Current Knowledge about Nonclassical Monocytes in Patients with Multiple Sclerosis, a Systematic Review
Abstract
:1. Introduction
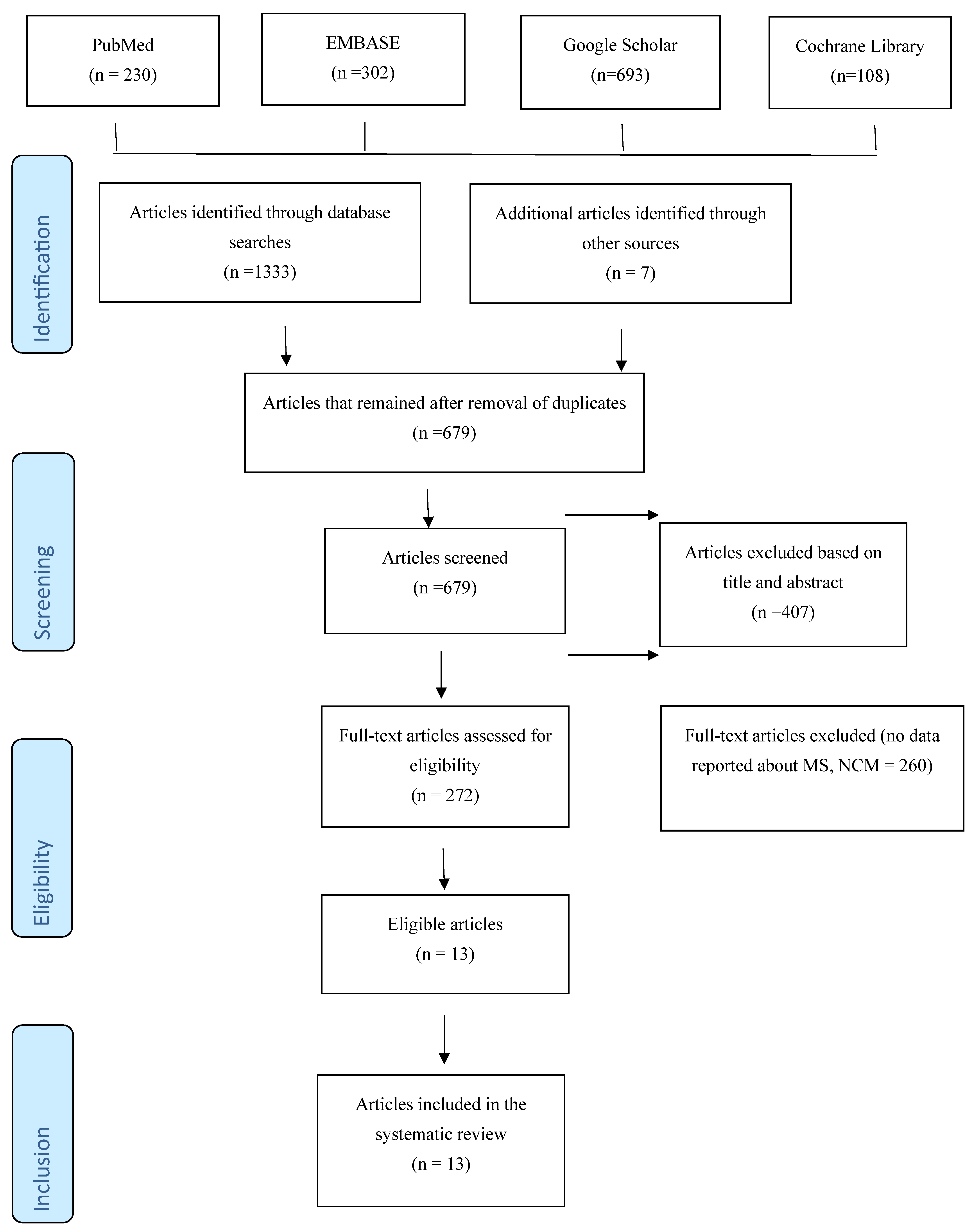
2. Methods
2.1. Inclusion and Exclusion Criteria
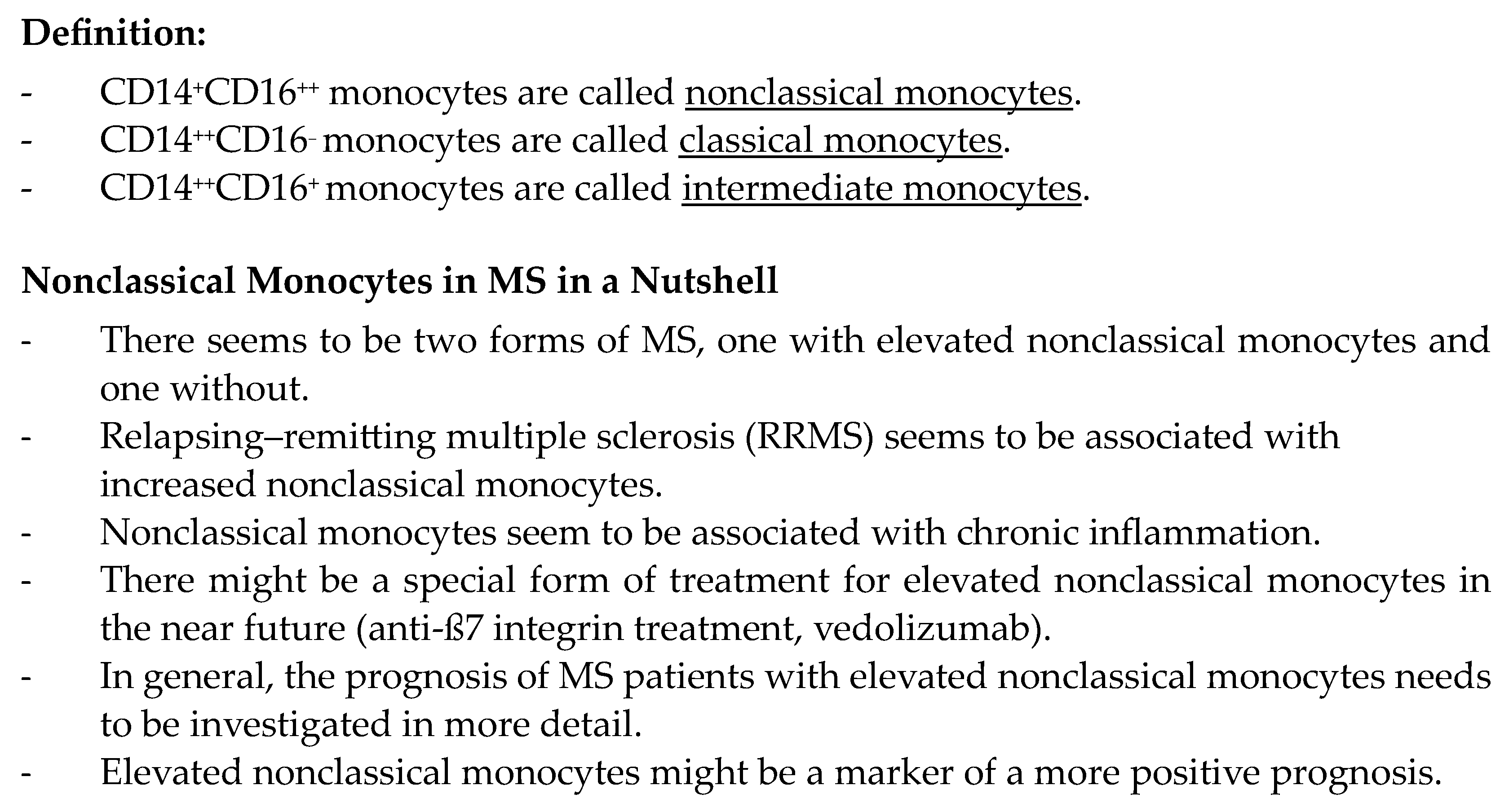
2.2. Limitations of the Study
3. Results
4. Discussion
4.1. Current Knowledge
4.2. The Role of Monocytes in Clinical Disease
4.3. Practical Use
5. Conclusions
Funding
Conflicts of Interest
References
- Ajami, B.; Steinman, L. Nonclassical monocytes: Are they the next therapeutic targets in multiple sclerosis? Immunol. Cell Biol. 2018, 96, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Narasimhan, P.B.; Marcovecchio, P.; Hamers, A.A.; Hedrick, C.C. Nonclassical Monocytes in Health and Disease. Annu. Rev. Immunol. 2019, 37, 439–456. [Google Scholar] [CrossRef] [PubMed]
- Tahir, S.; Steffens, S. Nonclassical monocytes in cardiovascular physiology and disease. Am. J. Physiol. Physiol. 2021, 320, C761–C770. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.; Tacke, R.; Hedrick, C.C.; Hanna, R.N. Nonclassical Patrolling Monocyte Function in the Vasculature. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 1306–1316. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.-M.; Hadadi, E.; Dang, T.-M.; Yeap, W.-H.; Tan, C.T.-Y.; Ng, T.-P.; Larbi, A.; Wong, S.-C. The pro-inflammatory phenotype of the human non-classical monocyte subset is attributed to senescence. Cell Death Dis. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kapellos, T.S.; Bonaguro, L.; Gemünd, I.; Reusch, N.; Saglam, A.; Hinkley, E.R.; Schultze, J.L. Human Monocyte Subsets and Phenotypes in Major Chronic Inflammatory Diseases. Front. Immunol. 2019, 10, 2035. [Google Scholar] [CrossRef] [PubMed]
- Makinde, H.M.; Cuda, C.M.; Just, T.B.; Perlman, H.R.; Schwulst, S.J. Nonclassical Monocytes Mediate Secondary Injury, Neurocognitive Outcome, and Neutrophil Infiltration after Traumatic Brain Injury. J. Immunol. 2017, 199, 3583–3591. [Google Scholar] [CrossRef] [PubMed]
- Padgett, L.E.; Marcovecchio, P.M.; Olingy, C.E.; Araujo, D.J.; Steel, K.; Dinh, H.Q.; Alimadadi, A.; Zhu, Y.P.; Meyer, M.A.; Kiosses, W.B.; et al. Nonclassical monocytes potentiate anti-tumoral CD8+ T cell responses in the lungs. Front. Immunol. 2023, 14, 1101497. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, M.; Christensen, T.; Stilund, M.; Møller, H.J.; Petersen, E.L.; Petersen, T. Activated monocytes and markers of inflammation in newly diagnosed multiple sclerosis. Immunol. Cell Biol. 2020, 98, 549–562. [Google Scholar] [CrossRef]
- Haschka, D.; Tymoszuk, P.; Bsteh, G.; Petzer, V.; Berek, K.; Theurl, I.; Berger, T.; Weiss, G. Expansion of Neutrophils and Classical and Nonclassical Monocytes as a Hallmark in Relapsing-Remitting Multiple Sclerosis. Front. Immunol. 2020, 11, 594. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, C.; Franchi, T.; Mathew, G.; Kerwan, A.; Nicola, M.; Griffin, M.; Agha, M.; Agha, R. PRISMA 2020 statement: What’s new and the importance of reporting guidelines. Int. J. Surg. 2021, 88, 105918. [Google Scholar] [CrossRef] [PubMed]
- Sanfilippo, F.; Tigano, S.; Palumbo, G.J.; Astuto, M.; Murabito, P. Importance of inclusion criteria in systematic reviews. Br. J. Anaesth. 2020, 125, e398–e399. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, L.; Yu, C.; Yang, X.-F.; Wang, H. Monocyte and macrophage differentiation: Circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomark. Res. 2014, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.J.; Finck, T.L.K.; Pellkofer, H.L.; Reichardt, H.M.; Lühder, F. Glucocorticoid Therapy of Multiple Sclerosis Patients Induces Anti-inflammatory Polarization and Increased Chemotaxis of Monocytes. Front. Immunol. 2019, 10, 1200. [Google Scholar] [CrossRef] [PubMed]
- Khater, S.S.; Mohamed, H.G.; Saleh, R.M.M.A.; Taha, S.I.A.; Kamal, N.E.E.M. Monocyte Subsets in Relapsing Remitting Multiple Sclerosis Egyptian Patients. Mult. Scler. Relat. Disord. 2023, 80, 105260. [Google Scholar] [CrossRef]
- Gjelstrup, M.C.; Stilund, M.; Petersen, T.; Møller, H.J.; Petersen, E.L.; Christensen, T. Subsets of activated monocytes and markers of inflammation in incipient and progressed multiple sclerosis. Immunol. Cell Biol. 2017, 96, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Kong, B.S.; Kim, Y.; Kim, G.Y.; Hyun, J.-W.; Kim, S.-H.; Jeong, A.; Kim, H.J. Increased frequency of IL-6-producing non-classical monocytes in neuromyelitis optica spectrum disorder. J. Neuroinflammation 2017, 14, 191. [Google Scholar] [CrossRef] [PubMed]
- Waschbisch, A.; Schröder, S.; Schraudner, D.; Sammet, L.; Weksler, B.; Melms, A.; Pfeifenbring, S.; Stadelmann, C.; Schwab, S.; Linker, R.A. Pivotal Role for CD16+ Monocytes in Immune Surveillance of the Central Nervous System. J. Immunol. 2016, 196, 1558–1567. [Google Scholar] [CrossRef] [PubMed]
- Maleki, A.F.; Cisbani, G.; Laflamme, N.; Prefontaine, P.; Plante, M.-M.; Baillargeon, J.; Rangachari, M.; Gosselin, J.; Rivest, S. Selective Immunomodulatory and Neuroprotective Effects of a NOD2 Receptor Agonist on Mouse Models of Multiple Sclerosis. Neurotherapeutics 2021, 18, 889–904. [Google Scholar] [CrossRef]
- Kapate, N.; Dunne, M.; Kumbhojkar, N.; Prakash, S.; Wang, L.L.-W.; Graveline, A.; Park, K.S.; Suja, V.C.; Goyal, J.; Clegg, J.R.; et al. A backpack-based myeloid cell therapy for multiple sclerosis. Proc. Natl. Acad. Sci. USA 2023, 120, e2221535120. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Arndt, L.; Kerkering, J.; Kuehl, T.; Gil Infante, A.; Paul, F.; Rosiewicz, K.S.; Siffrin, V.; Alisch, M. Inflammatory Cytokines Associated with Multiple Sclerosis Directly Induce Alterations of Neuronal Cytoarchitecture in Human Neurons. J. Neuroimmune Pharmacol. 2023, 18, 145–159. [Google Scholar] [CrossRef] [PubMed]
- Adriani, M.; Nytrova, P.; Mbogning, C.; Hässler, S.; Medek, K.; Jensen, P.E.H.; Creeke, P.; Warnke, C.; Ingenhoven, K.; Hemmer, B.; et al. Monocyte NOTCH2 expression predicts IFN-β immunogenicity in multiple sclerosis patients. J. Clin. Investig. 2018, 3, e99274. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, A.; Rosado, P.; Rosado, L.; Fonseca, A.M.; Coucelo, M.; Paiva, A. Alterations in peripheral blood monocyte and dendritic cell subset homeostasis in relapsing-remitting multiple sclerosis patients. J. Neuroimmunol. 2020, 350, 577433. [Google Scholar] [CrossRef] [PubMed]
- Chung, R.; Chawla, A.; Peh, W. Clinics in diagnostic imaging (178). Singap. Med. J. 2017, 58, 289–293. [Google Scholar] [CrossRef]
- Haase, S.; Linker, R.A. Inflammation in multiple sclerosis. Ther. Adv. Neurol. Disord. 2021, 14, 17562864211007687. [Google Scholar] [CrossRef] [PubMed]
- Lyadova, I.; Gerasimova, T.; Nenasheva, T. Macrophages Derived from Human Induced Pluripotent Stem Cells: The Diversity of Protocols, Future Prospects, and Outstanding Questions. Front. Cell Dev. Biol. 2021, 9, 640703. [Google Scholar] [CrossRef] [PubMed]
- Michaličková, D.; Öztürk, H.K.; Slanař, O. Targeting leukocytes in multiple sclerosis: Therapeutic perspectives. Transl. Neuroimmunol. Vol. 8 2023, 1, 129–143. [Google Scholar] [CrossRef]
- Baughman, R.P.; Valerie, D. Sarcoidosis: A Clinician’s Guide; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018; ISBN 9780323544306. [Google Scholar]
- Spiteri, A.G.; Wishart, C.L.; Pamphlett, R.; Locatelli, G.; King, N.J.C. Microglia and monocytes in inflammatory CNS disease: Integrating phenotype and function. Acta Neuropathol. 2021, 143, 179–224. [Google Scholar] [CrossRef]
- Strizova, Z.; Benesova, I.; Bartolini, R.; Novysedlak, R.; Cecrdlova, E.; Foley, L.K.; Striz, I. M1/M2 macrophages and their overlaps—Myth or reality? Clin. Sci. 2023, 137, 1067–1093. [Google Scholar] [CrossRef]
- Liu, Z.; Wei, W.; Zhang, J.; Yang, X.; Feng, Z.; Zhang, B.; Hou, X. Single-cell transcriptional profiling reveals aberrant gene expression patterns and cell states in autoimmune diseases. Mol. Immunol. 2024, 165, 68–81. [Google Scholar] [CrossRef]
- Rahmberg, A.R.; Wu, C.; Shin, T.; Hong, S.G.; Pei, L.; Hickman, H.D.; Dunbar, C.E.; Brenchley, J.M. Ongoing production of tissue-resident macrophages from hematopoietic stem cells in healthy adult macaques. Eur. J. Immunol. 2022, 2, 521067. [Google Scholar] [CrossRef]
- Rossi, B.; Santos-Lima, B.; Terrabuio, E.; Zenaro, E.; Constantin, G. Common Peripheral Immunity Mechanisms in Multiple Sclerosis and Alzheimer’s Disease. Front. Immunol. 2021, 12. [Google Scholar] [CrossRef]
- Lehman, N.; Kowalska, W.; Zarobkiewicz, M.; Mazurek, M.; Mrozowska, K.; Bojarska-Junak, A.; Rola, R. Pro- vs. Anti-Inflammatory Features of Monocyte Subsets in Glioma Patients. Int. J. Mol. Sci. 2023, 24, 1879. [Google Scholar] [CrossRef] [PubMed]
- Sabir, F.; Farooq, R.K.; Ur Rehman, A.; Ahmed, N. Monocyte as an Emerging Tool for Targeted Drug Delivery: A Review. Curr. Pharm. Des. 2019, 24, 5296–5312. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.-C.; Lin, H.-C.; Yang, Y.-H.; Hsu, C.-W.; Chen, N.-C.; Tsai, W.-C.; Cheng, B.-C.; Tsai, N.-W. Neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio are associated with a 2-year relapse in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 58, 103514. [Google Scholar] [CrossRef]
- D’amico, E.; Zanghì, A.; Parrinello, N.L.; Romano, A.; Palumbo, G.A.; Chisari, C.G.; Toscano, S.; Di Raimondo, F.; Zappia, M.; Patti, F. Immunological Subsets Characterization in Newly Diagnosed Relapsing–Remitting Multiple Sclerosis. Front. Immunol. 2022, 13, 819136. [Google Scholar] [CrossRef] [PubMed]
- Frisch, E.S.; Häusler, D.; Weber, M.S. Natalizumab Promotes Activation of Peripheral Monocytes in Patients with Multiple Sclerosis. Neurol. Neuroimmunol. Neuroinflammation 2023, 10. [Google Scholar] [CrossRef]
- Crucian, B.; Dunne, P.; Friedman, H.; Ragsdale, R.; Pross, S.; Widen, R. Alterations in Peripheral Blood Mononuclear Cell Cytokine Production in Response to Phytohemagglutinin in Multiple Sclerosis Patients [Internet]. US National Library of Medicine. 2021. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC170236/ (accessed on 11 February 2024).
- Rasmussen, E.B.; Eriksen, L.L.; Greisen, S.R.; Hansen, A.L.; Carstensen, M.; Sandahl, T.D.; Støy, S.; Kragstrup, T.W. Diminished Non-Classical Monocytes in the Blood Associate with Disease Severity in Alcoholic Hepatitis. Clin. Exp. Gastroenterol. 2021, 14, 259–267. [Google Scholar] [CrossRef]
- Fransson, J.; Bachelin, C.; Deknuydt, F.; Ichou, F.; Guillot-Noël, L.; Ponnaiah, M.; Gloaguen, A.; Maillart, E.; Stankoff, B.; Tenenhaus, A.; et al. Dysregulated functional and metabolic re-sponse in multiple sclerosis patient macrophages correlate with a more inflammatory state, reminiscent of trained immunity. bioRxiv 2021. [Google Scholar] [CrossRef]
- Austermann, J.; Roth, J.; Barczyk-Kahlert, K. The Good and the Bad: Monocytes’ and Macrophages’ Diverse Functions in Inflammation. Cells 2022, 11, 1979. [Google Scholar] [CrossRef]
- Chuluundorj, D.; Harding, S.A.; Abernethy, D.; La Flamme, A.C. Expansion and preferential activation of the CD14+CD16+ monocyte subset during multiple sclerosis. Immunol. Cell Biol. 2014, 92, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.; Marcondes, N.A.; Hax, V.; Moreira, I.F.d.S.; Ueda, C.Y.; Piovesan, R.R.; Xavier, R.; Chakr, R. Flow cytometry evaluation of CD14/CD16 monocyte subpopulations in systemic sclerosis patients: A cross sectional controlled study. Adv. Rheumatol. 2021, 61, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Menasria, R.; Canivet, C.; Piret, J.; Boivin, G. Infiltration Pattern of Blood Monocytes into the Central Nervous System during Experimental Herpes Simplex Virus Encephalitis. PLoS ONE 2015, 10, e0145773. [Google Scholar] [CrossRef]
- Chilunda, V.; Martinez-Aguado, P.; Xia, L.C.; Cheney, L.; Murphy, A.; Veksler, V.; Ruiz, V.; Calderon, T.M.; Berman, J.W. Transcriptional Changes in CD16+ Monocytes May Contribute to the Pathogenesis of COVID-19. Front. Immunol. 2021, 12, 665773. [Google Scholar] [CrossRef] [PubMed]
- Beyers, C. Modulation of monocyte responses by Progressive Multiple Sclerosis Therapy. Eur. J. Immunol. 2023, 1, 1–133. [Google Scholar] [CrossRef]
- Robichon, K.; Patel, V.; Connor, B.; La Flamme, A.C. Clozapine reduces infiltration into the CNS by targeting migration in experimental autoimmune encephalomyelitis. J. Neuroinflammation 2020, 17, 1–15. [Google Scholar] [CrossRef]
- Radandish, M.; Khalilian, P.; Esmaeil, N. The Role of Distinct Subsets of Macrophages in the Pathogenesis of MS and the Impact of Different Therapeutic Agents on These Populations. Front. Immunol. 2021, 12, 667705. [Google Scholar] [CrossRef]
- Mužinić Režić, N.R.; Markotić, A.; Pavelin, S.; Polančec, D.; Buljubašić Šoda, M.; Bralić, A.; Šoda, J.; Mastelić, A.; Mikac, U.; Jerković, A.; et al. Expression of CD40 and CD192 in Classical Monocytes in Multiple Sclerosis Patients Assessed with Transcranial Magnetic Stimulation. Biomedicines 2023, 11, 2870. [Google Scholar] [CrossRef]
- Bai, R.; Li, Z.; Lv, S.; Wang, R.; Hua, W.; Wu, H.; Dai, L. Persistent Inflammation and Non-AIDS Comorbidities During ART: Coming of the Age of Monocytes. Front. Immunol. 2022, 13, 820480. [Google Scholar] [CrossRef]
- Lin, L.Y.; Juillard, P.; Hawke, S.; Marsh-Wakefield, F.; Grau, G.E. Oral Cladribine Impairs Intermediate, but Not Conventional, Monocyte Transmigration in Multiple Sclerosis Patients across a Model Blood-Brain Barrier. Int. J. Mol. Sci. 2023, 24, 6487. [Google Scholar] [CrossRef] [PubMed]
- Garré, J.M.; Yang, G. Contributions of monocytes to nervous system disorders. J. Mol. Med. 2018, 96, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Prineas, J.W.; Parratt, J.D.E. Multiple Sclerosis: Microglia, Monocytes, and Macrophage-Mediated Demyelination. J. Neuropathol. Exp. Neurol. 2021, 80, 975–996. [Google Scholar] [CrossRef] [PubMed]
- Amoruso, A.; Blonda, M.; Gironi, M.; Grasso, R.; Di Francescantonio, V.; Scaroni, F.; Furlan, R.; Verderio, C.; Avolio, C. Immune and central nervous system-related miRNAs expression profiling in monocytes of multiple sclerosis patients. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef]
- Monaghan, K.L.; Zheng, W.; Hu, G.; Wan, E.C.K. Monocytes and Monocyte-Derived Antigen-Presenting Cells Have Distinct Gene Signatures in Experimental Model of Multiple Sclerosis. Front. Immunol. 2019, 10, 2779. [Google Scholar] [CrossRef]
| Study | Research Design | Research Subjects | MS Cases | Healthy Controls | Monocyte Definition | MS Sclerosis Duration | EDSS Criteria Reported by Authors | EDSS Score | Mean Age of MS Patients | Mean Age of Healthy Controls | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Carstensen et al. [9] | Cohort study | Humans | CIS = 22 RRMS = 33 PMS = 6 RIS = 6 SC = 22 | None | CD14 and CD16 | 2 years | McDonald criteria | CIS = 2 RRMS = 2.5 PMS = 3.0 RIS = N/A SC = N/A | CIS = 38 RRMS = 37 PMS = 52 RIS = 39.5 SC = 37 | None | Incipient MS patients had reduced levels of nonclassical monocytes compared to SC and RIS patients. Notably, human endogenous retrovirus (HERV) expression was exhibited in nonclassical monocytes notwithstanding MS due to inflammatory activation. |
| Haschka et al. [10] | Cohort study | Humans | N = 65 | N = 15 | CD15+ neutrophils Classical monocytes Nonclassical monocytes | Active PMS—over 6 months PMSI—no progression over the last 6 months RRMSa—relapse within the last 3 months RRMSi—no relapse within the last 3 months | McDonald criteria | Baseline = ≤5.5 After treatment = Not indicated | MS = 44 years | HD = 44 years | Patients with inactive relapsing–remitting multiple sclerosis (RRMSi) had expanded volumes of classical and nonclassical monocytes, distinguishing between RRMSi and other types of MS. |
| Yang et al. [14] | Clinical trial | Humans | Not indicated | Not indicated | CD14 CD16 | Not indicated | Not indicated | Not indicated | Not indicated | Not indicated | Unlike those in the control group, the monocytes in MS patients exhibited an elevated inflammatory profile with a high expression of CD40, CD86, CD64, and CCR2. Trichuris suis (TsSP) modulated the function and phenotype of macrophages, lowering the production and expression of inflammatory cytokines, thereby promoting an anti-inflammatory M2 signature. |
| Fischer et al. [15] | Clinical trial | Humans | N = 30 | N = 30 | CD14 CD16 | Not indicated | McDonald criteria | RRMS = 2.54 SPMS = 6.12 PPMS = 5.5 Healthy controls = N/A | 49.9 | 29.4 | Classical CD14++CD16− monocytes were found to be more abundant in MS patients than in healthy individuals, while nonclassical CD14+CD16++ monocytes were less frequent in MS patients. In addition, glucocorticoid treatment polarized monocytes into an anti-inflammatory phenotype, enabling their migration into the central nervous system and causing them to suppress pathogenic immune responses. |
| Khater et al. [16] | Cross-sectional study | Humans | N =22 patients in relapse N = 22 patients in remission | N = 44 | CD14 CD16 | 3–6 years | McDonald criteria | Baseline = 2.74 ± 1.34 Results Classical = −0.202 Intermediate = 0.188 Nonclassical = 0.231 | 50 years | 50 years | Patients with relapse and remission experienced an increase in all three monocyte subsets (classical, intermediate, and nonclassical). The increase in the monocyte subsets suggests their role in disease pathology since they are attributable to disease activity. These findings suggest a possible MS diagnostic tool and therapeutic target for MS. |
| Gjelstrup et al. [17] | Clinical trial | Humans | N = 40 patients | N = 20 healthy controls | CD14 CD16 CD40 CD163 CD192 | 11–33 months | McDonald criteria | Not indicated | Not indicated | Not indicated | Patients with MS had expanded nonclassical monocytes. The results indicate the relevance of monocytes, specifically nonclassical monocytes, in monitoring inflammatory diseases. |
| Kong et al. [18] | Clinical trial | Humans | N = aquaporin 4IgG-positive NMOSD patients N = 20 MS patients | N = 20 healthy controls | CD14 CD16 | Not indicated | McDonald criteria | Baseline = 2.5 (average) Outcome = 2.13 | Not indicated | Not indicated | An altered monocyte inflammatory response was indicated by elevated cell-surface molecules and a reciprocal dysregulation of anti-inflammatory and inflammatory cytokines. Notably, the monocytes from neuromyelitis optica spectrum disorder patients exhibited greater amounts of CD14+CD16++ nonclassical monocytes compared to the MS patients and healthy controls. |
| Waschbisch et al. [19] | Randomized clinical trial | Humans | RRMS patients (n = 40) | HD (n = 40) | CD14+ CD16++ | Less than 2 months | McDonald criteria | HD = N/A RRMS = 1.5 NAT = 2.5 FTY = 2.0 IFN = 2.5 | 50 years | 50 years | CD16+ monocytes were functional but reduced in the blood samples of MS patients. CD16+ monocytes were enriched in cerebrospinal fluid and were dominant among the CSF monocyte population. Conversely, MS patients with relapsing–remitting conditions exhibited an inverse CD16+ to CD16− ratio. |
| Maleki et al. [20] | Experimental study | EAE mice | N = 20 | N = 10 | CD14 CD16 CD14++ CD16+ | 7 weeks | Not indicated | Not indicated | 7 weeks | 7 weeks | Muramyl dipeptide (MDP) treatment delayed EAE onset and decreased leucocyte infiltration in the central nervous system of mice. The results indicate the benefits of MDP in the progressive and early stages of EAE and can guide the development of MS medications and therapies. |
| Kapate et al. [21] | Experimental study | EAE mice | N = 3 | N = 3 | MHCII, CD80, CD86, and iNOS | 48 h | Not indicated | Not indicated | 6–11 weeks | 6–11 weeks | The backpack-based intervention regulated the resident cells and infiltrated the myeloid cell compartments in the brain and the spinal cord, decreasing inflammation. |
| Meyer-Arndt et al. [22] | Experimental study | Humans | N = 4 RRMS donors | N = 5 allogeneic donors | CD14+ CD16+ | Not indicated | Not indicated | Not indicated | 30 years | 47 years | Lipoic acid treatment inhibited monocytes from excreting the cytokines responsible for MS. |
| Adriani [23] | Experimental study | Humans | IFN-β–treated patients (n = 15) Treatment-naive patients (n = 10) | Healthy donors (HCs, n = 10) | CD14+ CD16+ | 9–18 months | McDonald criteria | Not indicated | Not indicated | Not indicated | During treatment with IFN-β, NOTCH2 expression on CD14+ monocytes and an increased release of proinflammatory monocytes predicted nADA development in MS patients. |
| Monteiro et al. [24] | Randomized clinical trial | Humans | N = 30 patients in remission N = 8 patients in relapse | Not indicated | CD14 CD16 | 2 years | McDonald criteria | Not indicated | 51 years | NA | Plasmacytoid (pDC) and myeloid (mDC) dendritic cells decreased during remission but returned to normal values upon relapse. During both conditions, nonclassical monocytes decreased in frequency. |
| Paper | Significant Findings |
|---|---|
| Carstensen et al. [9] | Incipient MS patients have reduced levels of nonclassical monocytes compared to patients with SC and RIS. |
| Haschka et al. [10] | Patients with inactive relapsing–remitting MS have expanded numbers of classical and nonclassical monocytes. |
| Fischer et al. [15] | Classical CD14++CD16− monocytes are abundant in MS patients, but they have low levels of nonclassical CD14+CD16++ monocytes. These monocytes have anti-inflammatory effects. |
| Khater et al. [16] | Relapsing–remitting MS patients have an increase in all three monocyte subsets, revealing their role in disease pathology. |
| Gjelstrup et al. [17] | MS patients have abundant levels of nonclassical monocytes, and these have roles in monitoring inflammatory disease. |
| Kong et al. [18] | Elevated cell surface molecules and reciprocal dysregulation of the inflammatory and anti-inflammatory cytokines causes an altered monocyte inflammatory response. |
| Waschbisch et al. [19] | MS patients have reduced levels of CD16+ monocytes in their blood, but these monocytes are abundant in their CSF. |
| Maleki et al. [20] | Muramyl dipeptide (MDP) can delay EAE onset and prevent infiltration of the central nervous system in mice. |
| Monteiro et al. [24] | Monocyte levels are altered during remission and they normalize upon relapse. |
| The 10 Most Important Findings |
|---|
|
|
|
|
|
|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arneth, B. Current Knowledge about Nonclassical Monocytes in Patients with Multiple Sclerosis, a Systematic Review. Int. J. Mol. Sci. 2024, 25, 7372. https://doi.org/10.3390/ijms25137372
Arneth B. Current Knowledge about Nonclassical Monocytes in Patients with Multiple Sclerosis, a Systematic Review. International Journal of Molecular Sciences. 2024; 25(13):7372. https://doi.org/10.3390/ijms25137372
Chicago/Turabian StyleArneth, Borros. 2024. "Current Knowledge about Nonclassical Monocytes in Patients with Multiple Sclerosis, a Systematic Review" International Journal of Molecular Sciences 25, no. 13: 7372. https://doi.org/10.3390/ijms25137372





