SOXC Transcription Factors as Diagnostic Biomarkers and Therapeutic Targets for Arthritis
Abstract
:1. Introduction
2. SOXC Transcription Factors under In Vivo Inflammatory Conditions Associated with Arthritis
3. SOXC Transcription Factors as Potential Diagnostic Biomarkers of Arthritis
3.1. SOX4 as a Potential Diagnostic Biomarker of Osteoarthritis
3.2. SOX4 as a Potential Diagnostic Biomarker of Rheumatoid Arthritis
3.3. SOX11 Is Dysregulated during Osteoarthritis
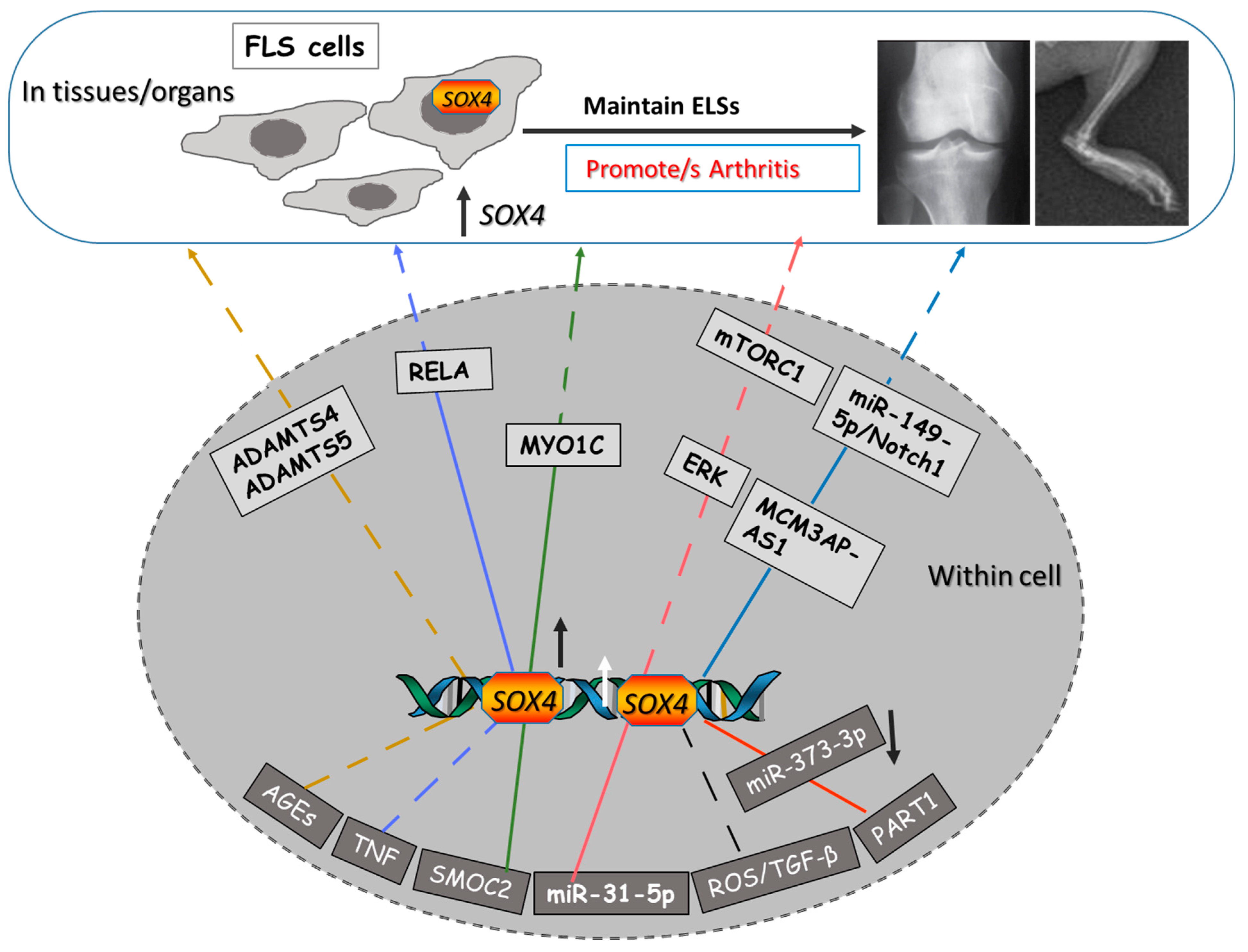
4. Signaling Mechanisms Involved in SOXC TFs Promoting Arthritis
5. SOX4 as a Therapeutic Target of Arthritis
6. Upstream Molecules That Can Target SOX4 to Treat Arthritis
7. Transcriptional Activity of SOX4 in Arthritis
8. SOX4 and Its Implications in Osteoporosis
9. SOX4 Involvement in Other Autoimmune Disorders
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pap, T.; Korb-Pap, A. Cartilage damage in osteoarthritis and rheumatoid arthritis—Two unequal siblings. Nat. Rev. Rheumatol. 2015, 11, 606–615. [Google Scholar] [CrossRef]
- Koopman, P.; Gubbay, J.; Vivian, N.; Goodfellow, P.; Lovell-Badge, R. Male development of chromosomally female mice transgenic for Sry. Nature 1991, 351, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Kamachi, Y.; Kondoh, H. Sox proteins: Regulators of cell fate specification and differentiation. Development 2013, 140, 4129–4144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.-J.; Jiang, D.-M. LncRNA PART1 modulates chondrocyte proliferation, apoptosis, and extracellular matrix degradation in osteoarthritis via regulating miR-373-3p/SOX4 axis. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 8175–8185. [Google Scholar] [PubMed]
- Ye, X.; Yin, C.; Huang, X.; Huang, Y.; Ding, L.; Jin, M.; Wang, Z.; Wei, J.; Li, X. ROS/TGF-β signal mediated accumulation of SOX4 in OA-FLS promotes cell senescence. Exp. Gerontol. 2021, 156, 111616. [Google Scholar] [CrossRef]
- Xiong, X.; Liu, L.; Xu, F.; Wu, X.; Yin, Z.; Dong, Y.; Qian, P. Feprazone Ameliorates TNF-α-Induced Loss of Aggrecan via Inhibition of the SOX-4/ADAMTS-5 Signaling Pathway. ACS Omega 2021, 6, 7638–7645. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Hu, Q.-F.; Li, J.; Shi, C.-J.; Luo, J.-W.; Tian, W.-C.; Pan, L.-W. SOX4-activated lncRNA MCM3AP-AS1 aggravates osteoarthritis progression by modulating miR-149-5p/Notch1 signaling. Cytokine 2022, 152, 155805. [Google Scholar] [CrossRef]
- Takahata, Y.; Nakamura, E.; Hata, K.; Wakabayashi, M.; Murakami, T.; Wakamori, K.; Yoshikawa, H.; Matsuda, A.; Fukui, N.; Nishimura, R. Sox4 is involved in osteoarthritic cartilage deterioration through induction of ADAMTS4 and ADAMTS5. FASEB J. 2019, 33, 619–630. [Google Scholar] [CrossRef]
- Xu, F.; Lv, Y.-M.; Wang, H.-B.; Song, Y.-C. miR-31-5p/SOX4 Axis Affects Autophagy and Apoptosis of Chondrocytes by Regulating Extracellular Regulated Protein Kinase/Mechanical Target of Rapamycin Kinase Signalling. Pathobiology 2022, 89, 63–73. [Google Scholar] [CrossRef]
- Jones, K.; Ramirez-Perez, S.; Niu, S.; Gangishetti, U.; Drissi, H.; Bhattaram, P. SOX4 and RELA Function as Transcriptional Partners to Regulate the Expression of TNF- Responsive Genes in Fibroblast-Like Synoviocytes. Front. Immunol. 2022, 13, 789349. [Google Scholar] [CrossRef]
- A Ahmed, E.; Ibrahim, H.-I.M.; Khalil, H.E. Pinocembrin Reduces Arthritic Symptoms in Mouse Model via Targeting Sox4 Signaling Molecules. J. Med. Food 2021, 24, 282–291. [Google Scholar] [CrossRef]
- Xu, S.; Yu, J.; Wang, Z.; Ni, C.; Xia, L.; Tang, T. SOX11 promotes osteoarthritis through induction of TNF-α. Pathol. Res. Pr. 2019, 215, 152442. [Google Scholar] [CrossRef] [PubMed]
- Kan, A.; Ikeda, T.; Fukai, A.; Nakagawa, T.; Nakamura, K.; Chung, U.-I.; Kawaguchi, H.; Tabin, C.J. SOX11 contributes to the regulation of GDF5 in joint maintenance. BMC Dev. Biol. 2013, 13, 4. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Fan, J.; Ding, X.; Sun, Y.; Cui, Z.; Liu, W. Tanshinone I Inhibits IL-1β-Induced Apoptosis, Inflammation And Extracellular Matrix Degradation In Chondrocytes CHON-001 Cells And Attenuates Murine Osteoarthritis. Drug Des. Dev. Ther. 2019, ume 13, 3559–3568. [Google Scholar] [CrossRef] [Green Version]
- Pan, W.; Wang, H.; Ruan, J.; Zheng, W.; Chen, F.; Kong, J.; Wang, Y. lncRNA myocardial infarction-associated transcript (MIAT) knockdown alleviates LPS-induced chondrocytes inflammatory injury via regulating miR-488-3p/sex determining region Y-related HMG-box 11 (SOX11) axis. Open Life Sci. 2021, 16, 511–522. [Google Scholar] [CrossRef]
- Yi, P.; Xu, X.; Yao, J.; Qiu, B. Analysis of mRNA Expression and DNA Methylation Datasets According to the Genomic Distribution of CpG Sites in Osteoarthritis. Front. Genet. 2021, 12, 618803. [Google Scholar] [CrossRef] [PubMed]
- Yoshitomi, H.; Kobayashi, S.; Miyagawa-Hayashino, A.; Okahata, A.; Doi, K.; Nishitani, K.; Murata, K.; Ito, H.; Tsuruyama, T.; Haga, H.; et al. Human Sox4 facilitates the development of CXCL13-producing helper T cells in inflammatory environments. Nat. Commun. 2018, 9, 3762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lefebvre, V.; Bhattaram, P. SOXC Genes and the Control of Skeletogenesis. Curr. Osteoporos. Rep. 2016, 14, 32–38. [Google Scholar] [CrossRef] [Green Version]
- Pitzalis, C.; Jones, G.W.; Bombardieri, M.; Jones, S.A. Ectopic lymphoid-like structures in infection, cancer and autoimmunity. Nat. Rev. Immunol. 2014, 14, 447–462. [Google Scholar] [CrossRef]
- Gu-Trantien, C.; Loi, S.; Garaud, S.; Equeter, C.; Libin, M.; de Wind, A.; Ravoet, M.; Le Buanec, H.; Sibille, C.; Manfouo-Foutsop, G.; et al. CD4(+) follicular helper T cell infiltration predicts breast cancer survival. J. Clin. Investig. 2013, 123, 2873–2892. [Google Scholar] [CrossRef] [Green Version]
- Corsiero, E.; Nerviani, A.; Bombardieri, M.; Pitzalis, C. Ectopic Lymphoid Structures: Powerhouse of Autoimmunity. Front. Immunol. 2016, 7, 430. [Google Scholar] [CrossRef] [Green Version]
- Nerviani, A.; Pitzalis, C. Role of chemokines in ectopic lymphoid structures formation in autoimmunity and cancer. J. Leukoc. Biol. 2018, 104, 333–341. [Google Scholar] [CrossRef] [Green Version]
- Bhattaram, P.; Muschler, G.; Wixler, V.; Lefebvre, V. Inflammatory Cytokines Stabilize SOXC Transcription Factors to Mediate the Transformation of Fibroblast-Like Synoviocytes in Arthritic Disease. Arthritis Rheumatol. 2018, 70, 371–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanieh, H.; Ahmed, E.A.; Vishnubalaji, R.; Alajez, N.M. SOX4: Epigenetic regulation and role in tumorigenesis. Semin. Cancer Biol. 2019, 67, 91–104. [Google Scholar] [CrossRef]
- Nygaard, G.; Firestein, G.S. Restoring synovial homeostasis in rheumatoid arthritis by targeting fibroblast-like synoviocytes. Nat. Rev. Rheumatol. 2020, 16, 316–333. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, R.E.; Foxwell, B.M. Signalling, Inflammation and Arthritis: NF-Kappab and its Relevance to Arthritis and Inflammation. Rheumatol (Oxf.) 2008, 47, 584–590. [Google Scholar] [CrossRef] [Green Version]
- Komatsu, N.; Okamoto, K.; Sawa, S.; Nakashima, T.; Oh-Hora, M.; Kodama, T.; Tanaka, S.; A Bluestone, J.; Takayanagi, H. Pathogenic conversion of Foxp3+ T cells into TH17 cells in autoimmune arthritis. Nat. Med. 2014, 20, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Di Liu, D.; Li, R.; Xu, S.; Shi, M.; Kuang, Y.; Wang, J.; Shen, C.; Qiu, Q.; Liang, L.; Xiao, Y.; et al. SMOC2 promotes aggressive behavior of fibroblast-like synoviocytes in rheumatoid arthritis through transcriptional and post-transcriptional regulating MYO1C. Cell Death Dis. 2022, 13, 1035. [Google Scholar] [CrossRef]
- Xu, L.; Shunmei, E.; Lin, S.; Hou, Y.; Lin, W.; He, W.; Wang, H.; Li, G. Sox11-modified mesenchymal stem cells accelerate cartilage defect repair in SD rats. Cell Tissue Res. 2019, 376, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Iliopoulos, D.; Malizos, K.N.; Oikonomou, P.; Tsezou, A. Integrative MicroRNA and Proteomic Approaches Identify Novel Osteoarthritis Genes and Their Collaborative Metabolic and Inflammatory Networks. PLoS ONE 2008, 3, e3740. [Google Scholar] [CrossRef]
- Sock, E.; Rettig, S.D.; Enderich, J.; Bösl, M.R.; Tamm, E.R.; Wegner, M. Gene targeting reveals a widespread role for the high-mobility-group transcription factor Sox11 in tissue remodeling. Mol. Cell Biol. 2004, 24, 6635–6644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishimura, R.; Hata, K.; Takahata, Y.; Murakami, T.; Nakamura, E.; Ohkawa, M.; Ruengsinpinya, L. Role of Signal Transduction Pathways and Transcription Factors in Cartilage and Joint Diseases. Int. J. Mol. Sci. 2020, 21, 1340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Ma, H.; Zhang, H.; Deng, C.; Xin, P. Recent advances on signaling pathways and their inhibitors in rheumatoid arthritis. Clin. Immunol. 2021, 230, 108793. [Google Scholar] [CrossRef]
- Kato, K.; Bhattaram, P.; Penzo-Méndez, A.; Gadi, A.; Lefebvre, V. SOXC Transcription Factors Induce Cartilage Growth Plate Formation in Mouse Embryos by Promoting Noncanonical WNT Signaling. J. Bone Miner Res. 2015, 30, 1560–1571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pap, T.; Dankbar, B.; Wehmeyer, C.; Korb-Pap, A.; Sherwood, J. Synovial fibroblasts and articular tissue remodelling: Role and mechanisms. Semin. Cell Dev. Biol. 2020, 101, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Ngondo, R.P.; Carbon, P. Transcription factor abundance controlled by an auto-regulatory mechanism involving a transcription start site switch. Nucleic Acids Res. 2014, 42, 2171–2184. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Gu, Z.; He, Y.; Wang, C.; Duan, J. The effect of SOX4 gene 3′UTR polymorphisms on osteoporosis. J. Orthop. Surg. Res. 2021, 16, 321. [Google Scholar] [CrossRef] [PubMed]
- Duncan, E.L.; Danoy, P.; Kemp, J.P.; Leo, P.J.; McCloskey, E.; Nicholson, G.C.; Eastell, R.; Prince, R.L.; Eisman, J.A.; Jones, G.; et al. Genome-wide association study using extreme truncate selection identifies novel genes affecting bone mineral density and fracture risk. PLoS Genet. 2011, 7, e1001372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nissen-Meyer, L.S.H.; Jemtland, R.; Gautvik, V.T.; Pedersen, M.E.; Paro, R.; Fortunati, D.; Pierroz, D.D.; Stadelmann, V.A.; Reppe, S.; Reinholt, F.P.; et al. Osteopenia, decreased bone formation and impaired osteoblast development in Sox4 heterozygous mice. J. Cell Sci. 2007, 120, 2785–2795. [Google Scholar] [CrossRef] [Green Version]
- Lefebvre, V. Roles and regulation of SOX transcription factors in skeletogenesis. Vertebr. Skelet. Dev. Curr. Top. Dev. Biol. 2019, 133, 171–193. [Google Scholar] [CrossRef]
- Kodrič, K.; Čamernik, K.; Černe, D.; Komadina, R.; Marc, J. P4 medicine and osteoporosis: A systematic review. Wien. Klin. Wochenschr. 2016, 128 (Suppl. 7), 480–491. [Google Scholar] [CrossRef] [PubMed]
- Panach, L.; Serna, E.; Tarín, J.J.; Cano, A.; García-Pérez, M.Á. A translational approach from an animal model identifies CD80 as a candidate gene for the study of bone phenotypes in postmenopausal women. Osteoporos. Int. 2017, 28, 2445–2455. [Google Scholar] [CrossRef]
- Kuwahara, M.; Yamashita, M.; Shinoda, K.; Tofukuji, S.; Onodera, A.; Shinnakasu, R.; Motohashi, S.; Hosokawa, H.; Tumes, D.; Iwamura, C.; et al. The Transcription Factor Sox4 Is a Downstream Target of Signaling by the Cytokine TGF-beta and Suppresses T(H)2 Differentiation. Nat. Immunol. 2012, 13, 778–786. [Google Scholar] [CrossRef] [Green Version]
- Gerner, M.C.; Ziegler, L.S.; Schmidt, R.L.J.; Krenn, M.; Zimprich, F.; Uyanik-Ünal, K.; Konstantopoulou, V.; Derdak, S.; Del Favero, G.; Schwarzinger, I.; et al. The TGF-b/SOX4 axis and ROS-driven autophagy co-mediate CD39 expression in regulatory T-cells. FASEB J. 2020, 34, 8367–8384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moncrieffe, H.; Nistala, K.; Hunter, P.; Kamhieh, Y.; Wedderburn, L. CD39: A regulatory role in childhood arthritis. Pediatr. Rheumatol. 2008, 6 (Suppl. 1), P10. [Google Scholar] [CrossRef] [Green Version]
- Hinrichs, A.C.; Blokland, S.L.M.; Lopes, A.P.; Wichers, C.G.K.; Kruize, A.A.; Pandit, A.; Radstake, T.R.D.J.; van Roon, J.A.G. Transcriptome Analysis of CCR9+ T Helper Cells From Primary Sjögren’s Syndrome Patients Identifies CCL5 as a Novel Effector Molecule. Front. Immunol. 2021, 12, 702733. [Google Scholar] [CrossRef]
- Jin, L.; Kawai, T.; Cha, S.; Yu, Q. Interleukin-7 Enhances the Th1 Response to Promote the Development of Sjögren’s Syndrome-like Autoimmune Exocrinopathy in Mice. Arthritis Rheum. 2013, 65, 2132–2142. [Google Scholar] [CrossRef] [Green Version]
- Potzner, M.R.; Griffel, C.; Lütjen-Drecoll, E.; Bösl, M.R.; Wegner, M.; Sock, E. Prolonged Sox4 Expression in Oligodendrocytes Interferes with Normal Myelination in the Central Nervous System. Mol. Cell. Biol. 2007, 27, 5316–5326. [Google Scholar] [CrossRef] [Green Version]
| I. SOX4 Function on OA | Experimental Model | Involved Downstream/Upstream Molecules | Ref. |
|---|---|---|---|
| SOX4 as a therapeutic target of OA | Chondrocytes cells and cartilage samples from patients and controls | PART1 mediates OA progression through regulating the miR-373-3p/SOX4 axis | [4] |
| SOX4 as an early diagnostic marker of OA and a novel therapeutic target | FLS cells | ROS/TGF-β-associated OA-FLS senescence | [5] |
| Through inhibiting SOX4, azilsartan prevents AGEs-induced degradation of aggrecan | Injured chondrocytes cell model | Upregulating SOX4 by AGEs is mediated by p38 | [6] |
| SOX4-activated lncRNA MCM3AP-AS1 aggravates OA progression | Cartilage tissues from the knee joint of OA patients and patients who underwent amputation but did not have OA | Activated lncRNA MCM3AP modulating miR-149-5p/Notch1 signaling | [7] |
| SOX4 is involved in OA cartilage deterioration, through the upregulation of ADAMTS4 and ADAMTS5 | Articular cell lines, mouse femoral head cartilage, and patient samples | SOX4 upregulates ADAMTS4 and Adamts5 via binding to the gene promoters | [8] |
| miR-31-5p promotes the survival and autophagy of OA chondrocytes | OA patients’ cartilage tissues | miR-31-5p inhibits the activation of mTORC1 in an ERK-dependent manner by the direct targeting and suppression of SOX4 | [9] |
| SOX4 protein is a target of a proinflammatory cytokine-initiated molecular axis enhancing arthritic lesions in synovial joints | Mice, FLS culture, and human synovium specimens from OA patients undergoing total knee arthroplasty | TNF and other pro-inflammatory cytokines | [23] |
| II. SOX4 Function on RA | |||
| SOX4 and RELA regulate the gene expression of TNF downstream signaling molecules leading to the FLS transformation of RA progression | FLS from wild type and mutant SOXC mice | NF-κB, RelA/p65, SOX4 and TNF | [10] |
| PCB reduces SOX4 which could then be a therapeutic drug in treatment of RA | adjuvant-induced arthritis mouse model | NF-κB, miR-132, miR-202-5p, and miR-7235 | [11] |
| exFoxp3 cells are transformed into TH17 cells that induce higher levels of SOX4 to promote inflammation in joints | Patients’ splenic, synovial tissues and blood cells, and mice | N.A. | [27] |
| SOX4 is upregulated in synovial CD4+ T cells and further correlates with ELS formation in the RA synovium of patients | Cultured T cell | SOX4 contributes to CXCL13 production and ELS formation at inflammatory sites in humans | [17] |
| As a downstream of SMCO2, SOX4 binds to MYOIC to enhance migration and invasion | human STs and FLSs cells | SMCO2 and MYOIC | [28] |
| SOX11 Function in OA | Experimental Model | Involved Downstream/Upstream Molecules | Ref. |
|---|---|---|---|
| SOX11 promotes osteoarthritis through the induction of TNF-α. | Chondrocytes CHON-001 cells and knee tissues from patients | IL-1β, TNF-α | [12] |
| SOX11 induces chondrogenesis and cartilage defect repair by regulating β-catenin. | Rat mesenchymal stem cells | β-catenin | [29] |
| SOX11 potentially regulates GDF5 expression and is then involved in the pathogenesis of osteoarthritis. | OA cell model | GDF5 | [13] |
| In OA patients, inflammatory cytokines stabilize the SOX11 protein in human inflamed synovium and FLS. | Cartilage tissues from the knee joint of OA patients or patients who underwent amputation but did not have OA | Activated lncRNA MCM3AP modulating miR-149-5p/Notch1 signaling. | [7] |
| Via targeting SOX4, tanshinone I inhibits IL-1β-induced inflammation and attenuates murine OA. | Chondrogenic cell line, OA murine model | IL-1β-induced collagen II, aggrecan degradation, SOX11 downregulation, and MMP-13 and p-NF-κB. | [14] |
| Upregulating miR-488-3p reduced the incidence of LPS-causing chondrocyte injury through inhibiting SOX11. | Knee cartilage and normal tissues | miR-488-3p and NF-κB | [15] |
| SOX11 promotes osteoarthritic cartilage deterioration via the induction of ADAMTS4 and ADAMTS5. | Mouse femoral head cartilage | SOX11 upregulated ADAMTS4 and Adamts5 gene promoter activities by binding to their gene promoters. | [8] |
| Higher SOX11 mRNA levels in OA could be related to methylation in the 3′UTR region of the gene. | Knee articular cartilage | Differentially methylated genes | [16] |
| SOX11 was identified as a novel OA protein downregulated during OA. | Osteoarthritic and normal chondrocytes | N.A. | [30] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, E.A.; Alzahrani, A.M. SOXC Transcription Factors as Diagnostic Biomarkers and Therapeutic Targets for Arthritis. Int. J. Mol. Sci. 2023, 24, 4215. https://doi.org/10.3390/ijms24044215
Ahmed EA, Alzahrani AM. SOXC Transcription Factors as Diagnostic Biomarkers and Therapeutic Targets for Arthritis. International Journal of Molecular Sciences. 2023; 24(4):4215. https://doi.org/10.3390/ijms24044215
Chicago/Turabian StyleAhmed, Emad A., and Abdullah M. Alzahrani. 2023. "SOXC Transcription Factors as Diagnostic Biomarkers and Therapeutic Targets for Arthritis" International Journal of Molecular Sciences 24, no. 4: 4215. https://doi.org/10.3390/ijms24044215
APA StyleAhmed, E. A., & Alzahrani, A. M. (2023). SOXC Transcription Factors as Diagnostic Biomarkers and Therapeutic Targets for Arthritis. International Journal of Molecular Sciences, 24(4), 4215. https://doi.org/10.3390/ijms24044215






