β-Secretase-1: In Silico Drug Reposition for Alzheimer’s Disease
Abstract
1. Introduction
2. Results and Discussion
3. Materials and Methods
3.1. Substrate, Inhibitors and DrugBank Data Base Preparation
3.2. Protein Preparation
3.3. Molecular Docking
3.4. ADME and Toxicological Properties and 2D Similitud Structure Prediction
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khot, K.B.; Gopan, G.; Bandiwadekar, A.; Jose, J. Current advancements related to phytobioactive compounds based liposomal delivery for neurodegenerative diseases. Ageing Res. Rev. 2023, 83, 101806. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Li, Y.; Meng, X. Vitamin D and neurodegenerative diseases. Heliyon 2023, 9, e12877. [Google Scholar] [CrossRef] [PubMed]
- Ishola, A.A.; Oyinloye, B.E.; Ajiboye, B.O.; Kappo, A.P. Molecular Docking Studies of Flavonoids from Andrographis paniculata as Potential Acetylcholinesterase, Butyrylcholinesterase and Monoamine Oxidase Inhibitors towards the Treatment of Neurodegenerative Diseases. Biointerface Res. Appl. Chem. 2020, 11, 9871–9879. [Google Scholar] [CrossRef]
- Mollaamin, F.; Monajjemi, M. Aging Genome Modification and Editing using the Crispr-Cas9 system: Anti-Alzheimer Study by Docking Methods. Biointerface Res. Appl. Chem. 2022, 13, 224. [Google Scholar] [CrossRef]
- Chen, P.; Zhao, K.; Zhang, H.; Wei, Y.; Wang, P.; Wang, D.; Song, C.; Yang, H.; Zhang, Z.; Yao, H.; et al. Altered global signal topography in Alzheimer’s disease. Ebiomedicine 2023, 89, 104455. [Google Scholar] [CrossRef]
- Scheltens, P.; De Strooper, B.; Kivipelto, M.; Holstege, H.; Chételat, G.; Teunissen, C.E.; Cummings, J.; van der Flier, W.M. Alzheimer’s disease. Lancet 2021, 397, 1577–1590. [Google Scholar] [CrossRef]
- Wang, D.; Honnorat, N.; Fox, P.T.; Ritter, K.; Eickhoff, S.B.; Seshadri, S.; Habes, M. Deep neural network heatmaps capture Alzheimer’s disease patterns reported in a large meta-analysis of neuroimaging studies. Neuroimage 2023, 269, 119929. [Google Scholar] [CrossRef]
- Nalivaeva, N.N.; Turner, A.J. AChE and the amyloid precursor protein (APP)—Cross-talk in Alzheimer’s disease. Chem.-Biol. Interact. 2016, 259, 301–306. [Google Scholar] [CrossRef]
- Peitzika, S.-C.; Pontiki, E. A Review on Recent Approaches on Molecular Docking Studies of Novel Compounds Targeting Acetylcholinesterase in Alzheimer Disease. Molecules 2023, 28, 1084. [Google Scholar] [CrossRef]
- Jaipea, S.; Saehlim, N.; Sutcharitruk, W.; Athipornchai, A.; Ingkaninan, K.; Saeeng, R. Synthesis of piperine analogues as AChE and BChE inhibitors for the treatment of Alzheimer’s disease. Phytochem. Lett. 2023, 53, 216–221. [Google Scholar] [CrossRef]
- Georgieva, D.; Nikolova, D.; Vassileva, E.; Kostova, B. Chitosan-Based Nanoparticles for Targeted Nasal Galantamine Delivery as a Promising Tool in Alzheimer’s Disease Therapy. Pharmaceutics 2023, 15, 829. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Singh, E. Antioxidants: An approach for restricting oxidative stress induced neurodegeneration in Alzheimer’s disease. Inflammopharmacology 2023, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, P.; Suwalsky, M.; Jemiola-Rzeminska, M.; Strzalka, K. Studies on the interaction of NMDA receptor antagonist memantine with cell membranes: A mini-review. Chem. Biol. Interact. 2018, 283, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Podkowa, K.; Czarnacki, K.; Borończyk, A.; Borończyk, M.; Paprocka, J. The NMDA receptor antagonists memantine and ketamine as anti-migraine agents. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2023, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Pichardo-Rojas, D.; Pichardo-Rojas, P.S.; Cornejo-Bravo, J.M.; Serrano-Medina, A. Memantine as a neuroprotective agent in ischemic stroke: Preclinical and clinical analysis. Front. Neurosci. 2023, 17, 1096372. [Google Scholar] [CrossRef] [PubMed]
- Koly, H.K.; Sutradhar, K.; Rahman, S. Acetylcholinesterase inhibition of Alzheimer’s disease: Identification of potential phytochemicals and designing more effective derivatives to manage disease condition. J. Biomol. Struct. Dyn. 2023, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.; Ran, Y.; Xie, F.; Liu, Y.; Wei, C.; Luan, X.; Wu, J. Design, synthesis, and biological evaluation of novel N-Benzyl piperidine derivatives as potent HDAC/AChE inhibitors for Alzheimer’s disease. Bioorg. Med. Chem. 2023, 80, 117178. [Google Scholar] [CrossRef] [PubMed]
- El-Damasy, A.K.; Park, J.E.; Kim, H.J.; Lee, J.; Bang, E.-K.; Kim, H.; Keum, G. Identification of New N-methyl-piperazine Chalcones as Dual MAO-B/AChE Inhibitors. Pharmaceuticals 2023, 16, 83. [Google Scholar] [CrossRef]
- Müller, S.A.; Shmueli, M.D.; Feng, X.; Tüshaus, J.; Schumacher, N.; Clark, R.; Smith, B.E.; Chi, A.; Rose-John, S.; Kennedy, M.E.; et al. The Alzheimer’s disease-linked protease BACE1 modulates neuronal IL-6 signaling through shedding of the receptor gp130. Mol. Neurodegener. 2023, 18, 13. [Google Scholar] [CrossRef]
- Nisa, N.; Rasmita, B.; Arati, C.; Uditraj, C.; Siddhartha, R.; Dinata, R.; Bhanushree, B.; Bidanchi, R.M.; Manikandan, B.; Laskar, S.A.; et al. Repurposing of phyto-ligand molecules from the honey bee products for Alzheimer’s disease as novel inhibitors of BACE-1: Small molecule bioinformatics strategies as amyloid-based therapy. Environ. Sci. Pollut. Res. 2023, 30, 51143–51169. [Google Scholar] [CrossRef]
- Martins, M.M.; Branco, P.S.; Ferreira, L.M. Enhancing the Therapeutic Effect in Alzheimer’s Disease Drugs: The role of Polypharmacology and Cholinesterase inhibitors. ChemistrySelect 2023, 8, e202300461. [Google Scholar] [CrossRef]
- Hillen, H. Editorial: Beta-Amyloid oligomer specific treatments for Alzheimer’s disease. Front. Neurosci. 2023, 17, 1034158. [Google Scholar] [CrossRef]
- Low, J.D.; Bartberger, M.D.; Cheng, Y.; Whittington, D.; Xue, Q.; Wood, S.; Allen, J.R.; Minatti, A.E. Diastereoselective synthesis of fused cyclopropyl-3-amino-2,4-oxazine β-amyloid cleaving enzyme (BACE) inhibitors and their biological evaluation. Bioorganic Med. Chem. Lett. 2018, 28, 1111–1115. [Google Scholar] [CrossRef] [PubMed]
- Munj, S.M.; Patil, P.B. Drug Discovery to Drug Development of Bace1 Inhibitor as Anti-Alzheimers’s: A Review. Curr. Top. Med. Chem. 2022, 23, 77–97. [Google Scholar] [CrossRef]
- Bakthavachalam, D.; Arumugam, S. Identification and characterization of bioactive peptides from marine crustacean crabs: A possible drug candidate for Alzheimer’s disease. Aquac. Int. 2023, 1–14. [Google Scholar] [CrossRef]
- Ding, M.; Niu, H.; Guan, P.; Hu, X. Molecularly imprinted sensor based on poly-o-phenylenediamine-hydroquinone polymer for β-amyloid-42 detection. Anal. Bioanal. Chem. 2023, 415, 1545–1557. [Google Scholar] [CrossRef]
- Acquasaliente, L.; De Filippis, V. The Role of Proteolysis in Amyloidosis. Int. J. Mol. Sci. 2022, 24, 699. [Google Scholar] [CrossRef]
- Weglinski, C.; Jeans, A. Amyloid-β in Alzheimer’s disease—Front and centre after all? Neuronal Signal. 2023, 7, NS20220086. [Google Scholar] [CrossRef]
- Stevenson-Hoare, J.; Heslegrave, A.; Leonenko, G.; Fathalla, D.; Bellou, E.; Luckcuck, L.; Marshall, R.; Sims, R.; Morgan, B.P.; Hardy, J.; et al. Plasma biomarkers and genetics in the diagnosis and prediction of Alzheimer’s disease. Brain 2022, 146, 690–699. [Google Scholar] [CrossRef]
- Suswidiantoro, V.; Ridlawati, F.; Karim, D.D.A.; Pratiwi, M.; Dwiningrum, R.; Safutri, W.; Putri, D.K.; Pisacha, I.M.; Rahayu, K.W. Pre-Dominance Herbs Medicine against Alzheimer’s Disease, In Vivo Studies: A Literature Review. J. Aisyah J. Ilmu. Kesehat. 2023, 8, 343–350. [Google Scholar] [CrossRef]
- Hoi, M.M.; Yue, Q. Emerging roles of astrocytes in blood-brain barrier disruption upon amyloid-beta insults in Alzheimer’s disease. Neural Regen. Res. 2023, 18, 1890–1902. [Google Scholar] [CrossRef]
- Tautou, M.; Descamps, F.; Larchanché, P.-E.; Buée, L.; El Bakali, J.; Melnyk, P.; Sergeant, N. A Polyaminobiaryl-Based β-secretase Modulator Alleviates Cognitive Impairments, Amyloid Load, Astrogliosis, and Neuroinflammation in APPSwe/PSEN1ΔE9 Mice Model of Amyloid Pathology. Int. J. Mol. Sci. 2023, 24, 5285. [Google Scholar] [CrossRef] [PubMed]
- Voss, T.; Kost, J.; Mercer, S.P.; Furtek, C.; Randolph, C.; Lines, C.; Egan, M.F.; Cummings, J.L. Progression from Prodromal Alzheimer’s Disease to Mild Alzheimer’s Disease Dementia in the Verubecestat APECS Study: Adjudicating Diagnostic Transitions. J. Alzheimer’s Dis. 2023, 92, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, M. Docking studies suggest the important role of interactions among the catalytic dyad and inhibitors for designing Bace1 specific inhibitors. J. Mol. Struct. 2020, 1208, 127893. [Google Scholar] [CrossRef]
- Salinas, G.L.R.; Rincón, A.L.; Machorro, J.G.; Basurto, J.C.; Archundia, M.M. In Silico Screening of Drugs That Target Different Forms of E Protein for Potential Treatment of COVID-19. Pharmaceuticals 2023, 16, 296. [Google Scholar] [CrossRef]
- Ortiz-Miravalles, L.; Sánchez-Angulo, M.; Sanz, J.M.; Maestro, B. Drug Repositioning as a Therapeutic Strategy against Streptococcus pneumoniae: Cell Membrane as Potential Target. Int. J. Mol. Sci. 2023, 24, 5831. [Google Scholar] [CrossRef]
- Qin, S.; Li, W.; Yu, H.; Xu, M.; Li, C.; Fu, L.; Sun, S.; He, Y.; Lv, J.; He, W.; et al. Guiding Drug Repositioning for Cancers Based on Drug Similarity Networks. Int. J. Mol. Sci. 2023, 24, 2244. [Google Scholar] [CrossRef]
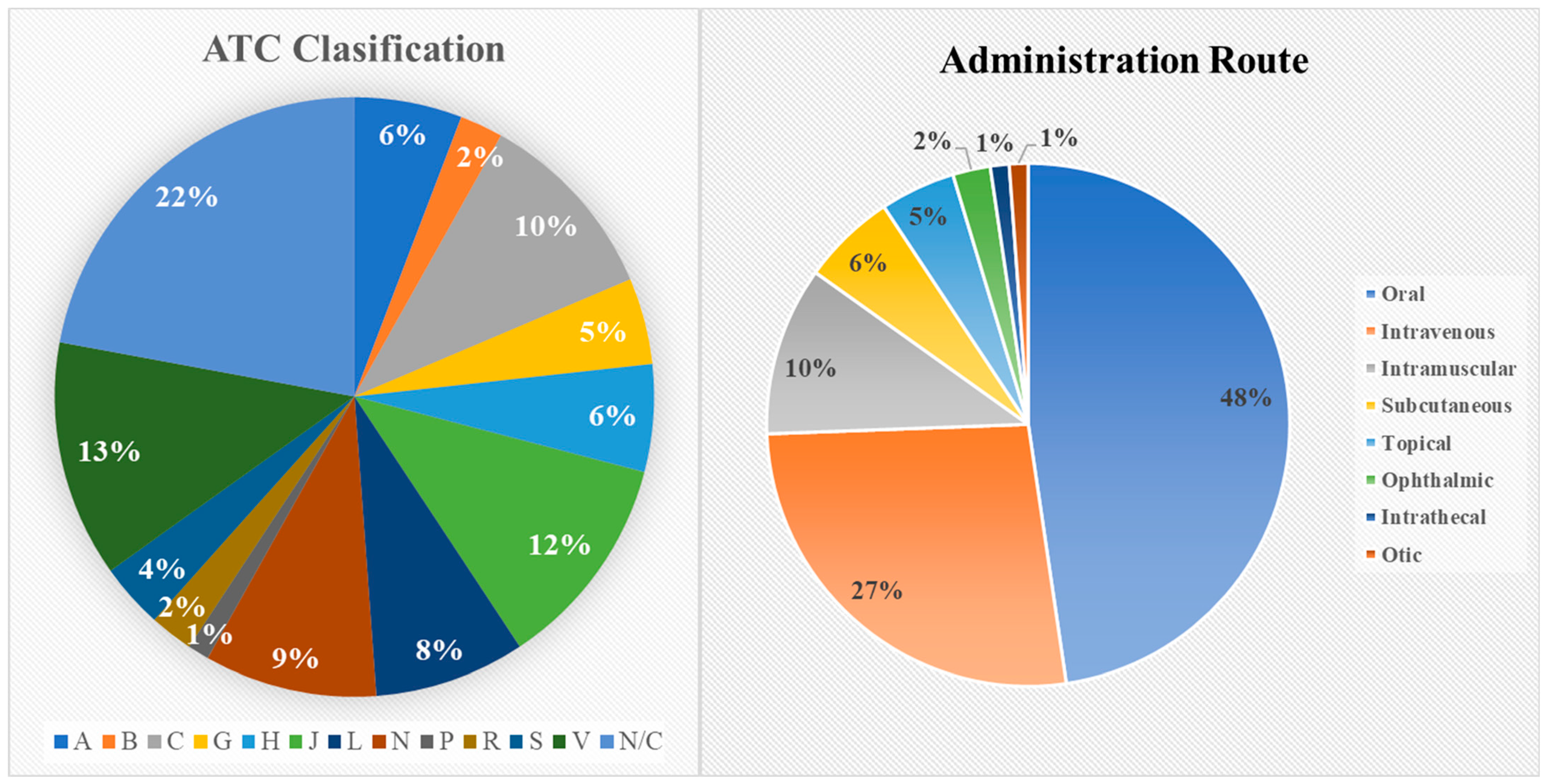
- Wishart, D.S.; Feunang, Y.D.; Guo, A.C.; Lo, E.J.; Marcu, A.; Grant, J.R.; Sajed, T.; Johnson, D.; Li, C.; Sayeeda, Z.; et al. DrugBank 5.0: A Major Update to the DrugBank Database for 2018. Nucleic Acids Res. 2018, 46, D1074–D1082. [Google Scholar] [CrossRef]
- Pratt, N.L.; Kerr, M.; Barratt, J.D.; Kemp-Casey, A.; Ellett, L.K.; Ramsay, E.; Roughead, L. The validity of the Rx-Risk Comorbidity Index using medicines mapped to the Anatomical Therapeutic Chemical (ATC) Classification System. BMJ Open 2018, 8, e021122. [Google Scholar] [CrossRef]
- Schrödinger, LLC. Schrödinger Release 2023-1: MacroModel; Schrödinger Inc.: New York, NY, USA, 2021. [Google Scholar]
- Schrödinger, LLC. Schrödinger Release 2022-3: LigPrep; Schrödinger Inc.: New York, NY, USA, 2021. [Google Scholar]
- Carrasco-Carballo, A.; Mendoza-Lara, D.F.; Rojas-Morales, J.A.; Altriste, V.; Merino-Montiel, P.; Luna, F.; Sandoval-Ramirez, J. In Silico Study of Coumarins Derivatives with Potential Use in Systemic Diseases. Biointerface Res. Appl. Chem. 2022, 13, 240. [Google Scholar] [CrossRef]
- Schrödinger, L.E. Schrödinger Release 2021-4: Protein Preparation Wizard; Schrödinger Inc.: New York, NY, USA, 2021. [Google Scholar]
- Schrödinger, LLC. Schrödinger Release 2023-1: Glide; Schrödinger Inc.: New York, NY, USA, 2021. [Google Scholar]
- Schrödinger, LLC. Schrödinger Release 2022-3: QikProp; Schrödinger Inc.: New York, NY, USA, 2021. [Google Scholar]
- Daina, A.; Michielin, O.; Zoete, V. SwissTargetPrediction: Updated data and new features for efficient prediction of protein targets of small molecules. Nucleic Acids Res. 2019, 47, W357–W364. [Google Scholar] [CrossRef] [PubMed]
- Filimonov, D.; Lagunin, A.A.; Gloriozova, T.A.; Rudik, A.; Druzhilovskii, D.S.; Pogodin, P.V.; Poroikov, V.V. Prediction of the Biological Activity Spectra of Organic Compounds Using the Pass Online Web Resource. Chem. Heterocycl. Compd. 2014, 50, 444–457. [Google Scholar] [CrossRef]

| DrugBank ID | Name | Binding Energy (kcal/mol) | Clinical Uses |
|---|---|---|---|
| DB14642 | Lypressin | −8.669 | Diabetes insipidus |
| DB00035 | Desmopressin | −8.298 | Antidiuretic, antihemophilic, and von Willebrand disease |
| DB06636 | Isavuconazonium | −7.587 | antifungal |
| DB01232 | Saquinavir | −7.501 | HIV-1 |
| DB00104 | Octreotide | −7.156 | Acromegaly and diarrhea-associated carcinoid tumors |
| DB11190 | Pantethine | −6.965 | dietary supplement |
| DB11691 | Naldemedine | −6.946 | Opioid-induced constipation |
| DB14753 | Hydroxystilbamidine | −6.689 | Blastomycosis, antifungal, and antitrypanosomal |
| DB00952 | Naratriptan | −6.648 | Migraine |
| DB00998 | Frovatriptan | −6.612 | Migraine |
| DB04703 | Hesperidin | −6.602 | Hemorrhoids, mild allergies |
| DB00430 | Cefpiramide | −6.595 | Antibiotic |
| DB01288 | Fenoterol | −6.550 | Asthma |
| DB00295 | Morphine | −6.467 | acute and chronic pain |
| DB01608 | Periciazine | −6.362 | Treatment of aggressiveness, impulsivity, and hostility |
| DB00481 | Raloxifene | −6.36 | Prevention of osteoporosis and breast cancer |
| DB08907 | Canagliflozin | −6.335 | Diabetes mellitus type 2 |
| DB00350 | Minoxidil | −6.334 | Hypertension |
| DB00284 | Acarbose | −6.274 | Diabetes mellitus type 2 |
| DB00489 | Sotalol | −6.249 | ventricular arrhythmias |
| DB00623 | Fluphenazine | −6.24 | Neuroleptic |
| DB00221 | Isoetharine | −6.204 | Emphysema, bronchitis, and asthma |
| DB00118 | Ademetionine | −6.18 | Chronic liver disease, depression, and osteoarthritis |
| DB00370 | Mirtazapine | −6.168 | antidepressant |
| DB12141 | Gilteritinib | −6.14 | relapsed acute myeloid leukemia |
| DB08995 | Diosmin | −6.135 | vascular enhancement |
| DB00850 | Perphenazine | −6.119 | Schizophrenia |
| DB12783 | Benserazide | −6.118 | Parkinson |
| DB12015 | Alpelisib | −6.09 | Cancer |
| DB01627 | Lincomycin | −6.075 | Antibiotic |
| DB00179 | Masoprocol | −6.073 | actinic keratoses |
| DB06401 | Bazedoxifene | −6.07 | menopause and osteoporosis |
| DB04861 | Nebivolol | −6.061 | Hypertension and heart failure |
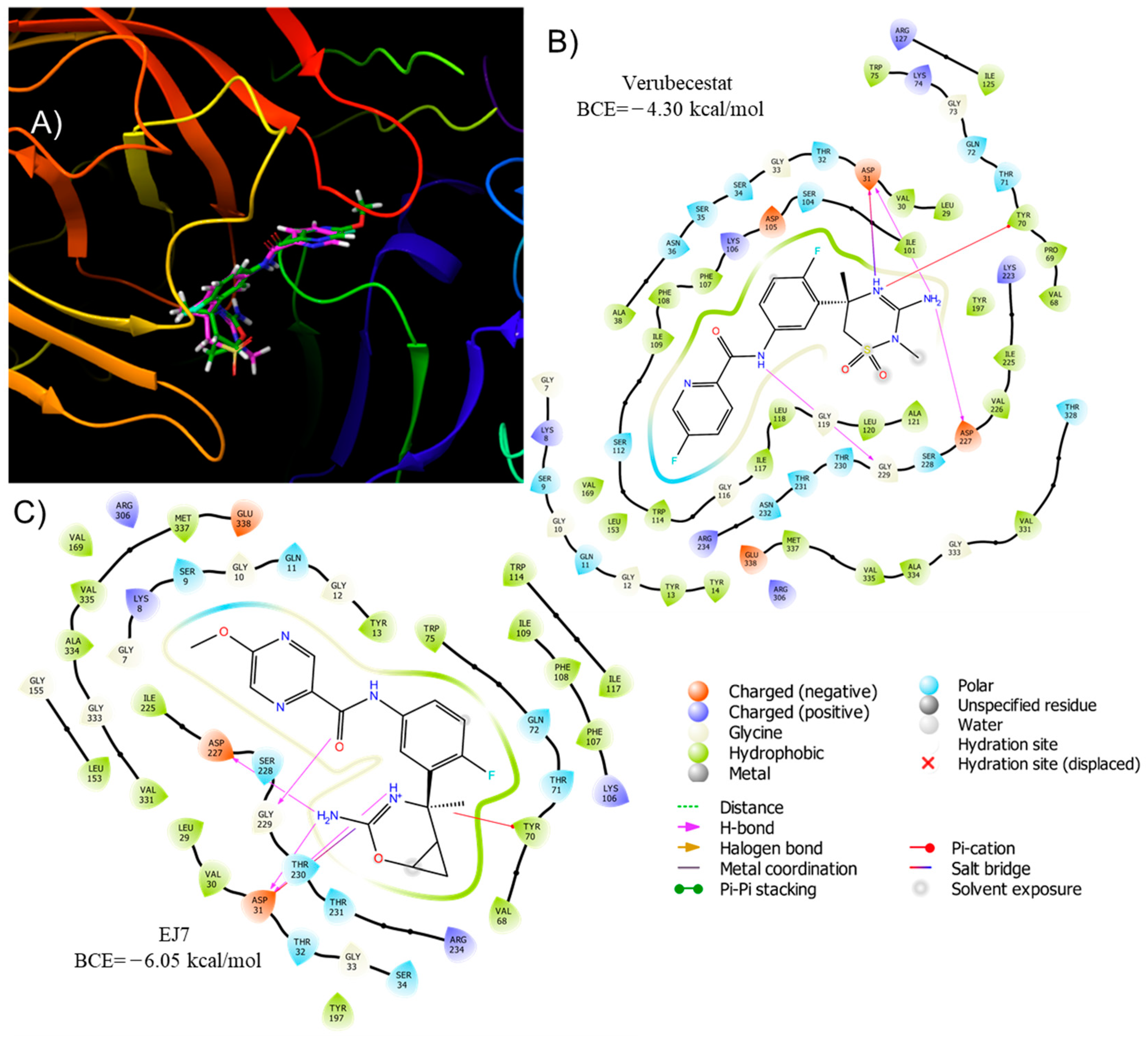
| DB12285 | Verubecestat | −4.298 | Alzheimer’s disease: β-secretase-1 inhibitor |
| Not Assigned | EJ7 | −6.050 | Alzheimer’s Disease Clinical trials |
| Name | Mol Weight | LogP | LogS | H-Bond (D/A) | Lipinsky Rule | QPlogBB * | CNS * | HOA * | #metab | PSA * | Jm * |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Desmopressin | 1069.22 | −5.81 | −10.59 | 12.5/26.3 | 3 | −10.59 | −2 | 1 | 18 | 493.82 | 0.000554 |
| Isavuconazonium | 717.77 | 1.73 | −5.16 | 2.0/9.0 | 3 | −0.61 | 0 | 1 | 15 | 159.37 | 0.000124 |
| Saquinavir | 670.85 | 2.56 | −3.61 | 5.0/13.7 | 3 | −2.13 | −2 | 2 | 7 | 181.08 | 0.006794 |
| Octreotide | 1019.24 | −0.18 | −0.05 | 9.5/20.1 | 3 | −6.01 | −2 | 1 | 17 | 351.65 | 0.006562 |
| Pantethine | 554.72 | −1.30 | −1.09 | 6.0/15.8 | 3 | −4.48 | −2 | 1 | 6 | 221.48 | 0.398822 |
| Naldemedine | 570.64 | 2.67 | −3.86 | 2.0/10.8 | 1 | −1.23 | −2 | 2 | 6 | 146.65 | 0.000286 |
| Hydroxystilbamidine | 280.33 | 0.80 | −2.23 | 7.0/3.8 | 1 | −2.62 | −2 | 2 | 1 | 117.38 | 0.000005 |
| Naratriptan | 335.46 | 2.19 | −3.69 | 2.0/6.5 | 0 | −0.56 | 1 | 3 | 3 | 70.45 | 0.000582 |
| Frovatriptan | 243.31 | 0.88 | −1.97 | 4.0/4.0 | 0 | −0.48 | 0 | 3 | 4 | 79.59 | 0.005498 |
| Hesperidin | 610.57 | −1.25 | −3.31 | 7.0/20.1 | 3 | −4.20 | −2 | 1 | 11 | 237.30 | 0.00026 |
| Cefpiramide | 612.63 | 1.70 | −5.68 | 2.3/13.0 | 2 | −4.72 | −2 | 1 | 7 | 260.97 | 0.0 |
| Fenoterol | 303.36 | 0.77 | −1.36 | 5.0/5.5 | 0 | −1.69 | −2 | 2 | 7 | 102.59 | 0.015216 |
| Raloxifene | 473.59 | 4.14 | −4.35 | 2.0/6.3 | 0 | −0.72 | 0 | 3 | 5 | 77.06 | 0.000973 |
| Fluphenazine | 437.52 | 4.33 | −4.13 | 1.0/6.2 | 0 | 0.66 | 2 | 3 | 7 | 36.16 | 0.000174 |
| Isoetharine | 239.31 | 0.52 | −1.17 | 4.0/4.7 | 0 | −0.71 | −1 | 2 | 4 | 74.28 | 0.368272 |
| Gilteritinib | 552.72 | 3.16 | −4.86 | 3.0/12.0 | 2 | −0.55 | 0 | 2 | 6 | 117.52 | 0.000001 |
| Diosmin | 608.55 | −1.22 | −3.23 | 7.0/19.8 | 3 | −4.23 | −2 | 1 | 9 | 237.23 | 0.000273 |
| Benserazide | 257.25 | −1.71 | 0.10 | 7.0/7.5 | 1 | −2.11 | −2 | 2 | 8 | 154.48 | 0.015535 |
| Alpelisib | 441.47 | 2.37 | −4.60 | 3.0/7.0 | 0 | −0.81 | −1 | 3 | 6 | 108.59 | 0.003243 |
| Lincomycin | 406.54 | 0.19 | −1.33 | 5.0/13.5 | 0 | −1.30 | −2 | 2 | 7 | 120.41 | 0.052177 |
| Masoprocol | 302.37 | 2.30 | −2.94 | 4.0/3.0 | 0 | −1.69 | −2 | 3 | 6 | 88.39 | 0.060709 |
| Bazedoxifene | 470.61 | 5.86 | −6.68 | 2.0/4.3 | 1 | −0.69 | 1 | 1 | 6 | 57.80 | 0.000017 |
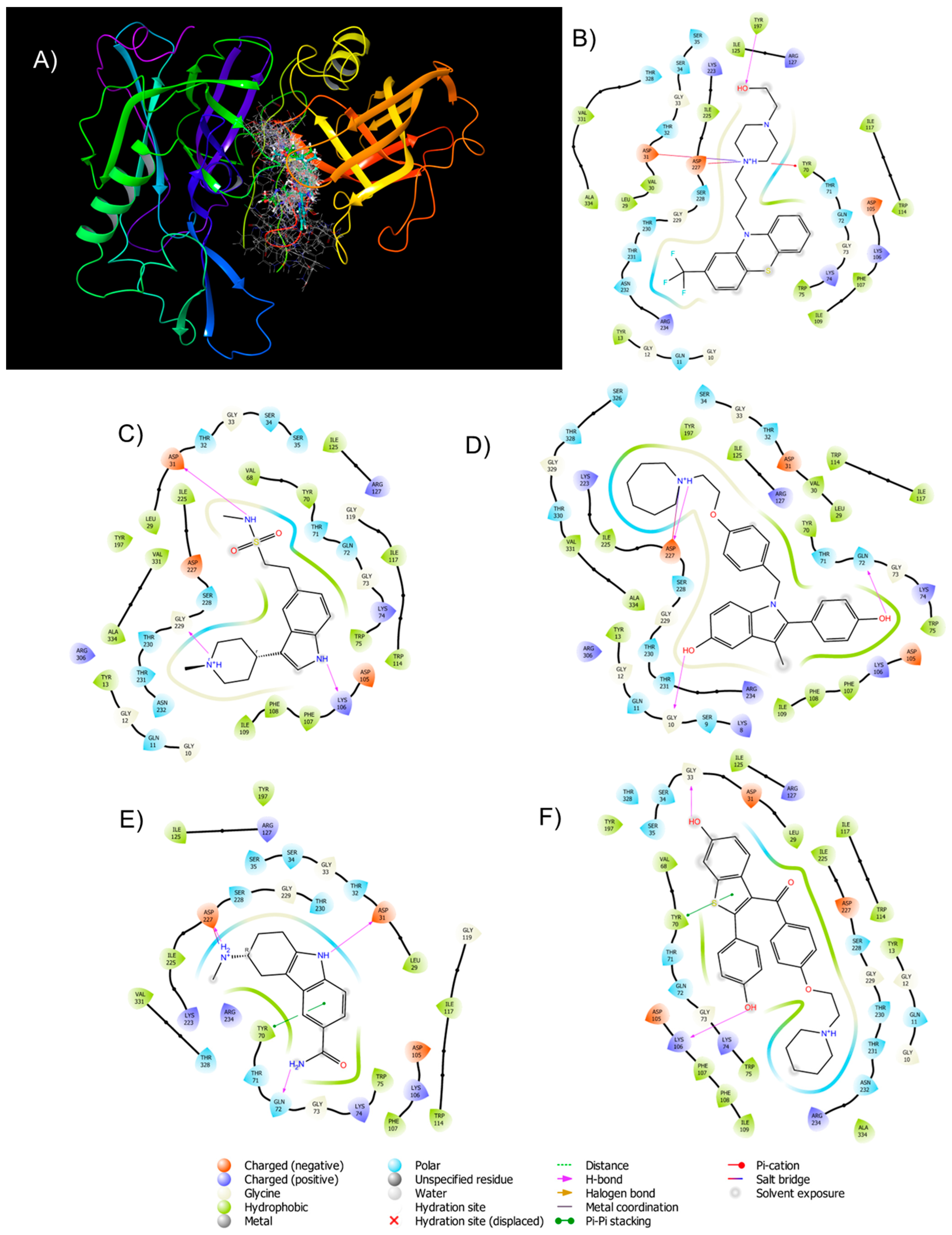
| Name | Charged (+) | Charged (−) | Gly | Polar | Hydrophobic | H-Bond | Pi-Pi Stacking | Pi-Cation | Salt Bidge |
|---|---|---|---|---|---|---|---|---|---|
| Fluphenazine | Lys74, Lys106, Arg127, Lys223, Arg234 | Asp31, Asp105, Asp227 | Gly10, Gly12, Gly33, Gly73, Gly229 | Gln11, Thr32, Ser34, Ser35, Thr71, Gln72, Ser228, Thr230, Thr231, Asn232, Thr328 | Try13, Leu29, Val30, Try70, Trp75, Phe107, Ile109, Trp114, Ile117, Try197, Ile225, Val331, Ala334 | Try197 | - | Try70 | Asp31, Asp227 |
| Naratriptan | Lys74, Lys106, Arg127, Arg306 | Asp31, Asp105, Asp227 | Gly10, Gly12, Gly33, Gly72, Gly119, Gly229 | Gln11, Thr32, Ser34, Ser35, Thr71, Gln72, Ser228, Thr230, Thr231, Asn232 | Leu29, Val68, Try70, Try197, Ile225 | Asp31, Lys106, Gly229 | - | - | - |
| Frovatriptan | Lys74, Lys106, Arg127, Lys223, Arg234 | Asp31, Asp105, Asp227 | Gly33, Gly119, Glu229 | Thr32, Ser34, Ser35, Thr71, Gln72, Ser228, Thr230, Thr328 | Leu29, Trp75, Phe107, Trp114, Ile117, Ile125, Try197, Ile225, Val331 | Asp31, Asp227 | Try70 | Asp227 | - |
| Raloxifene | Lys74, Lys106, Arg127, Arg234 | Asp31, Asp105, Asp227 | Gly10, Gly12, Gly229 | Gln11, Ser34, Ser35, Thr71, Gln72, Ser228, Thr230, Thr231, Asn232, Thr328 | Try13, Leu29, Val68, Trp75, Phe107, Phe108, Ile109, Trp114, Ile117, Ile125, Try197, Ile225, Ala334 | Gly33, Lys106 | Try70 | - | - |
| Bazedoxifene | Lys8, Lys74, Lys106, Arg127, Lys223, Arg234, Arg306 | Asp31, Asp105, Asp227 | Gly10, Gly12, Gly33, Gly73 | Ser9, Gln11, Thr32, Ser34, Thr71, Gln72, Thr230, Thr231, Ser326, Thr330, Thr328 | Try13, Leu29, Val30, Try70, Trp75, Phe107, Phe108, Ile109, Trp114, Ile117, Ile127, Try197, Ile225, Val331, Ala334 | Gly10, Gln72, Asp227 | - | - | Asp227 |
| Verubecestat | Lys8, Lys74, Lys106, Arg127, Lys223, Arg234 | Asp31, Asp105, Asp227, Glu338 | Gly10, Glu12, Gly33, Gly76, Gly119, Gly229, Glu333 | Ser9, Gln11, Thr32, Ser34, Ser35, Asn36, Thr71, Gln72, Ser112, Ser228, Thr230, Thr231, Asn232, Thr328 | Try13, Leu29, Val30, Ala38, Val68, Pro69, Try70, Trp75, Phe107, Phe108, Ile109, Trp114, Ile117, Ile125, Val331, Ala334, Val335 | Asp31(2), Asp227, Gly229 | - | Try70 | Asp31 |
| EJ7 | Lys8, Lys74, Lys106, Arg127, Arg234, Arg306 | Asp31, Asp227, Glu338 | Gly7, Gly10, Gly12, Gly33, Gly73, Gly115, Gly119, Gly229, Gly333 | Ser9, Gln11, Thr32, Ser34, Ser35, Asn36, Thr71, Gln72, Ser112, Ser228, Thr230, Thr231, Asn232 | Leu29, Val30, Ala38, Val68, Pro69, Try70, Trp75, Phe107, Phe108, Ile109, Trp114, Ile117, Leu153, Ile225, Val331, Ala334, Val335, Met337 | Asp31(2), Asp227, Gly229 | - | Try70 | Asp31 |
| Name | Adverse Effects |
|---|---|
| Fluphenazine | Drowsiness, lethargy, dizziness, lightheadedness, nausea, loss of appetite, sweating, dry mouth, blurred vision, headache, constipation. |
| Naratriptan | Severe chest pain, heaviness, tightness or pain in the chest, throat, and sleepiness, burning sensation, tingling, numbness, seizures. |
| Frovatriptan | Sudden severe stomach pain, bloody diarrhea, severe chest pain, difficulty breathing, irregular heartbeat, cramps, numbness, chest pain or pressure, agitation, hallucination, hyperactive reflexes, diarrhea. |
| Raloxifene | Hot flashes, leg cramps, swelling in the hands, feet, ankles, or lower legs, generates flu syndrome, joint pain, sweating, difficulty sleeping. |
| Bazedoxifene | Nausea, heartburn, stomach pain, diarrhea, muscle spasms, neck, and throat pain |
| Verubecestat | Injuries, falls, suicidal ideation, weight loss, sleep disorders, rashes, hair color change, dizziness, anxiety. |
| EJ7 | No reports by preclinical studies. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galeana-Ascencio, R.A.; Mendieta, L.; Limon, D.I.; Gnecco, D.; Terán, J.L.; Orea, M.L.; Carrasco-Carballo, A. β-Secretase-1: In Silico Drug Reposition for Alzheimer’s Disease. Int. J. Mol. Sci. 2023, 24, 8164. https://doi.org/10.3390/ijms24098164
Galeana-Ascencio RA, Mendieta L, Limon DI, Gnecco D, Terán JL, Orea ML, Carrasco-Carballo A. β-Secretase-1: In Silico Drug Reposition for Alzheimer’s Disease. International Journal of Molecular Sciences. 2023; 24(9):8164. https://doi.org/10.3390/ijms24098164
Chicago/Turabian StyleGaleana-Ascencio, Roberto A., Liliana Mendieta, Daniel I. Limon, Dino Gnecco, Joel L. Terán, María L. Orea, and Alan Carrasco-Carballo. 2023. "β-Secretase-1: In Silico Drug Reposition for Alzheimer’s Disease" International Journal of Molecular Sciences 24, no. 9: 8164. https://doi.org/10.3390/ijms24098164
APA StyleGaleana-Ascencio, R. A., Mendieta, L., Limon, D. I., Gnecco, D., Terán, J. L., Orea, M. L., & Carrasco-Carballo, A. (2023). β-Secretase-1: In Silico Drug Reposition for Alzheimer’s Disease. International Journal of Molecular Sciences, 24(9), 8164. https://doi.org/10.3390/ijms24098164






