Deoxynivalenol Mycotoxin Inhibits Rabies Virus Replication In Vitro
Abstract
1. Introduction
2. Results
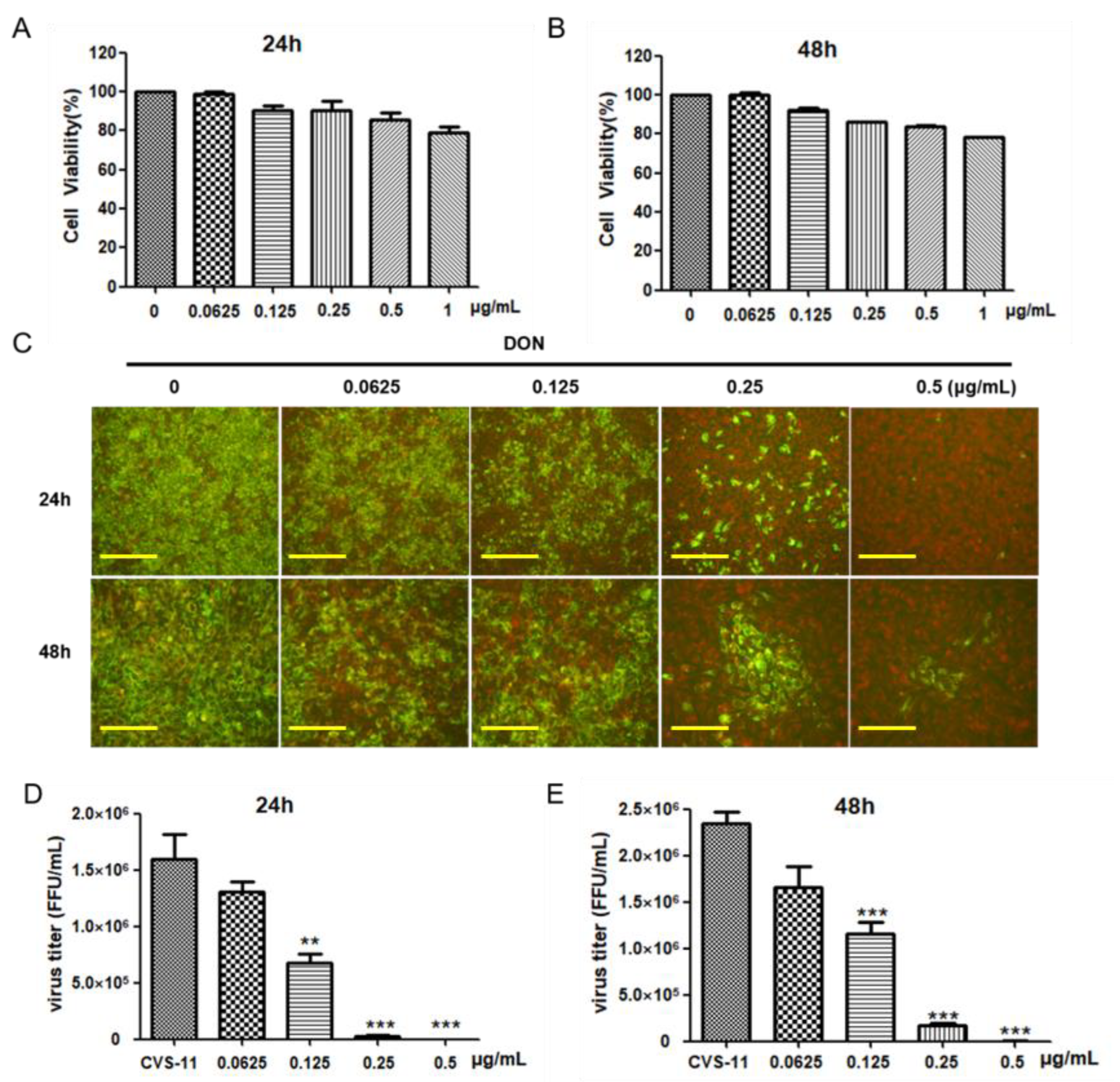
2.1. DON Exhibits Anti-Rabies Virus Activity in BHK-21 Cells
2.2. DON Target Replication Phase of Viral Infection Cycle
2.3. DON Can Inhibit the Binding, Entry, and Release of Rabies Viruses but Cannot Directly Inactivate Viruses
2.4. DON Inhibits the Replication of SC-16 and CTN-1 Strains
2.5. DON May Affect the Replication of Rabies Virus through Apoptosis
3. Discussion
4. Materials and Methods
4.1. Cell Culture, Virus, and Compounds
4.2. Quantitative Reverse Transcription PCR (qRT-PCR)
4.3. Direct Fluorescent Antibody Test
4.4. Fluorescent Focus Unit (FFU) Assay
4.5. Antiviral Assay
4.6. Time-of-Drug-Addition Assay
4.7. Viral Binding, Entry, and Release Assay
4.8. Viral Particle Inactivation Assay
4.9. Cell Viability Assay
4.10. Determination of Cell Mortality
4.11. Data Statistics and Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, S.P.; Wu, G.; Fooks, A.R.; Ma, J.; Banyard, A.C. Trying to treat the untreatable: Experimental approaches to clear rabies virus infection from the CNS. J. Gen. Virol. 2019, 100, 1171–1186. [Google Scholar] [CrossRef] [PubMed]
- Hatz, C.F.; Kuenzli, E.; Funk, M. Rabies: Relevance, prevention, and management in travel medicine. Infect. Dis. Clin. N. Am. 2012, 26, 739–753. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.C. Rabies in the critical care unit: Diagnostic and therapeutic approaches. Can. J. Neurol. Sci. 2011, 38, 689–695. [Google Scholar] [CrossRef]
- Schnell, M.J.; McGettigan, J.P.; Wirblich, C.; Papaneri, A. The cell biology of rabies virus: Using stealth to reach the brain. Nat. Rev. Microbiol. 2010, 8, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Albertini, A.A.; Schoehn, G.; Weissenhorn, W.; Ruigrok, R.W. Structural aspects of rabies virus replication. Cell. Mol. Life Sci. 2008, 65, 282–294. [Google Scholar] [CrossRef] [PubMed]
- Atici, Y.T.; Oguzoglu, T.C. The comparison of full G and N gene sequences from turkish rabies virus field strains. Virus Res. 2022, 315, 198790. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Sereno, Z.E.; Streicker, D.G.; Medina-Rodriguez, A.T.; Benavides, J.A. Drivers of Spatial Expansions of Vampire Bat Rabies in Colombia. Viruses 2022, 14, 2318. [Google Scholar] [CrossRef] [PubMed]
- Davis, B.M.; Rall, G.F.; Schnell, M.J. Everything You Always Wanted to Know about Rabies Virus (but Were Afraid to Ask). Annu. Rev. Virol. 2015, 2, 451–471. [Google Scholar] [CrossRef]
- Lafon, M. Evasive strategies in rabies virus infection. Adv. Virus Res. 2011, 79, 33–53. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.G.; Wu, X.; Franka, R.; Rupprecht, C.E. Design of future rabies biologics and antiviral drugs. Adv. Virus Res. 2011, 79, 345–363. [Google Scholar] [CrossRef] [PubMed]
- Anindita, P.D.; Sasaki, M.; Okada, K.; Ito, N.; Sugiyama, M.; Saito-Tarashima, N.; Minakawa, N.; Shuto, S.; Otsuguro, S.; Ichikawa, S.; et al. Ribavirin-related compounds exert in vitro inhibitory effects toward rabies virus. Antivir. Res. 2018, 154, 1–9. [Google Scholar] [CrossRef]
- Appolinario, C.M.; Jackson, A.C. Antiviral therapy for human rabies. Antivir. Ther. 2015, 20, 1–10. [Google Scholar] [CrossRef]
- Yamada, K.; Noguchi, K.; Komeno, T.; Furuta, Y.; Nishizono, A. Efficacy of Favipiravir (T-705) in Rabies Postexposure Prophylaxis. J. Infect. Dis. 2016, 213, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Rogee, S.; Larrous, F.; Jochmans, D.; Ben-Khalifa, Y.; Neyts, J.; Bourhy, H. Pyrimethamine inhibits rabies virus replication in vitro. Antivir. Res. 2019, 161, 1–9. [Google Scholar] [CrossRef]
- Marosi, A.; Forgach, P.; Gyuranecz, M.; Sulyok, K.M.; Bakonyi, T. Evaluation of in vitro inhibitory potential of type-I interferons and different antiviral compounds on rabies virus replication. Vaccine 2019, 37, 4663–4672. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.G.; Jackson, F.R.; Morgan, C.N.; Carson, W.C.; Martin, B.E.; Gallardo-Romero, N.; Ellison, J.A.; Greenberg, L.; Hodge, T.; Squiquera, L.; et al. Antiviral Ranpirnase TMR-001 Inhibits Rabies Virus Release and Cell-to-Cell Infection In Vitro. Viruses 2020, 12, 177. [Google Scholar] [CrossRef]
- Kali, S.; Jallet, C.; Azebi, S.; Cokelaer, T.; Da Fonseca, J.P.; Wu, Y.; Barbier, J.; Cintrat, J.C.; Gillet, D.; Tordo, N. Broad spectrum compounds targeting early stages of rabies virus (RABV) infection. Antivir. Res. 2021, 188, 105016. [Google Scholar] [CrossRef] [PubMed]
- Pestka, J.J. Deoxynivalenol: Mechanisms of action, human exposure, and toxicological relevance. Arch. Toxicol. 2010, 84, 663–679. [Google Scholar] [CrossRef]
- Pestka, J.J.; Smolinski, A.T. Deoxynivalenol: Toxicology and potential effects on humans. J. Toxicol. Environ. Health B Crit. Rev. 2005, 8, 39–69. [Google Scholar] [CrossRef]
- Wu, Q.; Wang, X.; Nepovimova, E.; Miron, A.; Liu, Q.; Wang, Y.; Su, D.; Yang, H.; Li, L.; Kuca, K. Trichothecenes: Immunomodulatory effects, mechanisms, and anti-cancer potential. Arch. Toxicol. 2017, 91, 3737–3785. [Google Scholar] [CrossRef]
- Savard, C.; Pinilla, V.; Provost, C.; Segura, M.; Gagnon, C.A.; Chorfi, Y. In vitro effect of deoxynivalenol (DON) mycotoxin on porcine reproductive and respiratory syndrome virus replication. Food Chem. Toxicol. 2014, 65, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Arunachalam, C.; Doohan, F.M. Trichothecene toxicity in eukaryotes: Cellular and molecular mechanisms in plants and animals. Toxicol. Lett. 2013, 217, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; You, L.; Wu, W.; Wang, X.; Chrienova, Z.; Nepovimova, E.; Wu, Q.; Kuca, K. The neurotoxicity of trichothecenes T-2 toxin and deoxynivalenol (DON): Current status and future perspectives. Food Chem. Toxicol. 2020, 145, 111676. [Google Scholar] [CrossRef]
- Tang, W.F.; Tsai, H.P.; Chang, Y.H.; Chang, T.Y.; Hsieh, C.F.; Lin, C.Y.; Lin, G.H.; Chen, Y.L.; Jheng, J.R.; Liu, P.C.; et al. Perilla (Perilla frutescens) leaf extract inhibits SARS-CoV-2 via direct virus inactivation. Biomed. J. 2021, 44, 293–303. [Google Scholar] [CrossRef]
- Wu, Q.H.; Wang, X.; Yang, W.; Nussler, A.K.; Xiong, L.Y.; Kuca, K.; Dohnal, V.; Zhang, X.J.; Yuan, Z.H. Oxidative stress-mediated cytotoxicity and metabolism of T-2 toxin and deoxynivalenol in animals and humans: An update. Arch. Toxicol. 2014, 88, 1309–1326. [Google Scholar] [CrossRef] [PubMed]
- Pestka, J.J. Mechanisms of deoxynivalenol-induced gene expression and apoptosis. Food Addit. Contam. Part A Chem. Anal. Control. Expo. Risk Assess. 2008, 25, 1128–1140. [Google Scholar] [CrossRef]
- Tani, N.; Dohi, Y.; Onji, Y.; Yonemasu, K. Antiviral activity of trichothecene mycotoxins (deoxynivalenol, fusarenon-X, and nivalenol) against herpes simplex virus types 1 and 2. Microbiol. Immunol. 1995, 39, 635–637. [Google Scholar] [CrossRef]
- Liu, D.; Ge, L.; Wang, Q.; Su, J.; Chen, X.; Wang, C.; Huang, K. Low-level contamination of deoxynivalenol: A threat from environmental toxins to porcine epidemic diarrhea virus infection. Environ. Int. 2020, 143, 105949. [Google Scholar] [CrossRef]
- Yu, J.; Xiao, H.; Yang, W.; Dellicour, S.; Kraemer, M.U.G.; Liu, Y.; Cai, J.; Huang, Z.X.Y.; Zhang, Y.; Feng, Y.; et al. The impact of anthropogenic and environmental factors on human rabies cases in China. Transbound. Emerg. Dis. 2020, 67, 2544–2553. [Google Scholar] [CrossRef] [PubMed]
- Zandi, F.; Khalaj, V.; Goshadrou, F.; Meyfour, A.; Gholami, A.; Enayati, S.; Mehranfar, M.; Rahmati, S.; Kheiri, E.V.; Badie, H.G.; et al. Rabies virus matrix protein targets host actin cytoskeleton: A protein-protein interaction analysis. Pathog. Dis. 2021, 79, ftaa075. [Google Scholar] [CrossRef]
- Suja, M.S.; Mahadevan, A.; Madhusudana, S.N.; Shankar, S.K. Role of apoptosis in rabies viral encephalitis: A comparative study in mice, canine, and human brain with a review of literature. Pathol. Res. Int. 2011, 2011, 374286. [Google Scholar] [CrossRef] [PubMed]
- Cliquet, F.; Picard-Meyer, E. Rabies and rabies-related viruses: A modern perspective on an ancient disease. Rev. Sci. Tech. 2004, 23, 625–642. [Google Scholar] [CrossRef] [PubMed]
- Thomson, B.J. Viruses and apoptosis. Int. J. Exp. Pathol. 2001, 82, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fan, M.; Chu, X.; Zhang, Y.; Rahman, S.U.; Jiang, Y.; Chen, X.; Zhu, D.; Feng, S.; Li, Y.; et al. Deoxynivalenol induces toxicity and apoptosis in piglet hippocampal nerve cells via the MAPK signaling pathway. Toxicon 2018, 155, 1–8. [Google Scholar] [CrossRef]
- Behrens, M.; Huwel, S.; Galla, H.J.; Humpf, H.U. Blood-Brain Barrier Effects of the Fusarium Mycotoxins Deoxynivalenol, 3 Acetyldeoxynivalenol, and Moniliformin and Their Transfer to the Brain. PLoS ONE 2015, 10, e0143640. [Google Scholar] [CrossRef]
- Tu, Y.; Wu, W.; Guo, Y.; Lu, F.; Li, X.; Xu, D.; Zou, D.; Tu, Y.; Chai, Y.; He, L. Up-regulation of hsa-miR-221-3p induced by UVB affects proliferation and apoptosis of keratinocytes via Bcl-xL/Bax pathway. Photodermatol. Photoimmunol. Photomed. 2021, 37, 269–277. [Google Scholar] [CrossRef]
- Atabaki, R.; Khaleghzadeh-Ahangar, H.; Esmaeili, N.; Mohseni-Moghaddam, P. Role of Pyroptosis, a Pro-Inflammatory Programmed Cell Death, in Epilepsy. Cell Mol. Neurobiol. 2023, 43, 1049–1059. [Google Scholar] [CrossRef]
- Bonnet, M.S.; Roux, J.; Mounien, L.; Dallaporta, M.; Troadec, J.D. Advances in deoxynivalenol toxicity mechanisms: The brain as a target. Toxins 2012, 4, 1120–1138. [Google Scholar] [CrossRef]
- Lawson, K.F.; Hertler, R.; Charlton, K.M.; Campbell, J.B.; Rhodes, A.J. Safety and immunogenicity of ERA strain of rabies virus propagated in a BHK-21 cell line. Can. J. Vet. Res. 1989, 53, 438–444. [Google Scholar]
- Tu, Z.; Xu, M.; Zhang, J.; Feng, Y.; Hao, Z.; Tu, C.; Liu, Y. Pentagalloylglucose Inhibits the Replication of Rabies Virus via Mediation of the miR-455/SOCS3/STAT3/IL-6 Pathway. J. Virol. 2019, 93, e00539-19. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Singh, K.P.; Cherian, S.; Saminathan, M.; Kapoor, S.; Manjunatha Reddy, G.B.; Panda, S.; Dhama, K. Rabies-epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: A comprehensive review. Vet. Q. 2017, 37, 212–251. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.C.; Noguchi, A.; Inoue, S.; Tang, Q.; Rayner, S.; Liang, G.D. Comparison of RFFIT tests with different standard sera and testing procedures. Virol. Sin. 2012, 27, 187–193. [Google Scholar] [CrossRef] [PubMed]




| Gene (Abbreviation) | Sequence (5′→3′) |
|---|---|
| β-actin | F: GTGCTATGTTGCTCTAGACTTCG |
| R: ATGCCACAGGATTCCATA | |
| Rabies virus N gene | F: AATCTCACCGCAAGGGAAGC |
| R: ATGCAGCAATAACCGTCGCA | |
| Caspase 3 | F: GGAATGGCATGTCGATCTGGT |
| R: ACTGTCCGTCTCAATCCCAC | |
| BAX | F: CCCGAGAGGTCTTTTTCCGAG |
| R: CCAGCCCATGATGGTTCTGAT | |
| Bcl-xL | F: TATTGGTGAGTCGGATCGCA |
| R: CTCTCAGCTGCTGCATTGTT | |
| IL-6 | F: ACTCCCTCTCCACAAGCGCCTT |
| R: TGGCATCTTCTTCCAGGCGTCCC | |
| TNF-α | F: GCCCACGTTGTAGCCAATGTCAAA |
| R: GTTGTCTTTCAGCTTCACGCCGTT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Q.; He, Q.; Zhu, W. Deoxynivalenol Mycotoxin Inhibits Rabies Virus Replication In Vitro. Int. J. Mol. Sci. 2023, 24, 7793. https://doi.org/10.3390/ijms24097793
Liu Q, He Q, Zhu W. Deoxynivalenol Mycotoxin Inhibits Rabies Virus Replication In Vitro. International Journal of Molecular Sciences. 2023; 24(9):7793. https://doi.org/10.3390/ijms24097793
Chicago/Turabian StyleLiu, Qian, Qing He, and Wuyang Zhu. 2023. "Deoxynivalenol Mycotoxin Inhibits Rabies Virus Replication In Vitro" International Journal of Molecular Sciences 24, no. 9: 7793. https://doi.org/10.3390/ijms24097793
APA StyleLiu, Q., He, Q., & Zhu, W. (2023). Deoxynivalenol Mycotoxin Inhibits Rabies Virus Replication In Vitro. International Journal of Molecular Sciences, 24(9), 7793. https://doi.org/10.3390/ijms24097793




