The Role of the PAX Genes in Renal Cell Carcinoma
Abstract
1. Introduction
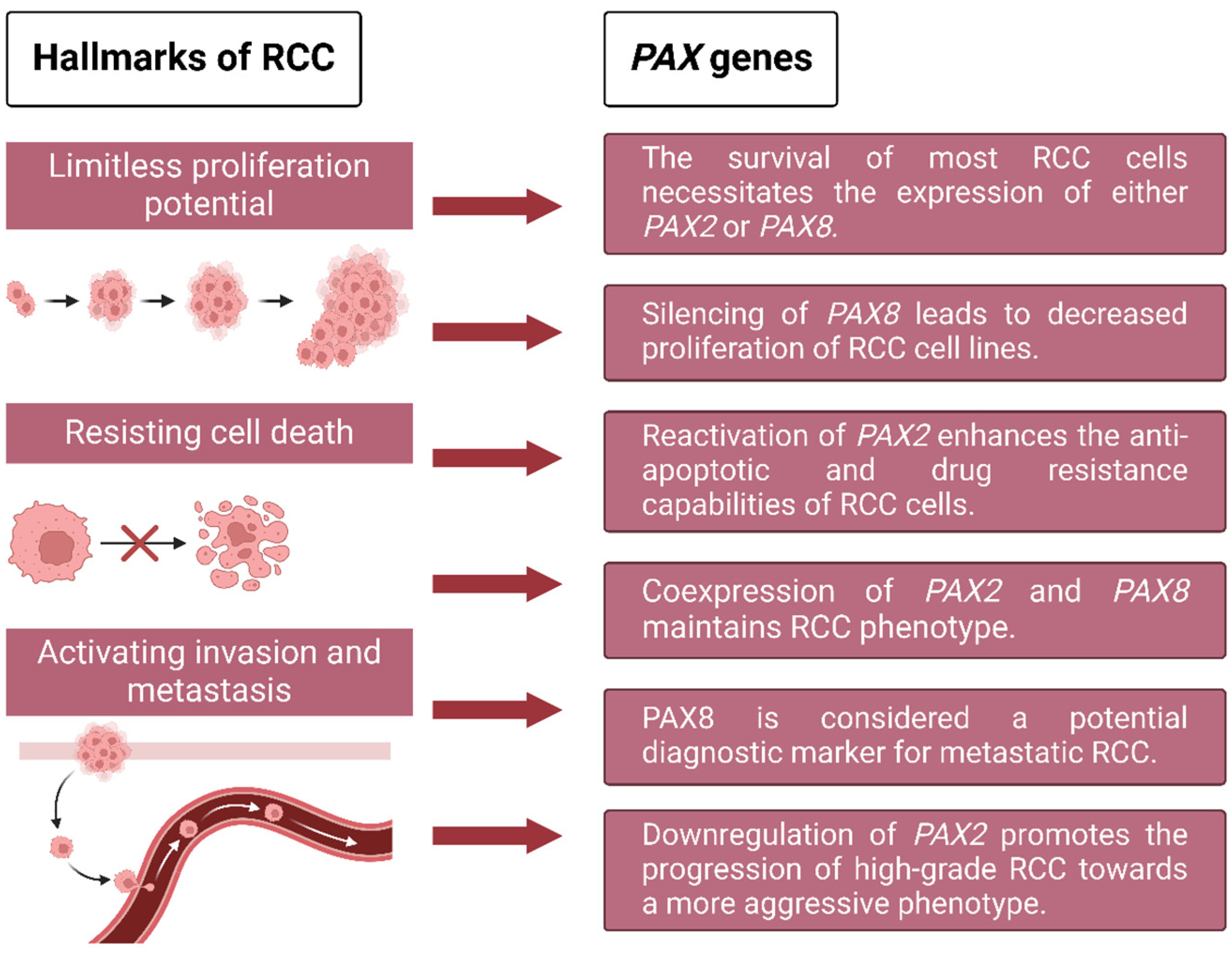
2. Recruitment of PAX Gene Expression Enables Renal Cell Carcinomas to Survive, Proliferate, and Metastasize
2.1. PAX Genes in Renal Cell Carcinoma Survival and Proliferation
2.2. PAX Genes in Renal Cell Carcinoma Metastasis
3. Different Renal Cell Carcinoma Subtypes Are Distinguished by Molecular Features with Various Roles
3.1. Molecular Features of Different Renal Cell Carcinoma Subtypes
3.2. The Role of VHL Loss in Clear Cell Renal Cell Carcinoma
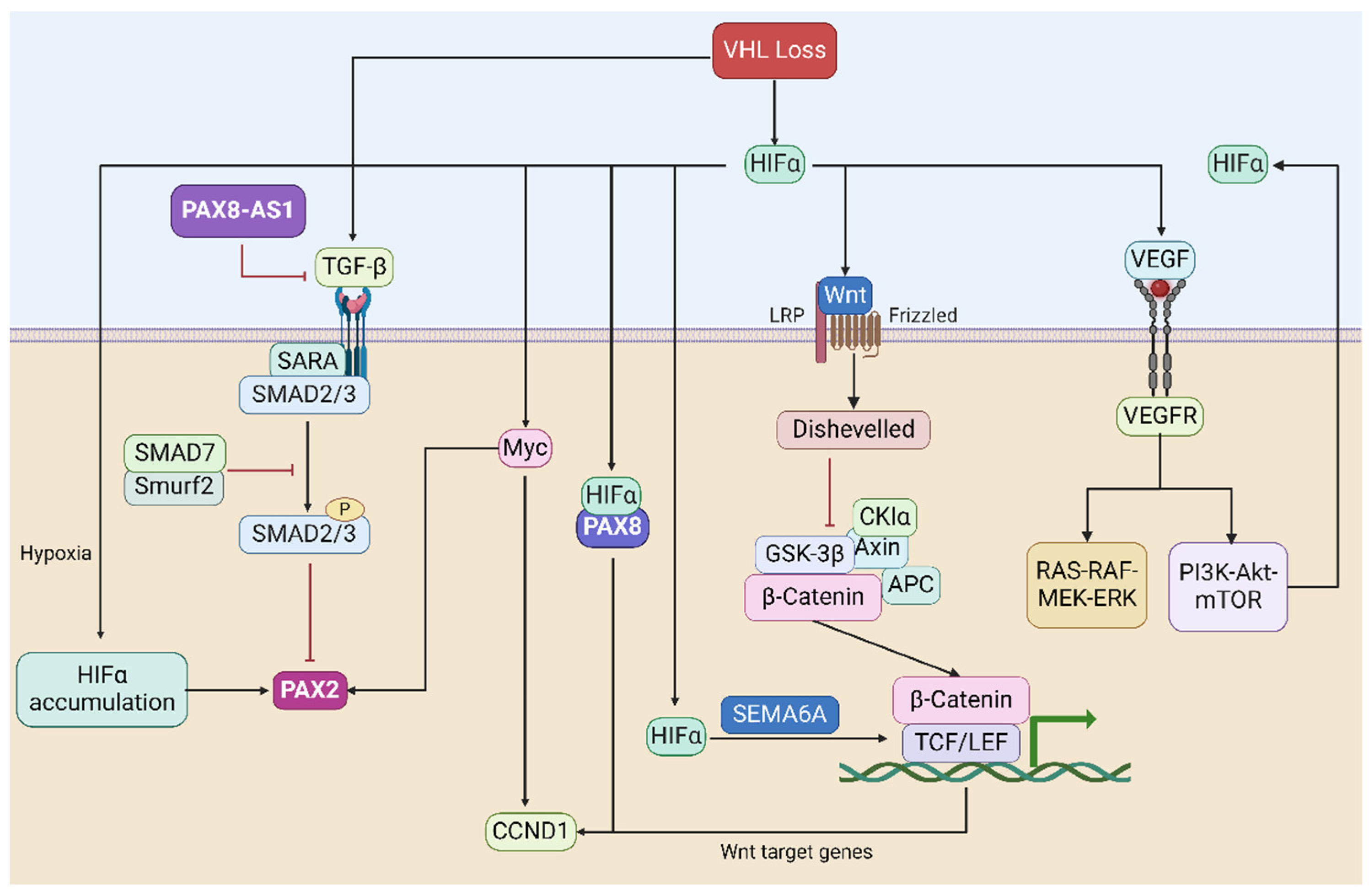
4. Signaling Pathways with Important Roles in Renal Cell Carcinoma and Their Relationship to PAX
4.1. The HIF-Based Hypoxia Signaling Pathway
4.2. The TGF-β Signaling Pathway
4.3. The VEGF-Related Signaling Pathway
4.4. The MYC-Related Signaling Pathway
4.5. The Wnt/β-Catenin Signaling Pathway
5. The Development of PAX-Related Therapeutic Strategies in Renal Cell Carcinoma
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rini, B.I.; Campbell, S.C.; Escudier, B. Renal cell carcinoma. Lancet 2009, 373, 1119–1132. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.W.; Wang, L.; Panian, J.; Dhanji, S.; Derweesh, I.; Rose, B.; Bagrodia, A.; McKay, R.R. Treatment Landscape of Renal Cell Carcinoma. Curr. Treat. Options Oncol. 2023, 24, 1889–1916. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cirillo, L.; Innocenti, S.; Becherucci, F. Global epidemiology of kidney cancer. Nephrol. Dial. Transplant. 2024, 39, 920–928. [Google Scholar] [CrossRef] [PubMed]
- Bukavina, L.; Bensalah, K.; Bray, F.; Carlo, M.; Challacombe, B.; Karam, J.A.; Kassouf, W.; Mitchell, T.; Montironi, R.; O’Brien, T.; et al. Epidemiology of Renal Cell Carcinoma: 2022 Update. Eur. Urol. 2022, 82, 529–542. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, C.G.; Almomani, S.N.; Hossain, S.M.; Eccles, M.R. Co-Expression of Multiple PAX Genes in Renal Cell Carcinoma (RCC) and Correlation of High PAX Expression with Favorable Clinical Outcome in RCC Patients. Int. J. Mol. Sci. 2023, 24, 11432. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Linehan, W.M.; Ricketts, C.J. The Cancer Genome Atlas of renal cell carcinoma: Findings and clinical implications. Nat. Rev. Urol. 2019, 16, 539–552. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Tan, P.; Ishihara, M.; Bayley, N.A.; Schokrpur, S.; Reynoso, J.G.; Zhang, Y.; Lim, R.J.; Dumitras, C.; Yang, L.; et al. Tumor heterogeneity in VHL drives metastasis in clear cell renal cell carcinoma. Signal Transduct. Target. Ther. 2023, 8, 155. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thompson, B.; Davidson, E.A.; Liu, W.; Nebert, D.W.; Bruford, E.A.; Zhao, H.; Dermitzakis, E.T.; Thompson, D.C.; Vasiliou, V. Overview of PAX gene family: Analysis of human tissue-specific variant expression and involvement in human disease. Hum. Genet. 2021, 140, 381–400. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, C.G.; Eccles, M.R. PAX Genes in Cancer; Friends or Foes? Front. Genet. 2012, 3, 6. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bouchard, M.; Souabni, A.; Mandler, M.; Neubüser, A.; Busslinger, M. Nephric lineage specification by Pax2 and Pax8. Genes Dev. 2002, 16, 2958–2970. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Narlis, M.; Grote, D.; Gaitan, Y.; Boualia, S.K.; Bouchard, M. Pax2 and pax8 regulate branching morphogenesis and nephron differentiation in the developing kidney. J. Am. Soc. Nephrol. 2007, 18, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Grimley, E.; Dressler, G.R. Are Pax proteins potential therapeutic targets in kidney disease and cancer? Kidney Int. 2018, 94, 259–267. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, S.R.; Dressler, G.R. The genetics and epigenetics of kidney development. Semin. Nephrol. 2013, 33, 314–326. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kakun, R.R.; Melamed, Z.; Perets, R. PAX8 in the Junction between Development and Tumorigenesis. Int. J. Mol. Sci. 2022, 23, 7410. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gupta, R.; Balzer, B.; Picken, M.; Osunkoya, A.O.; Shet, T.; Alsabeh, R.; Luthringer, D.; Paner, G.P.; Amin, M.B. Diagnostic implications of transcription factor Pax 2 protein and transmembrane enzyme complex carbonic anhydrase IX immunoreactivity in adult renal epithelial neoplasms. Am. J. Surg. Pathol. 2009, 33, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Shaw, T.; Barr, F.G.; Üren, A. The PAX Genes: Roles in Development, Cancer, and Other Diseases. Cancers 2024, 16, 1022. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peters, H.; Wilm, B.; Sakai, N.; Imai, K.; Maas, R.; Balling, R. Pax1 and Pax9 synergistically regulate vertebral column development. Development 1999, 126, 5399–5408. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, M.; Shigetani, Y.; Hirano, S.; Satoh, N.; Kuratani, S. Pax1/Pax9-Related genes in an agnathan vertebrate, Lampetra japonica: Expression pattern of LjPax9 implies sequential evolutionary events toward the gnathostome body plan. Dev. Biol. 2000, 223, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Amiel, J.; Audollent, S.; Joly, D.; Dureau, P.; Salomon, R.; Tellier, A.L.; Augé, J.; Bouissou, F.; Antignac, C.; Gubler, M.C.; et al. PAX2 mutations in renal-coloboma syndrome: Mutational hotspot and germline mosaicism. Eur. J. Hum. Genet. 2000, 8, 820–826. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, A.; de la Roza, G.; Ro, J.Y.; Shen, S.S.; Truong, L.D. PAX2 and PAX8 expression in primary and metastatic renal tumors: A comprehensive comparison. Arch. Pathol. Lab. Med. 2012, 136, 1541–1551. [Google Scholar] [CrossRef] [PubMed]
- Knoepp, S.M.; Kunju, L.P.; Roh, M.H. Utility of PAX8 and PAX2 immunohistochemistry in the identification of renal cell carcinoma in diagnostic cytology. Diagn. Cytopathol. 2012, 40, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Hueber, P.A.; Waters, P.; Clark, P.; Eccles, M.; Goodyer, P. PAX2 inactivation enhances cisplatin-induced apoptosis in renal carcinoma cells. Kidney Int. 2006, 69, 1139–1145, Erratum in Kidney Int. 2006, 70, 1666. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Cui, S.; Li, W.; Zhao, Y.; Yan, X.; Xu, J. PAX3 is a biomarker and prognostic factor in melanoma: Database mining. Oncol. Lett. 2019, 17, 4985–4993. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ko, J.; Fonseca, V.A.; Wu, H. Pax4 in Health and Diabetes. Int. J. Mol. Sci. 2023, 24, 8283. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nasri Nasrabadi, P.; Martin, D.; Gharib, E.; Robichaud, G.A. The Pleiotropy of PAX5 Gene Products and Function. Int. J. Mol. Sci. 2022, 23, 10095. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Azuma, N.; Yamaguchi, Y.; Handa, H.; Tadokoro, K.; Asaka, A.; Kawase, E.; Yamada, M. Mutations of the PAX6 gene detected in patients with a variety of optic-nerve malformations. Am. J. Hum. Genet. 2003, 72, 1565–1570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bleu, M.; Gaulis, S.; Lopes, R.; Sprouffske, K.; Apfel, V.; Holwerda, S.; Pregnolato, M.; Yildiz, U.; Cordo’, V.; Dost, A.F.M.; et al. PAX8 activates metabolic genes via enhancer elements in Renal Cell Carcinoma. Nat. Commun. 2019, 10, 3739. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wachtel, M.; Schäfer, B.W. Unpeaceful roles of mutant PAX proteins in cancer. Semin. Cell Dev. Biol. 2015, 44, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Dumont, S.N.; Lazar, A.J.; Bridge, J.A.; Benjamin, R.S.; Trent, J.C. PAX3/7-FOXO1 fusion status in older rhabdomyosarcoma patient population by fluorescent in situ hybridization. J. Cancer Res. Clin. Oncol. 2012, 138, 213–220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sorensen, P.H.; Lynch, J.C.; Qualman, S.J.; Tirabosco, R.; Lim, J.F.; Maurer, H.M.; Bridge, J.A.; Crist, W.M.; Triche, T.J.; Barr, F.G. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: A report from the children’s oncology group. J. Clin. Oncol. 2002, 20, 2672–2679. [Google Scholar] [CrossRef] [PubMed]
- Hueber, P.A.; Iglesias, D.; Chu, L.L.; Eccles, M.; Goodyer, P. In vivo validation of PAX2 as a target for renal cancer therapy. Cancer Lett. 2008, 265, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Robson, E.J.; He, S.J.; Eccles, M.R. A PANorama of PAX genes in cancer and development. Nat. Rev. Cancer 2006, 6, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Muratovska, A.; Zhou, C.; He, S.; Goodyer, P.; Eccles, M.R. Paired-Box genes are frequently expressed in cancer and often required for cancer cell survival. Oncogene 2003, 22, 7989–7997. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R.; Ranghini, E.; Dressler, G.R. Mechanisms of gene activation and repression by Pax proteins in the developing kidney. Pediatr. Nephrol. 2014, 29, 589–595. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Sharma, R.; Sanchez-Ferras, O.; Bouchard, M. Pax genes in renal development, disease and regeneration. Semin. Cell Dev. Biol. 2015, 44, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.S.; Jiang, T.; Huang, B.; Chen, P.S.; Ouyang, J. Epithelial-mesenchymal transition of renal tubules: Divergent processes of repairing in acute or chronic injury? Med. Hypotheses 2013, 81, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Buttiglieri, S.; Deregibus, M.C.; Bravo, S.; Cassoni, P.; Chiarle, R.; Bussolati, B.; Camussi, G. Role of Pax2 in apoptosis resistance and proinvasive phenotype of Kaposi’s sarcoma cells. J. Biol. Chem. 2004, 279, 4136–4143. [Google Scholar] [CrossRef] [PubMed]
- Brun, T.; Duhamel, D.L.; Hu He, K.H.; Wollheim, C.B.; Gauthier, B.R. The transcription factor PAX4 acts as a survival gene in INS-1E insulinoma cells. Oncogene 2007, 26, 4261–4271. [Google Scholar] [CrossRef] [PubMed]
- Shi, K.; Yin, X.; Cai, M.C.; Yan, Y.; Jia, C.; Ma, P.; Zhang, S.; Zhang, Z.; Gu, Z.; Zhang, M.; et al. PAX8 regulon in human ovarian cancer links lineage dependency with epigenetic vulnerability to HDAC inhibitors. eLife 2019, 8, e44306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Doberstein, K.; Pfeilschifter, J.; Gutwein, P. The transcription factor PAX2 regulates ADAM10 expression in renal cell carcinoma. Carcinogenesis 2011, 32, 1713–1723. [Google Scholar] [CrossRef] [PubMed]
- Di Palma, T.; Filippone, M.G.; Pierantoni, G.M.; Fusco, A.; Soddu, S.; Zannini, M. Pax8 has a critical role in epithelial cell survival and proliferation. Cell Death Dis. 2013, 4, e729. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, J.; Zhao, X.; Qi, J.; Yang, C.; Cheng, H.; Ren, Y.; Huang, L. Eight proteins play critical roles in RCC with bone metastasis via mitochondrial dysfunction. Clin. Exp. Metastasis 2015, 32, 605–622. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hoefflin, R.; Harlander, S.; Schäfer, S.; Metzger, P.; Kuo, F.; Schönenberger, D.; Adlesic, M.; Peighambari, A.; Seidel, P.; Chen, C.Y.; et al. HIF-1α and HIF-2α differently regulate tumour development and inflammation of clear cell renal cell carcinoma in mice. Nat. Commun. 2020, 11, 4111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stuart, E.T.; Haffner, R.; Oren, M.; Gruss, P. Loss of p53 function through PAX-mediated transcriptional repression. EMBO J. 1995, 14, 5638–5645. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frost, V.; Grocott, T.; Eccles, M.R.; Chantry, A. Self-regulated Pax gene expression and modulation by the TGFbeta superfamily. Crit. Rev. Biochem. Mol. Biol. 2008, 43, 371–391. [Google Scholar] [CrossRef] [PubMed]
- Pei, D.; Shu, X.; Gassama-Diagne, A.; Thiery, J.P. Mesenchymal-epithelial transition in development and reprogramming. Nat. Cell Biol. 2019, 21, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Harada, K.; Miyake, H.; Kusuda, Y.; Fujisawa, M. Expression of epithelial-mesenchymal transition markers in renal cell carcinoma: Impact on prognostic outcomes in patients undergoing radical nephrectomy. BJU Int. 2012, 110 Pt C, E1131–E1137. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Li, C.G.; Chantry, A.; Stayner, C.; Horsfield, J.; Eccles, M.R. SMAD proteins directly suppress PAX2 transcription downstream of transforming growth factor-beta 1 (TGF-β1) signalling in renal cell carcinoma. Oncotarget 2018, 9, 26852–26867. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mazal, P.R.; Stichenwirth, M.; Koller, A.; Blach, S.; Haitel, A.; Susani, M. Expression of aquaporins and PAX-2 compared to CD10 and cytokeratin 7 in renal neoplasms: A tissue microarray study. Mod. Pathol. 2005, 18, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Truong, L.D.; Shen, S.S. Immunohistochemical diagnosis of renal neoplasms. Arch. Pathol. Lab. Med. 2011, 135, 92–109. [Google Scholar] [CrossRef] [PubMed]
- Grote, D.; Souabni, A.; Busslinger, M.; Bouchard, M. Pax 2/8-regulated Gata 3 expression is necessary for morphogenesis and guidance of the nephric duct in the developing kidney. Development 2006, 133, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Boualia, S.K.; Gaitan, Y.; Tremblay, M.; Sharma, R.; Cardin, J.; Kania, A.; Bouchard, M. A core transcriptional network composed of Pax2/8, Gata3 and Lim1 regulates key players of pro/mesonephros morphogenesis. Dev. Biol. 2013, 382, 555–566. [Google Scholar] [CrossRef] [PubMed]
- Salvi, A.; Hardy, L.R.; Heath, K.N.; Watry, S.; Pergande, M.R.; Cologna, S.M.; Burdette, J.E. PAX8 modulates the tumor microenvironment of high grade serous ovarian cancer through changes in the secretome. Neoplasia 2023, 36, 100866. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aili, A.; Wen, J.; Xue, L.; Wang, J. Mutational Analysis of PBRM1 and Significance of PBRM1 Mutation in Anti-PD-1 Immunotherapy of Clear Cell Renal Cell Carcinoma. Front. Oncol. 2021, 11, 712765. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gu, X.; Enane, F.; Tohme, R.; Schuerger, C.; Radivoyevitch, T.; Parker, Y.; Zuberi, E.; Przychodzen, B.; Jha, B.K.; Lindner, D.; et al. PBRM1 loss in kidney cancer unbalances the proximal tubule master transcription factor hub to repress proximal tubule differentiation. Cell Rep. 2021, 36, 109747. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jiang, F.; Richter, J.; Schraml, P.; Bubendorf, L.; Gasser, T.; Sauter, G.; Mihatsch, M.J.; Moch, H. Chromosomal imbalances in papillary renal cell carcinoma: Genetic differences between histological subtypes. Am. J. Pathol. 1998, 153, 1467–1473. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Durinck, S.; Stawiski, E.W.; Pavía-Jiménez, A.; Modrusan, Z.; Kapur, P.; Jaiswal, B.S.; Zhang, N.; Toffessi-Tcheuyap, V.; Nguyen, T.T.; Pahuja, K.B.; et al. Spectrum of diverse genomic alterations define non-clear cell renal carcinoma subtypes. Nat. Genet. 2015, 47, 13–21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cancer Genome Atlas Research Network; Linehan, W.M.; Spellman, P.T.; Ricketts, C.J.; Creighton, C.J.; Fei, S.S.; Davis, C.; Wheeler, D.A.; Murray, B.A.; Schmidt, L.; et al. Comprehensive Molecular Characterization of Papillary Renal-Cell Carcinoma. N. Engl. J. Med. 2016, 374, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Casuscelli, J.; Weinhold, N.; Gundem, G.; Wang, L.; Zabor, E.C.; Drill, E.; Wang, P.I.; Nanjangud, G.J.; Redzematovic, A.; Nargund, A.M.; et al. Genomic landscape and evolution of metastatic chromophobe renal cell carcinoma. JCI Insight 2017, 2, e92688. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Speicher, M.R.; Schoell, B.; du Manoir, S.; Schröck, E.; Ried, T.; Cremer, T.; Störkel, S.; Kovacs, A.; Kovacs, G. Specific loss of chromosomes 1, 2, 6, 10, 13, 17, and 21 in chromophobe renal cell carcinomas revealed by comparative genomic hybridization. Am. J. Pathol. 1994, 145, 356–364. [Google Scholar] [PubMed] [PubMed Central]
- Davis, C.F.; Ricketts, C.J.; Wang, M.; Yang, L.; Cherniack, A.D.; Shen, H.; Buhay, C.; Kang, H.; Kim, S.C.; Fahey, C.C.; et al. The somatic genomic landscape of chromophobe renal cell carcinoma. Cancer Cell 2014, 26, 319–330. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mitchell, T.J.; Turajlic, S.; Rowan, A.; Nicol, D.; Farmery, J.H.R.; O’Brien, T.; Martincorena, I.; Tarpey, P.; Angelopoulos, N.; Yates, L.R.; et al. TRACERx Renal Consortium. Timing the Landmark Events in the Evolution of Clear Cell Renal Cell Cancer: TRACERx Renal. Cell 2018, 173, 611–623.e17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El-Mokadem, I.; Fitzpatrick, J.; Bondad, J.; Rauchhaus, P.; Cunningham, J.; Pratt, N.; Fleming, S.; Nabi, G. Chromosome 9p deletion in clear cell renal cell carcinoma predicts recurrence and survival following surgery. Br. J. Cancer 2014, 111, 1381–1390. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dalgliesh, G.L.; Furge, K.; Greenman, C.; Chen, L.; Bignell, G.; Butler, A.; Davies, H.; Edkins, S.; Hardy, C.; Latimer, C.; et al. Systematic sequencing of renal carcinoma reveals inactivation of histone modifying genes. Nature 2010, 463, 360–363. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brannon, A.R.; Reddy, A.; Seiler, M.; Arreola, A.; Moore, D.T.; Pruthi, R.S.; Wallen, E.M.; Nielsen, M.E.; Liu, H.; Nathanson, K.L.; et al. Molecular Stratification of Clear Cell Renal Cell Carcinoma by Consensus Clustering Reveals Distinct Subtypes and Survival Patterns. Genes Cancer 2010, 1, 152–163. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bihr, S.; Ohashi, R.; Moore, A.L.; Rüschoff, J.H.; Beisel, C.; Hermanns, T.; Mischo, A.; Corrò, C.; Beyer, J.; Beerenwinkel, N.; et al. Expression and Mutation Patterns of PBRM1, BAP1 and SETD2 Mirror Specific Evolutionary Subtypes in Clear Cell Renal Cell Carcinoma. Neoplasia 2019, 21, 247–256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brugarolas, J. PBRM1 and BAP1 as novel targets for renal cell carcinoma. Cancer J. 2013, 19, 324–332. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mazumder, S.; Higgins, P.J.; Samarakoon, R. Downstream Targets of VHL/HIF-α Signaling in Renal Clear Cell Carcinoma Progression: Mechanisms and Therapeutic Relevance. Cancers 2023, 15, 1316. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, J.; Zhang, Q. VHL and Hypoxia Signaling: Beyond HIF in Cancer. Biomedicines 2018, 6, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaelin, W.G., Jr. The von Hippel-Lindau tumor suppressor protein and clear cell renal carcinoma. Clin. Cancer Res. 2007, 13 Pt 2, 680s–684s. [Google Scholar] [CrossRef] [PubMed]
- Lonser, R.R.; Glenn, G.M.; Walther, M.; Chew, E.Y.; Libutti, S.K.; Linehan, W.M.; Oldfield, E.H. von Hippel-Lindau disease. Lancet 2003, 361, 2059–2067. [Google Scholar] [CrossRef] [PubMed]
- Iwai, K.; Yamanaka, K.; Kamura, T.; Minato, N.; Conaway, R.C.; Conaway, J.W.; Klausner, R.D.; Pause, A. Identification of the von Hippel-lindau tumor-suppressor protein as part of an active E3 ubiquitin ligase complex. Proc. Natl. Acad. Sci. USA 1999, 96, 12436–12441. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Siemeister, G.; Weindel, K.; Mohrs, K.; Barleon, B.; Martiny-Baron, G.; Marmé, D. Reversion of deregulated expression of vascular endothelial growth factor in human renal carcinoma cells by von Hippel-Lindau tumor suppressor protein. Cancer Res. 1996, 56, 2299–2301. [Google Scholar] [PubMed]
- Gudas, L.J.; Fu, L.; Minton, D.R.; Mongan, N.P.; Nanus, D.M. The role of HIF1α in renal cell carcinoma tumorigenesis. J. Mol. Med. 2014, 92, 825–836. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kamura, T.; Sato, S.; Iwai, K.; Czyzyk-Krzeska, M.; Conaway, R.C.; Conaway, J.W. Activation of HIF1alpha ubiquitination by a reconstituted von Hippel-Lindau (VHL) tumor suppressor complex. Proc. Natl. Acad. Sci. USA 2000, 97, 10430–10435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raval, R.R.; Lau, K.W.; Tran, M.G.; Sowter, H.M.; Mandriota, S.J.; Li, J.L.; Pugh, C.W.; Maxwell, P.H.; Harris, A.L.; Ratcliffe, P.J. Contrasting properties of hypoxia-inducible factor 1 (HIF-1) and HIF-2 in von Hippel-Lindau-associated renal cell carcinoma. Mol. Cell Biol. 2005, 25, 5675–5686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Perrotta, S.; Roberti, D.; Bencivenga, D.; Corsetto, P.; O’Brien, K.A.; Caiazza, M.; Stampone, E.; Allison, L.; Fleck, R.A.; Scianguetta, S.; et al. Effects of Germline VHL Deficiency on Growth, Metabolism, and Mitochondria. N. Engl. J. Med. 2020, 382, 835–844. [Google Scholar] [CrossRef] [PubMed]
- Brand, M.D.; Nicholls, D.G. Assessing mitochondrial dysfunction in cells. Biochem. J. 2011, 435, 297–312, Erratum in Biochem. J. 2011, 437, 575. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Z.; Ying, Z.; Bosy-Westphal, A.; Zhang, J.; Schautz, B.; Later, W.; Heymsfield, S.B.; Müller, M.J. Specific metabolic rates of major organs and tissues across adulthood: Evaluation by mechanistic model of resting energy expenditure. Am. J. Clin. Nutr. 2010, 92, 1369–1377. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lunt, S.Y.; Vander Heiden, M.G. Aerobic glycolysis: Meeting the metabolic requirements of cell proliferation. Annu. Rev. Cell Dev. Biol. 2011, 27, 441–464. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, B.; Arige, V.; Khan, A.A.; Reddy, S.S.; Barthwal, M.K.; Mahapatra, N.R. Hypoxia-mediated regulation of mitochondrial transcription factors in renal epithelial cells: Implications for hypertensive renal physiology. Hypertens. Res. 2021, 44, 154–167. [Google Scholar] [CrossRef] [PubMed]
- Szeto, H.H.; Liu, S.; Soong, Y.; Seshan, S.V.; Cohen-Gould, L.; Manichev, V.; Feldman, L.C.; Gustafsson, T. Mitochondria Protection after Acute Ischemia Prevents Prolonged Upregulation of IL-1β and IL-18 and Arrests CKD. J. Am. Soc. Nephrol. 2017, 28, 1437–1449. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, O.C.; Maxwell, P.H.; Pollard, P.J. Renal cell carcinoma: Translational aspects of metabolism and therapeutic consequences. Kidney Int. 2013, 84, 667–681. [Google Scholar] [CrossRef] [PubMed]
- Fukushi, A.; Kim, H.D.; Chang, Y.C.; Kim, C.H. Revisited Metabolic Control and Reprogramming Cancers by Means of the Warburg Effect in Tumor Cells. Int. J. Mol. Sci. 2022, 23, 10037. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Koppenol, W.H.; Bounds, P.L.; Dang, C.V. Otto Warburg’s contributions to current concepts of cancer metabolism. Nat. Rev. Cancer 2011, 11, 325–337, Erratum in Nat. Rev. Cancer 2011, 11, 618. [Google Scholar] [CrossRef] [PubMed]
- Hervouet, E.; Simonnet, H.; Godinot, C. Mitochondria and reactive oxygen species in renal cancer. Biochimie 2007, 89, 1080–1088. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Li, W.; Yuan, J.; Bullova, P.; Wu, J.; Zhang, X.; Liu, Y.; Plescher, M.; Rodriguez, J.; Bedoya-Reina, O.C.; et al. Impaired oxygen-sensitive regulation of mitochondrial biogenesis within the von Hippel-Lindau syndrome. Nat. Metab. 2022, 4, 739–758, Erratum in Nat. Metab. 2022, 4, 1421. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lu, J.; Tan, M.; Cai, Q. The Warburg effect in tumor progression: Mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett. 2015, 356 Pt A, 156–164. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chinopoulos, C.; Seyfried, T.N. Mitochondrial Substrate-Level Phosphorylation as Energy Source for Glioblastoma: Review and Hypothesis. ASN Neuro 2018, 10, 1759091418818261. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Banumathy, G.; Cairns, P. Signaling pathways in renal cell carcinoma. Cancer Biol. Ther. 2010, 10, 658–664. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schödel, J.; Grampp, S.; Maher, E.R.; Moch, H.; Ratcliffe, P.J.; Russo, P.; Mole, D.R. Hypoxia, Hypoxia-inducible Transcription Factors, and Renal Cancer. Eur. Urol. 2016, 69, 646–657. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Luu, V.D.; Boysen, G.; Struckmann, K.; Casagrande, S.; von Teichman, A.; Wild, P.J.; Sulser, T.; Schraml, P.; Moch, H. Loss of VHL and hypoxia provokes PAX2 up-regulation in clear cell renal cell carcinoma. Clin. Cancer Res. 2009, 15, 3297–3304. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, P.H.; Wiesener, M.S.; Chang, G.W.; Clifford, S.C.; Vaux, E.C.; Cockman, M.E.; Wykoff, C.C.; Pugh, C.W.; Maher, E.R.; Ratcliffe, P.J. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 1999, 399, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Ivan, M.; Kondo, K.; Yang, H.; Kim, W.; Valiando, J.; Ohh, M.; Salic, A.; Asara, J.M.; Lane, W.S.; Kaelin, W.G., Jr. HIFalpha targeted for VHL-mediated destruction by proline hydroxylation: Implications for O2 sensing. Science 2001, 292, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Isono, T.; Chano, T.; Yoshida, T.; Kageyama, S.; Kawauchi, A.; Suzaki, M.; Yuasa, T. Hydroxyl-HIF2-alpha is potential therapeutic target for renal cell carcinomas. Am. J. Cancer Res. 2016, 6, 2263–2276. [Google Scholar] [PubMed] [PubMed Central]
- Gao, S.L.; Yin, R.; Zhang, L.F.; Wang, S.M.; Chen, J.S.; Wu, X.Y.; Yue, C.; Zuo, L.; Tang, M. The oncogenic role of MUC12 in RCC progression depends on c-Jun/TGF-β signalling. J. Cell Mol. Med. 2020, 24, 8789–8802. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peng, D.; Fu, M.; Wang, M.; Wei, Y.; Wei, X. Targeting TGF-β signal transduction for fibrosis and cancer therapy. Mol. Cancer 2022, 21, 104. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tretbar, S.; Krausbeck, P.; Müller, A.; Friedrich, M.; Vaxevanis, C.; Bukur, J.; Jasinski-Bergner, S.; Seliger, B. TGF-β inducible epithelial-to-mesenchymal transition in renal cell carcinoma. Oncotarget 2019, 10, 1507–1524. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hanna, C.; Hubchak, S.C.; Liang, X.; Rozen-Zvi, B.; Schumacker, P.T.; Hayashida, T.; Schnaper, H.W. Hypoxia-inducible factor-2α and TGF-β signaling interact to promote normoxic glomerular fibrogenesis. Am. J. Physiol. Renal Physiol. 2013, 305, F1323–F1331. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Han, J.; Zhou, W.; Jia, M.; Wen, J.; Jiang, J.; Shi, J.; Zhang, K.; Ma, H.; Liu, J.; Ren, J.; et al. Expression quantitative trait loci in long non-coding RNA PAX8-AS1 are associated with decreased risk of cervical cancer. Mol. Genet. Genom. 2016, 291, 1743–1748. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Xu, T.; Hu, H.; Hua, F. Overexpression of PAX8-AS1 Inhibits Malignant Phenotypes of Papillary Thyroid Carcinoma Cells via miR-96-5p/PKN2 Axis. Int. J. Endocrinol. 2021, 2021, 5499963. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, Y.; Tong, Z.W.; Zhou, Y.; Sun, Y.; Xie, Y.; Li, R.; Liu, H. Inhibition of lncRNA-PAX8-AS1-N directly associated with VEGF/TGF-β1/8-OhdG enhances podocyte apoptosis in diabetic nephropathy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 6864–6872. [Google Scholar] [CrossRef] [PubMed]
- Shang, D.; Liu, Y.; Yang, P.; Chen, Y.; Tian, Y. TGFBI-promoted adhesion, migration and invasion of human renal cell carcinoma depends on inactivation of von Hippel-Lindau tumor suppressor. Urology 2012, 79, 966.e1–966.e7. [Google Scholar] [CrossRef] [PubMed]
- Siveen, K.S.; Prabhu, K.; Krishnankutty, R.; Kuttikrishnan, S.; Tsakou, M.; Alali, F.Q.; Dermime, S.; Mohammad, R.M.; Uddin, S. Vascular Endothelial Growth Factor (VEGF) Signaling in Tumour Vascularization: Potential and Challenges. Curr. Vasc. Pharmacol. 2017, 15, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Du, X.; Rizzi, J.P.; Liberzon, E.; Chakraborty, A.A.; Gao, W.; Carvo, I.; Signoretti, S.; Bruick, R.K.; Josey, J.A.; et al. On-target efficacy of a HIF-2α antagonist in preclinical kidney cancer models. Nature 2016, 539, 107–111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mei, X.; Shu, J.; Huang, R.; Chu, X.; Tian, Y. Expression of VEGF, CD73 and their relationship with clinical pathology, microvessel density, and prognosis in renal cell carcinoma. Transl. Androl. Urol. 2020, 9, 1366–1373. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Lu, Y.H.; Tang, C.; Xue, M.; Li, X.Y.; Chang, Y.P.; Cheng, Y.; Li, T.; Yu, X.C.; Sun, B.; et al. Calcium Dobesilate Restores Autophagy by Inhibiting the VEGF/PI3K/AKT/mTOR Signaling Pathway. Front. Pharmacol. 2019, 10, 886. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Su, C.C. Tanshinone IIA inhibits gastric carcinoma AGS cells by decreasing the protein expression of VEGFR and blocking Ras/Raf/MEK/ERK pathway. Int. J. Mol. Med. 2018, 41, 2389–2396. [Google Scholar] [CrossRef] [PubMed]
- Fonsato, V.; Buttiglieri, S.; Deregibus, M.C.; Puntorieri, V.; Bussolati, B.; Camussi, G. Expression of Pax2 in human renal tumor-derived endothelial cells sustains apoptosis resistance and angiogenesis. Am. J. Pathol. 2006, 168, 706–713. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chaves-Moreira, D.; Mitchell, M.A.; Arruza, C.; Rawat, P.; Sidoli, S.; Nameki, R.; Reddy, J.; Corona, R.I.; Afeyan, L.K.; Klein, I.A.; et al. The transcription factor PAX8 promotes angiogenesis in ovarian cancer through interaction with SOX17. Sci. Signal. 2022, 15, eabm2496. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baluapuri, A.; Wolf, E.; Eilers, M. Target gene-independent functions of MYC oncoproteins. Nat. Rev. Mol. Cell Biol. 2020, 21, 255–267. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Solé, X.; Hernández, P.; de Heredia, M.L.; Armengol, L.; Rodríguez-Santiago, B.; Gómez, L.; Maxwell, C.A.; Aguiló, F.; Condom, E.; Abril, J.; et al. Genetic and genomic analysis modeling of germline c-MYC overexpression and cancer susceptibility. BMC Genom. 2008, 9, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hwang, I.Y.; Roe, J.S.; Seol, J.H.; Kim, H.R.; Cho, E.J.; Youn, H.D. pVHL-mediated transcriptional repression of c-Myc by recruitment of histone deacetylases. Mol. Cells. 2012, 33, 195–201. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, S.L.; Chen, Y.W.; Tran, S.; Liu, F.; Nestoridi, E.; Hébert, M.J.; Ingelfinger, J.R. Pax-2 and N-myc regulate epithelial cell proliferation and apoptosis in a positive autocrine feedback loop. Pediatr. Nephrol. 2007, 22, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Gordan, J.D.; Lal, P.; Dondeti, V.R.; Letrero, R.; Parekh, K.N.; Oquendo, C.E.; Greenberg, R.A.; Flaherty, K.T.; Rathmell, W.K.; Keith, B.; et al. HIF-alpha effects on c-Myc distinguish two subtypes of sporadic VHL-deficient clear cell renal carcinoma. Cancer Cell 2008, 14, 435–446. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gordan, J.D.; Thompson, C.B.; Simon, M.C. HIF and c-Myc: Sibling rivals for control of cancer cell metabolism and proliferation. Cancer Cell 2007, 12, 108–113. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, H.; Gao, P.; Fukuda, R.; Kumar, G.; Krishnamachary, B.; Zeller, K.I.; Dang, C.V.; Semenza, G.L. HIF-1 inhibits mitochondrial biogenesis and cellular respiration in VHL-deficient renal cell carcinoma by repression of C-MYC activity. Cancer Cell 2007, 11, 407–420. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Xu, T.; Xie, T.; Yang, L.; Wang, G.; Gao, Y.; Xi, G.; Zhang, X. CDC42EP3 promotes glioma progression via regulation of CCND1. Cell Death Dis. 2022, 13, 290. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, T.; Niu, X.; Liao, L.; Cho, E.A.; Yang, H. The contributions of HIF-target genes to tumor growth in RCC. PLoS ONE 2013, 8, e80544. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, S.A.; Hirosue, S.; Rodrigues, P.; Vojtasova, E.; Richardson, E.K.; Ge, J.; Syafruddin, S.E.; Speed, A.; Papachristou, E.K.; Baker, D.; et al. The renal lineage factor PAX8 controls oncogenic signalling in kidney cancer. Nature 2022, 606, 999–1006. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miller, J.R. The Wnts. Genome Biol. 2002, 3, REVIEWS3001. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ji, J.; Xu, Y.; Xie, M.; He, X.; Ren, D.; Qiu, T.; Liu, W.; Chen, Z.; Shi, W.; Zhang, Z.; et al. VHL-HIF-2α axis-induced SEMA6A upregulation stabilized β-catenin to drive clear cell renal cell carcinoma progression. Cell Death Dis. 2023, 14, 83. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kruck, S.; Eyrich, C.; Scharpf, M.; Sievert, K.D.; Fend, F.; Stenzl, A.; Bedke, J. Impact of an altered Wnt1/β-catenin expression on clinicopathology and prognosis in clear cell renal cell carcinoma. Int. J. Mol. Sci. 2013, 14, 10944–10957. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, L.; Gong, L. Impact of WNT Pathway Blockade on the Biological Characteristics of Renal Tubular Epithelial Cells Stably Transfected with PAX2. Ann. Clin. Lab. Sci. 2021, 51, 368–375. [Google Scholar] [PubMed]
- Nusse, R.; Clevers, H. Wnt/β-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell 2017, 169, 985–999. [Google Scholar] [CrossRef] [PubMed]
- Piotrowska, Ż.; Niezgoda, M.; Młynarczyk, G.; Acewicz, M.; Kasacka, I. Comparative Assessment of the WNT/β-Catenin Pathway, CacyBP/SIP, and the Immunoproteasome Subunit LMP7 in Various Histological Types of Renal Cell Carcinoma. Front. Oncol. 2020, 10, 566637. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, C.M.; Ji, S.; Li, Y.; Fu, L.Y.; Jiang, T.; Meng, F.D. β-Catenin promotes cell proliferation, migration, and invasion but induces apoptosis in renal cell carcinoma. OncoTargets Ther. 2017, 10, 711–724. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ueno, K.; Hirata, H.; Majid, S.; Tabatabai, Z.L.; Hinoda, Y.; Dahiya, R. IGFBP-4 activates the Wnt/beta-catenin signaling pathway and induces M-CAM expression in human renal cell carcinoma. Int. J. Cancer 2011, 129, 2360–2369. [Google Scholar] [CrossRef] [PubMed]
- Saadi-Kheddouci, S.; Berrebi, D.; Romagnolo, B.; Cluzeaud, F.; Peuchmaur, M.; Kahn, A.; Vandewalle, A.; Perret, C. Early development of polycystic kidney disease in transgenic mice expressing an activated mutant of the beta-catenin gene. Oncogene 2001, 20, 5972–5981. [Google Scholar] [CrossRef] [PubMed]
- Atkins, M.B.; Clark, J.I.; Quinn, D.I. Immune checkpoint inhibitors in advanced renal cell carcinoma: Experience to date and future directions. Ann. Oncol. 2017, 28, 1484–1494. [Google Scholar] [CrossRef] [PubMed]
- Gebrael, G.; Sahu, K.K.; Agarwal, N.; Maughan, B.L. Update on combined immunotherapy for the treatment of advanced renal cell carcinoma. Hum. Vaccines Immunother. 2023, 19, 2193528. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grimley, E.; Liao, C.; Ranghini, E.J.; Nikolovska-Coleska, Z.; Dressler, G.R. Inhibition of Pax2 Transcription Activation with a Small Molecule that Targets the DNA Binding Domain. ACS Chem. Biol. 2017, 12, 724–734. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bradford, S.T.J.; Grimley, E.; Laszczyk, A.M.; Lee, P.H.; Patel, S.R.; Dressler, G.R. Identification of Pax protein inhibitors that suppress target gene expression and cancer cell proliferation. Cell Chem. Biol. 2022, 29, 412–422.e4. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lasorsa, F.; Rutigliano, M.; Milella, M.; Ferro, M.; Pandolfo, S.D.; Crocetto, F.; Autorino, R.; Battaglia, M.; Ditonno, P.; Lucarelli, G. Cancer Stem Cells in Renal Cell Carcinoma: Origins and Biomarkers. Int. J. Mol. Sci. 2023, 24, 13179. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Swetha, G.; Chandra, V.; Phadnis, S.; Bhonde, R. Glomerular parietal epithelial cells of adult murine kidney undergo EMT to generate cells with traits of renal progenitors. J. Cell. Mol. Med. 2011, 15, 396–413. [Google Scholar] [CrossRef]
- Milella, M.; Rutigliano, M.; Lasorsa, F.; Ferro, M.; Bianchi, R.; Fallara, G.; Crocetto, F.; Pandolfo, S.D.; Barone, B.; d’Amati, A.; et al. The Role of MUC1 in Renal Cell Carcinoma. Biomolecules 2024, 14, 315. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barata, P.C.; Rini, B.I. Treatment of renal cell carcinoma: Current status and future directions. CA Cancer J. Clin. 2017, 67, 507–524. [Google Scholar] [CrossRef]
- Jin, J.; Xie, Y.; Zhang, J.S.; Wang, J.Q.; Dai, S.J.; He, W.F.; Li, S.Y.; Ashby, C.R., Jr.; Chen, Z.S.; He, Q. Sunitinib resistance in renal cell carcinoma: From molecular mechanisms to predictive biomarkers. Drug Resist. Updates 2023, 67, 100929. [Google Scholar] [CrossRef]

| Groups | * PAX Genes | HL | Structural | EA | ER | RC | References |
|---|---|---|---|---|---|---|---|
| I | PAX1 | 20p11 | PD+OCT | Skeleton, thymus | No or low expression | Netural or favourable | [8,17,18] |
| PAX9 | 14q12 | PD+OCT | Skeleton, craniofacial, tooth | No or low expression | Netural or favourable | [12,17,18] | |
| II | PAX2 | 10q24 | PD+OCT+partial HD | CNS, kidney, eye, ear | High expression | Tumor-promoting | [19,20,21,22] |
| PAX5 | 9p13 | PD+OCT+partial HD | CNS, B cells, testis | No or low expression | Netural or favourable | [8,12,25] | |
| PAX8 | 2q12 | PD+OCT+partial HD | CNS, kidney, thyroid | High expression | Tumor-promoting | [8,10,27] | |
| III | PAX3 | 2q35 | PD+OCT+HD | CNS, neural crest, skeletal muscle | No or low expression | Netural or favourable | [8,12,23] |
| PAX7 | 1p36 | PD+OCT+HD | CNS, craniofacial, skeletal muscle | No or low expression | Netural or favourable | [8,12] | |
| IV | PAX4 | 7q32 | PD+HD | CNS, Pancreas | No or low expression | Netural or favourable | [8,12,24] |
| PAX6 | 11p13 | PD+HD | CNS, eye, pancreas | No or low expression | Netural or favourable | [8,26] |
| PAX | Methods | Model | Main Outcomes | Authors, Year [Reference] |
|---|---|---|---|---|
| PAX2 | SiRNA inactivation of PAX2 | RCC cell lines | PAX2 inactivation enhances cisplatin-induced apoptosis in renal carcinoma cells | Hueber et al., 2006 [22] |
| PAX2 | shRNA targeting PAX2 | RCC cell lines and nude mice | Subcutaneous ACHN/shPAX2 xenografts in nude mice respond better to cisplatin therapy than control ACHN tumors | Hueber et al., 2008 [31] |
| PAX2 | Virtual screening and experimental validation | RCC cell lines | A small molecule inhibitor (EG1) targeting the DNA binding domain of PAX2 | Grimley et al., 2017 [132] |
| PAX8 | Large-scale functional genomic screens (ChIP-seq, RNA-seq, and ATAC-seq) | RCC cell lines | PAX8 silencing results in decreased proliferation of RCC cell lines | Bleu et al., 2019 [27] |
| PAX2 | Unbiased cell-based high-throughput screening assay | RCC cell lines | Three triazolo pyrimidine derivatives were identified that inhibited PAX-mediated transcriptional activation of reporter genes and suppressed proliferation of PAX2-positive RCC cells. | Bradford et al., 2022 [133] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.; Hossain, S.M.; Eccles, M.R. The Role of the PAX Genes in Renal Cell Carcinoma. Int. J. Mol. Sci. 2024, 25, 6730. https://doi.org/10.3390/ijms25126730
Li L, Hossain SM, Eccles MR. The Role of the PAX Genes in Renal Cell Carcinoma. International Journal of Molecular Sciences. 2024; 25(12):6730. https://doi.org/10.3390/ijms25126730
Chicago/Turabian StyleLi, Lei, Sultana Mehbuba Hossain, and Michael R. Eccles. 2024. "The Role of the PAX Genes in Renal Cell Carcinoma" International Journal of Molecular Sciences 25, no. 12: 6730. https://doi.org/10.3390/ijms25126730
APA StyleLi, L., Hossain, S. M., & Eccles, M. R. (2024). The Role of the PAX Genes in Renal Cell Carcinoma. International Journal of Molecular Sciences, 25(12), 6730. https://doi.org/10.3390/ijms25126730







