Hemostatic Collagen Sponge with High Porosity Promotes the Proliferation and Adhesion of Fibroblasts and Osteoblasts
Abstract
:1. Introduction
2. Results
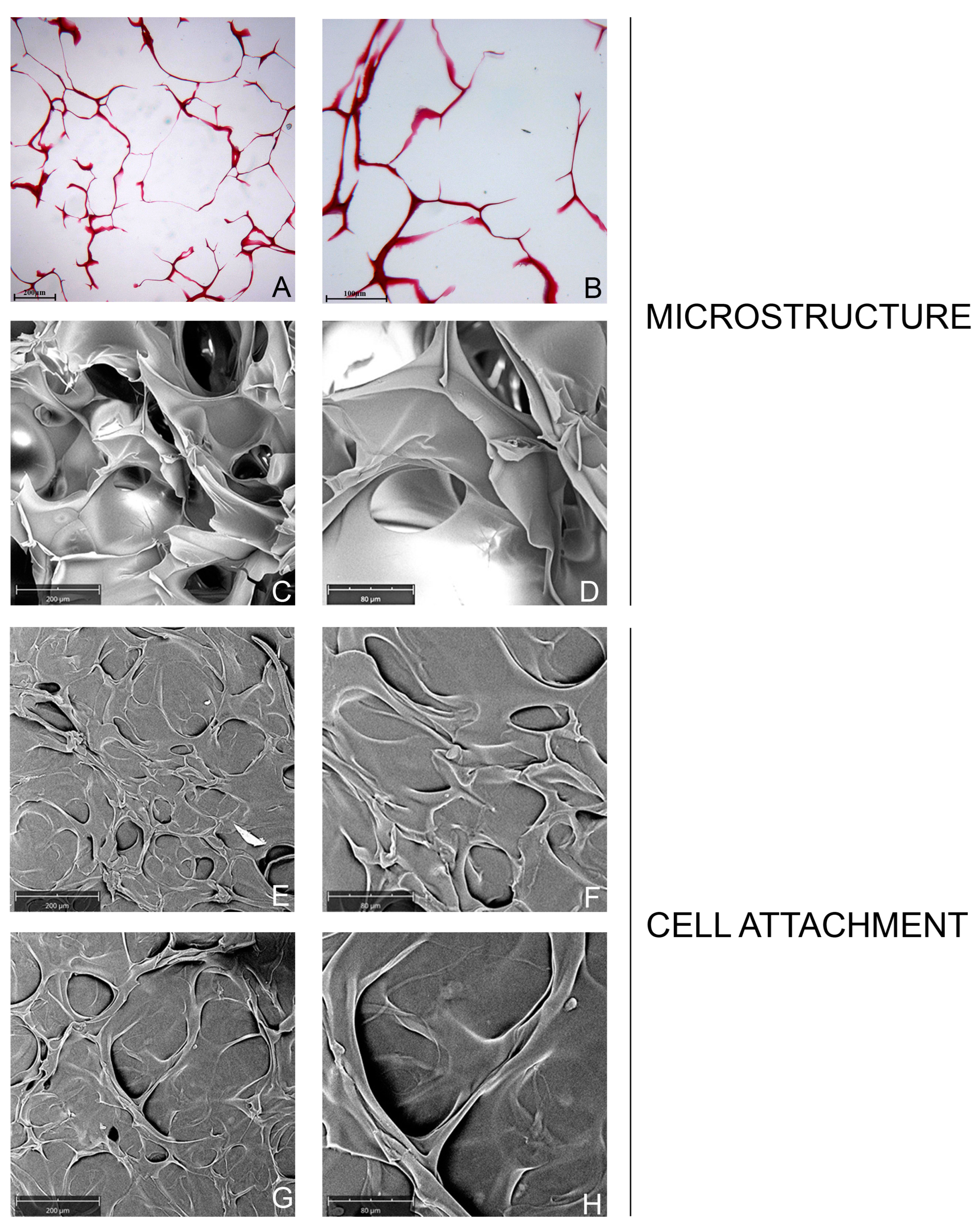
2.1. Characterization of Collagen Sponge
2.1.1. Microstructure and Porosity
2.1.2. Cell Attachment and Cell Morphology
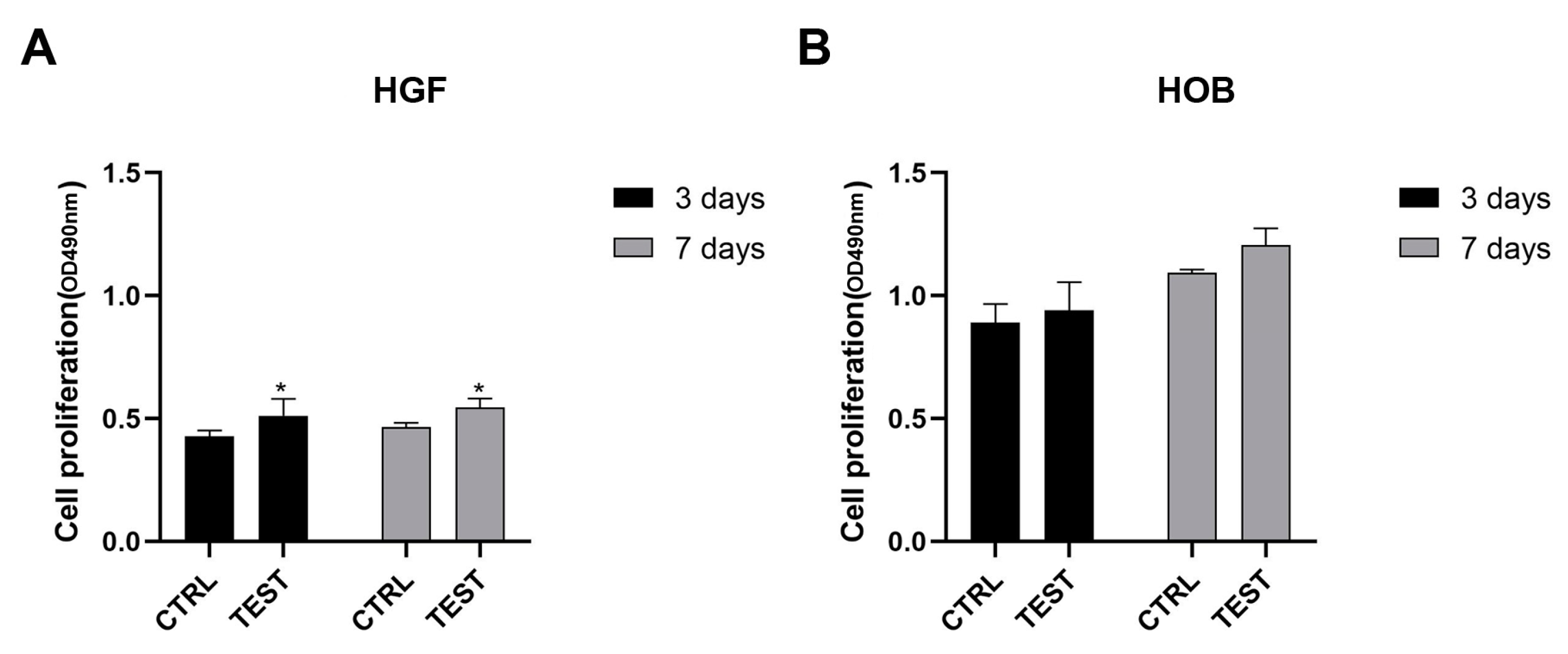
2.2. Biological Activity
2.2.1. Cell Viability
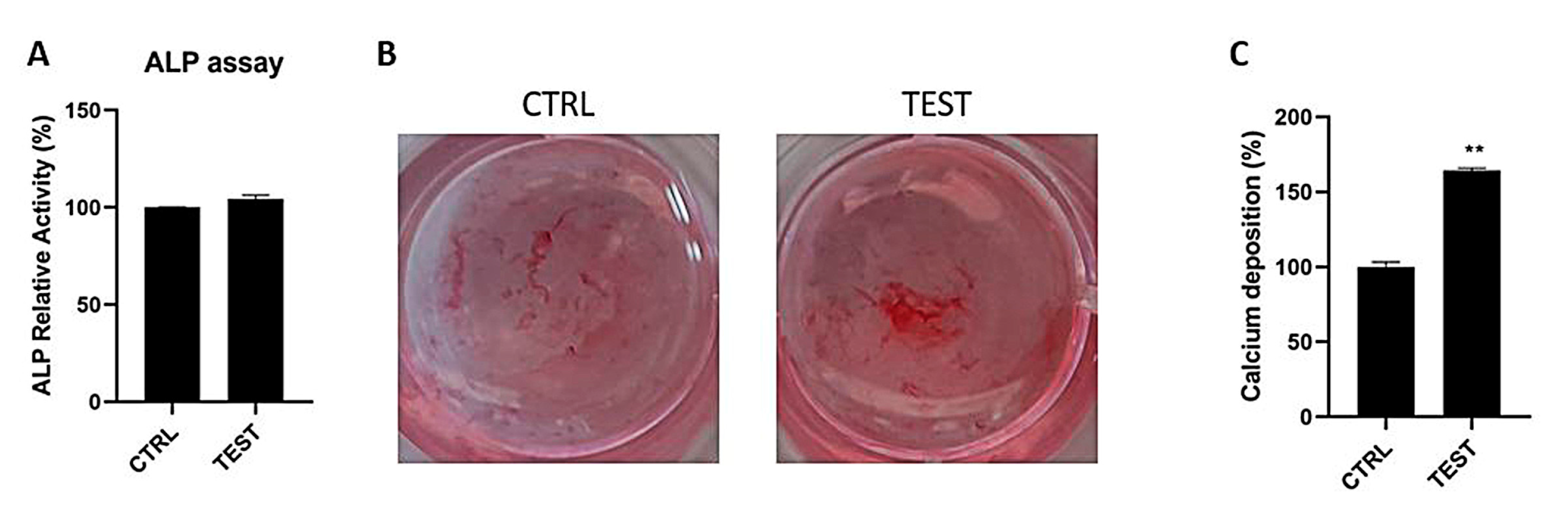
2.2.2. Mineralization Activity of Osteoblasts
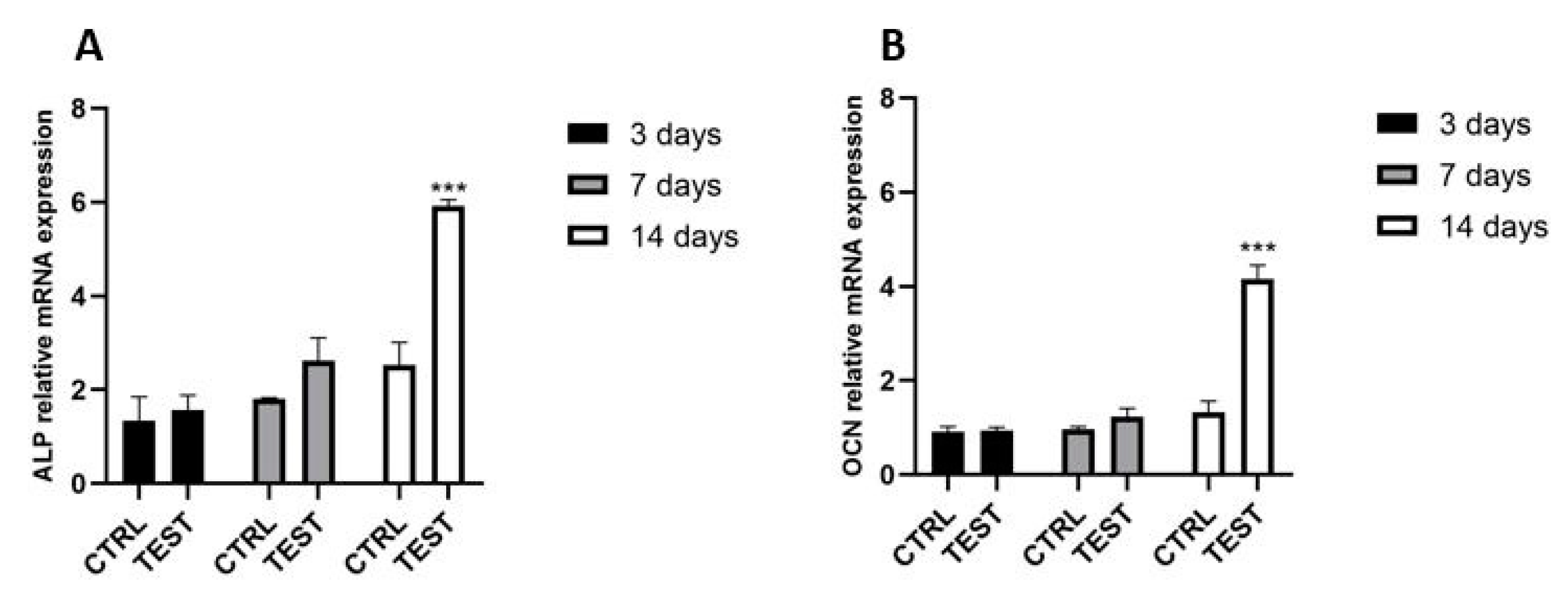
2.2.3. Gene Expression of ALP and OCN in Osteoblasts
3. Discussion
4. Materials and Methods
4.1. Study Design
- i.
- Histological characterization of the sponge alone
- ii.
- SEM characterization of the sponge alone and porosity evaluation
- iii.
- The adhesion of HGFs and HOBs by SEM at 3 and 7 days
- iv.
- Viability of HGFs and HOB by MTT at 3 and 7 days
- v.
- Phosphatase alkaline (ALP) levels of HOBs at 7 days
- vi.
- Mineralization of HOBs at 14 days
- vii.
- Gene expression of constitutive markers of HOBs at 3, 7 and 14 days
4.2. Characterization of the Material
4.2.1. SEM Analyses
4.2.2. Determination of Porosity
4.2.3. Histological Analyses
4.3. Biological In Vitro Tests
4.3.1. Cell Cultures
4.3.2. Cell Viability
4.3.3. Cell Adhesion
4.3.4. ALP Assay
4.3.5. Alizarin Red Staining and the Quantification of Calcium Deposition
4.3.6. Gene Expression
4.3.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Scalise, A.; Calamita, R.; Tartaglione, C.; Pierangeli, M.; Bolletta, E.; Gioacchini, M.; Gesuita, R.; di Benedetto, G. Improving Wound Healing and Preventing Surgical Site Complications of Closed Surgical Incisions: A Possible Role of Incisional Negative Pressure Wound Therapy. A Systematic Review of the Literature. Int. Wound J. 2016, 13, 1260–1281. [Google Scholar] [CrossRef] [PubMed]
- Dalgleish, L.; Campbell, J.; Finlayson, K.; Barakat-Johnson, M.; Beath, A.; Ingleman, J.; Parker, C.; Coyer, F. Understanding Skin Failure: A Scoping Review. Adv. Ski. Wound Care 2021, 34, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Pastar, I.; Stojadinovic, O.; Yin, N.C.; Ramirez, H.; Nusbaum, A.G.; Sawaya, A.; Patel, S.B.; Khalid, L.; Isseroff, R.R.; Tomic-Canic, M. Epithelialization in Wound Healing: A Comprehensive Review. Adv. Wound Care 2014, 3, 445–464. [Google Scholar] [CrossRef] [PubMed]
- Groenewold, M.D.; Gribnau, A.J.; Ubbink, D.T. Topical Haemostatic Agents for Skin Wounds: A Systematic Review. BMC Surg. 2011, 11, 15. [Google Scholar] [CrossRef]
- Yu, P.; Zhong, W. Hemostatic Materials in Wound Care. Burn. Trauma 2021, 9, tkab019. [Google Scholar] [CrossRef]
- Kular, J.K.; Basu, S.; Sharma, R.I. The Extracellular Matrix: Structure, Composition, Age-Related Differences, Tools for Analysis and Applications for Tissue Engineering. J. Tissue Eng. 2014, 5, 2041731414557112. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Raines, R.T. Collagen-Based Biomaterials for Wound Healing. Biopolymers 2014, 101, 821–833. [Google Scholar] [CrossRef]
- Muthukumar, T.; Sreekumar, G.; Sastry, T.P.; Chamundeeswari, M. Collagen as a Potential Biomaterial in Biomedical Applications. Rev. Adv. Mater. Sci. 2018, 53, 29–39. [Google Scholar] [CrossRef]
- Ferrario, C.; Rusconi, F.; Pulaj, A.; Macchi, R.; Landini, P.; Paroni, M.; Colombo, G.; Martinello, T.; Melotti, L.; Gomiero, C.; et al. From Food Waste to Innovative Biomaterial: Sea Urchin-Derived Collagen for Applications in Skin Regenerative Medicine. Mar. Drugs 2020, 18, 414. [Google Scholar] [CrossRef]
- Sasaki, J.-I.; Abe, G.L.; Li, A.; Thongthai, P.; Tsuboi, R.; Kohno, T.; Imazato, S. Barrier Membranes for Tissue Regeneration in Dentistry. Biomater. Investig. Dent. 2021, 8, 54–63. [Google Scholar] [CrossRef]
- Mamoun, J. Dry Socket Etiology, Diagnosis, and Clinical Treatment Techniques. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Graziani, F.; D’Aiuto, F.; Gennai, S.; Petrini, M.; Nisi, M.; Cirigliano, N.; Landini, L.; Bruno, R.M.; Taddei, S.; Ghiadoni, L. Systemic Inflammation after Third Molar Removal: A Case-Control Study. J. Dent. Res. 2017, 96, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Park, J.B. Effects of Fibroblast Growth Factor 2 on Osteoblastic Proliferation and Differentiation by Regulating Bone Morphogenetic Protein Receptor Expression. J. Craniofac. Surg. 2011, 22, 1880–1882. [Google Scholar] [CrossRef] [PubMed]
- Polo-Corrales, L.; Latorre-Esteves, M.; Ramirez-Vick, J.E. Scaffold Design for Bone Regeneration. J. Nanosci. Nanotechnol. 2014, 14, 15–56. [Google Scholar] [CrossRef] [PubMed]
- Loh, Q.L.; Choong, C. Three-Dimensional Scaffolds for Tissue Engineering Applications: Role of Porosity and Pore Size. Tissue Eng. Part B Rev. 2013, 19, 485–502. [Google Scholar] [CrossRef]
- Ventre, M.; Causa, F.; Netti, P.A. Determinants of Cell-Material Crosstalk at the Interface: Towards Engineering of Cell Instructive Materials. J. R Soc. Interface 2012, 9, 2017–2032. [Google Scholar] [CrossRef]
- Freed, L.E.; Langer, R.; Martin, I.; Pellis, N.R.; Vunjak-Novakovic, G. Tissue Engineering of Cartilage in Space. Proc. Natl. Acad. Sci. USA 1997, 94, 13885–13890. [Google Scholar] [CrossRef]
- Janik, H.; Marzec, M. A Review: Fabrication of Porous Polyurethane Scaffolds. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 48, 586–591. [Google Scholar] [CrossRef]
- Song, X.; Zhu, C.; Fan, D.; Mi, Y.; Li, X.; Fu, R.Z.; Duan, Z.; Wang, Y.; Feng, R.R. A Novel Human-Like Collagen Hydrogel Scaffold with Porous Structure and Sponge-Like Properties. Polymers 2017, 9, 638. [Google Scholar] [CrossRef]
- Dutta, R.C.; Dey, M.; Dutta, A.K.; Basu, B. Competent Processing Techniques for Scaffolds in Tissue Engineering. Biotechnol. Adv. 2017, 35, 240–250. [Google Scholar] [CrossRef]
- Yannas, I.V.; Burke, J.F.; Orgill, D.P.; Skrabut, E.M. Wound Tissue Can Utilize a Polymeric Template to Synthesize a Functional Extension of Skin. Science 1982, 215, 174–176. [Google Scholar] [CrossRef] [PubMed]
- Wada, Y.; Kataoka, H.; Yokose, S.; Ishizuya, T.; Miyazono, K.; Gao, Y.H.; Shibasaki, Y.; Yamaguchi, A. Changes in Osteoblast Phenotype during Differentiation of Enzymatically Isolated Rat Calvaria Cells. Bone 1998, 22, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Davies, O.G.; Cox, S.C.; Azoidis, I.; McGuinness, A.J.; Cooke, M.; Heaney, L.M.; Grover, L.M. Osteoblast-Derived Vesicle Protein Content Is Temporally Regulated during Osteogenesis: Implications for Regenerative Therapies. Front. Bioeng. Biotechnol. 2019, 7, 92. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Lu, Y.; Wang, Y.; Ge, L.; Zhai, N.; Han, J. A Protocol for Isolation and Identification and Comparative Characterization of Primary Osteoblasts from Mouse and Rat Calvaria. Cell Tissue Bank 2019, 20, 173–182. [Google Scholar] [CrossRef]
- Reich, A.; Bae, A.S.; Barnes, A.M.; Cabral, W.A.; Hinek, A.; Stimec, J.; Hill, S.C.; Chitayat, D.; Marini, J.C. Type V OI Primary Osteoblasts Display Increased Mineralization despite Decreased COL1A1 Expression. J. Clin. Endocrinol. Metab. 2015, 100, E325–E332. [Google Scholar] [CrossRef]
- Torun Köse, G.; Kenar, H.; Hasirci, N.; Hasirci, V. Macroporous Poly(3-Hydroxybutyrate-Co-3-Hydroxyvalerate) Matrices for Bone Tissue Engineering. Biomaterials 2003, 24, 1949–1958. [Google Scholar] [CrossRef]
- Petrini, M.; Pierfelice, T.V.; D’amico, E.; di Pietro, N.; Pandolfi, A.; D’arcangelo, C.; de Angelis, F.; Mandatori, D.; Schiavone, V.; Piattelli, A.; et al. Influence of Nano, Micro, and Macro Topography of Dental Implant Surfaces on Human Gingival Fibroblasts. Int. J. Mol. Sci. 2021, 22, 9871. [Google Scholar] [CrossRef]
- Chang, S.J.; Huang, Y.T.; Yang, S.C.; Kuo, S.M.; Lee, M.W. In Vitro Properties of Gellan Gum Sponge as the Dental Filling to Maintain Alveolar Space. Carbohydr. Polym. 2012, 88, 684–689. [Google Scholar] [CrossRef]
- Pierfelice, T.V.; D’amico, E.; Iezzi, G.; Piattelli, A.; di Pietro, N.; D’arcangelo, C.; Comuzzi, L.; Petrini, M. Nanoporous Titanium Enriched with Calcium and Phosphorus Promotes Human Oral Osteoblast Bioactivity. Int. J. Environ. Res. Public Health 2022, 19, 6212. [Google Scholar] [CrossRef]

| Characteristics | Pore Size (Mean ± SD, µm) (Min–Max) |
|---|---|
| Longitudinal (N = 40) | |
| Collagen sponge | 244.69 ± 80.01 (106.69–336.36) |
| Gene | Forward Primer (5′-3′) | Reverse Primer (5′-3′) |
|---|---|---|
| OCN ALP | TCAGCCAACTCGTCACAGTC AATGAGTGAGTGACCATCCTGG | GGCGCTACCTGTATCAATGG GCACCCCAAGACCTGCTTTAT |
| βACT | CCAGAGGCGTACAGGGATAG | GAGAAGATGACCCAGGACTCTC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Amico, E.; Pierfelice, T.V.; Lepore, S.; Iezzi, G.; D’Arcangelo, C.; Piattelli, A.; Covani, U.; Petrini, M. Hemostatic Collagen Sponge with High Porosity Promotes the Proliferation and Adhesion of Fibroblasts and Osteoblasts. Int. J. Mol. Sci. 2023, 24, 7749. https://doi.org/10.3390/ijms24097749
D’Amico E, Pierfelice TV, Lepore S, Iezzi G, D’Arcangelo C, Piattelli A, Covani U, Petrini M. Hemostatic Collagen Sponge with High Porosity Promotes the Proliferation and Adhesion of Fibroblasts and Osteoblasts. International Journal of Molecular Sciences. 2023; 24(9):7749. https://doi.org/10.3390/ijms24097749
Chicago/Turabian StyleD’Amico, Emira, Tania Vanessa Pierfelice, Stefania Lepore, Giovanna Iezzi, Camillo D’Arcangelo, Adriano Piattelli, Ugo Covani, and Morena Petrini. 2023. "Hemostatic Collagen Sponge with High Porosity Promotes the Proliferation and Adhesion of Fibroblasts and Osteoblasts" International Journal of Molecular Sciences 24, no. 9: 7749. https://doi.org/10.3390/ijms24097749






