Collagen VI in the Musculoskeletal System
Abstract
1. Introduction
2. Collagen VI Expression, Assembly, and Secretion
3. Collagen VI in Tissues Relevant for the Musculoskeletal System
4. Skeletal Muscle
4.1. General Aspects
4.2. Animal Models
4.3. Clinical Studies
5. Bone
5.1. General Aspects
5.2. Animal Models
5.3. Clinical Studies
6. Tendon
6.1. General Aspects
6.2. Animal Models
6.3. Clinical Studies
7. Cartilage
7.1. General Aspects
7.2. Animal Models
7.3. Clinical Studies
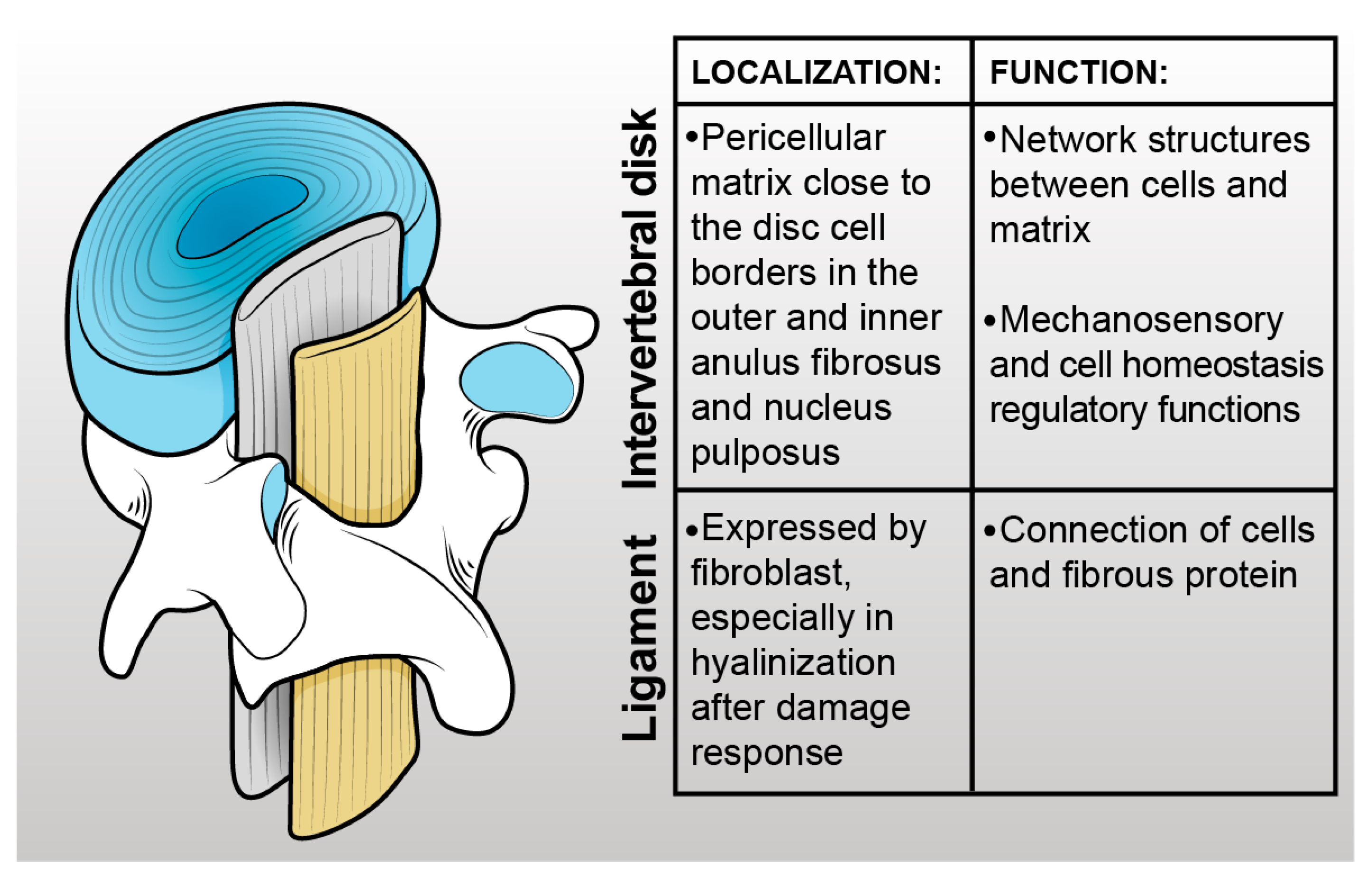
8. Ligament
8.1. General Aspects
8.2. Animal Models
8.3. Clinical Studies
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Kapandji, I.A. The physiology of the joints. Churchill Livingstone 1977, 2, 186–189. [Google Scholar]
- Hessle, H.; Engvall, E. Type VI collagen. Studies on its localization, structure, and biosynthetic form with monoclonal antibodies. J. Biol. Chem. 1984, 259, 3955–3961. [Google Scholar] [CrossRef]
- Cescon, M.; Gattazzo, F.; Chen, P.; Bonaldo, P. Collagen VI at a glance. J. Cell Sci. 2015, 128, 3525–3531. [Google Scholar] [CrossRef]
- Gara, S.K.; Grumati, P.; Urciuolo, A.; Bonaldo, P.; Kobbe, B.; Koch, M.; Paulsson, M.; Wagener, R. Three novel collagen VI chains with high homology to the α3 chain. J. Biol. Chem. 2008, 283, 10658–10670. [Google Scholar] [CrossRef]
- Fitzgerald, J.; Rich, C.; Zhou, F.H.; Hansen, U. Three novel collagen VI chains, alpha4(VI), alpha5(VI), and alpha6(VI). J. Biol. Chem. 2008, 283, 20170–20180. [Google Scholar] [CrossRef] [PubMed]
- Caria, F.; Cescon, M.; Gualandi, F.; Pichiecchio, A.; Rossi, R.; Rimessi, P.; Piccinelli, S.C.; Cassarino, S.G.; Gregorio, I.; Galvagni, A.; et al. Autosomal recessive Bethlem myopathy. Neurology 2009, 73, 1883–1891. [Google Scholar] [CrossRef]
- Briñas, L.; Richard, P.; Quijano-Roy, S.; Gartioux, C.; Ledeuil, C.; Lacène, E.; Makri, S.; Ferreiro, A.; Maugenre, S.; Topaloglu, H. Early onset collagen VI myopathies: Genetic and clinical correlations. Ann. Neurol. 2010, 68, 511–520. [Google Scholar] [CrossRef]
- Merlini, L.; Martoni, E.; Grumati, P.; Sabatelli, P.; Squarzoni, S.; Urciuolo, A.; Ferlini, A.; Gualandi, F.; Bonaldo, P. Autosomal recessive myosclerosis myopathy is a collagen VI disorder. Neurology 2008, 71, 1245–1253. [Google Scholar] [CrossRef]
- Lampe, A.K.; Bushby, K.M.D. Collagen VI related muscle disorders. J. Med. Genet. 2005, 42, 673–685. [Google Scholar] [CrossRef]
- Merlini, L.; Bernardi, P. Therapy of collagen VI-related myopathies (Bethlem and Ullrich). Neurother. J. Am. Soc. Exp. Neurother. 2008, 5, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Bonaldo, P.; Russo, V.; Bucciotti, F.; Bressan, G.M.; Colombatti, A. α1 chain of chick type VI collagen: The complete cDNA sequence reveals a hybrid molecule made of one short collagen and three von Willebrand factor type A-like domains. J. Biol. Chem. 1989, 264, 5575–5580. [Google Scholar] [CrossRef] [PubMed]
- Bonaldo, P.; Russo, V.; Bucciotti, F.; Doliana, R.; Colombatti, A. Structural and functional features of the alpha 3 chain indicate a bridging role for chicken collagen VI in connective tissues. Biochemistry 1990, 29, 1245–1254. [Google Scholar] [CrossRef] [PubMed]
- Doliana, R.; Bonaldo, P.; Colombatti, A. «Multiple forms of chicken alpha 3(VI) collagen chain generated by alternative splicing in type A repeated domains. J. Cell Biol. 1990, 111, 2197–2205. [Google Scholar] [CrossRef] [PubMed]
- Dziadek, M.; Kazenwadel, J.S.; Hendrey, J.A.; Pan, T.-C.; Zhang, R.-Z.; Chu, M.-L. Alternative splicing of transcripts for the alpha3 chain of mouse collagen VI: Identification of an abundant isoform lacking domains N7–N10 in mouse and human. Matrix Biol. 2002, 21, 227–241. [Google Scholar] [CrossRef]
- Saitta, B.; Stokes, D.G.; Vissing, H.; Timpl, R.; Chu, M.L. Alternative splicing of the human alpha 2 (VI) collagen gene generates multiple mRNA transcripts which predict three protein variants with distinct carboxyl termini. J. Biol. Chem. 1990, 265, 6473–6480. [Google Scholar] [CrossRef] [PubMed]
- Engel, J.; Furthmayr, H.; Odermatt, E.; von der Mark, H.; Aumailley, M.; Fleischmajer, R.; Timpl, R. Structure and Macromolecular Organization of Type VI Collagena. Ann. N. Y. Acad. Sci. 1985, 460, 25–37. [Google Scholar] [CrossRef]
- Colombatti, A.; Mucignat, M.T.; Bonaldo, P. Secretion and Matrix Assembly of Recombinant Type VI Collagen*. J. Biol. Chem. 1995, 270, 13105–13111. [Google Scholar] [CrossRef]
- Colombatti, A.; Bonaldo, P.; Ainger, K.; Bressan, G.M.; Volpin, D. Biosynthesis of chick type VI collagen. I. Intracellular assembly and molecular structure. J. Biol. Chem. 1987, 262, 14454–14460. [Google Scholar] [CrossRef]
- Colombatti, A.; Bonaldo, P. Biosynthesis of chick type VI collagen. II. Processing and secretion in fibroblasts and smooth muscle cells. J. Biol. Chem. 1987, 262, 14461–14466. [Google Scholar] [CrossRef]
- Chu, M.L.; Pan, T.C.; Conway, D.; Saitta, B.; Stokes, D.; Kuo, H.J.; Glanville, R.W.; Timpl, R.; Mann, K.; Deutzmann, R. The Structure of Type VI Collagen a. Ann. N. Y. Acad. Sci. 1990, 580, 55–63. [Google Scholar] [CrossRef]
- Knupp, C.; Pinali, C.; Munro, P.M.; Gruber, H.E.; Sherratt, M.J.; Baldock, C.; Squire, J.M. Structural correlation between collagen VI microfibrils and collagen VI banded aggregates. J. Struct. Biol. 2006, 154, 312–326. [Google Scholar] [CrossRef] [PubMed]
- Lamandé, S.R.; Mörgelin, M.; Selan, C.; Jöbsis, G.J.; Baas, F.; Bateman, J.F. Kinked collagen VI tetramers and reduced microfibril formation as a result of Bethlem myopathy and introduced triple helical glycine mutations. J. Biol. Chem. 2002, 277, 1949–1956. [Google Scholar] [CrossRef] [PubMed]
- Persikov, A.V.; Ramshaw, J.A.; Kirkpatrick, A.; Brodsky, B. Amino acid propensities for the collagen triple-helix. Biochemistry 2000, 39, 14960–14967. [Google Scholar] [CrossRef] [PubMed]
- Lamandé, S.; Sigalas, E.; Pan, T.; Chu, M.; Dziadek, M.; Timpl, R.; Bateman, J. The Role of the α3(VI) Chain in Collagen VI Assembly: Expression of an α3(vi) chain lacking n-terminal modules n10–n7 restores collagen vi assembly, secretion, and matrix deposition in an α3(vi)-deficient cell line. J. Biol. Chem. 1998, 273, 7423–7430. [Google Scholar] [CrossRef] [PubMed]
- Furthmayr, H.; Wiedemann, H.; Timpl, R.; Odermatt, E.; Engel, J. Electron-microscopical approach to a structural model of intima collagen. Biochem. J. 1983, 211, 303–311. [Google Scholar] [CrossRef]
- Ball, S.; Bella, J.; Kielty, C.; Shuttleworth, A. Structural basis of type VI collagen dimer formation. J. Biol. Chem. 2003, 278, 15326–15332. [Google Scholar] [CrossRef]
- Bernardi, P.; Bonaldo, P. Dysfunction of Mitochondria and Sarcoplasmic Reticulum in the Pathogenesis of Collagen VI Muscular Dystrophies. Ann. N. Y. Acad. Sci. 2008, 1147, 303–311. [Google Scholar] [CrossRef]
- Fitzgerald, J.; Mörgelin, M.; Selan, C.; Wiberg, C.; Keene, D.; Lamandé, S.; Bateman, J. The N-terminal N5 Subdomain of the α3(VI) Chain Is Important for Collagen VI Microfibril Formation*. J. Biol. Chem. 2001, 276, 187–193. [Google Scholar] [CrossRef]
- Kuo, H.-J.; Maslen, C.L.; Keene, D.R.; Glanville, R.W. Type VI collagen anchors endothelial basement membranes by interacting with type IV collagen. J. Biol. Chem. 1997, 272, 26522–26529. [Google Scholar] [CrossRef]
- Sabatelli, P.; Bonaldo, P.; Lattanzi, G.; Braghetta, P.; Bergamin, N.; Capanni, C.; Mattioli, E.; Columbaro, M.; Ognibene, A.; Pepe, G.; et al. Collagen VI deficiency affects the organization of fibronectin in the extracellular matrix of cultured fibroblasts. Matrix Biol. 2001, 20, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Bidanset, D.J.; Guidry, C.; Rosenberg, L.C.; Choi, H.U.; Timpl, R.; Hook, M. Binding of the proteoglycan decorin to collagen type VI. J. Biol. Chem. 1992, 267, 5250–5256. [Google Scholar] [CrossRef] [PubMed]
- Tillet, E.; Wiedemann, H.; Golbik, R.; Pan, T.C.; Zhang, R.Z.; Mann, K.; Chu, M.L.; Timpl, R. Recombinant expression and structural and binding properties of α1(VI) and α2(VI) chains of human collagen type VI. Eur. J. Biochem. 1994, 221, 177–187. [Google Scholar] [CrossRef]
- Hansen, U.; Allen, J.M.; White, R.; Moscibrocki, C.; Bruckner, P.; Bateman, J.F.; Fitzgerald, J. WARP Interacts with Collagen VI-Containing Microfibrils in the Pericellular Matrix of Human Chondrocytes. PLoS ONE 2012, 7, e52793. [Google Scholar] [CrossRef]
- Specks, U.; Mayer, U.; Nischt, R.; Spissinger, T.; Mann, K.; Timpl, R.; Engel, J.; Chu, M.L. Structure of recombinant N-terminal globule of type VI collagen alpha 3 chain and its binding to heparin and hyaluronan. EMBO J. 1992, 11, 4281–4290. [Google Scholar] [CrossRef] [PubMed]
- Fitch, J.M.; Birk, D.E.; Linsenmayer, C.; Linsenmayer, T.F. Stromal assemblies containing collagen types IV and VI and fibronectin in the developing embryonic avian cornea. Dev. Biol. 1991, 144, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Wiberg, C.; Hedbom, E.; Khairullina, A.; Lamandé, S.R.; Oldberg, A.; Timpl, R.; Mörgelin, M.; Heinegård, D. Biglycan and decorin bind close to the n-terminal region of the collagen VI triple helix. J. Biol. Chem. 2001, 276, 18947–18952. [Google Scholar] [CrossRef] [PubMed]
- Maraldi, N.M.; Sabatelli, P.; Columbaro, M.; Zamparelli, A.; Manzoli, F.A.; Bernardi, P.; Bonaldo, P.; Merlini, L. Collagen VI myopathies: From the animal model to the clinical trial. Adv. Enzyme Regul. 2009, 49, 197–211. [Google Scholar] [CrossRef]
- Bönnemann, C.G. The collagen VI-related myopathies: Muscle meets its matrix. Nat. Rev. Neurol. 2011, 7, 379–390. [Google Scholar] [CrossRef]
- Turrina, A.; Martínez-González, M.A.; Stecco, C. The muscular force transmission system: Role of the intramuscular connective tissue. J. Bodyw. Mov. Ther. 2013, 17, 95–102. [Google Scholar] [CrossRef]
- Csapo, R.; Gumpenberger, M.; Wessner, B. Skeletal Muscle Extracellular Matrix—What Do We Know About Its Composition, Regulation, and Physiological Roles? A Narrative Review. Front. Physiol. 2020, 11, 253. [Google Scholar] [CrossRef]
- Gara, S.K.; Grumati, P.; Squarzoni, S.; Sabatelli, P.; Urciuolo, A.; Bonaldo, P.; Paulsson, M.; Wagener, R. Differential and restricted expression of novel collagen VI chains in mouse. Matrix Biol. J. Int. Soc. Matrix Biol. 2011, 30, 248–257. [Google Scholar] [CrossRef]
- Sabatelli, P.; Gualandi, F.; Gara, S.K.; Grumati, P.; Zamparelli, A.; Martoni, E.; Pellegrini, C.; Merlini, L.; Ferlini, A.; Bonaldo, P.; et al. Expression of collagen VI α5 and α6 chains in human muscle and in Duchenne muscular dystrophy-related muscle fibrosis. Matrix Biol. J. Int. Soc. Matrix Biol. 2012, 31, 187–196. [Google Scholar] [CrossRef]
- Braghetta, P.; Ferrari, A.; Fabbro, C.; Bizzotto, D.; Volpin, D.; Bonaldo, P.; Bressan, G.M. An enhancer required for transcription of the Col6a1 gene in muscle connective tissue is induced by signals released from muscle cells. Exp. Cell Res. 2008, 314, 3508–3518. [Google Scholar] [CrossRef]
- Zou, Y.; Zhang, R.-Z.; Sabatelli, P.; Chu, M.-L.; Bönnemann, C.G. Muscle Interstitial Fibroblasts Are the Main Source of Collagen VI Synthesis in Skeletal Muscle: Implications for Congenital Muscular Dystrophy Types Ullrich and Bethlem. J. Neuropathol. Exp. Neurol. 2008, 67, 144–154. [Google Scholar] [CrossRef]
- Urciuolo, A.; Quarta, M.; Morbidoni, V.; Gattazzo, F.; Molon, S.; Grumati, P.; Montemurro, F.; Tedesco, F.S.; Blaauw, B.; Cossu, G.; et al. Collagen VI regulates satellite cell self-renewal and muscle regeneration. Nat. Commun. 2013, 4, 1964. [Google Scholar] [CrossRef] [PubMed]
- Cescon, M.; Gregorio, I.; Eiber, N.; Borgia, D.; Fusto, A.; Sabatelli, P.; Scorzeto, M.; Megighian, A.; Pegoraro, E.; Hashemolhosseini, S. Collagen VI is required for the structural and functional integrity of the neuromuscular junction. Acta Neuropathol. 2018, 136, 483–499. [Google Scholar] [CrossRef]
- Jöbsis, G.J.; Keizers, H.; Vreijling, J.P.; de Visser, M.; Speer, M.C.; Wolterman, R.A.; Baas, F.; Bolhuis, P.A. Type VI collagen mutations in Bethlem myopathy, an autosomal dominant myopathy with contractures. Nat. Genet. 1996, 14, 113–115. [Google Scholar] [CrossRef] [PubMed]
- Vanegas, O.C.; Bertini, E.; Zhang, R.Z.; Petrini, S.; Minosse, C.; Sabatelli, P.; Giusti, B.; Chu, M.L.; Pepe, G. Ullrich scleroatonic muscular dystrophy is caused by recessive mutations in collagen type VI. Proc. Natl. Acad. Sci. USA 2001, 98, 7516–7521. [Google Scholar] [CrossRef]
- Bonaldo, P.; Braghetta, P.; Zanetti, M.; Piccolo, S.; Volpin, D.; Bressan, G.M. Collagen VI deficiency induces early onset myopathy in the mouse: An animal model for Bethlem myopathy. Hum. Mol. Genet. 1998, 7, 2135–2140. [Google Scholar] [CrossRef] [PubMed]
- Irwin, W.A.; Bergamin, N.; Sabatelli, P.; Reggiani, C.; Megighian, A.; Merlini, L.; Braghetta, P.; Columbaro, M.; Volpin, D.; Bressan, G.M.; et al. Mitochondrial dysfunction and apoptosis in myopathic mice with collagen VI deficiency. Nat. Genet. 2003, 35, 367–371. [Google Scholar] [CrossRef]
- Angelin, A.; Tiepolo, T.; Sabatelli, P.; Grumati, P.; Bergamin, N.; Golfieri, C.; Mattioli, E.; Gualandi, F.; Ferlini, A.; Merlini, L.; et al. Mitochondrial dysfunction in the pathogenesis of Ullrich congenital muscular dystrophy and prospective therapy with cyclosporins. Proc. Natl. Acad. Sci. USA 2007, 104, 991–996. [Google Scholar] [CrossRef]
- Bernardi, P.; Bonaldo, P. Mitochondrial dysfunction and defective autophagy in the pathogenesis of collagen VI muscular dystrophies. Cold Spring Harb. Perspect. Biol. 2013, 5, a011387. [Google Scholar] [CrossRef]
- Menazza, S.; Blaauw, B.; Tiepolo, T.; Toniolo, L.; Braghetta, P.; Spolaore, B.; Reggiani, C.; Di Lisa, F.; Bonaldo, P.; Canton, M. Oxidative stress by monoamine oxidases is causally involved in myofiber damage in muscular dystrophy. Hum. Mol. Genet. 2010, 19, 4207–4215. [Google Scholar] [CrossRef] [PubMed]
- Grumati, P.; Coletto, L.; Sabatelli, P.; Cescon, M.; Angelin, A.; Bertaggia, E.; Blaauw, B.; Urciuolo, A.; Tiepolo, T.; Merlini, L.; et al. Autophagy is defective in collagen VI muscular dystrophies, and its reactivation rescues myofiber degeneration. Nat. Med. 2010, 16, 1313–1320. [Google Scholar] [CrossRef]
- Chrisam, M.; Pirozzi, M.; Castagnaro, S.; Blaauw, B.; Polishchuck, R.; Cecconi, F.; Grumati, P.; Bonaldo, P. Reactivation of autophagy by spermidine ameliorates the myopathic defects of collagen VI-null mice. Autophagy 2015, 11, 2142–2152. [Google Scholar] [CrossRef] [PubMed]
- Metti, S.; Gambarotto, L.; Chrisam, M.; La Spina, M.; Baraldo, M.; Braghetta, P.; Blaauw, B.; Bonaldo, P. Corrigendum: The Polyphenol Pterostilbene Ameliorates the Myopathic Phenotype of Collagen VI Deficient Mice via Autophagy Induction. Front. Cell Dev. Biol. 2021, 8, 580933. [Google Scholar] [CrossRef]
- Tonelotto, V.; Consorti, C.; Facchinello, N.; Trapani, V.; Sabatelli, P.; Giraudo, C.; Spizzotin, M.; Cescon, M.; Bertolucci, C.; Bonaldo, P. Collagen VI ablation in zebrafish causes neuromuscular defects during developmental and adult stages. Matrix Biol. J. Int. Soc. Matrix Biol. 2022, 112, 39–61. [Google Scholar] [CrossRef] [PubMed]
- Doane, K.J.; Yang, G.; Birk, D.E. Corneal cell-matrix interactions: Type VI Collagen promotes adhesion and spreading of corneal fibroblasts. Exp. Cell Res. 1992, 200, 490–499. [Google Scholar] [CrossRef]
- Pfaff, M.; Aumailley, M.; Specks, U.; Knolle, J.; Zerwes, H.G.; Timpl, R. Integrin and Arg-Gly-Asp Dependence of Cell Adhesion to the Native and Unfolded Triple Helix of Collagen Type VI. Exp. Cell Res. 1993, 206, 167–176. [Google Scholar] [CrossRef]
- Tulla, M.; Pentikäinen, O.T.; Viitasalo, T.; Käpylä, J.; Impola, U.; Nykvist, P.; Nissinen, L.; Johnson, M.S.; Heino, J. Selective binding of collagen subtypes by integrin α1I, α2I, and α10I domains. J. Biol. Chem. 2001, 276, 48206–48212. [Google Scholar] [CrossRef] [PubMed]
- Marcelino, J.; McDevitt, C.A. Attachment of articular cartilage chondrocytes to the tissue form of type VI collagen. Biochim. Biophys. Acta BBA-Protein Struct. Mol. Enzymol. 1995, 1249, 180–188. [Google Scholar] [CrossRef]
- Petrini, S.; Tessa, A.; Stallcup, W.B.; Sabatelli, P.; Pescatori, M.; Giusti, B.; Carrozzo, R.; Verardo, M.; Bergamin, N.; Columbaro, M.; et al. Altered expression of the MCSP/NG2 chondroitin sulfate proteoglycan in collagen VI deficiency. Mol. Cell. Neurosci. 2005, 30, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Doane, K.J.; Howell, S.J.; Birk, D.E. Identification and functional characterization of two type VI collagen receptors, alpha 3 beta 1 integrin and NG2, during avian corneal stromal development. Invest. Ophthalmol. Vis. Sci. 1998, 39, 263–275. [Google Scholar] [PubMed]
- Bürgi, J.; Kunz, B.; Abrami, L.; Deuquet, J.; Piersigilli, A.; Scholl-Bürgi, S.; Lausch, E.; Unger, S.; Superti-Furga, A.; van der Goot, F.G. CMG2/ANTXR2 regulates extracellular collagen VI which accumulates in hyaline fibromatosis syndrome. Nat. Commun. 2017, 8, 15861. [Google Scholar] [CrossRef] [PubMed]
- Jöbsis, G.J.; Boers, J.M.; Barth, P.G.; de Visser, M. Bethlem myopathy: A slowly progressive congenital muscular dystrophy with contractures. Brain J. Neurol. 1999, 122, 649–655. [Google Scholar] [CrossRef]
- Merlini, L.; Morandi, L.; Granata, C.; Ballestrazzi, A. Bethlem myopathy: Early-onset benign autosomal dominant myopathy with contractures. Description of two new families. Neuromuscul. Disord. NMD 1994, 4, 503–511. [Google Scholar] [CrossRef]
- Ullrich, O. Kongenitale, atonisch-sklerotische Muskeldystrophie. Monatsschr Kinderheilkd 1930, 47, 502–510. [Google Scholar]
- Ullrich, O. Kongenitale, atonisch-sklerotische Muskeldystrophie, ein weiterer Typus der heredodegenerativen Erkrankungen des neuromuskulären Systems. Z. Für Gesamte Neurol. Psychiatr. 1930, 126, 171–201. [Google Scholar] [CrossRef]
- Nonaka, I.; Une, Y.; Ishihara, T.; Miyoshino, S.; Nakashima, T.; Sugita, H. A clinical and histological study of Ullrich’s disease (congenital atonic-sclerotic muscular dystrophy). Neuropediatrics 1981, 12, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Voit, T. Congenital muscular dystrophies: 1997 update. Brain Dev. 1998, 20, 65–74. [Google Scholar] [CrossRef]
- Merlini, L.; Angelin, A.; Tiepolo, T.; Braghetta, P.; Sabatelli, P.; Zamparelli, A.; Ferlini, A.; Maraldi, N.M.; Bonaldo, P.; Bernardi, P. Cyclosporin A corrects mitochondrial dysfunction and muscle apoptosis in patients with collagen VI myopathies. Proc. Natl. Acad. Sci. USA 2008, 105, 5225–5229. [Google Scholar] [CrossRef]
- Merlini, L.; Sabatelli, P.; Armaroli, A.; Gnudi, S.; Angelin, A.; Grumati, P.; Michelini, M.E.; Franchella, A.; Gualandi, F.; Bertini, E.; et al. Cyclosporine A in Ullrich congenital muscular dystrophy: Long-term results. Oxid. Med. Cell. Longev. 2011, 2011, 139194. [Google Scholar] [CrossRef]
- Sorato, E.; Menazza, S.; Zulian, A.; Sabatelli, P.; Gualandi, F.; Merlini, L.; Bonaldo, P.; Canton, M.; Bernardi, P.; Di Lisa, F. Monoamine oxidase inhibition prevents mitochondrial dysfunction and apoptosis in myoblasts from patients with collagen VI myopathies. Free Radic. Biol. Med. 2014, 75, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Castagnaro, S.; Pellegrini, C.; Pellegrini, M.; Chrisam, M.; Sabatelli, P.; Toni, S.; Grumati, P.; Ripamonti, C.; Pratelli, L.; Maraldi, N.M.; et al. Autophagy activation in COL6 myopathic patients by a low-protein-diet pilot trial. Autophagy 2016, 12, 2484–2495. [Google Scholar] [CrossRef]
- Sabatelli, P.; Merlini, L.; Di Martino, A.; Cenni, V.; Faldini, C. Early Morphological Changes of the Rectus Femoris Muscle and Deep Fascia in Ullrich Congenital Muscular Dystrophy. Int. J. Environ. Res. Public. Health 2022, 19, 1252. [Google Scholar] [CrossRef]
- Higuchi, I.; Horikiri, T.; Niiyama, T.; Suehara, M.; Shiraishi, T.; Hu, J.; Uchida, Y.; Saito, A.; Nakagawa, M.; Arimura, K.; et al. Pathological characteristics of skeletal muscle in Ullrich’s disease with collagen VI deficiency. Neuromuscul. Disord. 2003, 13, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Izu, Y.; Ezura, Y.; Mizoguchi, F.; Kawamata, A.; Nakamoto, T.; Nakashima, K.; Hayata, T.; Hemmi, H.; Bonaldo, P.; Noda, M. Type VI collagen deficiency induces osteopenia with distortion of osteoblastic cell morphology. Tissue Cell 2012, 44, 1–6. [Google Scholar] [CrossRef]
- Christensen, S.E.; Coles, J.M.; Zelenski, N.A.; Furman, B.D.; Leddy, H.A.; Zauscher, S.; Bonaldo, P.; Guilak, F. Altered Trabecular Bone Structure and Delayed Cartilage Degeneration in the Knees of Collagen VI Null Mice. PLoS ONE 2012, 7, e33397. [Google Scholar] [CrossRef] [PubMed]
- Keene, D.R.; Sakai, L.Y.; Burgeson, R.E. Human bone contains type III collagen, type VI collagen, and fibrillin: Type III collagen is present on specific fibers that may mediate attachment of tendons, ligaments, and periosteum to calcified bone cortex. J. Histochem. Cytochem. Off. J. Histochem. Soc. 1991, 39, 59–69. [Google Scholar] [CrossRef]
- Harada, S.; Rodan, G.A. Control of osteoblast function and regulation of bone mass. Nature 2003, 423, 349–355. [Google Scholar] [CrossRef]
- Stark, Z.; Savarirayan, R. Osteopetrosis. Orphanet J. Rare Dis. 2009, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Cummings, S.R.; Melton, L.J. Epidemiology and outcomes of osteoporotic fractures. Lancet Lond. Engl. 2002, 359, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Pham, H.T.; Kram, V.; Dar, Q.-A.; Komori, T.; Ji, Y.; Mohassel, P.; Rooney, J.; Li, L.; Kilts, T.; Bonnemann, C.; et al. Collagen VIα2 chain deficiency causes trabecular bone loss by potentially promoting osteoclast differentiation through enhanced TNFα signaling. Sci. Rep. 2020, 10, 13749. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Kirk, M.; Kahn, A.J. The role of type I collagen in the regulation of the osteoblast pheno type. J. Bone Miner. Res. 1996, 11, 1139–1145. [Google Scholar] [CrossRef]
- Harumiya, S.; Gibson, M.A.; Koshihara, Y. Antisense suppression of collagen VI synthesis results in reduced expression of collagen I in normal human osteoblast-like cells. Biosci. Biotechnol. Biochem. 2002, 66, 2743–2747. [Google Scholar] [CrossRef] [PubMed]
- Ueno, K.; Katayama, T.; Miyamoto, T.; Koshihara, Y. Interleukin-4 enhances in vitro mineralization in human osteoblast-like cells. Biochem. Biophys. Res. Commun. 1992, 189, 1521–1526. [Google Scholar] [CrossRef]
- Ishibashi, H.; Harumiya, S.; Koshihara, Y. Involvement of type VI collagen in interlekin-4-induced mineralization by human osteoblast-like cells in vitro. Biochem. Biophys. Acta 1999, 1472, 153–164. [Google Scholar] [CrossRef]
- Ishibashi, H.; Karube, S.; Yamakawa, A.; Koshihara, Y. Interleukin-4 stimulates pro-alpha 1(VI) collagen gene expression in cultured human osteoblast-like cells. Biochem. Biophys. Res. Commun. 1995, 211, 727–734. [Google Scholar] [CrossRef]
- Alexopoulos, L.G.; Youn, I.; Bonaldo, P.; Guilak, F. Developmental and osteoarthritic changes in Col6a1-knockout mice: Biomechanics of type VI collagen in the cartilage pericellular matrix. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 2009, 60, 771–779. [Google Scholar] [CrossRef]
- Giesen, E.B.W.; Ding, M.; Dalstra, M.; van Eijden, T.M.G.J. Changed Morphology and Mechanical Properties of Cancellous Bone in the Mandibular Condyles of Edentate People. J. Dent. Res. 2004, 83, 255–259. [Google Scholar] [CrossRef]
- Damrongrungruang, T.; Kuroda, S.; Kondo, H.; Aoki, K.; Ohya, K.; Kasugai, S. A Simple Murine Model for Immobilization Osteopenia. Clin. Orthop. Relat. Res. 2004, 425, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Toni, S.; Morandi, R.; Busacchi, M.; Tardini, L.; Merlini, L.; Battistini, N.C.; Pellegrini, M. Nutritional status evaluation in patients affected by bethlem myopathy and ullrich congenital muscular dystrophy. Front. Aging Neurosci. 2014, 6, 315. [Google Scholar] [CrossRef] [PubMed]
- Bönnemann, C.G. The collagen VI-related myopathies Ullrich congenital muscular dystrophy and Bethlem myopathy. Handb. Clin. Neurol. 2011, 101, 81–96. [Google Scholar] [CrossRef] [PubMed]
- Philippe, V.; Pruna, L.; Fattah, M.A.; Pascal, V.; Kaminsky, P. Decreased bone mineral density in adult patients with muscular dystrophy. Jt. Bone Spine 2011, 78, 651–652. [Google Scholar] [CrossRef] [PubMed]
- Screen, H.R.; Berk, D.E.; Kadler, K.E.; Ramirez, F.; Young, M.F. Tendon functional extracellular matrix. J. Orthop. Res. 2015, 33, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Kastelic, J.; Galeski, A.; Baer, E. The multicomposite structure of tendon. Connect. Tissue Res. 1978, 6, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Young, B.B.; Ezura, Y.; Favata, M.; Soslowsky, L.J.; Chakravarti, S.; Birk, D.E. Development of tendon structure and function: Regulation of collagen fibrillogenesis. J. Musculoskelet. Neuronal Interact. 2005, 5, 5–21. [Google Scholar] [PubMed]
- Antoniel, M.; Traina, F.; Merlini, L.; Andrenacci, D.; Tigani, D.; Santi, S.; Cenni, V.; Sabatelli, P.; Faldini, C.; Squarzoni, S. Tendon Extracellular Matrix Remodeling and Defective Cell Polarization in the Presence of Collagen VI Mutations. Cells 2020, 9, 409. [Google Scholar] [CrossRef] [PubMed]
- Kielty, C.M.; Whittaker, S.P.; Grant, M.E.; Shuttleworth, C.A. Type VI collagen microfibrils: Evidence for a structural association with hyaluronan. J. Cell Biol. 1992, 118, 979–990. [Google Scholar] [CrossRef]
- Leiphart, R.J.; Pham, H.; Harvey, T.; Komori, T.; Kilts, T.M.; Shetye, S.S.; Weiss, S.N.; Adams, S.M.; Birk, D.E.; Soslowsky, L.J.; et al. Coordinate roles for collagen VI and biglycan in regulating tendon collagen fibril structure and function. Matrix Biol. Plus 2022, 13, 100099. [Google Scholar] [CrossRef]
- Izu, Y.; Ansorge, H.L.; Zhang, G.; Soslowsky, L.; Bonaldo, P.; Chu, M.-L.; Birk, D. Dysfunctional tendon collagen fibrillogenesis in collagen VI null mice. Matrix Biol. J. Int. Soc. Matrix Biol. 2011, 30, 53–61. [Google Scholar] [CrossRef]
- Pan, T.C.; Zhang, R.Z.; Markova, D.; Arita, M.; Zhang, Y.; Bogdanovich, S.; Khurana, T.S.; Bönnemann, C.G.; Birk, D.E.; Chu, M.L. COL6A3 protein deficiency in mice leads to muscle and tendon defects similar to human collagen VI congenital muscular dystrophy. J. Biol. Chem. 2013, 288, 14320–14331. [Google Scholar] [CrossRef]
- Tagliavini, F.; Pellegrini, C.; Sardone, F.; Squarzoni, S.; Paulsson, M.; Wagener, R.; Gualandi, F.; Trabanelli, C.; Ferlini, A.; Merlini, L.; et al. Defective collagen VI α6 chain expression in the skeletal muscle of patients with collagen VI-related myopathies. Biochim. Biophys. Acta 2014, 1842, 1604–1612. [Google Scholar] [CrossRef]
- Sardone, F.; Traina, F.; Bondi, A.; Merlini, L.; Santi, S.; Maraldi, N.M.; Faldini, C.; Sabatelli, P. Tendon Extracellular Matrix Alterations in Ullrich Congenital Muscular Dystrophy. Front. Aging Neurosci. 2016, 8, 131. [Google Scholar] [CrossRef]
- Kobayasi, T. Abnormality of dermal collagen fibrils in Ehlers Danlos syndrome. Anticipation of the abnormality for the inherited hypermobile disorders. Eur. J. Dermatol. EJD 2004, 14, 221–229. [Google Scholar] [PubMed]
- Sun, M.; Connizzo, B.K.; Adams, S.M.; Freedman, B.R.; Wenstrup, R.J.; Soslowsky, L.J.; Birk, D.E. Targeted Deletion of Collagen V in Tendons and Ligaments Results in a Classic Ehlers-Danlos Syndrome Joint Phenotype. Am. J. Pathol. 2015, 185, 1436–1447. [Google Scholar] [CrossRef]
- Heinemeier, K.M.; Kjaer, M. In vivo investigation of tendon responses to mechanical loading. J. Musculoskelet. Neuronal Interact. 2011, 11, 115–123. [Google Scholar]
- Narici, M.V.; Maganaris, C.N. Plasticity of the muscle-tendon complex with disuse and aging. Exerc. Sport Sci. Rev. 2007, 35, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Tatari, H. The structure, physiology, and biomechanics of articular cartilage: Injury and repair. Acta Orthop. Traumatol. Turc. 2007, 41, 1–5. [Google Scholar] [PubMed]
- Cohen, N.P.; Foster, R.J.; Mow, V.C. Composition and dynamics of articular cartilage: Structure, function, and maintaining healthy state. J. Orthop. Sports Phys. Ther. 1998, 28, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Horikawa, O.; Nakajima, H.; Kikuchi, T.; Ichimura, S.; Yamada, H.; Fujikawa, K.; Toyama, Y. Distribution of type VI collagen in chondrocyte microenvironment: Study of chondrons isolated from human normal and degenerative articular cartilage and cultured chondrocytes. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2004, 9, 29–36. [Google Scholar] [CrossRef]
- Söder, S.; Hambach, L.; Lissner, R.; Kirchner, T.; Aigner, T. Ultrastructural localization of type VI collagen in normal adult and osteoarthritic human articular cartilage. Osteoarthr. Cartil. 2002, 10, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Ronzière, M.C.; Ricard-Blum, S.; Tiollier, J.; Hartmann, D.J.; Garrone, R.; Herbage, D. Comparative analysis of collagens solubilized from human foetal, and normal and osteoarthritic adult articular cartilage, with emphasis on type VI collagen. Biochim. Biophys. Acta 1990, 1038, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Mankin, H.J.; Lippiello, L. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. J. Bone Jt. Surg. Am. 1970, 52, 424–434. [Google Scholar] [CrossRef]
- Lee, D.A.; Bentley, G.; Archer, C.W. The control of cell division in articular chondrocytes. Osteoarthr. Cartil. 1993, 1, 137–146. [Google Scholar] [CrossRef]
- Zelenski, N.A.; Leddy, H.A.; Sanchez-Adams, J.; Zhang, J.; Bonaldo, P.; Liedtke, W.; Guilak, F. Type VI collagen regulates pericellular matrix properties, chondrocyte swelling, and mechanotransduction in mouse articular cartilage. Arthritis Rheumatol. 2015, 67, 1286–1294. [Google Scholar] [CrossRef]
- Hayes, A.J.; Shu, C.C.; Lord, M.S.; Little, C.B.; Whitelock, J.M.; Melrose, J. Pericellular colocalisation and interactive properties of type VI collagen and perlecan in the intervertebral disc. Eur. Cell. Mater. 2016, 32, 40–57. [Google Scholar] [CrossRef]
- Berg, E.J.; Ashurst, J.V. Anatomy, Back, Cauda Equina. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022; Available online: http://www.ncbi.nlm.nih.gov/books/NBK513251 (accessed on 18 August 2022).
- Huang, Y.-C.; Hu, Y.; Li, Z.; Luk, K.D.K. Biomaterials for intervertebral disc regeneration: Current status and looming challenges. J. Tissue Eng. Regen. Med. 2018, 12, 2188–2202. [Google Scholar] [CrossRef]
- van Uden, S.; Silva-Correia, J.; Oliveira, J.M.; Reis, R.L. Current strategies for treatment of intervertebral disc degeneration: Substitution and regeneration possibilities. Biomater. Res. 2017, 21, 22. [Google Scholar] [CrossRef]
- Waxenbaum, J.A.; Reddy, V.; Futterman, B. Anatomy, Back, Intervertebral Discs. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022; Available online: http://www.ncbi.nlm.nih.gov/books/NBK470583 (accessed on 18 August 2022).
- Tonelotto, V.; Trapani, V.; Bretaud, S.; Heumüller, S.E.; Wagener, R.; Ruggiero, F.; Bonaldo, P. Spatio-temporal expression and distribution of collagen VI during zebrafish development. Sci. Rep. 2019, 9, 19851. [Google Scholar] [CrossRef]
- Mork, L.; Crump, G. Zebrafish Craniofacial Development: A Window into Early Patterning. Curr. Top. Dev. Biol. 2015, 115, 235–269. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Hohenester, E.; Zhang, R.; Gotta, S.; Speer, M.; Tandan, R.; Timpl, R.; Chu, M. A Bethlem myopathy Gly to Glu mutation in the von Willebrand factor A domain N2 of the collagen alpha3(VI) chain interferes with protein folding. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2000, 14, 761–768. [Google Scholar] [CrossRef]
- TPan, C.; Zhang, R.-Z.; Sudano, D.G.; Marie, S.K.; Bönnemann, C.G.; Chu, M.-L. New molecular mechanism for Ullrich congenital muscular dystrophy: A heterozygous in-frame deletion in the COL6A1 gene causes a severe phenotype. Am. J. Hum. Genet. 2003, 73, 355–369. [Google Scholar] [CrossRef]
- Demir, E.; Ferreiro, A.; Sabatelli, P.; Allamand, V.; Makri, S.; Echenne, B.; Maraldi, M.; Merlini, L.; Topaloglu, H.; Guicheney, P. Collagen VI status and clinical severity in Ullrich congenital muscular dystrophy: Phenotype analysis of 11 families linked to the COL6 loci. Neuropediatrics 2004, 35, 103–112. [Google Scholar] [CrossRef]
- Pullig, O.; Weseloh, G.; Swoboda, B. Expression of type VI collagen in normal and osteoarthritic human cartilage. Osteoarthr. Cartil. 1999, 7, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Nugent, A.E.; Speicher, D.M.; Gradisar, I.; McBurney, D.L.; Baraga, A.; Doane, K.J.; Horton, W.E., Jr. Advanced Osteoarthritis in Humans Is Associated With Altered Collagen VI Expression and Upregulation of ER-stress Markers Grp78 and Bag-1. J. Histochem. Cytochem. 2009, 57, 923–931. [Google Scholar] [CrossRef]
- Smeriglio, P.; Dhulipala, L.; Lai, J.H.; Goodman, S.B.; Dragoo, J.L.; Smith, R.L.; Maloney, W.J.; Yang, F.; Bhutani, N. Collagen VI Enhances Cartilage Tissue Generation by Stimulating Chondrocyte Proliferation. Tissue Eng. Part A 2015, 21, 840–849. [Google Scholar] [CrossRef]
- Bobzin, L.; Roberts, R.R.; Chen, H.-J.; Crump, J.G.; Merrill, A.E. Development and maintenance of tendons and ligaments. Dev. Camb. Engl. 2021, 148, dev186916. [Google Scholar] [CrossRef]
- Sardone, F.; Traina, F.; Tagliavini, F.; Pellegrini, C.; Merlini, L.; Squarzoni, S.; Santi, S.; Neri, S.; Faldini, C.; Maraldi, N.; et al. Effect of mechanical strain on the collagen VI pericellular matrix in anterior cruciate ligament fibroblasts. J. Cell. Physiol. 2014, 229, 878–886. [Google Scholar] [CrossRef]
- Kawahara, E.; Oda, Y.; Katsuda, S.; Nakanishi, I.; Aoyama, K.; Tomita, K. Microfilamentous type VI collagen in the hyalinized stroma of the hypertrophied ligamentum flavum. Virchows Arch. A Pathol. Anat. Histopathol. 1991, 419, 373–380. [Google Scholar] [CrossRef]
- Inamasu, J.; Guiot, B.H.; Sachs, D.C. Ossification of the posterior longitudinal ligament: An update on its biology, epidemiology, and natural history. Neurosurgery 2006, 58, 1027–1039. [Google Scholar] [CrossRef] [PubMed]
- Loughenbury, P.R.; Wadhwani, S.; Soames, R.W. The posterior longitudinal ligament and peridural (epidural) membrane. Clin. Anat. N. 2006, 19, 487–492. [Google Scholar] [CrossRef]
- Putz, R. Anatomic-functional viewpoints in treatment of injuries of the spine. Langenbecks Arch. Chir. Suppl. Kongressband Dtsch. Ges. Chir. Kongr. 1992, 1992, 256–262. [Google Scholar]
- Kong, Q.; Ma, X.; Li, F.; Guo, Z.; Qi, Q.; Li, W.; Yuan, H.-f.; Wang, Z.; Chen, Z. COL6A1 polymorphisms associated with ossification of the ligamentum flavum and ossification of the posterior longitudinal ligament. Spine 2007, 32, 2834–2838. [Google Scholar] [CrossRef]
- Okamoto, K.; Kobashi, G.; Washio, M.; Sasaki, S.; Yokoyama, T.; Miyake, Y.; Sakamoto, N.; Ohta, K.; Inaba, Y.; Tanaka, H. Dietary habits and risk of ossification of the posterior longitudinal ligaments of the spine (OPLL); findings from a case-control study in Japan. J. Bone Miner. Metab. 2004, 22, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Kobashi, G.; Washio, M.; Okamoto, K.; Sasaki, S.; Yokoyama, T.; Miyake, Y.; Sakamoto, N.; Ohta, K.; Inaba, Y.; Tanaka, H. High body mass index after age 20 and diabetes mellitus are independent risk factors for ossification of the posterior longitudinal ligament of the spine in Japanese subjects: A case-control study in multiple hospitals. Spine 2004, 29, 1006–1010. [Google Scholar] [CrossRef]
- Matsunaga, S.; Yamaguchi, M.; Hayashi, K.; Sakou, T. Genetic analysis of ossification of the posterior longitudinal ligament. Spine 1999, 24, 937–938; discussion 939. [Google Scholar] [CrossRef]
- Taketomi, E.; Sakou, T.; Matsunaga, S.; Yamaguchi, M. Family study of a twin with ossification of the posterior longitudinal ligament in the cervical spine. Spine 1992, 17, S55–S56. [Google Scholar] [CrossRef]
- Sakou, T.; Taketomi, E.; Matsunaga, S.; Yamaguchi, M.; Sonoda, S.; Yashiki, S. Genetic study of ossification of the posterior longitudinal ligament in the cervical spine with human leukocyte antigen haplotype. Spine 1991, 16, 1249–1252. [Google Scholar] [CrossRef]
- Tanaka, T.; Ikari, K.; Furushima, K.; Okada, A.; Tanaka, H.; Furukawa, K.-I.; Yoshida, K.; Ikeda, T.; Ikegawa, S.; Hunt, S.C.; et al. Genomewide linkage and linkage disequilibrium analyses identify COL6A1, on chromosome 21, as the locus for ossification of the posterior longitudinal ligament of the spine. Am. J. Hum. Genet. 2003, 73, 812–822. [Google Scholar] [CrossRef] [PubMed]
- Epstein, N.E. Ossification of the yellow ligament and spondylosis and/or ossification of the posterior longitudinal ligament of the thoracic and lumbar spine. J. Spinal Disord. 1999, 12, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Tsukahara, S.; Miyazawa, N.; Akagawa, H.; Forejtova, S.; Pavelka, K.; Tanaka, T.; Toh, S.; Tajima, A.; Akiyama, I.; Inoue, I. COL6A1, the candidate gene for ossification of the posterior longitudinal ligament, is associated with diffuse idiopathic skeletal hyperostosis in Japanese. Spine 2005, 30, 2321–2324. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Martino, A.; Cescon, M.; D’Agostino, C.; Schilardi, F.; Sabatelli, P.; Merlini, L.; Faldini, C. Collagen VI in the Musculoskeletal System. Int. J. Mol. Sci. 2023, 24, 5095. https://doi.org/10.3390/ijms24065095
Di Martino A, Cescon M, D’Agostino C, Schilardi F, Sabatelli P, Merlini L, Faldini C. Collagen VI in the Musculoskeletal System. International Journal of Molecular Sciences. 2023; 24(6):5095. https://doi.org/10.3390/ijms24065095
Chicago/Turabian StyleDi Martino, Alberto, Matilde Cescon, Claudio D’Agostino, Francesco Schilardi, Patrizia Sabatelli, Luciano Merlini, and Cesare Faldini. 2023. "Collagen VI in the Musculoskeletal System" International Journal of Molecular Sciences 24, no. 6: 5095. https://doi.org/10.3390/ijms24065095
APA StyleDi Martino, A., Cescon, M., D’Agostino, C., Schilardi, F., Sabatelli, P., Merlini, L., & Faldini, C. (2023). Collagen VI in the Musculoskeletal System. International Journal of Molecular Sciences, 24(6), 5095. https://doi.org/10.3390/ijms24065095







