Risk Effects of rs1799945 Polymorphism of the HFE Gene and Intergenic Interactions of GWAS-Significant Loci for Arterial Hypertension in the Caucasian Population of Central Russia
Abstract
1. Introduction
2. Results
2.1. Functional Annotation of AH-Associated SNPs
2.1.1. Non-Synonymous and Epigenetic-Significant Loci
2.1.2. Plausible Gene Expression (eQTL) and Splicing (sQTL) Regulatory Potential of AH-Involved SNPs
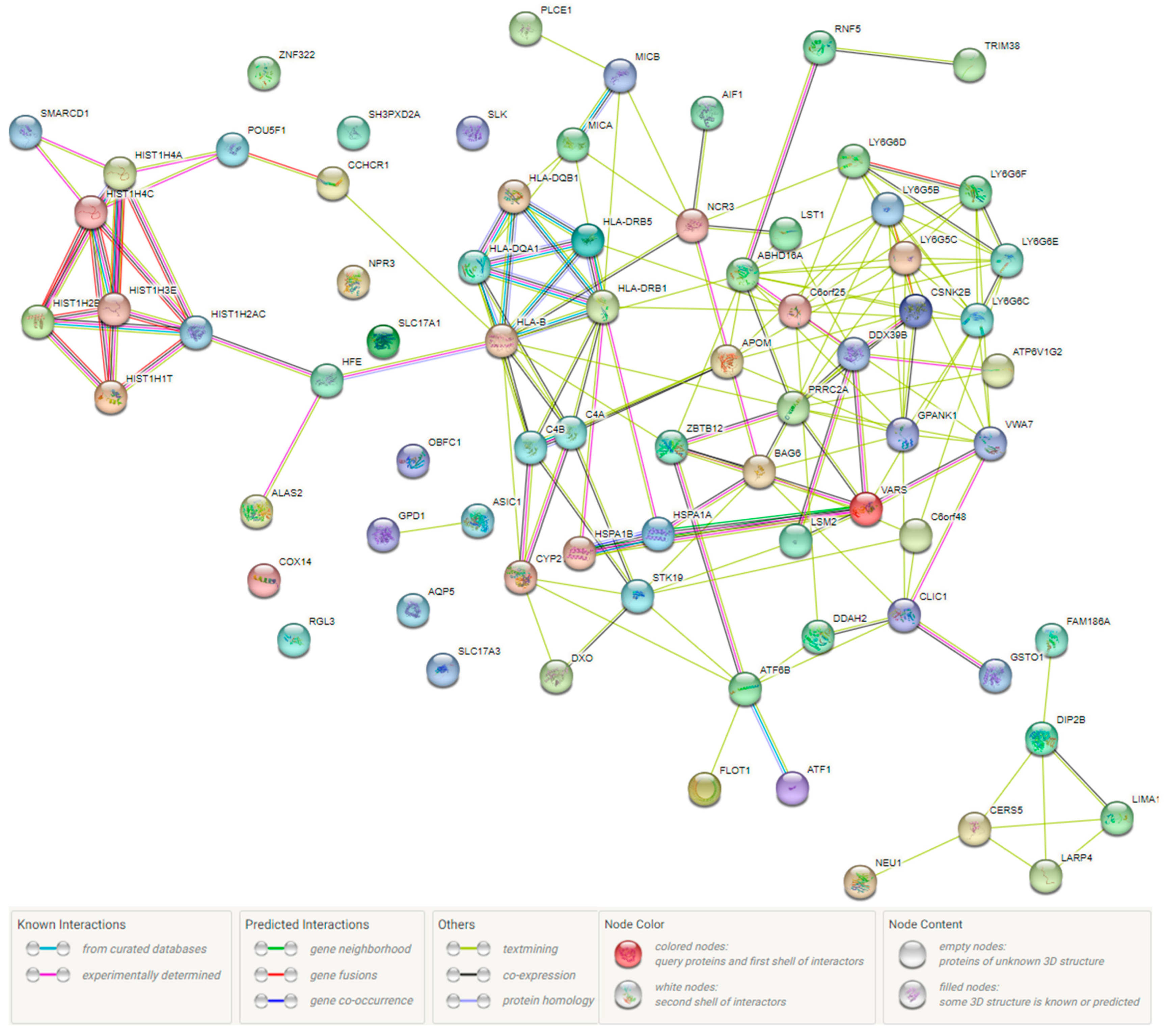
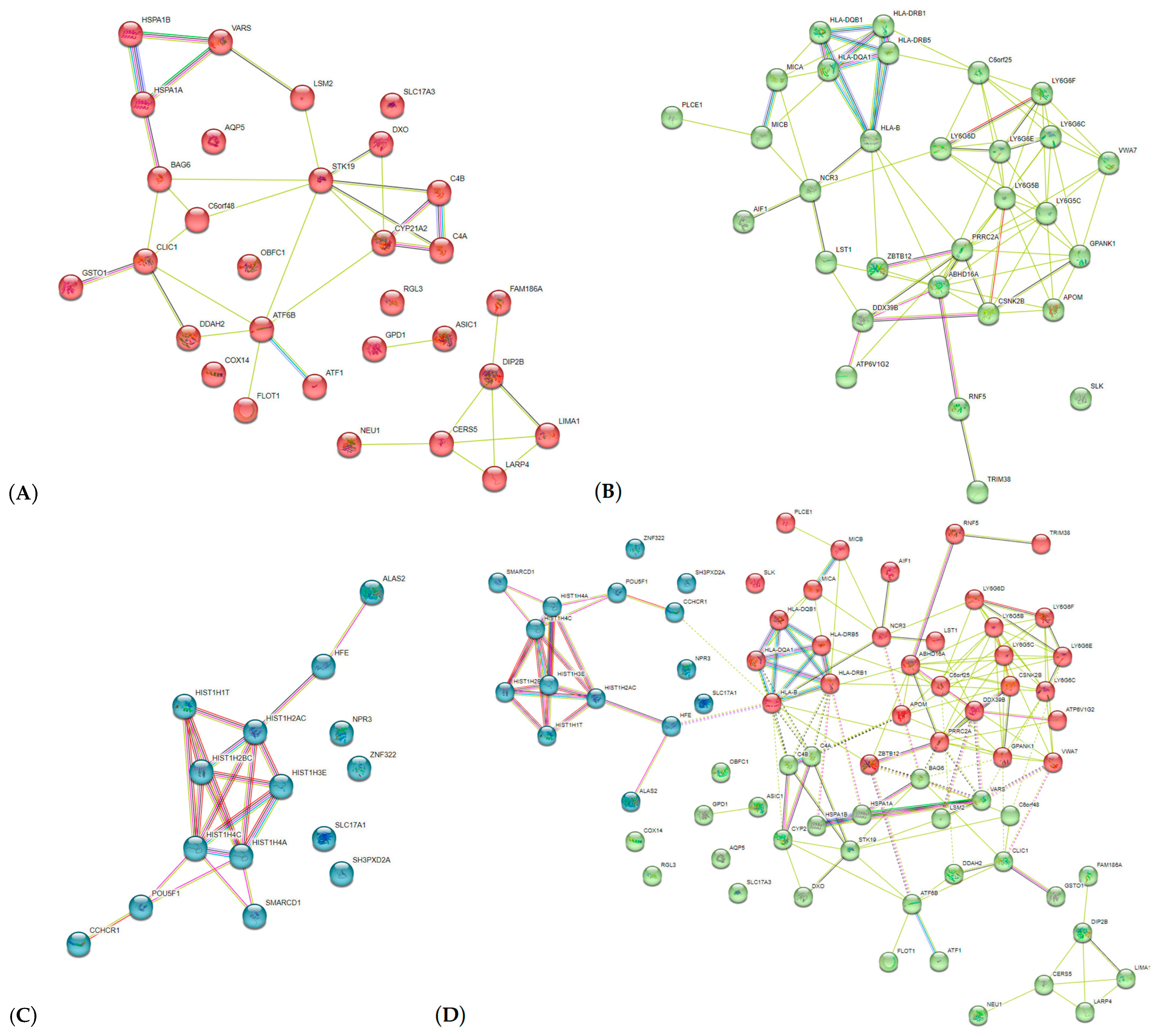
2.1.3. Pathway Analysis of AH-Associated Genes
3. Discussion
4. Materials and Methods
4.1. Study Subjects
4.2. Experimental Genetic Analysis (DNA Isolation; SNPs Selection; SNPs Genotyping)
4.3. Statistical Analysis of Genetic Data
4.4. SNPs/Gene Predict Functionality/Functions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef] [PubMed]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R.; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.H.; Liu, P.; Roth, G.A.; Ng, M.; Biryukov, S.; Marczak, L.; Alexander, L.; Estep, K.; Hassen Abate, K.; Akinyemiju, T.F.; et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990–2015. JAMA 2017, 317, 165–182. [Google Scholar] [CrossRef]
- Ehret, G.B. Genome-wide association studies: Contribution of genomics to understanding blood pressure and essential hypertension. Curr. Hypertens. Rep. 2010, 12, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Ehret, G.B.; Caulfield, M.J. Genes for blood pressure: An opportunity to understand hypertension. Eur. Heart J. 2013, 34, 951–961. [Google Scholar] [CrossRef]
- Evangelou, E.; Warren, H.R.; Mosen-Ansorena, D.; Mifsud, B.; Pazoki, R.; Gao, H.; Ntritsos, G.; Dimou, N.; Cabrera, C.P.; Karaman, I.; et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat. Genet. 2018, 50, 1412–1425. [Google Scholar] [CrossRef]
- Surendran, P.; Feofanova, E.V.; Lahrouchi, N.; Ntalla, I.; Karthikeyan, S.; Cook, J.; Chen, L.; Mifsud, B.; Yao, C.; Kraja, A.T.; et al. Discovery of rare variants associated with blood pressure regulation through meta-analysis of 1.3 million individuals. Nat. Genet. 2020, 52, 1314–1332. [Google Scholar] [CrossRef]
- Lip, S.; Padmanabhan, S. Genomics of Blood Pressure and Hypertension: Extending the Mosaic Theory Toward Stratification. Can. J. Cardiol. 2020, 36, 694–705. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, W.; Li, Z.; Xu, C.; Tian, X.; Zhang, D. Heritability and genome-wide association study of blood pressure in Chinese adult twins. Mol. Genet. Genom. Med. 2021, 9, e1828. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhan, S.; Dominiczak, A.F. Genomics of hypertension: The road to precision medicine. Nat. Rev. Cardiol. 2021, 18, 235–250. [Google Scholar] [CrossRef] [PubMed]
- Bushueva, O.; Solodilova, M.; Churnosov, M.; Ivanov, V.; Polonikov, A. The Flavin-containing monooxygenase 3 gene and essential hypertension: The joint effect of polymorphism E158K and cigarette smoking on disease susceptibility. Int. J. Hypertens. 2014, 2014, 712169. [Google Scholar] [CrossRef]
- Polonikov, A.V.; Ushachev, D.V.; Ivanov, V.P.; Churnosov, M.I.; Freidin, M.B.; Ataman, A.V.; Harbuzova, V.Y.; Bykanova, M.A.; Bushueva, O.Y.; Solodilova, M.A. Altered erythrocyte membrane protein composition mirrors pleiotropic effects of hypertension susceptibility genes and disease pathogenesis. J. Hypertens. 2015, 33, 2265–2277. [Google Scholar] [CrossRef]
- Polonikov, A.V.; Bushueva, O.Y.; Bulgakova, I.V.; Freidin, M.B.; Churnosov, M.I.; Solodilova, M.A.; Shvetsov, Y.D.; Ivanov, V.P. A comprehensive contribution of genes for aryl hydrocarbon receptor signaling pathway to hypertension susceptibility. Pharmacogenet. Genom. 2017, 27, 57–69. [Google Scholar] [CrossRef]
- Fan, W.; Qu, X.; Li, J.; Wang, X.; Bai, Y.; Cao, Q.; Ma, L.; Zhou, X.; Zhu, W.; Liu, W.; et al. Associations between polymorphisms of the ADIPOQ gene and hypertension risk: A systematic and meta-analysis. Sci. Rep. 2017, 9, 41683. [Google Scholar] [CrossRef]
- Polonikov, A.; Bykanova, M.; Ponomarenko, I.; Sirotina, S.; Bocharova, A.; Vagaytseva, K.; Stepanov, V.; Churnosov, M.; Bushueva, O.; Solodilova, M.; et al. The contribution of CYP2C gene subfamily involved in epoxygenase pathway of arachidonic acids metabolism to hypertension susceptibility in Russian population. Clin. Exp. Hypertens. 2017, 39, 306–311. [Google Scholar] [CrossRef]
- Moskalenko, M.I.; Milanova, S.N.; Ponomarenko, I.V.; Polonikov, A.V.; Churnosov, M.I. Study of associations of polymorphism of matrix metalloproteinases genes with the development of arterial hypertension in men. Kardiologiia 2019, 59, 31–39. [Google Scholar] [CrossRef]
- Zhang, H.; Pushkarev, B.; Zhou, J.; Mu, Y.; Bolshakova, O.; Shrestha, S.; Wang, N.; Jian, B.; Jin, M.; Zhang, K.; et al. CACNA1C rs1006737 SNP increases the risk of essential hypertension in both Chinese Han and ethnic Russian people of Northeast Asia. Medicine 2021, 100, e24825. [Google Scholar] [CrossRef]
- Moskalenko, M.; Ponomarenko, I.; Reshetnikov, E.; Dvornyk, V.; Churnosov, M. Polymorphisms of the matrix metalloproteinase genes are associated with essential hypertension in a Caucasian population of Central Russia. Sci. Rep. 2021, 11, 5224. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Yamazaki, K.; Kamatani, Y.; Kubo, M.; Matsuda, K.; Asai, S. A genome-wide association study identifies a novel candidate locus at the DLGAP1 gene with susceptibility to resistant hypertension in the Japanese population. Sci. Rep. 2021, 11, 19497. [Google Scholar] [CrossRef] [PubMed]
- Alsamman, A.M.; Almabrazi, H.; Zayed, H. Whole-Genome Sequencing of 100 Genomes Identifies a Distinctive Genetic Susceptibility Profile of Qatari Patients with Hypertension. J. Pers. Med. 2022, 12, 722. [Google Scholar] [CrossRef] [PubMed]
- Jamshidi, J.; Asnaashari, A.; Alipoor, R.; Mohammadi, S.; Roostaei, S.; Samadian, M.M.; Honarmand Aliabadi, S.; Bahramali, E. ATP2B1 rs2681472 and STK39 rs35929607 polymorphisms and risk of Hypertension in Iranian Population. Med. J. Islam. Repub. Iran 2018, 32, 14. [Google Scholar] [CrossRef] [PubMed]
- Lule, S.A.; Mentzer, A.J.; Namara, B.; Muwenzi, A.G.; Nassanga, B.; Kizito, D.; Akurut, H.; Lubyayi, L.; Tumusiime, J.; Zziwa, C.; et al. A genome-wide association and replication study of blood pressure in Ugandan early adolescents. Mol. Genet. Genom. Med. 2019, 7, e00950. [Google Scholar] [CrossRef]
- Soltész, B.; Pikó, P.; Sándor, J.; Kósa, Z.; Ádány, R.; Fiatal, S. The genetic risk for hypertension is lower among the Hungarian Roma population compared to the general population. PLoS ONE 2020, 15, e0234547. [Google Scholar] [CrossRef]
- Kaur, H.; Crawford, D.C.; Liang, J.; Benchek, P.; Zhu, X.; Kallianpur, A.R.; Bush, W.S.; COGENT BP Consortium. Replication of European hypertension associations in a case-control study of 9534 African Americans. PLoS ONE 2021, 16, e0259962. [Google Scholar] [CrossRef]
- Althwab, S.A.; Ahmed, A.A.; Rasheed, Z.; Alkhowailed, M.; Hershan, A.; Alsagaby, S.; Alblihed, M.A.; Alaqeel, A.; Alrehaili, J.; Alhumaydhi, F.A.; et al. ATP2B1 genotypes rs2070759 and rs2681472 polymorphisms and risk of hypertension in Saudi population. Nucleosides Nucleotides Nucleic Acids 2021, 40, 1075–1089. [Google Scholar] [CrossRef]
- International Consortium for Blood Pressure Genome-Wide Association Studies; Ehret, G.B.; Munroe, P.B.; Rice, K.M.; Bochud, M.; Johnson, A.D.; Chasman, D.I.; Smith, A.V.; Tobin, M.D.; Verwoert, G.C.; et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011, 478, 103–109. [Google Scholar] [CrossRef]
- Surendran, P.; Drenos, F.; Young, R.; Warren, H.; Cook, J.P.; Manning, A.K.; Grarup, N.; Sim, X.; Barnes, D.R.; Witkowska, K.; et al. Trans-ancestry meta-analyses identify rare and common variants associated with blood pressure and hypertension. Nat. Genet. 2016, 48, 1151–1161. [Google Scholar] [CrossRef]
- Liu, C.; Kraja, A.T.; Smith, J.A.; Brody, J.A.; Franceschini, N.; Bis, J.C.; Rice, K.; Morrison, A.C.; Lu, Y.; Weiss, S.; et al. Meta-analysis identifies common and rare variants influencing blood pressure and overlapping with metabolic trait loci. Nat. Genet. 2016, 48, 1162–1170. [Google Scholar] [CrossRef] [PubMed]
- Ehret, G.B.; Ferreira, T.; Chasman, D.I.; Jackson, A.U.; Schmidt, E.M.; Johnson, T.; Thorleifsson, G.; Luan, J.; Donnelly, L.A.; Kanoni, S.; et al. The genetics of blood pressure regulation and its target organs from association studies in 342,415 individuals. Nat. Genet. 2016, 48, 1171–1184. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.J.; Ehret, G.B.; Nandakumar, P.; Ranatunga, D.; Schaefer, C.; Kwok, P.Y.; Iribarren, C.; Chakravarti, A.; Risch, N. Genome-wide association analyses using electronic health records identify new loci influencing blood pressure variation. Nat. Genet. 2017, 49, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Wain, L.V.; Vaez, A.; Jansen, R.; Joehanes, R.; van der Most, P.J.; Erzurumluoglu, A.M.; O’Reilly, P.F.; Cabrera, C.P.; Warren, H.R.; Rose, L.M.; et al. Novel Blood Pressure Locus and Gene Discovery Using Genome-Wide Association Study and Expression Data Sets from Blood and the Kidney. Hypertension 2017, 70, e4–e19. [Google Scholar] [CrossRef] [PubMed]
- Sung, Y.J.; Winkler, T.W.; de Las Fuentes, L.; Bentley, A.R.; Brown, M.R.; Kraja, A.T.; Schwander, K.; Ntalla, I.; Guo, X.; Franceschini, N.; et al. A Large-Scale Multi-ancestry Genome-wide Study Accounting for Smoking Behavior Identifies Multiple Significant Loci for Blood Pressure. Am. J. Hum. Genet. 2018, 102, 375–400. [Google Scholar] [CrossRef]
- Gill, D.; Benyamin, B.; Moore, L.S.P.; Monori, G.; Zhou, A.; Koskeridis, F.; Evangelou, E.; Laffan, M.; Walker, A.P.; Tsilidis, K.K.; et al. Associations of genetically determined iron status across the phenome: A mendelian randomization study. PLoS Med. 2019, 16, e1002833. [Google Scholar] [CrossRef]
- Lu, W.; Pikhart, H.; Tamosiunas, A.; Kubinova, R.; Capkova, N.; Malyutina, S.; Pająk, A.; Bobak, M. Prevalence, awareness, treatment and control of hypertension, diabetes and hypercholesterolemia, and associated risk factors in the Czech Republic, Russia, Poland and Lithuania: A cross-sectional study. BMC Public Health 2022, 22, 883. [Google Scholar] [CrossRef]
- Talbert, P.B.; Henikoff, S. Histone variants at a glance. J. Cell Sci. 2021, 134, jcs244749. [Google Scholar] [CrossRef]
- Li, Y.; Wang, Y.; Zhang, C.; Yuan, W.; Wang, J.; Zhu, C.; Chen, L.; Huang, W.; Zeng, W.; Wu, X.; et al. ZNF322, a novel human C2H2 Kruppel-like zinc-finger protein, regulates transcriptional activation in MAPK signaling pathways. Biochem. Biophys. Res. Commun. 2004, 325, 1383–1392. [Google Scholar] [CrossRef]
- GeneCards: The Human Gene Database. Available online: https://www.genecards.org/cgi-bin/carddisp.pl?gene=STN1 (accessed on 16 October 2022).
- Wan, M.; Qin, J.; Songyang, Z.; Liu, D. OB fold-containing protein 1 (OBFC1), a human homolog of yeast Stn1, associates with TPP1 and is implicated in telomere length regulation. J. Biol. Chem. 2009, 284, 26725–26731. [Google Scholar] [CrossRef]
- Said, M.A.; Eppinga, R.N.; Hagemeijer, Y.; Verweij, N.; van der Harst, P. Telomere Length and Risk of Cardiovascular Disease and Cancer. J. Am. Coll. Cardiol. 2017, 70, 506–507. [Google Scholar] [CrossRef] [PubMed]
- Maubaret, C.G.; Salpea, K.D.; Romanoski, C.E.; Folkersen, L.; Cooper, J.A.; Stephanou, C.; Li, K.W.; Palmen, J.; Hamsten, A.; Neil, A.; et al. Association of TERC and OBFC1 haplotypes with mean leukocyte telomere length and risk for coronary heart disease. PLoS ONE 2013, 8, e83122. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Iturbe, B.; Pons, H.; Johnson, R.J. Role of the Immune System in Hypertension. Physiol. Rev. 2017, 97, 1127–1164. [Google Scholar] [CrossRef] [PubMed]
- Drummond, G.R.; Vinh, A.; Guzik, T.J.; Sobey, C.G. Immune mechanisms of hypertension. Nat. Rev. Immunol. 2019, 19, 517–532. [Google Scholar] [CrossRef]
- Carnagarin, R.; Matthews, V.; Zaldivia, M.T.K.; Peter, K.; Schlaich, M.P. The bidirectional interaction between the sympathetic nervous system and immune mechanisms in the pathogenesis of hypertension. Br. J. Pharmacol. 2019, 176, 1839–1852. [Google Scholar] [CrossRef]
- Mikolajczyk, T.P.; Guzik, T.J. Adaptive Immunity in Hypertension. Curr. Hypertens. Rep. 2019, 21, 68. [Google Scholar] [CrossRef]
- Churnosov, M.; Abramova, M.; Reshetnikov, E.; Lyashenko, I.V.; Efremova, O.; Churnosova, M.; Ponomarenko, I. Polymorphisms of hypertension susceptibility genes as a risk factors of preeclampsia in the Caucasian population of central Russia. Placenta 2022, 129, 51–61. [Google Scholar] [CrossRef]
- Litovkina, O.; Nekipelova, E.; Dvornyk, V.; Polonikov, A.; Efremova, O.; Zhernakova, N.; Reshetnikov, E.; Churnosov, M. Genes involved in the regulation of vascular homeostasis determine renal survival rate in patients with chronic glomerulo-nephritis. Gene 2014, 546, 112–116. [Google Scholar] [CrossRef]
- Reshetnikov, E.A.; Akulova, L.Y.; Dobrodomova, I.S.; Dvornyk, V.Y.; Polonikov, A.V.; Churnosov, M.I. The insertion-deletion polymorphism of the ACE gene is associated with increased blood pressure in women at the end of pregnancy. J. Renin Angiotensin Aldosterone Syst. 2015, 16, 623–632. [Google Scholar] [CrossRef]
- Ivanova, T.A. Polymorphic loci of AC026703.1 and HFE genes are associated with severe hypertension. Res. Results Biomed. 2023, 9, 22–38. [Google Scholar] [CrossRef]
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert 802 Consultation; World Health Organization: Geneva, Switzerland, 2003; 148p. [Google Scholar]
- Ponomarenko, I.; Reshetnikov, E.; Altuchova, O.; Polonikov, A.; Sorokina, I.; Yermachenko, A.; Dvornyk, V.; Golovchenko, O.; Churnosov, M. Association of genetic polymorphisms with age at menarche in Russian women. Gene 2019, 686, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Eliseeva, N.; Ponomarenko, I.; Reshetnikov, E.; Dvornyk, V.; Churnosov, M. LOXL1 gene polymorphism candidates for exfoliation glaucoma are also associated with a risk for primary open-angle glaucoma in a Caucasian population from central Russia. Mol. Vis. 2021, 27, 262–269. [Google Scholar] [PubMed]
- Ward, L.D.; Kellis, M. HaploReg v4: Systematic mining of putative causal variants, cell types, regulators and target genes for human complex traits and disease. Nucleic Acids Res. 2016, 44, D877–D881. [Google Scholar] [CrossRef]
- Abramova, M.; Churnosova, M.; Efremova, O.; Aristova, I.; Reshetnikov, E.; Polonikov, A.; Churnosov, M.; Ponomarenko, I. Effects of pre-pregnancy over-weight/obesity on the pattern of association of hypertension susceptibility genes with preeclampsia. Life 2022, 12, 2018. [Google Scholar] [CrossRef] [PubMed]
- Abramova, M.Y. Genetic markers of severe preeclampsia. Res. Results Biomed. 2022, 8, 305–316. [Google Scholar] [CrossRef]
- Reshetnikov, E.; Zarudskaya, O.; Polonikov, A.; Bushueva, O.; Orlova, V.; Krikun, E.; Dvornyk, V.; Churnosov, M. Genetic markers for inherited thrombophilia are associated with fetal growth retardation in the population of Central Russia. J. Obstet. Gynaecol. Res. 2017, 43, 1139–1144. [Google Scholar] [CrossRef]
- Golovchenko, O.; Abramova, M.; Ponomarenko, I.; Reshetnikov, E.; Aristova, I.; Polonikov, A.; Dvornyk, V.; Churnosov, M. Functionally significant polymorphisms of ESR1and PGR and risk of intrauterine growth restriction in population of Central Russia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 253, 52–57. [Google Scholar] [CrossRef]
- Starikova, D.; Ponomarenko, I.; Reshetnikov, E.; Dvornyk, V.; Churnosov, M. Novel Data about Association of the Functionally Significant Polymorphisms of the MMP9 Gene with Exfoliation Glaucoma in the Caucasian Population of Central Russia. Ophthalmic Res. 2021, 64, 458–464. [Google Scholar] [CrossRef]
- Sirotina, S.; Ponomarenko, I.; Kharchenko, A.; Bykanova, M.; Bocharova, A.; Vagaytseva, K.; Stepanov, V.; Churnosov, M.; Solodilova, M.; Polonikov, A. A Novel Polymorphism in the Promoter of the CYP4A11 Gene Is Associated with Susceptibility to Coronary Artery Disease. Dis. Markers 2018, 2018, 5812802. [Google Scholar] [CrossRef]
- Tikunova, E.; Ovtcharova, V.; Reshetnikov, E.; Dvornyk, V.; Polonikov, A.; Bushueva, O.; Churnosov, M. Genes of tumor necrosis factors and their receptors and the primary open angle glaucoma in the population of Central Russia. Int. J. Ophthalmol. 2017, 10, 1490–1494. [Google Scholar] [CrossRef]
- Pavlova, N.; Demin, S.; Churnosov, M.; Reshetnikov, E.; Aristova, I.; Churnosova, M.; Ponomarenko, I. The Modifying Effect of Obesity on the Association of Matrix Metalloproteinase Gene Polymorphisms with Breast Cancer Risk. Biomedicines 2022, 10, 2617. [Google Scholar] [CrossRef] [PubMed]
- Ponomarenko, I.; Reshetnikov, E.; Polonikov, A.; Verzilina, I.; Sorokina, I.; Elgaeva, E.E.; Tsepilov, Y.A.; Yermachenko, A.; Dvornyk, V.; Churnosov, M. Candidate genes for age at menarche are associated with endometriosis. Reprod. Biomed. Online 2020, 41, 943–956. [Google Scholar] [CrossRef] [PubMed]
- Purcell, S.; Neale, B.; Todd-Brown, K.; Thomas, L.; Ferreira, M.A.R.; Bender, D.; Maller, J.; Sklar, P.; de Bakker, P.I.W.; Daly, M.J.; et al. PLINK: A Tool Set for Whole-Genome Association and Population-Based Linkage Analyses. Am. J. Hum. Genet. 2007, 81, 559–575. [Google Scholar] [CrossRef]
- Calle, M.L.; Urrea, V.; Malats, N.; Van Steen, K. Mbmdr: An R package for exploring gene-gene interactions associated with binary or quantitative traits. Bioinformatics 2010, 26, 2198–2199. [Google Scholar] [CrossRef] [PubMed]
- Ponomarenko, I.V. Using the method of Multifactor Dimensionality Reduction (MDR) and its modifications for analysis of gene-gene and gene-environment interactions in genetic-epidemiological studies (review). Res. Results Biomed. 2019, 5, 4–21. [Google Scholar] [CrossRef]
- Sourceforge. Available online: http://sourceforge.net/projects/mdr (accessed on 22 November 2022).
- Pavlova, N.; Demin, S.; Churnosov, M.; Reshetnikov, E.; Aristova, I.; Churnosova, M.; Ponomarenko, I. Matrix Metalloproteinase Gene Polymorphisms Are Associated with Breast Cancer in the Caucasian Women of Russia. Int. J. Mol. Sci. 2022, 23, 12638. [Google Scholar] [CrossRef]
- Reshetnikov, E.; Ponomarenko, I.; Golovchenko, O.; Sorokina, I.; Batlutskaya, I.; Yakunchenko, T.; Dvornyk, V.; Polonikov, A.; Churnosov, M. The VNTR polymorphism of the endothelial nitric oxide synthase gene and blood pressure in women at the end of pregnancy. Taiwan J. Obstet. Gynecol. 2019, 58, 390–395. [Google Scholar] [CrossRef]
- Minyaylo, O.; Ponomarenko, I.; Reshetnikov, E.; Dvornyk, V.; Churnosov, M. Functionally significant polymorphisms of the MMP-9 gene are associated with peptic ulcer disease in the Caucasian population of Central Russia. Sci. Rep. 2021, 11, 13515. [Google Scholar] [CrossRef]
- Che, R.; Jack, J.R.; Motsinger-Reif, A.A.; Brown, C.C. An adaptive permutation approach for genome-wide association study: Evaluation and recommendations for use. BioData Min. 2014, 7, 9. [Google Scholar] [CrossRef]
- Adzhubei, I.; Jordan, D.M.; Sunyaev, S.R. Predicting functional effect of human missense mutations using PolyPhen-2. Curr. Protoc. Hum. Genet. 2013, 76, 7–20. [Google Scholar] [CrossRef]
- Kumar, P.; Henikoff, S.; Ng, P.C. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat. Protoc. 2009, 7, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Westra, H.J.; Peters, M.J.; Esko, T.; Yaghootkar, H.; Schurmann, C.; Kettunen, J.; Christiansen, M.W.; Fairfax, B.P.; Schramm, K.; Powell, J.E.; et al. Systematic identification of trans eQTLs as putative drivers of known disease associations. Nat. Genet. 2013, 45, 1238–1243. [Google Scholar] [CrossRef] [PubMed]
- GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science 2020, 369, 1318–1330. [Google Scholar] [CrossRef] [PubMed]
- Gene Ontology Consortium. The Gene Ontology resource: Enriching a GOld mine. Nucleic Acids Res. 2021, 49, D325–D334. [Google Scholar] [CrossRef] [PubMed]
- Franz, M.; Rodriguez, H.; Lopes, C.; Zuberi, K.; Montojo, J.; Bader, G.D.; Morris, Q. GeneMANIA update 2018. Nucleic Acids Res. 2018, 46, W60–W64. [Google Scholar] [CrossRef] [PubMed]
- Szklarczyk, D.; Kirsch, R.; Koutrouli, M.; Nastou, K.; Mehryary, F.; Hachilif, R.; Gable, A.L.; Fang, T.; Doncheva, N.T.; Pyysalo, S.; et al. The STRING database in 2023: Protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 2023, 51, D638–D646. [Google Scholar] [CrossRef]
- Ponomarenko, I.; Reshetnikov, E.; Polonikov, A.; Verzilina, I.; Sorokina, I.; Yermachenko, A.; Dvornyk, V.; Churnosov, M. Candidate genes for age at menarche are associated with uterine leiomyoma. Front. Genet. 2021, 11, 512940. [Google Scholar] [CrossRef]
- Golovchenko, I.; Aizikovich, B.; Golovchenko, O.; Reshetnikov, E.; Churnosova, M.; Aristova, I.; Ponomarenko, I.; Churnosov, M. Sex Hormone Candidate Gene Polymorphisms Are Associated with Endometriosis. Int. J. Mol. Sci. 2022, 23, 13691. [Google Scholar] [CrossRef]
- Ponomarenko, I.; Reshetnikov, E.; Polonikov, A.; Sorokina, I.; Yermachenko, A.; Dvornyk, V.; Churnosov, M. Candidate genes for age at menarche are associated with endometrial hyperplasia. Gene 2020, 757, 4933. [Google Scholar] [CrossRef]
- Novakov, V.; Novakova, O.; Churnosova, M.; Sorokina, I.; Aristova, I.; Polonikov, A.; Reshetnikov, E.; Churnosov, M. Intergenic Interactions of SBNO1, NFAT5 and GLT8D1 Determine the Susceptibility to Knee Osteoarthritis among Europeans of Russia. Life 2023, 13, 405. [Google Scholar] [CrossRef]
- Feitosa, M.F.; Kraja, A.T.; Chasman, D.I.; Sung, Y.J.; Winkler, T.W.; Ntalla, I.; Guo, X.; Franceschini, N.; Heng, C.K.; Sim, X.; et al. Novel genetic associations for blood pressure identified via gene-alcohol interaction in up to 570K individuals across multipleancestries. PLoS ONE 2018, 13, e0198166. [Google Scholar] [CrossRef]
- German, C.A.; Sinsheimer, J.S.; Klimentidis, Y.C.; Zhou, H.; Zhou, J.J. Ordered multinomial regression for genetic association analysis of ordinal phenotypes at Biobank scale. Genet. Epidemiol. 2019, 44, 248–260. [Google Scholar] [CrossRef]
- Giri, A.; Hellwege, J.N.; Keaton, J.M.; Park, J.; Qiu, C.X.; Warren, H.R.; Torstenson, E.S.; Kovesdy, C.P.; Sun, Y.V.; Wilson, O.D.; et al. Trans-ethnic association study of blood pressure determinants in over 750,000 individuals. Nat. Genet. 2019, 51, 51–62. [Google Scholar] [CrossRef]
- Hartiala, J.A.; Han, Y.; Jia, Q.; Hilser, J.R.; Huang, P.; Gukasyan, J.; Schwartzman, W.S.; Cai, Z.; Biswas, S.; Trégouët, D.A.; et al. Genome-wide analysis identifies novel susceptibility loci for myocardial infarction. Eur. Heart J. 2021, 42, 919–933. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.; Jin, H.-S.; Kim, S.-S.; Shin, D. Identifying Interactions between Dietary Sodium, Potassium, Sodium–Potassium Ratios, and FGF5 rs16998073 Variants and Their Associated Risk for Hypertension in Korean Adults. Nutrients 2020, 12, 2121. [Google Scholar] [CrossRef] [PubMed]
- Kato, N.; Loh, M.; Takeuchi, F.; Verweij, N.; Wang, X.; Zhang, W.; Kelly, T.N.; Saleheen, D.; Lehne, B.; Leach, I.M.; et al. Trans-ancestry genome-wide association study identifies 12 genetic loci influencing blood pressure and implicates a role for DNA methylation. Nat. Genet. 2015, 47, 1282–1293. [Google Scholar] [CrossRef] [PubMed]
- Koyama, S.; Ito, K.; Terao, C.; Akiyama, M.; Horikoshi, M.; Momozawa, Y.; Matsunaga, H.; Ieki, H.; Ozaki, K.; Onouchi, Y.; et al. Population-specific and trans-ancestry genome-wide analyses identify distinct and shared genetic risk loci for coronary artery disease. Nat. Genet. 2020, 52, 1169–1177. [Google Scholar] [CrossRef]
- Levy, D.; Ehret, G.B.; Rice, K.; Verwoert, G.C.; Launer, L.J.; Dehghan, A.; Glazer, N.L.; Morrison, A.C.; Johnson, A.D.; Aspelund, T.; et al. Genome-wide association study of blood pressure and hypertension. Nat. Genet. 2009, 41, 677–687. [Google Scholar] [CrossRef]
- Nelson, C.P.; Goel, A.; Butterworth, A.S.; Kanoni, S.; Webb, T.R.; Marouli, E.; Zeng, L.; Ntalla, I.; Lai, F.Y.; Hopewell, J.C.; et al. Association analyses based on false discovery rate implicate new loci for coronary artery disease. Nat. Genet. 2017, 49, 1385–1391. [Google Scholar] [CrossRef]
- Nikpay, M.; Goel, A.; Won, H.H.; Hall, L.M.; Willenborg, C.; Kanoni, S.; Saleheen, D.; Kyriakou, T.; Nelson, C.P.; Hopewell, J.C.; et al. A comprehensive 1000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat. Genet. 2015, 47, 1121–1130. [Google Scholar] [CrossRef]
- Sakaue, S.; Kanai, M.; Tanigawa, Y.; Karjalainen, J.; Kurki, M.; Koshiba, S.; Narita, A.; Konuma, T.; Yamamoto, K.; Akiyama, M.; et al. A cross-population atlas of genetic associations for 220 human phenotypes. Nat. Genet. 2021, 53, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- Shungin, D.; Winkler, T.W.; Croteau-Chonka, D.C.; Ferreira, T.; Locke, A.E.; Mägi, R.; Strawbridge, R.J.; Pers, T.H.; Fischer, K.; Justice, A.E.; et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature 2015, 518, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Tachmazidou, I.; Süveges, D.; Min, J.L.; Ritchie, G.R.S.; Steinberg, J.; Walter, K.; Iotchkova, V.; Schwartzentruber, J.; Huang, J.; Memari, Y.; et al. Whole-Genome Sequencing Coupled to Imputation Discovers Genetic Signals for Anthropometric Traits. Am. J. Hum. Genet. 2017, 100, 865–884. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, F.; Akiyama, M.; Matoba, N.; Katsuya, T.; Nakatochi, M.; Tabara, Y.; Narita, A.; Saw, W.Y.; Moon, S.; Spracklen, C.N.; et al. Interethnic analyses of blood pressure loci in populations of East Asian and European descent. Nat. Commun. 2018, 9, 5052. [Google Scholar] [CrossRef]
- Wain, L.V.; Verwoert, G.C.; O’Reilly, P.F.; Shi, G.; Johnson, T.; Johnson, A.D.; Bochud, M.; Rice, K.M.; Henneman, P.; Smith, A.V.; et al. Genome-wide association study identifies six new loci influencing pulse pressure and mean arterial pressure. Nat. Genet. 2011, 43, 1005–1011. [Google Scholar] [CrossRef]
- Zhou, W.; Nielsen, J.B.; Fritsche, L.G.; Dey, R.; Gabrielsen, M.E.; Wolford, B.N.; LeFaive, J.; VandeHaar, P.; Gagliano, S.A.; Gifford, A.; et al. Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat. Genet. 2018, 50, 1335–1341. [Google Scholar] [CrossRef]
- Zhu, Z.; Wang, X.; Li, X.; Lin, Y.; Shen, S.; Liu, C.L.; Hobbs, B.D.; Hasegawa, K.; Liang, L.; International COPD Genetics Consortium; et al. Genetic overlap of chronic obstructive pulmonary disease and cardiovascular disease-related traits: A large-scale genome-wide cross-trait analysis. Respir. Res. 2019, 20, 64. [Google Scholar] [CrossRef]

| Gene (SNP, Major/Minor Alleles) | n | Allelic Model | Additive Model | Dominant Model | Recessive Model | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||||||
| L95 | U95 | L95 | U95 | L95 | U95 | L95 | U95 | ||||||||||
| Model 1 | |||||||||||||||||
| AC026703.1 (rs1173771,G/A) | 1317 | 0.90 | 0.77 | 1.06 | 0.216 | 0.89 | 0.69 | 1.14 | 0.354 | 0.75 | 0.51 | 1.10 | 0.140 | 1.03 | 0.65 | 1.62 | 0.905 |
| HFE (rs1799945,C/G) | 1373 | 0.94 | 0.77 | 1.15 | 0.550 | 1.04 | 0.78 | 1.40 | 0.781 | 0.90 | 0.63 | 1.28 | 0.559 | 2.53 | 1.03 | 6.23 | 0.043 |
| BAG6 (rs805303,G/A) | 1349 | 0.97 | 0.82 | 1.14 | 0.683 | 0.87 | 0.68 | 1.11 | 0.264 | 0.95 | 0.67 | 1.34 | 0.750 | 0.65 | 0.40 | 1.04 | 0.075 |
| PLCE1 (rs932764,A/G) | 1319 | 0.87 | 0.74 | 1.02 | 0.094 | 0.81 | 0.63 | 1.04 | 0.096 | 0.65 | 0.43 | 1.02 | 0.056 | 0.88 | 0.58 | 1.32 | 0.525 |
| OBFC1 (rs4387287,C/A) | 1260 | 0.90 | 0.67 | 1.22 | 0.550 | 0.90 | 0.65 | 1.25 | 0.542 | 0.90 | 0.61 | 1.33 | 0.605 | 0.79 | 0.31 | 1.99 | 0.611 |
| ARHGAP42 (rs633185,C/G) | 1377 | 1.02 | 0.85 | 1.22 | 0.813 | 1.09 | 0.84 | 1.42 | 0.525 | 1.08 | 0.76 | 1.52 | 0.673 | 1.25 | 0.68 | 2.32 | 0.472 |
| CERS5 (rs7302981,G/A) | 1302 | 1.03 | 0.87 | 1.22 | 0.711 | 0.94 | 0.73 | 1.21 | 0.615 | 1.03 | 0.71 | 1.48 | 0.882 | 0.76 | 0.47 | 1.22 | 0.249 |
| ATP2B1 (rs2681472,A/G) | 1329 | 1.04 | 0.82 | 1.31 | 0.762 | 1.17 | 0.82 | 1.67 | 0.384 | 1.17 | 0.79 | 1.74 | 0.437 | 1.51 | 0.41 | 5.50 | 0.532 |
| TBX2 (rs8068318,T/C) | 1292 | 1.10 | 0.92 | 1.33 | 0.297 | 1.14 | 0.86 | 1.52 | 0.356 | 1.17 | 0.82 | 1.66 | 0.398 | 1.25 | 0.61 | 2.55 | 0.541 |
| RGL3 (rs167479,T/G) | 1333 | 0.93 | 0.79 | 1.09 | 0.367 | 0.82 | 0.64 | 1.05 | 0.110 | 0.86 | 0.57 | 1.29 | 0.460 | 0.69 | 0.47 | 1.02 | 0.061 |
| Model 2 | |||||||||||||||||
| AC026703.1 (rs1173771,G/A) | 0.89 | 0.69 | 1.15 | 0.374 | 0.76 | 0.51 | 1.11 | 0.153 | 1.03 | 0.65 | 1.64 | 0.893 | |||||
| HFE (rs1799945,C/G) | 1.01 | 0.75 | 1.36 | 0.946 | 0.87 | 0.61 | 1.25 | 0.465 | 2.48 | 1.02 | 6.07 | 0.045 | |||||
| BAG6 (rs805303,G/A) | 0.89 | 0.69 | 1.14 | 0.343 | 0.98 | 0.69 | 1.39 | 0.906 | 0.65 | 0.40 | 1.06 | 0.085 | |||||
| PLCE1 (rs932764,A/G) | 0.81 | 0.63 | 1.04 | 0.093 | 0.64 | 0.42 | 1.02 | 0.054 | 0.88 | 0.58 | 1.33 | 0.535 | |||||
| OBFC1 (rs4387287,C/A) | 0.88 | 0.63 | 1.22 | 0.448 | 0.87 | 0.59 | 1.29 | 0.490 | 0.78 | 0.30 | 2.01 | 0.608 | |||||
| ARHGAP42 (rs633185,C/G) | 1.11 | 0.85 | 1.44 | 0.455 | 1.01 | 0.78 | 1.56 | 0.592 | 1.28 | 0.69 | 2.36 | 0.441 | |||||
| CERS5 (rs7302981,G/A) | 0.93 | 0.72 | 1.21 | 0.600 | 1.01 | 0.70 | 1.46 | 0.948 | 0.76 | 0.47 | 1.24 | 0.275 | |||||
| ATP2B1 (rs2681472,A/G) | 1.15 | 0.80 | 1.66 | 0.451 | 1.17 | 0.78 | 1.76 | 0.448 | 1.20 | 0.32 | 4.52 | 0.792 | |||||
| TBX2 (rs8068318,T/C) | 1.15 | 0.86 | 1.54 | 0.348 | 1.17 | 0.84 | 1.72 | 0.324 | 1.14 | 0.55 | 2.36 | 0.716 | |||||
| RGL3 (rs167479,T/G) | 0.80 | 0.63 | 1.03 | 0.078 | 0.81 | 0.54 | 1.22 | 0.320 | 0.68 | 0.46 | 1.01 | 0.057 | |||||
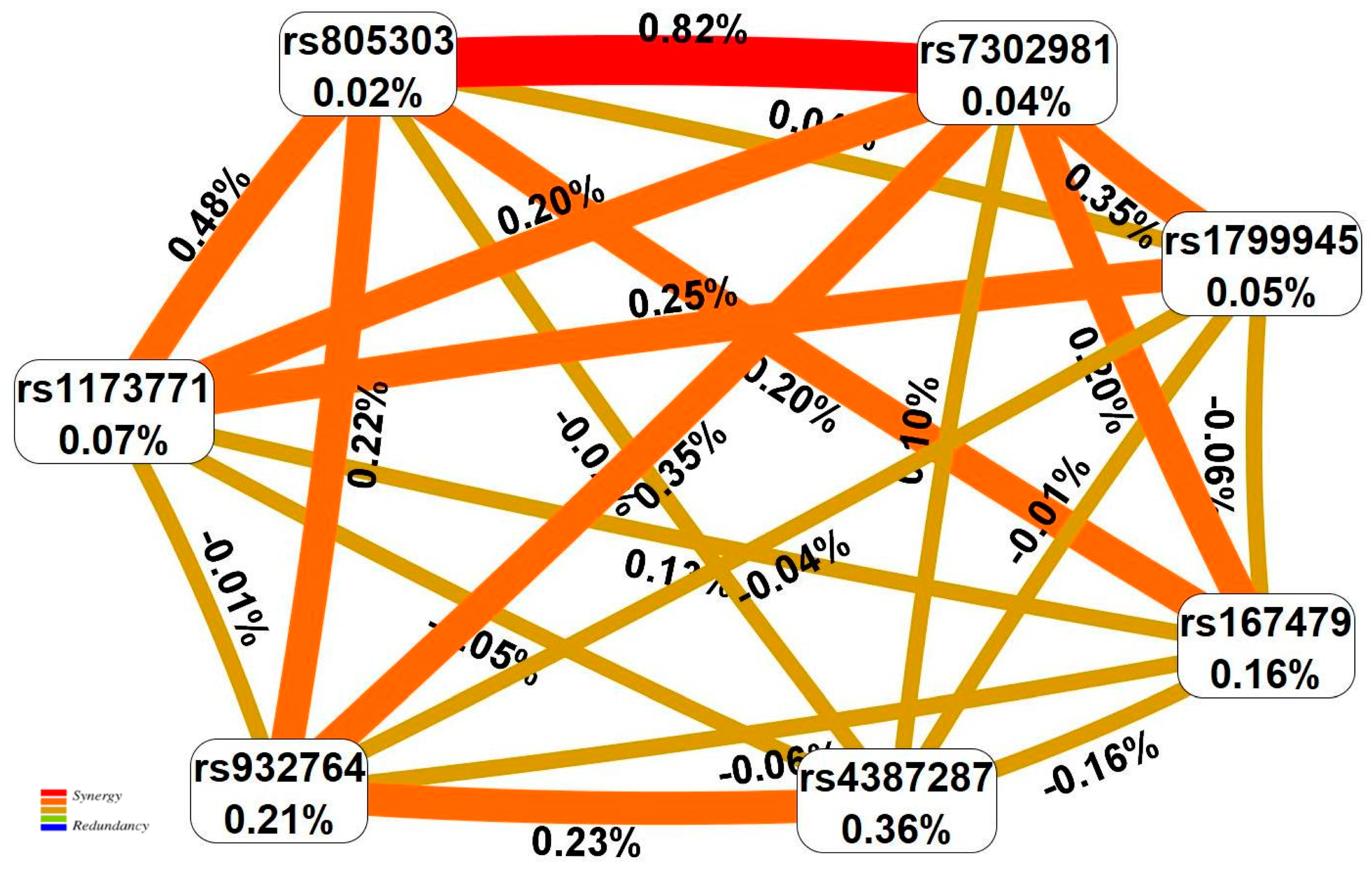
| N | SNP × SNP Interaction Models | NH | betaH | WH | NL | betaL | WL | pperm |
|---|---|---|---|---|---|---|---|---|
| Two-order interaction models | ||||||||
| 1 | rs7302981 CERS5 × rs805303 BAG6 | 2 | 0.372 | 8.02 | 3 | −0.433 | 9.26 | 0.037 |
| 2 | rs805303 BAG6 × rs1173771 AC026703.1 | 1 | 1.318 | 7.99 | 2 | −0.498 | 9.44 | 0.047 |
| Three-order interaction models | ||||||||
| 1 | rs932764 PLCE1 × rs7302981 CERS5 × rs805303 BAG6 | 1 | 0.766 | 3.74 | 2 | −0.799 | 22.25 | 0.001 |
| 2 | rs932764 PLCE1 × rs805303 BAG6 × rs4387287 OBFC1 | 2 | 0.861 | 14.33 | 5 | −0.668 | 20.70 | 0.006 |
| 3 | rs7302981 CERS5 × rs805303 BAG6 × rs1173771 AC026703.1 | 3 | 0.575 | 11.10 | 3 | −1.085 | 20.18 | 0.006 |
| Four-order interaction models | ||||||||
| 1 | rs7302981 CERS5 × rs805303 BAG6 × rs1173771 AC026703.1 × rs167479 RGL3 | 1 | 0.659 | 6.64 | 10 | −1.089 | 47.36 | <0.001 |
| 2 | rs7302981 CERS5 × rs1799945 HFE × rs805303 BAG6 × rs167479 RGL3 | 2 | 0.682 | 10.03 | 9 | −1.085 | 43.66 | <0.001 |
| 3 | rs932764 PLCE1 × rs7302981 CERS5 × rs805303 BAG6 × rs167479 RGL3 | 3 | 0.895 | 11.66 | 6 | −1.081 | 38.10 | 0.001 |
| Parameters | AH, Mean ± SD, % (n) | Controls, Mean ± SD, % (n) | p |
|---|---|---|---|
| N | 939 | 466 | |
| Gender (Male/ Female) | 60.06/39.94 (564/375) | 55.15/44.85 (257/209) | 0.09 |
| Age (years) | 58.08 ± 8.91 | 57.82 ± 9.52 | 0.77 |
| BMI (kg/m2) | 30.78 ± 5.08 | 24.94 ± 3.14 | <0.001 |
| SBP (mmHg) | 182.48 ± 28.26 | 122.58 ± 11.49 | <0.001 |
| DBP (mmHg) | 105.84 ± 13.47 | 77.65 ± 6.93 | <0.001 |
| TC (mM) | 5.71 ± 1.29 | 5.26 ± 1.04 | <0.001 |
| HDL-C (mM) | 1.34 ± 0.42 | 1.52 ± 0.42 | <0.001 |
| LDL-C (mM) | 3.78 ± 1.11 | 3.22 ± 0.74 | <0.001 |
| TG (mM) | 1.92 ± 1.03 | 1.22 ± 0.71 | <0.001 |
| BG (mM) | 5.92 ± 1.68 | 4.88 ± 0.95 | <0.001 |
| Smoking | 38.33 (353) | 19.76 (84) | <0.001 |
| Alcohol abuse | 5.79 (53) | 3.12 (13) | 0.051 |
| Low physical activity | 58.68 (551) | 27.47 (128) | <0.001 |
| Low fruit/vegetable consumption | 11.39 (107) | 8.15 (38) | 0.074 |
| High fatty foods consumption | 24.71 (232) | 10.30 (48) | <0.001 |
| High sodium consumption | 16.72 (157) | 13.30 (62) | 0.113 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanova, T.; Churnosova, M.; Abramova, M.; Ponomarenko, I.; Reshetnikov, E.; Aristova, I.; Sorokina, I.; Churnosov, M. Risk Effects of rs1799945 Polymorphism of the HFE Gene and Intergenic Interactions of GWAS-Significant Loci for Arterial Hypertension in the Caucasian Population of Central Russia. Int. J. Mol. Sci. 2023, 24, 8309. https://doi.org/10.3390/ijms24098309
Ivanova T, Churnosova M, Abramova M, Ponomarenko I, Reshetnikov E, Aristova I, Sorokina I, Churnosov M. Risk Effects of rs1799945 Polymorphism of the HFE Gene and Intergenic Interactions of GWAS-Significant Loci for Arterial Hypertension in the Caucasian Population of Central Russia. International Journal of Molecular Sciences. 2023; 24(9):8309. https://doi.org/10.3390/ijms24098309
Chicago/Turabian StyleIvanova, Tatiana, Maria Churnosova, Maria Abramova, Irina Ponomarenko, Evgeny Reshetnikov, Inna Aristova, Inna Sorokina, and Mikhail Churnosov. 2023. "Risk Effects of rs1799945 Polymorphism of the HFE Gene and Intergenic Interactions of GWAS-Significant Loci for Arterial Hypertension in the Caucasian Population of Central Russia" International Journal of Molecular Sciences 24, no. 9: 8309. https://doi.org/10.3390/ijms24098309
APA StyleIvanova, T., Churnosova, M., Abramova, M., Ponomarenko, I., Reshetnikov, E., Aristova, I., Sorokina, I., & Churnosov, M. (2023). Risk Effects of rs1799945 Polymorphism of the HFE Gene and Intergenic Interactions of GWAS-Significant Loci for Arterial Hypertension in the Caucasian Population of Central Russia. International Journal of Molecular Sciences, 24(9), 8309. https://doi.org/10.3390/ijms24098309







