Abstract
Pancreatic cancer is an aggressive malignancy with high mortality rates and poor prognoses. Despite rapid progress in the diagnosis and treatment of pancreatic cancer, the efficacy of current therapeutic strategies remains limited. Hence, better alternative therapeutic options for treating pancreatic cancer need to be urgently explored. Mesenchymal stromal cells (MSCs) have recently received much attention as a potential therapy for pancreatic cancer owing to their tumor-homing properties. However, the specific antitumor effect of MSCs is still controversial. To this end, we aimed to focus on the potential anti-cancer treatment prospects of the MSC-based approach and summarize current challenges in the clinical application of MSCs to treat pancreatic cancer.
1. Introduction
Pancreatic cancer, an aggressive human malignant tumor, is often termed a silent killer owing to its poor prognosis, and its incidence has been increasing over the years [1,2,3]. The mortality rate within one year after diagnosis is approximately 75%, and the 5-year survival rate is no more than 8% [4,5,6]. Pancreatic ductal adenocarcinoma (PDAC) accounts for 90% of all pancreatic tumors, and other subtypes include acinar carcinoma, pancreatoblastoma, and neuroendocrine neoplasms [3]. Approximately 50% of patients with PDAC display no symptoms during the early stage, and by the time a diagnosis is confirmed, they are in the late stage of PDAC [3,7,8]. Thus, most patients miss opportunities for radical surgical resection in the early stage and can only undergo radiotherapy and chemotherapy later. However, owing to the special extracellular matrix barrier of pancreatic cancer and resistance to chemotherapeutic drugs, some cancer cells cannot be killed [9,10]. Furthermore, approximately 40% of patients with PDAC experience tumor recurrence even after surgical resection and die within one year [11,12,13]. Despite the rapid progress in the diagnosis and therapy of pancreatic cancer, the efficacy of present therapeutic measures remains poor [7]. Therefore, identifying alternative treatment strategies for the better management of pancreatic cancer is an urgent requirement.
As a carrier of anti-tumor drugs, mesenchymal stromal cells (MSCs) can be genetically engineered to release various agents such as treatment proteins, suicide genes, and oncolytic viruses to decrease cancer growth and progression [14,15]. The application of MSCs as therapeutic biological carriers in cytotherapy has some distinct advantages, including low immunogenicity, tumor tropism, a massive expansion in vitro, and the ability to transfer various therapeutic agents [16,17,18,19]. Reportedly, MSCs can home to tumor locations and survive in the tumor microenvironment (TME) [16,20,21]. Recent research has indicated that MSCs could be used as a promising “weapon” in treating pancreatic cancer [22,23,24].
Despite the therapeutic potential of MSCs in several diseases, their applications in the treatment of cancer are still controversial. Although MSCs have been found to promote tumor initiation and progression, emerging research has indicated the beneficial effects of MSCs in cancer therapy [17,25,26,27]. In this review, we aimed to focus on the potential anti-cancer treatment prospects of the MSC-based approach and summarize current challenges in the clinical application of MSCs for treating pancreatic cancer.
2. Treatments and Challenges of Pancreatic Cancer
Based on the extent of the tumor, patients are often divided into four categories, namely those with resectable, borderline resectable, locally advanced, and metastatic tumors. Although the 5-year survival rate of patients who can undergo surgical resection is 10–25%, surgery remains the only curative intervention [7,28,29]. Adjuvant chemotherapy, namely the modified FOLFIRINOX (fluorouracil, oxaliplatin, irinotecan, leucovorin) and gemcitabine plus capecitabine or gemcitabine alone, is recommended after PDAC resection for patients with high and poor functional status, respectively [3]. Additionally, neoadjuvant and perioperative treatments are recommended for resectable and borderline resectable tumors. Eradication of occult metastatic disease could increase the number of patients eligible for systematic treatment. Despite the controversial role of radiotherapy in localized PDAC, the present guidelines support neoadjuvant chemotherapy with or without radiotherapy for local diseases as a therapeutic intervention [3,30,31]. In approximately 80% of inoperable locally advanced PDAC cases, poor efficacy has been observed for new adjuvant therapy; therefore, the surgical resection rate cannot be increased. The modified FOLFIRINOX or albumin-bound paclitaxel and gemcitabine are used to slow down tumor progression [3,7,32]. Furthermore, the role of radiation in locally advanced PDAC is still controversial. About 50% of patients have distant metastasis at the time of diagnosis, and systemic chemotherapy continues to be the primary intervention for alleviating cancer-related symptoms and prolonging life [7]. Currently, gemcitabine and albumin-bound paclitaxel or modified FOLFIRINOX is still the standard first-line therapy for metastatic patients [3,7,33,34].
Based on current studies, the failure of chemotherapy, targeted therapy, and immunotherapy for pancreatic cancer may be attributed to the special characteristics of pancreatic cancer, including high malnutrition, immunosuppression, hypoxia, and desmoplastic characteristics [35]. Pancreatic tumor cells are surrounded by an abundant desmoplastic stroma that forms the TME and is composed of fibroblasts, pancreatic stellate cells (PSCs), MSCs, immune cells, blood vessels, and extracellular matrix proteins [36]. This abundant stroma is a physical barrier that hinders the effective delivery of chemotherapies to tumors. Furthermore, the specific TME plays key roles in tumor biology and modulates the immune recognition of pancreatic cancer cells [37,38].
The failure of conventional chemotherapy is due to chemotherapy resistance and abnormally abundant extracellular matrix [39,40]. Therapies targeting programmed death 1 or programmed death 1 ligand 1 (PD-1/PD-L1) have been rapidly developed as antitumor therapy for several cancers [41]. However, the desmoplastic TME aids the cancer cells in escaping the immune checkpoints (PD-1/PD-L1) and promotes the growth and metastasis of pancreatic cancer. Thus, current anti-PD-1/PD-L1 immunotherapy has a poor therapeutic effect on pancreatic cancer [4,42,43]. Chimeric antigen receptor (CAR)-modified T-cell therapy is being rapidly developed for various cancers; however, it has been unsuccessful in displaying a potential clinical value and improving survival in pancreatic cancer [44,45]. Owing to the physical and environmental barriers in pancreatic cancer-specific TME, the infiltration of CAR-modified T cells is limited [45], as well as emerging exhaustion and missing persistence.
Hence, to overcome the pathophysiological barrier of pancreatic cancer, several MSC-based therapy strategies have been proposed.
3. Tumor-Homing Properties of MSCs
MSCs are adult stem cells capable of multilineage differentiation and self-renewal [46,47]. MSCs exist in most tissues and are usually extracted from various sources, including bone marrow, umbilical cord, menstrual blood, placenta, adipose tissues, and muscles [19,48,49,50]. To date, MSCs have been shown to treat multiple diseases owing to their immunomodulatory and anti-inflammatory effects and tissue repair ability [18,51,52]. They thus have excellent application prospects in regenerative medicine.
MSCs can accurately migrate to injured tissues and organs and play a key role in inhibiting inflammation, decreasing tissue fibrosis formation, and promoting regeneration, thereby indicating that MSCs can selectively migrate to certain sites in the body [53,54]. Moreover, MSCs have been found to selectively migrate to primary and metastatic tumor locations, thus revealing the tumor-homing capacity of MSCs [16,20,21,55,56,57,58,59]. However, despite reports that MSCs could migrate to tumor locations in various types of tumors, the potential mechanisms by which MSCs home to tumors are still unclear.
MSCs express various chemokines and cell adhesion molecules that coordinate the mobilization of MSCs to the damage locations [15,60,61,62,63,64]. Recent research has found that the tumor-homing capacity of MSCs could be regulated by the cooperation of cytokines, chemokines, and adhesion molecules [15,24,65,66,67,68]. Hence, this observation indicates that the homing capabilities of MSCs could depend on the inflammatory microenvironment of the tumor.
MSCs are involved in the initiation, development, progression, and metastasis of tumors [69]. They can directly affect tumor development through crosstalk with tumors or the release of soluble molecules [14]. Although MSCs are indicated to exhibit pro-tumor effects [70], they can also inhibit the growth of tumors by various mechanisms, such as inhibiting tumor cell proliferation and promoting tumor cell death [71]. Furthermore, owing to their tumor-homing properties, MSCs and their exosomes have been considered promising tools for the accurate and selective release of antitumor molecules, RNA, or anticancer drugs that aid in reducing tumor cell viability and invasive characteristics [16,17,72,73,74]. Therefore, MSCs may serve as a potential tumor-targeted therapeutic strategy.
On infusing MSCs into rats, MSCs could home to pancreatic cancer sites to exert their anticancer effects [57,58]. However, the mechanism by which MSCs crosstalk with tumor cells has not yet been elucidated, and consequently, translational medicine progress has been limited. Thus, the underlying molecular mechanism by which MSCs crosstalk with tumors needs further exploration; this will aid in improving the effectiveness of MSC therapeutic potential.
4. MSC Therapy for Pancreatic Cancer
4.1. Native MSCs
Naïve MSCs have some potential advantages for treatment, such as abundance, low immunogenicity, and ease of isolation and in vitro expansion. Hence, it is widely applied to various diseases including cancer. Cousin et al. found that native human adipose tissue-derived mesenchymal stromal cells (AD-MSCs) inhibit pancreatic cancer cell proliferation and promote tumor cell death by inhibiting the cell cycle at the G1 phase [75]. Doi et al. observed that native rat umbilical cord matrix-derived stem cells (UCMSCs) decrease the growth of pancreatic tumors in mouse peritoneal models and increase the overall survival time of mice [76]. Furthermore, native human amniotic MSCs inhibit the proliferation of pancreatic cancer cells and promote apoptosis of pancreatic cancer cells by inhibiting the expression of EGFR, c-Src, and SGK223 [77]. However, although native MSCs can inhibit the growth and angiogenesis in various tumor cells, they might act as a double-edged sword while cross-talking and interacting with tumor cells [78]. Thus, the effectiveness of MSCs in decreasing the growth of pancreatic cancer needs further exploration.
4.2. Genetically Engineered MSCs
Genetically modified MSCs are promising potential cancer therapies to further enhance the efficacy of MSCs to target tumor cells. These MSCs deliver anti-proliferative, pro-apoptotic, and anti-angiogenic molecules to target tumor cells [70,79]. These effects might depend on several mechanisms: MSCs preferentially migrate to locations of inflammation, ischemia, and malignancy; genetically modified MSCs only release therapeutic gene products in the special TME; transgenes encoding biologic agents might themselves exhibit targeted and differential effects in tumor cells [80]. Previous studies have shown that selective targeting of therapeutic gene expression by MSCs is feasible and effective in the treatment of various cancers [81,82,83]. For example, MSCs were genetically modified to express gene products, including IFNs, CX3CL1, FLT3, tumor necrosis factor α-related apoptosis-inducing ligand (TRAIL), HGF, and GDEPT, with direct anti-tumor activity in various cancers, such as melanoma, glioma, and breast, lung, and prostate cancers [74,80,84]. This “Trojan horse” that combines MSCs with gene therapy represents a new therapeutic strategy for targeting and treating cancers.
TRAIL is a therapeutic protein that induces tumor cell death; however, pancreatic cancer cells present intrinsic resistance toward TRAIL by the expression of anti-apoptotic proteins like the X-linked inhibitor of apoptosis protein (XIAP) [85,86]. Inhibiting XIAP could promote TRAIL-induced apoptosis of pancreatic cancer cells [87,88]. Mohr et al. found that the TRAIL-modified mouse bone marrow MSCs (BM-MSCs) deliver soluble TRAIL that suppresses the metastatic growth of pancreatic cancers [89]. Moreover, TRAIL-transfected pancreas-derived MSCs can promote pancreatic cancer cell death [90]. Recently, Spano et al. observed that human AD-MSCs can be modified to efficiently release soluble TRAIL, inducing pancreatic cancer cell death and inhibiting the growth of PDAC [91]. Furthermore, by using photochemical internalization for enhanced transfection efficiency of secreting TRAIL from MSCs, the pancreatic tumor-homing properties of MSCs were enhanced [58]. This finding may provide a potential therapeutic strategy in pancreatic cancer gene therapy and clinical applications.
Zischek et al. found that the suicide gene herpes simplex virus thymidine kinase (HSV-TK)-engineered mouse MSCs can decrease the growth and metastasis of primary pancreatic cancer [92]. Sun et al. showed that NK4-modified rat BM-MSCs can inhibit the proliferation and migration of pancreatic cancer cells [93]. Schug et al. found that NIS-modified MSCs combined with 131I application can inhibit the growth of pancreatic cancer cells [94]. Notably, in a pancreatic cancer model, Tie2/TK-engineered MSCs can significantly decrease primary tumor growth [95]. Moreover, IFN-β-engineered BM-MSCs can selectively home to locations of primary and metastatic pancreatic cancers, regulating TME and reducing the growth of pancreatic cancer [96]. IL-15-engineered UCMSCs can specifically home to pancreatic cancer sites, and a sufficient amount of UCMSC-IL15 has been observed to survive to release IL-15, which could significantly suppress the growth of pancreatic cancer [97]. Furthermore, IL-10-engineered BM-MSCs can decrease the growth of pancreatic cancer by reducing the expression of IL-6 and TNF-a and inhibiting tumor angiogenesis [98].
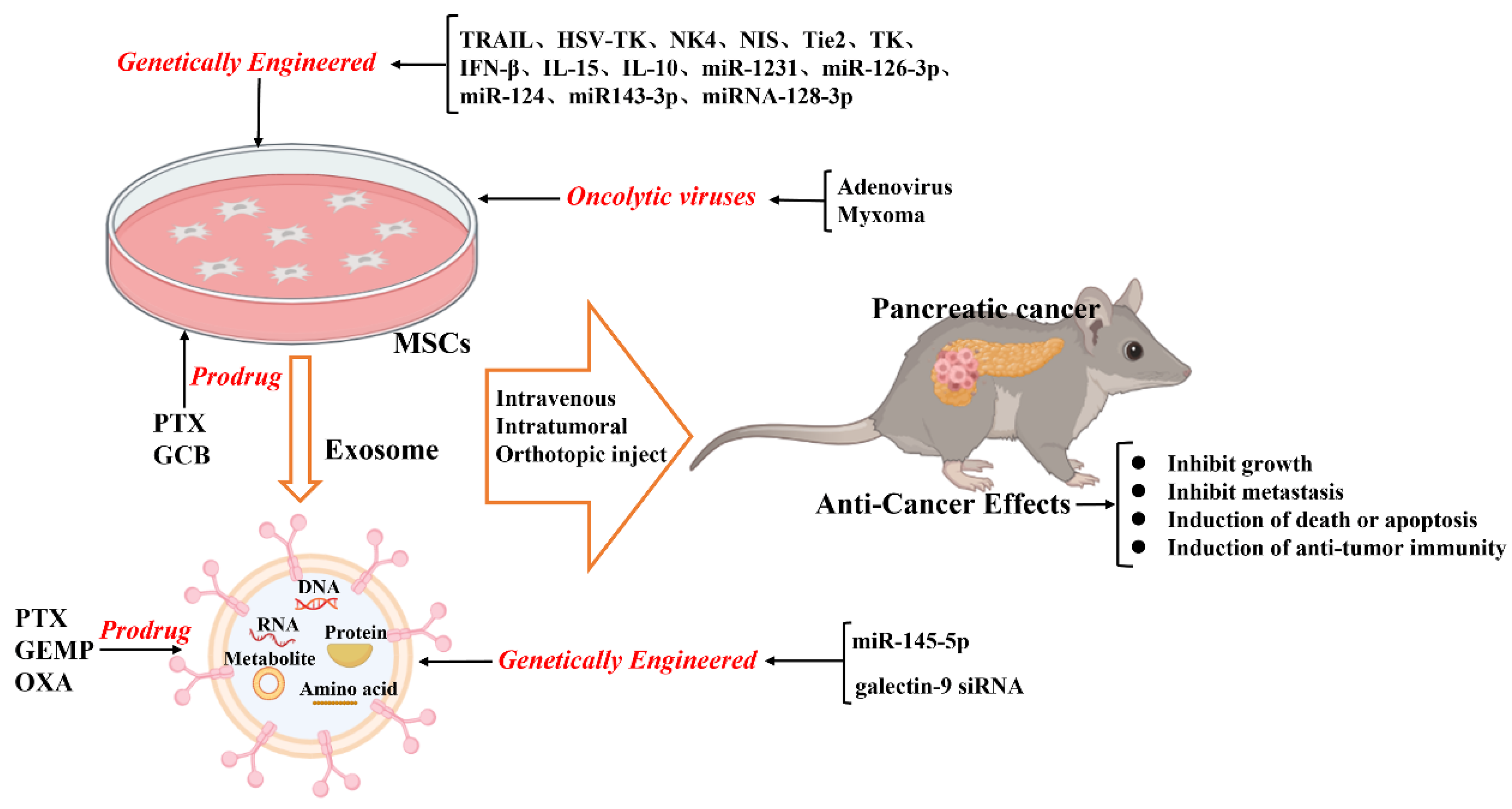
In summary, combining MSCs with selective gene treatment results in enhanced therapeutic effects on inhibiting tumor growth; this might aid in developing new tools for pancreatic cancer treatment (Figure 1).
Figure 1.
Schematic illustration of the current anticancer treatment based on mesenchymal stromal cells (MSCs) and MSC-derived exosomes.
4.3. Exosomes as a Vehicle for Therapy Delivery
Thus far, numerous studies have found that MSCs can secrete extracellular vesicles), including microvesicles (100–2000 nm in diameter) and exosomes (30–150 nm in diameter), which act as paracrine mediators between MSCs and target cells [99,100,101]. Exosomes can deliver cargo (nucleic acids, proteins, lipids, amino acids, and metabolites) from the originating cells to the target cells [101,102,103]. Compared with those of artificial nanocarriers, exosomes, as natural vesicles secreted by cells, have double lipid membranes, better biocompatibility, lower immunogenicity, stronger targeting specificity, deeper tissue permeability, and longer circulating half-life [101,104,105,106,107]. Based on these advantages, exosomes have been applied for engineering functional cargo loads, such as packaged nucleic acid, functional proteins, and other therapeutic molecules into exosomes [100,101,108,109,110]. MSC-derived exosomes have been recently transfected with functional RNAs to target cells, suggesting their potential as an alternative for cell-based therapy.
Notably, exosomes have been shown to transfer microRNAs (miRNAs) to target cancer cell proliferation, differentiation, and metastasis [109,111,112,113,114]. For example, miRNA-100 carried by MSC-derived exosomes suppress tumor angiogenesis and breast cancer progression via the mTOR/HIF1A/VEGF pathway [115]. Additionally, Li et al. showed that engineered exosomes from UCMSCs enriched with miR-302a significantly inhibit endometrial cancer cell proliferation and migration by decreasing cyclin D1 expression and inhibiting the AKT pathway [116]. Furthermore, modified miR-199a derived from AD-MSC exosomes can improve hepatocellular carcinoma (HCC) chemosensitivity through the mTOR signaling pathway [117]. Therefore, these observations suggest that exogenous miRNA delivered by MSC-derived exosomes could be an effective anticancer therapy strategy.
On modifying the normal fibroblast-like mesenchymal cell-derived exosomes to deliver short interfering RNA or short hairpin RNA to target oncogenic KrasG12D, tumor growth was found to be decreased in multiple mouse models of pancreatic cancer, thereby increasing the overall survival [118]. This study offers insight into the target therapeutic potential of exosomes in pancreatic cancer. Furthermore, infusing the exosomes derived from miRNA-engineered MSCs, which contain abundant MSC-sourced anti-tumorigenic miRNAs, can represent a potentially new therapeutic measure for pancreatic cancer. For example, the exosomes extracted from miR-1231-modified BM-MSCs with high levels of miR-1231 reduce the proliferation of pancreatic cancer cells [119]. Overexpressed miR-126-3p derived from BM-MSC exosomes inhibit the proliferation, invasion, and metastasis of pancreatic tumor cells and induce their apoptosis in vitro and in vivo by inhibiting the expression of ADAM9 [120]. Exosomes derived from miRNA-MSCs release miR-124 and miR143-3p in pancreatic tumor cells, inhibiting the proliferation of tumor cells [121,122]. The exosomes derived from miRNA-128-3p-modified UCMSCs can inhibit the proliferation, invasion, and migration of pancreatic cancer cells via the miRNA-128-3p/Galectin-3 axis [123]. Yao et al. found that BM-MSC-derived exosomes reduce the expression of miR-338-5p in pancreatic cancer cells via circ_0030167 and targeting WIF1, thereby inhibiting the Wnt8/β-catenin signaling pathway [124]. Notably, in a recent study, the exosomes were applied for cargo loading miR-145-5p. Exosomes derived from UCMSCs modified with an intra-tumor injection of miR-145-5p, which deliver exogenous miR-145-5p, decrease the growth of pancreatic tumors by inhibiting the expression of SMAD3 [125]. This study revealed a novel insight that exosomes might be an attractive therapeutic tool for the clinical administration of miRNAs in patients with PDAC. Taken together, exogenous functional RNAs released by exosomes derived from MSCs may serve as potential targets for treating pancreatic cancer (Figure 1).
4.4. MSC-Mediated Drug Delivery
MSCs can incorporate chemotherapeutic drugs in vitro, subsequently releasing the effective concentration of drugs in their conditioned medium to exert therapeutic effects [126,127,128]. Furthermore, tumor-homing properties of MSCs allow them to precisely deliver the drug to the tumor location; this has been widely studied as a targeted delivery agent of anti-cancer drugs [27,78,129]. For example, paclitaxel (PTX)-loaded MSCs inhibit the growth of leukemia cells, decrease angiogenesis, and increase survival [130]. Moreover, PTX-loaded MSCs inhibit the proliferation of human myeloma cells [131].
The proliferation of stromal fibroblasts and the deposition of extracellular matrix, which are the defining characteristics of PDAC, lead to a fibrotic state known as desmoplastic or reactive stroma [45,132]. Therefore, this could make it difficult to acquire an effective drug concentration by the common route of administration. Notably, after the MSCs were preconditioned to high doses of PTX, they intracellularly accumulate the drug and then release it, thereby inhibiting pancreatic tumor cell proliferation [133]. Brini et al. demonstrated that PTX-loaded gingival interdental papilla MSCs can release a sufficient amount of PTX to inhibit the proliferation of pancreatic tumor cells [134]. Moreover, gemcitabine (GCB)-loaded BM-MSCs decrease the proliferation of human pancreatic cancer cells in vitro [135]. Nevertheless, PTX and GCB have not yet been shown to be delivered in the PDAC location by MSCs. Thus, MSC-mediated delivery of anti-cancer drugs needs to be further explored in vivo.
Exosomes can be loaded with therapeutic drugs and then used to release them into the target cells [136,137]. The methods applied for directly loading drugs inside exosomes include incubation, electroporation, sonication, extrusion, freeze-thaw cycles, and saponin application. Presently, the most commonly applied methods are incubation and electroporation [114,137]. As drug carriers, exosomes are widely studied as therapeutic agents and can potentially be clinically applied. Recently, GEMP- and PTX-loaded exosomes revealed superiorities in homing and penetrating abilities that aided in inhibiting the growth of pancreatic tumors in vivo [138]. Additionally, Zhou et al. found that BM-MSC-derived exosomes containing electroporation-loaded galectin-9 siRNA and modified with oxaliplatin (OXA) increase drug accumulation in the tumor location and reduce the growth of pancreatic tumors [139]. Thus, MSC-derived exosomes could act as a potential nanoscale drug delivery platform for treating pancreatic cancer (Figure 1).
4.5. Delivery of Oncolytic Viruses
The oncolytic virus has revealed promising results in the treatment of several cancers in various clinical trials [140,141,142]. It can directly cause oncolysis and spread to adjacent tumor cells to activate an anti-cancer immune response. Oncolytic viruses can replicate and selectively target tumor cells, but they cannot bind or effectively replicate in most normal cells. MSCs have been shown to protect viruses from immune clearance through a unique cell carrier tool before delivering them to metastatic tumor sites [143,144,145]. Although the tumor-homing ability of MSCs makes them a promising candidate for systemically delivering oncolytic viruses to tumor location, infection and particle production by MSCs remain areas of concern. The viruses genetically modified for improved delivery by MSCs are aimed at enhancing oncolysis and improving virus production in tumor cells [146].
Kaczorowski et al. showed that oncolytic adenovirus-TRAIL-modified BM-MSCs can precisely migrate to tumor sites, but not in normal cells, inhibiting the growth of pancreatic cancer [147]. Na et al. found that oncolytic adenovirus-RLX-PCDP-loaded BM-MSC carrier can be released to target pancreatic tumors and induce effective viral replication and relaxin expression, which inhibit the growth of pancreatic cancer [148]. Additionally, myxoma-TNFSF14-loaded AD-MSCs can home to pancreatic cancer sites; oncolytic viruses are efficiently delivered, inhibit the growth of PDAC, and increase overall survival [57]. Altogether, oncolytic virus-mediated gene treatment is a promising approach to treating pancreatic cancer (Figure 1). However, some drawbacks of using a virus as a vector for clinical therapy, including packaged space limitation, increased risk of insertional mutagenesis, immune clearance, and limitations of producing high titer virus for clinical application, need to be overcome.
5. Challenges of MSCs in Treating Pancreatic Cancer
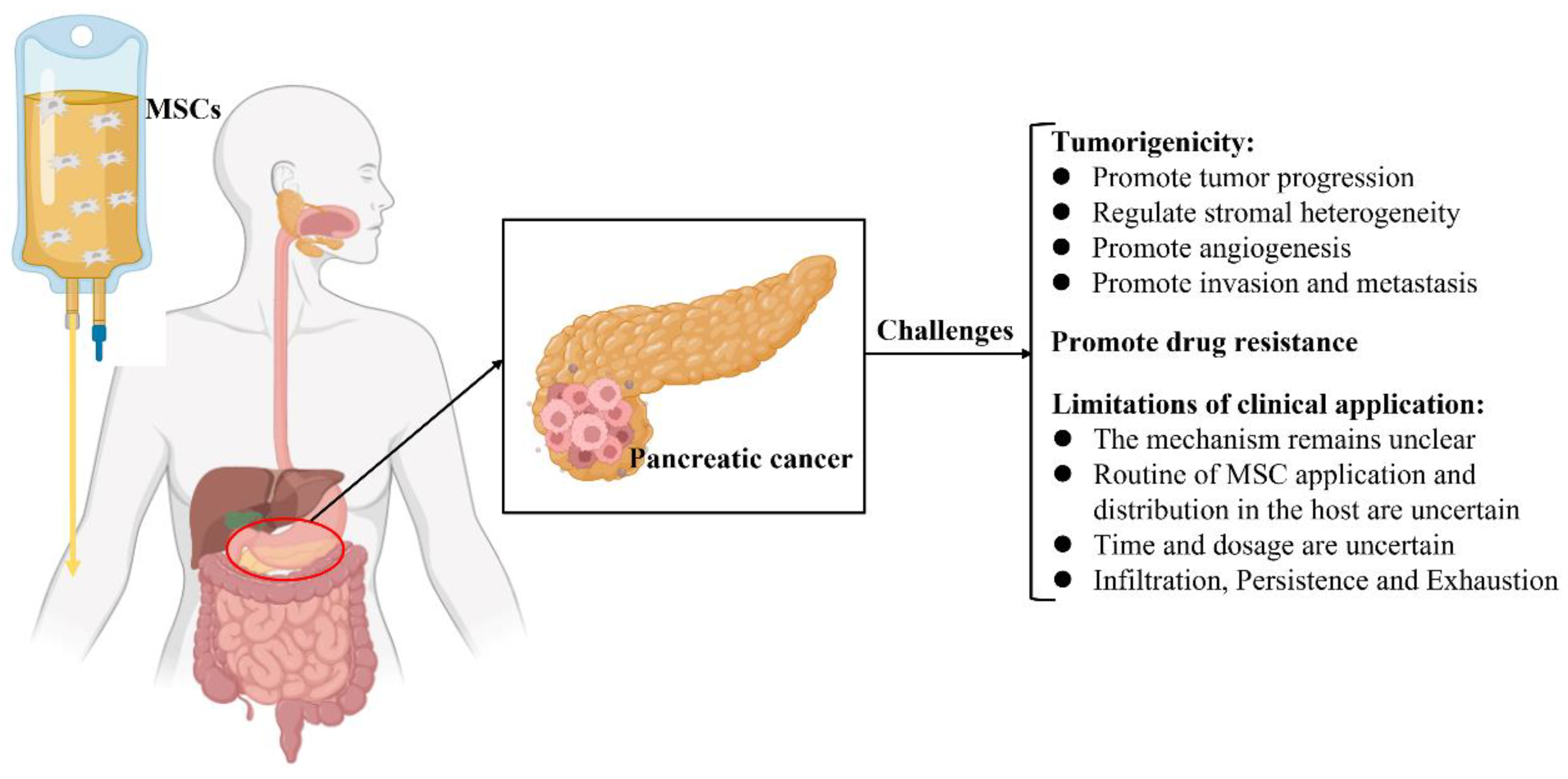
MSCs have been used as a therapeutic intervention for tumors; nevertheless, they are reportedly involved in tumor progression, including tumorigenesis, tumor growth, metastasis, and regulation of the TME [23,113]. Furthermore, the potential mechanisms by which MSCs crosstalk with tumor cells in the TME have not yet been elucidated [22,23,24,149]. Hence, the clinical application of MSCs in the treatment of pancreatic cancer remains controversial and challenging (Figure 2).
Figure 2.
Schematic illustration of the current challenges of mesenchymal stromal cell treatment in pancreatic cancer.
5.1. Tumorigenicity
Numerous studies have shown that MSCs have inherent tumorigenicity properties [17,55,150,151,152,153]. MSCs possess the molecular potential to affect and direct several crucial processes, which are important for tumor development, as the cells contain an abundant source of various biochemical mediators [14,22]. MSCs have been successfully isolated from various types of tumor tissues, such as HCC, glioma, gastric cancer, breast cancer, ovarian cancer, prostate cancer, colon cancer, and pancreatic cancer, indicating that MSC is a distinct stromal cell type in the TME that participates in tumor development [17,154]. It consists of stromal cells that include tumor-associated fibroblasts, tumor endothelial cells, immune and inflammatory cells, and bone marrow-derived cells [155,156]. Interactions between tumor cells and the TME tremendously impact tumor development, metastasis, and drug resistance [157,158].
MSCs can reportedly modulate stromal heterogeneity in various solid tumors, including pancreatic cancer [151,159]. Furthermore, MSCs regulate specific secretory molecules in the TME and promote the progression and invasion of pancreatic cancer [152,160]. AD-MSCs migrate to pancreatic cancer locations to serve as a major source of a-SMA+ cells and promote tumor progression [55,56]. Nevertheless, the mechanism underlying the mobilization of these intricate molecules remains unclear. Notably, Ganguly et al. found that MUC5AC acts as a systemic carrier of tumor secretome and can alter stromal maturation in pancreatic cancer by mobilizing AD-MSCs via CD44 and CD29/ITGB1 clustering [161]. Moreover, Miyazaki et al. found that AD-MSCs can differentiate into different pancreatic cancer-associated fibroblast subtypes, thus driving tumor heterogeneity and playing a key role in the development and drug resistance of PDAC [162]. Kabashima et al. found that BM-MSC-derived myofibroblasts modulate epithelial-to-mesenchymal transition and augment stemness-associated genes in PDAC [163]. Furthermore, BM-MSCs can reportedly migrate to tumor vessels and promote pancreatic cancer angiogenesis [164].
Tumor-associated macrophages (TAMs) are the predominant immune cells in the TME and are involved in tumorigenesis, immune escape, metastasis, and chemotherapeutic resistance [165]. TAMs have become a potential target for developing new cancer treatments [166] and are frequently involved in pancreatic cancer progression and the Warburg effect [167]. Reportedly, MSCs promote the progression and growth of pancreatic cancer by inducing alternating polarization of macrophages [168]. This could provide a potential new therapeutic strategy for PDAC.
Moreover, UCMSC-derived exosomes promote the growth of PDAC, which might be regulated via the delivery of miRNAs to the tumor cells to mediate the relevant signaling pathways [169]. Thus, MSCs promote the progression of pancreatic cancer.
5.2. MSCs Promote Drug Resistance
MSCs have been revealed to induce and play an important role in the drug resistance of tumor cells in the TME [136,170]. Several potential mechanisms underlying this phenomenon might include promoting active drug sequestration, decreasing drug concentration, and delivering specific RNA, proteins, and functional small molecules into target cells to induce dysregulation of relevant signaling pathways. For example, Roodhart et al. found that endogenous MSCs are activated on treatment with platinum analogs and release some mediators to protect tumor cells against a range of chemotherapeutics. By a metabolomics method, the results showed that two distinct platinum-induced polyunsaturated fatty acids derived from MSCs, 12-oxo-5,8,10-heptadecatrienoic acid and hexadeca-4,7,10,13-tetraenoic acid [16:4 (n−3)], induce resistance to platinum-based chemotherapy [171]. Furthermore, MSC-derived exosomes induce drug resistance in various tumor cells. Wang et al. showed that BM-MSC-derived exosomes play key roles in drug resistance in multiple myeloma and induce their proliferation, migration, and survival [172]. Moreover, MSC-derived exosomes promote drug resistance in gastric cancer cells via activating the CaM-Ks/Raf/MEK/ERK pathway [173]. MSCs promote the expression of SNHG7 in pancreatic tumor cells, inducing the stemness and FOLFIRINOX resistance through the Notch1/Jagged1/Hes-1 axis [174]. Hence, MSCs might induce drug resistance in pancreatic tumor cells; these obstacles should be overcome for MSCs to be clinically applied.
5.3. Limitations of the Clinical Applications of MSCs
Several studies have demonstrated the efficacy and safety of various types of MSCs and MSC-derived exosomes in pancreatic cancer therapy; nevertheless, their clinical applications have some limitations.
5.3.1. Routines of MSC Application and Distribution in the Host
Numerous studies have reported the tumor-homing properties of MSCs; however, the migration and distribution of MSCs in the body are not yet clearly understood. In animal experiments, the most common method of infusion of MSCs is through the intravenous (IV) or intraperitoneal (i.p.) route [175]. Nevertheless, owing to their size and the small dimensions of the lung vessels, a large number of MSCs are temporarily distributed in the lung after IV administration [176,177,178,179,180]. Notably, three days after IV administration, most of the MSCs are recruited to the tumor locations in an orthotopic pancreatic cancer model of athymic nude mice; only some MSCs are observed in the lung [164]. An orthotopic xenograft model of human pancreatic cancer built by directly injecting Panc02 pancreatic cancer cells into the pancreas and followed by intravenously injecting MSCs showed that three days after administration, the MSCs are recruited to the growing tumor vasculature of cancer [95]. Similarly, when MSCs are intraperitoneally injected into an orthotopic xenograft model of human pancreatic cancer built using i.p. PANC-1, most MSCs are observed in specific organ sites of the tumor and metastatic lesions after seven days [96]. After three weeks, MSCs are observed only in the tumor tissues but not in the fat tissues or on the intraperitoneal organ surfaces [76]. These results indicate that intravenously and intraperitoneally administered MSCs can primarily migrate to the pancreatic cancer site, thus inhibiting the growth of tumors. Upon injecting pancreatic cancer cells into the pancreatic nape of the neck and simultaneously orthotopically injecting MSCs into the pancreas, a higher pancreas-targeted distribution of the MSCs is noticed than that observed when MSCs are intravenously injected [57]. Therefore, the intravenously, intratumorally, and orthotopically infused MSCs may be effective; nonetheless, determining the best route of administration requires further investigation.
5.3.2. Timing and Dosage
The anti-tumor effect of exogenous MSCs depends on the time of their inoculation in tumor-bearing animals. MSCs infused during the initial phase of tumor growth exert anti-tumor effects, whereas those infused during the progressive stage of tumor development induce immune escape and promote the growth of the tumor [181]. Thus, the best time for treatment needs to be established. According to current studies, when MSCs are infused in the pancreatic cancer model during the early stage of solid tumorigenesis, the growth of tumors can be inhibited [57,76,97]. However, infusing MSCs in the pancreatic cancer model during the progressive stage of tumor development (10–17 days) can also inhibit the growth of tumors [75,89,92,95]. Although approximately 1 × 105 to 1 × 106 cells are usually infused in pancreatic cancer animal models, the most appropriate dose of MSCs has not yet been confirmed [57,89,94,97]. Therefore, the optimal dose and route of administration need to be elucidated.
5.3.3. Infiltration, Persistence, and Exhaustion
Although CAR-modified T cells reveal a new potential option in cancers, current CAR T-cell clinical trials in pancreatic cancer have been unable to increase survival and exhibit any significant response. This might be due to obstacles such as T-cell infiltration, persistence, and exhaustion [45]. The TME in pancreatic cancer comprises tumor cells, endothelial cells, immune cells, stromal cells, extracellular matrix, and a broad spectrum of enzymes, cytokines, and growth factors [182]. As a dense stroma surrounds pancreas cancer, successful immunotherapy and chemotherapy are required to break through the physical and environmental barriers in the TME [183]. Additionally, owing to the complex TME, CAR T-cell treatment in pancreatic cancer leads to T-cell exhaustion and persistence [184,185]. Similarly, successful MSCs treatments for pancreatic cancer should also be able to overcome the physical and environmental barriers in the TME, including infiltration, persistence, and exhaustion. Thus, further clinical trials need to be carried out.
MSC isolation and expansion remain a challenge. Even when subjected to similar isolation and culture conditions, the MSCs obtained from different sources can be heterogeneous [186]. This observation reveals the heterogeneous nature of a typical MSC population and their potential to migrate to different tissues, promote tissue repair, or inhibit inflammation [187]. Thus, the differences in approaches used for culturing and expanding MSCs need to be studied to determine whether these differences affect their phenotype and functional properties [187]. Furthermore, standard protocols for characterizing MSC-derived exosomes owing to their heterogeneous nature that may have diverse effects on the target cells remain lacking [188]. Moreover, patients who receive MSC-derived exosomes need to be closely monitored to determine the optimal dosage with the best therapeutic efficiency [109]. Lastly, MSCs manufactured for cancer therapy should meet the standards of good manufacturing practices and regulations.
6. Conclusions and Perspectives
MSCs can home to tumor locations and survive in the TME owing to their tumor-homing properties. Thus, MSCs or MSC-derived exosomes, as a carrier of anti-cancer drugs, can be genetically modified to deliver various agents to inhibit tumor growth. The application of MSCs or MSC-derived exosomes as carriers for tumor target therapy has numerous advantages, including low immunogenicity, tumor tropism, easy rapid isolation and expansion, and the ability to release various therapeutic agents. In the recent decade, remarkable progress has been made in the field of engineered MSC-based tumor-targeted therapy for pancreatic cancer. However, the clinical application of MSC-based therapy in the treatment of pancreatic cancer still faces many challenges. Thus, overcoming these challenges is necessary. Subsequently, the crosstalk between MSCs and tumor cells to increase the clinical safety of MSC-based therapeutic measures need to be clarified. Thus, future research should be focused on the long-term follow-up of MSC-treated tumor-bearing animals to address all safety concerns related to the plasticity of MSCs and their possible pro-tumorigenic effects. In summary, MSC-based therapies are emerging as an attractive option for the treatment of pancreatic cancer.
Author Contributions
Z.M. and J.H. contributed equally to this study. Z.M., J.H., J.L., B.Z., W.W., J.X. and X.Y. contributed to the writing and revising of the manuscript. J.X. and X.Y. supervised the review. All authors have read and agreed to the published version of the manuscript.
Funding
This study was jointly supported by the National Natural Science Foundation of China (82200717, U21A20374, and 82072698), Shanghai Municipal Science and Technology Major Project (21JC1401500), Scientific Innovation Project of Shanghai Education Committee (2019-01-07-00-07-E00057), Clinical Research Plan of Shanghai Hospital Development Center (SHDC2020CR1006A), and Xuhui District Artificial Intelligence Medical Hospital Cooperation Project (2021-011).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
All authors declare no conflicts of interest.
Abbreviations
MSCs: mesenchymal stromal cells; PDAC: pancreatic ductal adenocarcinoma; TME: tumor microenvironment; PSCs: pancreatic stellate cells; PD-1/PD-L1: programmed death 1 or programmed death 1 ligand 1; AD-MSCs: adipose tissue-derived mesenchymal stromal cells; UCMSCs: umbilical cord matrix-derived stem cells; TRAIL: tumor necrosis factor α-related apoptosis-inducing ligand; XIAP: X-linked inhibitor of apoptosis protein; BM-MSCs: bone marrow-derived mesenchymal stromal cells; HSV-TK: herpes simplex virus thymidine kinase; HCC: hepatocellular carcinoma; PTX: paclitaxel; GCB: gemcitabine; OXA: oxaliplatin; IV: intravenous.
References
- Wu, W.; He, X.-K.; Yang, L.; Wang, Q.; Bian, X.; Ye, J.; Li, Y.; Li, L. Rising trends in pancreatic cancer incidence and mortality in 2000–2014. Clin. Epidemiol. 2018, 10, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.M.; Turk, T.; Al-Husseini, M.J.; Abdel-Rahman, O. Trends in pancreatic adenocarcinoma incidence and mortality in the United States in the last four decades; a SEER-based study. BMC Cancer 2018, 18, 688. [Google Scholar] [CrossRef]
- Park, W.; Chawla, A.; O’Reilly, E. Pancreatic Cancer: A Review. JAMA 2021, 326, 851–862. [Google Scholar] [CrossRef]
- Kleeff, J.; Korc, M.; Apte, M.; La Vecchia, C.; Johnson, C.; Biankin, A.; Neale, R.; Tempero, M.; Tuveson, D.; Hruban, R.; et al. Pancreatic cancer. Nat. Rev. Dis. Primers 2016, 2, 16022. [Google Scholar] [CrossRef]
- Adamska, A.; Domenichini, A.; Falasca, M. Pancreatic Ductal Adenocarcinoma: Current and Evolving Therapies. Int. J. Mol. Sci. 2017, 18, 1338. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.; Miller, K.; Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, J.; Surana, R.; Valle, J.; Shroff, R. Pancreatic cancer. Lancet 2020, 395, 2008–2020. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Xu, J.-W.; Cheng, Y.-G.; Gao, J.-Y.; Hu, S.-Y.; Wang, L.; Zhan, H.X. Early detection of pancreatic cancer: Where are we now and where are we going? Int. J. Cancer 2017, 141, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.-F.; Shang, W.-T.; Lu, G.-H.; Guo, K.-X.; Deng, H.; Zhu, X.-H.; Wang, C.-C.; Tian, J. Decreasing hyaluronic acid combined with drug-loaded nanoprobes improve the delivery and efficacy of chemotherapeutic drugs for pancreatic cancer. Cancer Lett. 2021, 523, 1–9. [Google Scholar] [CrossRef]
- Cai, H.; Wang, R.; Guo, X.; Song, M.; Yan, F.; Ji, B.; Liu, Y. Combining Gemcitabine-Loaded Macrophage-like Nanoparticles and Erlotinib for Pancreatic Cancer Therapy. Mol. Pharm. 2021, 18, 2495–2506. [Google Scholar] [CrossRef]
- Crippa, S.; Belfiori, G.; Bissolati, M.; Partelli, S.; Pagnanelli, M.; Tamburrino, D.; Gasparini, G.; Rubini, C.; Zamboni, G.; Falconi, M. Recurrence after surgical resection of pancreatic cancer: The importance of postoperative complications beyond tumor biology. HPB 2021, 23, 1666–1673. [Google Scholar] [CrossRef] [PubMed]
- Nienhuijs, S.W.; Akker, S.A.V.D.; de Vries, E.; de Hingh, I.H.; Visser, O.; Lemmens, V.E. Nationwide Improvement of Only Short-Term Survival After Resection for Pancreatic Cancer in The Netherlands. Pancreas 2012, 41, 1063–1066. [Google Scholar] [CrossRef] [PubMed]
- Barugola, G.; Partelli, S.; Marcucci, S.; Sartori, N.; Capelli, P.; Bassi, C.; Pederzoli, P.; Falconi, M. Resectable Pancreatic Cancer: Who Really Benefits From Resection? Ann. Surg. Oncol. 2009, 16, 3316–3322. [Google Scholar] [CrossRef] [PubMed]
- Lan, T.; Luo, M.; Wei, X. Mesenchymal stem/stromal cells in cancer therapy. J. Hematol. Oncol. 2021, 14, 195. [Google Scholar] [CrossRef]
- Hmadcha, A.; Martin-Montalvo, A.; Gauthier, B.; Soria, B.; Capilla-Gonzalez, V. Therapeutic Potential of Mesenchymal Stem Cells for Cancer Therapy. Front. Bioeng. Biotechnol. 2020, 8, 43. [Google Scholar] [CrossRef]
- Timaner, M.; Tsai, K.K.; Shaked, Y. The multifaceted role of mesenchymal stem cells in cancer. Semin. Cancer Biol. 2019, 60, 225–237. [Google Scholar] [CrossRef]
- Yin, Z.; Jiang, K.; Li, R.; Dong, C.; Wang, L. Multipotent mesenchymal stromal cells play critical roles in hepatocellular carcinoma initiation, progression and therapy. Mol. Cancer 2018, 17, 178. [Google Scholar] [CrossRef]
- Galipeau, J.; Sensébé, L. Mesenchymal Stromal Cells: Clinical Challenges and Therapeutic Opportunities. Cell Stem Cell 2018, 22, 824–833. [Google Scholar] [CrossRef]
- Zhou, T.; Yuan, Z.; Weng, J.; Pei, D.; Du, X.; He, C.; Lai, P. Challenges and advances in clinical applications of mesenchymal stromal cells. J. Hematol. Oncol. 2021, 14, 24. [Google Scholar] [CrossRef]
- Mirzaei, H.; Sahebkar, A.; Avan, A.; Jaafari, M.R.; Salehi, R.; Salehi, H.; Baharvand, H.; Rezaei, A.; Hadjati, J.; Pawelek, J.M.; et al. Application of Mesenchymal Stem Cells in Melanoma: A Potential Therapeutic Strategy for Delivery of Targeted Agents. Curr. Med. Chem. 2016, 23, 455–463. [Google Scholar] [CrossRef]
- Houghton, J.; Stoicov, C.; Nomura, S.; Rogers, A.B.; Carlson, J.; Li, H.; Cai, X.; Fox, J.G.; Goldenring, J.R.; Wang, T.C. Gastric Cancer Originating from Bone Marrow-Derived Cells. Science 2004, 306, 1568–1571. [Google Scholar] [CrossRef] [PubMed]
- Błogowski, W.; Bodnarczuk, T.; Starzyńska, T. Concise Review: Pancreatic Cancer and Bone Marrow-Derived Stem Cells. STEM CELLS Transl. Med. 2016, 5, 938–945. [Google Scholar] [CrossRef] [PubMed]
- Moniri, M.R.; Dai, L.-J.; Warnock, G.L. The challenge of pancreatic cancer therapy and novel treatment strategy using engineered mesenchymal stem cells. Cancer Gene Ther. 2014, 21, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Chopra, N.; Choudhury, S.; Bhargava, S.; Wajid, S.; Ganguly, N. Potentials of “stem cell-therapy” in pancreatic cancer: An update. Pancreatology 2019, 19, 1034–1042. [Google Scholar] [CrossRef]
- Chu, Y.; Zhu, C.; Wang, Q.; Liu, M.; Wan, W.; Zhou, J.; Han, R.; Yang, J.; Luo, W.; Liu, C.; et al. Adipose-derived mesenchymal stem cells induced PAX8 promotes ovarian cancer cell growth by stabilizing TAZ protein. J. Cell. Mol. Med. 2021, 25, 4434–4443. [Google Scholar] [CrossRef] [PubMed]
- Karnoub, A.E.; Dash, A.B.; Vo, A.P.; Sullivan, A.; Brooks, M.W.; Bell, G.W.; Richardson, A.L.; Polyak, K.; Tubo, R.; Weinberg, R.A. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 2007, 449, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Huang, L.; Li, Y.; Fang, B.; Li, G.; Chen, L.; Xu, L. Mesenchymal Stem Cells and Cancer: Clinical Challenges and Opportunities. BioMed Res. Int. 2019, 2019, 2820853. [Google Scholar] [CrossRef]
- Millikan, K.W.; Deziel, D.J.; Silverstein, J.C.; Kanjo, T.M.; Christein, J.D.; Doolas, A.; Prinz, R.A. Prognostic Factors Associated with Resectable Adenocarcinoma of the Head of the Pancreas. Am. Surg. 1999, 65, 618–624. [Google Scholar] [CrossRef]
- Okasha, H.; Elkholy, S.; El-Sayed, R.; Wifi, M.-N.; El-Nady, M.; El-Nabawi, W.; El-Dayem, W.A.; Radwan, M.I.; Farag, A.; El-Sherif, Y.; et al. Real time endoscopic ultrasound elastography and strain ratio in the diagnosis of solid pancreatic lesions. World J. Gastroenterol. 2017, 23, 5962–5968. [Google Scholar] [CrossRef]
- Katz, M.H.G.; Ou, F.S.; Herman, J.M.; Ahmad, S.A.; Wolpin, B.; Marsh, R.; Behr, S.; Shi, Q.; Chuong, M.; Schwartz, L.H.; et al. Alliance for clinical trials in oncology (ALLIANCE) trial A021501: Preoperative extended chemotherapy vs. chemotherapy plus hypofractionated radiation therapy for borderline resectable adenocarcinoma of the head of the pancreas. BMC Cancer 2017, 17, 505. [Google Scholar] [CrossRef]
- Allen, P.J.; Kuk, D.; Castillo, C.F.-D.; Basturk, O.; Wolfgang, C.L.; Cameron, J.L.; Lillemoe, K.D.; Ferrone, C.R.; Morales-Oyarvide, V.; He, J.; et al. Multi-institutional Validation Study of the American Joint Commission on Cancer (8th Edition) Changes for T and N Staging in Patients With Pancreatic Adenocarcinoma. Ann. Surg. 2017, 265, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Pluchino, L.A.; D’Amico, T.A. National Comprehensive Cancer Network Guidelines: Who Makes Them? What Are They? Why Are They Important? Ann. Thorac. Surg. 2020, 110, 1789–1795. [Google Scholar] [CrossRef] [PubMed]
- Wang-Gillam, A.; Li, C.-P.; Bodoky, G.; Dean, A.; Shan, Y.-S.; Jameson, G.; Macarulla, T.; Lee, K.-H.; Cunningham, D.; Blanc, J.F.; et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): A global, randomised, open-label, phase 3 trial. Lancet 2016, 387, 545–557. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.-L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef]
- Wu, J.; Liang, C.; Chen, M.; Su, W. Association between tumor-stroma ratio and prognosis in solid tumor patients: A systematic review and meta-analysis. Oncotarget 2016, 7, 68954–68965. [Google Scholar] [CrossRef]
- Neesse, A.; Algül, H.; Tuveson, D.A.; Gress, T. Stromal biology and therapy in pancreatic cancer: A changing paradigm. Gut 2015, 64, 1476–1484. [Google Scholar] [CrossRef]
- Garin-Chesa, P.; Old, L.J.; Rettig, W.J. Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc. Natl. Acad. Sci. USA 1990, 87, 7235–7239. [Google Scholar] [CrossRef]
- Torphy, R.J.; Zhu, Y.; Schulick, R.D. Immunotherapy for pancreatic cancer: Barriers and breakthroughs. Ann. Gastroenterol. Surg. 2018, 2, 274–281. [Google Scholar] [CrossRef]
- Lunardi, S.; Muschel, R.J.; Brunner, T.B. The stromal compartments in pancreatic cancer: Are there any therapeutic targets? Cancer Lett. 2014, 343, 147–155. [Google Scholar] [CrossRef]
- Samulitis, B.K.; Pond, K.W.; Pond, E.; Cress, A.; Patel, H.; Wisner, L.; Patel, C.; Dorr, R.T.; Landowski, T.H. Gemcitabine resistant pancreatic cancer cell lines acquire an invasive phenotype with collateral hypersensitivity to histone deacetylase inhibitors. Cancer Biol. Ther. 2014, 16, 43–51. [Google Scholar] [CrossRef]
- Yi, M.; Zheng, X.; Niu, M.; Zhu, S.; Ge, H.; Wu, K. Combination strategies with PD-1/PD-L1 blockade: Current advances and future directions. Mol. Cancer 2022, 21, 28. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.; Xiong, G.; Cao, Z.; Yang, G.; Zheng, S.; Song, X.; You, L.; Zheng, L.; Zhang, T.; Zhao, Y. PD-1/PD-L1 and immunotherapy for pancreatic cancer. Cancer Lett. 2017, 407, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Brahmer, J.R.; Tykodi, S.S.; Chow, L.Q.M.; Hwu, W.-J.; Topalian, S.L.; Hwu, P.; Drake, C.G.; Camacho, L.H.; Kauh, J.; Odunsi, K.; et al. Safety and Activity of Anti-PD-L1 Antibody in Patients with Advanced Cancer. N. Engl. J. Med. 2012, 366, 2455–2465. [Google Scholar] [CrossRef] [PubMed]
- DeSelm, C.J.; Tano, Z.E.; Varghese, A.M.; Adusumilli, P.S. CAR T-cell therapy for pancreatic cancer. J. Surg. Oncol. 2017, 116, 63–74. [Google Scholar] [CrossRef]
- Henze, J.; Tacke, F.; Hardt, O.; Alves, F.; Al Rawashdeh, W. Enhancing the Efficacy of CAR T Cells in the Tumor Microenvironment of Pancreatic Cancer. Cancers 2020, 12, 1389. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Yang, X.; Han, Z.-P.; Qu, F.-F.; Shao, L.; Shi, Y.-F. Mesenchymal stem cells: A new trend for cell therapy. Acta Pharmacol. Sin. 2013, 34, 747–754. [Google Scholar] [CrossRef]
- Mishra, P.J.; Banerjee, D. Activation and Differentiation of Mesenchymal Stem Cells. Methods Mol. Biol. 2017, 1554, 201–209. [Google Scholar] [CrossRef]
- Crisan, M.; Yap, S.; Casteilla, L.; Chen, C.-W.; Corselli, M.; Park, T.S.; Andriolo, G.; Sun, B.; Zheng, B.; Zhang, L.; et al. A Perivascular Origin for Mesenchymal Stem Cells in Multiple Human Organs. Cell Stem Cell 2008, 3, 301–313. [Google Scholar] [CrossRef]
- Ma, Z.; Zhou, J.; Yang, T.; Xie, W.; Song, G.; Song, Z.; Chen, J. Mesenchymal stromal cell therapy for pancreatitis: Progress and challenges. Med. Res. Rev. 2021, 41, 2474–2488. [Google Scholar] [CrossRef]
- Viswanathan, S.; Shi, Y.; Galipeau, J.; Krampera, M.; Leblanc, K.; Martin, I.; Nolta, J.; Phinney, D.; Sensebe, L. Mesenchymal stem versus stromal cells: International Society for Cell & Gene Therapy (ISCT(R)) Mesenchymal Stromal Cell committee position statement on nomenclature. Cytotherapy 2019, 21, 1019–1024. [Google Scholar]
- Song, N.; Scholtemeijer, M.; Shah, K. Mesenchymal Stem Cell Immunomodulation: Mechanisms and Therapeutic Potential. Trends Pharmacol. Sci. 2020, 41, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Krampera, M.; Le Blanc, K. Mesenchymal stromal cells: Putative microenvironmental modulators become cell therapy. Cell Stem Cell 2021, 28, 1708–1725. [Google Scholar] [CrossRef]
- Devine, S.M.; Cobbs, C.; Jennings, M.; Bartholomew, A.; Hoffman, R. Mesenchymal stem cells distribute to a wide range of tissues following systemic infusion into nonhuman primates. Blood 2003, 101, 2999–3001. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Ge, Y.; Zhang, C.; Zhang, L.; Xu, J.; Qi, L.; Li, W. Progress of Mesenchymal Stem Cell-Derived Exosomes in Tissue Repair. Curr. Pharm. Des. 2020, 26, 2022–2037. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Daquinag, A.; Traktuev, D.O.; Amaya-Manzanares, F.; Simmons, P.J.; March, K.L.; Pasqualini, R.; Arap, W.; Kolonin, M.G. White Adipose Tissue Cells Are Recruited by Experimental Tumors and Promote Cancer Progression in Mouse Models. Cancer Res 2009, 69, 5259–5266. [Google Scholar] [CrossRef] [PubMed]
- Okumura, T.; Ohuchida, K.; Kibe, S.; Iwamoto, C.; Ando, Y.; Takesue, S.; Nakayama, H.; Abe, T.; Endo, S.; Koikawa, K.; et al. Adipose tissue-derived stromal cells are sources of cancer-associated fibroblasts and enhance tumor progression by dense collagen matrix. Int. J. Cancer 2019, 144, 1401–1413. [Google Scholar] [CrossRef] [PubMed]
- Jazowiecka-Rakus, J.; Hadrys, A.; Rahman, M.; McFadden, G.; Fidyk, W.; Chmielik, E.; Pazdzior, M.; Grajek, M.; Kozik, V.; Sochanik, A. Myxoma Virus Expressing LIGHT (TNFSF14) Pre-Loaded into Adipose-Derived Mesenchymal Stem Cells Is Effective Treatment for Murine Pancreatic Adenocarcinoma. Cancers 2021, 13, 1394. [Google Scholar] [CrossRef]
- Han, J.; Hwang, H.S.; Na, K. TRAIL-secreting human mesenchymal stem cells engineered by a non-viral vector and photochemical internalization for pancreatic cancer gene therapy. Biomaterials 2018, 182, 259–268. [Google Scholar] [CrossRef]
- Karp, J.M.; Teo, G.S.L. Mesenchymal Stem Cell Homing: The Devil Is in the Details. Cell Stem Cell 2009, 4, 206–216. [Google Scholar] [CrossRef]
- Lau, T.T.; Wang, D.-A. Stromal cell-derived factor-1 (SDF-1): Homing factor for engineered regenerative medicine. Expert Opin. Biol. Ther. 2011, 11, 189–197. [Google Scholar] [CrossRef]
- Vicinanza, C.; Lombardi, E.; Da Ros, F.; Marangon, M.; Durante, C.; Mazzucato, M.; Agostini, F. Modified mesenchymal stem cells in cancer therapy: A smart weapon requiring upgrades for wider clinical applications. World J. Stem Cells 2022, 14, 54–75. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Liu, N.; Yi, B.; Zhang, X.; Gao, B.; Zhang, Y.; Xu, R.; Li, X.; Dai, Y. Transplanted hUCB-MSCs migrated to the damaged area by SDF-1/CXCR4 signaling to promote functional recovery after traumatic brain injury in rats. Neurol. Res. 2015, 37, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Ringe, J.; Strassburg, S.; Neumann, K.; Endres, M.; Notter, M.; Burmester, G.-R.; Kaps, C.; Sittinger, M. Towards in situ tissue repair: Human mesenchymal stem cells express chemokine receptors CXCR1, CXCR2 and CCR2, and migrate upon stimulation with CXCL8 but not CCL2. J. Cell. Biochem. 2007, 101, 135–146. [Google Scholar] [CrossRef] [PubMed]
- De Ugarte, D.A.; Alfonso, Z.; Zuk, P.A.; Elbarbary, A.; Zhu, M.; Ashjian, P.; Benhaim, P.; Hedrick, M.H.; Fraser, J.K. Differential expression of stem cell mobilization-associated molecules on multi-lineage cells from adipose tissue and bone marrow. Immunol. Lett. 2003, 89, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Wang, S.; Zhao, R.C. The roles of mesenchymal stem cells in tumor inflammatory microenvironment. J. Hematol. Oncol. 2014, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Volarevic, V.; Ljujic, B.; Stojkovic, P.; Lukic, A.; Arsenijevic, N.; Stojkovic, M. Human stem cell research and regenerative medicine--present and future. Br. Med Bull. 2011, 99, 155–168. [Google Scholar] [CrossRef]
- Momin, E.N.; Vela, G.; Zaidi, H.A.; Quinones-Hinojosa, A. The Oncogenic Potential of Mesenchymal Stem Cells in the Treatment of Cancer: Directions for Future Research. Curr. Immunol. Rev. 2010, 6, 137–148. [Google Scholar] [CrossRef]
- Kucerova, L.; Altanerova, V.; Matuskova, M.; Tyciakova, S.; Altaner, C. Adipose Tissue–Derived Human Mesenchymal Stem Cells Mediated Prodrug Cancer Gene Therapy. Cancer Res 2007, 67, 6304–6313. [Google Scholar] [CrossRef]
- Ridge, S.M.; Sullivan, F.J.; Glynn, S.A. Mesenchymal stem cells: Key players in cancer progression. Mol. Cancer 2017, 16, 31. [Google Scholar] [CrossRef]
- Galland, S.; Stamenkovic, I. Mesenchymal stromal cells in cancer: A review of their immunomodulatory functions and dual effects on tumor progression. J. Pathol. 2019, 250, 555–572. [Google Scholar] [CrossRef]
- Fathi, E.; Sanaat, Z.; Farahzadi, R. Mesenchymal stem cells in acute myeloid leukemia: A focus on mechanisms involved and therapeutic concepts. Blood Res. 2019, 54, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Khakoo, A.Y.; Pati, S.; Anderson, S.A.; Reid, W.; Elshal, M.F.; Rovira, I.I.; Nguyen, A.T.; Malide, D.; Combs, C.A.; Hall, G. Human mesenchymal stem cells exert potent antitumorigenic effects in a model of Kaposi’s sarcoma. J. Exp. Med. 2006, 203, 1235–1247. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, R.M.; Khan, S.; Barry, F.P.; O’Brien, T.; Kerin, M.J. Advances in mesenchymal stem cell-mediated gene therapy for cancer. Stem Cell Res. Ther. 2010, 1, 25. [Google Scholar] [CrossRef] [PubMed]
- Shah, K. Mesenchymal stem cells engineered for cancer therapy. Adv. Drug Deliv. Rev. 2012, 64, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Cousin, B.; Ravet, E.; Poglio, S.; De Toni, F.; Bertuzzi, M.; Lulka, H.; Touil, I.; André, M.; Grolleau, J.-L.; Péron, J.-M.; et al. Adult Stromal Cells Derived from Human Adipose Tissue Provoke Pancreatic Cancer Cell Death both In Vitro and In Vivo. PLoS ONE 2009, 4, e6278. [Google Scholar] [CrossRef] [PubMed]
- Doi, C.; Maurya, D.K.; Pyle, M.M.; Troyer, D.; Tamura, M. Cytotherapy with naive rat umbilical cord matrix stem cells significantly attenuates growth of murine pancreatic cancer cells and increases survival in syngeneic mice. Cytotherapy 2010, 12, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, Z.; Safari, F. Evaluating the in vitro therapeutic effects of human amniotic mesenchymal stromal cells on MiaPaca2 pancreatic cancer cells using 2D and 3D cell culture model. Tissue Cell 2021, 68, 101479. [Google Scholar] [CrossRef]
- Chulpanova, D.S.; Kitaeva, K.V.; Tazetdinova, L.G.; James, V.; Rizvanov, A.A.; Solovyeva, V.V. Application of Mesenchymal Stem Cells for Therapeutic Agent Delivery in Anti-tumor Treatment. Front. Pharmacol. 2018, 9, 259. [Google Scholar] [CrossRef]
- Mohammadi, M.; Jaafari, M.R.; Mirzaei, H.R.; Mirzaei, H. Mesenchymal stem cell: A new horizon in cancer gene therapy. Cancer Gene Ther. 2016, 23, 285–286. [Google Scholar] [CrossRef]
- Keung, E.Z.; Nelson, P.J.; Conrad, C. Concise Review: Genetically Engineered Stem Cell Therapy Targeting Angiogenesis and Tumor Stroma in Gastrointestinal Malignancy. Stem Cells 2013, 31, 227–235. [Google Scholar] [CrossRef]
- De Palma, M.; Mazzieri, R.; Politi, L.S.; Pucci, F.; Zonari, E.; Sitia, G.; Mazzoleni, S.; Moi, D.; Venneri, M.A.; Indraccolo, S.; et al. Tumor-Targeted Interferon-α Delivery by Tie2-Expressing Monocytes Inhibits Tumor Growth and Metastasis. Cancer Cell 2008, 14, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Niess, H.; Bao, Q.; Conrad, C.; Zischek, C.; Notohamiprodjo, M.; Schwab, F.; Schwarz, B.; Huss, R.; Jauch, K.-W.; Nelson, P.J.; et al. Selective Targeting of Genetically Engineered Mesenchymal Stem Cells to Tumor Stroma Microenvironments Using Tissue-Specific Suicide Gene Expression Suppresses Growth of Hepatocellular Carcinoma. Ann. Surg. 2011, 254, 767–774, discussion 774–765. [Google Scholar] [CrossRef]
- Mueller, L.P.; Lützkendorf, J.; Widder, M.; Nerger, K.; Caysa, H.; Mueller, T.D. TRAIL-transduced multipotent mesenchymal stromal cells (TRAIL-MSC) overcome TRAIL resistance in selected CRC cell lines in vitro and in vivo. Cancer Gene Ther. 2011, 18, 229–239. [Google Scholar] [CrossRef]
- Levy, O.; Brennen, W.N.; Han, E.; Rosen, D.M.; Musabeyezu, J.; Safaee, H.; Ranganath, S.; Ngai, J.; Heinelt, M.; Milton, Y.; et al. A prodrug-doped cellular Trojan Horse for the potential treatment of prostate cancer. Biomaterials 2016, 91, 140–150. [Google Scholar] [CrossRef]
- Vogler, M.; Dürr, K.; Jovanovic, M.; Debatin, K.-M.; Fulda, S. Regulation of TRAIL-induced apoptosis by XIAP in pancreatic carcinoma cells. Oncogene 2007, 26, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Niidome, T.; Huang, L. Gene Therapy Progress and Prospects: Nonviral vectors. Gene Ther. 2002, 9, 1647–1652. [Google Scholar] [CrossRef] [PubMed]
- Vogler, M.; Walczak, H.; Stadel, D.; Haas, T.L.; Genze, F.; Jovanovic, M.; Bhanot, U.; Hasel, C.; Möller, P.; Gschwend, J.E.; et al. Small Molecule XIAP Inhibitors Enhance TRAIL-Induced Apoptosis and Antitumor Activity in Preclinical Models of Pancreatic Carcinoma. Cancer Res. 2009, 69, 2425–2434. [Google Scholar] [CrossRef] [PubMed]
- Vogler, M.; Walczak, H.; Stadel, D.; Haas, T.L.; Genze, F.; Jovanovic, M.; Gschwend, J.E.; Simmet, T.; Debatin, K.-M.; Fulda, S. Targeting XIAP Bypasses Bcl-2–Mediated Resistance to TRAIL and Cooperates with TRAIL to Suppress Pancreatic Cancer Growth In vitro and In vivo. Cancer Res. 2008, 68, 7956–7965. [Google Scholar] [CrossRef]
- Mohr, A.; Albarenque, S.M.; Deedigan, L.; Yu, R.; Reidy, M.; Fulda, S.; Zwacka, R.M. Targeting of XIAP Combined with Systemic Mesenchymal Stem Cell-Mediated Delivery of sTRAIL Ligand Inhibits Metastatic Growth of Pancreatic Carcinoma Cells. STEM CELLS 2010, 28, 2109–2120. [Google Scholar] [CrossRef]
- Moniri, M.R.; Sun, X.-Y.; Rayat, J.; Dai, D.; Ao, Z.; He, Z.; Verchere, C.B.; Dai, L.-J.; Warnock, G.L. TRAIL-engineered pancreas-derived mesenchymal stem cells: Characterization and cytotoxic effects on pancreatic cancer cells. Cancer Gene Ther. 2012, 19, 652–658. [Google Scholar] [CrossRef]
- Spano, C.; Grisendi, G.; Golinelli, G.; Rossignoli, F.; Prapa, M.; Bestagno, M.; Candini, O.; Petrachi, T.; Recchia, A.; Miselli, F.; et al. Soluble TRAIL Armed Human MSC As Gene Therapy For Pancreatic Cancer. Sci. Rep. 2019, 9, 1788. [Google Scholar] [CrossRef] [PubMed]
- Zischek, C.; Niess, H.; Ischenko, I.; Conrad, C.; Huss, R.; Jauch, K.-W.; Nelson, P.J.; Bruns, C. Targeting Tumor Stroma Using Engineered Mesenchymal Stem Cells Reduces the Growth of Pancreatic Carcinoma. Ann. Surg. 2009, 250, 747–753. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.-P.; Zhang, B.-L.; Duan, J.-W.; Wu, H.-H.; Wang, B.-Q.; Yu, Z.-P.; Yang, W.-J.; Shan, Y.-F.; Zhou, M.-T.; Zhang, Q.-Y. Effect of NK4 Transduction in Bone Marrow-Derived Mesenchymal Stem Cells on Biological Characteristics of Pancreatic Cancer Cells. Int. J. Mol. Sci. 2014, 15, 3729–3745. [Google Scholar] [CrossRef]
- Schug, C.; Gupta, A.; Urnauer, S.; Steiger, K.; Cheung, P.F.-Y.; Neander, C.; Savvatakis, K.; Schmohl, K.A.; Trajkovic-Arsic, M.; Schwenk, N.; et al. A Novel Approach for Image-Guided 131I Therapy of Pancreatic Ductal Adenocarcinoma Using Mesenchymal Stem Cell-Mediated NIS Gene Delivery. Mol. Cancer Res. 2019, 17, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Conrad, C.; Hüsemann, Y.; Niess, H.; von Luettichau, I.; Huss, R.; Bauer, C.; Jauch, K.-W.; Klein, C.A.; Bruns, C.; Nelson, P.J. Linking Transgene Expression of Engineered Mesenchymal Stem Cells and Angiopoietin-1–induced Differentiation to Target Cancer Angiogenesis. Ann. Surg. 2011, 253, 566–571. [Google Scholar] [CrossRef]
- Kidd, S.; Caldwell, L.; Dietrich, M.; Samudio, I.; Spaeth, E.; Watson, K.; Shi, Y.; Abbruzzese, J.; Konopleva, M.; Andreeff, M.; et al. Mesenchymal stromal cells alone or expressing interferon-beta suppress pancreatic tumors in vivo, an effect countered by anti-inflammatory treatment. Cytotherapy 2010, 12, 615–625. [Google Scholar] [CrossRef]
- Jing, W.; Chen, Y.; Lu, L.; Hu, X.; Shao, C.; Zhang, Y.; Zhou, X.; Zhou, Y.; Wu, L.; Liu, R.; et al. Human Umbilical Cord Blood–Derived Mesenchymal Stem Cells Producing IL15 Eradicate Established Pancreatic Tumor in Syngeneic Mice. Mol. Cancer Ther. 2014, 13, 2127–2137. [Google Scholar] [CrossRef]
- Zhao, C.; Pu, Y.; Zhang, H.; Hu, X.; Zhang, R.; He, S.; Zhao, Q.; Mu, B. IL10-modified Human Mesenchymal Stem Cells inhibit Pancreatic Cancer growth through Angiogenesis Inhibition. J. Cancer 2020, 11, 5345–5352. [Google Scholar] [CrossRef]
- Heldring, N.; Mäger, I.; Wood, M.J.; Le Blanc, K.; Andaloussi, S.E. Therapeutic Potential of Multipotent Mesenchymal Stromal Cells and Their Extracellular Vesicles. Hum. Gene Ther. 2015, 26, 506–517. [Google Scholar] [CrossRef]
- Keshtkar, S.; Azarpira, N.; Ghahremani, M.H. Mesenchymal stem cell-derived extracellular vesicles: Novel frontiers in regenerative medicine. Stem Cell Res. Ther. 2018, 9, 63. [Google Scholar] [CrossRef]
- Kalluri, R.; LeBleu, V.S. The biology, function, and biomedical applications of exosomes. Science 2020, 367, eaau6977. [Google Scholar] [CrossRef] [PubMed]
- Marote, A.; Teixeira, F.G.; Pinheiro, B.; Salgado, A.J. MSCs-Derived Exosomes: Cell-Secreted Nanovesicles with Regenerative Potential. Front. Pharmacol. 2016, 7, 231. [Google Scholar] [CrossRef] [PubMed]
- Vizoso, F.J.; Eiro, N.; Cid, S.; Schneider, J.; Perez-Fernandez, R. Mesenchymal Stem Cell Secretome: Toward Cell-Free Therapeutic Strategies in Regenerative Medicine. Int. J. Mol. Sci. 2017, 18, 1852. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, G.; Tu, C.; Chen, X.; Yang, B.; Huo, Y.; Li, Y.; Chen, A.-Z.; Lan, P.; Zhang, Y.S.; et al. High-throughput single-cell analysis of exosome mediated dual drug delivery, in vivo fate and synergistic tumor therapy. Nanoscale 2020, 12, 13742–13756. [Google Scholar] [CrossRef]
- Malhotra, H.; Sheokand, N.; Kumar, S.; Chauhan, A.S.; Kumar, M.; Jakhar, P.; Boradia, V.M.; Raje, C.I.; Raje, M. Exosomes: Tunable Nano Vehicles for Macromolecular Delivery of Transferrin and Lactoferrin to Specific Intracellular Compartment. J. Biomed. Nanotechnol. 2016, 12, 1101–1114. [Google Scholar] [CrossRef]
- Alvarez-Erviti, L.; Seow, Y.; Yin, H.; Betts, C.; Lakhal, S.; Wood, M.J.A. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011, 29, 341–345. [Google Scholar] [CrossRef]
- Shao, J.; Zaro, J.; Shen, Y. Advances in Exosome-Based Drug Delivery and Tumor Targeting: From Tissue Distribution to Intracellular Fate. Int. J. Nanomed. 2020, 15, 9355–9371. [Google Scholar] [CrossRef]
- Yaghoubi, Y.; Movassaghpour, A.; Zamani, M.; Talebi, M.; Mehdizadeh, A.; Yousefi, M. Human umbilical cord mesenchymal stem cells derived-exosomes in diseases treatment. Life Sci. 2019, 233, 116733. [Google Scholar] [CrossRef]
- Xunian, Z.; Kalluri, R. Biology and therapeutic potential of mesenchymal stem cell-derived exosomes. Cancer Sci. 2020, 111, 3100–3110. [Google Scholar] [CrossRef]
- Mendt, M.; Rezvani, K.; Shpall, E. Mesenchymal stem cell-derived exosomes for clinical use. Bone Marrow Transplant. 2019, 54, 789–792. [Google Scholar] [CrossRef]
- Ohno, S.-I.; Takanashi, M.; Sudo, K.; Ueda, S.; Ishikawa, A.; Matsuyama, N.; Fujita, K.; Mizutani, T.; Ohgi, T.; Ochiya, T.; et al. Systemically Injected Exosomes Targeted to EGFR Deliver Antitumor MicroRNA to Breast Cancer Cells. Mol. Ther. 2013, 21, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Shibayama, Y.; Kondo, T.; Ohya, H.; Fujisawa, S.-I.; Teshima, T.; Iseki, K. Upregulation of microRNA-126-5p is associated with drug resistance to cytarabine and poor prognosis in AML patients. Oncol. Rep. 2015, 33, 2176–2182. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.-X.; Zhang, K.; Shen, B.-B.; Li, J.-N. Mesenchymal stem cell-derived exosomes for gastrointestinal cancer. World J. Gastrointest. Oncol. 2021, 13, 1981–1996. [Google Scholar] [CrossRef]
- Zhang, F.; Guo, J.; Zhang, Z.; Qian, Y.; Wang, G.; Duan, M.; Zhao, H.; Yang, Z.; Jiang, X. Mesenchymal stem cell-derived exosome: A tumor regulator and carrier for targeted tumor therapy. Cancer Lett. 2021, 526, 29–40. [Google Scholar] [CrossRef]
- Pakravan, K.; Babashah, S.; Sadeghizadeh, M.; Mowla, S.; Mossahebi-Mohammadi, M.; Ataei, F.; Dana, N.; Javan, M. MicroRNA-100 shuttled by mesenchymal stem cell-derived exosomes suppresses in vitro angiogenesis through modulating the mTOR/HIF-1alpha/VEGF signaling axis in breast cancer cells. Cell Oncol. 2017, 40, 457–470. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, L.L.; Yao, J.L.; Wang, K.; Ai, H. Human Umbilical Cord Mesenchymal Stem Cell-Derived Extracellular Vesicles Inhibit Endometrial Cancer Cell Proliferation and Migration through Delivery of Exogenous miR-302a. Stem Cells Int. 2019, 2019, 8108576. [Google Scholar] [CrossRef]
- Lou, G.; Chen, L.; Xia, C.; Wang, W.; Qi, J.; Li, A.; Zhao, L.; Chen, Z.; Zheng, M.; Liu, Y. MiR-199a-modified exosomes from adipose tissue-derived mesenchymal stem cells improve hepatocellular carcinoma chemosensitivity through mTOR pathway. J. Exp. Clin. Cancer Res. 2020, 39, 4. [Google Scholar] [CrossRef] [PubMed]
- Kamerkar, S.; LeBleu, V.S.; Sugimoto, H.; Yang, S.; Ruivo, C.F.; Melo, S.A.; Lee, J.J.; Kalluri, R. Exosomes facilitate therapeutic targeting of oncogenic KRAS in pancreatic cancer. Nature 2017, 546, 498–503. [Google Scholar] [CrossRef]
- Shang, S.; Wang, J.; Chen, S.; Tian, R.; Zeng, H.; Wang, L.; Xia, M.; Zhu, H.; Zuo, C. Exosomal miRNA-1231 derived from bone marrow mesenchymal stem cells inhibits the activity of pancreatic cancer. Cancer Med. 2019, 8, 7728–7740. [Google Scholar] [CrossRef]
- Wu, D.-M.; Wen, X.; Han, X.-R.; Wang, S.; Wang, Y.-J.; Shen, M.; Fan, S.-H.; Zhang, Z.-F.; Shan, Q.; Li, M.-Q.; et al. RETRACTED: Bone Marrow Mesenchymal Stem Cell-Derived Exosomal MicroRNA-126-3p Inhibits Pancreatic Cancer Development by Targeting ADAM9. Mol. Ther. Nucleic Acids 2019, 16, 229–245. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, N.; Wei, Y.; Zhou, D.; Lin, R.; Wang, X.; Shi, B. Anticancer effects of miR-124 delivered by BM-MSC derived exosomes on cell proliferation, epithelial mesenchymal transition, and chemotherapy sensitivity of pancreatic cancer cells. Aging 2020, 12, 19660–19676. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Xu, Y.; Wei, Y.; Lv, L.; Liu, N.; Lin, R.; Wang, X.; Shi, B. Human Mesenchymal Stem Cell-Derived Exosomal microRNA-143 Promotes Apoptosis and Suppresses Cell Growth in Pancreatic Cancer via Target Gene Regulation. Front. Genet. 2021, 12, 581694. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Ji, J.; Chen, X.; Xu, W.; Chen, H.; Zhu, S.; Wu, J.; Wu, Y.; Sun, Y.; Sai, W.Z. Human umbilical cord mesenchymal stem cell-derived exosomes carrying hsa-miRNA-128-3p suppress pancreatic ductal cell carcinoma by inhibiting Galectin-3. Clin. Transl. Oncol. 2022, 24, 517–531. [Google Scholar] [CrossRef]
- Yao, X.; Mao, Y.; Wu, D.; Zhu, Y.; Lu, J.; Huang, Y.; Guo, Y.; Wang, Z.; Zhu, S.; Li, X. Exosomal circ_0030167 derived from BM-MSCs inhibits the invasion, migration, proliferation and stemness of pancreatic cancer cells by sponging miR-338-5p and targeting the Wif1/Wnt8/beta-catenin axis. Cancer Lett. 2021, 512, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Cao, F.; Sun, H.; Wang, Y.; Liu, S.; Wu, Y.; Cui, Q.; Mei, W.; Li, F. Exosomes derived from human umbilical cord mesenchymal stromal cells deliver exogenous miR-145-5p to inhibit pancreatic ductal adenocarcinoma progression. Cancer Lett. 2019, 442, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Pessina, A.; Bonomi, A.; Coccè, V.; Invernici, G.; Navone, S.; Cavicchini, L.; Sisto, F.; Ferrari, M.; Viganò, L.; Locatelli, A.; et al. Mesenchymal Stromal Cells Primed with Paclitaxel Provide a New Approach for Cancer Therapy. PLoS ONE 2011, 6, e28321. [Google Scholar] [CrossRef]
- Bonomi, A.; Coccè, V.; Cavicchini, L.; Sisto, F.; Dossena, M.; Balzarini, P.; Portolani, N.; Ciusani, E.; Parati, E.; Alessandri, G.; et al. Adipose Tissue-Derived Stromal Cells Primed in Vitro with Paclitaxel Acquire Anti-Tumor Activity. Int. J. Immunopathol. Pharmacol. 2013, 26, 33–41. [Google Scholar] [CrossRef]
- Pessina, A.; Cocce, V.; Bonomi, A.; Cavicchini, L.; Sisto, F.; Ferrari, M.; Ciusani, E.; Navone, S.; Marfia, G.; Parati, E.; et al. Human skin-derived fibroblasts acquire in vitro anti-tumor potential after priming with Paclitaxel. Anticancer Agents Med. Chem. 2013, 13, 523–530. [Google Scholar]
- Babajani, A.; Soltani, P.; Jamshidi, E.; Farjoo, M.H.; Niknejad, H. Recent Advances on Drug-Loaded Mesenchymal Stem Cells With Anti-neoplastic Agents for Targeted Treatment of Cancer. Front. Bioeng. Biotechnol. 2020, 8, 748. [Google Scholar] [CrossRef]
- Pessina, A.; Coccè, V.; Pascucci, L.; Bonomi, A.; Cavicchini, L.; Sisto, F.; Ferrari, M.; Ciusani, E.; Crovace, A.; Falchetti, M.L.; et al. Mesenchymal stromal cells primed with Paclitaxel attract and kill leukaemia cells, inhibit angiogenesis and improve survival of leukaemia-bearing mice. Br. J. Haematol. 2013, 160, 766–778. [Google Scholar] [CrossRef]
- Bonomi, A.; Steimberg, N.; Benetti, A.; Berenzi, A.; Alessandri, G.; Pascucci, L.; Boniotti, J.; Coccè, V.; Sordi, V.; Pessina, A.; et al. Paclitaxel-releasing mesenchymal stromal cells inhibit the growth of multiple myeloma cells in a dynamic 3D culture system. Hematol. Oncol. 2017, 35, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Varghese, A.M. Chimeric antigen receptor (CAR) T and other T cell strategies for pancreas adenocarcinoma. Chin. Clin. Oncol. 2017, 6, 66. [Google Scholar] [CrossRef] [PubMed]
- Bonomi, A.; Silini, A.; Vertua, E.; Signoroni, P.B.; Coccè, V.; Cavicchini, L.; Sisto, F.; Alessandri, G.; Pessina, A.; Parolini, O. Human amniotic mesenchymal stromal cells (hAMSCs) as potential vehicles for drug delivery in cancer therapy: An in vitro study. Stem Cell Res. Ther. 2015, 6, 155. [Google Scholar] [CrossRef] [PubMed]
- Brini, A.; Cocce, V.; Ferreira, L.; Giannasi, C.; Cossellu, G.; Gianni, A.; Angiero, F.; Bonomi, A.; Pascucci, L.; Falchetti, M. Cell-mediated drug delivery by gingival interdental papilla mesenchymal stromal cells (GinPa-MSCs) loaded with paclitaxel. Expert Opin. Drug Deliv. 2016, 13, 789–798. [Google Scholar] [CrossRef]
- Bonomi, A.; Sordi, V.; Dugnani, E.; Ceserani, V.; Dossena, M.; Coccè, V.; Cavicchini, L.; Ciusani, E.; Bondiolotti, G.; Piovani, G.; et al. Gemcitabine-releasing mesenchymal stromal cells inhibit in vitro proliferation of human pancreatic carcinoma cells. Cytotherapy 2015, 17, 1687–1695. [Google Scholar] [CrossRef]
- Eltoukhy, H.S.; Sinha, G.; Moore, C.A.; Sandiford, O.A.; Rameshwar, P. Immune modulation by a cellular network of mesenchymal stem cells and breast cancer cell subsets: Implication for cancer therapy. Cell. Immunol. 2018, 326, 33–41. [Google Scholar] [CrossRef]
- Haney, M.; Klyachko, N.; Zhao, Y.; Gupta, R.; Plotnikova, E.; He, Z.; Patel, T.; Piroyan, A.; Sokolsky, M.; Kabanov, A. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J. Control. Release 2015, 207, 18–30. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhou, W.; Chen, X.; Wang, Q.; Li, C.; Chen, Q.; Zhang, Y.; Lu, Y.; Ding, X.; Jiang, C. Bone marrow mesenchymal stem cells-derived exosomes for penetrating and targeted chemotherapy of pancreatic cancer. Acta Pharm. Sin. B 2020, 10, 1563–1575. [Google Scholar] [CrossRef]
- Zhou, W.; Zhou, Y.; Chen, X.; Ning, T.; Chen, H.; Guo, Q.; Zhang, Y.; Liu, P.; Zhang, Y.; Li, C.; et al. Pancreatic cancer-targeting exosomes for enhancing immunotherapy and reprogramming tumor microenvironment. Biomaterials 2021, 268, 120546. [Google Scholar] [CrossRef]
- Jiang, M.; Liu, Z.; Xiang, Y.; Ma, H.; Liu, S.; Liu, Y.; Zheng, D. Synergistic antitumor effect of AAV-mediated TRAIL expression combined with cisplatin on head and neck squamous cell carcinoma. BMC Cancer 2011, 11, 54. [Google Scholar] [CrossRef]
- Breitbach, C.J.; Burke, J.; Jonker, D.; Stephenson, J.; Haas, A.R.; Chow, L.Q.M.; Nieva, J.; Hwang, T.-H.; Moon, A.; Patt, R.; et al. Intravenous delivery of a multi-mechanistic cancer-targeted oncolytic poxvirus in humans. Nature 2011, 477, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Porter, D.L.; Levine, B.L.; Kalos, M.; Bagg, A.; June, C.H. Chimeric Antigen Receptor–Modified T Cells in Chronic Lymphoid Leukemia. N. Engl. J. Med. 2011, 365, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Mader, E.K.; Maeyama, Y.; Lin, Y.; Butler, G.W.; Russell, H.M.; Galanis, E.; Russell, S.J.; Dietz, A.B.; Peng, K.-W. Mesenchymal Stem Cell Carriers Protect Oncolytic Measles Viruses from Antibody Neutralization in an Orthotopic Ovarian Cancer Therapy Model. Clin. Cancer Res. 2009, 15, 7246–7255. [Google Scholar] [CrossRef]
- Dembinski, J.; Spaeth, E.L.; Fueyo, J.; Gomez-Manzano, C.; Studeny, M.; Andreeff, M.; Marini, F.C. Reduction of nontarget infection and systemic toxicity by targeted delivery of conditionally replicating viruses transported in mesenchymal stem cells. Cancer Gene Ther. 2010, 17, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Gumin, J.; Gao, F.; Hossain, A.; Shpall, E.J.; Kondo, A.; Kerrigan, B.C.P.; Yang, J.; Ledbetter, D.; Fueyo, J.; et al. Characterization of patient-derived bone marrow human mesenchymal stem cells as oncolytic virus carriers for the treatment of glioblastoma. J. Neurosurg. 2022, 136, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Hammer, K.; Kazcorowski, A.; Liu, L.; Behr, M.; Schemmer, P.; Herr, I.; Nettelbeck, D.M. Engineered adenoviruses combine enhanced oncolysis with improved virus production by mesenchymal stromal carrier cells. Int. J. Cancer 2015, 137, 978–990. [Google Scholar] [CrossRef]
- Kaczorowski, A.; Hammer, K.; Liu, L.; Villhauer, S.; Nwaeburu, C.; Fan, P.; Zhao, Z.; Gladkich, J.; Groß, W.; Nettelbeck, D.M.; et al. Delivery of improved oncolytic adenoviruses by mesenchymal stromal cells for elimination of tumorigenic pancreatic cancer cells. Oncotarget 2016, 7, 9046–9059. [Google Scholar] [CrossRef]
- Na, Y.; Nam, J.-P.; Hong, J.; Oh, E.; Shin, H.C.; Kim, H.S.; Kim, S.W.; Yun, C.-O. Systemic administration of human mesenchymal stromal cells infected with polymer-coated oncolytic adenovirus induces efficient pancreatic tumor homing and infiltration. J. Control. Release 2019, 305, 75–88. [Google Scholar] [CrossRef]
- Whiteside, T.L. Exosome and mesenchymal stem cell cross-talk in the tumor microenvironment. Semin. Immunol. 2018, 35, 69–79. [Google Scholar] [CrossRef]
- Harrell, C.R.; Volarevic, A.; Djonov, V.G.; Jovicic, N.; Volarevic, V. Mesenchymal Stem Cell: A Friend or Foe in Anti-Tumor Immunity. Int. J. Mol. Sci. 2021, 22, 12429. [Google Scholar] [CrossRef]
- Nieman, K.M.; Kenny, H.A.; Penicka, C.V.; Ladanyi, A.; Buell-Gutbrod, R.; Zillhardt, M.R.; Romero, I.L.; Carey, M.S.; Mills, G.B.; Hotamisligil, G.S.; et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat. Med. 2011, 17, 1498–1503. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Sakaguchi, M.; Maruyama, S.; Iioka, H.; Putranto, E.W.; Sumardika, I.W.; Tomonobu, N.; Kawasaki, T.; Homma, K.; Kondo, E. Stromal mesenchymal stem cells facilitate pancreatic cancer progression by regulating specific secretory molecules through mutual cellular interaction. J. Cancer 2018, 9, 2916–2929. [Google Scholar] [CrossRef] [PubMed]
- Corsten, M.F.; Shah, K. Therapeutic stem-cells for cancer treatment: Hopes and hurdles in tactical warfare. Lancet Oncol. 2008, 9, 376–384. [Google Scholar] [CrossRef]
- Waghray, M.; Yalamanchili, M.; Dziubinski, M.; Zeinali, M.; Erkkinen, M.; Yang, H.; Schradle, K.A.; Urs, S.; Di Magliano, M.P.; Welling, T.H.; et al. GM-CSF Mediates Mesenchymal–Epithelial Cross-talk in Pancreatic Cancer. Cancer Discov. 2016, 6, 886–899. [Google Scholar] [CrossRef]
- Belli, C.; Trapani, D.; Viale, G.; D’Amico, P.; Duso, B.A.; Della Vigna, P.; Orsi, F.; Curigliano, G. Targeting the microenvironment in solid tumors. Cancer Treat. Rev. 2018, 65, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Quante, M.; Tu, S.P.; Tomita, H.; Gonda, T.; Wang, S.S.; Takashi, S.; Baik, G.H.; Shibata, W.; DiPrete, B.; Betz, K.S.; et al. Bone Marrow-Derived Myofibroblasts Contribute to the Mesenchymal Stem Cell Niche and Promote Tumor Growth. Cancer Cell 2011, 19, 257–272. [Google Scholar] [CrossRef]
- Catalano, V.; Turdo, A.; Di Franco, S.; Dieli, F.; Todaro, M.; Stassi, G. Tumor and its microenvironment: A synergistic interplay. Semin. Cancer Biol. 2013, 23, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Giannoni, E.; Bianchini, F.; Masieri, L.; Serni, S.; Torre, E.; Calorini, L.; Chiarugi, P. Reciprocal Activation of Prostate Cancer Cells and Cancer-Associated Fibroblasts Stimulates Epithelial-Mesenchymal Transition and Cancer Stemness. Cancer Res. 2010, 70, 6945–6956. [Google Scholar] [CrossRef]
- Kidd, S.; Spaeth, E.; Watson, K.; Burks, J.; Lu, H.; Klopp, A.; Andreeff, M.; Marini, F.C. Origins of the Tumor Microenvironment: Quantitative Assessment of Adipose-Derived and Bone Marrow–Derived Stroma. PLoS ONE 2012, 7, e30563. [Google Scholar] [CrossRef]
- Zhou, H.; Su, X.; Fu, X.; Wu, G.; Luo, K.; Fang, Z.; Yu, F.; Liu, H.; Hu, H.; Chen, L. Mesenchymal stem cells promote pancreatic adenocarcinoma cells invasion by transforming growth factor-beta1 induced epithelial-mesenchymal transition. Oncotarget 2016, 7, 41294–41305. [Google Scholar] [CrossRef]
- Ganguly, K.; Cox, J.; Ghersi, D.; Grandgenett, P.; Hollingsworth, M.; Jain, M.; Kumar, S.; Batra, S. Mucin 5AC-Mediated CD44/ITGB1 Clustering Mobilizes Adipose-Derived Mesenchymal Stem Cells to Modulate Pancreatic Cancer Stromal Heterogeneity. Gastroenterology 2022, 162, 2032–2046.e2012. [Google Scholar] [CrossRef]
- Miyazaki, Y.; Oda, T.; Mori, N.; Kida, Y. Adipose-derived mesenchymal stem cells differentiate into pancreatic cancer-associated fibroblasts in vitro. FEBS Open Bio. 2020, 10, 2268–2281. [Google Scholar] [CrossRef]
- Kabashima-Niibe, A.; Higuchi, H.; Takaishi, H.; Masugi, Y.; Matsuzaki, Y.; Mabuchi, Y.; Funakoshi, S.; Adachi, M.; Hamamoto, Y.; Kawachi, S.; et al. Mesenchymal stem cells regulate epithelial-mesenchymal transition and tumor progression of pancreatic cancer cells. Cancer Sci. 2013, 104, 157–164. [Google Scholar] [CrossRef]
- Beckermann, B.M.; Kallifatidis, G.; Groth, A.; Frommhold, D.; Apel, A.; Mattern, J.; Salnikov, A.V.; Moldenhauer, G.; Wagner, W.; Diehlmann, A.; et al. VEGF expression by mesenchymal stem cells contributes to angiogenesis in pancreatic carcinoma. Br. J. Cancer 2008, 99, 622–631. [Google Scholar] [CrossRef] [PubMed]
- DeNardo, D.G.; Ruffell, B. Macrophages as regulators of tumour immunity and immunotherapy. Nat. Rev. Immunol. 2019, 19, 369–382. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Yu, Y.; Wang, X.; Zhang, T. Tumor-Associated Macrophages in Tumor Immunity. Front. Immunol. 2020, 11, 583084. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Zhou, Q.; Zheng, S.; Li, G.; Lin, Q.; Wei, L.; Fu, Z.; Zhang, B.; Liu, Y.; Li, Z. Tumor-associated macrophages promote progression and the Warburg effect via CCL18/NF-kB/VCAM-1 pathway in pancreatic ductal adenocarcinoma. Cell Death Dis. 2018, 9, 453. [Google Scholar] [CrossRef]
- Mathew, E.; Brannon, A.L.; Del Vecchio, A.; Garcia, P.E.; Penny, M.K.; Kane, K.T.; Vinta, A.; Buckanovich, R.J.; di Magliano, M.P. Mesenchymal Stem Cells Promote Pancreatic Tumor Growth by Inducing Alternative Polarization of Macrophages. Neoplasia 2016, 18, 142–151. [Google Scholar] [CrossRef]
- Ding, Y.; Mei, W.; Zheng, Z.; Cao, F.; Liang, K.; Jia, Y.; Wang, Y.; Liu, D.; Li, J.; Li, F. Exosomes secreted from human umbilical cord mesenchymal stem cells promote pancreatic ductal adenocarcinoma growth by transferring miR-100-5p. Tissue Cell 2021, 73, 101623. [Google Scholar] [CrossRef]
- Seebach, C.; Schultheiss, J.; Wilhelm, K.; Frank, J.; Henrich, D. Comparison of six bone-graft substitutes regarding to cell seeding efficiency, metabolism and growth behaviour of human mesenchymal stem cells (MSC) in vitro. Injury 2010, 41, 731–738. [Google Scholar] [CrossRef]
- Roodhart, J.M.; Daenen, L.G.; Stigter, E.C.; Prins, H.-J.; Gerrits, J.; Houthuijzen, J.M.; Gerritsen, M.G.; Schipper, H.S.; Backer, M.J.; van Amersfoort, M.; et al. Mesenchymal Stem Cells Induce Resistance to Chemotherapy through the Release of Platinum-Induced Fatty Acids. Cancer Cell 2011, 20, 370–383. [Google Scholar] [CrossRef]
- Wang, J.; Hendrix, A.; Hernot, S.; Lemaire, M.; De Bruyne, E.; Van Valckenborgh, E.; Lahoutte, T.; De Wever, O.; Vanderkerken, K.; Menu, E. Bone marrow stromal cell–derived exosomes as communicators in drug resistance in multiple myeloma cells. Blood 2014, 124, 555–566. [Google Scholar] [CrossRef]
- Ji, R.; Zhang, B.; Zhang, X.; Xue, J.; Yuan, X.; Yan, Y.; Wang, M.; Zhu, W.; Qian, H.; Xu, W. Exosomes derived from human mesenchymal stem cells confer drug resistance in gastric cancer. Cell Cycle 2015, 14, 2473–2483. [Google Scholar] [CrossRef]
- Cheng, D.; Fan, J.; Qin, K.; Zhou, Y.; Yang, J.; Ma, Y.; Shi, M.; Jin, J. LncRNA SNHG7 Regulates Mesenchymal Stem Cell Through the Notch1/Jagged1/Hes-1 Signaling Pathway and Influences Folfirinox Resistance in Pancreatic Cancer. Front. Oncol. 2021, 11, 719855. [Google Scholar] [CrossRef]
- Bao, Q.; Zhao, Y.; Niess, H.; Conrad, C.; Schwarz, B.; Jauch, K.-W.; Huss, R.; Nelson, P.J.; Bruns, C.J. Mesenchymal Stem Cell-Based Tumor-Targeted Gene Therapy in Gastrointestinal Cancer. Stem Cells Dev. 2012, 21, 2355–2363. [Google Scholar] [CrossRef]
- Barbash, I.; Chouraqui, P.; Baron, J.; Feinberg, M.; Etzion, S.; Tessone, A.; Miller, L.; Guetta, E.; Zipori, D.; Kedes, L. Systemic delivery of bone marrow-derived mesenchymal stem cells to the infarcted myocardium: Feasibility, cell migration, and body distribution. Circulation 2003, 108, 863–868. [Google Scholar] [CrossRef] [PubMed]
- Kraitchman, D.L.; Tatsumi, M.; Gilson, W.D.; Ishimori, T.; Kedziorek, D.; Walczak, P.; Segars, W.P.; Chen, H.H.; Fritzges, D.; Izbudak, I.; et al. Dynamic Imaging of Allogeneic Mesenchymal Stem Cells Trafficking to Myocardial Infarction. Circulation 2005, 112, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- Fischer, U.M.; Harting, M.T.; Jimenez, F.; Monzon-Posadas, W.O.; Xue, H.; Savitz, S.I.; Laine, G.A.; Cox, C.S., Jr. Pulmonary Passage is a Major Obstacle for Intravenous Stem Cell Delivery: The Pulmonary First-Pass Effect. Stem Cells Dev. 2009, 18, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Assis, A.C.M.; Carvalho, J.; Jacoby, B.A.; Ferreira, R.L.B.; Castanheira, P.; Diniz, S.O.F.; Cardoso, V.N.; Goes, A.M.; Ferreira, A.J. Time-Dependent Migration of Systemically Delivered Bone Marrow Mesenchymal Stem Cells to the Infarcted Heart. Cell Transplant. 2010, 19, 219–230. [Google Scholar] [CrossRef]
- Lee, R.H.; Yoon, N.; Reneau, J.C.; Prockop, D.J. Preactivation of Human MSCs with TNF-α Enhances Tumor-Suppressive Activity. Cell Stem Cell 2012, 11, 825–835. [Google Scholar] [CrossRef]
- Miloradovic, D.; Miloradovic, D.; Markovic, B.S.; Acovic, A.; Harrell, C.R.; Djonov, V.; Arsenijevic, N.; Volarevic, V. The Effects of Mesenchymal Stem Cells on Antimelanoma Immunity Depend on the Timing of Their Administration. Stem Cells Int. 2020, 2020, 8842659. [Google Scholar] [CrossRef]
- Allen, M.; Louise Jones, J. Jekyll and Hyde: The role of the microenvironment on the progression of cancer. J. Pathol. 2011, 223, 163–177. [Google Scholar] [CrossRef]
- D’Aloia, M.M.; Zizzari, I.G.; Sacchetti, B.; Pierelli, L.; Alimandi, M. CAR-T cells: The long and winding road to solid tumors. Cell Death Dis. 2018, 9, 282. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, M.; Wu, Z.; Tong, C.; Dai, H.; Guo, Y.; Liu, Y.; Huang, J.; Lv, H.; Luo, C.; et al. CD133-directed CAR T cells for advanced metastasis malignancies: A phase I trial. Oncoimmunology 2018, 7, e1440169. [Google Scholar] [CrossRef] [PubMed]
- Beatty, G.; Haas, A.; Maus, M.; Torigian, D.; Soulen, M.; Plesa, G.; Chew, A.; Zhao, Y.; Levine, B.; Albelda, S. Mesothelin-specific chimeric antigen receptor mRNA-engineered T cells induce anti-tumor activity in solid malignancies. Cancer Immunol. Res. 2014, 2, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.M.; Chamberlain, G.; Ashton, B.A.; Middleton, J. Recent advances into the understanding of mesenchymal stem cell trafficking. Br. J. Haematol. 2007, 137, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, G.; Fox, J.; Ashton, B.; Middleton, J. Concise Review: Mesenchymal Stem Cells: Their Phenotype, Differentiation Capacity, Immunological Features, and Potential for Homing. Stem Cells 2007, 25, 2739–2749. [Google Scholar] [CrossRef] [PubMed]
- Fujita, Y.; Kadota, T.; Araya, J.; Ochiya, T.; Kuwano, K. Clinical Application of Mesenchymal Stem Cell-Derived Extracellular Vesicle-Based Therapeutics for Inflammatory Lung Diseases. J. Clin. Med. 2018, 7, 355. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).