxol effect in glucocerebrosidase and α-synuclein transgenic mice. Ann. Neurol. 2016, 80, 766–775. [Google Scholar] [CrossRef] [PubMed]
- Stefanis, L. α-Synuclein in Parkinson’s disease. Cold Spring Harb. Perspect. Med. 2012, 2, a009399. [Google Scholar] [CrossRef] [PubMed]
- Stojkovska, I.; Krainc, D.; Mazzulli, J.R. Molecular mechanisms of α-synuclein and GBA1 in Parkinson’s disease. Cell Tissue Res. 2018, 373, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Goldman, S.M.; Marek, K.; Ottman, R.; Meng, C.; Comyns, K.; Chan, P.; Ma, J.; Marras, C.; Langston, J.W.; Ross, G.W.; et al. Concordance for Parkinson’s disease in twins: A 20-year update. Ann. Neurol. 2019, 85, 600–605. [Google Scholar] [CrossRef]
- Migdalska-Richards, A.; Mill, J. Epigenetic studies of schizophrenia: Current status and future directions. Curr. Opin. Behav. Sci. 2019, 25, 102–110. [Google Scholar] [CrossRef]
- Lunnon, K.; Smith, R.; Hannon, E.; De Jager, P.L.; Srivastava, G.; Volta, M.; Troakes, C.; Al-Sarraj, S.; Burrage, J.; Macdonald, R.; et al. Methylomic profiling implicates cortical deregulation of ANK1 in Alzheimer’s disease. Nat. Neurosci. 2014, 17, 1164–1170. [Google Scholar] [CrossRef]
- Francelle, L.; Lotz, C.; Outeiro, T.; Brouillet, E.; Merienne, K. Contribution of Neuroepigenetics to Huntington’s Disease. Front. Hum. Neurosci. 2017, 11, 17. [Google Scholar] [CrossRef]
- Liu, X.; Jiao, B.; Shen, L. The Epigenetics of Alzheimer’s Disease: Factors and Therapeutic Implications. Front. Genet. 2018, 9, 579. [Google Scholar] [CrossRef]
- Smith, A.; Smith, R.G.; Pishva, E.; Hannon, E.; Roubroeks, J.A.Y.; Burrage, J.; Troakes, C.; Al-Sarraj, S.; Sloan, C.; Mill, J.; et al. Parallel profiling of DNA methylation and hydroxymethylation highlights neuropathology-associated epigenetic variation in Alzheimer’s disease. Clin. Epigenet. 2019, 11, 52. [Google Scholar] [CrossRef]
- Laird, P.W. Principles and challenges of genome-wide DNA methylation analysis. Nat. Rev. Genet. 2010, 11, 191–203. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Chang, H.; Li, E.; Fan, G. Dynamic expression of de novo DNA methyltransferases Dnmt3a and Dnmt3b in the central nervous system. J. Neurosci. Res. 2005, 79, 734–746. [Google Scholar] [CrossRef]
- Jakovcevski, M.; Akbarian, S. Epigenetic mechanisms in neurological disease. Nat. Med. 2012, 18, 1194–1204. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Liu, X.; Deng, Y.; Qing, H. DNA methylation, a hand behind neurodegenerative diseases. Front. Aging Neurosci. 2013, 5, 85. [Google Scholar] [CrossRef] [PubMed]
- Landgrave-Gómez, J.; Mercado-Gómez, O.; Guevara-Guzmán, R. Epigenetic mechanisms in neurological and neurodegenerative diseases. Front. Cell. Neurosci. 2015, 9, 58. [Google Scholar] [PubMed]
- Jowaed, A.; Schmitt, I.; Kaut, O.; Wüllner, U. Methylation regulates alpha-synuclein expression and is decreased in Parkinson’s disease patients’ brains. J. Neurosci. 2010, 30, 6355–6359. [Google Scholar] [CrossRef]
- Matsumoto, L.; Takuma, H.; Tamaoka, A.; Kurisaki, H.; Date, H.; Tsuji, S.; Iwata, A. CpG demethylation enhances alpha-synuclein expression and affects the pathogenesis of Parkinson’s disease. PLoS ONE 2010, 5, e15522. [Google Scholar] [CrossRef]
- De Boni, L.; Tierling, S.; Roeber, S.; Walter, J.; Giese, A.; Kretzschmar, H.A. Next-generation sequencing reveals regional differences of the α-synuclein methylation state independent of Lewy body disease. Neuromol. Med. 2011, 13, 310–320. [Google Scholar] [CrossRef]
- Desplats, P.; Spencer, B.; Coffee, E.; Patel, P.; Michael, S.; Patrick, C.; Adame, A.; Rockenstein, E.; Masliah, E. Alpha-synuclein sequesters Dnmt1 from the nucleus: A novel mechanism for epigenetic alterations in Lewy body diseases. J. Biol. Chem. 2011, 286, 9031–9037. [Google Scholar] [CrossRef]
- Pihlstrøm, L.; Berge, V.; Rengmark, A.; Toft, M. Parkinson’s disease correlates with promoter methylation in the α-synuclein gene. Mov. Disord. 2015, 30, 577–580. [Google Scholar] [CrossRef]
- Guhathakurta, S.; Evangelista, B.A.; Ghosh, S.; Basu, S.; Kim, Y.-S. Hypomethylation of intron1 of α-synuclein gene does not correlate with Parkinson’s disease. Mol. Brain 2017, 10, 6. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Sánchez, L.; Águeda-Gómez, B.; Aparicio, S.; Pérez-Tur, J. Epigenetic Study in Parkinson’s Disease: A Pilot Analysis of DNA Methylation in Candidate Genes in Brain. Cells 2018, 7, 150. [Google Scholar] [CrossRef] [PubMed]
- Surmeier, D.J.; Obeso, J.A.; Halliday, G.M. Selective neuronal vulnerability in Parkinson disease. Nat. Rev. Neurosci. 2017, 18, 101–113. [Google Scholar] [CrossRef]
- Fearnley, J.M.; Lees, A.J. Ageing and Parkinson’s disease: Substantia nigra regional selectivity. Brain 1991, 114 Pt 5, 2283–2301. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.R.; Smith, R.G.; Condliffe, D.; Hannon, E.; Schalkwyk, L.; Mill, J.; Lunnon, K. Increased DNA methylation near TREM2 is consistently seen in the superior temporal gyrus in Alzheimer’s disease brain. Neurobiol. Aging 2016, 47, 35–40. [Google Scholar] [CrossRef] [PubMed]


| Sex | Age | PMD | Cause of Death | FC | PUT | SN | GBA1 Mutation |
|---|---|---|---|---|---|---|---|
| Control cases | |||||||
| F | 81 | 44.55 | Carcinoma (breast) | X | - | ||
| M | 95 | 89.20 | Heart failure | X | X | - | |
| M | 87 | 39.25 | Bronchopneumonia | X | X | X | - |
| M | 63 | 42.0 | Congestive heart disease | X | X | - | |
| F | 64 | 79.0 | Carcinoma (bowel) | X | - | ||
| F | 53 | 29.5 | Intra-cerebral hemorrhage | X | - | ||
| F | 82 | 77.25 | Unknown | X | X | X | - |
| M | 43 | 15.00 | Heart failure | X | - | ||
| M | 71 | 38.50 | Mesothelioma | X | - | ||
| M | 38 | 80.35 | Carcinoma (gastric) | X | - | ||
| Idiopathic PD cases | |||||||
| F | 55 | 31.20 | Idiopathic PD | X | X | X | - |
| M | 67 | 35.10 | Myocardial infarct | X | - | ||
| M | 66 | 43.10 | Pneumonia | X | X | - | |
| F | 61 | 25.30 | End stage idiopathic PD | X | - | ||
| M | 91 | 36.20 | Idiopathic PD, dementia | X | X | - | |
| M | 85 | 28.30 | PD, immobility | X | X | - | |
| M | 65 | 31.20 | Aspiration pneumonia | X | X | - | |
| M | 68 | 38.50 | Gradual deterioration | X | X | X | - |
| M | 75 | 28.00 | Chest infection | X | X | X | - |
| M | 63 | 69.00 | Heart failure | X | X | X | - |
| F | 62 | 46.20 | Gradual deterioration | X | X | - | |
| M | 59 | 94.00 | Chest infection | X | - | ||
| M | 66 | 30.00 | Atypical PD, gradual deterioration | X | X | X | - |
| M | 81 | 49.00 | Aspiration pneumonia | X | X | X | - |
| M | 65 | 55 | Unknown | X | X | - | |
| PD-GBA1 cases | |||||||
| M | 62 | 34.00 | Progressive deterioration | X | X | G193E | |
| M | 55 | 8.00 | Progressive degeneration | X | R131C | ||
| F | 67 | 45.00 | Myocardial infarct | X | L444P | ||
| M | 57 | 28.00 | Bronchopneumonia | X | X | X | RecA456P |
| F | 64 | Unknown | Unknown | X | |||
| M | 91 | 60.45 | Ischemic bowel, sepsis | X | N370S | ||
| M | 85 | 48.15 | Chest infection | N370S | |||
| M | 68 | 86.15 | PD, dementia | X | X | R463C | |
| M | 62 | 46.00 | Cardiac arrest | X | X | D409H | |
| F | 64 | 92.00 | Respiratory failure | X | X | X | RecNciI |
| M | 59 | 42.45 | Multiple system atrophy | X | X | X | L444P |
| F | 57 | 85.40 | Bronchopneumonia | X | X | L444P | |
| M | 82 | 54.40 | Congestive heart failure | X | X | N370S | |
| Assay | PCR Primers | Length | Pyrosequencing Primers |
|---|---|---|---|
| 1 | F: 5′-TGTTGACTTGGCCTCCTTGCACTTCCAT-3′ R: 5′-CCCTCAGCTATCTACCCTGAGCA-3′ | 164 bp | 5′-CCAGCACTTGTTAACCC-3′ |
| 2 | F: 5′-CAGGTCAAGTCTCTTTCCTTAGGCTCCC-3′ R: 5′-GCCTCCTTGCACTTCCATTTCATTA-3′ | 247 bp | 5′-AGCAGCCTAATCTCTC-3′ |
| 3 | F: 5′-CTTTCCCCTTCCCCTCCC-3′ R: 5′-CCCCTCTCTTGGGCCCCTTCTGGT-3′ | 350 bp | 5′-CTAGGGATGATGCCTCTTC-3′ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, A.R.; Richards, D.M.; Lunnon, K.; Schapira, A.H.V.; Migdalska-Richards, A. DNA Methylation of α-Synuclein Intron 1 Is Significantly Decreased in the Frontal Cortex of Parkinson’s Individuals with GBA1 Mutations. Int. J. Mol. Sci. 2023, 24, 2687. https://doi.org/10.3390/ijms24032687
Smith AR, Richards DM, Lunnon K, Schapira AHV, Migdalska-Richards A. DNA Methylation of α-Synuclein Intron 1 Is Significantly Decreased in the Frontal Cortex of Parkinson’s Individuals with GBA1 Mutations. International Journal of Molecular Sciences. 2023; 24(3):2687. https://doi.org/10.3390/ijms24032687
Chicago/Turabian StyleSmith, Adam R., David M. Richards, Katie Lunnon, Anthony H. V. Schapira, and Anna Migdalska-Richards. 2023. "DNA Methylation of α-Synuclein Intron 1 Is Significantly Decreased in the Frontal Cortex of Parkinson’s Individuals with GBA1 Mutations" International Journal of Molecular Sciences 24, no. 3: 2687. https://doi.org/10.3390/ijms24032687
APA StyleSmith, A. R., Richards, D. M., Lunnon, K., Schapira, A. H. V., & Migdalska-Richards, A. (2023). DNA Methylation of α-Synuclein Intron 1 Is Significantly Decreased in the Frontal Cortex of Parkinson’s Individuals with GBA1 Mutations. International Journal of Molecular Sciences, 24(3), 2687. https://doi.org/10.3390/ijms24032687






