In Silico Electrophysiological Investigation of Transient Receptor Potential Melastatin-4 Ion Channel Biophysics to Study Detrusor Overactivity
Abstract
:1. Introduction
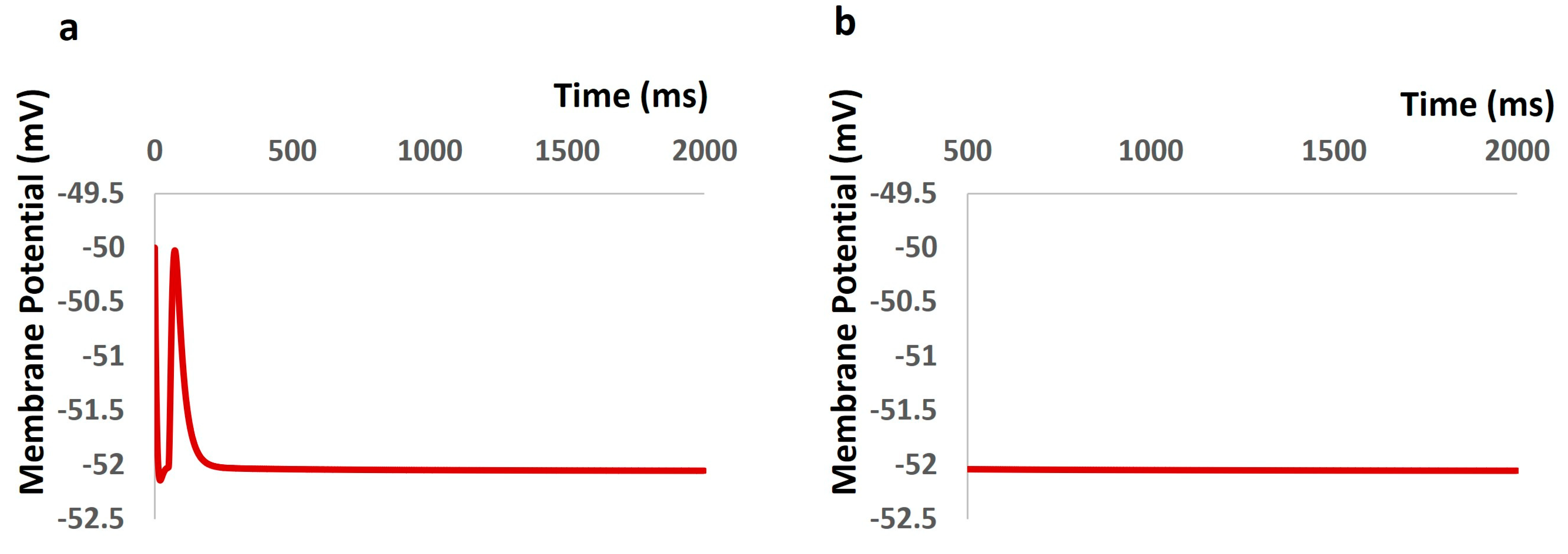
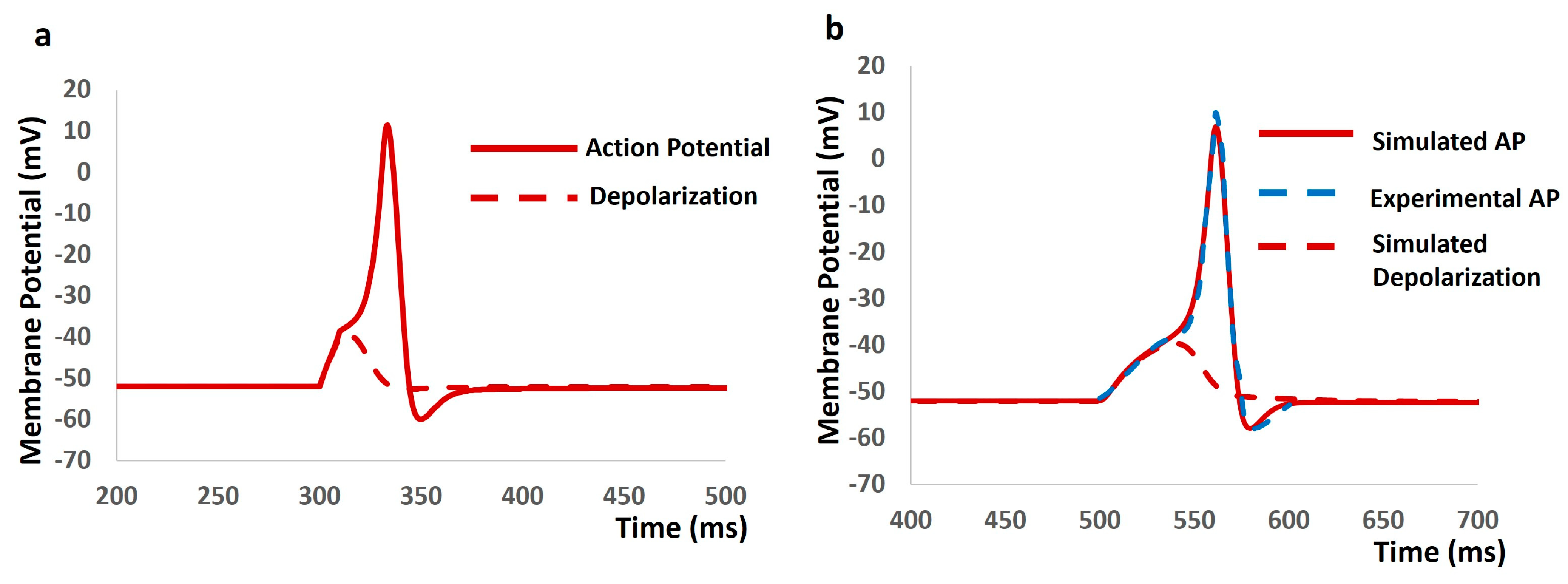
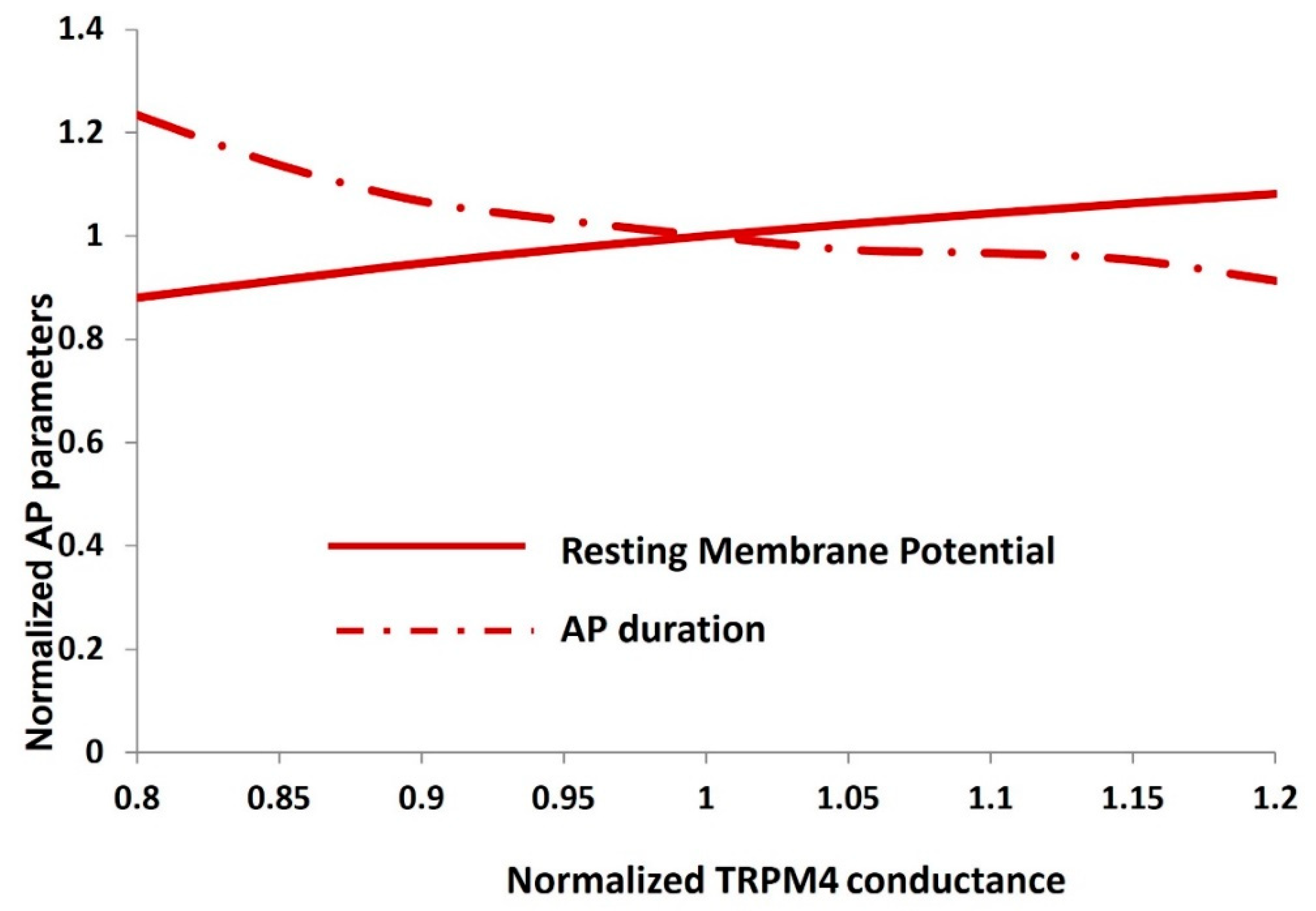
2. Results
3. Discussion
4. Materials and Methods
4.1. Model Adaptation
4.2. General Membrane Current Descriptions
= 328.1084 × b, KO1C1 = 154.1736 × b, KO2C2 = 33.6594 × b, KO3C3= 0.097312 × b, KO4C4 = 0.000406 × b × cai
KC4C3 = 3 × Kcoff × cai, KC3C2 = 4 × Kcoff × cai, KC2C1 = 3 × Kcoff × cai, KC1C0 = Kcoff × cai
KO0O1 = 3 × Kon × cai, KO1O2 = 4 × Kon × cai, KO2O3 = 3 × Kon × cai, KO3O4 = Kon × cai
KO4O3 = 3 × Kooff × cai, KO3O2 = 4 × Kooff × cai, KO2O1 = 3 × Kooff × cai, KO1O0 = Kooff × cai
4.3. TRPM 4 Channel with Ca2+ Sensing Mechanism
4.4. Whole DSM Cell Model and Simulation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Groat, W.C.; Yoshimura, N.A. Anatomy and physiology of the lower urinary tract. Handb. Clin. Neurol. 2015, 130, 61–108. [Google Scholar] [PubMed]
- Tyagi, S.; Tyagi, P.; Yoshimura, N.; Chancellor, M.B. Physiology of micturition. In Textbook of Female Urology and Urogynecology-Two-Volume Set; CRC Press: Boca Raton, FL, USA, 2017; pp. 232–246. [Google Scholar]
- Abrams, P. Describing bladder storage function: Overactive bladder syndrome and detrusor overactivity. Urology 2003, 62, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Wein, A.J.; Rackley, R.R. Overactive bladder: A better understanding of pathophysiology, diagnosis, and management. J. Urol. 2006, 175, S5–S10. [Google Scholar]
- Drake, M.J. The Overactive Bladder. In Textbook of Female Urology and Urogynecology-Two-Volume Set; CRC Press: Boca Raton, FL, USA, 2017; pp. 584–593. [Google Scholar]
- Chapple, C.R.; Mangera, A. Urgency incontinence and overactive bladder. In Oxford Textbook of Urological Surgery; Oxford University Press: Oxford, UK, 2017; pp. 282–288. [Google Scholar]
- Dwyer, P.L.; Rosamilia, A. Evaluation and diagnosis of the overactive bladder. Clin. Obstet. Gynecol. 2002, 45, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.S.; William, F.; McGhan, C.S. Comorbidities associated with overactive bladder. Am. J. Manag. Care 2000, 6, S574–S579. [Google Scholar] [PubMed]
- Palma-Zamora, I.D.; Atiemo, H.O. Understanding the economic impact of neurogenic lower urinary tract dysfunction. Urol. Clin. 2017, 44, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-Y.; Siu, K.-C.; Lin, K.-H. Impact of lower urinary tract symptoms on work productivity in female workers: A systematic review and meta-analysis. Neurourol. Urodyn. 2018, 37, 2323–2334. [Google Scholar] [CrossRef] [PubMed]
- Pierce, H.; Perry, L.; Chiarelli, P.; Gallagher, R. A systematic review of prevalence and impact of symptoms of pelvic floor dysfunction in identified workforce groups. J. Adv. Nurs. 2016, 72, 1718–1734. [Google Scholar] [CrossRef]
- Chakrabarty, B.J.; Crook; Drake, M.; Gilliland, N.; Gulur, D.; Kitney, D.; Manjunath, A.; Somov, P.; Vahabi, B. The Urinary Tract: Form and Function. In Lower Urinary Tract Symptoms in Adults: A Clinical Approach; Springer: Cham, Switzerland, 2020; pp. 1–17. [Google Scholar]
- Kitney, D.G. Bladder Spontaneous Activity: Influence of Mild Heating and Inert Injectables. Ph.D. Dissertation, University of Surrey, Guildford, UK, 2016. [Google Scholar]
- Bortolini, A.T.M.; Bilhar, A.P.M.; Castro, R.A. Neural control of lower urinary tract and targets for pharmacological therapy. Int. Urogynecol. J. 2014, 25, 1453–1462. [Google Scholar] [CrossRef]
- Afrashteh, B. Identification of Lower Urinary Tract Dysfunction after Spinal Cord Injury at Lumbosacral Level by Developing a Clinical Relevance Rat Model. Ph.D. Dissertation, University of Salzburg, Salzburg, Austria, 2023. [Google Scholar]
- Asl, S.O.K.Z. Analysis and Modeling of the Roles of Actin-Myosin Interactions in Bladder Smooth Muscle Biomechanics. Ph.D. Dissertation, Virginia Commonwealth University, Richmond, VA, USA, 2014. [Google Scholar]
- Guntu, V.S.K. Biophysical Modeling to Reverse Engineer Two Mammalian Neural Circuits Lower Urinar Y Tract and Hippocampus. Ph.D. Dissertation, University of Missouri, Columbia, MO, USA, 2020. [Google Scholar]
- Wyman, J.F.; Burgio, K.L.; Newman, D.K. Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence. Int. J. Clin. Pract. 2009, 63, 1177–1191. [Google Scholar] [CrossRef]
- Willis-Gray, M.G.; Alexis, A.D.; Elizabeth, J.G. Evaluation and management of overactive bladder: Strategies for optimizing care. Res. Rep. Urol. 2016, 8, 113–122. [Google Scholar] [PubMed]
- Smith, L.E.; Rebecca, K.W.; Rubin, G.J. A systematic review of factors associated with side-effect expectations from medical interventions. Health Expect. 2020, 23, 731–758. [Google Scholar] [CrossRef] [PubMed]
- Mostafaei, H.; Shariat, S.F.; Salehi-Pourmehr, H.; Janisch, F.; Mori, K.; Quhal, F.; Hajebrahimi, S. The clinical pharmacology of the medical treatment for overactive bladder in adults. Expert Rev. Clin. Pharmacol. 2020, 13, 707–720. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, A.; Nesbitt, A.; Joshi, A.; Clubb, A.; Perera, M. Overactive bladder syndrome: Management and treatment options. Aust. J. Gen. Pract. 2020, 49, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Fogaing, C.; Mossa, A.H.; Campeau, L. Are beta 3 adrenergic agonists now the preferred pharmacologic management of overactive bladder? Curr. Urol. Rep. 2020, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Duong, V.; Iwamoto, A.; Pennycuff, J.; Kudish, B.; Iglesia, C. A systematic review of neurocognitive dysfunction with overactive bladder medications. Int. Urogynecol. J. 2021, 32, 2693–2702. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, S.D.; Rickey, L.M. Medical Therapy with Antimuscarinics and ß3-Agonists. In Female Urinary Incontinence; Springer International Publishing: Cham, Switzerland, 2022; pp. 147–164. [Google Scholar]
- Drake, M.J.; Fry, C.H.; Hashitani, H.; Kirschner-Hermanns, R.; Rahnama, M.S.; Speich, J.E.; Tomoe, H.; Kanai, A.J.; McCloskey, K.D. What are the origins and relevance of spontaneous bladder contractions? ICI-RS 2017. Neurourol. Urodyn. 2018, 37, S13–S19. [Google Scholar] [CrossRef] [PubMed]
- Mitsui, R.; Lee, K.; Uchiyama, A.; Hayakawa, S.; Kinoshita, F.; Kajioka, S.; Eto, M.; Hashitani, H. Contractile elements and their sympathetic regulations in the pig urinary bladder: A species and regional comparative study. Cell Tissue Res. 2020, 379, 373–387. [Google Scholar] [CrossRef]
- Burdyga, T.V.; Wray, S. The relationship between the action potential, intracellular calcium and force in intact phasic, guinea-pig uretic smooth muscle. J. Physiol. 1999, 520, 867–883. [Google Scholar] [CrossRef]
- Ter Keurs, H.E.D.J.; Boyden, P.A. Calcium and arrhythmogenesis. Physiol. Rev. 2007, 87, 457–506. [Google Scholar] [CrossRef]
- Bolton, T.B.; Gordienko, D.V.; Pucovský, V.; Parsons, S.; Povstyan, O. Calcium release events in excitation–contraction coupling in smooth muscle. In Role of The Sarcoplasmic Reticulum in Smooth Muscle: Novartis Foundation Symposium 246; John Wiley & Sons, Ltd.: Chichester, UK, 2002; Volume 246, pp. 154–173. [Google Scholar]
- Sanders, K.M. Spontaneous electrical activity and rhythmicity in gastrointestinal smooth muscles. In Smooth Muscle Spontaneous Activity: Physiological and Pathological Modulation; Springer: Singapore, 2019; pp. 3–46. [Google Scholar]
- Boopathi, E.; Gomes, C.; Zderic, S.A.; Malkowicz, B.; Chakrabarti, R.; Patel, D.P.; Wein, A.J.; Chacko, S. Mechanical stretch upregulates proteins involved in Ca2+ sensitization in urinary bladder smooth muscle hypertrophy. Am. J. Physiol. Cell Physiol. 2014, 307, C542–C553. [Google Scholar] [CrossRef] [PubMed]
- Poley, R.N.; Dosier, C.R.; Speich, J.E.; Miner, A.S.; Ratz, P.H. Stimulated calcium entry and constitutive RhoA kinase activity cause stretch-induced detrusor contraction. Eur. J. Pharmacol. 2008, 599, 137–145. [Google Scholar] [CrossRef]
- Kajioka, S.; Nakayama, S.; McMurray, G.; Abe, K.; Brading, A.F. Ca2+ channel properties in smooth muscle cells of the urinary bladder from pig and human. Eur. J. Pharmacol. 2002, 443, 19–29. [Google Scholar] [CrossRef]
- Wu, C.; Sui, G.; Fry, C.H. The role of the L-type Ca2+ channel in refilling functional intracellular Ca2+ stores in guinea-pig detrusor smooth muscle. J. Physiol. 2002, 538, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Petkov, G.V. 14 Role of Ion Channels in Urinary Bladder Smooth Muscle Function. In Signal Transduction and Smooth Muscle; CRC Press: Boca Raton, FL, USA, 2018; p. 281. [Google Scholar]
- Wray, S.; Burdyga, T. Sarcoplasmic reticulum function in smooth muscle. Physiol. Rev. 2010, 90, 113–178. [Google Scholar] [CrossRef]
- Wu, C.; Fry, C.H. Na+/Ca2+ exchange and its role in intracellular Ca2+ regulation in guinea pig detrusor smooth muscle. Am. J. Physiol. Cell Physiol. 2001, 280, C1090–C1096. [Google Scholar] [CrossRef] [PubMed]
- Herrera, G.M.; Nelson, M.T. Sarcoplasmic reticulum and membrane currents. In Role of The Sarcoplasmic Reticulum in Smooth Muscle: Novartis Foundation Symposium 246; John Wiley & Sons, Ltd.: Chichester, UK, 2002; Volume 246, pp. 189–207. [Google Scholar]
- Provence, A. Kv7 Channels of the Urinary Bladder Smooth Muscle: Functional Roles and Therapeutic Potential. Ph.D. Thesis, University of South Carolina, Columbia, SC, USA, 2018. [Google Scholar]
- Takagi, H.; Hashitani, H. Effects of K+ channel openers on spontaneous action potentials in detrusor smooth muscle of the guinea-pig urinary bladder. Eur. J. Pharmacol. 2016, 789, 179–186. [Google Scholar] [CrossRef]
- Hayase, M.; Hashitani, H.; Kohri, K.; Suzuki, H. Role of K+ channels in regulating spontaneous activity in detrusor smooth muscle in situ in the mouse bladder. J. Urol. 2009, 181, 2355–2365. [Google Scholar] [CrossRef]
- Xin, W.; Cheng, Q.; Soder, R.P.; Petkov, G.V. Inhibition of phosphodiesterases relaxes detrusor smooth muscle via activation of the large-conductance voltage-and Ca2+-activated K+ channel. Am. J. Physiol. Cell Physiol. 2012, 302, C1361–C1370. [Google Scholar] [CrossRef]
- Hristov, K.L.; Parajuli, S.P.; Soder, R.P.; Cheng, Q.; Rovner, E.S.; Petkov, G.V. Suppression of human detrusor smooth muscle excitability and contractility via pharmacological activation of large conductance Ca2+-activated channels. Am. J. Physiol. Cell Physiol. 2012, 302, C1632–C1641. [Google Scholar] [CrossRef]
- Petkov, G.V. Role of potassium ion channels in detrusor smooth muscle function and dysfunction. Nat. Rev. Urol. 2012, 9, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Hristov, K.L.; Smith, A.C.; Parajuli, S.P.; Malysz, J.; Petkov, G.V. Large-conductance voltage-and Ca2+-activated K+ channel regulation by protein kinase C in guinea pig urinary bladder smooth muscle. Am. J. Physiol. Cell Physiol. 2014, 306, C460–C470. [Google Scholar] [CrossRef] [PubMed]
- Parajuli, S.P.; Petkov, G.V. Activation of muscarinic M3 receptors inhibits large-conductance voltage- and Ca2+-activated K+ channels in rat urinary bladder smooth muscle cells. Am. J. Physiol. Cell Physiol. 2013, 305, C207–C214. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.P. Modulators of Small and Intermediate Conductance Calcium-Activated Potassium Channel: Mechanism of Action and In Vivo Effects; University of California: Davis, CA, USA, 2012. [Google Scholar]
- Hristov, K.L.; Smith, A.C.; Parajuli, S.P.; Malysz, J.; Rovner, E.S.; Petkov, G.V. Novel regulatory mechanism in human urinary bladder: Central role of transient receptor potential melastatin 4 channels in detrusor smooth muscle function. Am. J. Physiol. Cell Physiol. 2016, 310, C600–C611. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, K.L. New life in overactive bladder. Focus on “Novel regulatory mechanism in human urinary bladder: Central role of transient receptor potential melastatin 4 channels in detrusor smooth muscle function”. Am. J. Physiol. Cell Physiol. 2016, 310, C597–C599. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Hristov, K.L.; Cheng, Q.; Xin, W.; Parajuli, S.P.; Earley, S.; Malysz, J.; Petkov, G.V. Novel role for the transient potential receptor melastatin 4 channel in guinea pig detrusor smooth muscle physiology. Am. J. Physiol. Cell Physiol. 2013, 304, C467–C477. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Parajuli, S.P.; Hristov, K.L.; Cheng, Q.; Soder, R.P.; Afeli, S.A.Y.; Earley, S.; Xin, W.; Malysz, J.; Petkov, G.V. TRPM4 channel: A new player in urinary bladder smooth muscle function in rats. Am. J. Physiol. Ren. Physiol. 2013, 304, F918–F929. [Google Scholar] [CrossRef] [PubMed]
- Provence, A.; Rovner, E.S.; Petkov, G.V. Regulation of transient receptor potential melastatin 4 channel by sarcoplasmic reticulum inositol trisphosphate receptors: Role in human detrusor smooth muscle function. Channels 2017, 11, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Launay, P.; Fleig, A.; Perraud, A.-L.; Scharenberg, A.M.; Penner, R.; Kinet, J.-P. TRPM4 is a Ca2+-activated nonselective cation channel mediating cell membrane depolarization. Cell 2002, 109, 397–407. [Google Scholar] [CrossRef]
- Parajuli, S.P.; Hristov, K.L.; Sullivan, M.N.; Xin, W.; Smith, A.C.; Earley, S.; Malysz, J.; Petkov, G.V. Control of urinary bladder smooth muscle excitability by the TRPM4 channel modulator 9-phenanthrol. Channels 2013, 7, 537–540. [Google Scholar] [CrossRef]
- Malysz, J.; Petkov, G.V. Urinary bladder smooth muscle ion channels: Expression, function, and regulation in health and disease. Am. J. Physiol. Ren. Physiol. 2020, 319, F257–F283. [Google Scholar] [CrossRef] [PubMed]
- Hegde, S.S.; Eglen, R.M. Muscarinic receptor subtypes modulating smooth muscle contractility in the urinary bladder. Life Sci. 1999, 64, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Ehlert, F.J. Contractile role of M2 and M3 muscarinic receptors in gastrointestinal, airway and urinary bladder smooth muscle. Life Sci. 2003, 74, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Andersson, K.-E. Potential benefits of muscarinic M3 receptor selectivity. Eur. Urol. Suppl. 2002, 1, 23–28. [Google Scholar] [CrossRef]
- Nausch, B.; Heppner, T.J.; Nelson, M.T. Nerve-released acetylcholine contracts urinary bladder smooth muscle by inducing action potentials independently of IP3-mediated calcium release. Am. J. Physiol. -Regul. Integr. Comp. Physiol. 2010, 299, R878–R888. [Google Scholar] [CrossRef] [PubMed]
- Goaillard, J.-M.; Marder, E. Ion channel degeneracy, variability, and covariation in neuron and circuit resilience. Annu. Rev. Neurosci. 2021, 44, 335–357. [Google Scholar] [CrossRef] [PubMed]
- Walpole, J.; Papin, J.A.; Peirce, S.M. Multiscale computational models of complex biological systems. Annu. Rev. Biomed. Eng. 2013, 15, 137–154. [Google Scholar] [CrossRef] [PubMed]
- Aliev, R.R.; Richards, W.; Wikswo, J.P. A simple nonlinear model of electrical activity in the intestine. J. Theor. Biol. 2000, 204, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Bursztyn, L.; Eytan, O.; Jaffa, A.J.; Elad, D. Mathematical model of excitation-contraction in a uterine smooth muscle cell. Am. J. Physiol. Cell Physiol. 2007, 292, C1816–C1829. [Google Scholar] [CrossRef]
- Tong, W.C.; Choi, C.Y.; Karche, S.; Holden, A.V.; Zhang, H.; Taggart, M.J. A computational model of the ionic currents, Ca2+ dynamics and action potentials underlying contraction of isolated uterine smooth muscle. PLoS ONE 2011, 6, e18685. [Google Scholar] [CrossRef]
- Rihana, S.; Terrien, J.; Germain, G.; Marque, C. Mathematical modeling of electrical activity of uterine muscle cells. Med. Biol. Eng. Comput. 2009, 47, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, C. # 2696 In Silico Electrophysiological Study Reveals Tamsulosin Mediates Ureter Smooth Muscle Contraction by Increasing Potassium Current. Nephrol. Dial. Transplant. 2023, 38 (Suppl. S1), gfad063c_2696. [Google Scholar]
- Mahapatra, C.; Manchanda, R. Computational studies on ureter smooth muscle: Modeling ion channels and their role in generating electrical activity. In Proceedings of the 2019 Summer Simulation Conference, Berlin, Germany, 22–24 July 2019; pp. 1–6. [Google Scholar]
- Mahapatra, C.; Pradhan, A. FC025: Physiological Role of KV Channel in Ureter Smooth Muscle Cell Investigated Quantitatively by Electrophysiological Modeling. Nephrol. Dial. Transplant. 2022, 37 (Suppl. S3), gfac100-001. [Google Scholar] [CrossRef]
- Poh, Y.C.; Corrias, A.; Cheng, N.; Buist, M.L. A quantitative model of human jejunal smooth muscle cell electrophysiology. PLoS ONE 2012, 7, e42385. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, C.; Manchanda, R. In-Silico Investigation of Castration on Vas Deferens Smooth Muscle Electrophysiology. FASEB J. 2022, 36. [Google Scholar] [CrossRef]
- Mahapatra, C.; Manchanda, R. Modeling Vas Deferens Smooth Muscle Electrophysiology: Role of Ion Channels in Generating Electrical Activity. In Soft Computing for Problem Solving: SocProS 2017, Volume 2; Springer: Singapore, 2019; pp. 655–663. [Google Scholar]
- Mahapatra, C. Modulating Effects of Castration on vas Deferens Smooth Muscle Electrical Activities: Insights from a Quantitative study. Fertil. Steril. 2021, 116, e349. [Google Scholar] [CrossRef]
- Mahapatra, C.; Manchanda, R. Modeling VAS Deferens Smooth Muscle Electrophysiology: Role of Ion Channels in Generating Electrical Activity. Biophys. J. 2020, 118, 259a–260a. [Google Scholar] [CrossRef]
- Corrias, A.; Buist, M.L. A quantitative model of gastric smooth muscle cellular activation. Ann. Biomed. Eng. 2007, 35, 1595–1607. [Google Scholar] [CrossRef]
- Corrias, A.; Buist, M.L. Quantitative cellular description of gastric slow wave activity. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 294, G989–G995. [Google Scholar] [CrossRef]
- Kapela, A.; Bezerianos, A.; Tsoukias, N.M. A mathematical model of Ca2+ dynamics in rat mesenteric smooth muscle cell: Agonist and NO stimulation. J. Theor. Biol. 2008, 253, 238–260. [Google Scholar] [CrossRef]
- Miftakhov, R.N.; Abdusheva, G.R.; Wingate, D.L. Model predictions of myoelectrical activity of the small bowel. Biol. Cybern. 1996, 74, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, C. Computational Study of Action Potential Generation in Urethral Smooth Muscle Cell. In Proceedings of the Computational Advances in Bio and Medical Sciences: 10th International Conference, ICCABS 2020, Virtual Event, 10–12 December 2020; Revised Selected Papers 10. Springer International Publishing: New, York, NY, USA, 2021; pp. 26–32. [Google Scholar]
- Mahapatra, C.; Adam, S.; Gupta, A. Computational modeling of electrophysiological properties in urethral smooth muscle cell. J. Comput. Neurosci. 2021, 49, S81–S83. [Google Scholar]
- Cha, C.Y.; Earm, K.H.; Youm, J.B.; Baek, E.B.; Kim, S.J.; Earm, Y.E. Electrophysiological modelling of pulmonary artery smooth muscle cells in the rabbits—Special consideration to the generation of hypoxic pulmonary vasoconstriction. Prog. Biophys. Mol. Biol. 2008, 96, 399–420. [Google Scholar] [CrossRef]
- Mahapatra, C.; Samuilik, I. A Mathematical Model of Spontaneous Action Potential Based on Stochastics Synaptic Noise Dynamics in Non-Neural Cells. Mathematics 2024, 12, 1149. [Google Scholar] [CrossRef]
- Mahapatra, C.; Brain, K.L.; Manchanda, R. A biophysically constrained computational model of the action potential of mouse urinary bladder smooth muscle. PLoS ONE 2018, 13, e0200712. [Google Scholar] [CrossRef]
- Mahapatra, C.; Dave, V.; Manchanda, R. A Mathematical Modeling of Voltage-gated Calcium ion channel-based Calcium Transient Response in UrinaryBladder Smooth Muscle Cell. Int. J. Pure Appl. Math. 2017, 117, 71–75. [Google Scholar]
- Mahapatra, C.; Manchanda, R. Simulation of In Vitro-Like Electrical Activities in Urinary Bladder Smooth Muscle Cells. J. Biomim. Biomater. Biomed. Eng. 2017, 33, 45–51. [Google Scholar] [CrossRef]
- Mahapatra, C.; Manchanda, R. Modulating Properties of Hyperpolarization-Activated Cation Current in Urinary Bladder Smooth Muscle Excitability: A Simulation Study. In Recent Findings in Intelligent Computing Techniques: Proceedings of the 5th ICACNI 2017, Volume 1; Springer: Singapore, 2019; pp. 261–266. [Google Scholar]
- Mahapatra, C.; Brain, K.L.; Manchanda, R. Computational study of Hodgkin-Huxley type calcium-dependent potassium current in urinary bladder over activity. In Proceedings of the 2018 IEEE 8th International Conference on Computational Advances in Bio and Medical Sciences (ICCABS), Las Vegas, NV, USA, 18–20 October 2018; IEEE: New, York, NY, USA; pp. 1–4. [Google Scholar]
- Dave, V.; Mahapatra, C.; Manchanda, R. A mathematical model of the calcium transient in urinary bladder smooth muscle cells. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; IEEE: New, York, NY, USA, 2015; pp. 5359–5362. [Google Scholar]
- Demion, M.; Bois, P.; Launay, P.; Guinamard, R. TRPM4, a Ca2+-activated nonselective cation channel in mouse sino-atrial node cells. Cardiovasc. Res. 2007, 73, 531–538. [Google Scholar] [CrossRef]
- Marom, S.; Marder, E. A biophysical perspective on the resilience of neuronal excitability across timescales. Nat. Rev. Neurosci. 2023, 24, 640–652. [Google Scholar] [CrossRef]
- Chow, K.-Y.; Wu, C.; Sui, G.P.; Fry, C.H. Role of the T-type Ca2+ current on the contractile performance of guinea pig detrusor smooth muscle. Neurourol. Urodyn. Off. J. Int. Cont. Soc. 2003, 22, 77–82. [Google Scholar] [CrossRef]
- Jaggar, J.H.; Porter, V.A.; Lederer, W.J.; Nelson, M.T. Calcium sparks in smooth muscle. Am. J. Physiol. -Cell Physiol. 2000, 278, C235–C256. [Google Scholar] [CrossRef] [PubMed]
- Hodgkin, A.L.; Huxley, A.F. A quantitative description of membrane current and its application to conduction and excitation in nerve. J. Physiol. 1952, 117, 500. [Google Scholar] [CrossRef] [PubMed]
- Noble, D. A modification of the Hodgkin—Huxley equations applicable to Purkinje fibre action and pacemaker potentials. J. Physiol. 1962, 160, 317. [Google Scholar] [CrossRef] [PubMed]
- Fry, C.H.; Cooklin, M.; Birns, J.; Mundy, A.R. Measurement of intercellular electrical coupling in guinea-pig detrusor smooth muscle. J. Urol. 1999, 161, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Geng, Y.; Magleby, K.L. Single-channel kinetics of BK (Slo1) channels. Front. Physiol. 2015, 5, 129016. [Google Scholar] [CrossRef] [PubMed]
- Heeger, D. Synaptic Input. 2000. Available online: https://www.cns.nyu.edu/~david/handouts/synapse.pdf (accessed on 19 June 2024).
- Hines, M.L.; Carnevale, N.T. The NEURON simulation environment. Neural Comput. 1997, 9, 1179–1209. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, T. Neuron simulation environment. Scholarpedia 2007, 2, 1378. [Google Scholar] [CrossRef]
- Spiess, A.-N.; Neumeyer, N. An evaluation of R 2 as an inadequate measure for nonlinear models in pharmacological and biochemical research: A Monte Carlo approach. BMC Pharmacol. 2010, 10, 1–11. [Google Scholar] [CrossRef]







| Ion Channel | Conductance (S/cm2) |
|---|---|
| T-type Ca2+ channel | 0.0002 |
| L-type Ca2+ channel | 0.0003 |
| Voltage-gated K+ channel-Kv1 | 0.0006 |
| Voltage-gated K+ channel-KDR | 0.0009 |
| Calcium-dependent K+ channel (BK) | 0.0008 |
| Calcium-dependent K+ channel (IK) | 0.0007 |
| Calcium-dependent K+ channel (SK) | 0.0001 |
| ATP-dependent K+ channel | 0.0001 |
| Inward-rectifying channel | 0.0001 |
| TRPM4 Channel | 0.0002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahapatra, C.; Thakkar, R. In Silico Electrophysiological Investigation of Transient Receptor Potential Melastatin-4 Ion Channel Biophysics to Study Detrusor Overactivity. Int. J. Mol. Sci. 2024, 25, 6875. https://doi.org/10.3390/ijms25136875
Mahapatra C, Thakkar R. In Silico Electrophysiological Investigation of Transient Receptor Potential Melastatin-4 Ion Channel Biophysics to Study Detrusor Overactivity. International Journal of Molecular Sciences. 2024; 25(13):6875. https://doi.org/10.3390/ijms25136875
Chicago/Turabian StyleMahapatra, Chitaranjan, and Ravindra Thakkar. 2024. "In Silico Electrophysiological Investigation of Transient Receptor Potential Melastatin-4 Ion Channel Biophysics to Study Detrusor Overactivity" International Journal of Molecular Sciences 25, no. 13: 6875. https://doi.org/10.3390/ijms25136875





