The “Asthma-Polycystic Ovary Overlap Syndrome” and the Therapeutic Role of Myo-Inositol
Abstract
:1. Introduction
| The European Society of Human Reproduction and Embryology and the American Society for Reproductive Medicine criteria (2003) [25]. (2 out of 3 criteria must be fulfilled) | Oligo/anovulation (oligomenorrhea or amenorrhea) | Clinical and/or biochemical hyperandrogenism | Polycystic ovaries (12 or more follicles, with a diameter of 2–9 mm and/or 10 mm ovarian volume) |
| The Androgen Excess and Polycystic Ovary Syndrome Society criteria (2009) [26]. (All criteria must be fulfilled) | Hyperandrogenism | Ovarian dysfunction (oligo-anovulation and/or polycystic ovaries) | Exclusion of other androgen-related disorders |
Asthma Endotypes
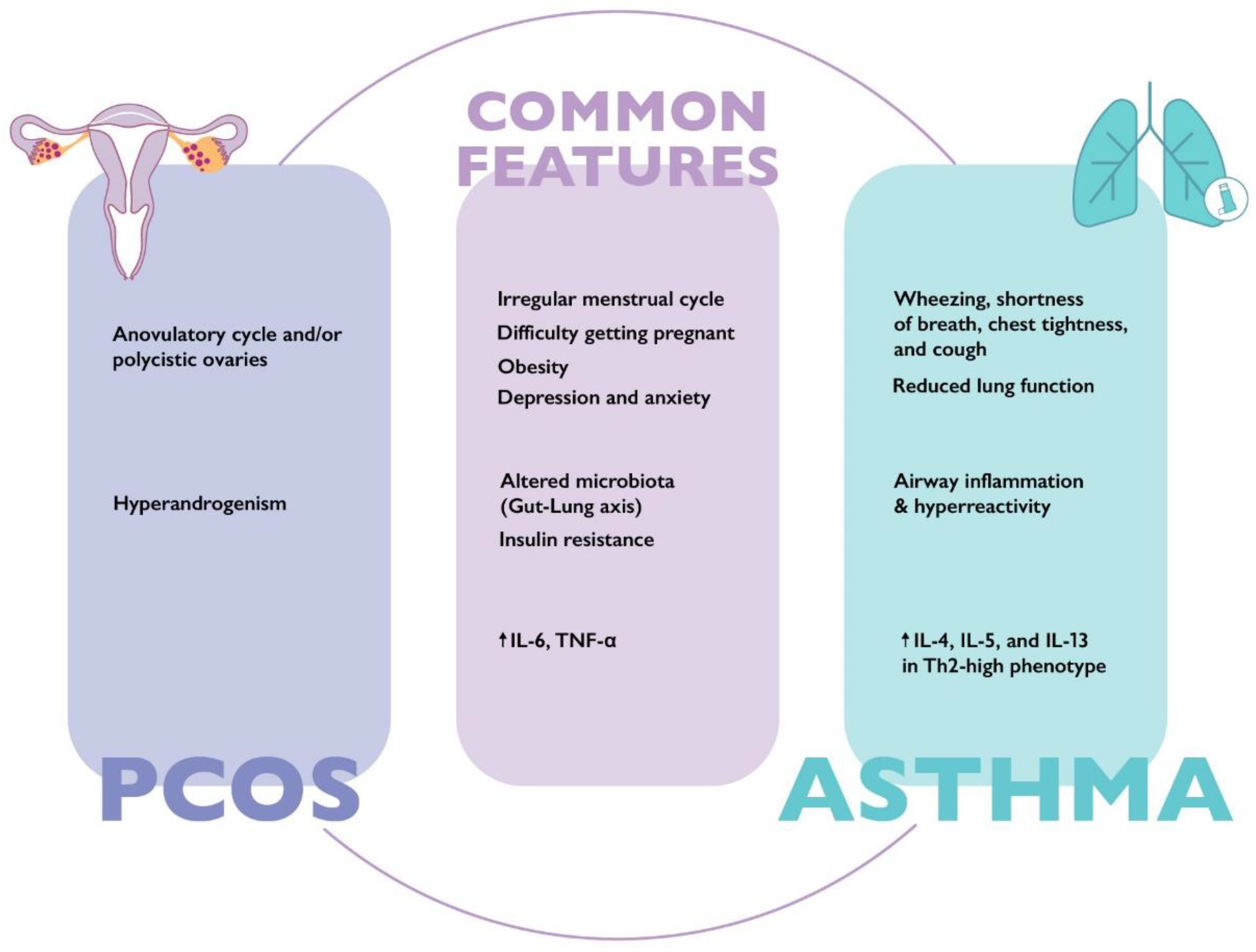
2. Clinical Overlap between Asthma and PCOS
2.1. Obesity
2.2. Insulin Resistance
2.3. Alterations in Gut Microbiota
2.4. Menstrual Cycle Abnormalities
2.5. Infertility
3. The Therapeutic Role of Myo-Inositol in Patients with “Asthma-PCOS Overlap Syndrome”
3.1. Structural and Functional Characteristics of Myo-Inositol
3.2. Therapeutic Role of Myo-Inositol in Lung Disorders
3.3. Routes of Drug Administration
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mattiuzzi, C.; Lippi, G. Worldwide asthma epidemiology: Insights from the Global Health Data Exchange database. Int. Forum. Allergy Rhinol. 2020, 10, 75–80. [Google Scholar] [CrossRef]
- Song, P.; Adeloye, D.; Salim, H.; Dos Santos, J.P.; Campbell, H.; Sheikh, A.; Rudan, I. Global, regional, and national prevalence of asthma in 2019: A systematic analysis and modelling study. J. Glob. Health 2022, 12, 04052. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Chen, S.; Chen, X.; Zou, W.; Liu, Z.; Wu, Y.; Hu, S. Global trends in the incidence and mortality of asthma from 1990 to 2019: An age-period-cohort analysis using the global burden of disease study 2019. Front. Public Health 2022, 10, 1036674. [Google Scholar] [CrossRef]
- Holgate, S.T.; Wenzel, S.; Postma, D.S.; Weiss, S.T.; Renz, H.; Sly, P.D. Asthma. Nat. Rev. Dis. Prim. 2015, 10, 15025. [Google Scholar] [CrossRef] [PubMed]
- Available online: www.ginasthma.org (accessed on 1 March 2023).
- Khatri, S.B.; Iaccarino, J.M.; Barochia, A.; Soghier, I.; Akuthota, P.; Brady, A.; Covar, R.A.; Debley, J.S.; Diamant, Z.; Fitzpatrick, A.M.; et al. American Thoracic Society Assembly on Allergy, Immunology, and Inflammation. Use of Fractional Exhaled Nitric Oxide to Guide the Treatment of Asthma: An Official American Thoracic Society Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2021, 204, 97–109. [Google Scholar]
- Kaplan, A.G.; Balter, M.S.; Bell, A.D.; Kim, H.; McIvor, R.A. Diagnosis of asthma in adults. CMAJ 2009, 181, E210–E220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varkonyi-Sepp, J.; Freeman, A.; Ainsworth, B.; Kadalayil, L.P.; Haitchi, H.M.; Kurukulaaratchy, R.J. Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome. J. Pers. Med. 2022, 12, 1435. [Google Scholar] [CrossRef]
- Graziottin, A.; Serafini, A. Perimenstrual asthma: From pathophysiology to treatment strategies. Multidiscip. Respir. Med. 2016, 11, 30. [Google Scholar] [CrossRef] [Green Version]
- Calcaterra, V.; Nappi, R.E.; Farolfi, A.; Tiranini, L.; Rossi, V.; Regalbuto, C.; Zuccotti, G. Perimenstrual Asthma in Adolescents: A Shared Condition in Pediatric and Gynecological Endocrinology. Children 2022, 9, 233. [Google Scholar] [CrossRef]
- Zhang, G.Q.; Ermis, S.S.O.; Rådinger, M.; Bossios, A.; Kankaanranta, H.; Nwaru, B. Sex Disparities in Asthma Development and Clinical Outcomes: Implications for Treatment Strategies. J. Asthma Allergy 2022, 15, 231–247. [Google Scholar] [CrossRef]
- Jenkins, C.R.; Boulet, L.P.; Lavoie, K.L.; Raherison-Semjen, C.; Singh, D. Personalized Treatment of Asthma: The Importance of Sex and Gender Differences. J. Allergy Clin. Immunol. Pract. 2022, 10, 963–971.e3. [Google Scholar] [CrossRef]
- Chowdhury, N.U.; Guntur, V.P.; Newcomb, D.C.; Wechsler, M.E. Sex and gender in asthma. Eur. Respir. Rev. 2021, 30, 210067. [Google Scholar] [CrossRef] [PubMed]
- Senna, G.; Latorre, M.; Bugiani, M.; Caminati, M.; Heffler, E.; Morrone, D.; Paoletti, G.; Parronchi, P.; Puggioni, F.; Blasi, F.; et al. Sex Differences in Severe Asthma: Results from Severe Asthma Network in Italy-SANI. Allergy Asthma. Immunol. Res. 2021, 13, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zhou, Z.Y.; Pan, J.X.; Huang, H.F. Associations Between Asthma and Polycystic Ovary Syndrome: Current Perspectives. Front. Endocrinol. 2022, 13, 936948. [Google Scholar] [CrossRef] [PubMed]
- Thuesen, B.H.; Husemoen, L.L.; Hersoug, L.G.; Pisinger, C.; Linneberg, A. Insulin resistance as a predictor of incident asthma-like symptoms in adults. Clin. Exp. Allergy 2009, 39, 700–707. [Google Scholar] [CrossRef]
- Rasquin Leon, L.I.; Anastasopoulou, C.; Mayrin, J.V. Polycystic Ovarian Disease; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Gibson-Helm, M.; Teede, H.; Dunaif, A.; Dokras, A. Delayed Diagnosis and a Lack of Information Associated with Dissatisfaction in Women With Polycystic Ovary Syndrome. J. Clin. Endocrinol. Metab. 2017, 102, 604–612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deswal, R.; Narwal, V.; Dang, A.; Pundir, C.S. The Prevalence of Polycystic Ovary Syndrome: A Brief Systematic Review. J. Hum. Reprod. Sci. 2020, 13, 261–271. [Google Scholar] [CrossRef]
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 2004, 81, 19–25. [Google Scholar] [CrossRef]
- Azziz, R.; Carmina, E.; Dewailly, D.; Diamanti-Kandarakis, E.; Escobar-Morreale, H.F.; Futterweit, W.; Janssen, O.E.; Legro, R.S.; Norman, R.J.; Taylor, A.E.; et al. Task Force on the Phenotype of the Polycystic Ovary Syndrome of The Androgen Excess and PCOS Society. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: The complete task force report. Fertil. Steril. 2009, 91, 456–488. [Google Scholar] [CrossRef]
- Louwers, Y.V.; Laven, J.S.E. Characteristics of polycystic ovary syndrome throughout life. Adv. Reprod. Health 2020, 14, 2633494120911038. [Google Scholar] [CrossRef]
- Çetinkaya Altuntaş, S.; Çelik, Ö.; Özer, Ü.; Çolak, S. Depression, anxiety, body image scores, and sexual dysfunction in patients with polycystic ovary syndrome according to phenotypes. Gynecol. Endocrinol. 2022, 38, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Htet, T.D.; Teede, H.J.; de Courten, B.; Loxton, D.; Real, F.G.; Moran, L.J.; Joham, A.E. Asthma in reproductive-aged women with polycystic ovary syndrome and association with obesity. Eur. Respir. J. 2017, 49, 1601334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, R.; Doherty, D.A. The potential implications of a PCOS diagnosis on a woman’s long-term health using data linkage. J. Clin. Endocrinol. Metab. 2015, 100, 911–919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glintborg, D.; Hass Rubin, K.; Nybo, M.; Abrahamsen, B.; Andersen, M. Morbidity and medicine prescriptions in a nationwide Danish population of patients diagnosed with polycystic ovary syndrome. Eur. J. Endocrinol. 2015, 172, 627–638. [Google Scholar] [CrossRef] [Green Version]
- Ricciardolo, F.L.M.; Sprio, A.E.; Baroso, A.; Gallo, F.; Riccardi, E.; Bertolini, F.; Carriero, V.; Arrigo, E.; Ciprandi, G. Characterization of T2-Low and T2-High asthma phenotypes in real-life. Biomedicines 2021, 9, 1684. [Google Scholar] [CrossRef]
- Wenzel, S.E. Asthma phenotypes: The evolution from clinical to molecular approaches. Nat. Med. 2012, 18, 716–725. [Google Scholar] [CrossRef]
- Logotheti, M.; Agioutantis, P.; Katsaounou, P.; Loutrari, H. Microbiome Research and Multi-Omics Integration for Personalized Medicine in Asthma. J. Pers. Med. 2021, 11, 1299. [Google Scholar] [CrossRef] [PubMed]
- Tantisira, K.G.; Weiss, S.T. Complex interactions in complex traits: Obesity and asthma. Thorax 2001, 56 (Suppl. S2), ii64–ii73. [Google Scholar]
- Thompson, C.A.; Eslick, S.R.; Berthon, B.S.; Wood, L.G. Asthma medication use in obese and healthy weight asthma: Systematic review/meta-analysis. Eur. Respir. J. 2021, 57, 2000612. [Google Scholar] [CrossRef] [PubMed]
- Peters-Golden, M.; Swern, A.; Bird, S.S.; Hustad, C.M.; Grant, E.; Edelman, J.M. Influence of body mass index on the response to asthma controller agents. Eur. Respir. J. 2006, 27, 495–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulet, L.P.; Franssen, E. Influence of obesity on response to fluticasone with or without salmeterol in moderate asthma. Respir. Med. 2007, 101, 2240–2247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, T.D.; Brigham, E.P.; Keet, C.A.; Brown, T.T.; Hansel, N.N.; McCormack, M.C. Association Between Prediabetes/Diabetes and Asthma Exacerbations in a Claims-Based Obese Asthma Cohort. J. Allergy. Clin. Immunol. Pract. 2019, 7, 1868–1873.e5. [Google Scholar] [CrossRef] [PubMed]
- Tiotiu, A.; Labor, M.; Nedeva, D.; Novakova, S.; Oguzulgen, I.K.; Mihaicuta, S.; Braido, F. How to apply the personalized medicine in obesity-associated asthma? Expert. Rev. Respir. Med. 2020, 14, 905–915. [Google Scholar] [CrossRef]
- Assad, N.; Qualls, C.; Smith, L.J.; Arynchyn, A.; Thyagarajan, B.; Schuyler, M.; Jacobs, D.R., Jr.; Sood, A. Body mass index is a stronger predictor than the metabolic syndrome for future asthma in women. The longitudinal CARDIA study. Am. J. Respir. Crit. Care Med. 2013, 188, 319–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glueck, C.G.; Goldenberg, N. Characteristics of obesity in polycystic ovary syndrome: Etiology, treatment, and genetics. Metabolism 2019, 92, 108–120. [Google Scholar] [CrossRef]
- Naderpoor, N.; Shorakae, S.; Joham, A.; Boyle, J.; De Courten, B.; Teede, H.J. Obesity and polycystic ovary syndrome. Minerva. Endocrinol. 2015, 40, 37–51. [Google Scholar]
- Carpaij, O.A.; van den Berge, M. The asthma-obesity relationship: Underlying mechanisms and treatment implications. Curr. Opin Pulm. Med. 2018, 24, 42–49. [Google Scholar] [CrossRef]
- Calixto, M.C.; Lintomen, L.; André, D.M.; Leiria, L.O.; Ferreira, D.; Lellis-Santos, C.; Anhê, G.F.; Bordin, S.; Landgraf, R.G.; Antunes, E. Metformin attenuates the exacerbation of the allergic eosinophilic inflammation in high fat-diet-induced obesity in mice. PLoS ONE 2013, 8, e76786. [Google Scholar] [CrossRef]
- Park, C.S.; Bang, B.R.; Kwon, H.S.; Moon, K.A.; Kim, T.B.; Lee, K.Y.; Moon, H.B.; Cho, Y.S. Metformin reduces airway inflammation and remodeling via activation of AMP-activated protein kinase. Biochem. Pharm. 2012, 84, 1660–1670. [Google Scholar] [CrossRef]
- Guo, Y.; Shi, J.; Wang, Q.; Hong, L.; Chen, M.; Liu, S.; Yuan, X.; Jiang, S. Metformin alleviates allergic airway inflammation and increases Treg cells in obese asthma. J. Cell. Mol. Med. 2021, 25, 2279–2284. [Google Scholar] [CrossRef]
- Ma, W.; Jin, Q.; Guo, H.; Han, X.; Xu, L.; Lu, S.; Wu, C. Corrigendum: Metformin Ameliorates Inflammation and Airway Remodeling of Experimental Allergic Asthma in Mice by Restoring AMPKα Activity. Front. Pharm. 2022, 21, 900127. [Google Scholar] [CrossRef]
- Wu, T.D.; Fawzy, A.; Akenroye, A.; Keet, C.; Hansel, N.N.; McCormack, M.C. Metformin Use and Risk of Asthma Exacerbation among Asthma Patients with Glycemic Dysfunction. J. Allergy Clin. Immunol. Pract. 2021, 9, 4014–4020.e4. [Google Scholar] [CrossRef]
- Wen, L.; Zhong, W.; Chai, Y.; Zhong, Q.; Gao, J.; Guan, L.; Zhang, M.; Huaiquan, L.; Haiyang, Y.; Qingxue, W.; et al. Association of Metformin Use with Asthma Exacerbation in Patients with Concurrent Asthma and Diabetes: A Systematic Review and Meta-Analysis of Observational Studies. Can. Respir. J. 2020, 2020, 9705604. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Loube, J.; Lee, R.; Bevans-Fonti, S.; Wu, T.D.; Barmine, J.H.; Jun, J.C.; McCormack, M.C.; Hansel, N.N.; Mitzner, W.; et al. Metformin Alleviates Airway Hyperresponsiveness in a Mouse Model of Diet-Induced Obesity. Front. Physiol. 2022, 13, 883275. [Google Scholar] [CrossRef] [PubMed]
- Calco, G.N.; Maung, J.N.; Jacoby, D.B.; Fryer, A.D.; Nie, Z. Insulin increases sensory nerve density and reflex bronchoconstriction in obese mice. JCI Insight. 2022, 24, e161898. [Google Scholar] [CrossRef] [PubMed]
- Barber, T.M.; Franks, S. Obesity, and polycystic ovary syndrome. Clin. Endocrinol. 2021, 95, 531–541. [Google Scholar] [CrossRef]
- Legro, R.S.; Castracane, V.D.; Kauffman, R.P. Detecting insulin resistance in polycystic ovary syndrome: Purposes and pitfalls. Obs. Gynecol. Surv. 2004, 59, 141–154. [Google Scholar] [CrossRef]
- Long, C.; Feng, H.; Duan, W.; Chen, X.; Zhao, Y.; Lan, Y.; Yue, R. Prevalence of polycystic ovary syndrome in patients with type 2 diabetes: A systematic review and meta-analysis. Front. Endocrinol. 2022, 13, 980405. [Google Scholar] [CrossRef]
- Lashen, H. Role of metformin in the management of polycystic ovary syndrome. Ther. Adv. Endocrinol. Metab. 2010, 1, 117–128. [Google Scholar] [CrossRef]
- Zhao, H.; Zhang, J.; Cheng, X.; Nie, X.; He, B. Insulin resistance in polycystic ovary syndrome across various tissues: An updated review of pathogenesis, evaluation, and treatment. J. Ovarian Res. 2023, 11, 9. [Google Scholar] [CrossRef] [PubMed]
- de Boer, G.M.; Tramper-Stranders, G.A.; Houweling, L.; van Zelst, C.M.; Pouw, N.; Verhoeven, G.T.; Boxma-de Klerk, B.M.; In ’t Veen, J.C.C.M.; van Rossum, E.F.C.; Hendriks, R.W.; et al. Adult but not childhood onset asthma is associated with the metabolic syndrome, independent from body mass index. Respir. Med. 2021, 188, 106603. [Google Scholar] [CrossRef] [PubMed]
- Karamzad, N.; Izadi, N.; Sanaie, S.; Ahmadian, E.; Eftekhari, A.; Sullman, M.J.M.; Safiri, S. Asthma and metabolic syndrome: A comprehensive systematic review and meta-analysis of observational studies. J. Cardiovasc. Thorac. Res. 2020, 12, 120–128. [Google Scholar] [CrossRef]
- Serafino-Agrusa, L.; Spatafora, M.; Scichilone, N. Asthma and metabolic syndrome: Current knowledge and future perspectives. World J. Clin. Cases 2015, 16, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Cardet, J.C.; Ash, S.; Kusa, T.; Camargo, C.A., Jr.; Israel, E. Insulin resistance modifies the association between obesity and current asthma in adults. Eur. Respir. J. 2016, 48, 403–410. [Google Scholar] [CrossRef] [Green Version]
- Huang, J.; Zhang, J.; Wang, X.; Jin, Z.; Zhang, P.; Su, H.; Sun, X. Effect of Probiotics on Respiratory Tract Allergic Disease and Gut Microbiota. Front. Nutr. 2022, 9, 821900. [Google Scholar] [CrossRef]
- Conlon, M.A.; Bird, A.R. The impact of diet and lifestyle on gut microbiota and human health. Nutrients 2014, 24, 17–44. [Google Scholar] [CrossRef] [PubMed]
- Tremellen, K.; Pearce, K. Dysbiosis of Gut Microbiota (DOGMA)—a novel theory for the development of polycystic ovarian syndrome. Med. Hypotheses 2012, 79, 104–112. [Google Scholar] [CrossRef]
- Molyneaux, P.L.; Cox, M.J.; Wells, A.U.; Kim, H.C.; Ji, W.; Cookson, W.O.C.; Moffatt, M.F.; Kim, D.S.; Toby, M.M. Changes in the respiratory microbiome during acute exacerbations of idiopathic pulmonary fibrosis. Respir. Res. 2017, 18, 29. [Google Scholar] [CrossRef] [Green Version]
- Ramírez-Labrada, A.G.; Isla, D.; Artal, A.; Arias, M.; Rezusta, A.; Pardo, J.; Gálvez, E.M. The influence of lung microbiota on lung carcinogenesis, immunity, and immunotherapy. Trends Cancer 2020, 6, 86–97. [Google Scholar] [CrossRef] [Green Version]
- Rastogi, S.; Mohanty, S.; Sharma, S.; Tripathi, P. Possible role of gut microbes and host’s immune response in gut-lung homeostasis. Front. Immunol. 2022, 13, 954339. [Google Scholar] [CrossRef]
- Liu, R.; Zhang, C.; Shi, Y.; Zhang, F.; Li, L.; Wang, X.; Ling, Y.; Fu, H.; Dong, W.; Shen, J.; et al. Dysbiosis of Gut Microbiota Associated with Clinical Parameters in Polycystic Ovary Syndrome. Front. Microbiol. 2017, 8, 324. [Google Scholar] [CrossRef]
- Lad, N.; Murphy, A.M.; Parenti, C.; Nelson, C.P.; Williams, N.C.; Sharpe, G.R.; McTernan, P.G. Asthma and obesity: Endotoxin another insult to add to injury? Clin. Sci. 2021, 135, 2729–2748. [Google Scholar] [CrossRef] [PubMed]
- Durack, J.; Lynch, S.V.; Nariya, S.; Bhakta, N.R.; Beigelman, A.; Castro, M.; Dyer, A.M.; Israel, E.; Kraft, M.; Martin, R.J.; et al. Features of the bronchial bacterial microbiome associated with atopy, asthma, and responsiveness to inhaled corticosteroid treatment. J. Allergy Clin. Immunol. 2017, 140, 63–75. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Ramos, J.L.; Pereira-Vega, A.R.; Alvarado-Gómez, F.; Maldonado-Pérez, J.A.; Svanes, C.; Gómez-Real, F. Risk factors for premenstrual asthma: A systematic review and meta-analysis. Expert Rev. Respir. Med. 2017, 11, 57–72. [Google Scholar] [CrossRef] [PubMed]
- Macsali, F.; Svanes, C.; Sothern, R.B.; Benediktsdottir, B.; Bjørge, L.; Dratva, J.; Franklin, K.A.; Holm, M.; Janson, C.; Johannessen, A.; et al. Menstrual cycle and respiratory symptoms in a general Nordic-Baltic population. Am. J. Respir. Crit. Care Med. 2013, 87, 366–373. [Google Scholar] [CrossRef]
- Yeung, E.H.; Zhang, C.; Mumford, S.L.; Ye, A.; Trevisan, M.; Chen, L.; Browne, R.W.; Wactawski-Wende, J.; Schisterman, E.F. Longitudinal study of insulin resistance and sex hormones over the menstrual cycle: The BioCycle Study. J. Clin. Endocrinol. Metab. 2010, 95, 5435–5442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ensom, M.H.; Chong, E.; Carter, D. Premenstrual symptoms in women with premenstrual asthma. Pharmacotherapy 1999, 19, 374–382. [Google Scholar] [CrossRef]
- Becerra-Diaz, M.; Song, M.; Heller, N. Androgen and Androgen Receptors as Regulators of Monocyte and Macrophage Biology in the Healthy and Diseased Lung. Front Immunol. 2020, 11, 1698. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.S.; McFarlane, L.C.; Lipworth, B.J. Modulation of airway reactivity and peak flow variability in asthmatics receiving the oral contraceptive pill. Am. J. Respir. Crit. Care Med. 1997, 155, 1273–12737. [Google Scholar] [CrossRef]
- Svanes, C.; Real, F.G.; Gislason, T.; Jansson, C.; Jögi, R.; Norrman, E.; Nyström, L.; Torén, K.; Omenaas, E. Association of asthma and hay fever with irregular menstruation. Thorax 2005, 60, 445–450. [Google Scholar] [CrossRef] [Green Version]
- Nejatbakhsh Samimi, L.; Fallahpour, M.; Khoshmirsafa, M.; Moosavi, S.A.J.; Bayati, P.; Baharlou, R.; Falak, R. The impact of 17β-estradiol and progesterone therapy on peripheral blood mononuclear cells of asthmatic patients. Mol. Biol. Rep. 2021, 48, 297–306. [Google Scholar] [CrossRef]
- Collée, J.; Mawet, M.; Tebache, L.; Nisolle, M.; Brichant, G. Polycystic ovarian syndrome and infertility: Overview and insights of the putative treatments. Gynecol. Endocrinol. 2021, 37, 869–874. [Google Scholar] [CrossRef]
- Gade, E.J.; Thomsen, S.F.; Lindenberg, S.; Backer, V. Female asthma has a negative effect on fertility: What is the connection? ISRN Allergy 2014, 27, 131092. [Google Scholar]
- Jöud, A.; Nilsson-Condori, E.; Schmidt, L.; Ziebe, S.; Vassard, D.; Mattsson, K. Infertility, pregnancy loss and assisted reproduction in women with asthma: A population-based cohort study. Hum. Reprod. 2022, 37, 2932–2941. [Google Scholar] [CrossRef] [PubMed]
- Bláfoss, J.; Hansen, A.V.; Malchau Lauesgaard, S.S.; Ali, Z.; Ulrik, C.S. Female asthma and atopy-impact on fertility: A systematic review. J. Asthma Allergy 2019, 12, 205–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gade, E.J.; Thomsen, S.F.; Lindenberg, S.; Backer, V. Fertility outcomes in asthma: A clinical study of 245 women with unexplained infertility. Eur. Respir. J. 2016, 47, 1144–1151. [Google Scholar] [CrossRef] [Green Version]
- Vejen Hansen, A.; Ali, Z.; Malchau, S.S.; Blafoss, J.; Pinborg, A.; Ulrik, C.S. Fertility treatment among women with asthma: A case-control study of 3689 women with live births. Eur. Respir. J. 2019, 53, 1800597. [Google Scholar] [CrossRef] [PubMed]
- Altun, T.; Jindal, S.; Greenseid, K.; Shu, J.; Pal, L. Low follicular fluid IL-6 levels in IVF patients are associated with increased likelihood of clinical pregnancy. J. Assist. Reprod. Genet. 2011, 28, 245–251. [Google Scholar] [CrossRef] [Green Version]
- Galazios, G.; Tsoulou, S.; Zografou, C.; Tripsianis, G.; Koutlaki, N.; Papazoglou, D.; Tsikouras, P.; Maltezos, E.; Liberis, V. The role of cytokines IL-6 and IL-8 in the pathogenesis of spontaneous abortions. J. Matern. Fetal. Neonatal. Med. 2011, 24, 1283–1285. [Google Scholar] [CrossRef] [PubMed]
- Unfer, V.; Nestler, J.E.; Kamenov, Z.A.; Prapas, N.; Facchinetti, F. Effects of Inositol(s) in Women with PCOS: A Systematic Review of Randomized Controlled Trials. Int. J. Endocrinol. 2016, 2016, 1849162. [Google Scholar] [CrossRef] [Green Version]
- Kamenov, Z.; Gateva, A. Inositols in PCOS. Molecules 2020, 27, 5566. [Google Scholar] [CrossRef] [PubMed]
- Cantelmi, T.; Lambiase, E.; Unfer, V.R.; Gambioli, R.; Unfer, V. Inositol treatment for psychological symptoms in Polycystic Ovary Syndrome women. Eur. Rev. Med. Pharm. Sci. 2021, 25, 2383–2389. [Google Scholar]
- Pkhaladze, L.; Russo, M.; Unfer, V.; Nordio, M.; Basciani, S.; Khomasuridze, A. Treatment of lean PCOS teenagers: A follow-up comparison between Myo-Inositol and oral contraceptives. Eur. Rev. Med. Pharm. Sci. 2021, 25, 7476–7485. [Google Scholar]
- Merviel, P.; James, P.; Bouée, S.; Le Guillou, M.; Rince, C.; Nachtergaele, C.; Kerlan, V. Impact of myo-inositol treatment in women with polycystic ovary syndrome in assisted reproductive technologies. Reprod. Health 2021, 19, 13. [Google Scholar] [CrossRef]
- Elsaid, S.; Rubin-Kahana, D.S.; Kloiber, S.; Kennedy, S.H.; Chavez, S.; Le Foll, B. Neurochemical Alterations in Social Anxiety Disorder (SAD): A Systematic Review of Proton Magnetic Resonance Spectroscopic Studies. Int. J. Mol. Sci. 2022, 26, 4754. [Google Scholar] [CrossRef]
- Taylor, C.W.; Tovey, S.C. IP(3) receptors: Toward understanding their activation. Cold Spring Harb. Perspect. Biol. 2010, 2, a004010. [Google Scholar] [CrossRef] [PubMed]
- Cappelli, V.; Musacchio, M.C.; Bulfoni, A.; Morgante, G.; De Leo, V. Natural molecules for the therapy of hyperandrogenism and metabolic disorders in PCOS. Eur. Rev. Med. Pharm. Sci. 2017, 21 (Suppl. S2), 15–29. [Google Scholar]
- Benvenga, S.; Antonelli, A. Inositol(s) in thyroid function, growth, and autoimmunity. Rev. Endocr. Metab. Disord. 2016, 17, 471–484. [Google Scholar] [CrossRef]
- Pundir, J.; Psaroudakis, D.; Savnur, P.; Bhide, P.; Sabatini, L.; Teede, H.; Coomarasamy, A.; Thangaratinam, S. Inositol treatment of anovulation in women with polycystic ovary syndrome: A meta-analysis of randomised trials. BJOG 2018, 125, 299–308. [Google Scholar] [CrossRef] [Green Version]
- Vartanyan, E.V.; Tsaturova, K.A.; Devyatova, E.A.; Mikhaylyukova, A.S.; Levin, V.A.; Petuhova, N.L.; Markin, A.V.; Steptsova, E.M. Improvement in quality of oocytes in polycystic ovarian syndrome in programs of in vitro fertilization. Gynecol. Endocrinol. 2017, 33 (Suppl. S1), 8–11. [Google Scholar] [CrossRef] [Green Version]
- Regidor, P.A.; Schindler, A.E. Myoinositol as a Safe and Alternative Approach in the Treatment of Infertile PCOS Women: A German Observational Study. Int. J. Endocrinol. 2016, 2016, 9537632. [Google Scholar] [CrossRef]
- Zacchè, M.M.; Caputo, L.; Filippis, S.; Zacchè, G.; Dindelli, M.; Ferrari, A. Efficacy of myo-inositol in the treatment of cutaneous disorders in young women with polycystic ovary syndrome. Gynecol. Endocrinol. 2009, 25, 508–513. [Google Scholar] [CrossRef]
- Minozzi, M.; D’Andrea, G.; Unfer, V. Treatment of hirsutism with myo-inositol: A prospective clinical study. Reprod. Biomed. Online 2008, 17, 579–582. [Google Scholar] [CrossRef]
- Vitagliano, A.; Saccone, G.; Cosmi, E.; Visentin, S.; Dessole, F.; Ambrosini, G.; Berghella, V. Inositol for the prevention of gestational diabetes: A systematic review and meta-analysis of randomized controlled trials. Arch. Gynecol. Obs. 2019, 299, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Carlomagno, G.; Unfer, V. Inositol safety: Clinical evidences. Eur. Rev. Med. Pharm. Sci. 2011, 15, 931–936. [Google Scholar]
- Genazzani, A.D.; Santagni, S.; Ricchieri, F.; Campedelli, A.; Rattighieri, E.; Chierchia, E.; Marini, G.; Despini, G.; Prati, A.; Simoncini, T. Myo-inositol modulates insulin and luteinizing hormone secretion in normal weight patients with polycystic ovary syndrome. J. Obs. Gynaecol. Res. 2014, 40, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Unfer, V.; Facchinetti, F.; Orrù, B.; Giordani, B.; Nestler, J. Myo-inositol effects in women with PCOS: A meta-analysis of randomized controlled trials. Endocr. Connect. 2017, 6, 647–658. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.Q.; Xing, C.; He, B. Short period-administration of myo-inositol and metformin on hormonal and glycolipid profiles in patients with polycystic ovary syndrome: A systematic review and updated meta-analysis of randomized controlled trials. Eur. Rev. Med. Pharm. Sci. 2022, 26, 1792–1802. [Google Scholar]
- Unfer, V.; Porcaro, G. Updates on the myo-inositol plus D-chiro-inositol combined therapy in polycystic ovary syndrome. Expert Rev. Clin. Pharm. 2014, 7, 623–631. [Google Scholar] [CrossRef]
- Crouch, E.; Wright, J.R. Surfactant proteins a and d and pulmonary host defense. Annu. Rev. Physiol. 2001, 63, 521–554. [Google Scholar] [CrossRef]
- Lugogo, N.; Francisco, D.; Addison, K.J.; Manne, A.; Pederson, W.; Ingram, J.L.; Green, C.L.; Suratt, B.T.; Lee, J.J.; Sunday, M.E.; et al. Obese asthmatic patients have decreased surfactant protein A levels: Mechanisms and implications. J. Allergy Clin. Immunol. 2018, 141, 918–926.e3. [Google Scholar] [CrossRef] [Green Version]
- Kwatia, M.A.; Doyle, C.B.; Cho, W.; Enhorning, G.; Ackerman, S.J. Combined activities of secretory phospholipases and eosinophil lysophospholipases induce pulmonary surfactant dysfunction by phospholipid hydrolysis. J. Allergy Clin. Immunol. 2007, 119, 838–847. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, Y.; Kuroki, Y.; Akino, T. Pulmonary surfactant protein D specifically binds to phosphatidylinositol. J. Biol. Chem. 1992, 267, 21244–21249. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, Y.; McCormack, F.X.; Mason, R.J.; Voelker, D.R. Chimeras of surfactant proteins A and D identify the carbohydrate recognition domains as essential for phospholipid interaction. J. Biol. Chem. 1994, 269, 29785–29792. [Google Scholar] [CrossRef]
- Lam, S.; McWilliams, A.; LeRiche, J.; MacAulay, C.; Wattenberg, L.; Szabo, E. A phase I study of myo-inositol for lung cancer chemoprevention. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1526–1531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, S.; Mandrekar, S.J.; Gesthalter, Y.; Allen Ziegler, K.L.; Seisler, D.K.; Midthun, D.E.; Mao, J.T.; Aubry, M.C.; McWilliams, A.; Sin, D.D.; et al. Cancer Prevention Network. A Randomized Phase IIb Trial of myo-Inositol in Smokers with Bronchial Dysplasia. Cancer Prev. Res. 2016, 9, 906–914. [Google Scholar] [CrossRef] [Green Version]
- Laganà, A.S.; Unfer, V.; Garzon, S.; Bizzarri, M. Role of inositol to improve surfactant functions and reduce IL-6 levels: A potential adjuvant strategy for SARS-CoV-2 pneumonia? Med. Hypotheses 2020, 144, 110262. [Google Scholar] [CrossRef]
- Hallman, M.; Bry, K.; Hoppu, K.; Lappi, M.; Pohjavuori, M. Inositol supplementation in premature infants with respiratory distress syndrome. N. Engl. J. Med. 1992, 326, 1233–1239. [Google Scholar] [CrossRef]
- Spengler, D.; Winoto-Morbach, S.; Kupsch, S.; Vock, C.; Blöchle, K.; Frank, S.; Rintz, N.; Diekötter, M.; Janga, H.; Weckmann, M.; et al. Novel therapeutic roles for surfactant-inositols and-phosphatidylglycerols in a neonatal piglet ARDS model: A translational study. Am. J. Physiol. Lung Cell. Mol. Physiol. 2018, 314, L32–L53. [Google Scholar] [CrossRef]
- Howlett, A.; Ohlsson, A.; Plakkal, N. Inositol in preterm infants at risk for or having respiratory distress syndrome. Cochrane Database Syst. Rev. 2015, 2, CD000366. [Google Scholar] [CrossRef]
- Baldassarre, M.P.A.; Di Tomo, P.; Centorame, G.; Pandolfi, A.; Di Pietro, N.; Consoli, A.; Formoso, G. Myoinositol Reduces Inflammation and Oxidative Stress in Human Endothelial Cells Exposed In Vivo to Chronic Hyperglycemia. Nutrients 2021, 13, 2210. [Google Scholar] [CrossRef] [PubMed]
- Gagliardo, R.; Chanez, P.; Mathieu, M.; Bruno, A.; Costanzo, G.; Gougat, C.; Vachier, I.; Bousquet, J.; Bonsignore, G.; Vignola, A.M. Persistent activation of nuclear factor-kappaB signaling pathway in severe uncontrolled asthma. Am. J. Respir. Crit. Care Med. 2003, 168, 1190–1198. [Google Scholar] [CrossRef] [Green Version]
- Alipour, S.; Mahmoudi, L.; Ahmadi, F. Pulmonary drug delivery: An effective and convenient delivery route to combat COVID-19. Drug Deliv. Transl. Res. 2022, 19, 1–11. [Google Scholar] [CrossRef]
- Spiga, A. Nebulized myo-Inositol increases oxygen saturation and relieves symptoms in patients with airways diseases. IJMDAT 2021, 4, e356. [Google Scholar]
- Orrù, B.; Circo, R.; Logoteta, P.; Petousis, S.; Carlomagno, G. Finding the best therapeutic approach for PCOS: The importance of inositol(s) bioavailability. Eur. Rev. Med. Pharm. Sci. 2017, 21 (Suppl. S2), 83–88. [Google Scholar]
- Dinicola, S.; Minini, M.; Unfer, V.; Verna, R.; Cucina, A.; Bizzarri, M. Nutritional and Acquired Deficiencies in Inositol Bioavailability. Correlations with Metabolic Disorders. Int. J. Mol. Sci. 2017, 18, 2187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Grazia, S.; Carlomagno, G.; Unfer, V.; Cavalli, P. Myo-inositol soft gel capsules may prevent the risk of coffee-induced neural tube defects. Expert Opin. Drug Deliv. 2012, 9, 1033–1039. [Google Scholar] [CrossRef]
- Kamenov, Z.; Kolarov, G.; Gateva, A.; Carlomagno, G.; Genazzani, A.D. Ovulation induction with myo-inositol alone and in combination with clomiphene citrate in polycystic ovarian syndrome patients with insulin resistance. Gynecol. Endocrinol. 2015, 31, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Raffone, E.; Rizzo, P.; Benedetto, V. Insulin sensitiser agents alone and in co-treatment with r-FSH for ovulation induction in PCOS women. Gynecol. Endocrinol. 2010, 26, 275–280. [Google Scholar] [CrossRef]
- Gerli, S.; Papaleo, E.; Ferrari, A.; Di Renzo, G.C. Randomized, double blind placebo-controlled trial: Effects of myo-inositol on ovarian function and metabolic factors in women with PCOS. Eur. Rev. Med. Pharm. Sci. 2007, 11, 347–354. [Google Scholar]
- Grases, F.; Simonet, B.M.; Vucenik, I.; Prieto, R.M.; Costa-Bauzá, A.; March, J.G.; Shamsuddin, A.M. Absorption and excretion of orally administered inositol hexaphosphate (IP(6) or phytate) in humans. Biofactors 2001, 15, 53–61. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Yoshida, K.; Uchida, M. Novel functions of bovine milk-derived alpha-lactalbumin: Anti-nociceptive and anti-inflammatory activity caused by inhibiting cyclooxygenase-2 and phospholipase A2. Biol. Pharm. Bull. 2009, 32, 366–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monastra, G.; Sambuy, Y.; Ferruzza, S.; Ferrari, D.; Ranaldi, G. Alpha-lactalbumin Effect on Myo-inositol Intestinal Absorption: In vivo and In vitro. Curr. Drug Deliv. 2018, 15, 1305–1311. [Google Scholar] [CrossRef]
- Montanino Oliva, M.; Buonomo, G.; Calcagno, M.; Unfer, V. Effects of myo-inositol plus alpha-lactalbumin in myo-inositol-resistant PCOS women. J. Ovarian Res. 2018, 10, 38. [Google Scholar] [CrossRef]
- Manish, R.P.; Jignesh, S.; Varsha, N. The Role of Alpha-Lactalbumin with Myoinositol in the Treatment of PCOS: A Review. Asian Res. J. Gynaecol. Obs. 2022, 8, 5–11. [Google Scholar]
- Izumi, H.; Ishizuka, S.; Inafune, A.; Hira, T.; Ozawa, K.; Shimizu, T.; Takase, M.; Hara, H. Alpha-Lactalbumin hydrolysate stimulates glucagon-like peptide-2 secretion and small intestinal growth in suckling rats. J. Nutr. 2009, 139, 1322–1327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Förster, C. Tight junctions and the modulation of barrier function in disease. Histochem. Cell Biol. 2008, 130, 55–70. [Google Scholar] [CrossRef] [Green Version]
- Lemmer, H.J.; Hamman, J.H. Paracellular drug absorption enhancement through tight junction modulation. Expert Opin. Drug Deliv. 2013, 10, 103–114. [Google Scholar] [CrossRef]
- Cardinale, V.; Lepore, E.; Basciani, S.; Artale, S.; Nordio, M.; Bizzarri, M.; Unfer, V. Positive Effects of α-Lactalbumin in the Management of Symptoms of Polycystic Ovary Syndrome. Nutrients 2022, 14, 3220. [Google Scholar] [CrossRef]
- D’Anna, R.; Corrado, F.; Loddo, S.; Gullo, G.; Giunta, L.; Di Benedetto, A. Myoinositol plus α-lactalbumin supplementation, insulin resistance and birth outcomes in women with gestational diabetes mellitus: A randomized, controlled study. Sci. Rep. 2021, 11, 8866. [Google Scholar] [CrossRef] [PubMed]
- Hernandez Marin, I.; Picconi, O.; Laganà, A.S.; Costabile, L.; Unfer, V. A multicenter clinical study with myo-inositol and alpha-lactalbumin in Mexican and Italian PCOS patients. Eur. Rev. Med. Pharm. Sci. 2021, 25, 3316–3324. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guarnieri, G.; Iervolino, M.; Cavallone, S.; Unfer, V.; Vianello, A. The “Asthma-Polycystic Ovary Overlap Syndrome” and the Therapeutic Role of Myo-Inositol. Int. J. Mol. Sci. 2023, 24, 6959. https://doi.org/10.3390/ijms24086959
Guarnieri G, Iervolino M, Cavallone S, Unfer V, Vianello A. The “Asthma-Polycystic Ovary Overlap Syndrome” and the Therapeutic Role of Myo-Inositol. International Journal of Molecular Sciences. 2023; 24(8):6959. https://doi.org/10.3390/ijms24086959
Chicago/Turabian StyleGuarnieri, Gabriella, Matteo Iervolino, Sara Cavallone, Vittorio Unfer, and Andrea Vianello. 2023. "The “Asthma-Polycystic Ovary Overlap Syndrome” and the Therapeutic Role of Myo-Inositol" International Journal of Molecular Sciences 24, no. 8: 6959. https://doi.org/10.3390/ijms24086959





