Identification of SIBO Subtypes along with Nutritional Status and Diet as Key Elements of SIBO Therapy
Abstract
:1. Introduction
2. Results
2.1. Demographic and Anthropometric Characteristics
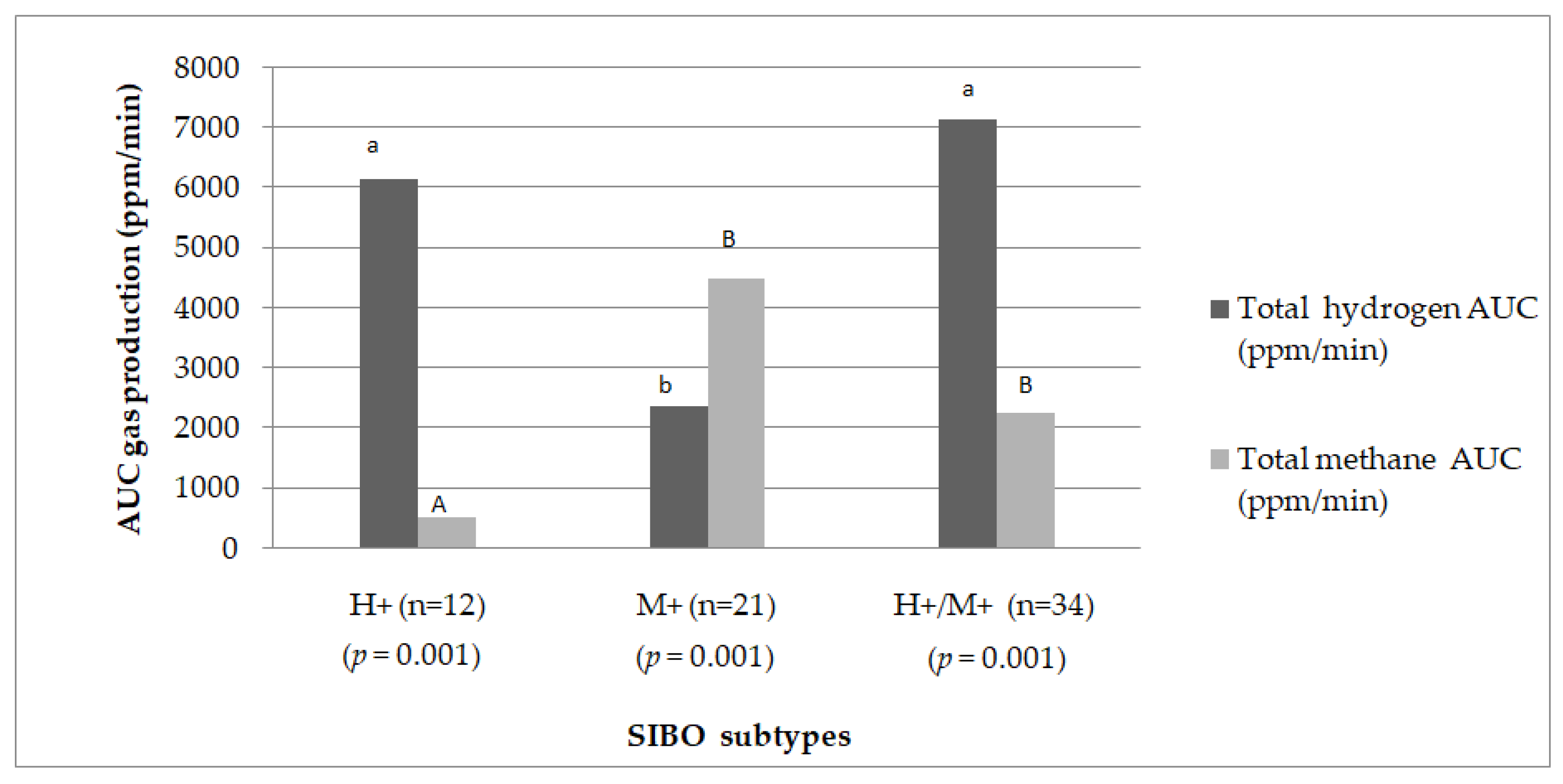
2.2. Hydrogen and Methane Production
2.3. Biochemical Parameters
2.4. Energy and Macronutrients Intake
2.5. Micronutrients Intake in SIBO Subtypes
2.6. Correlations
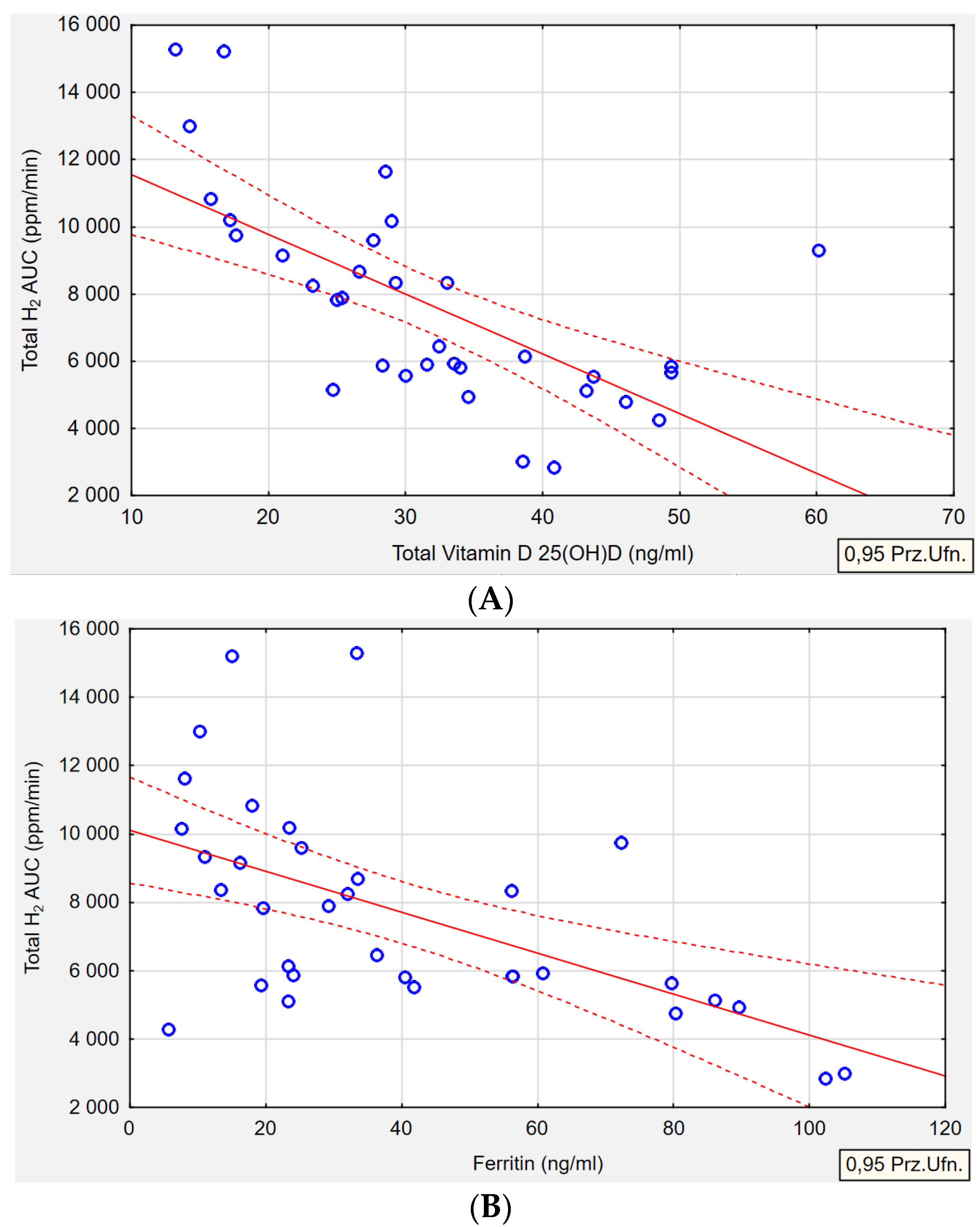
2.6.1. Biochemical Parameters Correlations
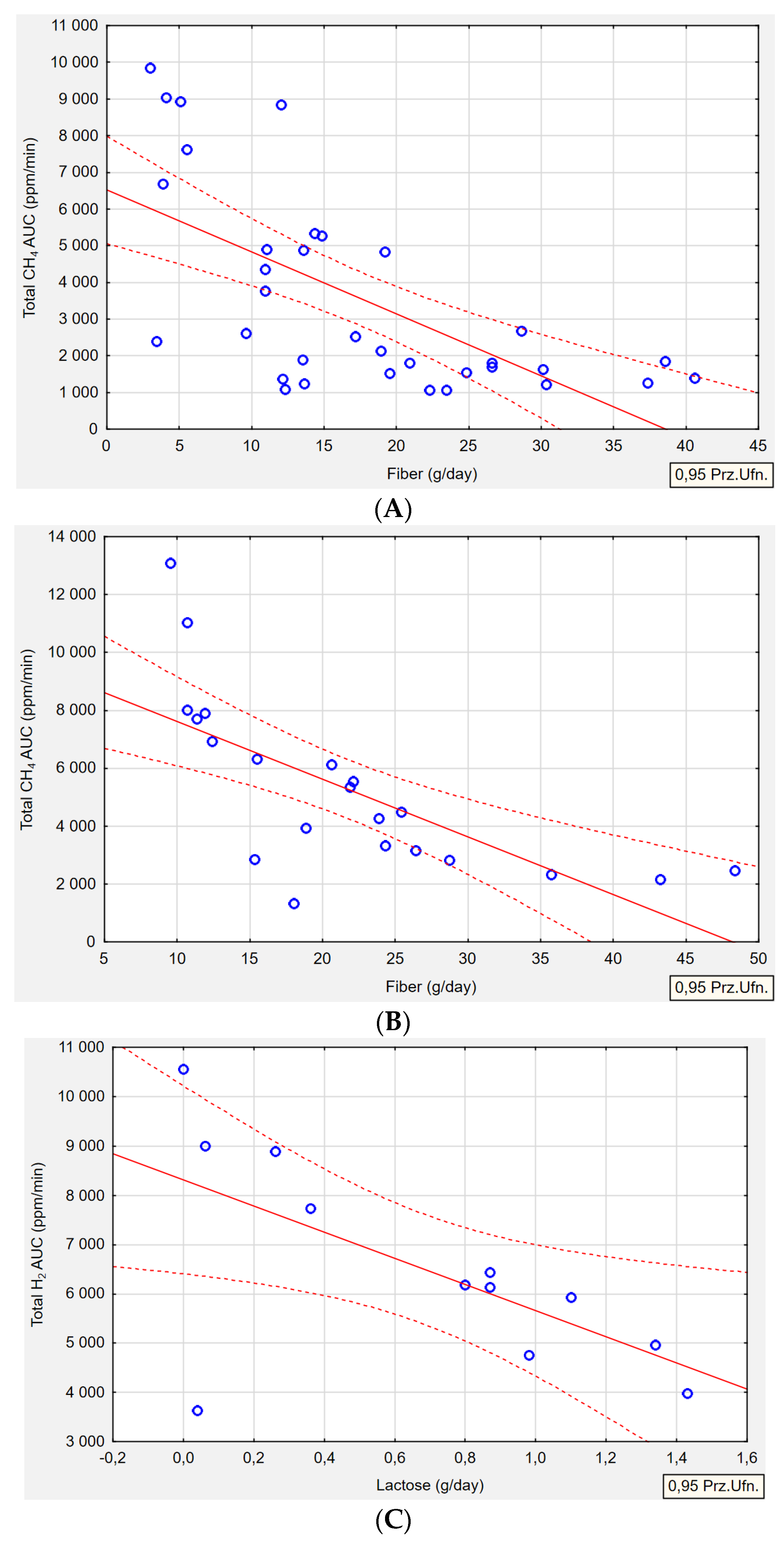
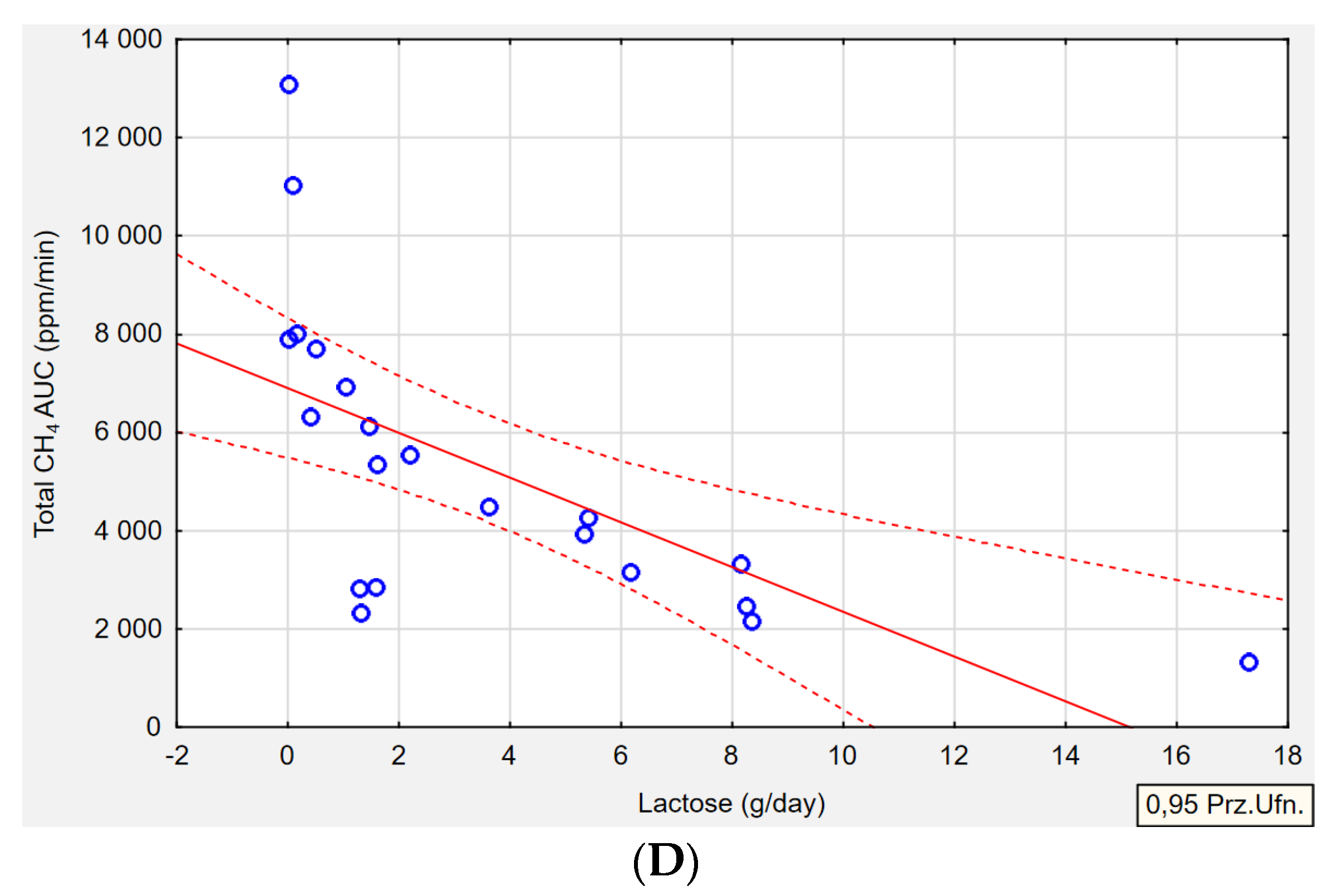
2.6.2. Dietary Correlations
3. Discussion
3.1. Biochemical Parameters
3.1.1. Vitamin D
3.1.2. Ferritin and Iron
3.1.3. Folic Acid
3.1.4. Vitamin B12 (Cobalamin)
3.2. Dietary Intake
3.2.1. Fiber
3.2.2. Lactose
3.2.3. Fat
3.2.4. Vitamin B12
3.2.5. Other Nutrients Intake
4. Materials and Methods
4.1. Sample
4.2. Lactulose Hydrogen–Methane Breath Test (LHMB)
4.3. Biochemical Assessment
4.4. Dietary Assessment Tool
4.5. Statistical Analysis
4.6. Outcome Measures
- Hydrogen-dominant SIBO (H+): H2 > 20 ppm from the baseline within 90 min, CH4 < 10 ppm any time during the test;
- Methane-dominant SIBO (M+): H2 < 20 ppm from the baseline within 90 min, CH4 >10 ppm any time during the test;
- Hydrogen–methane-dominant SIBO (H+/M+): H2 > 20 ppm from the baseline within 90 min, CH4 > 10 ppm any time during the test.
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, J.; Ho, W.T.P.; Liu, C.; Chow, S.K.H.; Ip, M.; Yu, J.; Wong, H.S.; Cheung, W.H.; Sung, J.J.Y.; Wong, R.M.Y. The Role of Gut Microbiota in Bone Homeostasis. Bone Jt. Res. 2021, 10, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Ogunrinola, G.A.; Oyewale, J.O.; Oshamika, O.O.; Olasehinde, G.I. The Human Microbiome and Its Impacts on Health. Int. J. Microbiol. 2020, 2020, 8045646. [Google Scholar] [CrossRef] [PubMed]
- Yamamura, R.; Inoue, K.Y.; Nishino, K.; Yamasaki, S. Intestinal and Fecal PH in Human Health. Front. Microbiomes 2023, 2, 1192316. [Google Scholar] [CrossRef]
- Avelar Rodriguez, D.; Ryan, P.M.D.; Toro Monjaraz, E.M.; Ramirez Mayans, J.A.; Quigley, E.M. Small Intestinal Bacterial Overgrowth in Children: A State-of-the-Art Review. Front. Pediatr. 2019, 7, 363. [Google Scholar] [CrossRef]
- Kastl, A.J.; Terry, N.A.; Wu, G.D.; Albenberg, L.G. The Structure and Function of the Human Small Intestinal Microbiota: Current Understanding and Future Directions. Cell. Mol. Gastroenterol. Hepatol. 2020, 9, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Ginnebaugh, B.; Chey, W.D.; Saad, R. Small Intestinal Bacterial Overgrowth: How to Diagnose and Treat (and Then Treat Again). Gastroenterol. Clin. N. Am. 2020, 49, 571–587. [Google Scholar] [CrossRef]
- Schlechte, J.; Skalosky, I.; Geuking, M.B.; McDonald, B. Long-Distance Relationships—Regulation of Systemic Host Defense against Infections by the Gut Microbiota. Mucosal Immunol. 2022, 15, 809–818. [Google Scholar] [CrossRef]
- Iacob, S.; Iacob, D.G.; Luminos, L.M. Intestinal Microbiota as a Host Defense Mechanism to Infectious Threats. Front. Microbiol. 2019, 9, 3328. [Google Scholar] [CrossRef]
- Takakura, W.; Pimentel, M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome—An Update. Front. Psychiatry 2020, 11, 664. [Google Scholar] [CrossRef]
- Skrzydło-Radomańska, B.; Cukrowska, B. How to Recognize and Treat Small Intestinal Bacterial Overgrowth? J. Clin. Med. 2022, 11, 6017. [Google Scholar] [CrossRef]
- Yao, Q.; Yu, Z.; Meng, Q.; Chen, J.; Liu, Y.; Song, W.; Ren, X.; Zhou, J.; Chen, X. The Role of Small Intestinal Bacterial Overgrowth in Obesity and Its Related Diseases. Biochem. Pharmacol. 2023, 212, 115546. [Google Scholar] [CrossRef] [PubMed]
- Rezaie, A.; Buresi, M.; Lembo, A.; Lin, H.; McCallum, R.; Rao, S.; Schmulson, M.; Valdovinos, M.; Zakko, S.; Pimentel, M. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. Am. J. Gastroenterol. 2017, 112, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Rezaie, A. Pros and Cons of Breath Testing for Small Intestinal Bacterial Overgrowth and Intestinal Methanogen Overgrowth. Gastroenterol. Hepatol. 2023, 19, 140–146. [Google Scholar]
- Villanueva-Millan, M.J.; Leite, G.; Wang, J.; Morales, W.; Parodi, G.; Pimentel, M.L.; Barlow, G.M.; Mathur, R.; Rezaie, A.; Sanchez, M.; et al. Methanogens and Hydrogen Sulfide Producing Bacteria Guide Distinct Gut Microbe Profiles and Irritable Bowel Syndrome Subtypes. Am. J. Gastroenterol. 2022, 117, 2055–2066. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.W.; Shorten, P.R.; Altermann, E.H.; Roy, N.C.; McNabb, W.C. Hydrogen Cross-Feeders of the Human Gastrointestinal Tract. Gut Microbes 2019, 10, 270–288. [Google Scholar] [CrossRef] [PubMed]
- Gaci, N.; Borrel, G.; Tottey, W.; O’Toole, P.W.; Brugère, J.F. Archaea and the Human Gut: New Beginning of an Old Story. World J. Gastroenterol. 2014, 20, 16062–16078. [Google Scholar] [CrossRef] [PubMed]
- Sroka, N.; Rydzewska-Rosołowska, A.; Kakareko, K.; Rosołowski, M.; Głowińska, I.; Hryszko, T. Show Me What You Have Inside—The Complex Interplay between SIBO and Multiple Medical Conditions—A Systematic Review. Nutrients 2023, 15, 90. [Google Scholar] [CrossRef] [PubMed]
- Bushyhead, D.; Quigley, E.M.M. Small Intestinal Bacterial Overgrowth—Pathophysiology and Its Implications for Definition and Management. Gastroenterology 2022, 163, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Singh, R.; Ro, S.; Ghoshal, U.C. Gut Microbiota Dysbiosis in Functional Gastrointestinal Disorders: Underpinning the Symptoms and Pathophysiology. JGH Open 2021, 5, 976–987. [Google Scholar] [CrossRef]
- Losurdo, G.; Leandro, G.; Ierardi, E.; Perri, F.; Barone, M.; Principi, M.; Di Leo, A. Breath Tests for the Non-Invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review with Meta-Analysis. J. Neurogastroenterol. Motil. 2020, 26, 16–28. [Google Scholar] [CrossRef]
- Adike, A.; DiBaise, J.K. Small Intestinal Bacterial Overgrowth: Nutritional Implications, Diagnosis, and Management. Gastroenterol. Clin. N. Am. 2018, 47, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Talley, N.J.; Holtmann, G. Current and Future Approaches for Diagnosing Small Intestinal Dysbiosis in Patients with Symptoms of Functional Dyspepsia. Front. Neurosci. 2022, 16, 830356. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Morrison, M.; Burger, D.; Martin, N.; Rich, J.; Jones, M.; Koloski, N.; Walker, M.M.; Talley, N.J.; Holtmann, G.J. Systematic Review with Meta-Analysis: The Prevalence of Small Intestinal Bacterial Overgrowth in Inflammatory Bowel Disease. Aliment. Pharmacol. Ther. 2019, 49, 624–635. [Google Scholar] [CrossRef] [PubMed]
- Ghoshal, U.C.; Shukla, R.; Ghoshal, U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver 2017, 11, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Losurdo, G.; D’abramo, F.S.; Indellicati, G.; Lillo, C.; Ierardi, E.; Di Leo, A. The Influence of Small Intestinal Bacterial Overgrowth in Digestive and Extra-Intestinal Disorders. Int. J. Mol. Sci. 2020, 21, 3531. [Google Scholar] [CrossRef] [PubMed]
- Ierardi, E.; Losurdo, G.; Sorrentino, C.; Giorgio, F.; Rossi, G.; Marinaro, A.; Romagno, K.R.; Di Leo, A.; Principi, M. Macronutrient Intakes in Obese Subjects with or without Small Intestinal Bacterial Overgrowth: An Alimentary Survey. Scand. J. Gastroenterol. 2016, 51, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Leeming, E.R.; Johnson, A.J.; Spector, T.D.; Roy, C.I.L. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients 2019, 11, 2862. [Google Scholar] [CrossRef] [PubMed]
- Ferenc, K.; Sokal-Dembowska, A.; Helma, K.; Motyka, E.; Jarmakiewicz-Czaja, S.; Filip, R. Modulation of the Gut Microbiota by Nutrition and Its Relationship to Epigenetics. Int. J. Mol. Sci. 2024, 25, 1228. [Google Scholar] [CrossRef] [PubMed]
- Hills, R.D.; Pontefract, B.A.; Mishcon, H.R.; Black, C.A.; Sutton, S.C.; Theberge, C.R. Gut Microbiome: Profound Implications for Diet and Disease. Nutrients 2019, 11, 1613. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Chang, H.W.; Yan, D.; Lee, K.M.; Ucmak, D.; Wong, K.; Abrouk, M.; Farahnik, B.; Nakamura, M.; Zhu, T.H.; et al. Influence of Diet on the Gut Microbiome and Implications for Human Health. J. Transl. Med. 2017, 15, 73. [Google Scholar] [CrossRef]
- Souza, C.; Rocha, R.; Cotrim, H.P. Diet and Intestinal Bacterial Overgrowth: Is There Evidence? World J. Clin. Cases 2022, 10, 4713–4716. [Google Scholar] [CrossRef] [PubMed]
- Halmos, E.P.; Power, V.A.; Shepherd, S.J.; Gibson, P.R.; Muir, J.G. A Diet Low in FODMAPs Reduces Symptoms of Irritable Bowel Syndrome. Gastroenterology 2014, 146, 67–75.e5. [Google Scholar] [CrossRef] [PubMed]
- Wielgosz-Grochowska, J.P.; Domanski, N.; Drywień, M.E. Efficacy of an Irritable Bowel Syndrome Diet in the Treatment of Small Intestinal Bacterial Overgrowth: A Narrative Review. Nutrients 2022, 14, 3382. [Google Scholar] [CrossRef] [PubMed]
- Losso, J.N. Food Processing, Dysbiosis, Gastrointestinal Inflammatory Diseases, and Antiangiogenic Functional Foods or Beverages. Annu. Rev. Food Sci. Technol. 2021, 12, 235–258. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, H.M.; Ralph, F.S.E.; Irving, P.M.; Whelan, K.; Lomer, M.C.E. Nutrient Intake, Diet Quality, and Diet Diversity in Irritable Bowel Syndrome and the Impact of the Low FODMAP Diet. J. Acad. Nutr. Diet. 2020, 120, 535–547. [Google Scholar] [CrossRef]
- Bellini, M.; Tonarelli, S.; Nagy, A.G.; Pancetti, A.; Costa, F.; Ricchiuti, A.; de Bortoli, N.; Mosca, M.; Marchi, S.; Rossi, A. Low FODMAP Diet: Evidence, Doubts, and Hopes. Nutrients 2020, 12, 148. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, H.M.; Scholz, M.; Lomer, M.C.; Ralph, F.S.; Irving, P.M.; Lindsay, J.O.; Fava, F.; Tuohy, K.; Whelan, K. Gut Microbiota Associations with Diet in Irritable Bowel Syndrome and the Effect of Low FODMAP Diet and Probiotics. Clin. Nutr. 2021, 40, 1861–1870. [Google Scholar] [CrossRef] [PubMed]
- Wielgosz-Grochowska, J.P.; Domanski, N.; Drywień, M.E. Influence of Body Composition and Specific Anthropometric Parameters on SIBO Type. Nutrients 2023, 15, 4035. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; O’Keefe, J. The Importance of Maintaining a Low Omega-6/Omega-3 Ratio for Reducing the Risk of Autoimmune Diseases, Asthma, and Allergies. Mo. Med. 2021, 118, 453–459. [Google Scholar]
- Simopoulos, A.P. The Importance of the Ratio of Omega-6/Omega-3 Essential Fatty Acids. Biomed. Pharmacother. 2002, 56, 365–379. [Google Scholar] [CrossRef]
- Pimentel, M.; Saad, R.J.; Long, M.D.; Rao, S.S.C. ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. Am. J. Gastroenterol. 2020, 115, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Frame, L.A.; Costa, E.; Jackson, S.A. Current Explorations of Nutrition and the Gut Microbiome: A Comprehensive Evaluation of the Review Literature. Nutr. Rev. 2020, 78, 798–812. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, E.M. The Role of Gut Microbiota in Nutritional Status. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Miazga, A.; Osiński, M.; Cichy, W.; Zaba, R. Current Views on the Etiopathogenesis, Clinical Manifestation, Diagnostics, Treatment and Correlation with Other Nosological Entities of SIBO. Adv. Med. Sci. 2015, 60, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Xu, Y.; Zhang, J.; Sun, Z.; Ban, Y.; Wang, B.; Hou, X.; Cai, Y.; Li, J.; Wang, M.; et al. Application of Methane and Hydrogen-Based Breath Test in the Study of Gestational Diabetes Mellitus and Intestinal Microbes. Diabetes Res. Clin. Pract. 2021, 176, 108818. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.A.; Baker, J.R.; Wamsteker, E.J.; Saad, R.; DiMagno, M.J. Small Intestinal Bacterial Overgrowth Is Common in Chronic Pancreatitis and Associates with Diabetes, Chronic Pancreatitis Severity, Low Zinc Levels, and Opiate Use. Am. J. Gastroenterol. 2019, 114, 1163–1171. [Google Scholar] [CrossRef] [PubMed]
- Tauber, M.; Avouac, J.; Benahmed, A.; Barbot, L.; Coustet, B.; Kahan, A.; Allanore, Y. Prevalence and Predictors of Small Intestinal Bacterial Overgrowth in Systemic Sclerosis Patients with Gastrointestinal Symptoms. Clin. Exp. Rheumatol. 2014, 32, 5–10. [Google Scholar]
- Kubota, Y.; Nagano, H.; Ishii, K.; Kono, T.; Kono, S.; Akita, S.; Mitsukawa, N.; Tanaka, T. Small Intestinal Bacterial Overgrowth as a Cause of Protracted Wound Healing and Vitamin D Deficiency in a Spinal Cord Injured Patient with a Sacral Pressure Sore: A Case Report. BMC Gastroenterol. 2020, 20, 283. [Google Scholar] [CrossRef]
- Stotzer, P.O.; Johansson, C.; Mellström, D.; Lindstedt, G.; Kilander, A.F. Bone Mineral Density in Patients with Small Intestinal Bacterial Overgrowth. Hepatogastroenterology 2003, 50, 1415–1418. [Google Scholar]
- Daru, J.; Allotey, J.; Peña-Rosas, J.P.; Khan, K.S. Serum Ferritin Thresholds for the Diagnosis of Iron Deficiency in Pregnancy: A Systematic Review. Transfus. Med. 2017, 27, 167–174. [Google Scholar] [CrossRef]
- Bohm, M.; Shin, A.; Teagarden, S.; Xu, H.; Gupta, A.; Siwiec, R.; Nelson, D.; Wo, J.M. Risk Factors Associated with Upper Aerodigestive Tract or Coliform Bacterial Overgrowth of the Small Intestine in Symptomatic Patients. J. Clin. Gastroenterol. 2020, 54, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Rosell-Díaz, M.; Santos-González, E.; Motger-Albertí, A.; Ramió-Torrentà, L.; Garre-Olmo, J.; Pérez-Brocal, V.; Moya, A.; Jové, M.; Pamplona, R.; Puig, J.; et al. Gut Microbiota Links to Serum Ferritin and Cognition. Gut Microbes 2023, 15, 2290318. [Google Scholar] [CrossRef] [PubMed]
- Rizos, E.; Pyleris, E.; Pimentel, M.; Triantafyllou, K.; Giamarellos-Bourboulis, E.J. Small Intestine Bacterial Overgrowth Can Form an Indigenous Proinflammatory Environment in the Duodenum: A Prospective Study. Microorganisms 2022, 10, 960. [Google Scholar] [CrossRef]
- Banaszak, M.; Górna, I.; Woźniak, D.; Przysławski, J.; Drzymała-Czyż, S. Association between Gut Dysbiosis and the Occurrence of SIBO, LIBO, SIFO and IMO. Microorganisms 2023, 11, 573. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.; Cacoub, P.; Macdougall, I.C.; Peyrin-Biroulet, L. Iron Deficiency Anaemia. Lancet 2016, 387, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Braun, V. Iron Uptake Mechanisms and Their Regulation in Pathogenic Bacteria. Int. J. Med. Microbiol. 2001, 291, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Bloor, S.R.; Schutte, R.; Hobson, A.R. Oral Iron Supplementation—Gastrointestinal Side Effects and the Impact on the Gut Microbiota. Microbiol. Res. 2021, 12, 491–502. [Google Scholar] [CrossRef]
- Triantafyllou, K.; Chang, C.; Pimentel, M. Methanogens, Methane and Gastrointestinal Motility. J. Neurogastroenterol. Motil. 2014, 20, 31–40. [Google Scholar] [CrossRef]
- Platovsky, A.; Tokayer, A. Folate Levels in Patients with Small Intestinal Bacterial Overgrowth (SIBO). Am. J. Gastroenterol. 2014, 109, S530. [Google Scholar] [CrossRef]
- Marie, I.; Ducrotté, P.; Denis, P.; Menard, J.F.; Levesque, H. Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Rheumatology 2009, 48, 1314–1319. [Google Scholar] [CrossRef]
- Kaniel, O.; Sherf-Dagan, S.; Szold, A.; Langer, P.; Khalfin, B.; Kessler, Y.; Raziel, A.; Sakran, N.; Motro, Y.; Goitein, D.; et al. The Effects of One Anastomosis Gastric Bypass Surgery on the Gastrointestinal Tract. Nutrients 2022, 14, 304. [Google Scholar] [CrossRef] [PubMed]
- Achufusi, T.G.O.; Sharma, A.; Zamora, E.A.; Manocha, D. Small Intestinal Bacterial Overgrowth: Comprehensive Review of Diagnosis, Prevention, and Treatment Methods. Cureus 2020, 12, e8860. [Google Scholar] [CrossRef] [PubMed]
- Quigley, E.M.M.; Murray, J.A.; Pimentel, M. AGA Clinical Practice Update on Small Intestinal Bacterial Overgrowth: Expert Review. Gastroenterology 2020, 159, 1526–1532. [Google Scholar] [CrossRef]
- Zaidel, O.; Lin, H.C. Uninvited Guests: The Impact of Small Intestinal Bacterial Overgrowth on Nutritional Status. Pract. Gastroenterol. 2003, 27, 27–30+33. [Google Scholar]
- Kok, D.E.; Steegenga, W.T.; Smid, E.J.; Zoetendal, E.G.; Ulrich, C.M.; Kampman, E. Bacterial Folate Biosynthesis and Colorectal Cancer Risk: More than Just a Gut Feeling. Crit. Rev. Food Sci. Nutr. 2020, 60, 244–256. [Google Scholar] [CrossRef] [PubMed]
- Engevik, M.A.; Morra, C.N.; Röth, D.; Engevik, K.; Spinler, J.K.; Devaraj, S.; Crawford, S.E.; Estes, M.K.; Kalkum, M.; Versalovic, J. Microbial Metabolic Capacity for Intestinal Folate Production and Modulation of Host Folate Receptors. Front. Microbiol. 2019, 10, 2305. [Google Scholar] [CrossRef] [PubMed]
- Madigan, K.E.; Bundy, R.; Weinberg, R.B. Distinctive Clinical Correlates of Small Intestinal Bacterial Overgrowth with Methanogens. Clin. Gastroenterol. Hepatol. 2022, 20, 1598–1605.e2. [Google Scholar] [CrossRef] [PubMed]
- Rowley, C.A.; Kendall, M.M. To B 12 or Not to B 12: Five Questions on the Role of Cobalamin in Host-Microbial Interactions. PLoS Pathog. 2019, 15, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Arango, L.F.; Barrett, H.L.; McIntyre, H.D.; Callaway, L.K.; Morrison, M.; Nitert, M.D. Contributions of the Maternal Oral and Gut Microbiome to Placental Microbial Colonization in Overweight and Obese Pregnant Women. Sci. Rep. 2017, 7, 2860. [Google Scholar] [CrossRef]
- Desai, M.S.; Seekatz, A.M.; Koropatkin, N.M.; Kamada, N.; Hickey, C.A.; Wolter, M.; Pudlo, N.A.; Kitamoto, S.; Terrapon, N.; Muller, A.; et al. A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility. Cell 2016, 167, 1339–1353. [Google Scholar] [CrossRef]
- Fu, J.; Zheng, Y.; Gao, Y.; Xu, W. Dietary Fiber Intake and Gut Microbiota in Human Health. Microorganisms 2022, 10, 2507. [Google Scholar] [CrossRef] [PubMed]
- Parlesak, A.; Klein, B.; Schecher, K.; Bode, J.C.; Bode, C. Prevalence of Small Bowel Bacterial Overgrowth and Its Association with Nutrition Intake in Nonhospitalized Older Adults. J. Am. Geriatr. Soc. 2003, 51, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Cortez, A.P.B.; Fisberg, M.; de Morais, M.B. Macronutrient Intakes in Overweight Adolescents with or without Small Intestinal Bacterial Overgrowth. Scand. J. Gastroenterol. 2017, 52, 228–229. [Google Scholar] [CrossRef] [PubMed]
- Saffouri, G.B.; Shields-Cutler, R.R.; Chen, J.; Yang, Y.; Lekatz, H.R.; Hale, V.L.; Cho, J.M.; Battaglioli, E.J.; Bhattarai, Y.; Thompson, K.J.; et al. Small Intestinal Microbial Dysbiosis Underlies Symptoms Associated with Functional Gastrointestinal Disorders. Nat. Commun. 2019, 10, 2012. [Google Scholar] [CrossRef] [PubMed]
- Jo, I.H.; Paik, C.-N.; Kim, Y.-J.; Lee, J.M.; Choi, S.Y.; Hong, K.P. Lactase Deficiency Diagnosed by Endoscopic Biopsy-Based Method Is Associated with Positivity to Glucose Breath Test. J. Neurogastroenterol. Motil. 2023, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Almeida, J.A.; Kim, R.; Stoita, A.; Mciver, C.J.; Kurtovic, J.; Riordan, S.M. Lactose Malabsorption in the Elderly: Role of Small Intestinal Bacterial Overgrowth. Scand. J. Gastroenterol. 2008, 43, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Perets, T.T.; Hamouda, D.; Layfer, O.; Ashorov, O.; Boltin, D.; Levy, S.; Niv, Y.; Dickman, R. Small Intestinal Bacterial Overgrowth May Increase the Likelihood of Lactose and Sorbitol but Not Fructose Intolerance False Positive Diagnosis. Ann. Clin. Lab. Sci. 2017, 47, 447–451. [Google Scholar] [PubMed]
- Enko, D.; Rezanka, E.; Stolba, R.; Halwachs-Baumann, G. Lactose Malabsorption Testing in Daily Clinical Practice: A Critical Retrospective Analysis and Comparison of the Hydrogen/Methane Breath Test and Genetic Test (C/T-13910 Polymorphism) Results. Gastroenterol. Res. Pract. 2014, 2014, 464382. [Google Scholar] [CrossRef] [PubMed]
- Scanu, A.M.; Bull, T.J.; Cannas, S.; Sanderson, J.D.; Sechi, L.A.; Dettori, G.; Zanetti, S.; Hermon-Taylor, J. Mycobacterium Avium Subspecies Paratuberculosis Infection in Cases of Irritable Bowel Syndrome and Comparison with Crohn’s Disease and Johne’s Disease: Common Neural and Immune Pathogenicities. J. Clin. Microbiol. 2007, 45, 3883–3890. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Misselwitz, B.; Dai, N.; Fox, M. Lactose Intolerance in Adults: Biological Mechanism and Dietary Management. Nutrients 2015, 7, 8020–8035. [Google Scholar] [CrossRef]
- Mathur, R.; Kim, G.; Morales, W.; Sung, J.; Rooks, E.; Pokkunuri, V.; Weitsman, S.; Barlow, G.M.; Chang, C.; Pimentel, M. Intestinal Methanobrevibacter Smithii but Not Total Bacteria Is Related to Diet-Induced Weight Gain in Rats. Obesity 2013, 21, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Agah, S.; Aminianfar, A.; Keshteli, A.H.; Bitarafan, V.; Adibi, P.; Esmaillzadeh, A.; Feinle-Bisset, C. Association between Dietary Macronutrient Intake and Symptoms in Uninvestigated Dyspepsia: Evidence from a Population-Based, Cross-Sectional Study. Nutrients 2022, 14, 2577. [Google Scholar] [CrossRef] [PubMed]
- Herdiana, Y. Functional Food in Relation to Gastroesophageal Reflux Disease (GERD). Nutrients 2023, 15, 3583. [Google Scholar] [CrossRef] [PubMed]
- Duncanson, K.R.; Talley, N.J.; Walker, M.M.; Burrows, T.L. Food and Functional Dyspepsia: A Systematic Review. J. Hum. Nutr. Diet. 2018, 31, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Cinquanta, L.; Fontana, D.E.; Bizzaro, N. Chemiluminescent Immunoassay Technology: What Does It Change in Autoantibody Detection? Autoimmun. Highlights 2017, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Proskurnin, M.; Samarina, T. Rapid Assessment of Iron in Blood Plasma and Serum by Spectrophotometry with Cloud-Point Extraction. F1000Research 2015, 4, 2–7. [Google Scholar] [CrossRef]
- Vargas-Uricoechea, H.; Nogueira, J.P.; Pinzón-Fernández, M.V.; Agredo-Delgado, V.; Vargas-Sierra, H.D. Population Status of Vitamin B12 Values in the General Population and in Individuals with Type 2 Diabetes, in Southwestern Colombia. Nutrients 2023, 15, 2357. [Google Scholar] [CrossRef]
- Elgormus, Y.; Okuyan, O.; Dumur, S.; Sayili, U.; Uzun, H. The Epidemiology of Deficiency of Vitamin B12 in Preschool Children in Turkey. Medicina 2023, 59, 1809. [Google Scholar] [CrossRef]
- Ashraf, M.J.; Cook, J.R.; Rothberg, M.B. Clinical Utility of Folic Acid Testing for Patients with Anemia or Dementia. J. Gen. Intern. Med. 2008, 23, 824–826. [Google Scholar] [CrossRef]
- Koulaouzidis, A.; Cottier, R.; Bhat, S.; Said, E.; Linaker, B.D.; Saeed, A.A. A Ferritin Level > 50 Μg/L Is Frequently Consistent with Iron Deficiency. Eur. J. Intern. Med. 2009, 20, 168–170. [Google Scholar] [CrossRef]
- Breymann, C.; Römer, T.; Dudenhausen, J.W. Treatment of Iron Deficiency in Women. Geburtshilfe Frauenheilkd. 2013, 73, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Gómez-Ramírez, S.; Besser, M.; Pavía, J.; Gomollón, F.; Liumbruno, G.M.; Bhandari, S.; Cladellas, M.; Shander, A.; Auerbach, M. Current Misconceptions in Diagnosis and Management of Iron Deficiency. Blood Transfus. 2017, 15, 422–437. [Google Scholar] [CrossRef] [PubMed]
- Girelli, D.; Ugolini, S.; Busti, F.; Marchi, G.; Castagna, A. Modern Iron Replacement Therapy: Clinical and Pathophysiological Insights. Int. J. Hematol. 2018, 107, 16–30. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Knovich, M.A.; Coffman, L.G.; Torti, F.M.; Torti, S.V. Serum Ferritin: Past, Present and Future. Biochim. Biophys. Acta-Gen. Subj. 2010, 1800, 760–769. [Google Scholar] [CrossRef]
- Szponar, L.; Wolnicka, K.; Rychlik, E. Album Fotografii Produktów i Potraw/Album of Photographs of Food Products and Dishes; National Food and Nutrition Institute: Warsaw, Poland, 2000; ISBN 8386060514. [Google Scholar]
- Wojtasik, A.; Woźniak, A.; Stoś, K.; Jarosz, M. Normy Żywienia Dla Populacji Polski i Ich Zastosowanie; Narodowy Instytut Zdrowia Publicznego: Warsaw, Poland, 2020; ISBN 9788365870285.
- Johansson, G.; Westerterp, K.R. Assessment of the Physical Activity Level with Two Questions: Validation with Doubly Labeled Water. Int. J. Obes. 2008, 32, 1031–1033. [Google Scholar] [CrossRef]
- Simopoulos, A.P.; DiNicolantonio, J.J. The Importance of a Balanced ω-6 to ω-3 Ratio in the Prevention and Management of Obesity. Open Heart 2016, 3, e000385. [Google Scholar] [CrossRef]

| H+ (n = 12) | M+ (n = 21) | H+/M+ (n = 34) | p-Value * | |
|---|---|---|---|---|
| Median (min–max) | Median (min–max) | Median (min–max) | ||
| Age (years) | 35.25 ± 11.67 | 33.29 ± 6.56 | 32.71 ± 8.23 | 0.776 |
| Gender | 0.921 | |||
| Female | 9 (75.0%) | 17 (80.9) | 27 (79.4%) | |
| Male | 3 (25.0%) | 4 (19.1%) | 7 (20.5%) | |
| Height (cm) | 172.5 (158.0–192.0) a | 170.0 (159.0–185.0) ab | 166.0 (153.0–189.0) b | 0.023 * |
| Weight (kg) | 65.7 (45.0–109.8) | 62.2 (45.8–92.3) | 61.3 (39.0–86.2) | 0.236 |
| BMI (kg/m2) | 21.8 (18.0–32.3) | 21.0 (17.2–32.6) | 21.7 (16.7–27.6) | 0.711 |
| PAL | 1.4 (1.4–1.6) | 1.4 (1.4–1.6) | 1.4 (1.4–1.7) | 0.487 |
| Parameter | SIBO Subtypes | p-Value * | ||
|---|---|---|---|---|
| H+ (n = 12) | M+ (n = 21) | H+/M+ (n = 34) | ||
| Median (min–max) | Median (min–max) | Median (min–max) | ||
| Vitamin D 25(OH)D Total (ng/mL) | 27.8 (13.2–37.6) | 26.3 (12.4–66.0) | 29.6 (13.2–60.1) | 0.389 |
| Vitamin B12 (pg/mL) | 307.5 (226.0–668.0) | 452.0 (218.0–846.0) | 437.5 (220.8–830.0) | 0.104 |
| Folicacid (ng/mL) | 6.2 (2.8–19.2) | 7.1 (3.1–15.0) | 6.4 (3.1–20.5) | 0.707 |
| Ferritin (ng/mL) | 62.0 (16.0–104.5) a | 35.0 (11.0–99.0) ab | 30.5 (5.6–105.2) b | 0.042 * |
| Iron (μg/dL) | 103.5 (84.0–168) | 81.0 (35.0–157.0) | 97.0 (31.0–185.0) | 0.319 |
| Level of Parameter | SIBO Subtypes | p-Value * | ||
|---|---|---|---|---|
| H+ (n = 12) | M+ (n = 21) | H+/M+ (n = 34) | ||
| Vitamin D 25(OH)D Total | 0.304 | |||
| Deficiency (<20 ng/mL) | 3 (25.0%) | 6 (28.5%) | 6 (17.6%) | |
| Suboptimal (20–30 ng/mL) | 5 (41.6%) | 9 (42.8%) | 12 (35.3%) | |
| Optimal (>30–50 ng/mL) | 4 (33.4%) | 9 (23.8%) | 15 (44.1%) | |
| High (50–100 ng/mL) | 0 (0%) | 1 (4.9%) | 1 (3%) | |
| Vitamin B12 | 0.098 | |||
| Borderline (<200–300 pg/mL) | 6 (50%) | 4 (19.0%) | 7 (20.5%) | |
| Optimal (>300–883 pg/mL) | 6 (50%) | 17 (81.0%) | 27 (75.5%) | |
| Folic acid | 0.504 | |||
| Low (<2.1–3.0 ng/mL) | 1 (8.3%) | 0 (0%) | 0 (0%) | |
| Borderline (>3.0–4.0 ng/mL) | 1 (8.3%) | 1 (4.8%) | 4 (11.8%) | |
| Optimal (>4.0–20.5 ng/mL) | 10 (83.4%) | 20 (95.2%) | 30 (88.2%) | |
| Ferritin (ng/mL) | 0.139 | |||
| Iron deficiency (<10.0–15.0 ng/mL) | 0 (0%) | 11 (52.4%) | 7 (20.5%) | |
| Early iron deficiency (>15.0–50.0 ng/mL) | 5 (41.7%) | 3 (14.3%) | 16 (47.1%) | |
| Optimal (>50.0–270 ng/mL) | 7 (58.3%) | 7 (33.3%) | 11 (32.4%) | |
| Iron | 0.504 | |||
| Low (<37.0 μg/dL W; <59.0 μg/dL M) | 0 (0%) | 1 (4.8%) | 6 (17.6%) | |
| Optimal (>37.0–145.0 μg/dL W; >59.0–158.0 μg/dL M) | 10 (83.4%) | 19 (90.4%) | 25 (73.6%) | |
| High (>145.0 μg/dL W; >158.0 μg/dL M) | 2 (16.6%) | 1 (4.8%) | 3 (8.8%) | |
| Energy and Nutrient Intake | SIBO Subtypes | p-Value * | ||
|---|---|---|---|---|
| H+ (n = 12) | M+ (n = 21) | H+/M+ (n = 34) | ||
| Median (min–max) | Median (min–max) | Median (min–max) | ||
| Energy (kcal) | 1785.5 (1330.0–2934.0) | 1785.0 (1249.0–2876.0) | 1695.0 (919.0–2971.0) | 0.794 |
| BEE (kcal) | 1390.0 (1076.0–2122.0) | 1415.0 (1186.0–1905.0) | 1285.0 (1054.0–1740.0) | 0.072 |
| TEE (kcal) | 1946.7 (1506.4–1506.4) | 1981.0 (1660.4–2667.0) | 1799.0 (1475.6–2436.0) | 0.156 |
| Carbohydrates (%E) | 49.3 (34.7–70.35) | 43.8 (27.3–52.6) | 44.3 (12.87–73.78) | 0.092 |
| Carbohydrates (g) | 241.4 (157.9–512.2) | 176.6 (128.6–315.0) | 214.9 (33.0–427.6) | 0.274 |
| Fiber (g) | 12.3 (7.1–19.4) a | 20.6 (9.5–48.4) b | 14.6 (2.9–40.6) ab | 0.036 * |
| Fructose (g) | 8.5 (1.4–24.7) | 4.4 (0.0–15.1) | 4.2 (0.0–16.4) | 0.110 |
| Lactose (g) | 0.8 (0.0–1.4) a | 1.6 (0–17.3) ab | 5.4 (0.0–27.1) b | 0.001 * |
| Protein (%E) | 15.6 (8.3–28.8) | 18.2 (9.4–23.9) | 17.3 (9.2–28.9) | 0.860 |
| Protein (g) | 69.9 (42.4–145.3) | 80.0 (38.4–171.1) | 77.8 (31.4–154.7) | 0.869 |
| Protein (g/kg) | 1.1 (0.6–2.5) | 1.4 (0.4–2.0) | 1.2 (0.5–2.3) | 0.752 |
| Fat (%E) | 32.1 (17.9–50.5) c | 40.6 (32.2–52.3) d | 41.4 (26.0–64.3) d | 0.019 |
| Fat (g) | 62.9 (31.5–131.0) | 80.6 (51.3–110.7) | 86.1 (29.6–148.0) | 0.210 |
| SFA (%E) | 10.2 (3.0–25.4) | 13.5 (5.9–27.3) | 14.2 (1.0–40.5) | 0.336 |
| SFA (g) | 21.8 (9.9–66.8) | 24.8 (12.5–54.3) | 28.5 (1.5–71.8) | 0.366 |
| MUFA (%E) | 14.9 (6.7–33.7) | 16.2 (10.8–24.6) | 17.9 (6.3–78.2) | 0.392 |
| MUFA (g) | 33.1 (9.9–88.5) | 31.5 (16.8–55.9) | 37.1 (6.5–126.8) | 0.673 |
| Omega-3 (g) | 1.6 (0.3–26.1) | 1.7 (0.4–6.8) | 1.2 (0.4–12.1) | 0.878 |
| Omega-6 (g) | 7.5 (1.3–12.9) | 6.8 (3.1–17.8) | 7.8 (2.0–20.9) | 0.693 |
| Ratio omega-6/omega-3 | 4:1 (0.5:1–15.1:1) | 6:1 (0.6:1–13.5:1) | 7.5:1 (0.5:1–17.4:1) | 0.300 |
| PUFA (%E) | 6.1 (1.5–15.5) | 4.8 (3.0–12.6) | 6.3 (2.4–13.5) | 0.339 |
| PUFA (g) | 11.1 (4.8–40.4) | 9.7 (4.3–26.4) | 12.5 (2.8–34.4) | 0.611 |
| Cholesterol (mg) | 296.9 (63.6–1028.0) | 527.0 (117.4–1014.1) | 327.7 (15.6–1159.0) | 0.355 |
| Level of Nutrient Intake | SIBO Subtypes | References Norm | p-Value * | ||
|---|---|---|---|---|---|
| H+ (n = 12) | M+ (n = 21) | H+/M+ (n = 34) | |||
| Energy (kcal/day) Insufficient Sufficient Excessive | 4 (33.3%) 6 (50%) 2 (16.7%) | 11 (52.4%) 4 (19.1%) 6 (28.5%) | 15 (44.1%) 5 (14.7%) 14 (41.2%) | TEE | 0.225 |
| Carbohydrates (E%) Insufficient Sufficient Excessive | 5 (41.7%) 5 (41.6%) 2 (16.7%) | 11 (52.4%) 10 (47.6%) - | 18 (53.0%) 13 (38.2%) 3 (8.8%) | EAR (45–56%) | 0.875 |
| Fiber (g/day) Insufficient Sufficient | 12 (100%) - | 15 (71.4%) 6 (28.6%) | 25 (73.5%) 9 (26.5%) | AI (>25 g/day) | 0.123 |
| Protein (g/kg/day) Insufficient Sufficient Excessive | 2 (16.7%) 1 (8.3%) 9 (75%) | 2 (9.5%) 2 (9.5%) 17 (81%) | 2 (5.9%) 3 (8.8%) 29 (85.3%) | EAR (0.73 g/kg/day) | 0.766 |
| Protein (E%) Insufficient Sufficient Excessive | 1 (8.3%) 8 (66.7%) 3 (25%) | 1 (4.8%) 16 (76.2%) 4 (19%) | 2 (5.9%) 26 (76.5%) 6 (17.6%) | EAR (10–20%E) | 0.943 |
| Fat (E%) Sufficient Excessive | 8 (66.7%) a 4 (33.3%) a | 5 (23.8%) b 16 (76.2%) b | 10 (29.4%) b 24 (70.6%) b | RI (20–35%E) | 0.032 * |
| SFA (E%) Sufficient Excessive | 6 (50.0%) 6 (50.0%) | 6 (26.6%) 15 (71.4%) | 9 (26.5%) 25 (73.5%) | (<10%) | 0.308 |
| Micronutrients Intake | SIBO Subtypes | p-Value * | ||
|---|---|---|---|---|
| H+ (n = 12) Median (min–max) | M+ (n = 21) Median (min–max) | H+/M+ (n = 34) Median (min–max) | ||
| Vitamin A (μg) | 1087.5 (425.7–1704.0) | 868.8 (234.9–4133.2) | 923.1 (279.1–3887.2) | 0.982 |
| Vitamin D (μg) | 2.1 (0.5–19.1) | 3.1 (0.6–15.6) | 2.53 (0.0–19.5) | 0.203 |
| Vitamin E (μg) | 8.5 (3.8–18.3) | 10.2 (2.2–22.0) | 11.1 (2.78–44.43) | 0.727 |
| Vitamin B12 (μg) | 1.7 (0.8–6.8) | 3.1 (0.8–9.5) | 2.7 (0.2–12.9) | 0.206 |
| Folate (μg) | 227.6 (90.1–444.6) | 284.6 (106.1–691.0) | 245.8 (41.0–541.0) | 0.432 |
| Iron (mg) | 8.8 (5.8–16.2) | 9.8 (5.1–17.3) | 10.0 (4.2–19.3) | 0.615 |
| Calcium (mg) | 402.9 (105.0–856.9) | 638.5 (7.5–1062.4) | 467.4 (40.7–1860.0) | 0.416 |
| Level of Micronutrients Intake | SIBO Subtypes | References Range | p-Value * | ||
|---|---|---|---|---|---|
| H+ (n = 12) | M+ (n = 21) | H+/M+ (n = 34) | |||
| Vitamin A (μg/day) Insufficient Sufficient | 2 (16.7%) 10 (83.3%) | 5 (23.8%) 16 (76.2%) | 16 (17.6%) 28 (82.4%) | EAR (500–630 μg) | 0.827 |
| Vitamin D (μg/day) Insufficient Sufficient | 11 (91.7%) 1 (8.3%) | 18 (85.7%) 3 (14.3%) | 33 (97.1%) 1 (2.9%) | AI (15 μg) | 0.301 |
| Vitamin E (μg/day) Insufficient Sufficient | 6 (50.0%) 6 (50.0%) | 8 (38.0%) 13 (62.0%) | 9 (26.5%) 25 (73.5%) | AI (8–10 μg) | 0.311 |
| Vitamin B12 (μg/day) Insufficient Sufficient | 7 (58.3%) a 5 (41.7%) a | 3 (19.0%) b 17 (81.0%) b | 8 (23.5%) b 26 (76.5%) b | EAR (2.0 μg) | 0.039 * |
| Folate (μg/day) Insufficient Sufficient | 9 (75.0%) 3 (25.0%) | 11 (52.4%) 10 (47.6%) | 24 (70.6%) 10 (29.4%) | EAR (320 μg) | 0.296 |
| Iron (mg/day) Insufficient Sufficient | 6 (50.0%) 6 (50.0%) | 7 (33.3%) 14 (66.7%) | 8 (23.5%) 26 (76.5%) | EAR (6–8 mg) | 0.235 |
| Calcium (mg/day) Insufficient Sufficient | 10 (83.3.%) 2 (16.7%) | 14 (66.7%) 7 (33.3%) | 25 (73.5%) 9 (26.5%) | EAR (800–1000 mg) | 0.586 |
| SIBO Subtypes | Relationship (Gas and Serum Level) | p Value and r |
|---|---|---|
| H+/M+ | H2 and vitamin D | p < 0.001, r = −0.6585 |
| H+/M+ | H2 and ferritin | p = 0.001, r = −0.5648 |
| M+ | CH4 and folic acid | p = 0.002, r = 0.6367 |
| SIBO Subtypes | Relationship (Gas and Dietary Intake) | p Value and r Value |
|---|---|---|
| H+/M+ | CH4 and fiber | (p =0.001, r = −0.6462) |
| M+ | CH4 and fiber | (p =0.001, r = −0.6969) |
| H+ | H2 and lactose | (p =0.027, r = −0.6338) |
| M+ | CH4 and lactose | (p =0.002, r = −0.6444 |
| Time before the LHMB | Conditions to Meet before Performing Test |
|---|---|
| 4 weeks | Discontinuation of antibiotics |
| 2 weeks | Avoiding probiotics |
| 1 week | Eliminating prokinetics |
| 3 days | Limiting fiber intake |
| 24–48 h | Implementing carbohydrate elimination diet |
| 12 h | Begin fasting |
| Day of LHMB | Continuing fast and drinking limited quantities of water (500 mL) No physical activity or smoking |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wielgosz-Grochowska, J.P.; Domanski, N.; Drywień, M.E. Identification of SIBO Subtypes along with Nutritional Status and Diet as Key Elements of SIBO Therapy. Int. J. Mol. Sci. 2024, 25, 7341. https://doi.org/10.3390/ijms25137341
Wielgosz-Grochowska JP, Domanski N, Drywień ME. Identification of SIBO Subtypes along with Nutritional Status and Diet as Key Elements of SIBO Therapy. International Journal of Molecular Sciences. 2024; 25(13):7341. https://doi.org/10.3390/ijms25137341
Chicago/Turabian StyleWielgosz-Grochowska, Justyna Paulina, Nicole Domanski, and Małgorzata Ewa Drywień. 2024. "Identification of SIBO Subtypes along with Nutritional Status and Diet as Key Elements of SIBO Therapy" International Journal of Molecular Sciences 25, no. 13: 7341. https://doi.org/10.3390/ijms25137341







