Hot Melt Extrusion as an Effective Process in the Development of Mucoadhesive Tablets Containing Scutellariae baicalensis radix Extract and Chitosan Dedicated to the Treatment of Oral Infections
Abstract
1. Introduction
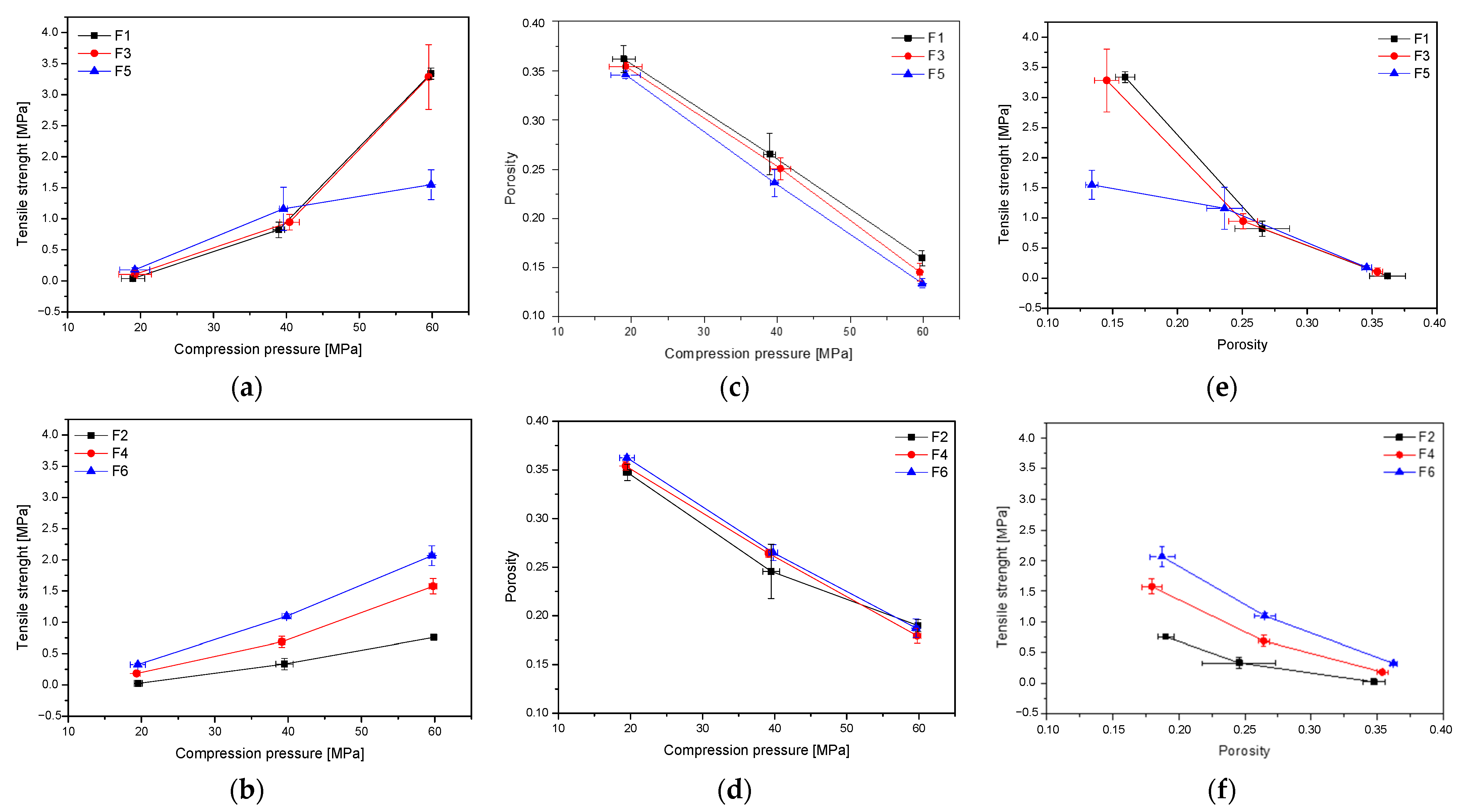
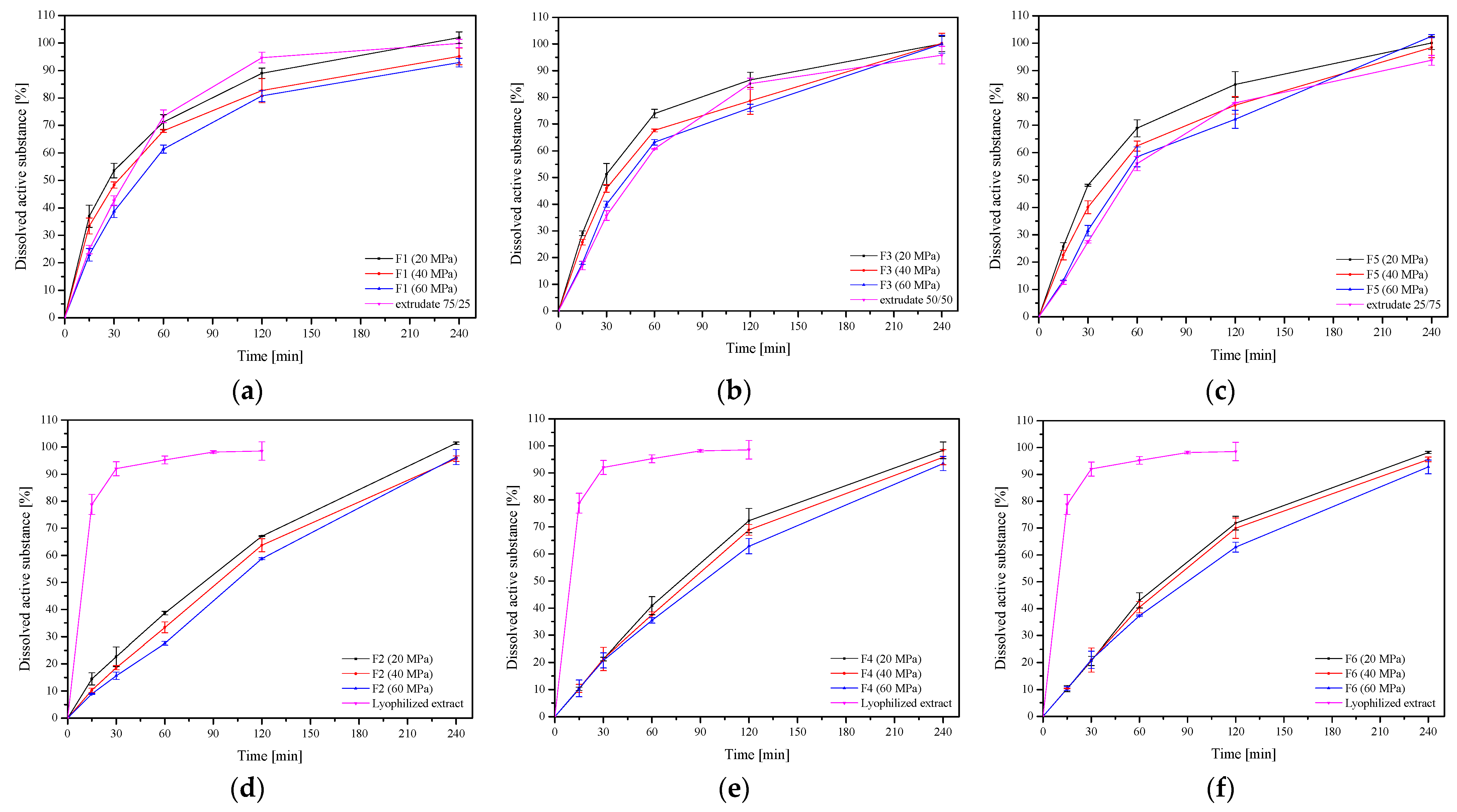
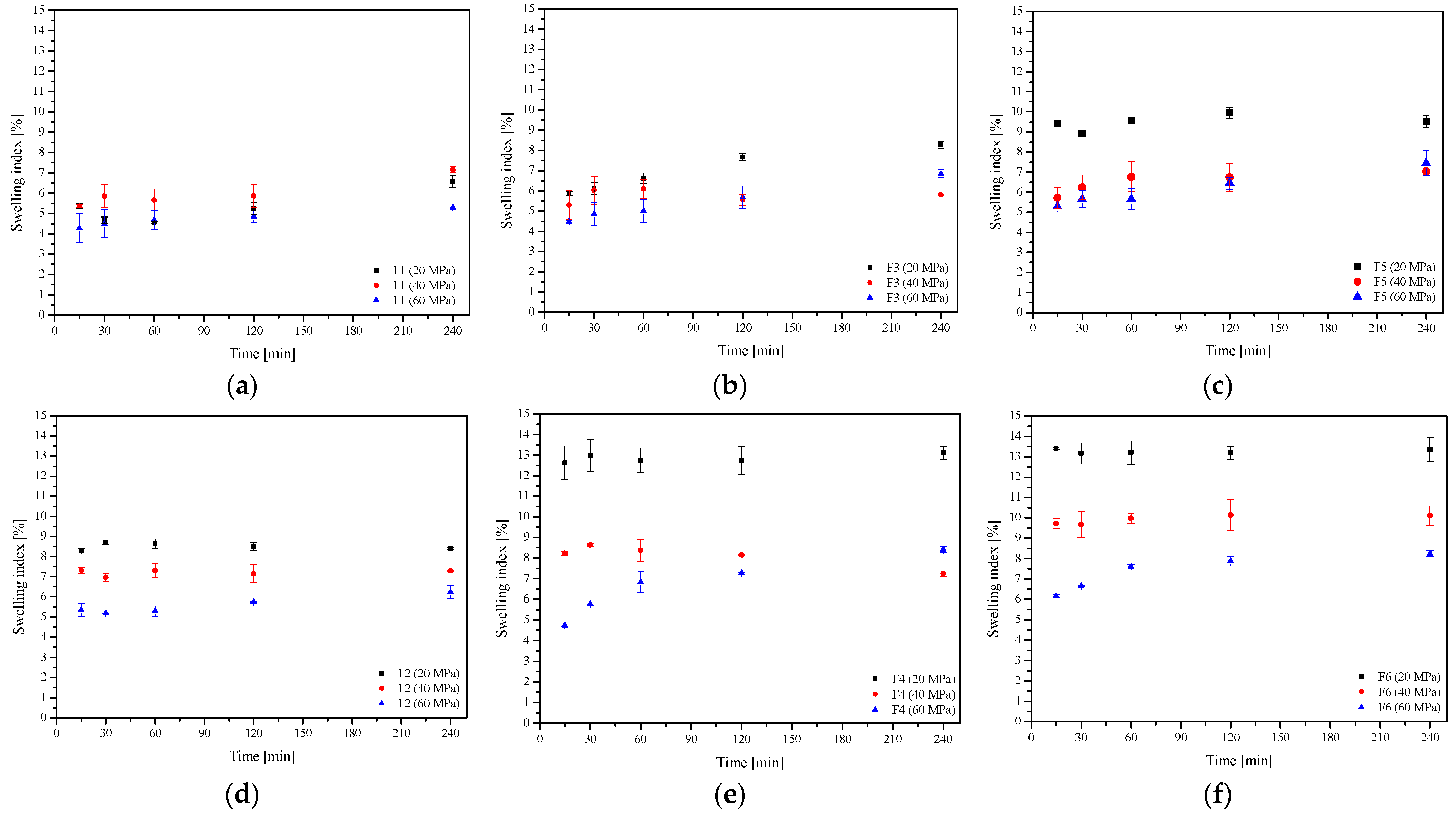
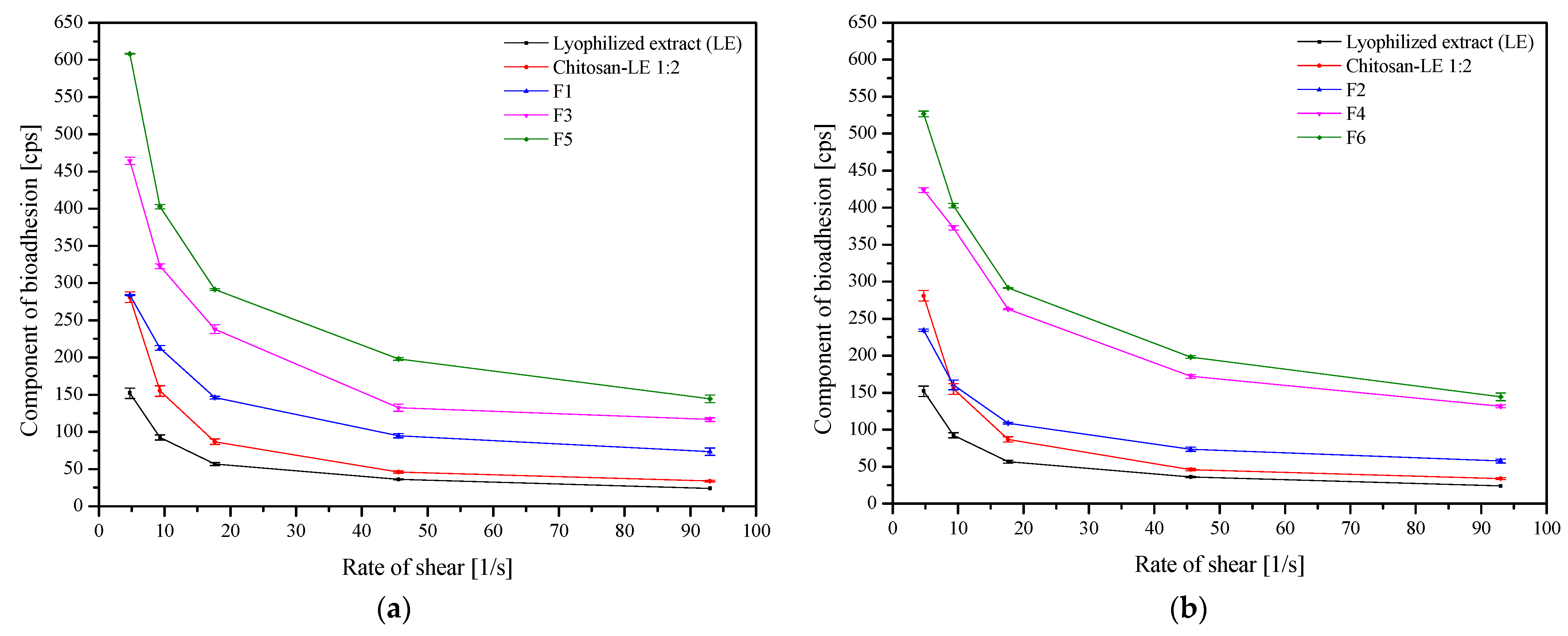
2. Results and Discussion
3. Materials and Methods
3.1. Plant Material
3.2. Chemicals and Reagents
3.3. Preparation of Solid Dispersion Systems
3.3.1. Preparation of Extract System
3.3.2. Hot Melt Extrusion (HME)
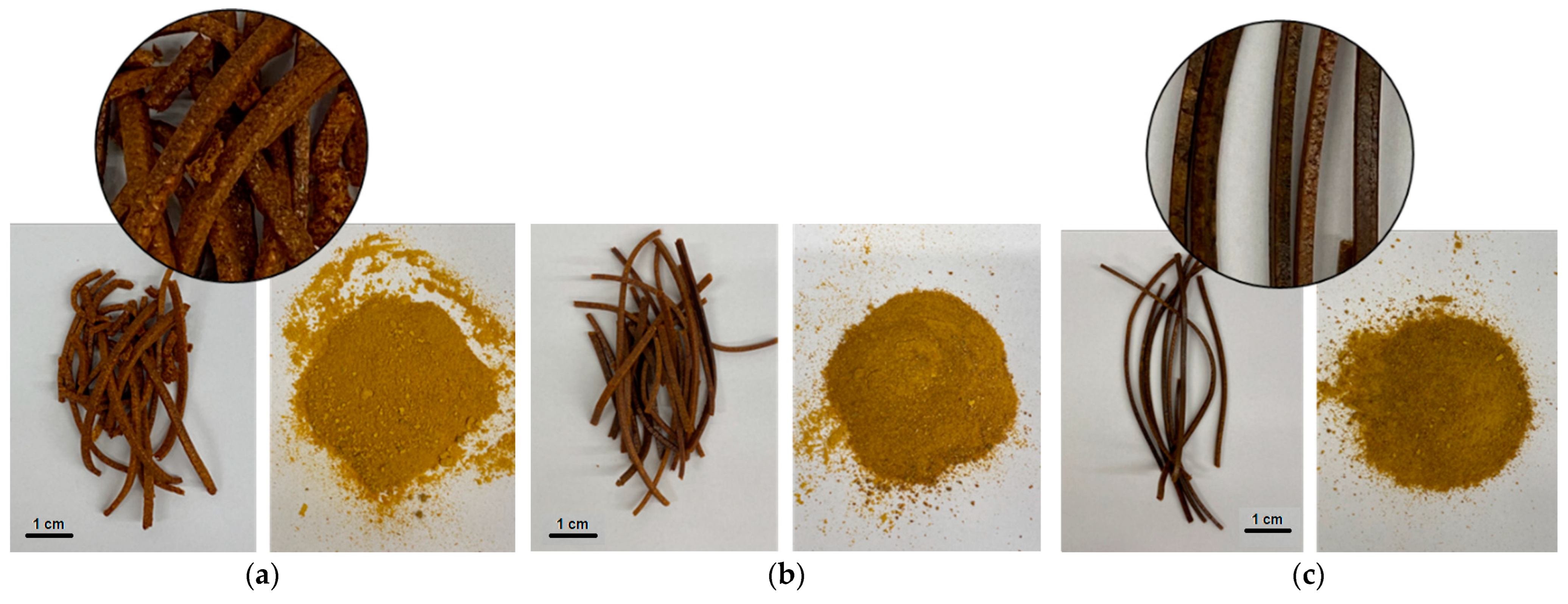
3.3.3. Extrudate Characterization
Powder X-ray Diffraction (PXRD)
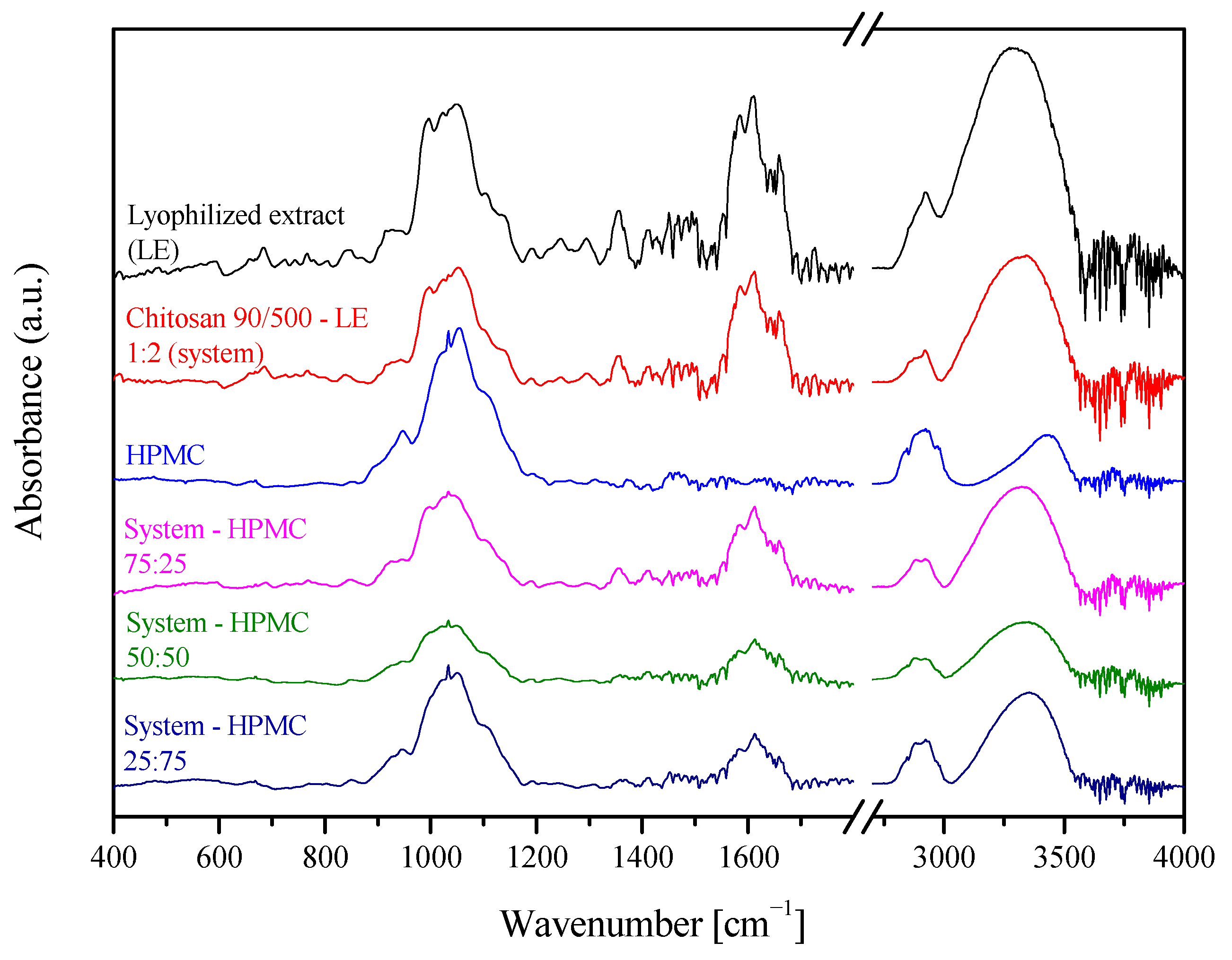
Fourier Transform Infrared Spectroscopy with Attenuated Total Reflectance (FTIR-ATR)
3.3.4. Determinations of Active Components Content
3.3.5. In Vitro Release Studies
3.3.6. Permeability Studies
3.3.7. Microbiological Activity Assay
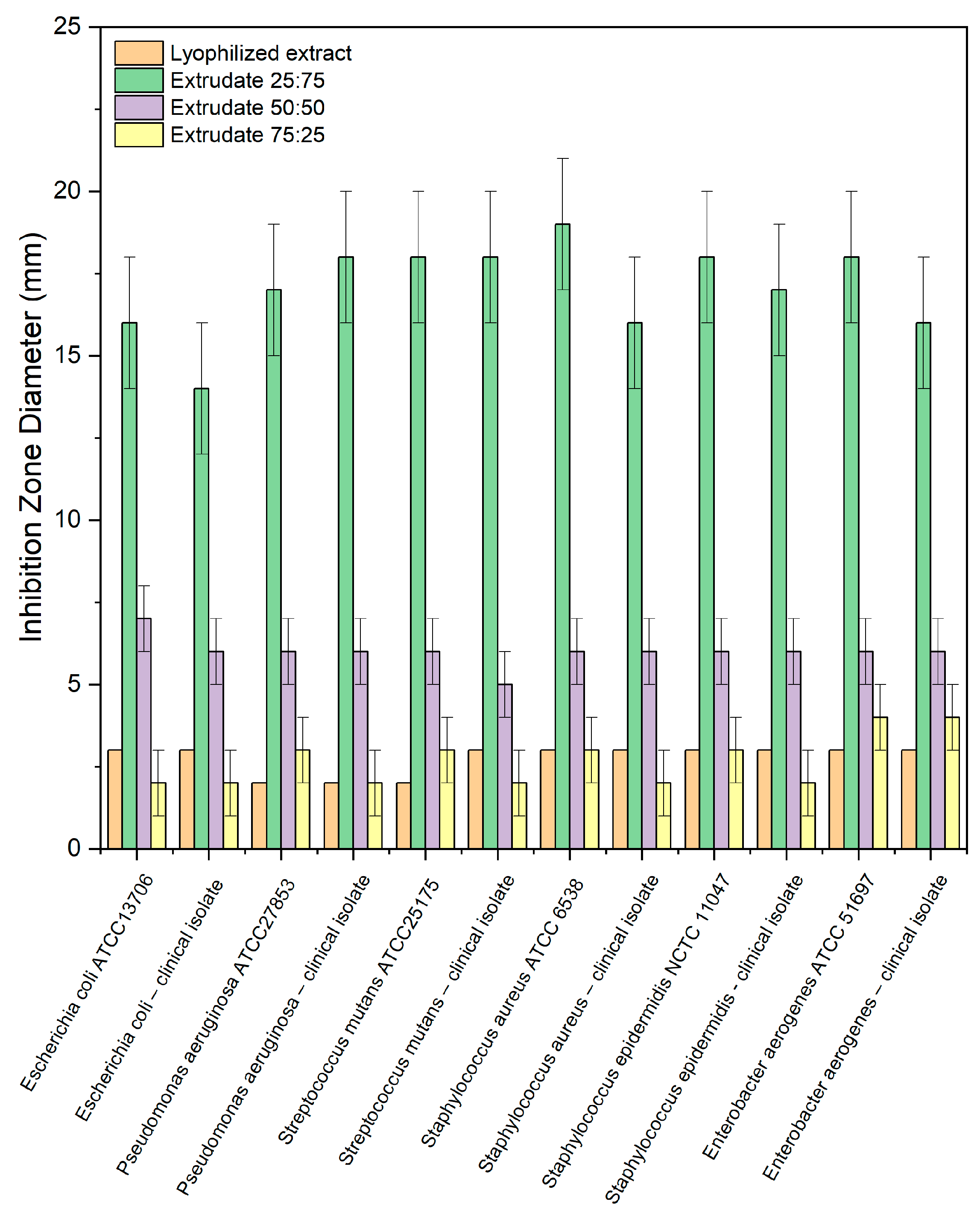
Well Diffusion Method
Liquid Culture Method
3.4. Tableting Process
3.4.1. Tablet Characterization
3.4.2. In Vitro Release Studies
3.4.3. Swelling Index
3.4.4. In Vitro Assessment of Mucin-Biopolymer Bioadhesive Bond Strength
3.4.5. Determination of the Residence Time
3.5. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oral Health. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 5 August 2022).
- Herrera, D.; Sanz, M.; Jepsen, S.; Needleman, I.; Roldán, S. A Systematic Review on the Effect of Systemic Antimicrobials as an Adjunct to Scaling and Root Planing in Periodontitis Patients. J. Clin. Periodontol. 2002, 29 (Suppl. 3), 136–159; discussion 160–162. [Google Scholar] [CrossRef]
- Hau, H.; Rohanizadeh, R.; Ghadiri, M.; Chrzanowski, W. A Mini-Review on Novel Intraperiodontal Pocket Drug Delivery Materials for the Treatment of Periodontal Diseases. Drug. Deliv. Transl. Res. 2014, 4, 295–301. [Google Scholar] [CrossRef]
- Wei, Y.; Deng, Y.; Ma, S.; Ran, M.; Jia, Y.; Meng, J.; Han, F.; Gou, J.; Yin, T.; He, H.; et al. Local Drug Delivery Systems as Therapeutic Strategies against Periodontitis: A Systematic Review. J. Control. Release 2021, 333, 269–282. [Google Scholar] [CrossRef]
- Zhao, Q.; Chen, X.-Y.; Martin, C. Scutellaria Baicalensis, the Golden Herb from the Garden of Chinese Medicinal Plants. Sci. Bull. 2016, 61, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Feng, L.; Zhang, Z.H.; Jia, X.B. The Anti-Inflammation Effect of Baicalin on Experimental Colitis through Inhibiting TLR4/NF-ΚB Pathway Activation. Int. Immunopharmacol. 2014, 23, 294–303. [Google Scholar] [CrossRef]
- Leung, K.C.-F.; Seneviratne, C.J.; Li, X.; Leung, P.C.; Lau, C.B.S.; Wong, C.-H.; Pang, K.Y.; Wong, C.W.; Wat, E.; Jin, L. Synergistic Antibacterial Effects of Nanoparticles Encapsulated with Scutellaria Baicalensis and Pure Chlorhexidine on Oral Bacterial Biofilms. Nanomaterials 2016, 6, 61. [Google Scholar] [CrossRef]
- Ren, M.; Zhao, Y.; He, Z.; Lin, J.; Xu, C.; Liu, F.; Hu, R.; Deng, H.; Wang, Y. Baicalein Inhibits Inflammatory Response and Promotes Osteogenic Activity in Periodontal Ligament Cells Challenged with Lipopolysaccharides. BMC Complement. Med. Ther. 2021, 21, 43. [Google Scholar] [CrossRef] [PubMed]
- Jakab, G.; Bogdán, D.; Mazák, K.; Deme, R.; Mucsi, Z.; Mándity, I.M.; Noszál, B.; Kállai-Szabó, N.; Antal, I. Physicochemical Profiling of Baicalin Along with the Development and Characterization of Cyclodextrin Inclusion Complexes. AAPS PharmSciTech 2019, 20, 314. [Google Scholar] [CrossRef] [PubMed]
- Ashour, E.A.; Majumdar, S.; Alsheteli, A.; Alshehri, S.; Alsulays, B.; Feng, X.; Gryczke, A.; Kolter, K.; Langley, N.; Repka, M.A. Hot Melt Extrusion as an Approach to Improve Solubility, Permeability and Oral Absorption of a Psychoactive Natural Product, Piperine. J. Pharm. Pharmacol. 2016, 68, 989–998. [Google Scholar] [CrossRef]
- Gao, N.; Guo, M.; Fu, Q.; He, Z. Application of Hot Melt Extrusion to Enhance the Dissolution and Oral Bioavailability of Oleanolic Acid. Asian J.Pharm. Sci. 2017, 12, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Patil, H.; Tiwari, R.V.; Repka, M.A. Hot-Melt Extrusion: From Theory to Application in Pharmaceutical Formulation. AAPS PharmSciTech 2015, 17, 20–42. [Google Scholar] [CrossRef] [PubMed]
- Simões, M.F.; Pinto, R.M.A.; Simões, S. Hot-Melt Extrusion in the Pharmaceutical Industry: Toward Filing a New Drug Application. Drug. Discov. Today 2019, 24, 1749–1768. [Google Scholar] [CrossRef] [PubMed]
- Paczkowska-Walendowska, M.; Cielecka-Piontek, J. Chitosan as a Functional Carrier for the Local Delivery Anti-Inflammatory Systems Containing Scutellariae Baicalensis Radix Extract. Pharmaceutics 2022, 14, 2148. [Google Scholar] [CrossRef]
- Wu, H.; Liu, Y.; Ci, T.; Ke, X. Application of HPMC HME Polymer as Hot Melt Extrusion Carrier in Carbamazepine Solid Dispersion. Drug. Dev. Ind. Pharm. 2020, 46, 1911–1918. [Google Scholar] [CrossRef]
- Krupa, A.; Cantin, O.; Strach, B.; Wyska, E.; Tabor, Z.; Siepmann, J.; Wróbel, A.; Jachowicz, R. In Vitro and in Vivo Behavior of Ground Tadalafil Hot-Melt Extrudates: How the Carrier Material Can Effectively Assure Rapid or Controlled Drug Release. Int. J. Pharm. 2017, 528, 498–510. [Google Scholar] [CrossRef]
- Bajwa, G.S.; Sammon, C.; Timmins, P.; Melia, C.D. Molecular and Mechanical Properties of Hydroxypropyl Methylcellulose Solutions during the Sol:Gel Transition. Polymer 2009, 50, 4571–4576. [Google Scholar] [CrossRef]
- Zhang, Y.; Luo, R.; Chen, Y.; Ke, X.; Hu, D.; Han, M. Application of Carrier and Plasticizer to Improve the Dissolution and Bioavailability of Poorly Water-Soluble Baicalein by Hot Melt Extrusion. AAPS PharmSciTech 2014, 15, 560–568. [Google Scholar] [CrossRef]
- Feng, Z.; Li, M.; Wang, W. Improvement of Dissolution and Tabletability of Carbamazepine Solid Dispersions with High Drug Loading Prepared by Hot-Melt Extrusion. Pharmazie 2019, 74, 523–528. [Google Scholar] [CrossRef]
- Li, C.L.; Martini, L.G.; Ford, J.L.; Roberts, M. The Use of Hypromellose in Oral Drug Delivery. J. Pharm. Pharmacol. 2005, 57, 533–546. [Google Scholar] [CrossRef]
- Chanaj-Kaczmarek, J.; Osmałek, T.; Szymańska, E.; Winnicka, K.; Karpiński, T.M.; Dyba, M.; Bekalarska-Dębek, M.; Cielecka-Piontek, J. Development and Evaluation of Thermosensitive Hydrogels with Binary Mixture of Scutellariae Baicalensis Radix Extract and Chitosan for Periodontal Diseases Treatment. Int. J. Mol. Sci. 2021, 22, 11319. [Google Scholar] [CrossRef]
- Joshi, S.C. Sol-Gel Behavior of Hydroxypropyl Methylcellulose (HPMC) in Ionic Media Including Drug Release. Materials 2011, 4, 1861–1905. [Google Scholar] [CrossRef]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic Modeling on Drug Release from Controlled Drug Delivery Systems. Acta Pol. Pharm. 2010, 67, 217–223. [Google Scholar]
- Fu, Y.; Kao, W.J. Drug Release Kinetics and Transport Mechanisms of Non-Degradable and Degradable Polymeric Delivery Systems. Expert. Opin. Drug. Deliv. 2010, 7, 429–444. [Google Scholar] [CrossRef]
- Menchicchi, B.; Fuenzalida, J.P.; Bobbili, K.B.; Hensel, A.; Swamy, M.J.; Goycoolea, F.M. Structure of Chitosan Determines Its Interactions with Mucin. Biomacromolecules 2014, 15, 3550–3558. [Google Scholar] [CrossRef] [PubMed]
- M. Ways, T.M.; Lau, W.M.; Khutoryanskiy, V.V. Chitosan and Its Derivatives for Application in Mucoadhesive Drug Delivery Systems. Polymers 2018, 10, 267. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Murthy, R.S.R. Effect of Different Polymer Concentration on Drug Release Rate and Physicochemical Properties of Mucoadhesive Gastroretentive Tablets. Indian. J. Pharm. Sci. 2015, 77, 705–714. [Google Scholar] [CrossRef]
- Chen, X.; Yan, J.; Yu, S.; Wang, P. Formulation and In Vitro Release Kinetics of Mucoadhesive Blend Gels Containing Matrine for Buccal Administration. AAPS PharmSciTech 2018, 19, 470–480. [Google Scholar] [CrossRef]
- Paczkowska-Walendowska, M.; Szymańska, E.; Winnicka, K.; Szwajgier, D.; Baranowska-Wójcik, E.; Ruchała, M.A.; Simon, M.; Cielecka-Piontek, J. Cyclodextrin as Functional Carrier in Development of Mucoadhesive Tablets Containing Polygoni Cuspidati Extract with Potential for Dental Applications. Pharmaceutics 2021, 13, 1916. [Google Scholar] [CrossRef] [PubMed]
- Bandi, S.P.; Bhatnagar, S.; Venuganti, V.V.K. Advanced Materials for Drug Delivery across Mucosal Barriers. Acta Biomater. 2021, 119, 13–29. [Google Scholar] [CrossRef]
- Tye, C.K.; Sun, C.C.; Amidon, G.E. Evaluation of the Effects of Tableting Speed on the Relationships between Compaction Pressure, Tablet Tensile Strength, and Tablet Solid Fraction. J. Pharm. Sci. 2005, 94, 465–472. [Google Scholar] [CrossRef]
- Costa, P.; Sousa Lobo, J.M. Modeling and Comparison of Dissolution Profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Hassan, E.E.; Gallo, J.M. A Simple Rheological Method for the in Vitro Assessment of Mucin-Polymer Bioadhesive Bond Strength. Pharm. Res. 1990, 7, 491–495. [Google Scholar] [CrossRef] [PubMed]
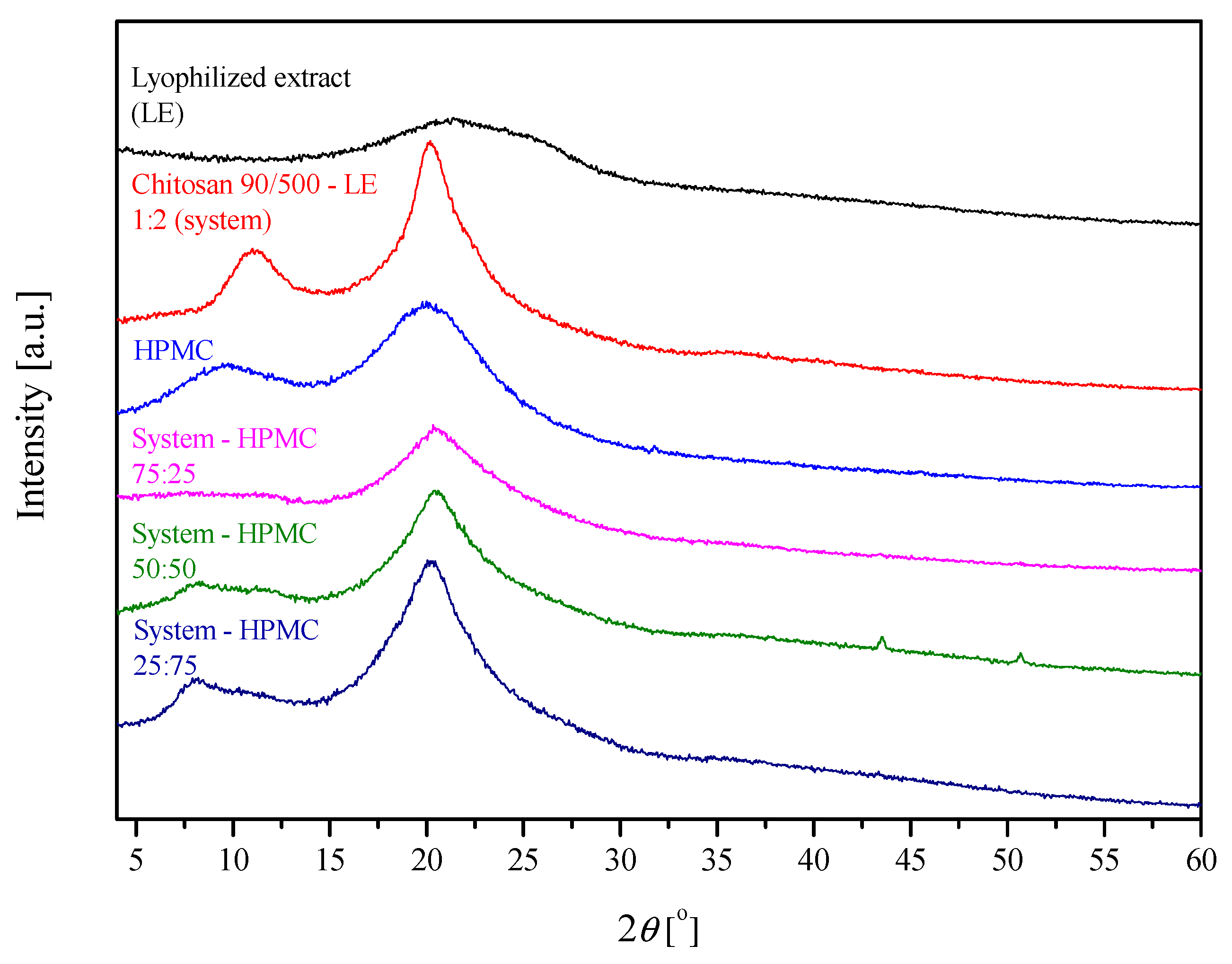

| Sample | Lyophilized Extract | Chitosan | HPMC | System-HPMC Extrudate 75:25 | System-HPMC Extrudate 50:50 | System-HPMC Extrudate 25:75 |
|---|---|---|---|---|---|---|
| (1) Peak position [2θ] | - | 11.14 | 9.77 | - | - | - |
| (2) Peak position [2θ] | 23.12 | 20.19 | 19.83 | 20.36 | 20.51 | 20.27 |
| Matrix peak position displacement [2θ] | - | - | - | - (2) 0.17 | - (2) 0.32 | - (2) 0.08 |
| Matrix peak position displacement [Å] | - | - | - | - (2) −0.03 | - (2) −0.07 | - (2) −0.02 |
| (1) Peak position [2θ] | - | 11.14 | 9.77 | - | - | - |
| (2) Peak position [2θ] | 23.12 | 20.19 | 19.83 | 20.36 | 20.51 | 20.27 |
| Matrix peak position displacement [2θ] | - | - | - | - (2) 0.17 | - (2) 0.32 | - (2) 0.08 |
| Lyophilized Extract | Extrudate 25:75 | Extrudate 50:50 | Extrudate 75:25 | |
|---|---|---|---|---|
| Number of microorganisms [CFU] | ||||
| Escherichia coli ATCC13706 | 6.9 × 102 → 3.9 × 107 | 4.8 × 102 → nd | 2.0 × 102 → 3.9 × 105 | 2.0 × 102 → 1.4 × 107 |
| Escherichia coli—clinical isolate | 3.4 × 102 → 5.1 × 107 | 2.0 × 102 → nd | 3.3 × 102 → 8.0 × 104 | 2.9 × 102 → 3.3 × 107 |
| Pseudomonas aeruginosa ATCC27853 | 2.1 × 102 → 5.9 × 107 | 2.7 × 102 → nd | 4.4 × 102 → 3.7 × 105 | 2.0 × 102 → 5.8 × 106 |
| Pseudomonas aeruginosa—clinical isolate | 2.5 × 102 → 6.0 × 106 | 2.0 × 102 → nd | 5.8 × 102 → 3.6 × 105 | 2.0 × 102 → 5.3 × 107 |
| Streptococcus mutans ATCC25175 | 6.9 × 102 → 3.9 × 107 | 4.8 × 102 → nd | 2.0 × 102 → 3.9 × 105 | 2.0 × 102 → 1.4 × 107 |
| Streptococcus mutans—clinical isolate | 3.4 × 102 → 5.1 × 107 | 2.0 × 102 → nd | 3.3 × 102 → 8.0 × 105 | 2.9 × 102 → 3.3 × 107 |
| Staphylococcus aureus ATCC 6538 | 2.6 × 102 → 3.0 × 107 | 3.6 × 102 → nd | 2.9 × 102 → 1.7 × 104 | 1.9 × 102 → 5.9 × 106 |
| Staphylococcus aureus—clinical isolate | 2.0 × 102 → 3.7 × 107 | 1.9 × 102 → nd | 2.6 × 102 → 3.0 × 105 | 3.4 × 102 → 3.0 × 106 |
| Staphylococcus epidermidis NCTC 11047 | 3.6 × 102 → 3.3 × 106 | 2.0 × 102 → nd | 2.5 × 102 → 3.2 × 104 | 2.1 × 102 → 3.6 × 107 |
| Staphylococcus epidermidis—clinical isolate | 7.7 × 102 → 8.5 × 104 | 2.9 × 102 → 3.3 × 102 | 3.4 × 102 → 5.1 × 104 | 2.9 × 102 → 3.0 × 108 |
| Enterobacter aerogenes ATCC 51697 | 2.6 × 102 → 3.0 × 105 | 3.6 × 102 → 3.0 × 102 | 2.9 × 102 → 1.7 × 105 | 1.9 × 102 → 5.9 × 106 |
| Enterobacter aerogenes—clinical isolate | 2.0 × 102 → 3.7 × 106 | 1.9 × 102 → nd | 2.6 × 102 → 3.0 × 104 | 3.4 × 102 → 3.0 × 106 |
| Formulation | F1 | F2 | F3 | F4 | F5 | F6 |
|---|---|---|---|---|---|---|
| Residence time (min) | 180 ± 5 | 220 ± 5 | 200 ± 5 | >240 | 220 ± 5 | >240 |
| Chitosan 90/500—Lyophilized Extract 1:2 (=System) | HPMC | |
|---|---|---|
| Ratio (w/w) | ||
| Extrudate 75:25 m/m | 75 | 25 |
| Extrudate 50:50 m/m | 50 | 50 |
| Extrudate 25:75 m/m | 25 | 75 |
| Formulation 1 (F1) | Formulation 2 (F2) | Formulation 3 (F3) | Formulation 4 (F4) | Formulation 5 (F5) | Formulation 6 (F6) | |
|---|---|---|---|---|---|---|
| Content (mg) per 1 tablet | ||||||
| Lyophilized extract—chitosan 90/500 2:1 w/w (=system) | - | 75.0 | - | 50.0 | - | 25.0 |
| HPMC 15.000 cP | - | 25.0 | - | 50.0 | - | 75.0 |
| System-HPMC 75:25 w/w extrudate | 100.0 | - | - | - | - | - |
| System-HPMC 50:50 w/w extrudate | - | - | 100.0 | - | - | - |
| System-HPMC 25:75 w/w extrudate | - | - | - | - | 100.0 | - |
| MCC | 20.0 | 20.0 | 20.0 | 20.0 | 20.0 | 20.0 |
| Stearate magnesium | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 |
| SUM | 121.2 | 121.2 | 121.2 | 121.2 | 121.2 | 121.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paczkowska-Walendowska, M.; Miklaszewski, A.; Szymanowska, D.; Skalicka-Woźniak, K.; Cielecka-Piontek, J. Hot Melt Extrusion as an Effective Process in the Development of Mucoadhesive Tablets Containing Scutellariae baicalensis radix Extract and Chitosan Dedicated to the Treatment of Oral Infections. Int. J. Mol. Sci. 2023, 24, 5834. https://doi.org/10.3390/ijms24065834
Paczkowska-Walendowska M, Miklaszewski A, Szymanowska D, Skalicka-Woźniak K, Cielecka-Piontek J. Hot Melt Extrusion as an Effective Process in the Development of Mucoadhesive Tablets Containing Scutellariae baicalensis radix Extract and Chitosan Dedicated to the Treatment of Oral Infections. International Journal of Molecular Sciences. 2023; 24(6):5834. https://doi.org/10.3390/ijms24065834
Chicago/Turabian StylePaczkowska-Walendowska, Magdalena, Andrzej Miklaszewski, Daria Szymanowska, Krystyna Skalicka-Woźniak, and Judyta Cielecka-Piontek. 2023. "Hot Melt Extrusion as an Effective Process in the Development of Mucoadhesive Tablets Containing Scutellariae baicalensis radix Extract and Chitosan Dedicated to the Treatment of Oral Infections" International Journal of Molecular Sciences 24, no. 6: 5834. https://doi.org/10.3390/ijms24065834
APA StylePaczkowska-Walendowska, M., Miklaszewski, A., Szymanowska, D., Skalicka-Woźniak, K., & Cielecka-Piontek, J. (2023). Hot Melt Extrusion as an Effective Process in the Development of Mucoadhesive Tablets Containing Scutellariae baicalensis radix Extract and Chitosan Dedicated to the Treatment of Oral Infections. International Journal of Molecular Sciences, 24(6), 5834. https://doi.org/10.3390/ijms24065834











