Molecular Mechanism Operating in Animal Models of Neurogenic Detrusor Overactivity: A Systematic Review Focusing on Bladder Dysfunction of Neurogenic Origin
Abstract
1. Introduction
2. Results
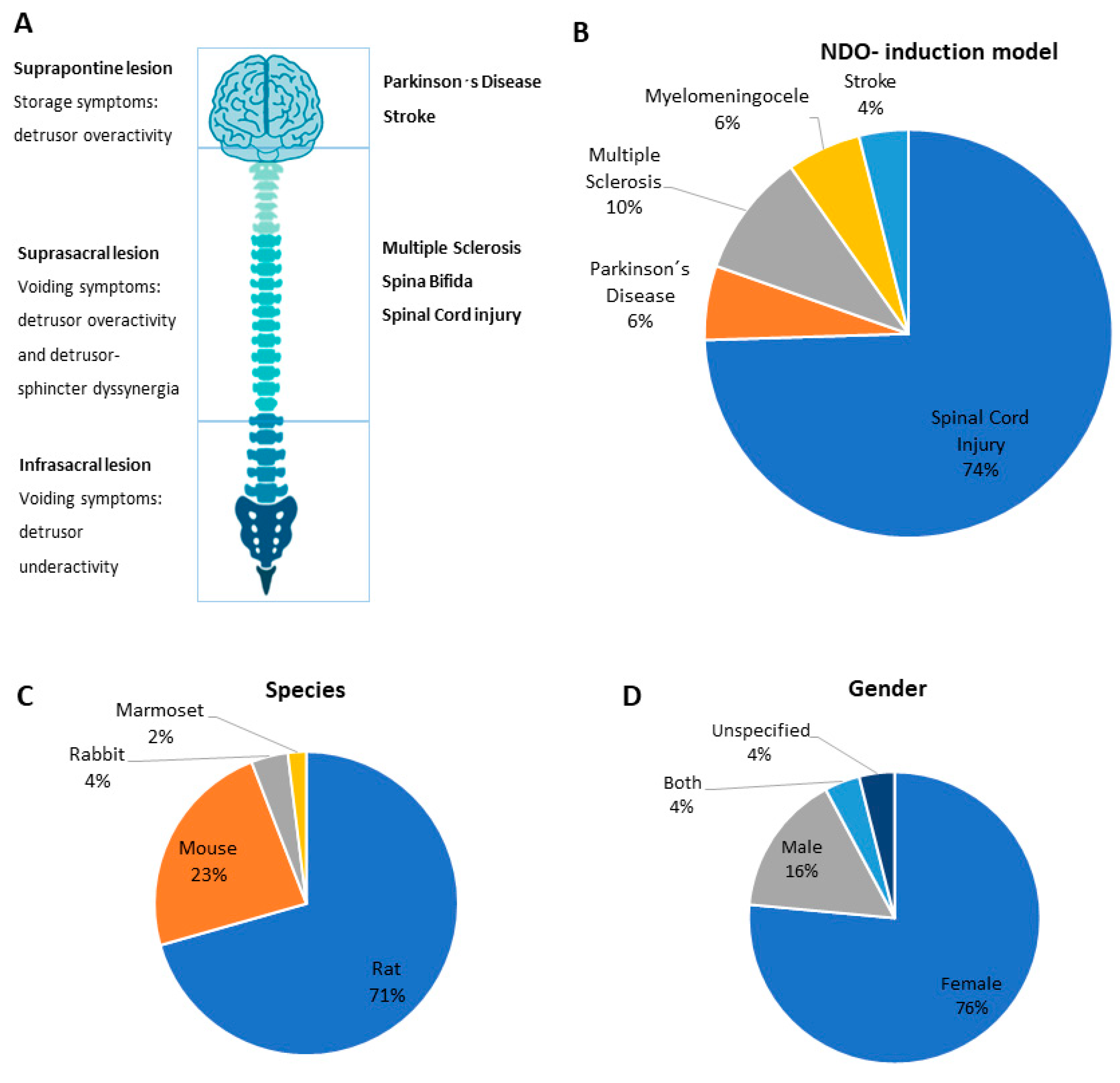
2.1. Induction Model and Assessment of Bladder Function
2.2. Animal Species and Sex
2.3. Changes in Bladder Tissue
2.4. Changes in Neuronal Tissue
3. Discussion
3.1. NDO-Driven Pathology and Induction Model
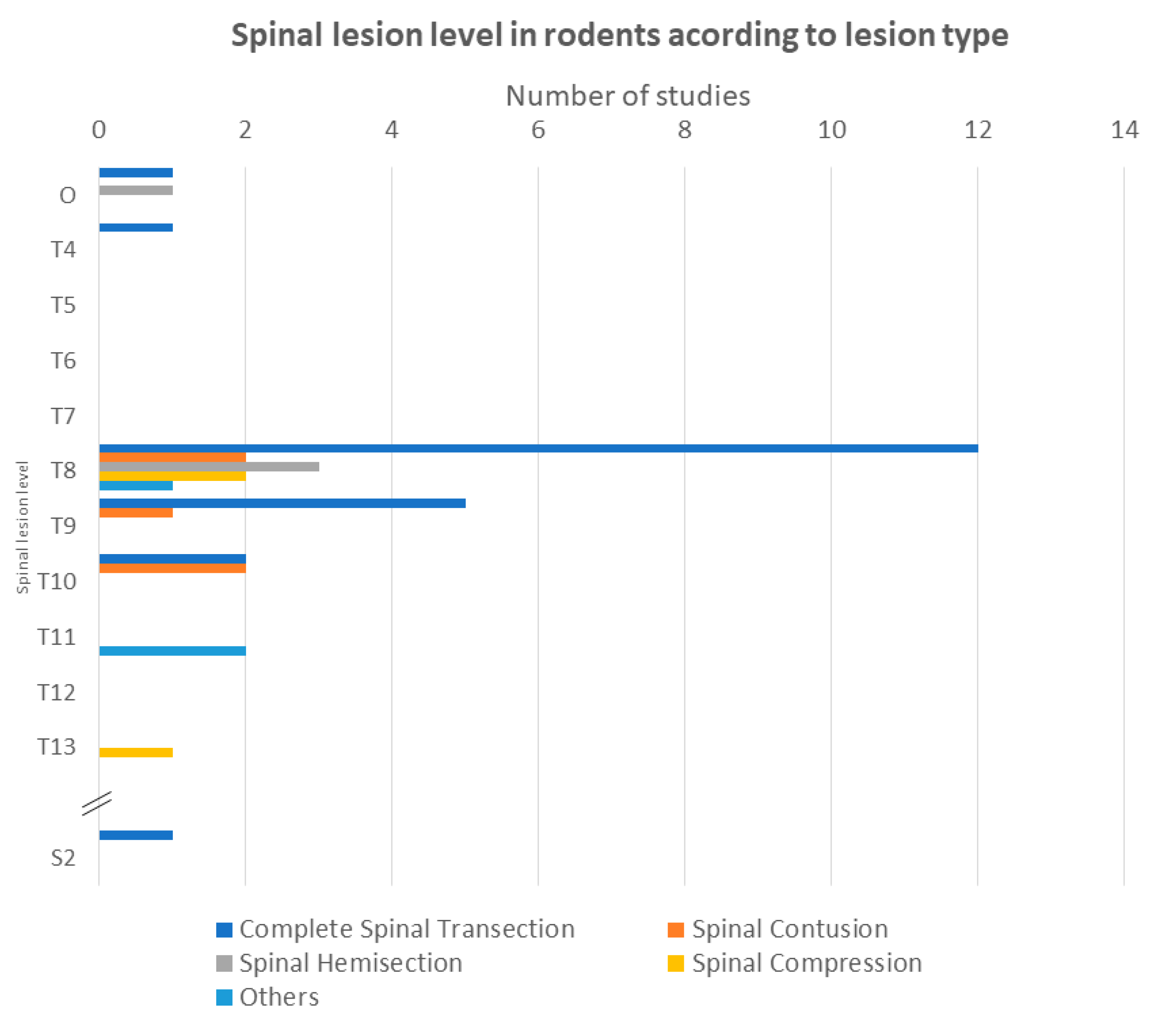
3.1.1. Spinal Cord Injury (SCI)
3.1.2. Multiple Sclerosis
3.1.3. Parkinson’s Disease
3.1.4. Meningomyelocele
3.1.5. Cerebral Vascular Accidents
3.2. Animal Species
3.3. Animal Sex
3.4. Urodynamic Recording
3.5. Changes in Bladder and Neural Tissue Morphology
3.6. Molecular Factors
3.6.1. Neurotrophic Factors
3.6.2. Inflammatory Mediators
3.6.3. Apoptosis-Related Factors
3.6.4. Muscarinic Receptors
3.6.5. Adrenergic Receptors
3.6.6. Purinergic Receptors and Transient Receptor Potential Channels
3.6.7. Neuronal Markers
3.6.8. Ischemia- and Fibrosis-Related Molecules
3.6.9. Myelin-Associated Proteins
4. Conclusions
5. Materials and Methods
5.1. Literature Search
5.2. Selection
5.3. Data Extraction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fowler, C.J.; Griffiths, D.; de Groat, W.C. The neural control of micturition. Nat. Rev. Neurosci. 2008, 9, 453–466. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, N. Neural control of the lower urinary tract. Int. J. Urol. 1997, 4, 111–125. [Google Scholar] [CrossRef] [PubMed]
- Andersson, K.-E.; Gratzke, C.J.T. Pharmacology of the lower urinary tract. In Textbook of the Neurogenic Bladder, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2008; pp. 81–100. [Google Scholar]
- Panicker, J.N. Neurogenic Bladder: Epidemiology, Diagnosis, and Management. Semin. Neurol. 2020, 40, 569–579. [Google Scholar] [CrossRef]
- Ginsberg, D. The epidemiology and pathophysiology of neurogenic bladder. Am. J. Manag. Care 2013, 19 (Suppl. 10), s191–s196. [Google Scholar] [PubMed]
- Miyazato, M.; Kadekawa, K.; Kitta, T.; Wada, N.; Shimizu, N.; de Groat, W.C.; Birder, L.A.; Kanai, A.J.; Saito, S.; Yoshimura, N. New Frontiers of Basic Science Research in Neurogenic Lower Urinary Tract Dysfunction. Urol. Clin. N. Am. 2017, 44, 491–505. [Google Scholar] [CrossRef]
- Gajewski, J.B.; Schurch, B.; Hamid, R.; Averbeck, M.; Sakakibara, R.; Agro, E.F.; Dickinson, T.; Payne, C.K.; Drake, M.J.; Haylen, B.T. An International Continence Society (ICS) report on the terminology for adult neurogenic lower urinary tract dysfunction (ANLUTD). Neurourol. Urodyn. 2018, 37, 1152–1161. [Google Scholar] [CrossRef]
- Chiang, C.H.; Chen, S.F.; Kuo, H.C. Video-urodynamic characteristics of lower urinary tract dysfunctions in patients with chronic brain disorders. Neurourol. Urodyn. 2022, 41, 255–263. [Google Scholar] [CrossRef]
- Welk, B.; Schneider, M.P.; Thavaseelan, J.; Traini, L.R.; Curt, A.; Kessler, T.M. Early urological care of patients with spinal cord injury. World J. Urol. 2018, 36, 1537–1544. [Google Scholar] [CrossRef]
- De Groat, W.C.J.U. A neurologic basis for the overactive bladder. Urology 1997, 50, 36–52. [Google Scholar] [CrossRef]
- De Groat, W.C.; Yoshimura, N. Mechanisms underlying the recovery of lower urinary tract function following spinal cord injury. Prog. Brain Res. 2006, 152, 59–84. [Google Scholar]
- De Groat, W.C.; Yoshimura, N. Afferent nerve regulation of bladder function in health and disease. In Sensory Nerves; Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2009; Volume 194, pp. 91–138. [Google Scholar]
- Birder, L.A.; Kullmann, F.A. Role of Neurogenic Inflammation in Local Communication in the Visceral Mucosa. Semin. Immunopathol. 2018, 40, 261–279. [Google Scholar] [CrossRef]
- Wu, S.-Y.; Jiang, Y.-H.; Jhang, J.-F.; Hsu, Y.-H.; Ho, H.-C.; Kuo, H.-C. Inflammation and Barrier Function Deficits in the Bladder Urothelium of Patients with Chronic Spinal Cord Injury and Recurrent Urinary Tract Infections. Biomedicines 2022, 10, 220. [Google Scholar] [CrossRef]
- Jiang, Y.-H.; Chen, S.-F.; Kuo, H.-C. Frontiers in the clinical applications of botulinum toxin A as treatment for neurogenic lower urinary tract dysfunction. Int. Neurourol. J. 2020, 24, 301. [Google Scholar] [CrossRef]
- Panicker, J.N.; Fowler, C.J.; Kessler, T.M. Lower urinary tract dysfunction in the neurological patient: Clinical assessment and management. Lancet Neurol. 2015, 14, 720–732. [Google Scholar] [CrossRef]
- Dorsher, P.T.; McIntosh, P.M. Neurogenic bladder. Adv. Urol. 2012, 2012, 816274. [Google Scholar] [CrossRef]
- Wada, N.; Karnup, S.; Kadekawa, K.; Shimizu, N.; Kwon, J.; Shimizu, T.; Gotoh, D.; Kakizaki, H.; de Groat, W.C.; Yoshimura, N. Current Knowledge and Novel Frontiers in Lower Urinary Tract Dysfunction after Spinal Cord Injury: Basic Research Perspectives. Urol. Sci. 2022, 33, 101–113. [Google Scholar] [CrossRef]
- Ahmed, H.U.; Shergill, I.S.; Arya, M.; Shah, P.J. Management of detrusor-external sphincter dyssynergia. Nat. Clin. Pract. Urol. 2006, 3, 368–380. [Google Scholar] [CrossRef]
- Park, S.E.; Elliott, S.; Noonan, V.K.; Thorogood, N.P.; Fallah, N.; Aludino, A.; Dvorak, M.F. Impact of bladder, bowel and sexual dysfunction on health status of people with thoracolumbar spinal cord injuries living in the community. J. Spinal Cord Med. 2017, 40, 548–559. [Google Scholar] [CrossRef]
- Dave, S.; Cho, J.J. Neurogenic Shock; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Ditunno, J.F.; Little, J.W.; Tessler, A.; Burns, A.S. Spinal shock revisited: A four-phase model. Spinal Cord 2004, 42, 383–395. [Google Scholar] [CrossRef] [PubMed]
- Hayes, K.C.; Davies, A.L.; Ashki, N.; Kramer, J.K.; Close, T.E. Re: Ditunno JF, Little JW, Tessler A, Burns AS. Spinal shock revisited: A four-phase model. Spinal Cord 2004; 42: 383–395. Spinal Cord 2007, 45, 395–396. [Google Scholar]
- Bywater, M.; Tornic, J.; Mehnert, U.; Kessler, T.M. Detrusor Acontractility after Acute Spinal Cord Injury-Myth or Reality? J. Urol. 2018, 199, 1565–1570. [Google Scholar] [CrossRef]
- De Groat, W.C.; Kawatani, M.; Hisamitsu, T.; Cheng, C.L.; Ma, C.P.; Thor, K.; Steers, W.; Roppolo, J.R. Mechanisms underlying the recovery of urinary bladder function following spinal cord injury. J. Auton. Nerv. Syst. 1990, 30, S71–S77. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.; Coelho, A.; Franquinho, F.; Sousa, M.M.; Cruz, F.; Cruz, C.D. Effects of early intravesical administration of resiniferatoxin to spinal cord-injured rats in neurogenic detrusor overactivity. Neurourol. Urodyn. 2019, 38, 1540–1550. [Google Scholar] [CrossRef]
- Frias, B.; Santos, J.; Morgado, M.; Sousa, M.M.; Gray, S.M.; McCloskey, K.D.; Allen, S.; Cruz, F.; Cruz, C.D. The role of brain-derived neurotrophic factor (BDNF) in the development of neurogenic detrusor overactivity (NDO). J. Neurosci. 2015, 35, 2146–2160. [Google Scholar] [CrossRef]
- Chambel, S.S.; Ferreira, A.; Oliveira, R.; Miranda, R.; Vale, L.; Reguenga, C.; Schwab, M.E.; Cruz, C.D. Development of Neurogenic Detrusor Overactivity after Thoracic Spinal Cord Injury Is Accompanied by Time-Dependent Changes in Lumbosacral Expression of Axonal Growth Regulators. Int. J. Mol. Sci. 2022, 23, 8667. [Google Scholar] [CrossRef]
- Zhang, T.; Yu, J.; Huang, Z.; Wang, G.; Zhang, R. Electroacupuncture improves neurogenic bladder dysfunction through activation of NGF/TrkA signaling in a rat model. J. Cell. Biochem. 2019, 120, 9900–9905. [Google Scholar] [CrossRef]
- Kullmann, F.A.; Beckel, J.M.; McDonnell, B.; Gauthier, C.; Lynn, A.M.; Wolf-Johnston, A.; Kanai, A.; Zabbarova, I.V.; Ikeda, Y.; de Groat, W.C.; et al. Involvement of TRPM4 in detrusor overactivity following spinal cord transection in mice. Naunyn Schmiedebergs Arch. Pharmacol. 2018, 391, 1191–1202. [Google Scholar] [CrossRef]
- Gotoh, D.; Shimizu, N.; Wada, N.; Kadekawa, K.; Saito, T.; Mizoguchi, S.; Morizawa, Y.; Hori, S.; Miyake, M.; Torimoto, K.; et al. Effects of a new β3-adrenoceptor agonist, vibegron, on neurogenic bladder dysfunction and remodeling in mice with spinal cord injury. Neurourol. Urodyn. 2020, 39, 2120–2127. [Google Scholar] [CrossRef]
- Chung, Y.G.; Seth, A.; Doyle, C.; Franck, D.; Kim, D.; Cristofaro, V.; Benowitz, L.I.; Tu, D.D.; Estrada, C.R.; Mauney, J.R.; et al. Inosine improves neurogenic detrusor overactivity following spinal cord injury. PLoS ONE 2015, 10, e0141492. [Google Scholar] [CrossRef]
- Shang, Z.; Jia, C.; Yan, H.; Cui, B.; Wu, J.; Wang, Q.; Gao, W.; Cui, X.; Li, J.; Ou, T. Injecting RNA interference lentiviruses targeting the muscarinic 3 receptor gene into the bladder wall inhibits neurogenic detrusor overactivity in rats with spinal cord injury. Neurourol. Urodyn. 2019, 38, 615–624. [Google Scholar] [CrossRef]
- Jia, C.; Xing, T.; Shang, Z.; Cui, X.; Wang, Q.; Ou, T. Botulinum toxin A improves neurogenic bladder fibrosis by suppressing transforming growth factor β1 expression in rats. Transl. Androl. Urol. 2021, 10, 2000–2007. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Gotoh, D.; Wada, N.; Tyagi, P.; Minagawa, T.; Ogawa, T.; Ishizuka, O.; Yoshimura, N. Time-dependent progression of neurogenic lower urinary tract dysfunction after spinal cord injury in the mouse model. Am. J. Physiol. Physiol. 2021, 321, F26–F32. [Google Scholar] [CrossRef]
- Ozsoy, O.; Ozsoy, U.; Stein, G.; Semler, O.; Skouras, E.; Schempf, G.; Wellmann, K.; Wirth, F.; Angelova, S.; Ankerne, J.; et al. Functional deficits and morphological changes in the neurogenic bladder match the severity of spinal cord compression. Restor. Neurol. Neurosci. 2012, 30, 363–381. [Google Scholar] [CrossRef] [PubMed]
- Munoz, A. Neurogenic bladder dysfunction does not correlate with astrocyte and microglia activation produced by graded force in a contusion-induced spinal cord injury. Brain Res. Bull. 2017, 131, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Wada, N.; Kadekawa, K.; Majima, T.; Shimizu, T.; Tyagi, P.; Kakizaki, H.; Yoshimura, N. Urodynamic effects of intravenous and intrathecal administration of E-series prostaglandin 1 receptor antagonist on detrusor overactivity in rats with spinal cord injury. Neurourol. Urodyn. 2018, 37, 132–137. [Google Scholar] [CrossRef]
- Wada, N.; Shimizu, T.; Takai, S.; Shimizu, N.; Tyagi, P.; Kakizaki, H.; Yoshimura, N. Combinational effects of muscarinic receptor inhibition and β3-adrenoceptor stimulation on neurogenic bladder dysfunction in rats with spinal cord injury. Neurourol. Urodyn. 2017, 36, 1039–1045. [Google Scholar] [CrossRef]
- Schneider, M.P.; Sartori, A.M.; Ineichen, B.V.; Moors, S.; Engmann, A.K.; Hofer, A.S.; Weinmann, O.; Kessler, T.M.; Schwab, M.E. Anti-Nogo-A antibodies as a potential causal therapy for lower urinary tract dysfunction after spinal cord injury. J. Neurosci. 2019, 39, 4066–4076. [Google Scholar] [CrossRef]
- Horst, M.; Heutschi, J.; van den Brand, R.; Andersson, K.E.; Gobet, R.; Sulser, T.; Courtine, G.; Eberli, D. Multisystem neuroprosthetic training improves bladder function after severe spinal cord injury. J. Urol. 2013, 189, 747–753. [Google Scholar] [CrossRef]
- Sadeghmousavi, S.; Soltani Khaboushan, A.; Jafarnezhad-Ansariha, F.; Nejad-Gashti, R.; Farsi, M.; Esmaeil-Pour, R.; Alijani, M.; Majidi Zolbin, M.; Niknejad, H.; Kajbafzadeh, A.M. The role of spinal cord tractography in detecting lesions following selective bladder afferent and efferent fibers injury: A novel method for induction of neurogenic lower urinary tract dysfunction in rabbit. Neurourol. Urodyn. 2022, 41, 1539–1552. [Google Scholar] [CrossRef]
- Coelho, A.; Oliveira, R.; Cruz, F.; Cruz, C.D. Impairment of sensory afferents by intrathecal administration of botulinum toxin A improves neurogenic detrusor overactivity in chronic spinal cord injured rats. Exp. Neurol. 2016, 285, 159–166. [Google Scholar] [CrossRef]
- Doyle, C.; Cristofaro, V.; Sack, B.S.; Mahmood, F.; Sullivan, M.P.; Adam, R.M. The role of the mucosa in modulation of evoked responses in the spinal cord injured rat bladder. Neurourol. Urodyn. 2018, 37, 1583–1593. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Cao, X.; Zhang, A.; Fang, Z.; Xu, J.; Gao, X. Posterior tibial nerve stimulation improves neurogenic bladder in rats with spinal cord injury through transient receptor potential/P2X signaling pathway. Neurourol. Urodyn. 2022, 41, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Wada, N.; Shimizu, T.; Takai, S.; Shimizu, N.; Kanai, A.J.; Tyagi, P.; Kakizaki, H.; Yoshimura, N. Post-injury bladder management strategy influences lower urinary tract dysfunction in the mouse model of spinal cord injury. Neurourol. Urodyn. 2017, 36, 1301–1305. [Google Scholar] [CrossRef] [PubMed]
- Sartori, A.M.; Hofer, A.S.; Scheuber, M.I.; Rust, R.; Kessler, T.M.; Schwab, M.E. Slow development of bladder malfunction parallels spinal cord fiber sprouting and interneurons’ loss after spinal cord transection. Exp. Neurol. 2022, 348, 113937. [Google Scholar] [CrossRef] [PubMed]
- Elkelini, M.S.; Bagli, D.J.; Fehlings, M.; Hassouna, M. Effects of intravesical onabotulinumtoxinA on bladder dysfunction and autonomic dysreflexia after spinal cord injury: Role of nerve growth factor. BJU Int. 2012, 109, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, N.; Doyal, M.F.; Goins, W.F.; Kadekawa, K.; Wada, N.; Kanai, A.J.; de Groat, W.C.; Hirayama, A.; Uemura, H.; Glorioso, J.C.; et al. Morphological changes in different populations of bladder afferent neurons detected by herpes simplex virus (HSV) vectors with cell-type-specific promoters in mice with spinal cord injury. Neuroscience 2017, 364, 190–201. [Google Scholar] [CrossRef]
- Takahashi, R.; Yoshizawa, T.; Yunoki, T.; Tyagi, P.; Naito, S.; de Groat, W.C.; Yoshimura, N. Hyperexcitability of bladder afferent neurons associated with reduction of Kv1.4 α-subunit in rats with spinal cord injury. J. Urol. 2013, 190, 2296–2304. [Google Scholar] [CrossRef]
- Munoz, A.; Yazdi, I.K.; Tang, X.; Rivera, C.; Taghipour, N.; Grossman, R.G.; Boone, T.B.; Tasciotti, E. Localized inhibition of P2X7R at the spinal cord injury site improves neurogenic bladder dysfunction by decreasing urothelial P2X3R expression in rats. Life Sci. 2017, 171, 60–67. [Google Scholar] [CrossRef]
- Sartori, A.M.; Salemi, S.; Hofer, A.S.; Baumgartner, V.; Eberli, D.; Liechti, M.D.; Schwab, M.E.; Kessler, T.M. Early Transcutaneous Tibial Nerve Stimulation Acutely Improves Lower Urinary Tract Function in Spinal Cord Injured Rats. Neurotrauma Rep. 2022, 3, 15–26. [Google Scholar] [CrossRef]
- Cho, Y.S.; Ko, I.G.; Kim, S.E.; Lee, S.M.; Shin, M.S.; Kim, C.J.; Kim, S.H.; Jin, J.J.; Kim, K.H. Oral mucosa stem cells alleviates spinal cord injury-induced neurogenic bladder symptoms in rats. J. Biomed. Sci. 2014, 21, 43. [Google Scholar] [CrossRef]
- Yao, M.; Liu, G.; Li, Y.; Song, H. Possible Mechanism of Placental Mesenchymal Stem Cell-Derived Neural Cell Transplantation on the Recovery of Neurogenic Bladder Function after Spinal Cord Injury. Cell. Mol. Biol. 2022, 67, 340–347. [Google Scholar] [CrossRef]
- Elkelini Dr, M.S.; Pravdivyi, I.; Hassouna, M.M. Mechanism of action of sacral nerve stimulation using a transdermal amplitude-modulated signal in a spinal cord injury rodent model. Can. Urol. Assoc. J. 2012, 6, 227–230. [Google Scholar] [CrossRef]
- Wang, X.; Gao, Q.; Yang, X.; Wang, W.; Gu, X.; Liu, G.; Yan, P.; Gao, G.; Yu, X.; Wang, Y.; et al. Long-term anodal block stimulation at sacral anterior roots promoted recovery of neurogenic bladder function in a rabbit model of complete spinal cord injury. Neural Regen. Res. 2012, 7, 352–358. [Google Scholar]
- Liu, Q.; Wu, C.; Huang, S.; Wu, Q.; Zhou, T.; Liu, X.; Liu, X.; Hu, X.; Li, L. Decreased hyperpolarization-activated cyclic nucleotide-gated channels are involved in bladder dysfunction associated with spinal cord injury. Int. J. Mol. Med. 2018, 41, 2609–2618. [Google Scholar] [CrossRef]
- Han, J.H.; Kim, S.E.; Ko, I.G.; Kim, J.; Kim, K.H. Afferent Pathway-Mediated Effect of α1 Adrenergic Antagonist, Tamsulosin, on the Neurogenic Bladder After Spinal Cord Injury. Int. Neurourol. J. 2017, 21, 178–188. [Google Scholar] [CrossRef]
- Yang, Y.D.; Yu, X.; Wang, X.M.; Mu, X.H.; He, F. Tanshinone IIA improves functional recovery in spinal cord injury-induced lower urinary tract dysfunction. Neural Regen. Res. 2017, 12, 267–275. [Google Scholar]
- Lee, G.; Park, H.; Park, H.S.; Lee, J.G. Modulation of alpha 1 adrenergic receptors on urinary bladder in rat spinal cord injury model. Int. Neurourol. J. 2012, 16, 62–68. [Google Scholar] [CrossRef]
- Cho, Y.S.; Kim, S.J.; Kim, K.H. Evaluation of PTEN inhibitor following spinal cord injury on recovery of voiding efficiency and motor function observed by regeneration in spinal cord. Int. Neurourol. J. 2020, 24, S104–S110. [Google Scholar] [CrossRef]
- Cui, X.; Jia, C.; Yan, H.; Shang, Z.; Xing, T.; Ou, T. Effect of 3-MA on the neurogenic urinary bladder after spinal cord injury in rats by inhibiting the autophagy reaction of urinary bladder detrusor muscle cells. Acta Med. Mediterr. 2021, 37, 2905–2910. [Google Scholar]
- Shimizu, N.; Gotoh, D.; Nishimoto, M.; Hashimoto, M.; Saito, T.; Fujita, K.; Hirayama, A.; Yoshimura, N.; Uemura, H. Efficacy of vibegron, a novel β3-adrenoreceptor agonist, for lower urinary tract dysfunction in mice with spinal cord injury. Int. J. Urol. 2021, 28, 1068–1072. [Google Scholar] [CrossRef]
- Gil-Tommee, C.; Vidal-Martinez, G.; Annette Reyes, C.; Vargas-Medrano, J.; Herrera, G.V.; Martin, S.M.; Chaparro, S.A.; Perez, R.G. Parkinsonian GM2 synthase knockout mice lacking mature gangliosides develop urinary dysfunction and neurogenic bladder. Exp. Neurol. 2019, 311, 265–273. [Google Scholar] [CrossRef] [PubMed]
- McMillan, M.T.; Pan, X.Q.; Smith, A.L.; Newman, D.K.; Weiss, S.R.; Ruggieri, M.R., Sr.; Malykhina, A.P. Coronavirus-induced demyelination of neural pathways triggers neurogenic bladder overactivity in a mouse model of multiple sclerosis. Am. J. Physiol. Ren. Physiol. 2014, 307, F612–F622. [Google Scholar] [CrossRef]
- Altuntas, C.Z.; Daneshgari, F.; Izgi, K.; Bicer, F.; Ozer, A.; Sakalar, C.; Grimberg, K.O.; Sayin, I.; Tuohy, V.K. Connective tissue and its growth factor CTGF distinguish the morphometric and molecular remodeling of the bladder in a model of neurogenic bladder. Am. J. Physiol. Ren. Physiol. 2012, 303, F1363–F1369. [Google Scholar] [CrossRef]
- Lee, S.; Nedumaran, B.; Hypolite, J.; Caldwell, B.; Rudolph, M.C.; Malykhina, A.P. Differential neurodegenerative phenotypes are associated with heterogeneous voiding dysfunction in a coronavirus-induced model of multiple sclerosis. Sci. Rep. 2019, 9, 10869. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Ding, Y.; Xue, R.; Jia, Z.; Huang, Z.; Ding, Y.; Gu, C.; Yang, J. Involvement of interstitial cells of Cajal in bladder dysfunction in mice with experimental autoimmune encephalomyelitis. Int. Urol. Nephrol. 2017, 49, 1353–1359. [Google Scholar] [CrossRef] [PubMed]
- Xue, R.; Jia, Z.; Kong, X.; Pi, G.; Ma, S.; Yang, J. Effects of PGE2 EP3/EP4 receptors on bladder dysfunction in mice with experimental autoimmune encephalomyelitis. Am. J. Physiol. Ren. Physiol. 2013, 305, F1656–F1662. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.C.; Lee, T.H.; Chang, S.D. Effect of umbilical cord blood stem cells transplantation on bladder dysfunction induced by cerebral ischemia in rats. Taiwan. J. Obstet. Gynecol. 2016, 55, 672–679. [Google Scholar] [CrossRef]
- Campeau, L.; Soler, R.; Sittadjody, S.; Pareta, R.; Nomiya, M.; Zarifpour, M.; Opara, E.C.; Yoo, J.J.; Andersson, K.E. Effects of Allogeneic Bone Marrow Derived Mesenchymal Stromal Cell Therapy on Voiding Function in a Rat Model of Parkinson Disease. J. Urol. 2014, 191, 850–859. [Google Scholar] [CrossRef]
- Cho, Y.S.; Ko, I.G.; Kim, C.J.; Kim, K.H. A novel intracerebral hemorrhage-induced rat model of neurogenic voiding dysfunction: Analysis of lower urinary tract function. Mol. Med. Rep. 2015, 12, 2563–2569. [Google Scholar] [CrossRef]
- Pritchard, S.; Jackson, M.J.; Hikima, A.; Lione, L.; Benham, C.D.; Chaudhuri, K.R.; Rose, S.; Jenner, P.; Iravani, M.M. Altered detrusor contractility in MPTP-treated common marmosets with bladder hyperreflexia. PLoS ONE 2017, 12, e0175797. [Google Scholar] [CrossRef]
- Shen, J.; Zhou, G.; Chen, H.; Bi, Y. Morphology of nervous lesion in the spinal cord and bladder of fetal rats with myelomeningocele at different gestational age. J. Pediatr. Surg. 2013, 48, 2446–2452. [Google Scholar] [CrossRef] [PubMed]
- Tekin, A.; Karakuş, O.Z.; Hakgüder, G.; Ateş, O.; Özer, E.; Olguner, M.; Akgür, F.M. Distribution of interstitial cells of Cajal in the bladders of fetal rats with retinoic acid induced myelomeningocele. Turk. J. Urol. 2016, 42, 285–289. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, L.; Bi, Y.; Shen, J.; Chen, H.; Ma, Y. The Mechanism of Bladder Injury in Fetal Rats With Myelomeningocele. Front. Neurol. 2022, 13, 861308. [Google Scholar] [CrossRef]
- De Groat, W.C.; Yoshimura, N. Plasticity in reflex pathways to the lower urinary tract following spinal cord injury. Exp. Neurol. 2012, 235, 123–132. [Google Scholar] [CrossRef]
- Kadekawa, K.; Majima, T.; Shimizu, T.; Wada, N.; de Groat, W.C.; Kanai, A.J.; Goto, M.; Yoshiyama, M.; Sugaya, K.; Yoshimura, N. The role of capsaicin-sensitive C-fiber afferent pathways in the control of micturition in spinal-intact and spinal cord-injured mice. Am. J. Physiol. Ren. Physiol. 2017, 313, F796–F804. [Google Scholar] [CrossRef]
- Vizzard, M.A. Alterations in growth-associated protein (GAP-43) expression in lower urinary tract pathways following chronic spinal cord injury. Somat. Mot. Res. 1999, 16, 369–381. [Google Scholar] [CrossRef]
- De Groat, W.C.; Yoshimura, N. Changes in afferent activity after spinal cord injury. Neurourol. Urodyn. 2010, 29, 63–76. [Google Scholar] [CrossRef]
- Panicker, J.N.; Seth, J.H. C-fibre sensory nerves—Not so silent as we think? BJU Int. 2013, 112, 129–130. [Google Scholar] [CrossRef]
- James, S.L.; Theadom, A.; Ellenbogen, R.G.; Bannick, M.S.; Montjoy-Venning, W.; Lucchesi, L.R.; Abbasi, N.; Abdulkader, R.; Abraha, H.N.; Adsuar, J.C. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 56–87. [Google Scholar] [CrossRef]
- Lee, Y.-S.; Lin, C.-Y.; Jiang, H.-H.; DePaul, M.; Lin, V.W.; Silver, J. Nerve regeneration restores supraspinal control of bladder function after complete spinal cord injury. J. Neurosci. 2013, 33, 10591–10606. [Google Scholar] [CrossRef]
- Lane, M.A.; Fuller, D.D.; White, T.E.; Reier, P.J. Respiratory neuroplasticity and cervical spinal cord injury: Translational perspectives. Trends Neurosci. 2008, 31, 538–547. [Google Scholar] [CrossRef]
- Sharif-Alhoseini, M.; Khormali, M.; Rezaei, M.; Safdarian, M.; Hajighadery, A.; Khalatbari, M.; Meknatkhah, S.; Rezvan, M.; Chalangari, M.; Derakhshan, P. Animal models of spinal cord injury: A systematic review. Spinal Cord 2017, 55, 714–721. [Google Scholar] [CrossRef]
- Breyer, B.N.; Fandel, T.M.; Alwaal, A.; Osterberg, E.C.; Shindel, A.W.; Lin, G.; Tanagho, E.A.; Lue, T.F. Comparison of spinal cord contusion and transection: Functional and histological changes in the rat urinary bladder. BJU Int. 2017, 119, 333–341. [Google Scholar] [CrossRef]
- Mitsui, T.; Murray, M.; Nonomura, K. Lower urinary tract function in spinal cord-injured rats: Midthoracic contusion versus transection. Spinal Cord 2014, 52, 658–661. [Google Scholar] [CrossRef]
- Blight, A. Animal models of spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2000, 6, 1–13. [Google Scholar] [CrossRef]
- Vignes, J.R.; Deloire, M.S.; Petry, K.G.; Nagy, F. Characterization and restoration of altered inhibitory and excitatory control of micturition reflex in experimental autoimmune encephalomyelitis in rats. J. Physiol. 2007, 578, 439–450. [Google Scholar] [CrossRef] [PubMed]
- Manack, A.; Motsko, S.P.; Haag-Molkenteller, C.; Dmochowski, R.R.; Goehring, E.L., Jr.; Nguyen-Khoa, B.A.; Jones, J.K. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol. Urodyn. 2011, 30, 395–401. [Google Scholar] [CrossRef]
- Procaccini, C.; de Rosa, V.; Pucino, V.; Formisano, L.; Matarese, G. Animal models of multiple sclerosis. Eur. J. Pharmacol. 2015, 759, 182–191. [Google Scholar] [CrossRef]
- Yeo, L.; Singh, R.; Gundeti, M.; Barua, J.M.; Masood, J. Urinary tract dysfunction in Parkinson’s disease: A review. Int. Urol. Nephrol. 2012, 44, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.; Seth, J.; Batla, A.; Hofereiter, J.; Bhatia, K.P.; Panicker, J.N. Nocturia in patients with Parkinson’s disease. Mov. Disord. Clin. Pract. 2016, 3, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Blackett, H.; Walker, R.; Wood, B. Urinary dysfunction in Parkinson’s disease: A review. Park. Relat. Disord. 2009, 15, 81–87. [Google Scholar] [CrossRef]
- Kitta, T.; Ouchi, M.; Chiba, H.; Higuchi, M.; Togo, M.; Abe-Takahashi, Y.; Kusakabe, N.; Shinohara, N. Animal model for lower urinary tract dysfunction in Parkinson’s disease. Int. J. Mol. Sci. 2020, 21, 6520. [Google Scholar] [CrossRef] [PubMed]
- De Jong, T.P.; Chrzan, R.; Klijn, A.J.; Dik, P. Treatment of the neurogenic bladder in spina bifida. Pediatr. Nephrol. 2008, 23, 889–896. [Google Scholar] [CrossRef]
- Danzer, E.; Schwarz, U.; Wehrli, S.; Radu, A.; Adzick, N.; Flake, A. Retinoic acid induced myelomeningocele in fetal rats: Characterization by histopathological analysis and magnetic resonance imaging. Exp. Neurol. 2005, 194, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Chou, Y.-C.; Jiang, Y.-H.; Harnod, T.; Lee, H.-T.; Kuo, H.-C. Stroke and lower urinary tract symptoms: A neurosurgical view. Urol. Sci. 2019, 30, 8. [Google Scholar]
- Han, K.S.; Heo, S.H.; Lee, S.J.; Jeon, S.H.; Yoo, K.H. Comparison of urodynamics between ischemic and hemorrhagic stroke patients; can we suggest the category of urinary dysfunction in patients with cerebrovascular accident according to type of stroke? Neurourol. Urodyn. 2010, 29, 387–390. [Google Scholar] [CrossRef]
- Casals, J.B.; Pieri, N.C.; Feitosa, M.L.; Ercolin, A.; Roballo, K.; Barreto, R.S.; Bressan, F.F.; Martins, D.S.; Miglino, M.A.; Ambrósio, C.E. The use of animal models for stroke research: A review. Comp. Med. 2011, 61, 305–313. [Google Scholar] [PubMed]
- Fry, C.; Daneshgari, F.; Thor, K.; Drake, M.; Eccles, R.; Kanai, A.; Birder, L. Animal models and their use in understanding lower urinary tract dysfunction. Neurourol. Urodyn. 2010, 29, 603–608. [Google Scholar] [CrossRef]
- Sartori, A.M.; Kessler, T.M.; Schwab, M.E. Methods for assessing lower urinary tract function in animal models. Eur. Urol. Focus 2021, 7, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Andersson, K.E.; Soler, R.; Füllhase, C. Rodent models for urodynamic investigation. Neurourol. Urodyn. 2011, 30, 636–646. [Google Scholar] [CrossRef] [PubMed]
- Pradidarcheep, W.; Wallner, C.; Dabhoiwala, N.F.; Lamers, W.H. Anatomy and histology of the lower urinary tract. In Urinary Tract; Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2011; Volume 202, pp. 117–148. [Google Scholar]
- Longhurst, P.A.; Levendusky, M. Influence of gender and the oestrous cycle on in vitro contractile responses of the rat urinary bladder to cholinergic stimulation. Br. J. Pharmacol. 2000, 131, 177. [Google Scholar] [CrossRef] [PubMed]
- Sigala, S.; Mirabella, G.; Peroni, A.; Pezzotti, G.; Simeone, C.; Spano, P.; Cunico, S.C. Differential gene expression of cholinergic muscarinic receptor subtypes in male and female normal human urinary bladder. J. Urol. 2002, 60, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Sigala, S.; Peroni, A.; Mirabella, G.; Fornari, S.; Palazzolo, F.; Pezzotti, G.; Simeone, C.; Cunico, S.C.; Spano, P. Alpha1 adrenoceptor subtypes in human urinary bladder: Sex and regional comparison. Life Sci. 2004, 76, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Yablonsky, F.; Riffaud, J.-P.; Lacolle, J.-Y.; Dausse, J.-P. α1-and α2-adrenoceptors in the smooth muscle of mal and female rabbit urethra. Eur. J. Pharmacol. 1986, 121, 1–8. [Google Scholar] [CrossRef]
- Patra, P.B.; Patra, S. Sex differences in the physiology and pharmacology of the lower urinary tract. J. Curr. Urol. 2012, 6, 179–188. [Google Scholar] [CrossRef]
- Kobayashi, H.; Yoshiyama, M.; Zakoji, H.; Takeda, M.; Araki, I. Sex differences in the expression profile of acid-sensing ion channels in the mouse urinary bladder: A possible involvement in irritative bladder symptoms. BJU Int. 2009, 104, 1746–1751. [Google Scholar] [CrossRef]
- Streng, T.; Santti, R.; Talo, A.J. Similarities and differences in female and male rat voiding. Neurourol. Urodyn. 2002, 21, 136–141. [Google Scholar] [CrossRef]
- Cruz, Y.; Downie, J.W. Sexually dimorphic micturition in rats: Relationship of perineal muscle activity to voiding pattern. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005, 289, R1307–R1318. [Google Scholar] [CrossRef]
- Yoshiyama, M.; Roppolo, J.; Thor, K.; de Groat, W. Effects of LY274614, a competitive NMDA receptor antagonist, on the micturition reflex in the urethane-anaesthetized rat. Br. J. Pharmacol. 1993, 110, 77. [Google Scholar] [CrossRef]
- Yoshiyama, M.; Roppolo, J.R.; de Groat, W.C. Effects of LY215490, a competitive α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) receptor antagonist, on the micturition reflex in the rat. J. Pharmacol. Exp. Ther. 1997, 280, 894–904. [Google Scholar]
- Yoshiyama, M.; Roppolo, J.R.; Takeda, M.; de Groat, W.C. Effects of urethane on reflex activity of lower urinary tract in decerebrate unanesthetized rats. Am. J. Physiol. Ren. Physiol. 2013, 304, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-L.; Ma, C.-P.; de Groat, W.C.B.r. Effect of capsaicin on micturition and associated reflexes in chronic spinal rats. Brain Res. 1995, 678, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, N.; Ogawa, S.; Sugiyama, R.; Homma, Y.; Igawa, Y. Influence of urethane-anesthesia on the effect of resiniferatoxin treatment on bladder function in rats with spinal cord injury. Neurourol. Urodyn. 2015, 34, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Field, K.; Lang, C. Hazards of urethane (ethyl carbamate): A review of the literature. Lab. Anim. 1988, 22, 255–262. [Google Scholar] [CrossRef]
- Van Asselt, E.; Choudhary, M.; Clavica, F.; van Mastrigt, R. Urethane anesthesia in acute lower urinary tract studies in the male rat. Lab. Anim. 2017, 51, 256–263. [Google Scholar] [CrossRef]
- Li, W.J.; Kim, J.M.; Oh, S.-J. Effects of level of consciousness on urodynamic procedure in female cats. J. Korean Med. Sci. 2011, 26, 803–806. [Google Scholar] [CrossRef]
- Fraser, M.O.; Smith, P.P.; Sullivan, M.P.; Bjorling, D.E.; Campeau, L.; Andersson, K.E.; Yoshiyama, M. Best practices for cystometric evaluation of lower urinary tract function in muriform rodents. Neurourol. Urodyn. 2020, 39, 1868–1884. [Google Scholar] [CrossRef]
- Morikawa, K.; Kakiuchi, M.; Fukuoka, M.; KATO, H.; ITO, Y.; GOMI, Y.J. Effects of various drugs on bladder function in conscious restrained-denervated rats placed in a restraining cage and produced by transection of the hypogastric nerve. Jpn. J. Pharmacol. 1990, 52, 405–411. [Google Scholar] [CrossRef]
- Alkis, O.; Zumrutbas, A.E.; Toktas, C.; Aybek, H.; Aybek, Z. The use of biomarkers in the diagnosis and treatment of overactive bladder: Can we predict the patients who will be resistant to treatment? Neurourol. Urodyn. 2017, 36, 390–393. [Google Scholar] [CrossRef]
- Schneider, M.P.; Hughes, F.M., Jr.; Engmann, A.K.; Purves, J.T.; Kasper, H.; Tedaldi, M.; Spruill, L.S.; Gullo, M.; Schwab, M.E.; Kessler, T.M. A novel urodynamic model for lower urinary tract assessment in awake rats. BJU Int. 2015, 115, 8–15. [Google Scholar] [CrossRef]
- Compérat, E.; Reitz, A.; Delcourt, A.; Capron, F.; Denys, P.; Chartier-Kastler, E. Histologic features in the urinary bladder wall affected from neurogenic overactivity—A comparison of inflammation, oedema and fibrosis with and without injection of botulinum toxin type A. Eur. Urol. 2006, 50, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, Y.; Kanai, A. Urotheliogenic modulation of intrinsic activity in spinal cord-transected rat bladders: Role of mucosal muscarinic receptors. Am. J. Physiol. Ren. Physiol. 2008, 295, F454–F461. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Yu, S.; Hu, X.; Li, Y.; You, X.; Tian, D.; Cheng, L.; Zheng, M.; Jing, J. Fibrotic Scar After Spinal Cord Injury: Crosstalk With Other Cells, Cellular Origin, Function, and Mechanism. Front. Cell Neurosci. 2021, 15, 720938. [Google Scholar] [CrossRef]
- Denk, F.; Bennett, D.L.; McMahon, S.B. Nerve Growth Factor and Pain Mechanisms. Annu. Rev. Neurosci. 2017, 40, 307–325. [Google Scholar] [CrossRef] [PubMed]
- Pezet, S.; McMahon, S.B. Neurotrophins: Mediators and modulators of pain. Annu. Rev. Neurosci. 2006, 29, 507–538. [Google Scholar] [CrossRef] [PubMed]
- Ochodnicky, P.; Cruz, C.D.; Yoshimura, N.; Cruz, F. Neurotrophins as regulators of urinary bladder function. Nat. Rev. Urol. 2012, 9, 628–637. [Google Scholar] [CrossRef]
- Cruz, C.D. Neurotrophins in bladder function: What do we know and where do we go from here? Neurourol. Urodyn. 2014, 33, 39–45. [Google Scholar] [CrossRef]
- Clemow, D.B.; Steers, W.D.; Tuttle, J.B. Stretch-activated signaling of nerve growth factor secretion in bladder and vascular smooth muscle cells from hypertensive and hyperactive rats. J. Cell Physiol. 2000, 183, 289–300. [Google Scholar] [CrossRef]
- Persson, K.; Steers, W.D.; Tuttle, J.B. Regulation of nerve growth factor secretion in smooth muscle cells cultured from rat bladder body, base and urethra. J. Urol. 1997, 157, 2000–2006. [Google Scholar] [CrossRef]
- Coelho, A.; Wolf-Johnston, A.S.; Shinde, S.; Cruz, C.D.; Cruz, F.; Avelino, A.; Birder, L.A. Urinary bladder inflammation induces changes in urothelial nerve growth factor and TRPV1 channels. Br. J. Pharmacol. 2015, 172, 1691–1699. [Google Scholar] [CrossRef]
- Kuo, H.C.; Liu, H.T.; Chancellor, M.B. Can urinary nerve growth factor be a biomarker for overactive bladder? Rev. Urol. 2010, 12, e69–e77. [Google Scholar] [PubMed]
- Guerios, S.D.; Wang, Z.Y.; Boldon, K.; Bushman, W.; Bjorling, D.E. Blockade of NGF and trk receptors inhibits increased peripheral mechanical sensitivity accompanying cystitis in rats. Am. J. Physiology. Regul. Integr. Comp. Physiol. 2008, 295, R111–R122. [Google Scholar] [CrossRef] [PubMed]
- Oddiah, D.; Anand, P.; McMahon, S.B.; Rattray, M. Rapid increase of NGF, BDNF and NT-3 mRNAs in inflamed bladder. Neuroreport 1998, 9, 1455–1458. [Google Scholar] [CrossRef] [PubMed]
- Seki, S.; Sasaki, K.; Fraser, M.O.; Igawa, Y.; Nishizawa, O.; Chancellor, M.B.; de Groat, W.C.; Yoshimura, N. Immunoneutralization of nerve growth factor in lumbosacral spinal cord reduces bladder hyperreflexia in spinal cord injured rats. J. Urol. 2002, 168, 2269–2274. [Google Scholar] [CrossRef] [PubMed]
- Seki, S.; Sasaki, K.; Igawa, Y.; Nishizawa, O.; Chancellor, M.B.; de Groat, W.C.; Yoshimura, N. Suppression of detrusor-sphincter dyssynergia by immunoneutralization of nerve growth factor in lumbosacral spinal cord in spinal cord injured rats. J. Urol. 2004, 171, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, N.; Bennett, N.E.; Hayashi, Y.; Ogawa, T.; Nishizawa, O.; Chancellor, M.B.; de Groat, W.C.; Seki, S. Bladder overactivity and hyperexcitability of bladder afferent neurons after intrathecal delivery of nerve growth factor in rats. J. Neurosci. 2006, 26, 10847–10855. [Google Scholar] [CrossRef]
- Ramer, L.M.; Ramer, M.S.; Steeves, J.D. Setting the stage for functional repair of spinal cord injuries: A cast of thousands. Spinal Cord 2005, 43, 134–161. [Google Scholar] [CrossRef]
- Cregg, J.M.; DePaul, M.A.; Filous, A.R.; Lang, B.T.; Tran, A.; Silver, J. Functional regeneration beyond the glial scar. Exp. Neurol. 2014, 253, 197–207. [Google Scholar] [CrossRef]
- Alizadeh, A.; Dyck, S.M.; Karimi-Abdolrezaee, S. Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Front. Neurol. 2019, 10, 282. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Miyazato, M.; Yokoyama, H.; Kita, M.; Hirao, Y.; Chancellor, M.B.; Yoshimura, N. Role of M2 and M3 muscarinic acetylcholine receptor subtypes in activation of bladder afferent pathways in spinal cord injured rats. Urology 2012, 79, 1184.e15–1184.e20. [Google Scholar] [CrossRef]
- Tyagi, P. Pathophysiology of the urothelium and detrusor. Can. Urol. Assoc. J. 2011, 5 (Suppl. 2), S128–S130. [Google Scholar] [CrossRef] [PubMed]
- Kennelly, M.; Dmochowski, R.; Schulte-Baukloh, H.; Ethans, K.; Del Popolo, G.; Moore, C.; Jenkins, B.; Guard, S.; Zheng, Y.; Karsenty, G. Efficacy and safety of onabotulinumtoxinA therapy are sustained over 4 years of treatment in patients with neurogenic detrusor overactivity: Final results of a long-term extension study. Neurourol. Urodyn 2015, 36, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Traini, C.; Vannucchi, M.G. The Botulinum Treatment of Neurogenic Detrusor Overactivity: The Double-Face of the Neurotoxin. Toxins 2019, 11, 614. [Google Scholar] [CrossRef] [PubMed]
- Schwinn, D.A.; Roehrborn, C.G. Alpha1-adrenoceptor subtypes and lower urinary tract symptoms. Int. J. Urol. 2008, 15, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Merrill, L.; Gonzalez, E.J.; Girard, B.M.; Vizzard, M.A. Receptors, channels, and signalling in the urothelial sensory system in the bladder. Nat. Rev. Urol. 2016, 13, 193–204. [Google Scholar] [CrossRef]
- Silver, J.; Miller, J.H. Regeneration beyond the glial scar. Nat. Rev. Neurosci. 2004, 5, 146–156. [Google Scholar] [CrossRef]
- Andrews, E.M.; Richards, R.J.; Yin, F.Q.; Viapiano, M.S.; Jakeman, L.B. Alterations in chondroitin sulfate proteoglycan expression occur both at and far from the site of spinal contusion injury. Exp. Neurol. 2012, 235, 174–187. [Google Scholar] [CrossRef]
- Giger, R.J.; Hollis, E.R., 2nd; Tuszynski, M.H. Guidance molecules in axon regeneration. Cold Spring Harb. Perspect. Biol. 2010, 2, a001867. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Cheriyan, T.; Ryan, D.J.; Weinreb, J.H.; Cheriyan, J.; Paul, J.C.; Lafage, V.; Kirsch, T.; Errico, T.J. Spinal cord injury models: A review. Spinal Cord 2014, 52, 588–595. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]

| Study | Model | Species | Sex | Induction Method | Urodynamic Findings | Changes in Bladder Tissue | Changes in Neuronal Tissue | Therapies/Mechanisms Identified |
|---|---|---|---|---|---|---|---|---|
| Chambel et al., 2022 [28] | SCI | Rat | Female | Complete cord transection T8/T9 | Cystometry under urethane anesthesia: at 7 dpi, bladder contractions were abolished, while at 28 dpi, the NDO was established, with the parameters of frequency, amplitude, basal pressure, and peak pressure augmenting in comparison with intact rats. | Changes in lumbosacral expression of axonal growth regulators: neurocan, phosfacan, nogoA, MAG, OMgp, RGMa: Increase at 7 dpi and decrease to basal levels at 28 dpi -Decrease in the DRG of those specific receptors: CSPG- and MAI-receptors. | NGF regulates the expression of receptors for axonal guidance cues in DRG neurons. When exposed to high levels of NGF, some repulsive cues decrease its expression. | |
| Zhang et al., 2019 [29] | SCI | Rat | Female | Complete cord transection T8/T9 at suprasacral levels | After acupuncture treatment: -Decrease in bladder weight; -Decrease in fibrosis levels and smooth muscle cell damage; -Increase in NGF and TRka and p-akt with treatment: nerve regeneration. | Sacral electroacupuncture therapy can improve the expression of both NGF/TrkA signaling and AKT signaling in the local nerve of the damaged spinal cord and is capable of improving micturition function after injury. | ||
| Kullmann et al., 2018 [30] | SCI | Mouse | Female | Complete cord transection at T8–T9 | -TRPM4 levels largely increase after SCT—earlier time points 3–7 days; -Blocking of TRPM4 activity (by an antagonist) reduces spontaneous muscle activity. | Pharmacological blocking of TRPV4 (9-phenanthrol-ANTAGONIST) reduces spontaneous phasic activity developed after SCI, showing its involvement in SCI-induced bladder neurogenic activity. | ||
| Gotoh et al., 2020 [31] | SCI | Mouse | Female | Complete cord transection T8–T9 | Awake cystometry: decreased number of non-voiding contractions in vibregon treated rats; the time required to induce the first voiding was higher. | Increase in mRNA levels of collagen, TGF-B1, FGF-2, HIF-a, VEGF-a (ischemic molecules); Vibregon treatment decreased the levels of collagen, TGF and HIF; collagen protein levels were not altered. | Vibregron (β3-adrenoceptor agonist) treatment reduces non-voiding contractions and decreases the expression levels of fibrosis- and ischemia-related molecules. | |
| Chung et al., 2015 [32] | SCI | Rat | Male | Complete transection, or cord compression | Awake cystometry: injured animals presented detrusor overactivity, showing frequent non-voiding contractions; treatment with inosine reduced the frequency and amplitude of detrusor contractions. | -Decreased expression of synaptophysin (SYP); -Decreased expression of NF200-positive axons in bladder; -Increased TRPV1 expression. Inosine treatment attenuated these alterations. | Inosine treatment (immediate or delayed) reduces urinary complications after SCI. The mechanisms are unclear, but it is known that it is not related to muscle contractility, and maybe is through TRPV1. | |
| Shang et al., 2019 [33] | SCI | Rat | Female | Complete transection at T9–T10 | Awake cystometry: increased basal pressure,maximum voiding pressure, threshold pressure, volume of residual urine, and number of voiding contractions; decreased inter-contraction interval. All features attenuated by treatment. | Decreases expression of M3 receptor mRNA in SCI animals, and treatment decreased this expression; M3 receptor protein expression does not correlate with changes in the level of M3 receptor mRNA. | Downregulation of M3 receptor expression in the bladder wall by lentivirus-mediated RNAi can significantly decrease urinary dysfunction, targeting NDO symptoms associated with SCI. | |
| Jia et al., 2021 [34] | SCI | Rat | Female | Complete transection at T10 | Awake cystometry: increase in non-voiding contractions; botox attenuated this, more in earlier treatments than late. | -Increase in bladder weight, levels of connective tissue/fibrosis; -TGF-β1 (TGF-β1 is a major driver of human fibrotic protein) expression increased.Treatment with BoNTA decreased significantly in the early group compared with the late group; mRNA levels were in line with this. | Early BoNTA injection had a tendency to prevent bladder fibrosis and improve NDO, downregulating TGF-β1 expression. | |
| Saito et al., 2021 [35] | SCI | Mouse | Female | Complete transection at T8/9 | Awake cystometry: -Non-voiding contractions were observed at 2 weeks post injury; bladder capacity was increased at 6 weeks; -DSD was observed 2 weeks post injury, but periodic EMG reductions that produce voiding were not observed at this time point, until 4 weeks. | Increase in BDNF at all injury timepoints: higher at 2 weeks and decreases at 4 and 6 weeks, but never returning to basal levels. | Increase in mRNA levels of TRPV1, ASIC1, ASIC3-, and piezo2 DRG L6-S1. | The development of DSD might be related to changes in the expression of mechanosensitive channels such as ASICs and Piezo2; changes in these channels are accompanied by changes in BDNF expression. |
| Oliveira et al., 2019 [26] | SCI | Rat | Female | Complete transection at T8/9 | Cystometry under urethane anesthesia: increased frequency of bladder contractions and higher peak pressures; RTX treatment attenuated this. | -Increase in bladder wall thickness; -Increase in bladder TRPV1; RTX treatment attenuated this. | -Severe loss of gray matter arrangement in dorsal and ventral horns, with white-matter disruption and several cavities; -Increase in lumbosacral spinal GAP43 and CGRP expression. | The neurotoxin RTX is capable of reducing urinary symptoms related to SCI; these effects were only seen in the bladder, not affecting the spinal cord. |
| Ozsoy et al., 2012 [36] | SCI | Rat | Female | Spinal compression at T8 | One week after SCI, all groups presented bladder areflexia; in the severe contusion group, urinary function did not improve. Mild contusion rats presented better scores following the third week after lesion. | Detrusor hyperinnervation: increases in β-III-tubulin. | Bladder function was significantly worse following severe compared to moderate compression injury. | |
| Munoz et al., 2017 [37] | SCI | Rat | Female | Spinal contusion at T8/T9: mild and severe | Cystometry under urethane anesthesia: after mild contusion, mice presented increased inter-contractile intervals, high number of non-voiding contractions, and longer duration of the IPHFO (duration of intra-luminal pressure high frequency oscillations). Severe contusion mice showed a high NVC frequency, practically absent IPHFO events, and small voiding volumes. | -GFAP increase (astrogliosis) and microglial activation in both groups 4 weeks after SCI (at injury level). | Independent of the impact intensity, a contusion SCI increases microglia and astrocyte infiltration into the injured region without a strong correlation with locomotor impairment; bladder dysfunction is worse in severe than mild contusion. | |
| Wada et al., 2018 [38] | SCI | Rat | Female | Complete transection at T9–T10 | Awake cystometry: the time to the first non-voiding contraction was significantly prolonged after both 0.1 and 1.0 mg/kg of intravenous administration of SC51089; other parameters were not altered. | Increase in PGE2 concentration of the L6 and S1 spinal segments; the mRNA expressions of EP1 receptors of the L6 and S1 spinal cord and DRG from SCI rats were increased. | SC51089-prostaglandin 1 receptor antagonist PGE2-induced EP1 receptor activation is involved in the initiation of C-fiber excitation to trigger NVC in SCI rats. | |
| Wada et al., 2017 [39] | SCI | Rat | Female | Complete transection T8–T9 | Awake cystometry: inter-contraction interval, bladder capacity, and bladder compliance were significantly increased in SCI animals treated with combination therapy, and not monotherapies; the time required for the first NVC was significantly prolonged in the oxybutynin and combination group. | Type 3 collagen, HIF-1a, TGF-β1, and FGF-β (actors involved in tissue remodeling and hipoxia) were reduced in oxybutynin and combination therapy; in mirabegron therapy, the expression of mRNA of HIF-1α and TGF-β1 was significantly reduced compared to controls. | The combination therapy of an anticholinergic agent (oxybutynin) and a b3-adrenoceptor agonist (mirabegron) elevated the bladder elastin level, reduced NVCs, and increased bladder compliance to a greater extent than the monotherapy of either drug in SCI. | |
| Shneider et al., 2019 [40] | SCI | Rat | Female | Incomplete or complete transection at T8 | Awake cystometry: bladder was areflexic the first week after injury; over the following 3 weeks, maximum detrusor pressure constantly increased, exceeding the baseline measurements at 4 weeks; reduction in voiding rates and urine volumes; reduction in bladder compliance; development of DSD. Treatment with aniti-Nogo-A improved several urodynamic parameters. | After 4 weeks, animals treated with vehicles showed decrease in CRF-positive innervation of Lam X; animals treated with anti-Nogo-A antibody presented values similar to intact rats; in the IML region, both injury groups showed a reduced CRF-positive fiber density; anti-Nogo-A antibody-treated rats showed a trend for higher GABAergic values, GAD2 mRNA-positive cells decreased in L6-S1. | Anti-Nogo-A antibody treatment improved urodynamic and electrophysiological parameters in SCI animals, namely a pronounced recovery of the physiological EUS function during voiding. This is likely due to protection of spared descending fibers from the PMC sprouted below the level of the injury in a specific target region, Lam X, thereby restoring functional input from the key bladder control system. | |
| Sadeghmousavi 2022 [41] | SCI | Rabbit | Male | Spinal cord cauterization at T12-L1 | Cystometry under urethane anesthesia: increase in bladder capacity, decrease in leak point pressure, increase in leak point volume. | Lymphoid tissue hyperplasia; nerve markers (NF200 and S100) positive at muscular sites. | In injured spinal segments, S100 was increased and NF-200 was diminished. | This method of NLUTD induction was without the leg’s neurological deficit, easily applicable, low-cost, and was accompanied by minimal surgical preparation and a satisfactory survival rate in comparison with other SCI animal models. |
| Horst et al., 2013 [42] | SCI | Rat | Female | Two opposite lateral hemisections (T7 and T11) | Awake cystometry: increased number of non-voiding contractions, showing signs of detrusor overactivity; the treatment significantly attenuated bladder dysfunction, but not to basal levels. | PGP 9.5 (general nerve marker) was increased in trained rats and decreased in non-trained rats (reduced detrusor hypertrophy); NF200 afferent fiber innervation was reduced in non-trained animals; the NF200:PGP ratio was significantly lower in trained RATS; non-trained rats showed a trend for low TH density. | A multisystem neuroprosthetic training program counteracts the emergence of neurogenic bladder dysfunction and improves bladder function in rats with severe SCI. | |
| Frias et al., 2015 [27] | SCI | Rat | Female | Complete transection at T9 | Cystometry under urethane anesthesia: one week after SCI, the animals presented bladder areflexia; four-week SCI, NDO was evident, with increase in the values of frequency, peak pressure, baseline pressure, and amplitude of urinary function; chronic BDNF sequestration during the first week promoted an earlier appearance of NDO; BDNF sequestration starting at 4 weeks almost abolished bladder contractions. | Time-dependent increase in BDNF expression: L5–L6 segments; GAP-43 expression increased after SCI in thin fibers coursing in the superficial laminae of the dorsal horn; continuous BDNF sequestration during spinal shock resulted in intense GAP-43 expression; increase in phosphoJNK in laminae I–II of the experimental groups in which axonal sprouting was more pronounced. | BDNF is involved in the long-term maintenance of NDO arising after SCI, as an important modulator of sensory afferent sprouting, the key mechanism underlying NDO emergence. | |
| Coelho et al., 2016 [43] | SCI | Rat | Female | Complete transection at T8 | Cystometry under urethane anesthesia: increased frequency and basal pressure; decreased amplitude of contractions; treatment with botox normalized these parameters to basal conditions. | Onabot/A cleaves SNAP-25 in L5-S1 spinal segments, coursing laminae I and II of the dorsal horns. Increase in CGRP expression at L5-S1 spinal cord (laminae III and IV) and at DRG level; treatment reduced this. Increase in ATF3 (marker of neuronal stress) expression; treatment further increased this. | Botulinum toxin A improves SCI-induced NDO, acting predominantly on bladder sensory fibres. The mechanism of action of Onabot/A includes the cleavage of SNAP-25 in sensory terminals but also impairment of basic cellular machinery in the cell body of sensory neurons. | |
| Doyle et al., 2018 [44] | SCI | Rat | Male | Complete transection at T8 | The level of the muscarinic M2 receptor was decreased in the mucosa of SCI bladders. | Detrusor-mucosa interactions are substantially altered in the neurogenic bladder. | ||
| Song et al., 2022 [45] | SCI | Rat | Female | Contusion at T10 | Awake cystometry: the basic pressure, maximum pressure, the pressure of leakage point, maximum capacity, residual urine volume, and internal bladder pressure were significantly increased in the SCI group compared with non-SCI groups; treatment improved these features. | -Bladder was enlarged, with a rough and thicker bladder wall; -Abnormal mucosa (both epithelium and lamina propria) with a significant inflammatory infiltrate with neutrophils and monocytes, accompanied by microvascular rupture and bleeding. Treatment improved lamina propria inflammation. | Reduction in mRNAs and proteins of TRPA1, TRPV1, P2X2, and P2X3 both in bladder and L6-S1 DRG; PTNS treatment attenuated this. | Posterior tibial nerve stimulation (PTNS) improves SCI-induced functional and histological impairment of the bladder, via the TRP/P2X signaling pathway. |
| Wada et al., 2017 [46] | SCI | Mouse | Female | Complete transection at the T8–T9 level | Awake cystometry: bladder capacity, post-void residual urine, and the number of non-voiding contractions during storage were larger when the bladder of SCI animals was only squeezed once daily, compared with twice and thrice. | -At 4 weeks after SCI, the bladder weight was reduced in animals who had their bladders more frequently squeezed; -Levels of NGF protein in the bladder mucosa of SCI mice were higher; -Levels of NGF were lower in animals who had their bladders more frequently squeezed. | The expression of P2X2, P2X3, TRPA1, and TRPV1 mRNA was increased in SCI mice (DRG), when compared to spinal intact mice. | The post-injury bladder management with an increased number of daily bladder emptying improves the storage and voiding LUTD after SCI, associated with the decrease in bladder NGF and reductions in C-fiber afferent marker receptors in bladder afferent pathways. |
| Sartori et al., 2022 [47] | SCI | Rat | Female | Incomplete transection at the T8–T9 level | Awake cystometry: Increased maximum intravesical pressure, voiding time, post-void residual volume, and the number of non-voiding contractions. Reduced maximum flow rate, voided volume, and voiding efficiency. | Reduction in the density of 5-HT-positive fibers in both lamina X and ventral horn. 5-HT density increased over time, but remains severely affected up to 4 weeks after SCI; -Decrease in CRF-positive fiber density in the intermedio-lateral column (and lamina X), but partially at 4 weeks; -Increase in CGRP density only 2–3 weeks after SCI; -Decrease in the glutamatergic neurons (VGLUT2 mRNA-positive) in the laminae I, II and III of the dorsal horn, but not in laminae IV–V and X; -Decrease in GABAergic cells (GAD2 mRNA-positive) in the laminae I, II, III, IV and V. | Detrusor overactivity is possibly influenced by the sprouting of afferent fibers of type C in the dorsal horn responding to bladder distension, while DSD might be driven by decreased bulbospinal input to and a reduced number of inhibitory GABAergic interneurons in the lumbosacral cord. | |
| Elkelini et al., 2012 [48] | SCI | Rat | Female | Complete transection at T4 | Awake cystometry: increased number of non-voiding contractions, basal pressure, and increase in maximum voiding pressure; intravesical onabotA reduced the number of uninhibited contractions and lowered the maximum pressure, but had no effect on resting pressure. | Increase in NGF bladder concentration; onabotA treatment significantly reduced NGF levels. | (3 weeks after SCT) Increase in NGF concentration in the dorsal root ganglia (DRG) of the T4 root; onabotA treatment decreased NGF concentration. | Intravesical onabotulinumtoxinA blocks autonomic dysreflexia in rats with T4-SCT, due to a decrease in NGF concentrations at the bladder and dorsal root ganglia T4, which suggests an afferent pathway modulation by intravesical onabotA treatment. |
| Shimizu et al., 2017 [49] | SCI | Mouse | Female | Complete transection of T8–T9 | -Increase in the number of CGRP and TRPV1 promoter vector-labeled cells in L1 and L6 DRG; the median cell size of CGRP neurons was increased, while TRPV1 was decreased; -Decrease in the number of NF200 promoter vector-labeled cells in L6 DRG; the median cell size of the NF200 neurons was larger. | SCI induces morphological changes in bladder afferent pathways, especially in the C-fiber cell population, along with upregulation of CGRP and TRPV1 expression in bladder afferent neurons. | ||
| Takahashi et al., 2013 [50] | SCI | Rat | Female | Complete transection at T9–T10 | The ratio of Kv1.4 α-subunit staining density in bladder afferent and unlabeled DRG neurons was lower in spinal transected animals. | The excitability of C-fiber bladder afferent neurons is increased in association with reduction in KA current density and Kv1.4 α-subunit expression in SCI rats. | ||
| Munoz et al., 2017 [51] | SCI | Rat | Female | Bilateral dorsal lesion T8–T9 | Cystometry under urethane anesthesia: SCI increased duration of intraluminal pressure, high-frequency oscillations, and non-voiding contractions’ frequency; These parameters were improved by P2X7R antagonist treatment. | -Increased expression of beta-actin marker; -Increased levels of urothelial P2X3 receptors; treatment with P2X7R antagonist attenuated both findings. | -Activation and infiltration of microglia in T7/T8 dorsal horn areas in non-BBG treated SCI groups. -The density of CD11b-positive microglia cells and the percentage of activated microglia were significantly reduced in treated rats. | P2X7R antagonist (BBG) induced a significant reduction in the frequency of non-voiding detrusor contractions, which was correlated with a lower amount of activated microglia. |
| Sartori et al., 2022 [52] | SCI | Rat | Female | Hemisection at T8–T9 | Awake cystometry: transcutaneous tibial nerve stimulation induced fewer episodes of non-voiding contractions, a lower maximum intravesical pressure during the storage phase, a higher voided volume, and a lower post-void residual volume in SCI rats, resulting in a higher voiding efficiency; the beneficial effect in bladder urodynamics disappeared one week after the end of the stimulation period. | The unstimulated sham animals had a bigger and heavier bladder compared with animals that underwent tibial nerve stimulation. | Higher density of CGRP-positive structures in layer I and II of the dorsal horn of L6 and S1 in the stimulated group (not statistically significant). | Application of transcutaneous tibial nerve stimulation in rats early after SCI had a beneficial influence on the development of lower urinary tract dysfunction that typically arises after an incomplete SCI. |
| Cho et al., 2014 [53] | SCI | Rat | Male | T11 damage using a surgical gouge | Cystomery under zolotyl anesthesia: increase in contraction pressure and the contraction time; oral mucosa stem cells transplantation into the injury area ameliorated these features | The transplantation of oral mucosa stem cells decreased the SCI lesion, once new tissues were increased in the surroundings of the damaged tissues, reduced apoptosis, and increased the spinal cord tissues SMA-α and Ki67 expressions; c-Fos and NGF expression in the neuronal voiding centers in SCI animals were also reduced by the treatment. | Transplantation of oral mucosa stem cells ameliorated the SCI-induced neurogenic bladder symptoms by inhibiting apoptosis and enhancing cell proliferation. As result, SCI-induced neuronal activation in the neuronal voiding centers was suppressed, showing the normalization of voiding function. | |
| Yao et al., 2022 [54] | SCI | Rat | Unspecified | Spinal compression at T13 | Cystometry under chloral hydrate: placental mesenchymal stem cell-derived neural cell transplantation increased the maximum bladder capacity and bladder compliance, and decreased the bladder basic pressure and urinary leakage pressure in SCI rats. | Placental mesenchymal stem cell-derived neural cell transplantation improves the ultrastructure of detrusor muscle tissue (reduces the rough endoplasmic reticulum, mitochondrial swelling, and thigh fibrils) and improves the elasticity and compliance of detrusor muscles. | -SCI up-regulates caspase-3 protein expression in the spinal cord; the TUNNEL value after placental mesenchymal stem cell transplantation decreased significantly in SCI rats. | Placental mesenchymal stem cell transplantation increased bladder dysfunction after SCI. Cell transplantation can rapidly differentiate into nerve cells to compensate for the massive apoptosis of cells associated with the lesion. |
| Elkelini et al., 2012 [55] | SCI | Rat | Female | Complete transection at T10 | Awake cystometry: transected rats developed uninhibited contractions, increased resting pressure, increased threshold pressure, and increased maximum voiding pressure; short-term sacral neurostimulation reduced the threshold pressure, but no other urodynamic parameters were significantly affected. | Increase in CGRP content (L6DRG); neurostimulation reduced this, | Sacral neuromodulation (SNM) reduced threshold pressure and CGRP content at L6 DRG, which may explain the modulatory effect on the C-fiber afferents supplying the urinary bladder. Chronic stimulation may be required to produce significant changes in all CMG parameters. | |
| Wang et al., 2012 [56] | SCI | Rabbit | Female | Spinal compression by aneurysm clip at T10 | Awake cystometry: 2 weeks after SCI, basal pressure, leak-point pressure, and residual urine volume increased; the detrusor was hyperactive during bladder filling, DSD occurred during voiding; bladder compliance was decreased. Four weeks of accumulated sacral anterior root stimulation of anodal block: intravesical pressure, maximum bladder pressure, maximum detrusor pressure, bladder leak-point pressure, resting pressure, and residual volume decreased, while bladder capacity and voiding volume increased. | -Bladder expression of the M2 receptor, P2X3 receptor, and NGF increased in SCI animals; decreased after 4-week electrical stimulation; -Expression of the M3 receptor and β2-adrenergic receptor decreased following SCI, increasing after 4-week electrical stimulation. | Long-term sacral anterior root stimulation of anodal block in rabbits following SCI could repair urinary function. The recovery neurotransmitter receptor expression and decreased NGF expression could be one of the mechanisms of action. | |
| Liu et al., 2018 [57] | SCI | Rat | Female | Complete transection at S2 | Cystometry under urethane anesthesia: typical voiding contractions of the bladder were not observed in SCI rats, they were replaced by several irregular micturition waves with low amplitude. | -Detrusor hypertrophy; -Increase in mesenchyme matter; -Increase in bladder volume; -The mRNA and protein expression levels of four HCN subtypes were decreased, with the HCN1 channel being the most significant; all four HCN subtypes were expressed in single bladder interstitial cells of Cajal-like cells (ICC-LCs); -The protein levels of Trip8b, Nedd4-2, and NRSF were upregulated, while filamin A was downregulated. | Decreased bladder HCN channel expression and function induced by altered regulatory proteins are involved in the pathological process of SCI-induced neurogenic bladder. | |
| Han et al., 2017 [58] | SCI | Rat | Female | T11 damage using a surgical gouge | Cystometry with zolotyl anesthesia: increased basal contraction pressure and contraction time; tamsulosin treatments decreased the basal contraction pressure and time, dose-dependently. | Increased c-Fos, NGF and NADPH-d expression in the vlPAG, PMC, and spinal dorsal horn (L5); tamsulosin treatment suppressed these increases. | Tamsulosin (α1-adrenoceptor antagonist) treatment suppressed NDO symptoms and c-fos and NGF augmentation after SCI, showing that it can be used to attenuate bladder dysfunction following SCI. | |
| Yang et al., 2017 [59] | SCI | Rat | Female | Contusion at T10 | Awake cystometry: reduction in inter-contraction interval, voided volume, and voiding efficiency; increased basal pressure, threshold pressure and bladder capacity. Bladder function was improved by treatment with tanshinone IIAh methylprednisolone. | -Increased bladder weight; -Increase in thickness of bladder detrusor; -Vascular alterations, edema, and proliferation of urothelial layers; the umbrella cell layer was disrupted and a marked neutrophil infiltration to the suburothelial tissue as well as blood vessel congestion and dilation was observed; treatment with tanshinone IIA and methylprednisolone reduced these features. | -Decrease in motor neurons in the anterior horn, paired with a reduction in Nissl body conspicuity; -DRGs L6-S1 presented a large number of inflammatory cells; -DRGs L6-S1 neurons cell bodies became hypertrophic and elongated with some of the nuclei shrunken or disappeared. Some Nissl bodies also disappeared or were replaced by vacuoles. All these features were attenuated by Tanshinone IIA and methylprednisolone treatments. | Tanshinone IIA and methylprednisolone improved functional recovery after SCI-induced lower urinary tract dysfunction by remodeling the spinal pathway involved in lower urinary tract control. |
| Lee at al., 2012 [60] | SCI | Rat | Female | Contusion at T8 | -Increased bladder weight; -Increased mRNA expression of GAPDH. In the control group, the most-expressed α1 AR subtype was α1a and in the SCI group α1d, but SCI had lower expression than all the suited receptors (α1a, α1b, α1d). | SCI modulates the α1 AR mRNA subtypes in rat urinary bladder. The relatively increased α1d or decreased α1a AR mRNA expression may be a therapeutic candidate for controlling symptoms of neurogenic bladder after SCI. | ||
| Cho et al., 2020 [61] | SCI | Rat | Male | Contusion at T8 | Awake cystometry: decreased bladder contraction pressure and contraction time; increased intercontractional interval. TGN administration attenuated these changes. | Increased VEGF, NGF, and BDNF expression in spinal injury site; TGN treatment suppressed the expression. | Treatment with a PTEN inhibitor (TGN) induced functional recovery and resulted in significantly lower expression of VEGF, NGF, and BDNF at injury site. | |
| Cui et al., 2021 [62] | SCI | Rat | Male | Complete transection at T9 | -Increase in collagen and reduction in smooth muscle fibers; disorganization of these fibers’ distribution; -The ratio of type I/III collagen in bladder smooth muscle cells was higher than in controls. Treatment with 3-methyladenine improved the overall histological changes. | -Enlargement of the space around the nerve cells in the spinal cord; appearance of blurred nucleolus, swollen cells, and vaculose. After treatment, the number of necrotic nerve cells and vacuoles in the spinal cord tissue was reduced and the degree of inflammatory infiltration was reduced; -Increased LC3-II expression levels; treatment reduced them; -Reduced MBP expression; treatment increased them. | 3-methyladenine reduces the loss of MBP and inhibits bladder detrusor dysfunction by inhibiting the autophagy response in bladder detrusor muscle cells. The inhibition of collagen fiber expression in the detrusor promotes the recovery of bladder function. | |
| Shimizu et al., 2021 [63] | SCI | Mouse | Female | Complete transection at T8–T9 | Awake cystometry: the number of NVCs was significantly reduced in vibegron-treated SCI mice compared to vehicle-treated control SCI mice. | Increased mRNA levels of TRPV1, TRPA1, ATF3, and iNOS in L6-S1 DRG were increased in SCI mice versus SI mice and decreased after vibegron treatment. | β3-adrenoceptor activation by vibegron improved the SCI-induced storage dysfunction, possibly through the reduction in C-fiber-related receptor expression and inflammation-related markers in DRG. | |
| Gil-Tomee et al., 2019 [64] | PD | Mouse | Both | GM2 synthase knockout (KO) mice | KO mice initially had more void spots that reduced with age. KO mice initially had bladder hyperreflexia and then developed hyporeflexia. | -Increased proNGF protein levels; -Abnormal myelination in bladder nerves. | Loss of TH in the VTA of GM2 KO mice compared to WT mice. | Dopaminergic damage in brain micturition centers impact voiding in association with a loss in mature ganglioside. |
| McMillan et al., 2014 [65] | MS | Mouse | Male | Experimental autoimmune encephalomyelitis (EAE) | Voiding spot assay: increased number of non-voiding contractions; decreased voided volume; shortened intermicturition intervals; decreased bladder capacity; reduced volume of voided urine. | -Upregulation of GFAP expression (gliosis) and decrease in MBP at the lesion site; -Several proinflammatory cytokines were upregulated in the brains at 1 wk, followed by a gradual recovery to baseline values by 4 wk -In the spinal cord, only IFN-γ levels were upregulated at 1 wk, suggestive of a mild inflammatory reaction; normal levels were observed at 4 wk. | Coronavirus-induced demyelination of the CNS causes the development of a neurogenic bladder that is comparable with neurogenic detrusor overactivity observed in patients with multiple sclerosis. | |
| Altuntas et al., 2012 [66] | MS | Mouse | Female | Experimental autoimmune encephalomyelitis (EAE) | -Increase in collagen; -Decrease in NGF, GDNF, muscarinic receptors, and purinergic receptors; -Increased expression of CTGF and TGF-β3 mRNAs (markers of the fibrosis cascade), | EAE-caused neurological disability in mice and contributes to marked bladder remodeling. Although all three components of detrusor smooth muscle, urothelium, and connective tissue contribute to the increased bladder mass, the role of connective tissue is more prominent and potentially detrimental. | ||
| Lee et al., 2019 [67] | MS | Mouse | Male | Coronavirus-induced encephalitis (CIE) | Voiding spot assay: at 10 wks post-inoculation, bladder capacity, the inter-micturition interval, and bladder pressure at voiding in all groups, except for the C-RELAP group, were similar to the respective values in the control group. Mice in the C-RELAP group developed overactive bladder phenotype. This means that the C-RELAP group develop a more severe and long-lasting type of neurogenic bladder overactivity than other groups, providing evidence of some correlation between the type of neurodegenerative changes in the CNS and type of developed voiding dysfunction in CIE mice. | Increased expression of TNF-α, Increased content of IFN-γ, IL-2, TGF-β and TNF-α | Decreased expression of IL-1β and IL-10 in the brain. The C-PRO group was characterized by a decreased expression of IL-1β, IL-6, IL-10, IL-17, and TNF-α. C-RELAP mice had a significantly reduced level of IL-4 in the brain. | Mice with CIE developed three phenotypes of neurologic impairment, mimicking different types of MS. |
| Jin et al., 2017 [68] | MS | Mouse | Unspecified | Experimental autoimmune encephalomyelitis (EAE) | Voiding spot assay: decrease in urine volume voided per micturition and increased frequency of urination; increased bladder diameter; features reverted with treatment. | -Decreased number of ICCs (c-Kit staining); treatment partially reverted this; -Increased expression of Panx1 and Cx43. | The effect of SCF on the loss of ICCs may offer a theoretical option for treating patients with MS-related voiding dysfunction. | |
| Xue et al., 2013 [69] | MS | Mouse | Female | Experimental autoimmune encephalomyelitis (EAE) | -EP3 and EP4 agonists increased micturition frequency and decreased void weight in EAE mice, compared with control mice treated with vehicles. | -The concentration of PGE2 level in the bladder increased as the EAE (severity) score increased; -Bladder weight to total body weight ratio was higher; -The expression of EP3 and EP4 receptors increased as EAE severity score increased, but no change in expression of EP1 and EP2 receptors was verified. | EAE-induced upregulation of EP3 and EP4 receptors in the bladder was accompanied by bladder dysfunction. However, EAE had no significant effect on EP1 and EP2 receptors. | |
| Liang et al., 2016 [70] | Cerebral ischemia | Rat | Female | Middle cerebral artery occlusion (MCAO) | -Increased peak voiding pressure and residual volume at 1 day, 3 days, and 7 days following ischemia induction, which declined after pre- and postischemic CD34+ cells treatment; -Decreased voided volumes and intercontraction intervals decreased after ischemia induction, but increased after pre- and postischemic CD34+ cell treatment at 3 days and 7 days. | NGF, M2, and M3 mRNA expression and immunoreactivity (except for M2) decreased after MCAO, but increased after preischemic CD34+ cell treatment. | Bladder dysfunction caused by MCAO may have a normal micturition restored by treatment with human umbilical cord blood-derived CD34+ cells. This urinary function improvement may be related to the expression of bladder NGF, M2, and M3. | |
| Campeau et al., 2014 [71] | PD | Rat | Female | Injection of 6-hydroxydopamine in the right medial forebrain bundle | Awake cystometry: increased bladder capacity, post-void volume, and threshold pressure; decreased after treatment with rBMSCs; urodynamic effects of the 6-OHDA lesion up to 42 days after injection. | -GFAP expression was present around rBMSC and ErBMSC graft sites, unlike the saline injection site, suggesting activated astrocytes around the graft sites; -There was IBA-1 expression at the injection site in all groups, but it vanished by the fourth week. Microglia infiltration was present around injected rBMSCs and ErBMSCs. | Transplantation of rBMSCs alone improved urodynamic pressure at 42 days after treatment more markedly than ErBMSCs. This improvement in rBMSC rats was associated with a higher number of TH-positive neurons in the treated SNpc, suggesting that functional improvement may require a juxtacrine effect. | |
| Cho et al., 2015 [72] | Intracerebral hemorrhage (ICH) | Rat | Female | Induction of ICH in the hippocampal CA1 region was performed using a stereotaxic frame and collagenase | Cystometry under zolotyl anesthesia: bladder contraction pressure and time were significantly increased and the voiding pressure and time decreased by the induction of ICH, as compared with the control treatment. | -c-Fos expression levels in the neuronal voiding centers (medial preoptic area, ventrolateral gray, pontine micturition center, and SC L4-L5) were increased; -NGF expression levels in the neuronal voiding centers were increased. | ICH-induced NLUTD rat model may be a more appropriate method to analyze NLUTD in stroke patients than a cerebral infarction model. | |
| Pritchard et al., 2017 [73] | PD | Marmoset | Both | MPTP injection | -Reduction in tyrosine hydroxylase expression in the substantia nigra. | The increased neurogenically mediated contractions where no extrinsic innervation exists might be due to long-term adaptive changes locally as a result of the loss of the nigrostriatal output. | ||
| Shen et al., 2013 [74] | Meningomyelocele | Rat | Fetuses from female rats | Gavage feeding of retinoic acid at embryonic day 10 (E10) | Decrease in β-III-Ttubulin- content at E16, E18, and E20. | -Increase in GFAP expression (in the dorsal region of the spinal cord); -Decrease in VAChT expression in the dorsal lateral nucleus of the spinal cord at all fetal ages. | Smooth muscle of the bladder in fetal rats with myelomeningocele is morphologically normal, while the innervation of the smooth muscle of the bladder is markedly decreased centrally and peripherally. Astrocytosis appears in a later embryonic stage, which could be related to nerve repair in the spinal cord. | |
| Tekin et al., 2016 [75] | Myelomeningocele | Rat | Fetuses from pregnant female rats | Gavage feeding of retinoic acid at embryonic day 10 (E10) | -The interstitial cells of Cajal (ICC) score of the MMC group is decreased. | The density of the ICC in the urinary bladder decreased in the neurogenic bladder developed in MMC. | ||
| Liu et al., 2022 [76] | Myelomeningocele | Rat | Fetuses from pregnant rats | Gavage feeding of retinoic acid at embryonic day 10 (E10) | -Inhibition of bladder cells proliferation, due to increased apoptosis in late embryonic stage (increased cleaved caspase 3); -Increase in α-SMA mRNA; -NeuN protein expression increased with time, with no significant difference between the MMC and CRL groups from E16 to E18; however, the expression of NeuN protein was significantly lower in the MMC group than in the CRL group from E20 to E22. | Bladder dysfunction in myelomeningocele fetal rats is related to the inhibition of proliferation, promotion of apoptosis, and reduction in bladder nerve and smooth muscle-related protein synthesis. |
| Molecular Factors | NDO Model | Tissue Layer | Bladder Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change | |
|---|---|---|---|---|---|
| Neurotrophic factors | |||||
| BDNF † [35] | SCI a,c | M | ↑ | ||
| NGF †‡ [29,46,48,56] | SCI c | W †‡ | ↑ | siRNA Intravesical onabotulinumtoxinA | |
| M † | ↑ | Increased number of daily bladder emptyings | |||
| D † | ↑ | Long-term sacral anterior root stimulation | |||
| Apoptosis-related factors | |||||
| GAPDH ‡ [60] | SCI c | W | ↑ | ||
| Receptors | |||||
| M2 receptor †‡ [44,56] | SCI c | M †‡ | ↓ | ||
| D † | ↑ | Long-term sacral anterior root stimulation (detrusor stroma) | |||
| M3 receptor †‡ [33,44,56] | SCI c | M ‡ | ↓ | ||
| D † | ↓ | Long-term sacral anterior root stimulation (detrusor stroma) | |||
| W ‡ | ↓ | M3 RNAi lentivirus | |||
| pTrkA † [29] | SCI c | W | ↑ | ||
| P2X2 †‡ [45] | SCI c | W | ↓ | Posterior tibial nerve stimulation (PTNS) | |
| P2X3 †‡ [45,51,56] | SCI c | W †‡ | ↓ | Posterior tibial nerve stimulation (PTNS) | |
| M† | ↑ | BBG (P2X7R antagonist) Long-term sacral anterior root stimulation | |||
| α1a, α1b, α1d -adrenergic receptors ‡ [60] | SCI c | W | ↓ | ||
| β2-adrenergic receptors † [56] | SCI c | M | ↓ | Long-term sacral anterior root stimulation | |
| Ionic channel proteins | |||||
| HCN channel proteins †‡ [57] | SCI c | W | ↓ | ||
| TRPA-1 †‡ [45] | SCI c | W | ↓ | Posterior tibial nerve stimulation (PTNS) | |
| TRPM-4 † [30] | SCI a | M, D | ↑* | 9-phenanthrol (TRPM-4 antagonist) | |
| TRPV-1 †‡ [26,32,45] | SCI c | W | ↑†c ↓†‡c | Inosine (decreases) Neurotoxin RTX (decreases) Posterior tibial nerve stimulation (PTNS) (increases) | |
| Neuronal markers | |||||
| NF200 † [32,41,42] | SCI c | W | ↓ | Inosine Multisystem neuroprosthetic training program | |
| D | ↓ | ||||
| NPY † [42] | SCI c | W | ↓ | Multisystem neuroprosthetic training program | |
| PGP 9.5 † [42] | SCI c | W | ↓ | Multisystem neuroprosthetic training program | |
| SYP † [32] | SCI c | W | ↓ | Inosine | |
| β-III-tubulin † [36] | SCI c | W | ↑ | ||
| Ischemia- and fibrosis-related molecules | |||||
| FGF-2 ‡ [31] | SCI c | W | ↑ | ||
| FGF-β ‡ [39] | SCI c | W | ↑ | Oxybutynin (anti-cholinergic agent) | |
| HIF-1α ‡ [31,39] | SCI c | W | ↑ | Vibegron and mirabegron (β3-adrenoceptor agonists) Oxybutynin (anti-cholinergic agent) | |
| TGF-β1 †‡ [31,34,39] | SCI c | W | ↑ | Vibegron and mirabegron (β3-adrenoceptor agonists) Oxybutynin (anti-cholinergic agent) BoNTA injection | |
| VEGF-α ‡ [31] | SCI c | W | ↑ | ||
| Other molecules | |||||
| Filamin A † [57] | SCI c | W | ↓ | ||
| Nedd4-2 † [57] | SCI c | W | ↑ | ||
| NRSF † [57] | SCI c | W | ↑ | ||
| pAKT † [29] | SCI c | W | ↑ | ||
| Trip8b † [57] | SCI c | W | ↑ | ||
| Molecular Factors | NDO Model | Site | Bladder Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change | |
| Neurotrophic factors | |||||
| GDNF ‡ [66] | MS | W | ↓ | ||
| NGF ‡ [66] | MS | W | ↓ | ||
| Inflammatory mediators | |||||
| IFN-γ † [67] | MS | W | ↑ | ||
| IL-2 † [67] | MS | W | ↑ | ||
| TNF-α † [67] | MS | W | ↑ | ||
| Receptors | |||||
| c-kit † [68] | MS | W | ↓ | Stem cell factor cytokine injection | |
| EP-3 and EP-4 † [69] | MS | W | ↑ | ||
| M3 receptor ‡ [66] | MS | W | ↓ | ||
| P2X1 ‡ [66] | MS | W | ↓ | ||
| Ionic channel proteins | |||||
| Panx 1 † [68] | MS | W | ↑ | Stem cell factor cytokine injection | |
| Ischemia- and fibrosis-related molecules | |||||
| CTGF ‡ [66] | MS | W | ↑ | ||
| TGF-β1 † [67] | MS | W | ↑ | ||
| TGF-β3 ‡ [66] | MS | W | ↑ | ||
| Other molecules | |||||
| Cx 43 † [68] | MS | W | ↑ | Stem cell factor cytokine injection | |
| Molecular Factors | NDO Model | Site | Bladder Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change | |
| Neurotrophic factors | |||||
| NGF †‡ [70] | CI | W | ↓ | Treatment with human umbilical cord blood-derived CD34+ cells | |
| Receptors | |||||
| M2 receptor †‡ [70] | CI | W | ↓‡ ↑† | Treatment with human umbilical cord blood-derived CD34+ cells | |
| M3 receptor †‡ [70] | CI | W | ↓ | Treatment with human umbilical cord blood-derived CD34+ cells | |
| Molecular Factors | NDO Model | Site | Bladder Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change | |
| Neurotrophic factors | |||||
| Pro-NGF † [64] | PD | W | ↑ | ||
| Molecular Factors | NDO Model | Site | Bladder Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change | |
| Apoptosis-related factors | |||||
| Caspase-3 † [76] | MMC | M, D | ↑ | ||
| Neuronal markers | |||||
| NeuN † [76] | MMC | W (E20–22) | ↓ | ||
| β-III-tubulin † [74] | MMC | D | ↓ | ||
| Molecular Factors | NDO Model | Location within the Nervous System | Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change |
|---|---|---|---|---|
| Neurotrophic factors | ||||
| BDNF † [27,61] | SCI a,c | Lumbar spinal cord a,c | ↑ | |
| Spinal injury level c | ↑ | Treatment with a PTEN inhibitor (TGN) | ||
| NGF †• [48,53,57,61] | SCI c | T4 DRG † | ↑ | |
| Neuronal voiding centers • | ↑ | Transplantation of oral mucosa stem cells Tamsolusin | ||
| Spinal injury site † | ↑ | Treatment with a PTEN inhibitor (TGN) | ||
| Inflammatory mediators | ||||
| PGE2 † [38] | SCI c | Lumbosacral spinal cord | ↑ | |
| Apoptosis-related factors | ||||
| Caspase-3 † [54] | SCI c | Spinal injury level | ↑ | Placental mesenchymal stem cell transplantation |
| Receptors | ||||
| CSPG-R ‡ [28] | SCI c | L5-S1 DRG | ↓ | |
| EP-1 ‡ [38] | SCI c | Lumbosacral spinal cord | ↑ | |
| MAI-R ‡ [28] | SCI c | L5-S1 DRG | ↓ | |
| P2X2 †‡ [45,46] | SCI c | L6-S1 DRG | ↑ ‡ ↓ †‡ | Increased number of daily bladder emptyings (decreases) Posterior tibial nerve stimulation (PTNS) (increases) |
| P2X3 †‡ [45,46] | SCI c | L6-S1 DRG | ↑ c ‡ ↓ c †‡ | Increased number of daily bladder emptyings (decreases) Posterior tibial nerve stimulation (PTNS) (increases) |
| Ionic channel proteins | ||||
| ASIC1 ‡ [35] | SCI a,c | L6-S1 DRG | ↑ | |
| ASIC2 ‡ [35] | SCI a,c | L6-S1 DRG | ↑ * | |
| ASIC3 ‡ [35] | SCI c | L6-S1 DRG | ↑ * | |
| Kv1.4 α-subunit ‡ [50] | SCI c | L6 DRG bladder afferent neurons | ↓ | |
| Piezo2 ‡ [35] | SCI c | L6-S1 DRG | ↑ | |
| TRPA-1 †‡ [45,46,63] | SCI c | L6-S1 DRGs | ↑ c ‡ ↓ c †‡ | Increased number of daily bladder emptyings (decreases) Vibegron (decreases) Posterior tibial nerve stimulation (PTNS) (increases) |
| TRPV-1 †‡• [35,45,46,49,63] | SCI a,c | L1, L6-S1 DRG †‡• a,c | ↑ a,c ‡• ↓ c †‡ | Increased number of daily bladder emptyings (decreases) Vibegron (decreases) Posterior tibial nerve stimulation (PTNS) (increases) |
| L6 DRG bladder afferent neurons c ‡ | ↑ | |||
| Neuronal markers | ||||
| 5-HT † [47] | SCI a,c | Lumbosacral spinal cord (lamina X and ventral horn) | ↓ | |
| CGRP †‡• [26,43,47,49] | SCI c | Lumbosacral spinal cord (Dorsal horn) † | ↑ | |
| L1 and L6 DRG • | ↑ | Sacral neuromodulation | ||
| L6 DRG bladder afferent neurons ‡ | ↑ | |||
| CRF † [40,47] | SCI a,c | Lumbosacral spinal cord (lamina X and intermediolateral column) | ↓ | Anti-Nogo-A antibody |
| GAD2 †‡ [40,47] | SCI c | Lumbosacral spinal cord | ↓ | Anti-Nogo-A antibody |
| NF200 • [49] | SCI c | L6 DRG | ↓ | |
| VGLUT-2 ‡ [47] | SCI c | Lumbosacral spinal cord (laminae I-III) | ↓ | |
| Ischemia and fibrosis-related molecules | ||||
| Neurocan † [28] | SCI a | Lumbosacral spinal cord | ↑ * | |
| Phosphacan † [28] | SCI a | Lumbosacral spinal cord | ↑ * | |
| VEGF-α † [61] | SCI c | Spinal injury level | ↑ | Treatment with a PTEN inhibitor (TGN) |
| Myelin-associated proteins | ||||
| MAG † [28] | SCI a | Lumbosacral spinal cord | ↑ * | |
| MBP † [62] | SCI a,c | Undefined (long spinal cord segment) | ↓ | 3-methyladenine |
| Nogo-A † [28] | SCI a | Lumbosacral spinal cord | ↑ * | |
| OMgp † [28] | SCI a | Lumbosacral spinal cord | ↑ * | |
| RGMa † [28] | SCI a | Lumbosacral spinal cord | ↑ * | |
| Other molecules | ||||
| ATF3 ‡ [63] | SCI c | L6-S1 DRG | ↑ | Vibegron |
| c-Fos • [53,57,58] | SCI c | Neuronal voiding centers | ↑ | Transplantation of oral mucosa stem cells Tamsolusin |
| Low lumbar spinal cord (dorsal horn) | ↑ | Tamsolusin | ||
| GAP-43 † [26,27] | SCI a,c | Lumbosacral spinal cord a,c | ↑ | |
| L5-S1 DRG a | ↑ * | |||
| GFAP † [37] | SCI c | Spinal injury level | ↑ | |
| iNOS ‡ [63] | SCI c | L6-S1 DRG | ↑ | Vibegron |
| LC3-II † [62] | SCI a,c | Undefined (long spinal cord segment) | ↑ | 3-methyladenine |
| NADPH-d • [58] | SCI c | Low lumbar spinal cord (dorsal horn) | ↑ | Tamsolusin |
| Neuronal voiding centers | ↑ | |||
| pJNK † [27] | SCI c | Lumbar spinal cord | ↑ | |
| S100 † [41] | SCI c | Spinal injury level | ↑ | |
| Molecular Factors | NDO Model | Location within the Nervous System | Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change |
| Inflammatory mediators | ||||
| IFN-γ † [65] | MS | Brain | ↑ (1 w) * | |
| Spinal cord | ↑ (1 w) * | |||
| IL-1β † [67] | MS | Brain | ↓ (10 w) | |
| IL-4 † [67] | MS | Brain | ↓ (10 w) | |
| IL-5 † [65] | MS | Brain | ↑ (1 w) * | |
| IL-6 † [65,67] | MS | Brain | ↑ (1 w) * ↓ (10 w) | |
| IL-10 † [67] | MS | Brain | ↓ (10 w) | |
| IL-17 † [65,67] | MS | Brain | ↑ (1 w) * ↓ (10 w) | |
| TNF-α † [65,67] | MS | Brain | ↑ (1 w) * ↓ (10 w) | |
| Myelin-associated proteins | ||||
| MBP † [65] | MS | Spinal lesion sites | ↓ | |
| Other molecules | ||||
| GFAP † [65] | MS | Spinal lesion sites | ↑ | |
| Molecular Factors | NDO Model | Location within the Nervous System | Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change |
| Neurotrophic factors | ||||
| NGF • [72] | ICH | Neuronal voiding centers | ↑ | |
| Neuronal markers | ||||
| TH • [64,73] | PD | Substancia nigra | ↓ | |
| Ventral tegmental area | ↓ | |||
| Molecular Factors | NDO Model | Location within the Nervous System | Expression after NDO Induction | Treatments That Reverted or Attenuated NDO-Related Expression Change |
| Neuronal markers | ||||
| VAChT † [74] | MMC | Dorsal lateral nucleus of the spinal cord | ↓ | |
| Other molecules | ||||
| GFAP † [74] | MMC | Lumbosacral spinal cord (only E20) | ↑ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira, A.; Nascimento, D.; Cruz, C.D. Molecular Mechanism Operating in Animal Models of Neurogenic Detrusor Overactivity: A Systematic Review Focusing on Bladder Dysfunction of Neurogenic Origin. Int. J. Mol. Sci. 2023, 24, 3273. https://doi.org/10.3390/ijms24043273
Ferreira A, Nascimento D, Cruz CD. Molecular Mechanism Operating in Animal Models of Neurogenic Detrusor Overactivity: A Systematic Review Focusing on Bladder Dysfunction of Neurogenic Origin. International Journal of Molecular Sciences. 2023; 24(4):3273. https://doi.org/10.3390/ijms24043273
Chicago/Turabian StyleFerreira, Ana, Diogo Nascimento, and Célia Duarte Cruz. 2023. "Molecular Mechanism Operating in Animal Models of Neurogenic Detrusor Overactivity: A Systematic Review Focusing on Bladder Dysfunction of Neurogenic Origin" International Journal of Molecular Sciences 24, no. 4: 3273. https://doi.org/10.3390/ijms24043273
APA StyleFerreira, A., Nascimento, D., & Cruz, C. D. (2023). Molecular Mechanism Operating in Animal Models of Neurogenic Detrusor Overactivity: A Systematic Review Focusing on Bladder Dysfunction of Neurogenic Origin. International Journal of Molecular Sciences, 24(4), 3273. https://doi.org/10.3390/ijms24043273






