Current Levels of Environmental Exposure to Cadmium in Industrialized Countries as a Risk Factor for Kidney Damage in the General Population: A Comprehensive Review of Available Data
Abstract
1. Introduction
2. The Kidney as One of the Most Important Organs in the Body
3. Main Causes of Kidney Dysfunction in the General Population
4. The Current Cd Exposure Level in Industrialized Countries
| Country | n | Expression of Cd Concentration | Cd in the Blood (μg/L) | Cd in the Urine (μg/L) (μg/g Creatinine) b | Reference | ||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | ||||
| Argentina | 172 | Median (range) | 0.36 (0.17–1.00) | 0.24 (0.01–1.5) | [95] | ||
| Bangladesh | 72 | Median (range) | 0.22 (0.01–1.5) | ||||
| Canada | 10,099 | GM (SE) | 0.35 (0.01) | 0.45 (0.01) † | [73] | ||
| 7082 | GM (SE) | 0.34 (0.01) | 0.43 (0.02) * | 0.35 (0.01) | 0.53 (0.01) * | [71] | |
| China | 896 | Median (P25–P75) | 1.34 (0.38–2.88) | 0.49 (0.31–0.65) NP | 0.38 (0.21–0.65) | 0.42 (0.23–0.70) NP | [84] |
| 78 | Median (P25–P75) | 1.44 (0.87–2.33) | 2.20 (1.42–3.00) | [96] | |||
| Ireland | 100 | Median (P25–P75) | 0.3 (0.2–0.6) | 0.4 (0.2–0.9) | [97] | ||
| South Korea | 12,099 | GM (95% Cl) | 0.76 (0.74–0.77) | 1.01 (0.99–1.03) NP | [58] | ||
| 643 | GM (GSD) | 1.10 (1.77) | 1.29 (1.78) * | 0.82 (2.04) | 1.04 (2.29) * | [29] | |
| 1907 | GM (P95) | 0.82 (2.34) | 1.36 (3.39) † | [37] | |||
| 3781 | Median (P25–P75) | 0.42 (0.19–0.77) | 0.43 (0.18–0.87) | [98] | |||
| Sweden | 109 | Mean (range) | 0.46 (0.02–2.3) | 0.54 (0.02–2.9) NP | 0.23 (0.04–0.80) | 0.34 (0.09–1.12) NP | [30] |
| Thailand | 392 | GM (SD) | 0.28 (0.84) | 0.23 (0.49) NS | [99] | ||
| 81 | GM (GSD) | 0.9 (2.2) | 0.5 (1.9) | 1.1 (2.3) NP | [100] | ||
| Turkey | 30 | Median (min–max) | 0.34 (0.11–0.84) | 0.42 (0.08–0.98) | [101] | ||
| USA | 3226 | GM (SE) | 0.49 (0.02) | [102] | |||
| 9662 | Mean ± SD | 0.52 ± 0.58 | 0.40 ± 0.47 | [103] | |||
| Denmark | 282 | GM (95% Cl) | 0.123 (0.112–0.350) | [104] | |||
| Iceland | 203 | GM (95% Cl) | 0.135 (0.119–0.153) | ||||
| Czech Republic | 300 | GM (95% Cl) | 0.132 (0.122–0.142) | ||||
| Poland | 228 | GM (95% Cl) | 0.408 (0.369–0.450) | ||||
| Croatia | 300 | GM (95% Cl) | 0.175 (0.160–0.192) | ||||
| Portugal | 295 | GM (95% Cl) | 0.109 (0.098–0.120) | ||||
| France | 393 | GM (95% Cl) | 0.365 (0.340–0.391) | ||||
| Luxembourg | 210 | GM (95% Cl) | 0.316 (0.288–0.347) | ||||
| Germany | 289 | GM (95% Cl) | 0.199 (0.186–0.213) | ||||
| China | 50 | GM (range) | 0.99 (0.23–2.6) | [105] | |||
| Croatia | 59 | GM (range) | 0.56 (0.15–4.4) | ||||
| Czech Republic | 50 | GM (range) | 0.41 (0.11–2.1) | ||||
| Ecuador | 25 | GM (range) | 0.61 (0.25–2.1) | ||||
| Morocco | 49 | GM (range) | 0.39 (0.15–1.8) | ||||
| Slovakia | 52 | GM (range) | 0.40 (0.17–2.1) | ||||
| Slovenia | 50 | GM (range) | 0.49 (0.21–2.2) | ||||
| Sweden (north) | 35 | GM (range) | 0.25 (0.08–1.8) | ||||
| Sweden (south) | 55 | GM (range) | 0.35 (0.11–2.6) | ||||
5. Kidneys as the Main Organ of Cd Accumulation in the Body
6. Cd as a Nephrotoxic Factor
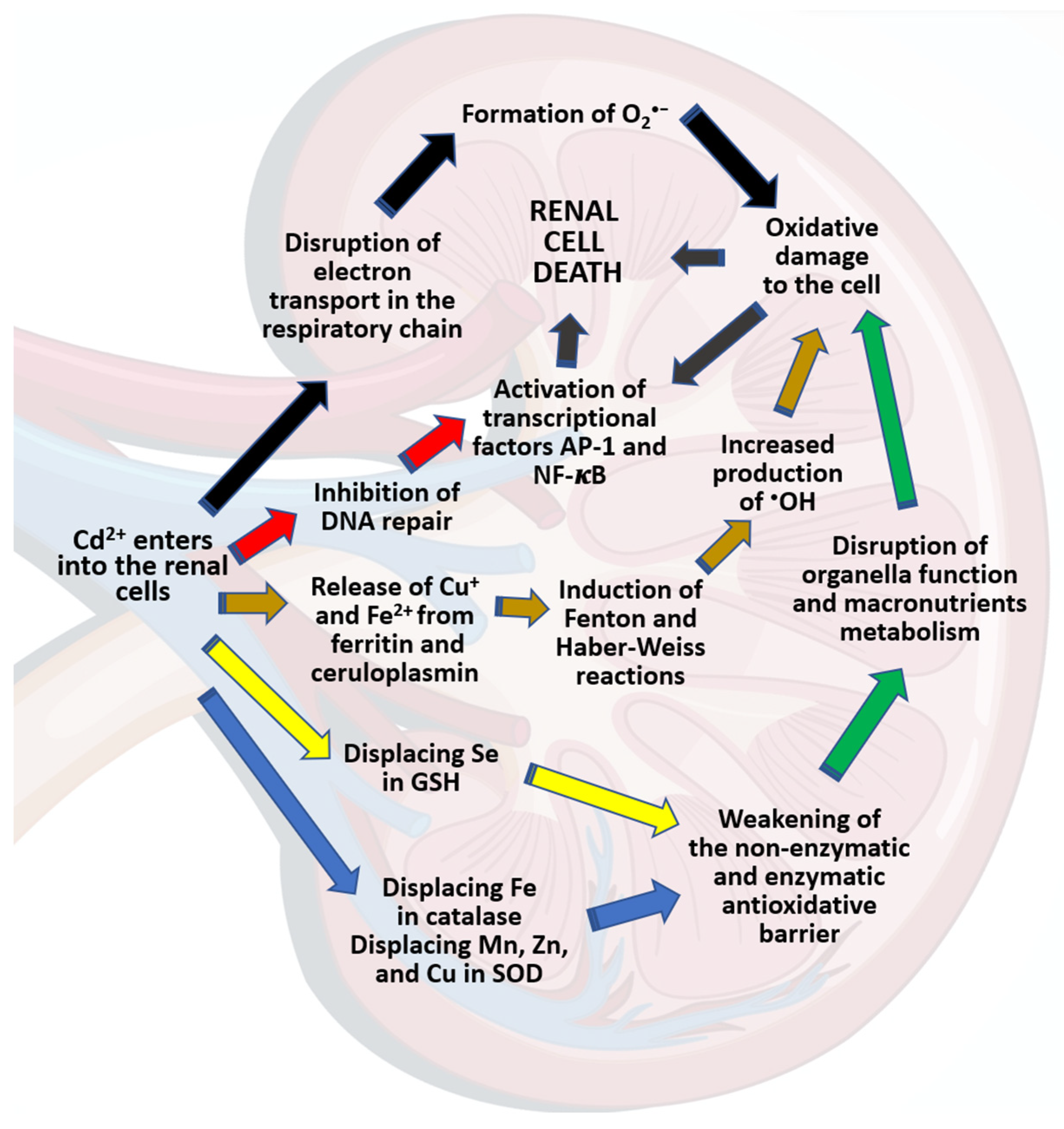
7. Mechanism of Cd Nephrotoxicity
8. Biomarkers of Cd-Induced Kidney Damage
9. Risk of Kidney Damage among the General Population at Current Environmental Cd Exposure Levels
| Expression of Data | Cd Concentration in the Urine (μg/g Creatinine) | Biomarkers of Tubular Damage | Biomarkers of Glomerular Damage | Reference | |||
|---|---|---|---|---|---|---|---|
| α1-MG (mg/g Creatinine) | β2-MG (μg/g Creatinine) | NAG (U/g Creatinine) | Albumin (mg/L) (mg/g Creatinine) b | eGFR (mL/min/1.73 m2) | |||
| Median (P25, P75) | M: 0.38 (0.21–0.65) F: 0.42 (0.23–0.70) | M: 370 (0.00, 3135) F: 280 (0.00, 2090) | M:10.31 (1.46, 199.09) F: 10.09 (2.16, 48.63) | M: 84.89 (19.30, 204.34) F: 78.56 (19.32, 239.60) | [84] | ||
| Median (P5–P95) | 2.1 (0.3–5.2) | 140 (40–1500) | 2.50 (0.09–15.0) | 2.6 (0.5–26.3) | [45] | ||
| GM (95% CI) | M: 0.82 (0.79, 0.86) F: 1.36 (1.31, 1.41) | M: 80.47 (72.22, 88.72) F: 79.86 (74.29, 85.43) | M: 4.17 (3.74, 4.59) F: 4.14 (3.74, 4.54) | M: 91.88 (90.63, 93.13) F: 97.89 (96.79, 98.99) | [37] | ||
| Median (IQR) | 0.41 (0.195–1.26) | 99.8 (71.0–186.80) | 109.52 ± 17.43 c | [155] | |||
| Mean (range) | 0.29 (0.04–1.12) | 5.1 (2.0–15.2) | 150 (10–1300) | 1.95 (0.18–4.88) | 4.8 (0.69–23.6) | 101 (77–140) 91 (43–178) | [30] |
| Median (GM) | 2.20 (2.10) | 1.30 (1.13) | 6.95 (6.13) | 1.40 (1.42) | [96] | ||
| Median (P5–P95) | <2.05 ≥2.05–<3.97 | 3.82 (0.00–17.27) 4.89 (0.00–19.42) | 60 (0.00–5000) 90 (0.00–1760) | 6.51 (2.93–62.83) 10.28 (3.69–82.69) | 2.84 (0.00–32.37) | 66.0 ± 11.3 | [164] |
| Median (min–max) | 0.19 (0.01–2.79) | 4.13 (0.47–60.1) | 6.87 (3.50–11.9) | [127] | |||
| Mean (range) | 0.11 (0.01–0.52) | 2.0 (0.11–31) | 6.3 (1.1–78) | [166] | |||
| Mean | <1.0 1.0–1.9 2.0–4.9 | 84.65 140.89 115.74 | 2.12 2.82 2.90 | [29] | |||
| GM (GSD) | M: 0.5 (1.9) F: 1.1 (2.3) | M: 249.6 (4.0) F: 187.2 (6.6) | M: 5.2 (2.1) F: 4.8 (2.3) | [100] | |||
| Mean (SD) | 1.08 (1.98) | 51.4 (2.64) | 4.01 (2.78) | [131] | |||
| Median (P25–P75) | 2.25 (1.20–5.10) d | 0.31 (0.07–6.49) | 110 (70–2800) | 5.10 (3.30–7.25) | 2.86 (0.46–7.03) | [81] | |

10. Exposure to Cd as a Factor Increasing the Risk of Kidney Damage Due to Other Causes
11. Conclusions and Outlook
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Kabir, H.; Gupta, A.K.; Tripathy, S. Fluoride and human health: Systematic appraisal of sources, exposures, metabolism, and toxicity. Crit. Rev. Environ. Sci. Technol. 2020, 50, 1116–1193. [Google Scholar] [CrossRef]
- Nordberg, G.F.; Bernard, A.; Diamond, G.L.; Duffus, J.H.; Illing, P.; Nordberg, M.; Bergdahl, I.A.; Jin, T.; Skerfving, S. Risk assessment of effects of cadmium on human health (IUPAC Technical Report). Pure Appl. Chem. 2018, 90, 755–808. [Google Scholar] [CrossRef]
- Rahman, H.H.; Niemann, D.; Munson-McGee, S.H. Environmental exposure to metals and the risk of high blood pressure: A cross-sectional study from NHANES 2015–2016. Environ. Sci. Pollut. Res. 2021, 29, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhu, G.; Wang, Z.; Zhou, H.; He, P.; Liu, Y.; Jin, T. The association between lead and cadmium co-exposure and renal dysfunction. Ecotoxicol. Environ. Saf. 2019, 173, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.B. Co-exposures to toxic metals cadmium, lead, and mercury and their impact on unhealthy kidney function. Environ. Sci. Pollut. Res. 2019, 26, 30112–30118. [Google Scholar] [CrossRef]
- Tsai, T.L.; Kuo, C.C.; Pan, W.H.; Chung, Y.T.; Chen, C.Y.; Wu, T.N.; Wang, S.L. The decline in kidney function with chromium exposure is exacerbated with co-exposure to lead and cadmium. Kidney Int. 2017, 92, 710–720. [Google Scholar] [CrossRef]
- Wu, W.; Zhang, K.; Jiang, S.; Liu, D.; Zhou, H.; Zhong, R.; Zeng, Q.; Cheng, L.; Miao, X.; Tong, Y.; et al. Association of co-exposure to heavy metals with renal function in a hypertensive population. Environ. Int. 2018, 112, 198–206. [Google Scholar] [CrossRef]
- Agency for Toxic Substances and Disease Registry. Substance Priority List. 2022. Available online: https://www.atsdr.cdc.gov/spl/index.html (accessed on 13 March 2023).
- Zhang, H.; Reynolds, M. Cadmium exposure in living organisms: A short review. Sci. Total Environ. 2019, 678, 761–767. [Google Scholar] [CrossRef]
- Zou, M.; Zhou, S.; Zhou, Y.; Jia, Z.; Guo, T.; Wang, J. Cadmium pollution of soil-rice ecosystems in rice cultivation dominated regions in China: A review. Environ. Pollut. 2021, 280, 116965. [Google Scholar] [CrossRef]
- Jung, C.R.; Nakayama, S.F.; Isobe, T.; Iwai-Shimada, M.; Kobayashi, Y.; Nishihama, Y.; Michikawa, T.; Sekiyama, M.; Taniguchi, Y.; Nitta, H.; et al. Exposure to heavy metals modifies optimal gestational weight gain: A large nationally representative cohort of the Japan Environment and Children’s Study. Environ. Int. 2021, 146, 106276. [Google Scholar] [CrossRef]
- Mężyńska, M.; Brzóska, M.M. Environmental exposure to cadmium—A risk for health of the general population in industrialized countries and preventive strategies. Environ. Sci. Pollut. Res. 2018, 25, 3211–3232. [Google Scholar] [CrossRef] [PubMed]
- Ruczaj, A.; Brzóska, M.M. Environmental exposure of the general population to cadmium as a risk factor of the damage to the nervous system: A critical review of current data. J. Appl. Toxicol. 2023, 43, 66–88. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Vesey, D.A.; Gobe, G.C. Health risk assessment of dietary cadmium intake: Do current guidelines indicate how much is safe? Environ. Health Perspect. 2017, 125, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, H.R.; Flannery, B.M.; Crosby, L.; Jones-Dominic, O.E.; Punzalan, C.; Middleton, K. A systematic review of adverse health effects associated with oral cadmium exposure. Regul. Toxicol. Pharmacol. 2022, 134, 105243. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Miozzi, E.; Loreto, C.; Matera, S.; Fenga, C.; Avola, R.; Ledda, C. Cadmium exposure and prostate cancer: Insights, mechanisms and perspectives. Front. Biosci. 2018, 23, 1687–1700. [Google Scholar] [CrossRef]
- Brzóska, M.M.; Galazyn-Sidorczuk, M.; Jurczuk, M.; Tomczyk, M. Protective effect of Aronia melanocarpa polyphenols on cadmium accumulation in the body: A study in a rat model of human exposure to this metal. Curr. Drug Targets 2015, 16, 1470–1487. [Google Scholar] [CrossRef]
- Fransson, M.N.; Barregard, L.; Sallsten, G.; Akerstrom, M.; Johanson, G. Physiologically-based toxicokinetic model for cadmium using markov-chain Monte Carlo analysis of concentrations in blood, urine, and kidney cortex from living kidney donors. Toxicol. Sci. 2014, 141, 365–376. [Google Scholar] [CrossRef]
- Hayashi, C.; Koizumi, N.; Nishio, H.; Koizumi, N.; Ikeda, M. Cadmium and other metal levels in autopsy samples from a cadmium-polluted area and non-polluted control areas in Japan. Biol. Trace Elem. Res. 2012, 145, 10–22. [Google Scholar] [CrossRef]
- Boonprasert, K.; Vesey, D.A.; Gobe, G.C.; Ruenweerayut, R.; Johnson, D.W.; Na-Bangchang, K.; Satarug, S. Is renal tubular cadmium toxicity clinically relevant? Clin. Kidney J. 2018, 11, 681–687. [Google Scholar] [CrossRef]
- Lane, E.A.; Canty, M.J.; More, S.J. Cadmium exposure and consequence for the health and productivity of farmed ruminants. Res. Vet. Sci. 2015, 101, 132–139. [Google Scholar] [CrossRef]
- Madrigal, J.M.; Ricardo, A.C.; Persky, V.; Turyk, M. Associations between blood cadmium concentration and kidney function in the U.S. population: Impact of sex, diabetes and hypertension. Environ. Res. 2019, 169, 180–188. [Google Scholar] [CrossRef]
- Nogawa, K.; Suwazono, Y.; Watanabe, Y.; Elinder, C.-G. Estimation of benchmark dose of cumulative cadmium exposure for renal tubular effect. Int. J. Environ. Res. 2021, 18, 5177. [Google Scholar] [CrossRef] [PubMed]
- Rani, A.; Kumar, A.; Lal, A.; Pant, M. Cellular mechanisms of cadmium-induced toxicity: A review. Int. J. Environ. Res. 2014, 24, 378–399. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Swaddiwudhipong, W.; Ruangyuttikarn, W.; Nishijo, M.; Ruiz, P. Modeling cadmium exposures in low- and high-exposure areas in Thailand. Environ. Health Perspect. 2013, 121, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Nawab, J.; Farooqi, S.; Xiaoping, W.; Khan, S.; Khan, A. Levels, dietary intake, and health risk of potentially toxic metals in vegetables, fruits, and cereal crops in Pakistan. Environ. Sci. Pollut. Res. 2018, 25, 5558–5571. [Google Scholar] [CrossRef]
- Satarug, S. Dietary cadmium intake and its effects on kidneys. Toxics 2018, 6, 15. [Google Scholar] [CrossRef]
- Callan, A.C.; Devine, A.; Qi, L.; Ng, J.C.; Hinwood, A.L. Investigation of the relationship between low environmental exposure to metals and bone mineral density, bone resorption and renal function. Int. J. Hyg. Environ. Health 2015, 218, 444–451. [Google Scholar] [CrossRef]
- Huang, M.; Choi, S.J.; Kim, D.W.; Kim, N.Y.; Bae, H.S.; Yu, S.; Kim, D.S.; Kim, H.; Choi, B.S.; Yu, I.J.; et al. Evaluation of factors associated with cadmium exposure and kidney function in the general population. Environ. Toxicol. 2013, 28, 563–570. [Google Scholar] [CrossRef]
- Wallin, M.; Sallsten, G.; Lundh, T.; Barregard, L. Low-level cadmium exposure and effects on kidney function. Occup. Environ. Med. 2014, 71, 848–854. [Google Scholar] [CrossRef]
- Barnett, L.M.A.; Cummings, B.S. Nephrotoxicity and renal pathophysiology: A contemporary perspective. Toxicol. Sci. 2018, 164, 379–390. [Google Scholar] [CrossRef]
- Johri, N.; Jacquillet, G.; Unwin, R. Heavy metal poisoning: The effects of cadmium on the kidney. BioMetals 2010, 23, 783–792. [Google Scholar] [CrossRef]
- Kim, S.Y.; Moon, A. Drug-induced nephrotoxicity and its biomarkers. Biomol. Ther. 2012, 20, 268–272. [Google Scholar] [CrossRef]
- Lv, J.C.; Zhang, L.X. Prevalence and disease burden of chronic kidney disease. Adv. Exp. Med. Biol. 2019, 1165, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Provenzano, M.; Coppolino, G.; Faga, T.; Garofalo, C.; Serra, R.; Andreucci, M. Epidemiology of cardiovascular risk in chronic kidney disease patients: The real silent killer. Rev. Cardiovasc. Med. 2019, 20, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D. Global prevalence of chronic kidney disease–a systematic review and meta-analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef] [PubMed]
- Eom, S.Y.; Seo, M.N.; Lee, Y.S.; Park, K.S.; Hong, Y.S.; Sohn, S.J.; Kim, Y.D.; Choi, B.S.; Lim, J.A.; Kwon, H.J.; et al. Low-level environmental cadmium exposure induces kidney tubule damage in the general population of Korean adults. Arch. Environ. Contam. Toxicol. 2017, 73, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, M.A.; Vaidya, V.S.; Bonventre, J.V. Biomarkers of nephrotoxic acute kidney injury. Toxicology 2018, 245, 182–193. [Google Scholar] [CrossRef]
- Thévenod, F.; Lee, W.K. Cadmium and cellular signaling cascades: Interactions between cell death and survival pathways. Arch. Toxicol. 2013, 87, 1743–1786. [Google Scholar] [CrossRef]
- Cui, X.; Cheng, H.; Liu, X.; Giubilato, E.; Critto, A.; Sun, H.; Zhang, L. Cadmium exposure and early renal effects in the children and adults living in a tungsten-molybdenum mining areas of South China. Environ. Sci. Pollut. Res. 2018, 25, 15089–15101. [Google Scholar] [CrossRef]
- Gerhardsson, L.; Englyst, V.; Lundström, N.G.; Sandberg, S.; Nordberg, G. Cadmium, copper and zinc in tissues of deceased copper smelter workers. J. Trace Elem. Med. Biol. 2002, 16, 261–266. [Google Scholar] [CrossRef]
- Klaassen, C.D.; Liu, J.; Diwan, B.A. Metallothionein protection of cadmium toxicity. Toxicol. Appl. Pharmacol. 2009, 238, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Sabolić, I.; Breljak, D.; Škarica, M.; Herak-Kramberger, C.M. Role of metallothionein in cadmium traffic and toxicity in kidneys and other mammalian organs. BioMetals 2010, 23, 897–926. [Google Scholar] [CrossRef] [PubMed]
- Prozialeck, W.C.; Edwards, J.R. Mechanisms of cadmium-induced proximal tubule injury: New insights with implications for biomonitoring and therapeutic interventions. J. Pharmacol. Exp. Ther. 2012, 343, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhu, G.; Wang, Z.; Liang, Y.; Chen, B.; He, P.; Nordberg, M.; Nordberg, G.F.; Ding, X.; Jin, T. The association between dietary cadmium exposure and renal dysfunction—The benchmark dose estimation of reference levels: The ChinaCad study. J. Appl. Toxicol. 2018, 38, 1365–1373. [Google Scholar] [CrossRef] [PubMed]
- Murabito, S.; Hallmark, B.F. Complications of kidney disease. Nurs. Clin. N. Am. 2018, 53, 579–588. [Google Scholar] [CrossRef]
- Järup, L.; Åkesson, A. Current status of cadmium as an environmental health problem. Toxicol. Appl. Pharmacol. 2009, 238, 201–208. [Google Scholar] [CrossRef]
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.M.; Yang, C.W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2019; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019. Available online: https://www.cdc.gov/kidneydisease/pdf/2019_National-Chronic-Kidney-Disease-Fact-Sheet.pdf (accessed on 13 March 2023).
- Anders, H.J.; Huber, T.B.; Isermann, B.; Schiffer, M. CKD in diabetes: Diabetic kidney disease versus nondiabetic kidney disease. Nat. Rev. Nephrol. 2018, 14, 361–377. [Google Scholar] [CrossRef]
- Hamrahian, S.M.; Falkner, B. Hypertension in chronic kidney disease. Adv. Exp. Med. Biol. 2017, 956, 307–325. [Google Scholar] [CrossRef]
- Matović, V.; Buha, A.; Dukić-Ćosić, D.; Bulat, Z. Insight into the oxidative stress induced by lead and/or cadmium in blood, liver and kidneys. Food Chem. Toxicol. 2015, 78, 130–140. [Google Scholar] [CrossRef]
- Nordberg, G.F. Historical perspectives on cadmium toxicology. Toxicol. Appl. Pharmacol. 2009, 238, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Liu, Y.; Liu, Y.; Liang, B.; Zhou, H.; Li, Y.; Zhang, Y.; Huang, J.; Yu, C.; Chen, K. An assessment of dietary exposure to cadmium in residents of Guangzhou, China. Int. J. Environ. Res. Public Health 2018, 15, 556. [Google Scholar] [CrossRef] [PubMed]
- Huili, Y.; Hezifan, Z.; Shuangnan, H.; Luyao, W.; Wenxiu, X.; Mi, M.; Yongming, L.; Zhenyan, H. Cadmium contamination in food crops: Risk assessment and control in smart age. Crit. Rev. Environ. Sci. Technol. 2023. [Google Scholar] [CrossRef]
- Badea, M.; Luzardo, O.P.; González-Antuña, A.; Zumbado, M.; Rogozea, L.; Floroian, L.; Alexandrescu, D.; Moga, M.; Gaman, L.; Radoi, M.; et al. Body burden of toxic metals and rare earth elements in non-smokers, cigarette smokers, and electronic cigarette users. Environ. Res. 2018, 166, 269–275. [Google Scholar] [CrossRef]
- Hecht, E.M.; Arheart, K.; Lee, D.J.; Hennekens, C.H.; Hlaing, W.W.M. A cross-sectional survey of cadmium biomarkers and cigarette smoking. Biomarkers 2016, 21, 429–435. [Google Scholar] [CrossRef]
- Park, E.; Kim, J.; Kim, B.; Park, E.Y. Association between environmental exposure to cadmium and risk of suspected non-alcoholic fatty liver disease. Chemosphere 2021, 266, 128947. [Google Scholar] [CrossRef]
- Song, Y.; Wang, Y.; Mao, W.; Sui, H.; Yong, L.; Yang, D.; Jiang, D.; Zhang, L.; Gong, Y. Dietary cadmium exposure assessment among the Chinese population. PLoS ONE 2017, 12, e0177978. [Google Scholar] [CrossRef]
- Kim, K.; Melough, M.M.; Vance, T.M.; Noh, H.; Koo, S.I.; Chun, O.K. Dietary cadmium intake and sources in the US. Nutrients 2019, 11, 2. [Google Scholar] [CrossRef]
- Sand, S.; Becker, W. Assessment of dietary cadmium exposure in Sweden and population health concern including scenario analysis. Food Chem. Toxicol. 2012, 50, 536–544. [Google Scholar] [CrossRef]
- Wang, Z.; Pan, L.; Liu, G.; Zhang, H.; Zhang, J.; Jiang, J.; Xiao, Y.; Bai, W.; Jiao, R.; Huang, W. Dietary exposure to cadmium of Shenzhen adult residents from a total diet study. Food Addit. Contam. Part A 2018, 35, 706–714. [Google Scholar] [CrossRef]
- Zhong, M.S.; Jiang, L.; Han, D.; Xia, T.X.; Yao, J.J.; Jia, X.Y.; Peng, C. Cadmium exposure via diet and its implication on the derivation of health-based soil screening values in China. J. Expo. Sci. Environ. Epidemiol. 2015, 25, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Su, L.; Chen, X.; Wang, S.; Cheng, Y.; Lin, S.; Ding, L.; Liu, J.; Chen, C.; Unverzagt, F.W.; et al. Higher blood cadmium level is associated with greater cognitive decline in rural Chinese adults aged 65 or older. Sci. Total Environ. 2020, 756, 144072. [Google Scholar] [CrossRef] [PubMed]
- El-Boshy, M.E.; Risha, E.F.; Abdelhamid, F.M.; Mubarak, M.S.; Hadda, T.B. Protective effects of selenium against cadmium induced hematological disturbances, immunosuppressive, oxidative stress and hepatorenal damage in rats. J. Trace Elem. Med. Biol. 2015, 29, 104–110. [Google Scholar] [CrossRef]
- Lin, Y.S.; Ho, W.C.; Caffrey, J.L.; Sonawane, B. Low serum zinc is associated with elevated risk of cadmium nephrotoxicity. Environ. Res. 2014, 134, 33–38. [Google Scholar] [CrossRef]
- Mijal, R.S.; Holzman, C.B. Blood cadmium levels in women of childbearing age vary by race/ethnicity. Environ. Res. 2010, 110, 505–512. [Google Scholar] [CrossRef]
- Vahter, M.; Åkesson, A.; Lidén, C.; Ceccatelli, S.; Berglund, M. Gender differences in the disposition and toxicity of metals. Environ. Res. 2007, 104, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Brzóska, M.M.; Borowska, S.; Tomczyk, M. Antioxidants as a potential preventive and therapeutic strategy for cadmium. Curr. Drug Targets 2016, 17, 1350–1384. [Google Scholar] [CrossRef] [PubMed]
- Mężyńska, M.; Brzóska, M.M. Review of polyphenol-rich products as potential protective and therapeutic factors against cadmium hepatotoxicity. J. Appl. Toxicol. 2019, 39, 117–145. [Google Scholar] [CrossRef]
- Garner, R.; Levallois, P. Cadmium levels and sources of exposure among Canadian adults. Health Rep. 2016, 27, 10–18. [Google Scholar]
- Jung, S.Y.; Kim, S.; Lee, K.; Kim, J.Y.; Bae, W.K.; Lee, K.; Han, J.-S.; Kim, S. Association between secondhand smoke exposure and blood lead and cadmium concentration in community dwelling women: The fifth Korea National Health and Nutrition Examination Survey (2010–2012). BMJ Open 2015, 5, e008218. [Google Scholar] [CrossRef]
- Garner, R.E.; Levallois, P. Associations between cadmium levels in blood and urine, blood pressure and hypertension among Canadian adults. Environ. Res. 2017, 155, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Ratelle, M.; Li, X.; Laird, B.D. Cadmium exposure in First Nations communities of the Northwest Territories, Canada: Smoking is a greater contributor than consumption of cadmium-accumulating organ meats. Environ. Sci. Process. Impacts 2018, 20, 1441–1453. [Google Scholar] [CrossRef] [PubMed]
- Shakeri, M.T.; Nezami, H.; Nakhaee, S.; Aaseth, J.; Mehrpour, O. Assessing heavy metal burden among cigarette smokers and non-smoking individuals in Iran: Cluster analysis and principal component analysis. Biol. Trace Elem. Res. 2021, 199, 4036–4044. [Google Scholar] [CrossRef] [PubMed]
- Repić, A.; Bulat, P.; Antonijević, B.; Antunović, M.; Džudović, J.; Buha, A.; Bulat, Z. The influence of smoking habits on cadmium and lead blood levels in the Serbian adult people. Environ. Sci. Pollut. Res. 2020, 27, 751–760. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Kim, H.R.; Lee, M.H.; Kim, N.H.; Wang, K.M.; Lee, S.H.; Park, O.; Hong, E.J.; Youn, J.W.; Kim, Y.Y. Smoking-related DNA methylation is differentially associated with cadmium concentration in blood. Biochem. Genet. 2020, 58, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Kim, Y.; Kim, Y.; Yoo, H.; Kang, H.T. Cigarette smoking in men and women and electronic cigarette smoking in men are associated with higher risk of elevated cadmium level in the blood. J. Korean Med. Sci. 2020, 35, e15. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Fagerberg, B.; Sallsten, G.; Borné, Y.; Hedblad, B.; Engström, G.; Barregard, L.; Andersson, E.M. Smoking-induced risk of future cardiovascular disease is partly mediated by cadmium in tobacco: Malmö Diet and Cancer Cohort Study. Environ. Health 2019, 18, 56. [Google Scholar] [CrossRef]
- Domingo-Relloso, A.; Riffo-Campos, A.L.; Haack, K.; Rentero-Garrido, P.; Ladd-Acosta, C.; Fallin, D.M.; Tang, W.Y.; Herreros-Martinez, M.; Gonzalez, J.R.; Bozack, A.K.; et al. Cadmium, smoking, and human blood DNA+ methylation profiles in adults from the strong heart study. Environ. Health Perspect. 2020, 128, 067005. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, P.; Liang, X.; Tan, C.S.; Tan, J.; Wang, J.; Huang, Q.; Huang, R.; Li, Z.; Chen, W.; et al. Associations between urinary excretion of cadmium and renal biomarkers in nonsmoking females: A cross-sectional study in rural areas of South China. Int. J. Environ. Res. Public Health 2015, 12, 11988–12001. [Google Scholar] [CrossRef]
- Agency for Toxic Substances & Disease Registry. Toxicological Profile: Cadmium. 2012. Available online: https://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=48&tid=15 (accessed on 13 March 2023).
- Wang, X.; Wang, Y.; Feng, L.; Tong, Y.; Chen, Z.; Ying, S.; Chen, T.; Li, T.; Xia, H.; Jiang, Z.; et al. Application of the benchmark dose (BMD) method to identify thresholds of cadmium-induced renal effects in non-polluted areas in China. PLoS ONE 2016, 11, e0161240. [Google Scholar] [CrossRef]
- Wang, D.; Sun, H.; Wu, Y.; Zhou, Z.; Ding, Z.; Chen, X.; Xu, Y. Tubular and glomerular kidney effects in the Chinese general population with low environmental cadmium exposure. Chemosphere 2016, 147, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Ke, S.; Cheng, X.Y.; Zhang, J.Y.; Jia, W.J.; Li, H.; Luo, H.F.; Ge, P.H.; Liu, Z.M.; Wang, H.M.; He, J.S.; et al. Estimation of the benchmark dose of urinary cadmium as the reference level for renal dysfunction: A large sample study in five cadmium polluted areas in China. BMC Public Health 2015, 15, 656. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.S.; Lee, B.K. National estimates of blood lead, cadmium, and mercury levels in the Korean general adult population. Int. Arch. Occup. Environ. Health 2011, 84, 53–63. [Google Scholar] [CrossRef]
- Afrifa, J.; Essien-Baidoo, S.; Ephraim, R.K.D.; Nkrumah, D.; Dankyira, D.O. Reduced eGFR, elevated urine protein and low level of personal protective equipment compliance among artisanal small scale gold miners at Bibiani-Ghana: A cross-sectional study. BMC Public Health 2017, 17, 601. [Google Scholar] [CrossRef] [PubMed]
- Byber, K.; Lison, D.; Verougstraete, V.; Dressel, H.; Hotz, P. Cadmium or cadmium compounds and chronic kidney disease in workers and the general population: A systematic review. Crit. Rev. Toxicol. 2016, 46, 191–240. [Google Scholar] [CrossRef]
- Cao, Z.R.; Cui, S.M.; Lu, X.X.; Chen, X.M.; Yang, X.; Cui, J.P.; Zhang, G.H. Effects of occupational cadmium exposure on workers’ cardiovascular system. Chin. J. Ind. Hyg. Occup. Dis. 2018, 36, 474–477, (In Chinese, with an English abstract). [Google Scholar] [CrossRef]
- Choi, W.J.; Kang, S.K.; Ham, S.; Chung, W.; Kim, A.J.; Kang, M. Chronic cadmium intoxication and renal injury among workers of a small-scale silver soldering company. Saf. Health Work 2020, 11, 235–240. [Google Scholar] [CrossRef]
- Gao, Y.; Zhang, Y.; Yi, J.; Zhou, J.; Huang, X.; Shi, X.; Xiao, S.; Lin, D. A longitudinal study on urinary cadmium and renal tubular protein excretion of nickel–cadmium battery workers after cessation of cadmium exposure. Int. Arch. Occup. Environ. Health 2016, 89, 1137–1145. [Google Scholar] [CrossRef]
- Hormozi, M.; Mirzaei, R.; Nakhaee, A.; Izadi, S.; Dehghan Haghighi, J. The biochemical effects of occupational exposure to lead and cadmium on markers of oxidative stress and antioxidant enzymes activity in the blood of glazers in tile industry. Toxicol. Ind. Health 2018, 34, 459–467. [Google Scholar] [CrossRef]
- Scammell, M.K.; Sennett, C.M.; Petropoulos, Z.E.; Kamal, J.; Kaufman, J.S. Environmental and occupational exposures in kidney disease. Semin. Nephrol. 2019, 39, 230–243. [Google Scholar] [CrossRef]
- Taha, M.M.; Mahdy-Abdallah, H.; Shahy, E.M.; Ibrahim, K.S.; Elserougy, S. Impact of occupational cadmium exposure on bone in sewage workers. Int. J. Occup. Environ. Health 2018, 24, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Rentschler, G.; Kippler, M.; Axmon, A.; Raqib, R.; Skerfving, S.; Vahter, M.; Broberg, K. Cadmium concentrations in human blood and urine are associated with polymorphisms in zinc transporter genes. Metallomics 2014, 6, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Huo, J.; Li, R.; Jia, Z.; Song, Y.; Chen, J.; Zhang, L. Benchmark dose estimation of urinary and blood cadmium as biomarkers of renal dysfunction among 40–75-year-old non-smoking women in rural areas of southwest China. J. Appl. Toxicol. 2019, 39, 1433–1443. [Google Scholar] [CrossRef] [PubMed]
- Rooney, J.P.K.; Michalke, B.; Geoghegan, G.; Heverin, M.; Bose-O’Reilly, S.; Hardiman, O.; Rakete, S. Urine concentrations of selected trace metals in a cohort of Irish adults. Environ. Sci. Pollut. Res. 2022, 29, 75356–75364. [Google Scholar] [CrossRef]
- Moon, M.K.; Lee, I.; Lee, A.; Park, H.; Kim, M.J.; Kim, S.; Cho, Y.H.; Hong, S.; Yoo, J.; Cheon, G.J.; et al. Lead, mercury, and cadmium exposures are associated with obesity but not with diabetes mellitus: Korean National Environmental Health Survey (KoNEHS) 2015–2017. Environ. Res. 2022, 204, 111888. [Google Scholar] [CrossRef]
- Satarug, S.; Gobe, G.C.; Ujjin, P.; Vesey, D.A. A comparison of the nephrotoxicity of low doses of cadmium and lead. Toxics 2020, 8, 18. [Google Scholar] [CrossRef]
- Nishijo, M.; Suwazono, Y.; Ruangyuttikarn, W.; Nambunmee, K.; Swaddiwudhipong, W.; Nogawa, K.; Nakagawa, H. Risk assessment for Thai population: Benchmark dose of urinary and blood cadmium levels for renal effects by hybrid approach of inhabitants living in polluted and non-polluted areas in Thailand. BMC Public Health 2014, 14, 702. [Google Scholar] [CrossRef]
- Yıldırım, E.; Derici, M.K.; Demir, E.; Apaydın, H.; Koçak, Ö.; Kan, Ö.; Görkem, Ü. Is the concentration of cadmium, lead, mercury, and selenium related to preterm birth? Biol. Trace Elem. Res. 2019, 191, 306–312. [Google Scholar] [CrossRef]
- Kim, J.; Garcia-Esquinas, E.; Navas-Acien, A.; Choi, Y.H. Blood and urine cadmium concentrations and walking speed in middle-aged and older U.S. adults. Environ. Pollut. 2018, 232, 97–104. [Google Scholar] [CrossRef]
- Yao, X.; Steven Xu, X.; Yang, Y.; Zhu, Z.; Zhu, Z.; Tao, F.; Yuan, M. Stratification of population in NHANES 2009–2014 based on exposure pattern of lead, cadmium, mercury, and arsenic and their association with cardiovascular, renal and respiratory outcomes. Environ. Int. 2021, 149, 106410. [Google Scholar] [CrossRef]
- Snoj Tratnik, J.; Kocman, D.; Horvat, M.; Andersson, A.M.; Juul, A.; Jacobsen, E.; Ólafsdóttir, K.; Klanova, J.; Andryskova, L.; Janasik, B.; et al. Cadmium exposure in adults across Europe: Results from the HBM4EU Aligned Studies survey 2014-2020. Int. J. Hyg. Environ. Health 2022, 246, 114050. [Google Scholar] [CrossRef]
- Pawlas, N.; Strömberg, U.; Carlberg, B.; Cerna, M.; Harari, F.; Harari, R.; Horvat, M.; Hruba, F.; Koppova, K.; Krskova, A.; et al. Cadmium, mercury and lead in the blood of urban women in Croatia, the Czech Republic, Poland, Slovakia, Slovenia, Sweden, China, Ecuador and Morocco. Int. J. Occup. Med. Environ. Health 2013, 26, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Dai, S.; Yin, Z.; Yuan, G.; Lu, H.; Jia, R.; Xu, J.; Song, X.; Li, L.; Shu, Y.; Liang, X.; et al. Quantification of metallothionein on the liver and kidney of rats by subchronic lead and cadmium in combination. Environ. Toxicol. Pharmacol. 2013, 36, 1207–1216. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Shu, Y. Cadmium transporters in the kidney and cadmium-induced nephrotoxicity. Int. J. Mol. Sci. 2015, 16, 1484–1494. [Google Scholar] [CrossRef]
- Satarug, S.; Baker, J.R.; Reilly, P.E.B.; Moore, M.R.; Williams, D.J. Cadmium levels in the lung, liver, kidney cortex, and urine samples from Australians without occupational exposure to metals. Arch. Environ. Health 2002, 57, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Suwazono, Y.; Kido, T.; Nakagawa, H.; Nishijo, M.; Honda, R.; Kobayashi, E.; Dochi, M.; Nogawa, K. Biological half-life of cadmium in the urine of inhabitants after cessation of cadmium exposure. Biomarkers 2009, 14, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Zalups, R.K.; Ahmad, S. Molecular handling of cadmium in transporting epithelia. Toxicol. Appl. Pharmacol. 2003, 186, 163–188. Available online: http://www.ncbi.nlm.nih.gov/pubmed/12620369 (accessed on 15 March 2023). [CrossRef]
- Mohseni, H.K.; Chettle, D.R. A history of in vivo neutron activation analysis in measurement of aluminum in human subjects. J. Alzheimer’s Dis. 2016, 50, 913–926. [Google Scholar] [CrossRef]
- Lech, T.; Sadlik, J.K. Cadmium concentration in human autopsy tissues. Biol. Trace Elem. Res. 2017, 179, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Benes, B.; Jakubec, K.; Smíd, J.; Spĕvácková, V. Determination of thirty-two elements in human autopsy tissue. Biol. Trace Elem. Res. 2000, 75, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Johansen, P.; Mulvad, G.; Pedersen, H.S.; Hansen, J.C.; Riget, F. Accumulation of cadmium in livers and kidneys in Greenlanders. Sci. Total Environ. 2006, 372, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Uetani, M.; Kobayashi, E.; Suwazono, Y.; Honda, R.; Nishijo, M.; Nakagawa, H.; Kido, T.; Nogawa, K. Tissue cadmium (Cd) concentrations of people living in a Cd polluted area, Japan. BioMetals 2006, 19, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Rahil-Khazen, R.; Bolann, B.J.; Myking, A.; Ulvik, R.J. Multi-element analysis of trace element levels in human autopsy tissues by using inductively coupled atomic emission spectrometry technique (ICP-AES). J. Trace Elem. Med. Biol. 2002, 16, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Chan Yoo, Y.; Ki Lee, S.; Yeol Yang, J.; Whan In, S.; Wook Kim, K.; Hyuck Chung, K.; Gyu Chung, M.; Young Choung, S. Organ distribution of heavy metals in autopsy material from normal Korean. J. Health Sci. 2002, 48, 186–194. [Google Scholar] [CrossRef]
- García, F.; Ortega, A.; Domingo, J.L.; Corbella, J. Accumulation of metals in autopsy tissues of subjects living in Tarragona County, Spain. J. Environ. Sci. Health Part A 2001, 36, 1767–1786. [Google Scholar] [CrossRef]
- Mari, M.; Nadal, M.; Schuhmacher, M.; Barbería, E.; García, F.; Domingo, J.L. Human exposure to metals: Levels in autopsy tissues of individuals living near a hazardous waste incinerator. Biol. Trace Elem. Res. 2014, 159, 15–21. [Google Scholar] [CrossRef]
- Barregard, L.; Sallsten, G.; Lundh, T.; Mölne, J. Low-level exposure to lead, cadmium and mercury, and histopathological findings in kidney biopsies. Environ. Res. 2022, 211, 113119. [Google Scholar] [CrossRef]
- Bulat, Z.P.; Đukić-Ćosić, D.; Đokić, M.; Bulat, P.; Matović, V. Blood and urine cadmium and bioelements profile in nickel-cadmium battery workers in Serbia. Toxicol. Ind. Health 2009, 25, 129–135. [Google Scholar] [CrossRef]
- Nordberg, M.; Jin, T.; Nordberg, G.F. Cadmium, metallothionein and renal tubular toxicity. IARC Sci. Publ. 1992, 118, 293–297. [Google Scholar]
- Ohta, H.; Yamauchi, Y.; Nakakita, M.; Tanaka, H.; Asami, S.; Seki, Y.; Yoshikawa, H. Relationship between renal dysfunction and bone metabolism disorder in male rats after long-term oral quantitative cadmium administration. Ind. Health 2000, 38, 339–355. [Google Scholar] [CrossRef]
- Riaz, M.A.; Nisa, Z.U.; Mehmood, A.; Anjum, M.S.; Shahzad, K. Metal-induced nephrotoxicity to diabetic and non-diabetic Wistar rats. Environ. Sci. Pollut. Res. 2019, 26, 31111–31118. [Google Scholar] [CrossRef] [PubMed]
- Andreollo, N.A.; Santos, E.F.; Araújo, M.R.; Lopes, L.R. Rat’s age versus human’s age: What is the relationship? Arq. Bras. Cir. Dig. 2012, 25, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Hyun, Y.Y.; Lee, K.B.; Chang, Y.; Rhu, S.; Oh, K.H.; Ahn, C. Environmental heavy metal exposure and chronic kidney disease in the general population. J. Korean Med. Sci. 2015, 30, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Stajnko, A.; Falnoga, I.; Tratnik, J.S.; Mazej, D.; Jagodic, M.; Krsnik, M.; Kobal, A.B.; Prezelj, M.; Kononenko, L.; Horvat, M. Low cadmium exposure in males and lactating females–estimation of biomarkers. Environ. Res. 2017, 152, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Kuzuhara, Y.; Sano, K.; Hayashi, C.; Kitanura, S. Heavy metals in autopsy samples. The concentration of heavy metals in autopsy samples: Humans lived in cadmium polluted and non-polluted areas. Kankyo Hoken Rep. 1985, 59, 154–155. [Google Scholar]
- Nogawa, K.; Kido, T. Biological monitoring of cadmium exposure in itai-itai disease epidemiology. Int. Arch. Occup. Environ. Health 1993, 65, S43–S46. [Google Scholar] [CrossRef]
- Yasuda, M.; Miwa, A.; Kitagawa, M. Morphometric studies of renal lesions in Itai-itai disease: Chronic cadmium nephropathy. Nephron 1995, 69, 14–19. [Google Scholar] [CrossRef]
- Lim, H.; Lim, J.A.; Choi, J.H.; Kwon, H.J.; Ha, M.; Kim, H.; Park, J.D. Associations of low environmental exposure to multiple metals with renal tubular impairment in Korean adults. Toxicol. Res. 2016, 32, 57–64. [Google Scholar] [CrossRef]
- Brzóska, M.M.; Kamiński, M.; Supernak-Bobko, D.; Zwierz, K.; Moniuszko-Jakoniuk, J. Changes in the structure and function of the kidney of rats chronically exposed to cadmium. I. Biochemical and histopathological studies. Arch. Toxicol. 2003, 77, 344–352. [Google Scholar] [CrossRef]
- Brzóska, M.M.; Kamiński, M.; Dziki, M.; Moniuszko-Jakoniuk, J. Changes in the structure and function of the kidney of rats chronically exposed to cadmium. II. Histoenzymatic studies. Arch. Toxicol. 2004, 78, 226–231. [Google Scholar] [CrossRef]
- Fay, M.; Alt, L.; Ryba, D.; Salamah, R.; Peach, R.; Papaeliou, A.; Zawadzka, S.; Weiss, A.; Patel, N.; Rahman, A.; et al. Cadmium nephrotoxicity is associated with altered microRNA expression in the rat renal cortex. Toxics 2018, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Bellinger, D.; Bolger, M.; Goyer, R.; Barraj, L.; Baines, J. WHO Food Additives Series 46, Cadmium. 2001. Available online: http://www.inchem.org/documents/jecfa/jecmono/v46je11.htm. (accessed on 13 March 2023).
- Satarug, S. Long-term exposure to cadmium in food and cigarette smoke, liver effects and hepatocellular carcinoma. Curr. Drug Metab. 2012, 13, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Waisberg, M.; Joseph, P.; Hale, B.; Beyersmann, D. Molecular and cellular mechanisms of cadmium carcinogenesis. Toxicology 2003, 192, 95–117. [Google Scholar] [CrossRef]
- Chen, X.X.; Xu, Y.M.; Lau, A.T.Y. Metabolic effects of long-term cadmium exposure: An overview. Environ. Sci. Pollut. Res. 2022, 29, 89874–89888. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Henmi, K.; Ogawa, K.; Suzuki, T. Cadmium-dependent generation of reactive oxygen species and mitochondrial DNA breaks in photosynthetic and non-photosynthetic strains of Euglena gracilis. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2003, 134, 227–234. [Google Scholar] [CrossRef]
- Klaassen, C.D.; Liu, J.; Choudhuri, S. Metallothionein: An intracellular protein to protect against cadmium toxicity. Annu. Rev. Pharmacol. 1999, 39, 267–294. [Google Scholar] [CrossRef]
- Lee, W.K.; Probst, S.; Santoyo-Sánchez, M.P.; Al-Hamdani, W.; Diebels, I.; von Sivers, J.K.; Kerek, E.; Prenner, E.J.; Thévenod, F. Initial autophagic protection switches to disruption of autophagic flux by lysosomal instability during cadmium stress accrual in renal NRK-52E cells. Arch. Toxicol. 2017, 91, 3225–3245. [Google Scholar] [CrossRef]
- Thévenod, F.; Lee, W.K.; Garrick, M.D. Iron and cadmium entry into renal mitochondria: Physiological and toxicological implications. Front. Cell Dev. Biol. 2020, 8, 848. [Google Scholar] [CrossRef]
- Aranda-Rivera, A.K.; Cruz-Gregorio, A.; Aparicio-Trejo, O.E.; Pedraza-Chaverri, J. Mitochondrial redox signaling and oxidative stress in kidney diseases. Biomolecules 2021, 11, 1144. [Google Scholar] [CrossRef]
- Valcke, M.; Ouellet, N.; Dubé, M.; Laouan Sidi, E.A.; LeBlanc, A.; Normandin, L.; Balion, C.; Ayotte, P. Biomarkers of cadmium, lead and mercury exposure in relation with early biomarkers of renal dysfunction and diabetes: Results from a pilot study among aging Canadians. Toxicol. Lett. 2019, 312, 148–156. [Google Scholar] [CrossRef]
- Zeng, T.; Liang, Y.; Chen, J.; Cao, G.; Yang, Z.; Zhao, X.; Tian, J.; Xin, X.; Lei, B.; Cai, Z. Urinary metabolic characterization with nephrotoxicity for residents under cadmium exposure. Environ. Int. 2021, 154, 106646. [Google Scholar] [CrossRef] [PubMed]
- Baiomy, A.A.; Mansour, A.A. Genetic and histopathological responses to cadmium toxicity in rabbit’s kidney and liver: Protection by ginger (Zingiber officinale). Biol. Trace Elem. Res. 2016, 170, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Jiao, X.; Luo, W.; Chen, J.; Xu, X.; Fang, Y.; Ding, X.; Yu, X. Kidney injury molecule-1 expression predicts structural damage and outcome in histological acute tubular injury. Ren. Fail. 2019, 41, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Bernard, A. Renal dysfunction induced by cadmium: Biomarkers of critical effects. BioMetals 2004, 17, 519–523. [Google Scholar] [CrossRef]
- Grau-Perez, M.; Pichler, G.; Galan-Chilet, I.; Briongos-Figuero, L.S.; Rentero-Garrido, P.; Lopez-Izquierdo, R.; Navas-Acien, A.; Weaver, V.; García-Barrera, T.; Gomez-Ariza, J.L.; et al. Urine cadmium levels and albuminuria in a general population from Spain: A gene-environment interaction analysis. Environ. Int. 2017, 106, 27–36. [Google Scholar] [CrossRef]
- Sakurai, M.; Suwazono, Y.; Nishijo, M.; Nogawa, K.; Watanabe, Y.; Ishizaki, M.; Morikawa, Y.; Kido, T.; Nakagawa, H. Relationship between urinary β2-microglobulin concentration and mortality in a cadmium-polluted area in Japan: A 35-year follow-up study. J. Appl. Toxicol. 2021, 41, 224–232. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Nishijo, M.; Ruangyuttikarn, W.; Gobe, G.C. The inverse association of glomerular function and urinary Β2-MG excretion and its implications for cadmium health risk assessment. Environ. Res. 2019, 173, 40–47. [Google Scholar] [CrossRef]
- Wang, H.; Dumont, X.; Haufroid, V.; Bernard, A. The physiological determinants of low-level urine cadmium: An assessment in a cross-sectional study among schoolchildren. Environ. Health 2017, 16, 99. [Google Scholar] [CrossRef]
- Hambach, R.; Lison, D.; D’Haese, P.C.; Weyler, J.; De Graef, E.; De Schryver, A.; Lamberts, L.V.; van Sprundel, M. Co-exposure to lead increases the renal response to low levels of cadmium in metallurgy workers. Toxicol. Lett. 2013, 222, 233–238. [Google Scholar] [CrossRef]
- Chaumont, A.; De Winter, F.; Dumont, X.; Haufroid, V.; Bernard, A. The threshold level of urinary cadmium associated with increased urinary excretion of retinol-binding protein and β2-microglobulin: A re-assessment in a large cohort of nickel-cadmium battery workers. Occup. Environ. Med. 2011, 68, 257–264. [Google Scholar] [CrossRef]
- Win-Thu, M.; Myint-Thein, O.; Win-Shwe, T.T.; Mar, O. Environmental cadmium exposure induces kidney tubular and glomerular dysfunction in the Myanmar adults. J. Toxicol. Sci. 2021, 46, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, M.; Ohashi, F.; Fukui, Y.; Sakuragi, S.; Moriguchi, J. Closer correlation of cadmium in urine than that of cadmium in blood with tubular dysfunction markers in urine among general women populations in Japan. Int. Arch. Occup. Environ. Health 2011, 84, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Penders, J.; Delanghe, J.R. Alpha 1-microglobulin: Clinical laboratory aspects and applications. Clin. Chim. 2004, 346, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Domingos, M.A.M.; Moreira, S.R.; Gomez, L.; Goulart, A.; Lotufo, P.A.; Benseñor, I.; Titan, S. Urinary retinol-binding protein: Relationship to renal function and cardiovascular risk factors in chronic kidney disease. PLoS ONE 2016, 11, e0162782. [Google Scholar] [CrossRef]
- Liu, C.X.; Li, Y.B.; Zhu, C.S.; Dong, Z.M.; Zhang, K.; Zhao, Y.; Xu, Y.L. Benchmark dose for cadmium exposure and elevated N-acetyl-β-d-glucosaminidase: A meta-analysis. Environ. Sci. Pollut. Res. 2016, 23, 20528–20538. [Google Scholar] [CrossRef]
- Ichimura, T.; Bonventre, J.V.; Bailly, V.; Wei, H.; Hession, C.A.; Cate, R.L.; Sanicola, M. Kidney injury molecule-1 (KIM-1), a putative epithelial cell adhesion molecule containing a novel immunoglobulin domain, is up-regulated in renal cells after injury. J. Biol. Chem. 1998, 273, 4135–4142. [Google Scholar] [CrossRef]
- Huang, Y.; Tian, Y.; Likhodii, S.; Randell, E. Baseline urinary KIM-1 concentration in detecting acute kidney injury should be interpreted with patient pre-existing nephropathy. Pract. Lab. Med. 2019, 15, e00118. [Google Scholar] [CrossRef]
- Martín-Granado, A.; Vázquez-Moncholí, C.; Luis-Yanes, M.I.; López-Méndez, M.; García-Nieto, V. Determination of Clara cell protein urinary elimination as a marker of tubular dysfunction. Pediatr. Nephrol. 2009, 24, 747–752. [Google Scholar] [CrossRef]
- Prozialeck, W.C.; Vaidya, V.S.; Liu, J.; Waalkes, M.P.; Edwards, J.R.; Lamar, P.C.; Bernard, A.M.; Dumont, X.; Bonventre, J.V. Kidney injury molecule-1 is an early biomarker of cadmium nephrotoxicity. Kidney Int. 2007, 72, 985–993. [Google Scholar] [CrossRef]
- Lv, Y.; Wang, P.; Huang, R.; Liang, X.; Wang, P.; Tan, J.; Chen, Z.; Dun, Z.; Wang, J.; Jiang, Q.; et al. Cadmium exposure and osteoporosis: A population-based study and benchmark dose estimation in Southern China. J. Bone Miner. Res. 2017, 32, 1990–2000. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Gobe, G.C. Cadmium-induced proteinuria: Mechanistic insights from dose–effect analyses. Int. J. Mol. Sci. 2023, 24, 1893. [Google Scholar] [CrossRef] [PubMed]
- Akerstrom, M.; Sallsten, G.; Lundh, T.; Barregard, L. Associations between urinary excretion of cadmium and proteins in a nonsmoking population: Renal toxicity or normal physiology. Environ. Health Perspect. 2013, 121, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, P.M.; Costanzi, S.; Naticchia, A.; Sturniolo, A.; Gambaro, G. Low level exposure to cadmium increases the risk of chronic kidney disease: Analysis of the NHANES 1999–2006. BMC Public Health 2010, 10, 304. [Google Scholar] [CrossRef] [PubMed]
- Weaver, V.; Navas-Acien, A.; Tellez-Plaza, M.; Guallar, E.; Muntner, P.; Silbergeld, E.; Jaar, B. Blood cadmium and lead and chronic kidney disease in US adults: A joint analysis. Am. J. Epidemiol. 2009, 170, 1156–1164. [Google Scholar] [CrossRef]
- Wu, C.Y.; Wong, C.S.; Chung, C.J.; Wu, M.Y.; Huang, Y.L.; Ao, P.L.; Lin, Y.F.; Lin, Y.C.; Shiue, H.S.; Su, C.T.; et al. The association between plasma selenium and chronic kidney disease related to lead, cadmium and arsenic exposure in a Taiwanese population. J. Hazard. Mater. 2019, 375, 224–232. [Google Scholar] [CrossRef]
- Arain, M.B.; Kazi, T.G.; Baig, J.A.; Afridi, H.I.; Uddin, S.; Brehman, K.D.; Panhwar, H.; Arain, S.S. Co-exposure of arsenic and cadmium through drinking water and tobacco smoking: Risk assessment on kidney dysfunction. Environ. Sci. Pollut. Res. 2014, 22, 350–357. [Google Scholar] [CrossRef]
- Li, X.; Li, R.; Yan, J.; Song, Y.; Huo, J.; Lan, Z.; Chen, J.; Zhang, L. Co-exposure of cadmium and lead on bone health in a southwestern Chinese population aged 40-75 years. J. Appl. Toxicol. 2020, 40, 352–362. [Google Scholar] [CrossRef]
- Sanders, A.P.; Mazzella, M.J.; Malin, A.J.; Hair, G.; Busgang, S.A.; Saland, J.M.; Curtin, P. Combined exposure to lead, cadmium, mercury, and arsenic and kidney health in adolescents age 12–19 in NHANES 2009–2014. Environ. Int. 2019, 131, 104993. [Google Scholar] [CrossRef]
- Zou, H.; Chen, Y.; Qu, H.; Sun, J.; Wang, T.; Ma, Y.; Yuan, Y.; Bian, J.; Liu, Z. Microplastics exacerbate cadmium-induced kidney injury by enhancing oxidative stress, autophagy, apoptosis, and fibrosis. Int. J. Mol. Sci. 2022, 23, 14411. [Google Scholar] [CrossRef]
- Lunyera, J.; Smith, S.R. Heavy metal nephropathy: Considerations for exposure analysis. Kidney Int. 2017, 92, 548–550. [Google Scholar] [CrossRef]
- Buser, M.C.; Ingber, S.Z.; Raines, N.; Fowler, D.A.; Scinicariello, F. Urinary and blood cadmium and lead and kidney function: NHANES 2007-2012. Int. J. Hyg. Environ. Health 2016, 219, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Harari, F.; Sallsten, G.; Christensson, A.; Petkovic, M.; Hedblad, B.; Forsgard, N.; Melander, O.; Nilsson, P.M.; Borné, Y.; Engström, G.; et al. Blood lead levels and decreased kidney function in a population-based cohort. Am. J. Kidney Dis. 2018, 72, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Drubay, D.; Ancelet, S.; Acker, A.; Kreuzer, M.; Laurier, D.; Rage, E. Kidney cancer mortality and ionizing radiation among French and German uranium miners. Radiat. Environ. Biophys. 2014, 53, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Dastan, D.; Karimi, S.; Larki–Harchegani, A.; Nili–Ahmadabadi, A. Protective effects of Allium hirtifolium Boiss extract on cadmium-induced renal failure in rats. Environ. Sci. Pollut. Res. 2019, 26, 18886–18892. [Google Scholar] [CrossRef]
- Gabr, S.A.; Alghadir, A.H.; Ghoniem, G.A. Biological activities of ginger against cadmium-induced renal toxicity. Saudi J. Biol. Sci. 2019, 26, 382–389. [Google Scholar] [CrossRef]
- Suliman Al–Gebaly, A. Ameliorative effect of Arctium lappa against cadmium genotoxicity and histopathology in kidney of Wistar rat. Pak. J. Biol. Sci. 2017, 20, 314–319. [Google Scholar] [CrossRef]
- Ramamurthy, C.H.; Subastri, A.; Suyavaran, A.; Subbaiah, K.C.; Valluru, L.; Thirunavukkarasu, C. Solanum torvum Swartz. fruit attenuates cadmium-induced liver and kidney damage through modulation of oxidative stress and glycosylation. Environ. Sci. Pollut. Res. 2016, 23, 7919–7929. [Google Scholar] [CrossRef]
- El–Aziz, A.G.S.; Mustafa, H.N.; Saleh, H.A.; El–Fark, M.M.O. Zingiber Officinale alleviates maternal and fetal hepatorenal toxicity induced by prenatal cadmium. Biomed. Pharmacol. J. 2018, 11, 1369–1380. [Google Scholar] [CrossRef]
- Gattea Al-Rikabi, Z.; Abbas, A.H.; Kadhum Oudah, H.; Sajer Nassir, H.; Ali, S.A. Histopathological study of liver and kidney tissues in C57 mice via chronic exposure to cadmium and zinc. Arch. Razi Inst. 2021, 76, 1501–1508. [Google Scholar] [CrossRef]
- Sanjeev, S.; Bidanchi, R.M.; Murthy, M.K.; Gurusubramanian, G.; Roy, V.K. Influence of ferulic acid consumption in ameliorating the cadmium-induced liver and renal oxidative damage in rats. Environ. Sci. Pollut. Res. 2019, 26, 20631–20653. [Google Scholar] [CrossRef]
- Huang, K.; Deng, Y.; Yuan, W.; Geng, J.; Wang, G.; Zou, F. Phospholipase D1 ameliorates apoptosis in chronic renal toxicity caused by low-dose cadmium exposure. Biomed Res. Int. 2020, 7091053. [Google Scholar] [CrossRef] [PubMed]
- Elkhadragy, M.F.; Al–Olayan, E.M.; Al–Amiery, A.A.; Abdel Moneim, A.E. Protective effects of Fragaria ananassa extract against cadmium chloride-induced acute renal toxicity in rats. Biol. Trace Elem. Res. 2018, 181, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Poontawee, W.; Natakankitkul, S.; Wongmekiat, O. Protective effect of Cleistocalyx nervosum var. paniala fruit extract against oxidative renal damage caused by cadmium. Molecules 2016, 21, 133. [Google Scholar] [CrossRef] [PubMed]
- Shen, R.; Liu, D.; Hou, C.; Liu, D.; Zhao, L.; Cheng, J.; Wang, D.; Bai, D. Protective effect of Potentilla anserina polysaccharide on cadmium-induced nephrotoxicity in vitro and in vivo. Food Funct. 2017, 8, 3636–3646. [Google Scholar] [CrossRef] [PubMed]
- Akinyemi, A.J.; Faboya, O.L.; Paul, A.A.; Olayide, I.; Faboya, O.A.; Oluwasola, T.A. Nephroprotective effect of essential oils from ginger (Zingiber officinale) and turmeric (Curcuma longa) rhizomes against cadmium-induced nephrotoxicity in rats. J. Oleo Sci. 2018, 67, 1339–1345. [Google Scholar] [CrossRef]
- Athmouni, K.; Belhaj, D.; Chawech, R.; Jarraya, R.; El Feki, A.; Ayadi, H. Characterization of polysaccharides isolated from Periploca angustifolia and its antioxidant activity and renoprotective potential against cadmium induced toxicity in HEK293 cells and rat kidney. Int. J. Biol. Macromol. 2019, 125, 730–742. [Google Scholar] [CrossRef]
- Ojo, O.A.; Ajiboye, B.O.; Oyinloye, B.E.; Ojo, A.B.; Olarewaju, O.I. Protective effect of Irvingia gabonensis stem bark extract on cadmium-induced nephrotoxicity in rats. Interdiscip. Toxicol. 2014, 7, 208–214. [Google Scholar] [CrossRef]


| Database | Total Number of Articles Found (Published in 2013–2023) | Number of Articles Excluded (Duplicates, Papers Out of Our Scope, or Papers Older than 10 Years) | Number of Articles Included in This Study |
|---|---|---|---|
| Pubmed | 3971 | 3896 | 75 |
| Scopus | 8571 | 8546 | 25 |
| Elsevier | 3064 | 3041 | 23 |
| Taylor & Francis Online | 2491 | 2482 | 9 |
| Country | n | Expression of Cd Concentration | Cd in the Blood (μg/L) and Urine b (μg/g Creatinine) | Reference | |
|---|---|---|---|---|---|
| Smokers | Non-Smokers | ||||
| Canada | 10,099 | GM (SE) | 1.63 (0.06) † 0.56 (0.02) † | 0.22 (0.01) 0.33 (0.01) | [73] |
| 144 | GM (P95) | 1.62 (3.75) * 0.467 (1.21) * | 0.265 (1.88) 0.333 (0.937) | [74] | |
| Iran | 140 | Mean (IQR) | 0.87 (0.67–1.31) NS | 0.81 (0.59–1.30) | [75] |
| Serbia | 81 | Mean ± 95% Cl | 2.41 ± 0.04 ‡ | 0.67 ± 0.04 | [76] |
| South Korea | 200 | Mean (SD) | 1.67 (0.68) NP | 0.83 (4.23) | [77] |
| 4744 | GM (SD) | 1.06 (0.02) ‡ | 0.89 (0.01) | [78] | |
| Sweden | 4304 | Median (P5, P95) | 1.00 (0.22–2.46) NP | 0.20 (0.09–0.46) | [79] |
| USA | 2325 | GM (95% Cl) | 1.17 (0.77–1.81) NP | 0.86 (0.54–1.36) | [80] |
| 6761 | GM (95% Cl) | 1.02 (0.97–1.06) ‡ 0.39 (0.36–0.41) ‡ | 0.24 (0.24–0.25) 0.20 (0.19–0.21) | [57] | |
| Region (n) | Expression of Cd Concentration | Cd Concentration in the Kidney (μg/g w.w.) | Reference | |
|---|---|---|---|---|
| Australia (61) | Mean ± SD | 15.45 ± 14.04 | [108] | |
| Czech Republic (70) | Mean (95% CI) | 28.7 (6.61–93.0) | [113] | |
| Greenland (95) | Mean ± SD | 15.97 ± 9.26 | [114] | |
| Japan (71) | GM ± GSD | Male, cortex: 72.1 ± 1.7 | Female, cortex: 83.9 ± 2.2 | [115] |
| Male, medulla: 18.3 ± 2.2 | Female, medulla: 24.5 ± 2.1 | |||
| Japan (41) | GM ± SD | Cortex: 82.7 ± 1.99 | Medulla: 36.1 ± 1.99 | [19] |
| Norway (28) | Mean (95% CI) | 20.5 (3.74–62.16) | [116] | |
| Poland (99) | Mean ± SD | 16.0 ± 13.2 | [112] | |
| South Korea (150) | Mean ± SD | 35 ± 18 | [117] | |
| Spain (78) | Mean (95% CI) | 10.8 (6.1–20.2) | [118] | |
| Spain (20) | Mean | 21.15 | [119] | |
| Sweden (10) | Median (95% CI) | 5.18 (2.29–29.99) | [41] | |
| Sweden (109) | Median (range) | 12.9 (1.50–55.0) | [120] | |
| Male: 10.9 (1.6–32.0) | Female: 14.7 (1.50–55.0) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smereczański, N.M.; Brzóska, M.M. Current Levels of Environmental Exposure to Cadmium in Industrialized Countries as a Risk Factor for Kidney Damage in the General Population: A Comprehensive Review of Available Data. Int. J. Mol. Sci. 2023, 24, 8413. https://doi.org/10.3390/ijms24098413
Smereczański NM, Brzóska MM. Current Levels of Environmental Exposure to Cadmium in Industrialized Countries as a Risk Factor for Kidney Damage in the General Population: A Comprehensive Review of Available Data. International Journal of Molecular Sciences. 2023; 24(9):8413. https://doi.org/10.3390/ijms24098413
Chicago/Turabian StyleSmereczański, Nazar M., and Małgorzata M. Brzóska. 2023. "Current Levels of Environmental Exposure to Cadmium in Industrialized Countries as a Risk Factor for Kidney Damage in the General Population: A Comprehensive Review of Available Data" International Journal of Molecular Sciences 24, no. 9: 8413. https://doi.org/10.3390/ijms24098413
APA StyleSmereczański, N. M., & Brzóska, M. M. (2023). Current Levels of Environmental Exposure to Cadmium in Industrialized Countries as a Risk Factor for Kidney Damage in the General Population: A Comprehensive Review of Available Data. International Journal of Molecular Sciences, 24(9), 8413. https://doi.org/10.3390/ijms24098413






