Metabolic Profile and Lipid Metabolism Phenotype in Mice with Conditional Deletion of Hepatic BMAL1
Abstract
1. Introduction
2. Results
2.1. Construction of Hepatocyte-Specific Bmal1 Knockout Mice and the CCG Profile in the Liver
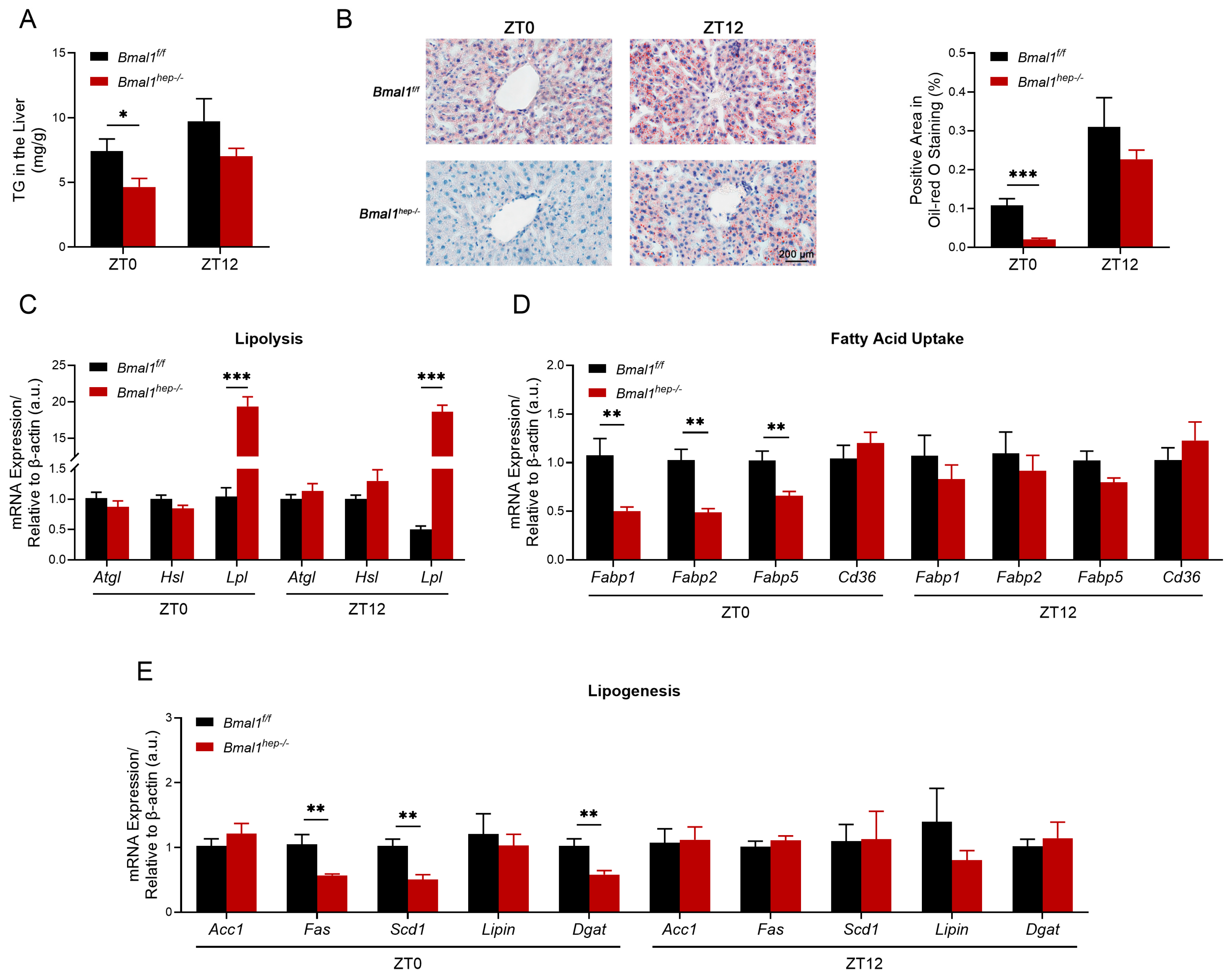
2.2. Profiles of Hepatic Lipid Metabolism in Hepatocyte-Specific Bmal1 Knockout Mice
2.3. Profiles of Hepatic Mitochondrial Function in Hepatocyte-Specific Bmal1 Knockout Mice
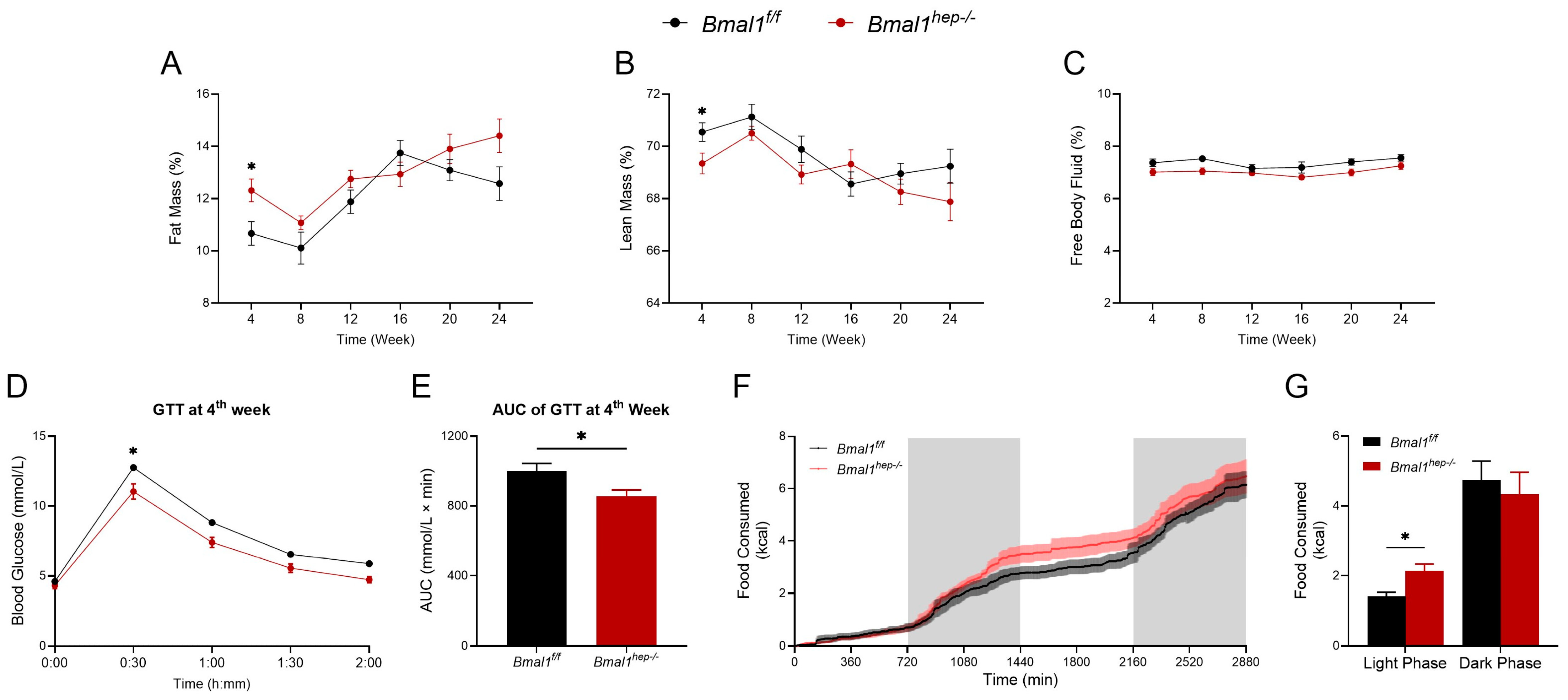
2.4. Profiles of Systemic Metabolism in Hepatocyte-Specific Bmal1 Knockout Mice
3. Discussion
4. Materials and Methods
4.1. Reagents and Antibodies
4.2. Hepatocyte-Specific Bmal1 Knockout Mouse Model
4.3. Protein Extraction and Immunoblotting
4.4. RNA Extraction and Quantitative RT-PCR Analysis
4.5. Measurement of Hepatic TG
4.6. Liver Oil Red O Staining
4.7. Mitochondrial Function Assays (O2K)
- (1)
- Substrates of complex I (2 M pyruvate, 2 M glutamate, and 0.4 M malate, i.e., PGM) were added to maintain stable respiratory values and obtained the leak value of complex I (CI leak).
- (2)
- Substrates of complex I-driven phosphorylating respiration (CI OXPHOS and 2.5 mM ADP) were added to maintain stable respiratory values.
- (3)
- The intactness of the mitochondrial outer membrane was assessed by addition of exogenous 10 uM cytochrome c.
- (4)
- Substrates of complex I- and complex II-driven phosphorylating respiration (CI+CII OXPHOS and 10 mM succinate) were added to maintain stable respiratory values.
- (5)
- Titrating concentrations of the mitochondrial uncoupler 0.1 Mm CCCP was added to reach the maximal, uncoupled respiration (CI+CII electron transfer system, ETS).
- (6)
- To fully inhibit complex I-driven respiration, 1 mM rotenone was added, and complex II-driven uncoupled respiration (CII electron transfer system, CII ETS) was measured.
- (7)
- To block mitochondrial respiration at the level of complex III, 5 mM antimycin A was added.
- (8)
- To measure cytochrome c oxidase (CIV or COX)-driven respiration, 0.8 mM ascorbate and 0.2 Mm TMPD were added.
4.8. Whole-Body Composition Analysis
4.9. Evaluation of Glucose Homeostasis
4.10. Metabolic Assessment
4.11. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barclay, J.L.; Tsang, A.H.; Oster, H. Interaction of central and peripheral clocks in physiological regulation. Prog. Brain Res. 2012, 199, 163–181. [Google Scholar]
- Richards, J.; Gumz, M.L. Advances in understanding the peripheral circadian clocks. FASEB J. 2012, 26, 3602–3613. [Google Scholar] [CrossRef]
- Lamia, K.A.; Storch, K.F.; Weitz, C.J. Physiological significance of a peripheral tissue circadian clock. Proc. Natl. Acad. Sci. USA 2008, 105, 15172–15177. [Google Scholar] [CrossRef]
- Oosterman, J.E.; Kalsbeek, A.; la Fleur, S.E.; Belsham, D.D. Impact of nutrients on circadian rhythmicity. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015, 308, R337–R350. [Google Scholar] [CrossRef]
- Mohawk, J.A.; Green, C.B.; Takahashi, J.S. Central and peripheral circadian clocks in mammals. Annu. Rev. Neurosci. 2012, 35, 445–462. [Google Scholar] [CrossRef]
- Yu, E.A.; Weaver, D.R. Disrupting the circadian clock: Gene-specific effects on aging, cancer, and other phenotypes. Aging 2011, 3, 479–493. [Google Scholar] [CrossRef]
- Jacobi, D.; Liu, S.H.; Burkewitz, K.; Kory, N.; Knudsen, N.H.; Alexander, R.K.; Unluturk, U.; Li, X.B.; Kong, X.H.; Hyde, A.L.; et al. Hepatic Bmal1 Regulates Rhythmic Mitochondrial Dynamics and Promotes Metabolic Fitness. Cell Metab. 2015, 22, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Jouffe, C.; Weger, B.D.; Martin, E.; Atger, F.; Weger, M.; Gobet, C.; Ramnath, D.; Charpagne, A.; Morin-Rivron, D.; Powell, E.E.; et al. Disruption of the circadian clock component BMAL1 elicits an endocrine adaption impacting on insulin sensitivity and liver disease. Proc. Natl. Acad. Sci. USA 2022, 119, e2200083119. [Google Scholar] [CrossRef]
- Guan, D.; Lazar, M.A. Interconnections between circadian clocks and metabolism. J. Clin. Investig. 2021, 131, e148278. [Google Scholar] [CrossRef]
- Pan, X.; Bradfield, C.A.; Hussain, M.M. Global and hepatocyte-specific ablation of Bmal1 induces hyperlipidaemia and enhances atherosclerosis. Nat. Commun. 2016, 7, 13011. [Google Scholar] [CrossRef]
- Lu, Z.; Li, X.; Wang, M.; Zhang, X.; Zhuang, R.; Wu, F.; Li, W.; Zhu, W.; Zhang, B. Liver-Specific Bmal1 Depletion Reverses the Beneficial Effects of Nobiletin on Liver Cholesterol Homeostasis in Mice Fed with High-Fat Diet. Nutrients 2023, 15, 2547. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Wang, Y.; Chen, R.; Gu, W.; Zhang, L.; Gu, J.; Wang, Z.; Liu, Y.; Sun, Q.; Zhang, K.; et al. Ambient fine particulate matter disrupts hepatic circadian oscillation and lipid metabolism in a mouse model. Environ. Pollut. 2020, 262, 114179. [Google Scholar] [CrossRef] [PubMed]
- Rudic, R.D.; McNamara, P.; Curtis, A.M.; Boston, R.C.; Panda, S.; Hogenesch, J.B.; Fitzgerald, G.A. BMAL1 and CLOCK, two essential components of the circadian clock, are involved in glucose homeostasis. PLoS Biol. 2004, 2, e377. [Google Scholar] [CrossRef] [PubMed]
- Chaix, A.; Lin, T.; Le, H.D.; Chang, M.W.; Panda, S. Time-Restricted Feeding Prevents Obesity and Metabolic Syndrome in Mice Lacking a Circadian Clock. Cell Metab. 2019, 29, 303–319.e4. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Tong, X.; Arthurs, B.; Guha, A.; Rui, L.; Kamath, A.; Inoki, K.; Yin, L. Liver clock protein BMAL1 promotes de novo lipogenesis through insulin-mTORC2-AKT signaling. J. Biol. Chem. 2014, 289, 25925–25935. [Google Scholar] [CrossRef] [PubMed]
- Manella, G.; Sabath, E.; Aviram, R.; Dandavate, V.; Ezagouri, S.; Golik, M.; Adamovich, Y.; Asher, G. The liver-clock coordinates rhythmicity of peripheral tissues in response to feeding. Nat. Metab. 2021, 3, 829–842. [Google Scholar] [CrossRef] [PubMed]
- Valcin, J.A.; Udoh, U.S.; Swain, T.M.; Andringa, K.K.; Patel, C.R.; Al Diffalha, S.; Baker, P.R.S.; Gamble, K.L.; Bailey, S.M. Alcohol and Liver Clock Disruption Increase Small Droplet Macrosteatosis, Alter Lipid Metabolism and Clock Gene mRNA Rhythms, and Remodel the Triglyceride Lipidome in Mouse Liver. Front. Physiol. 2020, 11, 1048. [Google Scholar] [CrossRef] [PubMed]
- Reddy, J.K.; Rao, M.S. Lipid metabolism and liver inflammation. II. Fatty liver disease and fatty acid oxidation. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 290, G852–G858. [Google Scholar] [CrossRef]
- Sinturel, F.; Spaleniak, W.; Dibner, C. Circadian rhythm of lipid metabolism. Biochem. Soc. Trans. 2022, 50, 1191–1204. [Google Scholar] [CrossRef] [PubMed]
- Ray, S.; Valekunja, U.K.; Stangherlin, A.; Howell, S.A.; Snijders, A.P.; Damodaran, G.; Reddy, A.B. Circadian rhythms in the absence of the clock gene Bmal1. Science 2020, 367, 800–806. [Google Scholar] [CrossRef]
- Adlanmerini, M.; Lazar, M.A. The REV-ERB Nuclear Receptors: Timekeepers for the Core Clock Period and Metabolism. Endocrinology 2023, 164, bqad069. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Tong, X.; Nelson, B.B.; Jin, E.; Sit, J.; Charney, N.; Yang, M.; Omary, M.B.; Yin, L. The hepatic BMAL1/AKT/lipogenesis axis protects against alcoholic liver disease in mice via promoting PPARα pathway. Hepatology 2018, 68, 883–896. [Google Scholar] [CrossRef]
- Zhan, C.; Chen, H.; Zhang, Z.; Shao, Y.; Xu, B.; Hua, R.; Yao, Q.; Liu, W.; Shen, Q. BMAL1 deletion protects against obesity and non-alcoholic fatty liver disease induced by a high-fat diet. Int. J. Obes. 2024, 48, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Shimba, S.; Ogawa, T.; Hitosugi, S.; Ichihashi, Y.; Nakadaira, Y.; Kobayashi, M.; Tezuka, M.; Kosuge, Y.; Ishige, K.; Ito, Y.; et al. Deficient of a clock gene, brain and muscle Arnt-like protein-1 (BMAL1), induces dyslipidemia and ectopic fat formation. PLoS ONE 2011, 6, e25231. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wei, L.; Zhao, C.; Li, J.; Liu, Z.; Zhang, M.; Wang, Y. Resveratrol Maintains Lipid Metabolism Homeostasis via One of the Mechanisms Associated with the Key Circadian Regulator Bmal1. Molecules 2019, 24, 2916. [Google Scholar] [CrossRef]
- Christofides, A.; Konstantinidou, E.; Jani, C.; Boussiotis, V.A. The role of peroxisome proliferator-activated receptors (PPAR) in immune responses. Metabolism 2021, 114, 154338. [Google Scholar] [CrossRef] [PubMed]
- Morishita, Y.; Miura, D.; Kida, S. PI3K regulates BMAL1/CLOCK-mediated circadian transcription from the Dbp promoter. Biosci. Biotechnol. Biochem. 2016, 80, 1131–1140. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, S.; Liu, T.; Borjigin, J.; Lin, J.D. Transcriptional coactivator PGC-1alpha integrates the mammalian clock and energy metabolism. Nature 2007, 447, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Ye, P.; Li, W.; Huang, X.; Zhao, S.; Chen, W.; Xia, Y.; Yu, W.; Rao, T.; Ning, J.; Zhou, X.; et al. BMAL1 regulates mitochondrial homeostasis in renal ischaemia-reperfusion injury by mediating the SIRT1/PGC-1α axis. J. Cell Mol. Med. 2022, 26, 1994–2009. [Google Scholar] [CrossRef]
- Liu, W.W.; Wei, S.Z.; Huang, G.D.; Liu, L.B.; Gu, C.; Shen, Y.; Wang, X.H.; Xia, S.T.; Xie, A.M.; Hu, L.F.; et al. BMAL1 regulation of microglia-mediated neuroinflammation in MPTP-induced Parkinson’s disease mouse model. FASEB J. 2020, 34, 6570–6581. [Google Scholar] [CrossRef]
- Mortola, J.P. Breathing around the clock: An overview of the circadian pattern of respiration. Eur. J. Appl. Physiol. 2004, 91, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.J.; Phillips, P.M.; Johnstone, A.F. A noninvasive method to study regulation of extracellular fluid volume in rats using nuclear magnetic resonance. Am. J. Physiol. Ren. Physiol. 2016, 310, F426–F431. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Zhang, L.; Qin, L.; Ding, H.; Li, R.; Gu, W.; Chen, R.; Zhang, Y.; Rajagoplan, S.; Zhang, K.; et al. Airborne PM2.5 pollution: A double-edged sword modulating hepatic lipid metabolism in middle-aged male mice. Environ. Pollut. 2023, 324, 121347. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Fonken, L.K.; Wang, A.; Maiseyeu, A.; Bai, Y.; Wang, T.Y.; Maurya, S.; Ko, Y.A.; Periasamy, M.; Dvonch, T.; et al. Central IKKβ inhibition prevents air pollution mediated peripheral inflammation and exaggeration of type II diabetes. Part. Fibre Toxicol. 2014, 11, 53. [Google Scholar] [CrossRef] [PubMed]


| Genes | Forward Primer | Reverse Primer |
|---|---|---|
| Acc1 | AAGGCTATGTGAAGGATG | CTGTCTGAAGAGGTTAGG |
| Acc2 | CTTGCTTCTCTTTCTGACTTG | GGCTTCCACCTTACTGTTG |
| Acox1 | CACGCACATCTTGGATGGTAGTCCG | ACGCTGGCTTCGAGTGAGGAAGTTA |
| Apob | AAACATGCAGAGCTACTTTGGAG | TTTAGGATCACTTCCTGGTCAAA |
| Atgl | GGAGACCAAGTGGAACATCTCA | AATAATGTTGGCACCTGCTTCA |
| Baml1 | GCAGTGCCACTGACTACCAAGA | TCCTGGACATTGCATTGCAT |
| Cd36 | TGGCCTTACTTGGGATTGG | CCAGTGTATATGTAGGCTCATCCA |
| Clock | ACCAACTGACTGGGAGTTTATG | TCTCAAGGAAGCACTGGAAAG |
| Cox5a | TGTCTGTTCCATTCGCTGCT | AGCCCATCGAAGGGAGTTTAC |
| Cpt1α | TGGCCGCATGTCAAGCCAGA | AGGAGAGCAGCACCTTCAGCGA |
| Cry1 | CTGGCGTGGAAGTCATCGT | CTGTCCGCCATTGAGTTCTATG |
| Cry2 | ATGTGTTCCCAAGGCTGTTC | GGTTTCTGCCCATTCAGTTC |
| Dbp1 | ACGCCCTGGCGTTTGCAGAA | TGGCCACTGCTTTTCCGCCT |
| Dgat1 | TGGTGTGTGGTGATGCTGATC | GCCAGGCGCTTCTCAA |
| Dgat2 | AGTGGCAATGCTATCATCATCGT | TCTTCTGGACCCATCGGCCCCAGGA |
| Drp1 | CAGGAATTGTTACGGTTCCCTAA | CCTGAATTAACTTGTCCCGTGA |
| Fabp1 | TCAAGCTGGAAGGTGACAATAA | GTCTCCATTGAGTTCAGTCACG |
| Fabp2 | TCGGTTCCTGAGGATACAAGAT | TTTGATGACTGTGGGATTGAAG |
| Fabp5 | ACAGGGTTTTTGCATTCCTG | TTGGTTCTTTCGAACCTTG |
| Fas | GCGGGTTCGTGAAACTGATAA | GCAAAATGGGCCTCCTTGATA |
| Hsl | CCAGCCTGAGGGCTTACTG | CTCCATTGACTGTGACATCTCG |
| Lipin | CTATGCTGCTTTTGGGAACCG | GGACACTCCCACTTGCTTGT |
| Lpl | TTGCCCTAAGGACCCCTGAA | TTGAAGTGGCAGTTAGACACAG |
| Mfn1 | ATGGCAGAAACGGTATCTCCA | GCCCTCAGTAACAAACTCCAGT |
| Mfn2 | AGAACTGGACCCGGTTACCA | CACTTCGCTGATACCCCTGA |
| Mtco1 | AAGCCTCCTTATTCGAGCCG | GGGGGCACCGATTATTAGGG |
| Mttp | GCTTCCGTTAAAGGTCACACA | TTTGTAGCCCACGCTGTCTT |
| Ndufa1 | CAGGCCCTTGGACACATAGT | GTCCACTGCGTACATCCACA |
| Ndufc1 | CGTAGTGCTGCGCTCGTTT | CTTCGACCGTGTTGAAGAGCAG |
| Ndufs6 | GGGGAAAAGATCACGCATACC | CAAAACGAACCCTCCTGTAGTC |
| Opa1 | TGGAAAATGGTTCGAGAGTCAG | CATTCCGTCTCTAGGTTAAAGCG |
| Per1 | GCCAGGTGTCGTGATTAAATTAGTC | GGGCTTTTGAGGTCTGGATAAA |
| Per2 | CAACAACCCACACACCAAAC | GCGGAATCGAATGGGAGAATA |
| Pgc1α | GAGAATGAGGCAAACTTGCTAGCG | TGCATGGTTCTGAGTGCTAAGACC |
| Pgc1β | AGAGGCACCCAGAGCGAAG | TTGTGGCATGCTGCAAATG |
| Pparα | GCGTACGGCAATGGCTITAT | GAACGGCTTCCTCAGGTTCTT |
| Pparγ | GCACTGCCTATGAGCACTTCA | CCCAAACCTGATGGCATTGTG |
| Rev-erbα | CATGGTGCTACTGTGTAAGGTGTGT | CACAGGCGTGCACTCCATAG |
| Rorα | GCGGTTGACCTCGGCATAT | ACGCTGGACTCTGCTGTTACC |
| Scd1 | CTCATGGTCCTGCTGCACTT | ACGTCATTCTGGAACGCCA |
| Sdhb | TGGATCTGAATAAGTGCGGACC | GCCAGAGTATTGCCTCCGTT |
| Sirt3 | CTACAGCAACCTTCAGCAGTAT | TCACATCAGCCCATATGTCTTC |
| Uqcr10 | TACTCCTTGCTGTTCCGCAG | CCACAGTTTCCCCTCGTTGA |
| Uqcrb | AGGCTTCCTGAGGACCTTTA | TCCTTAGGCAAGATCTGATGC |
| β-actin | TGTGATGGTGGGAATGGGTCAGAA | TGTGGTGCCAGATCTTCTCCATGT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gu, W.; Li, T.; Huang, Y.; Wang, R.; Zhang, L.; Chen, R.; Li, R.; Liu, C. Metabolic Profile and Lipid Metabolism Phenotype in Mice with Conditional Deletion of Hepatic BMAL1. Int. J. Mol. Sci. 2024, 25, 6070. https://doi.org/10.3390/ijms25116070
Gu W, Li T, Huang Y, Wang R, Zhang L, Chen R, Li R, Liu C. Metabolic Profile and Lipid Metabolism Phenotype in Mice with Conditional Deletion of Hepatic BMAL1. International Journal of Molecular Sciences. 2024; 25(11):6070. https://doi.org/10.3390/ijms25116070
Chicago/Turabian StyleGu, Weijia, Ting Li, Yuxin Huang, Ruiqing Wang, Lu Zhang, Rucheng Chen, Ran Li, and Cuiqing Liu. 2024. "Metabolic Profile and Lipid Metabolism Phenotype in Mice with Conditional Deletion of Hepatic BMAL1" International Journal of Molecular Sciences 25, no. 11: 6070. https://doi.org/10.3390/ijms25116070
APA StyleGu, W., Li, T., Huang, Y., Wang, R., Zhang, L., Chen, R., Li, R., & Liu, C. (2024). Metabolic Profile and Lipid Metabolism Phenotype in Mice with Conditional Deletion of Hepatic BMAL1. International Journal of Molecular Sciences, 25(11), 6070. https://doi.org/10.3390/ijms25116070







