Changes in Lipid Metabolism Enzymes in Rat Epididymal Fat after Chronic Central Leptin Infusion Are Related to Alterations in Inflammation and Insulin Signaling
Abstract
:1. Introduction
2. Results
2.1. Characteristics of the Experimental Groups
2.2. Leptin Reduces Peripheral NEFAs and Triglycerides (TG)
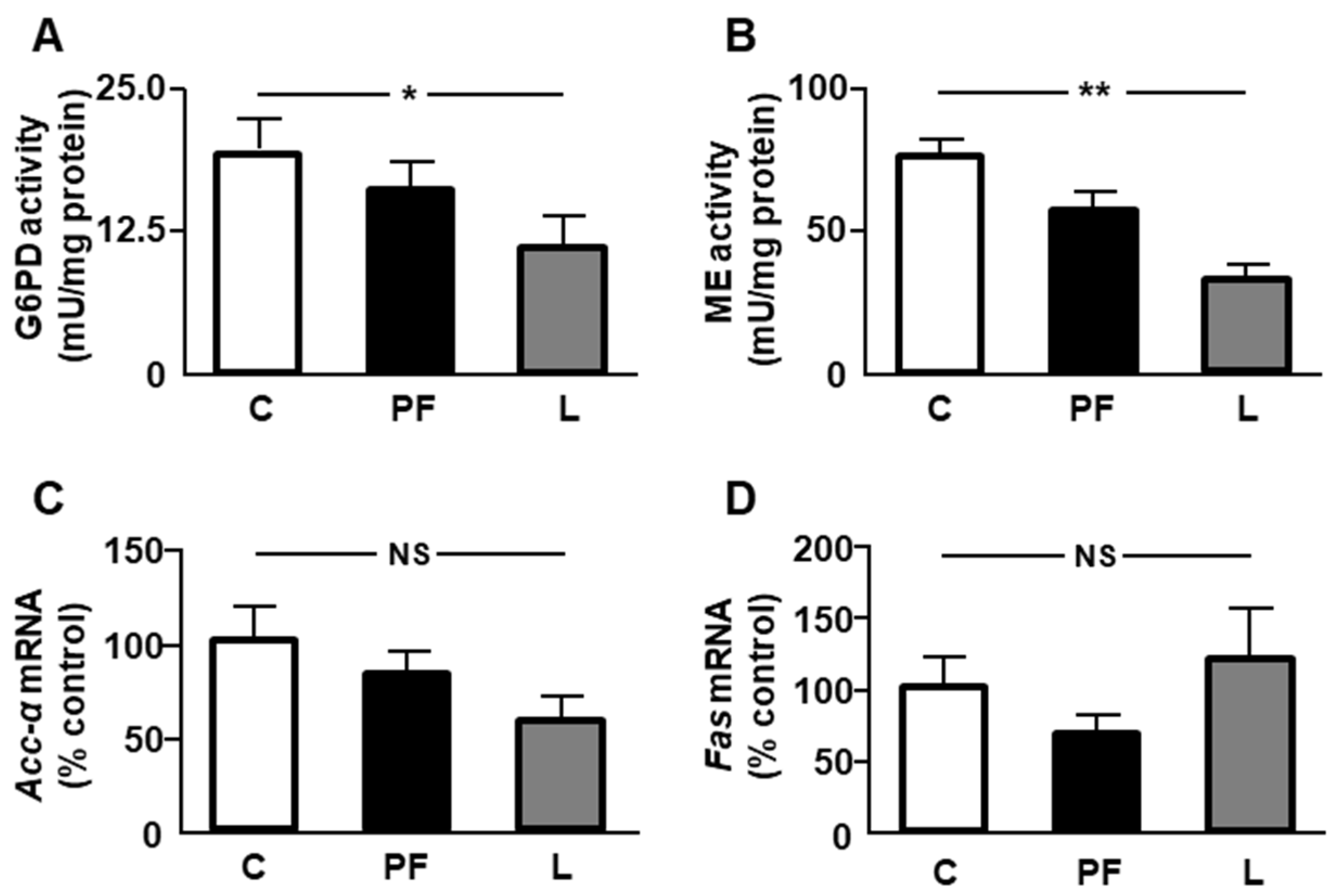
2.3. Effect of Leptin Infusion on Lipid Anabolism-Related Parameters in Epididymal Fat
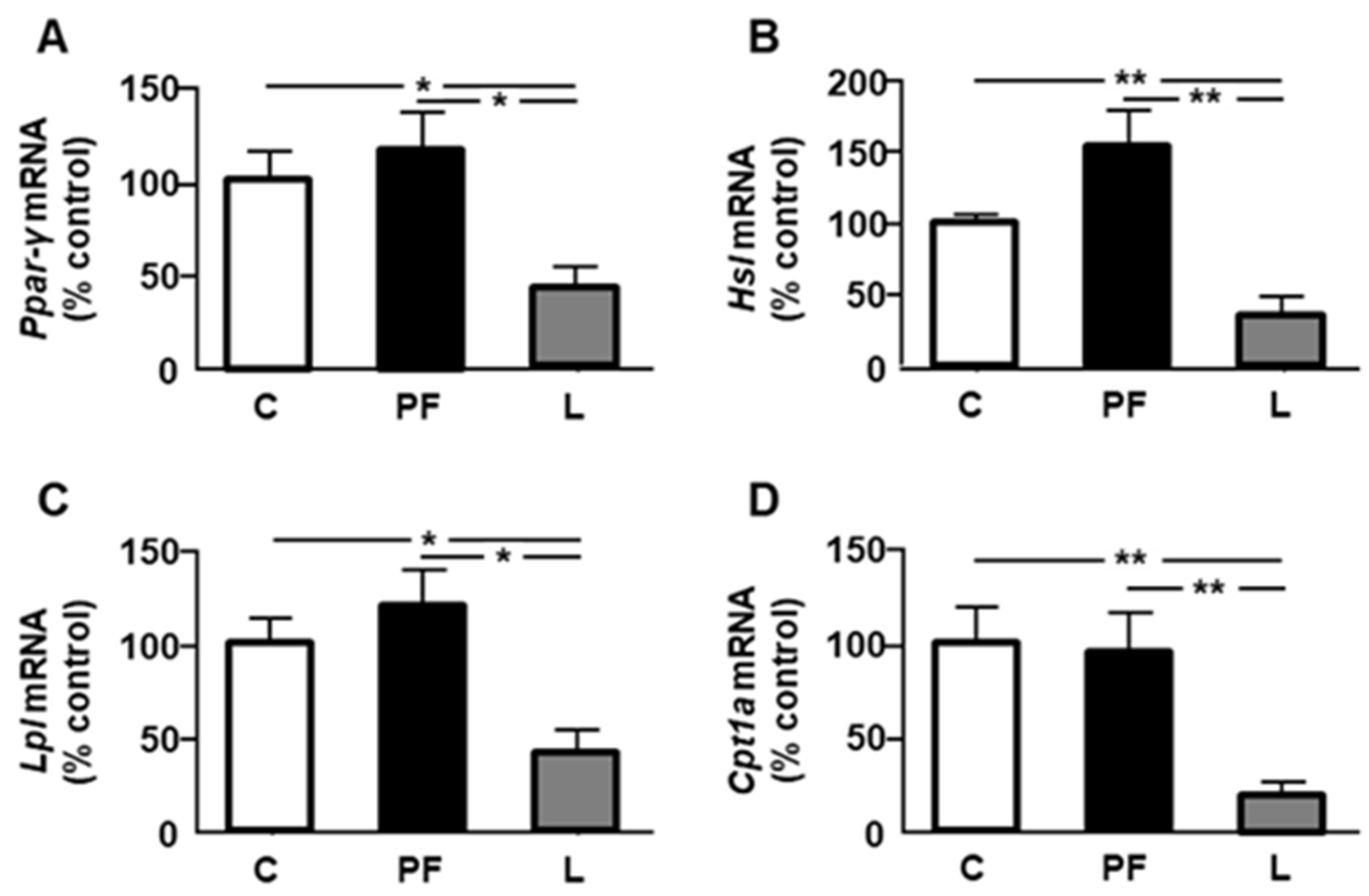
2.4. Leptin Infusion Reduces the Expression of PPAR-γ and Lipid Metabolic Markers in Epididymal Fat
2.5. Chronic Leptin Increases Activation of Inflammatory Signaling Targets in Epididymal Fat
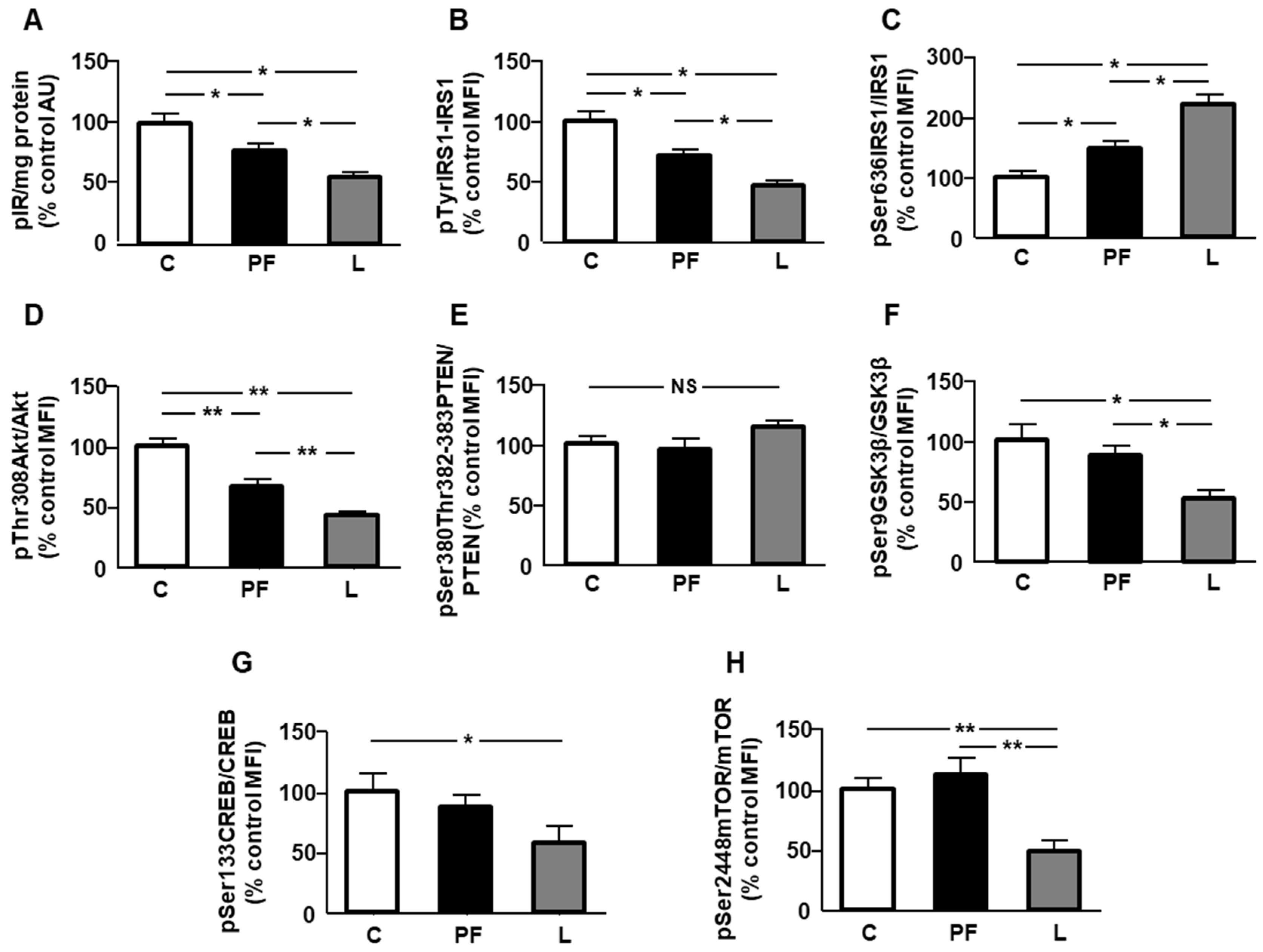
2.6. Leptin Reduced Insulin-Related Signaling in Epididymal Fat
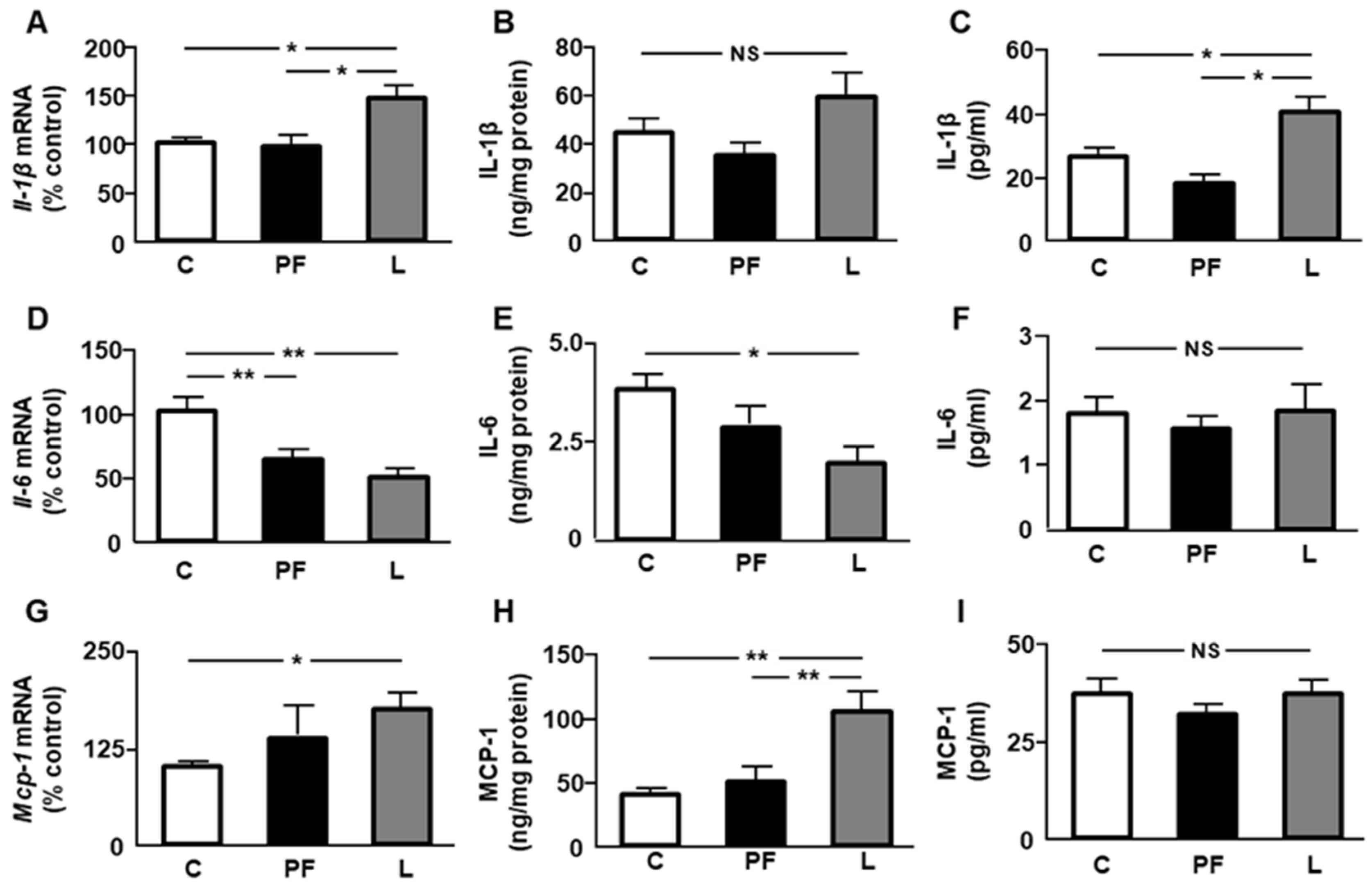
2.7. Changes in Inflammatory Markers after Leptin Infusion
2.8. Leptin Induces Changes in Anti-Inflammatory Interleukins
2.9. Correlation of Inflammatory Targets and Markers of Insulin Sensitivity with the Expression of Enzymes of Lipid Metabolism
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Animals Treatment and Experimental Design
4.3. Tissue Homogenization and Protein Quantification
4.4. Serum NEFAs and TGs Levels
4.5. ELISA
4.6. Multiplexed Bead Immunoassay
4.7. Enzyme Activity Assays
4.7.1. Glucose-6-Phosphate Dehydrogenase
4.7.2. Malic Enzyme
4.8. RNA Purification and Real Time PCR Analysis
4.9. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACC-α | Acetyl CoA carboxylase-α |
| Akt | Protein kinase B |
| CPT1A | Carnitine palmitoyl-transferase 1A |
| CREB | cAMP-response element binding protein |
| FAS | Fatty acid synthase |
| GSK3β | Glycogen synthase kinase 3β |
| G6PD | Glucose-6-phosphate dehydrogenase |
| HSL | Hormone-sensitive lipase |
| icv | Intracerebroventricular |
| IL | Interleukin |
| IR | Insulin receptor |
| IRS1 | Insulin receptor substrate 1 |
| JNK | c-Jun N-terminal kinase |
| LPL | Lipoprotein lipase |
| MCP-1 | Monocyte chemoattractant protein-1 |
| ME | Malic enzyme |
| mTOR | Mechanistic target of rapamycin |
| NADPH | Reduced nicotinamide adenine dinucleotide phosphate |
| NFkB | Nuclear factor kappa B |
| PF | Pair-fed |
| PPARγ | Peroxisome proliferator-activated receptor-γ |
| PTEN | Phosphatase and tensin homolog homolog deleted on chromosome 10 |
| p38MAPK | p38 mitogen-activated protein kinase |
| STAT3 | Signal transducer and activator of transcription 3 |
References
- Morais, J.B.S.; Dias, T.M.D.S.; Cardoso, B.E.P.; de Paiva Sousa, M.; Sousa, T.G.V.; Araújo, D.S.C.; Marreiro, D.D.N. Adipose tissue dysfunction: Impact on metabolic changes? Horm. Metab. Res. 2022, 54, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Gabriely, I.; Ma, X.H.; Yang, X.M.; Atzmon, G.; Rajala, M.W.; Berg, A.H.; Scherer, P.; Rossetti, L.; Barzilai, N. Removal of visceral fat prevents insulin resistance and glucose intolerance of aging: An adipokine-mediated process? Diabetes 2002, 51, 2951–2958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, S.; Hocking, S.; Watt, M.J.; Gunton, J.E. Metabolic effects of lipectomy and of adipose tissue transplantation. Obesity 2023, 31, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Narita, T.; Kobayashi, M.; Itakura, K.; Itagawa, R.; Kabaya, R.; Sudo, Y.; Okita, N.; Higami, Y. Differential response to caloric restriction of retroperitoneal, epididymal, and subcutaneous adipose tissue depots in rats. Exp. Gerontol. 2018, 104, 127–137. [Google Scholar] [CrossRef]
- Martins, F.F.; Marinho, T.S.; Cardoso, L.E.M.; Barbosa-da-Silva, S.; Souza-Mello, V.; Aguila, M.B.; Mandarim-de-Lacerda, C.A. Semaglutide (GLP-1 receptor agonist) stimulates browning on subcutaneous fat adipocytes and mitigates inflammation and endoplasmic reticulum stress in visceral fat adipocytes of obese mice. Cell. Biochem. Funct. 2022, 40, 903–913. [Google Scholar] [CrossRef]
- Wang, J.L.; Chinookoswong, N.; Scully, S.; Qi, M.; Shi, Z.Q. Differential effects of leptin in regulation of tissue glucose utilization in vivo. Endocrinology 1999, 140, 2117–2124. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.C.; Lord, R.A.; Anderson, G.M. Multiple leptin signalling pathways in the control of metabolism and fertility: A means to different ends? Int. J. Mol. Sci. 2021, 22, 9210. [Google Scholar] [CrossRef]
- Harris, R.B. Direct and indirect effects of leptin on adipocyte metabolism. Biochim. Biophys. Acta 2014, 1842, 414–423. [Google Scholar] [CrossRef] [Green Version]
- Ma, X.H.; Muzumdar, R.; Yang, X.M.; Gabriely, I.; Berger, R.; Barzilai, N. Aging is associated with resistance to effects of leptin on fat distribution and insulin action. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, B225–B231. [Google Scholar] [CrossRef] [Green Version]
- Garg, R.; Kumariya, S.; Katekar, R.; Verma, S.; Goand, U.K.; Gayen, J.R. JNK signaling pathway in metabolic disorders: An emerging therapeutic target. Eur. J. Pharmacol. 2021, 901, 174079. [Google Scholar] [CrossRef]
- Agrawal, S.; Gollapudi, S.; Su, H.; Gupta, S. Leptin activates human B cells to secrete TNF-α, IL-6, and IL-10 via JAK2/STAT3 and p38MAPK/ERK1/2 signaling pathway. J. Clin. Immunol. 2011, 31, 472–478. [Google Scholar] [CrossRef] [Green Version]
- Hendawy, A.S.; El-Lakkany, N.M.; Mantawy, E.M.; Hammam, O.A.; Botros, S.S.; El-Demerdash, E. Vildagliptin alleviates liver fibrosis in NASH diabetic rats via modulation of insulin resistance, oxidative stress, and inflammatory cascades. Life Sci. 2022, 304, 120695. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef] [PubMed]
- Barrios, V.; Campillo-Calatayud, A.; Guerra-Cantera, S.; Canelles, S.; Martín-Rivada, Á.; Frago, L.M.; Chowen, J.A.; Argente, J. Opposite effects of chronic central leptin infusion on activation of insulin signaling pathways in adipose tissue and liver are related to changes in the inflammatory environment. Biomolecules 2021, 11, 1734. [Google Scholar] [CrossRef] [PubMed]
- Drake, R.L.; McHugh, K.M.; Mucenski, C.G. Insulin and fructose regulate malic enzyme activity by different processes. Biochem. Biophys. Res. Commun. 1984, 121, 730–734. [Google Scholar] [CrossRef]
- Hafidi, M.E.; Buelna-Chontal, M.; Sánchez-Muñoz, F.; Carbó, R. Adipogenesis: A necessary but harmful strategy. Int. J. Mol. Sci. 2019, 20, 3657. [Google Scholar] [CrossRef] [Green Version]
- Holm, C. Molecular mechanisms regulating hormone-sensitive lipase and lipolysis. Biochem. Soc. Transact. 2003, 31, 1120–1124. [Google Scholar] [CrossRef]
- Reynisdottir, S.; Angelin, B.; Langin, D.; Lithell, H.; Eriksson, M.; Holm, C.; Arner, P. Adipose tissue lipoprotein lipase and hormone-sensitive lipase. Contrasting findings in familial combined hyperlipidemia and insulin resistance syndrome. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 2287–2292. [Google Scholar] [CrossRef]
- Bargut, T.C.; Souza-Mello, V.; Mandarim-de-Lacerda, C.A.; Aguila, M.B. Fish oil diet modulates epididymal and inguinal adipocyte metabolism in mice. Food Funct. 2016, 7, 1468–1476. [Google Scholar] [CrossRef]
- Burgos-Ramos, E.; Canelles, S.; Perianes-Cachero, A.; Arilla-Ferreiro, E.; Argente, J.; Barrios, V. Adipose tissue promotes a serum cytokine profile related to lower insulin sensitivity after chronic central leptin infusion. PLoS ONE 2012, 7, e46893. [Google Scholar] [CrossRef] [Green Version]
- Dalmas, E.; Rouault, C.; Abdennour, M.; Rovere, C.; Rizkalla, S.; Bar-Hen, A.; Nahon, J.L.; Bouillot, J.L.; Guerre-Millo, M.; Clément, K.; et al. Variations in circulating inflammatory factors are related to changes in calorie and carbohydrate intakes early in the course of surgery-induced weight reduction. Am. J. Clin. Nutr. 2011, 94, 450–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burgos-Ramos, E.; Sackmann-Sala, L.; Baquedano, E.; Cruz-Topete, D.; Barrios, V.; Argente, J.; Kopchick, J.J. Central leptin and insulin administration modulates serum cytokine- and lipoprotein-related markers. Metabolism 2012, 61, 1646–1657. [Google Scholar] [CrossRef] [PubMed]
- Vlavcheski, F.; Den Hartogh, D.J.; Giacca, A.; Tsiani, E. Amelioration of high-insulin-induced skeletal muscle cell insulin re-sistance by resveratrol is linked to activation of AMPK and restoration of GLUT4 translocation. Nutrients 2020, 12, 914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronti, T.; Lupattelli, G.; Mannarino, E. The endocrine function of adipose tissue: An update. Clin. Endocrinol. 2006, 64, 355–365. [Google Scholar] [CrossRef]
- Ding, C.; Chan, Z.; Magkos, F. Lean, but not healthy: The ‘metabolically obese, normal-weight’ phenotype. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 408–417. [Google Scholar] [CrossRef]
- Mazuecos, L.; Pintado, C.; Rubio, B.; Guisantes-Batán, E.; Andrés, A.; Gallardo, N. Leptin, acting at central level, increases FGF21 expression in white adipose tissue via PPARβ/δ. Int. J. Mol. Sci. 2021, 22, 4624. [Google Scholar] [CrossRef]
- O’Keefe, L.; Vu, T.; Simcocks, A.C.; Jenkin, K.A.; Mathai, M.L.; Hryciw, D.H.; Hutchinson, D.S.; McAinch, A.J. CB1 ligand AM251 induces weight loss and fat reduction in addition to increased systemic inflammation in diet-induced obesity. Int. J. Mol. Sci. 2022, 23, 11447. [Google Scholar] [CrossRef]
- Saggerson, E.D.; Greenbaum, A.L. The regulation of triglyceride synthesis and fatty acid synthesis in rat epididymal adipose tissue. Biochem. J. 1970, 119, 193–219. [Google Scholar] [CrossRef] [Green Version]
- Su, C.H.; Wang, C.Y.; Lan, K.H.; Li, C.P.; Chao, Y.; Lin, H.C.; Lee, S.D.; Lee, W.P. Akt phosphorylation at Thr308 and Ser473 is required for CHIP-mediated ubiquitination of the kinase. Cell. Signal. 2011, 23, 1824–1830. [Google Scholar] [CrossRef]
- Rather, G.M.; Pramono, A.A.; Szekely, Z.; Bertino, J.R.; Tedeschi, P.M. In cancer, all roads lead to NADPH. Pharmacol. Ther. 2021, 226, 107864. [Google Scholar] [CrossRef]
- Balsa, E.; Perry, E.A.; Bennett, C.F.; Jedrychowski, M.; Gygi, S.P.; Doench, J.G.; Puigserver, P. Defective NADPH production in mitochondrial disease complex I causes inflammation and cell death. Nat. Commun. 2020, 11, 2714. [Google Scholar] [CrossRef] [PubMed]
- Lapeire, L.; Hendrix, A.; Lecoutere, E.; Van Bockstal, M.; Vandesompele, J.; Maynard, D.; Braems, G.; Van Den Broecke, R.; Müller, C.; Bracke, M.; et al. Secretome analysis of breast cancer-associated adipose tissue to identify paracrine regulators of breast cancer growth. Oncotarget 2017, 8, 47239–47249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, D.; Yang, C.; Ma, J.; Chen, L.; Luo, J.; Ma, Y.; Loor, J.J. cAMP response element binding protein 1 (CREB1) promotes monounsaturated fatty acid synthesis and triacylglycerol accumulation in goat mammary epithelial cells. Animals 2020, 10, 1871. [Google Scholar] [CrossRef]
- Erion, D.M.; Ignatova, I.D.; Yonemitsu, S.; Nagai, Y.; Chatterjee, P.; Weismann, D.; Hsiao, J.J.; Zhang, D.; Iwasaki, T.; Stark, R.; et al. Prevention of hepatic steatosis and hepatic insulin resistance by knockdown of cAMP response element-binding protein. Cell Metab. 2009, 10, 499–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Dwairi, A.; Brown, A.R.; Pabona, J.M.; Van, T.H.; Hamdan, H.; Mercado, C.P.; Quick, C.M.; Wight, P.A.; Simmen, R.C.; Simmen, F.A. Enhanced gastrointestinal expression of cytosolic malic enzyme (ME1) induces intestinal and liver lipogenic gene expression and intestinal cell proliferation in mice. PLoS ONE 2014, 9, e113058. [Google Scholar] [CrossRef] [Green Version]
- Mahameed, M.; Sulieman, A.; Alkam, D.; Tirosh, B. Towards enhancing therapeutic glycoprotein bioproduction: Interventions in the PI3K/AKT/mTOR Pathway. Cell Struct. Funct. 2019, 44, 75–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamming, D.W.; Sabatini, D.M. A central role for mTOR in lipid homeostasis. Cell Metab. 2013, 18, 465–469. [Google Scholar] [CrossRef] [Green Version]
- Palhinha, L.; Liechocki, S.; Hottz, E.D.; Pereira, J.A.D.S.; de Almeida, C.J.; Moraes-Vieira, P.M.M.; Bozza, P.T.; Maya-Monteiro, C.M. Leptin induces proadipogenic and proinflammatory signaling in adipocytes. Front. Endocrinol. 2019, 10, 841. [Google Scholar] [CrossRef] [Green Version]
- Herrera-Vargas, A.K.; García-Rodríguez, E.; Olea-Flores, M.; Mendoza-Catalán, M.A.; Flores-Alfaro, E.; Navarro-Tito, N. Pro-angiogenic activity and vasculogenic mimicry in the tumor microenvironment by leptin in cancer. Cytokine Growth Factor Rev. 2021, 62, 23–41. [Google Scholar] [CrossRef]
- Gove, M.E.; Rhodes, D.H.; Pini, M.; van Baal, J.W.; Sennello, J.A.; Fayad, R.; Cabay, R.J.; Myers, M.G., Jr.; Fantuzzi, G. Role of leptin receptor-induced STAT3 signaling in modulation of intestinal and hepatic inflammation in mice. J. Leukoc. Biol. 2009, 85, 491–496. [Google Scholar] [CrossRef] [Green Version]
- Souza-Almeida, G.; Palhinha, L.; Liechocki, S.; da Silva Pereira, J.A.; Reis, P.A.; Dib, P.R.B.; Hottz, E.D.; Gameiro, J.; Vallochi, A.L.; de Almeida, C.J.; et al. Peripheral leptin signaling persists in innate immune cells during diet-induced obesity. J. Leukoc. Biol. 2021, 109, 1131–1138. [Google Scholar] [CrossRef] [PubMed]
- Porsche, C.E.; Delproposto, J.B.; Geletka, L.; O’Rourke, R.; Lumeng, C.N. Obesity results in adipose tissue T cell exhaustion. JCI Insight 2021, 6, e139793. [Google Scholar] [CrossRef]
- Borst, S.E.; Conover, C.F.; Bagby, G.J. Association of resistin with visceral fat and muscle insulin resistance. Cytokine 2005, 32, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Martinez, M.; Cabail, M.Z. The PI3K/Akt pathway in meta-inflammation. Int. J. Mol. Sci. 2022, 23, 15330. [Google Scholar] [CrossRef]
- Li, H.; Wang, C.; Zhao, J.; Guo, C. JNK downregulation improves olanzapine-induced insulin resistance by suppressing IRS1(Ser307) phosphorylation and reducing inflammation. Biomed. Pharmacother. 2021, 142, 112071. [Google Scholar] [CrossRef] [PubMed]
- Shaw, M.; Cohen, P.; Alessi, D.R. Further evidence that the inhibition of glycogen synthase kinase-3beta by IGF-1 is mediated by PDK1/PKB-induced phosphorylation of Ser-9 and not by dephosphorylation of Tyr-216. FEBS Lett. 1997, 416, 307–311. [Google Scholar] [CrossRef] [Green Version]
- Lappas, M. GSK3β is increased in adipose tissue and skeletal muscle from women with gestational diabetes where it regulates the inflammatory response. PLoS ONE 2014, 9, e115854. [Google Scholar] [CrossRef] [Green Version]
- Jorge-Torres, O.C.; Szczesna, K.; Roa, L.; Casal, C.; Gonzalez-Somermeyer, L.; Soler, M.; Velasco, C.D.; Martínez-San Segundo, P.; Petazzi, P.; Sáez, M.A.; et al. Inhibition of Gsk3b reduces Nfkb1 signaling and rescues synaptic activity to improve the Rett syndrome phenotype in Mecp2-knockout mice. Cell Rep. 2018, 23, 1665–1677. [Google Scholar] [CrossRef] [Green Version]
- Moseti, D.; Regassa, A.; Kim, W.K. Molecular regulation of adipogenesis and potential anti-adipogenic bioactive molecules. Int. J. Mol. Sci. 2016, 17, 124. [Google Scholar] [CrossRef] [Green Version]
- Bassols, J.; Ortega, F.J.; Moreno-Navarrete, J.M.; Peral, B.; Ricart, W.; Fernández-Real, J.M. Study of the proinflammatory role of human differentiated omental adipocytes. J. Cell. Biochem. 2009, 107, 1107–1117. [Google Scholar] [CrossRef]
- Tian, J.; Smith, A.; Nechtman, J.; Podolsky, R.; Aggarwal, S.; Snead, C.; Kumar, S.; Elgaish, M.; Oishi, P.; Göerlach, A.; et al. Effect of PPARgamma inhibition on pulmonary endothelial cell gene expression: Gene profiling in pulmonary hypertension. Physiol. Genomics 2009, 40, 48–60. [Google Scholar] [CrossRef]
- Sharma, S.; Sun, X.; Rafikov, R.; Kumar, S.; Hou, Y.; Oishi, P.E.; Datar, S.A.; Raff, G.; Fineman, J.R.; Black, S.M. PPAR-γ regulates carnitine homeostasis and mitochondrial function in a lamb model of increased pulmonary blood flow. PLoS ONE 2012, 7, e41555. [Google Scholar] [CrossRef] [PubMed]
- Picard, F.; Richard, D.; Huang, Q.; Deshaies, Y. Effects of leptin adipose tissue lipoprotein lipase in the obese ob/ob mouse. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 1088–1095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanchard, P.G.; Turcotte, V.; Côté, M.; Gélinas, Y.; Nilsson, S.; Olivecrona, G.; Deshaies, Y.; Festuccia, W.T. Peroxisome proliferator-activated receptor γ activation favours selective subcutaneous lipid deposition by coordinately regulating lipoprotein lipase modulators, fatty acid transporters and lipogenic enzymes. Acta Physiol. 2016, 217, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Chew, G.T.; Watts, G.F. Recent advances in pharmacotherapy for hypertriglyceridemia. Prog. Lipid Res. 2014, 56, 47–66. [Google Scholar] [CrossRef]
- Makoveichuk, E.; Vorrsjö, E.; Olivecrona, T.; Olivecrona, G. TNF-α decreases lipoprotein lipase activity in 3T3-L1 adipocytes by up-regulation of angiopoietin-like protein 4. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids 2017, 1862, 533–540. [Google Scholar] [CrossRef]
- Li, B.; Fang, J.; He, T.; Yin, S.; Yang, M.; Cui, H.; Ma, X.; Deng, J.; Ren, Z.; Hu, Y.; et al. Resistin up-regulates LPL expression through the PPARγ-dependent PI3K/AKT signaling pathway impacting lipid accumulation in RAW264.7 macrophages. Cytokine 2019, 119, 168–174. [Google Scholar] [CrossRef]
- Arner, P. Human fat cell lipolysis: Biochemistry, regulation and clinical role. Best Pract. Res. Clin. Endocrinol. Metab. 2005, 19, 471–482. [Google Scholar] [CrossRef]
- Lan, Y.L.; Lou, J.C.; Lyu, W.; Zhang, B. Update on the synergistic effect of HSL and insulin in the treatment of metabolic disorders. Ther. Adv. Endocrinol. Metab. 2019, 10, 2042018819877300. [Google Scholar] [CrossRef]
- Botion, L.M.; Green, A. Long-term regulation of lipolysis and hormone-sensitive lipase by insulin and glucose. Diabetes 1999, 48, 1691–1697. [Google Scholar] [CrossRef]
- Burgos-Ramos, E.; Canelles, S.; Frago, L.M.; Chowen, J.A.; Arilla-Ferreiro, E.; Argente, J.; Barrios, V. Improvement in glycemia after glucose or insulin overload in leptin-infused rats is associated with insulin-related activation of hepatic glucose metabolism. Nutr. Metab. 2016, 13, 19. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Wang, Q.; Zhu, S.; Huang, J.; Liu, Z.; Qi, R. Naringin reduces fat deposition by promoting the expression of lipolysis and β-oxidation related genes. Obes. Res. Clin. Pract. 2022, 17, 74–81. [Google Scholar] [CrossRef]
- Shiau, M.Y.; Chuang, P.H.; Yang, C.P.; Hsiao, C.W.; Chang, S.W.; Chang, K.Y.; Liu, T.M.; Chen, H.W.; Chuang, C.C.; Yuan, S.Y.; et al. Mechanism of interleukin-4 reducing lipid deposit by regulating hormone-sensitive lipase. Sci. Rep. 2019, 9, 11974. [Google Scholar] [CrossRef] [Green Version]
- Ikoma-Seki, K.; Nakamura, K.; Morishita, S.; Ono, T.; Sugiyama, K.; Nishino, H.; Hirano, H.; Murakoshi, M. Role of LRP1 and ERK and cAMP signaling pathways in lactoferrin-induced lipolysis in mature rat adipocytes. PLoS ONE 2015, 10, e0141378. [Google Scholar] [CrossRef] [Green Version]
- Barrios, V.; Frago, L.M.; Canelles, S.; Guerra-Cantera, S.; Arilla-Ferreiro, E.; Chowen, J.A.; Argente, J. Leptin modulates the response of brown adipose tissue to negative energy balance: Implication of the GH/IGF-I Axis. Int. J. Mol. Sci. 2021, 22, 2827. [Google Scholar] [CrossRef]
- Barrios, V.; López-Villar, E.; Frago, L.M.; Canelles, S.; Díaz-González, F.; Burgos-Ramos, E.; Frühbeck, G.; Chowen, J.A.; Argente, J. Cerebral insulin bolus revokes the changes in hepatic lipid metabolism induced by chronic central leptin infusion. Cells 2021, 10, 581. [Google Scholar] [CrossRef]
- Wagoner, B.; Hausman, D.B.; Harris, R.B. Direct and indirect effects of leptin on preadipocyte proliferation and differentiation. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2006, 290, R1557–R1564. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.S.; Smith, M.S.; Reda, D.; Suffredini, A.F.; McCoy, J.P., Jr. Multiplex bead array assays for detection of soluble cytokines: Comparisons of sensitivity and quantitative values among kits from multiple manufacturers. Cytom. B Clin. Cytom. 2004, 61, 35–39. [Google Scholar] [CrossRef]
- Perianes-Cachero, A.; Burgos-Ramos, E.; Puebla-Jiménez, L.; Canelles, S.; Viveros, M.P.; Mela, V.; Chowen, J.A.; Argente, J.; Arilla-Ferreiro, E.; Barrios, V. Leptin-induced downregulation of the rat hippocampal somatostatinergic system may potentiate its anorexigenic effects. Neurochem. Int. 2012, 61, 1385–1396. [Google Scholar] [CrossRef]
- Geer, B.W.; Krochko, D.; Williamson, J.H. Ontogeny, cell distribution, and the physiological role of NADP-malic enzyme in Drosophila melanogaster. Biochem. Genet. 1979, 17, 867–879. [Google Scholar] [CrossRef]


| p-p38MAPK | p-JNK | MCP-1 | mRNA Ppar-γ | p-IR | pTyr-IRS1 | p-Akt | |
|---|---|---|---|---|---|---|---|
| r p | r p | r p | r p | r p | r p | r p | |
| mRNA Acc-α | −0.26 NS | +0.29 NS | +0.31 NS | −0.36 NS | +0.37 NS | +0.33 NS | +0.36 NS |
| mRNA Fas | +0.14 NS | +0.22 NS | +0.37 NS | −0.30 NS | +0.21 NS | −0.08 NS | +0.10 NS |
| mRNA Hsl | −0.51 * | −0.65 * | −0.58 * | +0.84 *** | +0.42 NS | +0.38 NS | +0.39 NS |
| mRNA Lpl | −0.47 * | −0.71 ** | −0.63 ** | +0.99 *** | +0.48 * | +0.48 * | +0.45 * |
| mRNA Cpt1a | −0.35 NS | −0.60 ** | −0.72 ** | +0.87 *** | +0.61 ** | +0.53 * | +0.47 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casado, M.E.; Canelles, S.; Arilla-Ferreiro, E.; Frago, L.M.; Barrios, V. Changes in Lipid Metabolism Enzymes in Rat Epididymal Fat after Chronic Central Leptin Infusion Are Related to Alterations in Inflammation and Insulin Signaling. Int. J. Mol. Sci. 2023, 24, 7065. https://doi.org/10.3390/ijms24087065
Casado ME, Canelles S, Arilla-Ferreiro E, Frago LM, Barrios V. Changes in Lipid Metabolism Enzymes in Rat Epididymal Fat after Chronic Central Leptin Infusion Are Related to Alterations in Inflammation and Insulin Signaling. International Journal of Molecular Sciences. 2023; 24(8):7065. https://doi.org/10.3390/ijms24087065
Chicago/Turabian StyleCasado, María E., Sandra Canelles, Eduardo Arilla-Ferreiro, Laura M. Frago, and Vicente Barrios. 2023. "Changes in Lipid Metabolism Enzymes in Rat Epididymal Fat after Chronic Central Leptin Infusion Are Related to Alterations in Inflammation and Insulin Signaling" International Journal of Molecular Sciences 24, no. 8: 7065. https://doi.org/10.3390/ijms24087065






