Controlled Hypoxia Acutely Prevents Physical Inactivity-Induced Peripheral BDNF Decline
Abstract
1. Introduction
2. Results
2.1. Physiological Parameters
2.2. Effect 30 min Resting Phases under Normoxia on BDNF
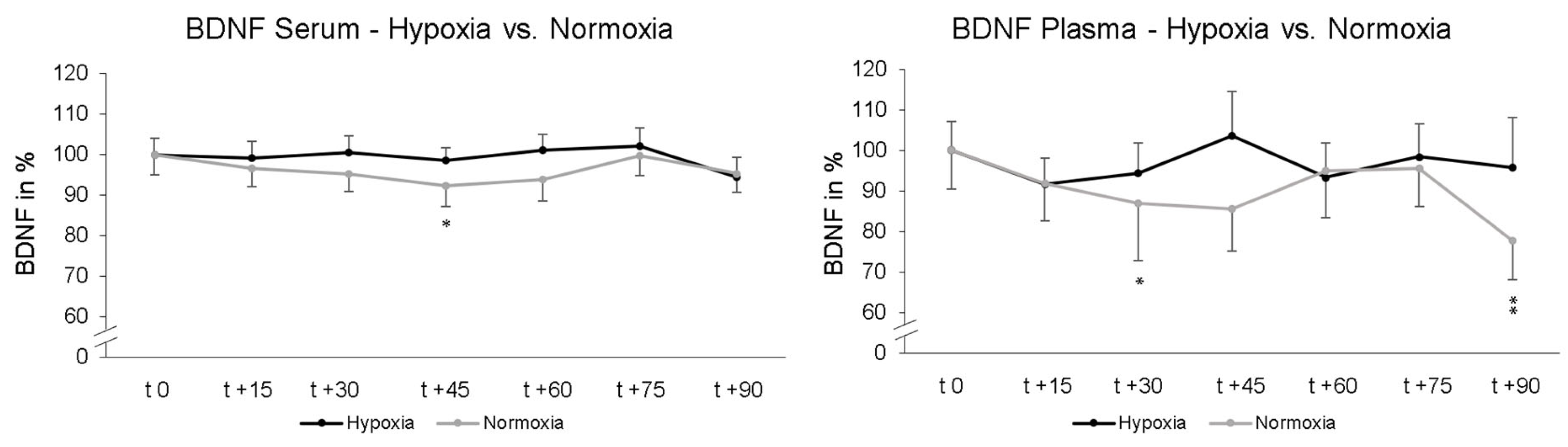
2.3. The Effect of 90 min Normobaric Hypoxia on BDNF
2.4. 24 h Follow-Up
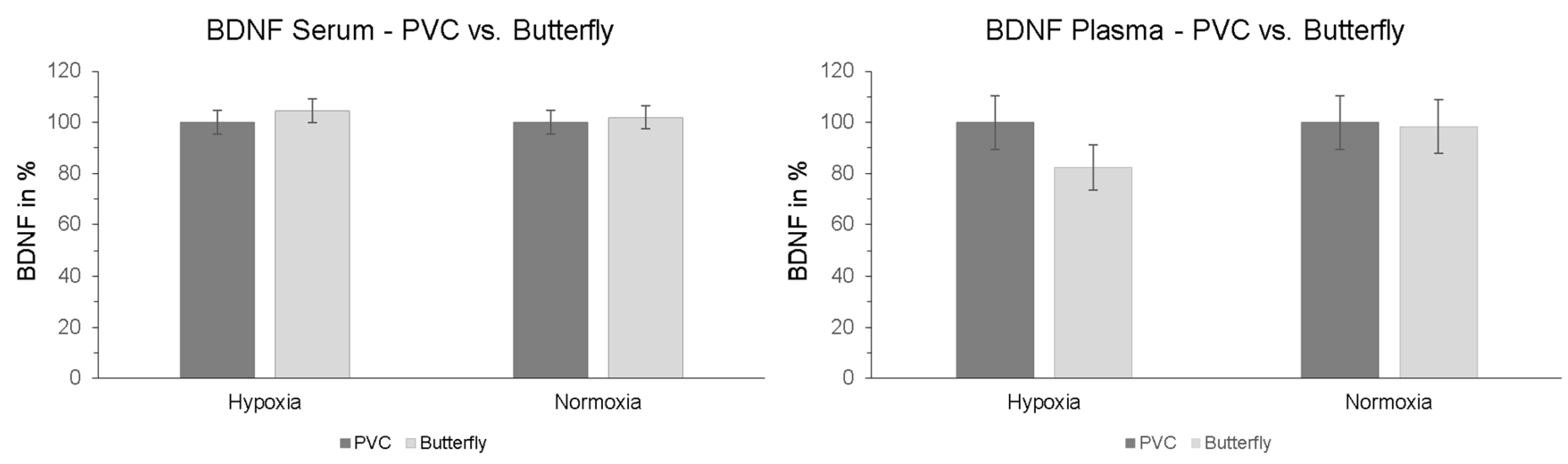
2.5. Effect of Peripheral Venous Catheter vs. Butterfly Needle on BDNF
2.6. d2-R Test
2.7. Digit Span Test
3. Materials and Methods
3.1. Participants
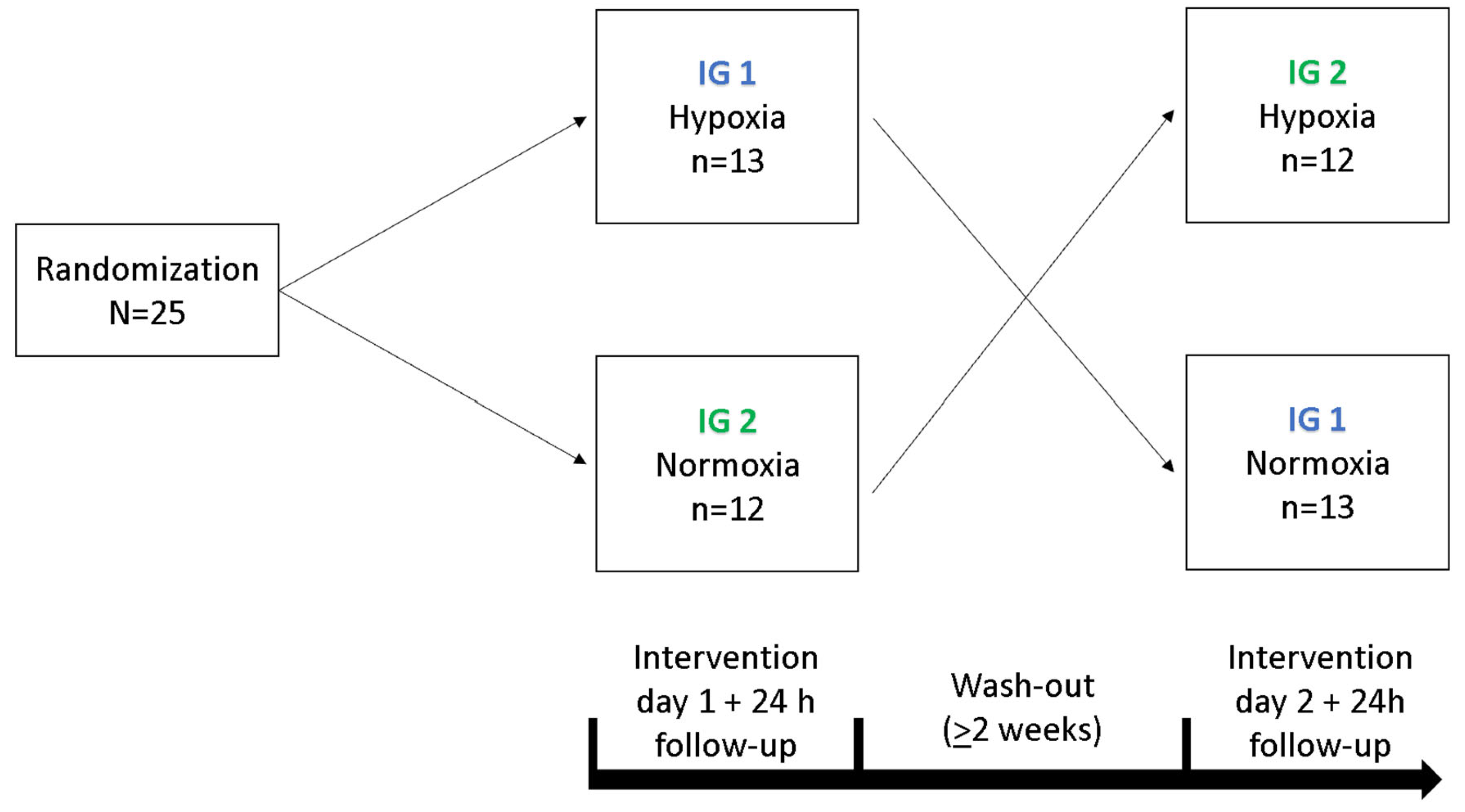
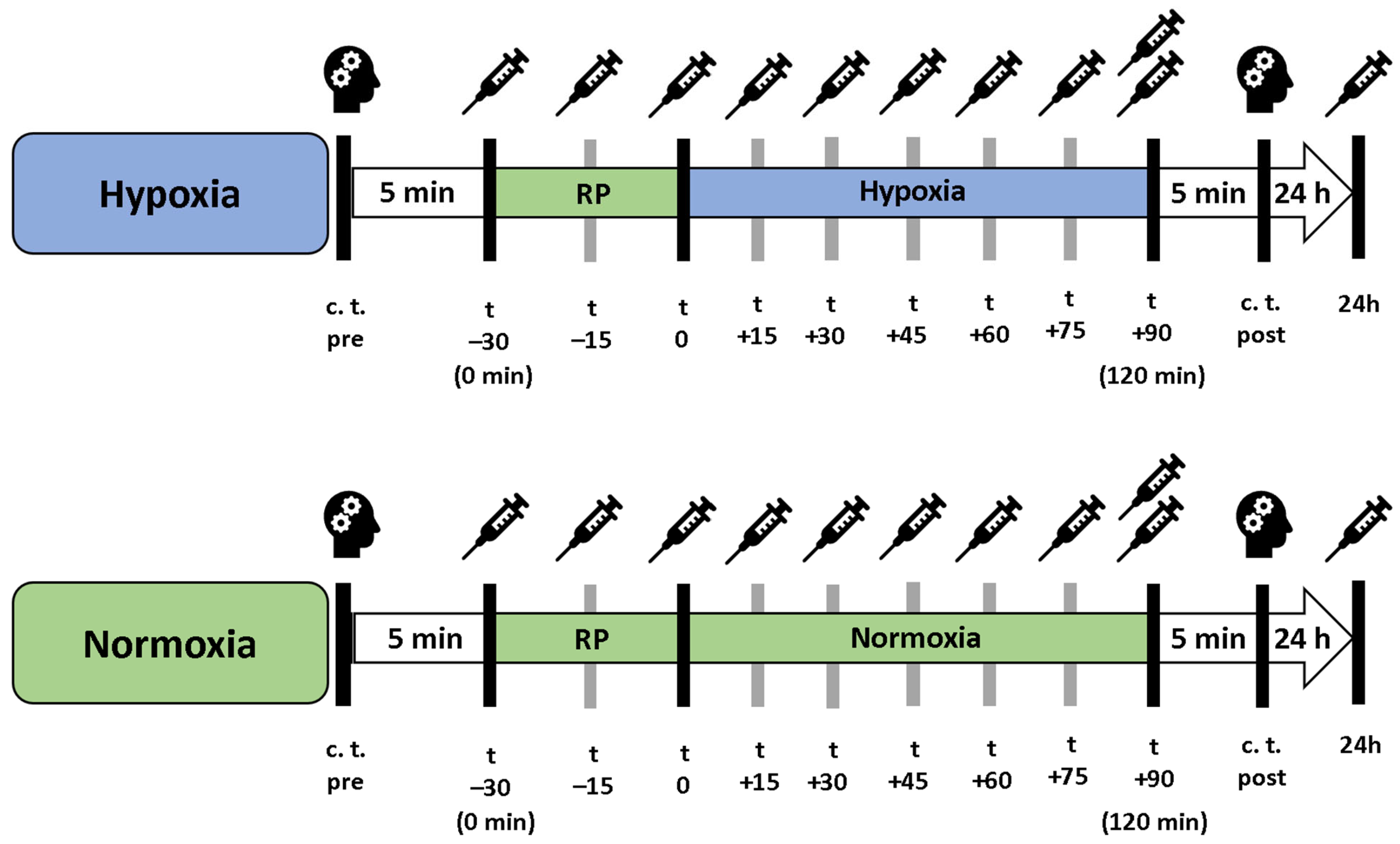
3.2. Experimental Design
3.3. Measurement of BDNF Levels
3.4. d2-R Test
3.5. Digit Span Test
3.6. Statistical Analysis
4. Discussion
- Standardized protocol for blood collection (arrival, sitting position for 30 min, avoiding time deviations).
- Standardized pre-analytic blood protocol (plasma: after blood collection 5 min blood sample in ice water, 15 min centrifugation at 2.000 g, aliquoting and storage at −80 °C; Serum: after blood collection 35 min blood sample storing at room temperature, 15 min centrifugation at 2.000 g, aliquoting and storage at −80 °C).
- Strict patient/participant recommendations and instructions prior to blood collection (e.g., no intensive physical exercise interventions in the last 3 days prior to blood collection, no vigorous physical activities directly before blood collection)
- Collection of potential influencing factors (e.g., smoking habits, potential use of drugs or alcohol, prior stays at altitude, diseases).
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BDNF | Brain-derived neurotrophic factor |
| CNS | Central nervous system |
| COPD | Chronic obstructive pulmonary disease |
| FiO2 | Fraction of inspired oxygen |
| NH | Normobaric hypoxia |
| NOR | Normoxia |
| ηp2 | Partial eta squared |
| O2 | Oxygen |
| paO2 | Arterial oxygen Partial pressure |
| PVC | Peripheral venous catheter |
| rmANOVA | Analyses of variance with repeated measurements |
| SpO2 | Peripheral oxygen saturation |
References
- Edelmann, E.; Leßmann, V.; Brigadski, T. Pre- and postsynaptic twists in BDNF secretion and action in synaptic plasticity. Neuropharmacology 2014, 76, 610–627. [Google Scholar] [CrossRef] [PubMed]
- Ferris, L.T.; Williams, J.S.; Shen, C.L. The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognitive function. Med. Sci. Sports Exerc. 2007, 39, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Laske, C.; Eschweiler, G.W. Brain-derived neurotrophic factor. Nervenarzt 2005, 77, 523–537. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Poo, M.M. Neurotrophin regulation of neural circuit development and function. Nat. Rev. Neurosci. 2013, 14, 7–23. [Google Scholar] [CrossRef] [PubMed]
- Brigadski, T.; Leßmann, V. The physiology of regulated BDNF release. Cell Tissue Res. 2020, 382, 15–45. [Google Scholar] [CrossRef] [PubMed]
- McGregor, C.E.; English, A.W. The role of BDNF in peripheral nerve regeneration: Activity-dependent treatments and Val66Met. Front. Cell. Neurosci. 2019, 12, 522. [Google Scholar] [CrossRef] [PubMed]
- Kermani, P.; Hempstead, B. Brain-Derived Neurotrophic Factor: A Newly Described Mediator of Angiogenesis. Trends Cardiovasc. Med. 2007, 17, 140–143. [Google Scholar] [CrossRef]
- Erickson, K.I.; Prakash, R.S.; Voss, M.W.; Chaddock, L.; Heo, S.; McLaren, M.; Pence, B.D.; Martin, S.A.; Vieira, V.J.; Woods, J.A.; et al. Brain-Derived Neurotrophic Factor Is Associated with Age-Related Decline in Hippocampal Volume. J. Neurosci. 2010, 30, 5368–5375. [Google Scholar] [CrossRef] [PubMed]
- Murer, M.G.; Yan, Q.; Raisman-Vozari, R. Brain-derived neurotrophic factor in the control human brain, and in Alzheimer’s disease and Parkinson’s disease. Prog. Neurobiol. 2001, 63, 71–124. [Google Scholar] [CrossRef]
- Miranda, M.; Morici, J.F.; Zanoni, M.B.; Bekinschtein, P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front. Cell. Neurosci. 2019, 13, 472800. [Google Scholar]
- Levada, O.A.; Cherednichenko, N.V.; Trailin, A.V.; Troyan, A.S. Plasma Brain-Derived Neurotrophic Factor as a Biomarker for the Main Types of Mild Neurocognitive Disorders and Treatment Efficacy: A Preliminary Study. Dis. Markers 2016, 2016, 4095723. [Google Scholar] [CrossRef]
- Schulte-Herbruggen, O.; Braun, A.; Rochlitzer, S.; Jockers-Scherubl, M.; Hellweg, R. Neurotrophic Factors—A Tool for Therapeutic Strategies in Neurological, Neuropsychiatric and Neuroimmunological Diseases? Curr. Med. Chem. 2007, 14, 2318–2329. [Google Scholar] [CrossRef]
- Mohammadi, A.; Amooeian, V.G.; Rashidi, E. Dysfunction in Brain-Derived Neurotrophic Factor Signaling Pathway and Susceptibility to Schizophrenia, Parkinson’s and Alzheimer’s Diseases. Curr. Gene Ther. 2018, 18, 45–63. [Google Scholar] [CrossRef] [PubMed]
- Komulainen, P.; Pedersen, M.; Hänninen, T.; Bruunsgaard, H.; Lakka, T.A.; Kivipelto, M.; Hassinen, M.; Rauramaa, T.H.; Pedersen, B.K.; Rauramaa, R. BDNF is a novel marker of cognitive function in ageing women: The DR’s EXTRA Study. Neurobiol. Learn. Mem. 2008, 90, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Ng, D.Q.; Cheng, I.; Wang, C.; Tan, C.J.; Toh, Y.L.; Koh, Y.Q.; Ke, Y.; Foo, K.M.; Chan, R.J.; Ho, H.K.; et al. Brain-derived neurotrophic factor as a biomarker in cancer-related cognitive impairment among adolescent and young adult cancer patients. Sci. Rep. 2023, 13, 16298. [Google Scholar]
- Giese, M.; Unternaehrer, E.; Brand, S.; Calabrese, P.; Holsboer-Trachsler, E.; Eckert, A. The Interplay of Stress and Sleep Impacts BDNF Level. PLoS ONE 2013, 8, e76050. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.L.; Chen, F.C.; Pan, C.Y.; Wang, C.H.; Huang, T.H.; Chen, T.C. Impact of acute aerobic exercise and cardiorespiratory fitness on visuospatial attention performance and serum BDNF levels. Psychoneuroendocrinology 2014, 41, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Chui, D.H.; Marcellino, M.; Marotta, F.; Sweed, H.; Solimene, U.; Vignali, A.I.; Xiao, W.; Ayala, A.; Cagnuolo, U.; Zerbinati, Z. A double-blind, Rct testing beneficial modulation of bdnf in middle-aged, Life style-stressed subjects: A clue to brain protection? J. Clin. Diagn. Res. 2014, 8, MC01–MC06. [Google Scholar]
- Lee, J.; Duan, W.; Mattson, M.P. Evidence that brain-derived neurotrophic factor is required for basal neurogenesis and mediates, in part, the enhancement of neurogenesis by dietary restriction in the hippocampus of adult mice. J. Neurochem. 2002, 82, 1367–1375. [Google Scholar] [CrossRef]
- Müller, P.; Rehfeld, K.; Schmicker, M.; Hökelmann, A.; Dordevic, M.; Lessmann, V.; Brigadski, T.; Kaufmann, J.; Müller, N.G. Evolution of neuroplasticity in response to physical activity in old age: The case for dancing. Front. Aging Neurosci. 2017, 9, 56. [Google Scholar] [CrossRef]
- Rehfeld, K.; Lüders, A.; Hökelmann, A.; Lessmann, V.; Kaufmann, J.; Brigadski, T.; Müller, P.; Müller, N.G. Dance training is superior to repetitive physical exercise in inducing brain plasticity in the elderly. PLoS ONE 2018, 13, e0196636. [Google Scholar] [CrossRef] [PubMed]
- Helan, M.; Aravamudan, B.; Hartman, W.R.; Thompson, M.A.; Johnson, B.D.; Pabelick, C.M.; Prakash, Y.S. BDNF Secretion by Human Pulmonary Artery Endothelial Cells in Response to Hypoxia. J. Mol. Cell. Cardiol. 2014, 68, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Hartman, W.; Helan, M.; Smelter, D.; Sathish, V.; Thompson, M.; Pabelick, C.M.; Johnson, B.; Prakash, Y.S. Role of hypoxia-induced brain derived neurotrophic factor in human pulmonary artery smooth muscle. PLoS ONE 2015, 10, e0129489. [Google Scholar] [CrossRef] [PubMed]
- Chroboczek, M.; Kujach, S.; Łuszczyk, M.; Grzywacz, T.; Soya, H. Acute Normobaric Hypoxia Lowers Executive Functions among Young Men despite Increase of BDNF Concentration. Int. J. Environ. Res. Public Health 2022, 19, 10802. [Google Scholar] [CrossRef] [PubMed]
- Vermehren-Schmaedick, A.; Jenkins, V.K.; Knopp, S.J.; Balkowiec, A.; Bissonnette, J.M. Acute intermittent hypoxia-induced expression of brain-derived neurotrophic factor is disrupted in the brainstem of methyl-CpG-binding protein 2 null mice. Neuroscience 2012, 206, 1–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Burtscher, J.; Mallet, R.T.; Pialoux, V.; Millet, G.P.; Burtscher, M. Adaptive Responses to Hypoxia and/or Hyperoxia in Humans. Antioxid. Redox Signal. 2022, 37, 887–912. [Google Scholar] [CrossRef] [PubMed]
- Dale, E.A.; Ben Mabrouk, F.; Mitchell, G.S. Unexpected benefits of intermittent hypoxia: Enhanced respiratory and nonrespiratory motor function. Physiology 2014, 29, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, F.J.; Xie, C.J.C. The role of hypoxia-inducible factors in metabolic diseases Frank. Nat. Rev. Endocrinol. 2018, 15, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Serebrovska, T.V.; Portnychenko, A.G.; Drevytska, T.I.; Portnichenko, V.I.; Xi, L.; Egorov, E.; Gavalko, A.V.; Naskalova, S.; Chizhova, V.; Shatylo, V.B. Intermittent hypoxia training in prediabetes patients: Beneficial effects on glucose homeostasis, hypoxia tolerance and gene expression. Exp. Biol. Med. 2017, 242, 1542–1552. [Google Scholar] [CrossRef]
- Burtscher, J.; Pasha, Q.; Chanana, N.; Millet, G.P.; Burtscher, M.; Strasser, B. Immune consequences of exercise in hypoxia: A narrative review. J. Sport Health Sci. 2023, 13, 297–310. [Google Scholar] [CrossRef]
- Enette, L.; Vogel, T.; Fanon, J.L.; Lang, P.O. Effect of Interval and Continuous Aerobic Training on Basal Serum and Plasma Brain-Derived Neurotrophic Factor Values in Seniors: A Systematic Review of Intervention Studies. Rejuvenation Res. 2017, 20, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Bosch-Marce, M.; Okuyama, H.; Wesley, J.B.; Sarkar, K.; Kimura, H.; Liu, Y.V.; Zhang, H.; Strazza, M.; Rey, S.; Savino, L.; et al. Effects of aging and hypoxia-inducible factor-1 activity on angiogenic cell mobilization and recovery of perfusion after limb ischemia. Circ. Res. 2007, 101, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Viscor, G.; Torrella, J.R.; Corral, L.; Ricart, A.; Javierre, C.; Pages, T.; Ventura, J.L. Physiological and biological responses to short-term intermittent hypobaric hypoxia exposure: From sports and mountain medicine to new biomedical applications. Front. Physiol. 2018, 9, 814. [Google Scholar] [CrossRef] [PubMed]
- Correia, S.C.; Moreira, P.I. Hypoxia-inducible factor 1: A new hope to counteract neurodegeneration? J. Neurochem. 2010, 112, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Shi, X.; Schenck, H.; Hall, J.R.; Ross, S.E.; Kline, G.P.; Chen, S.; Mallet, R.T.; Chen, P. Intermittent Hypoxia Training for Treating Mild Cognitive Impairment: A Pilot Study. Am. J. Alzheimer’s Dis. Other Dement. 2020, 35, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, J.; Mallet, R.T.; Burtscher, M.; Millet, G.P. Hypoxia and brain aging: Neurodegeneration or neuroprotection? Ageing Res. Rev. 2021, 68, 101343. [Google Scholar]
- Becke, A.; Müller, P.; Dordevic, M.; Lessmann, V.; Brigadski, T.; Müller, N.G. Daily intermittent normobaric hypoxia over 2 weeks reduces BDNF plasma levels in young adults—A randomized controlled feasibility study. Front. Physiol. 2018, 9, 1337. [Google Scholar] [CrossRef] [PubMed]
- Hubold, C.; Lang, U.E.; Gehring, H.; Schultes, B.; Schweiger, U.; Peters, A.; Hellweg, R.; Oltmanns, K.M. Increased serum brain-derived neurotrophic factor protein upon hypoxia in healthy young men. J. Neural Transm. 2009, 116, 1221–1225. [Google Scholar] [CrossRef] [PubMed]
- Schega, L.; Peter, B.; Brigadski, T.; Leßmann, V.; Isermann, B.; Hamacher, D.; Törpel, A. Effect of intermittent normobaric hypoxia on aerobic capacity and cognitive function in older people. J. Sci. Med. Sport 2016, 19, 941–945. [Google Scholar] [CrossRef]
- Tarassova, O.; Ekblom, M.M.; Moberg, M.; Lövdén, M.; Nilsson, J. Peripheral BDNF Response to Physical and Cognitive Exercise and Its Association With Cardiorespiratory Fitness in Healthy Older Adults. Front. Physiol. 2020, 11, 1–15. [Google Scholar] [CrossRef]
- Fujimura, H.; Altar, C.A.; Chen, R.; Nakamura, T.; Nakahashi, T.; Kambayashi, J.I.; Sun, B.; Tandon, N.N. Brain-derived neurotrophic factor is stored in human platelets and released by agonist stimulation. Thromb. Haemost. 2002, 87, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Radka, S.F.; Hoist, P.A.; Fritsche, M.; Altar, C.A. Presence of brain-derived neurotrophic factor in brain and human and rat but not mouse serum detected by a sensitive and specific immunoassay. Brain Res. 1996, 709, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Brickenkamp, R. Aufmerksamkeits-Belastungs-Test Handanweisung d-2 [Attention-Pressure-Test Manual d2]; Hogrefe: Goettingen, Germany, 1962. [Google Scholar]
- Wechsler, D. WAIS-IV: Wechsler Adult Intelligence Scale; Psychological Corporation: San Antonio, TX, USA, 2008. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; KNV Besorgung: Erfurt, Germany, 2017. [Google Scholar]
- Zembron-Lacny, A.; Dziubek, W.; Rynkiewicz, M.; Morawin, B.; Woźniewski, M. Peripheral brain-derived neurotrophic factor is related to cardiovascular risk factors in active and inactive elderly men. Braz. J. Med. Biol. Res. 2016, 49, e5253. [Google Scholar] [CrossRef] [PubMed]
- De Azevedo, K.P.M.; De Oliveira Segundo, V.H.; De Medeiros, G.C.B.S.; De Sousa Mata, Á.N.; García, D.Á.; De Carvalho Leitão, J.C.G.; Knackfuss, M.I.; Piuvezam, G. Effects of exercise on the levels of BDNF and executive function in adolescents: A protocol for systematic review and meta-Analysis. Medicine 2019, 98, e16445. [Google Scholar]
- Dinoff, A.; Herrmann, N.; Swardfager, W.; Lanctôt, K.L. The effect of acute exercise on blood concentrations of brain-derived neurotrophic factor in healthy adults: A meta-analysis. Eur. J. Neurosci. 2017, 46, 1635–1646. [Google Scholar] [CrossRef] [PubMed]
- Nurse, C.A.; Salman, S.; Scott, A.L. Hypoxia-regulated catecholamine secretion in chromaffin cells. Cell Tissue Res. 2018, 372, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.S.; Young, J.B.; Landsberg, L.; Dana, C.A. Sympathoadrenal responses to acute and chronic hypoxia in the rat. J. Clin. Investig. 1983, 71, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Michiels, C. Physiological and pathological responses to hypoxia. Am. J. Pathol. 2004, 164, 1875–1882. [Google Scholar] [CrossRef] [PubMed]
- Bilo, G.; Caravita, S.; Torlasco, C.; Parati, G. Blood pressure at high altitude: Physiology and clinical implications. Kardiol. Pol. 2019, 77, 596–603. [Google Scholar] [CrossRef]
- Knöbl, P. Thrombopenie auf der Intensivstation: Diagnose, Differenzialdiagnose und Therapie. Med. Klin-Intensiv. Und Notfallmedizin 2016, 111, 425–433. [Google Scholar] [CrossRef]
- Tamura, S.; Suzuki, H.; Hirowatari, Y.; Hatase, M.; Nagasawa, A.; Matsuno, K.; Kobayashi, S.; Moriyama, T. Release reaction of brain-derived neurotrophic factor (BDNF) through PAR1 activation and its two distinct pools in human platelets. Thromb. Res. 2011, 128, e55–e61. [Google Scholar] [CrossRef] [PubMed]
- Müller, P.; Duderstadt, Y.; Lessmann, V.; Müller, N.G. Lactate and BDNF: Key Mediators of Exercise Induced Neuroplasticity? J. Clin. Med. 2020, 9, 1136. [Google Scholar] [CrossRef] [PubMed]
- Schiffer, T.; Schulte, S.; Sperlich, B.; Achtzehn, S.; Fricke, H.; Strüder, H.K. Lactate infusion at rest increases BDNF blood concentration in humans. Neurosci. Lett. 2011, 488, 234–237. [Google Scholar] [CrossRef] [PubMed]
- Kiers, H.D.; Pickkers, P.; Kox, M. Hypoxemia in the presence or absence of systemic inflammation does not increase blood lactate levels in healthy volunteers. J. Crit. Care 2022, 71, 154116. [Google Scholar] [CrossRef] [PubMed]
- Treml, B.; Kleinsasser, A.; Stadlbauer, K.H.; Steiner, I.; Pajk, W.; Pilch, M.; Burtscher, M.; Knotzer, H. Cutaneous microvascular blood flow and reactivity in hypoxia. Front. Physiol. 2018, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Baker-Herman, T.L.; Fuller, D.D.; Bavis, R.W.; Zabka, A.G.; Golder, F.J.; Doperalski, N.J.; Johnson, R.A.; Watters, J.J.; Mitchell, G.S. BDNF is necessary and sufficient for spinal respiratory plasticity following intermittent hypoxia. Nat. Neurosci. 2004, 7, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, M. Auswirkungen akuter Höhenexposition: Welche Höhe ist gesundheitlich verträglich? Wien. Med. Wochenschr. 2010, 160, 362–371. [Google Scholar] [CrossRef]
- Satriotomo, I.; Nichols, N.L.; Dale, E.A.; Emery, A.T.; Dahlberg, J.M.; Mitchell, G.S. Repetitive acute intermittent hypoxia increases growth/neurotrophic factor expression in non-respiratory motor neurons. Neuroscience 2016, 322, 479–488. [Google Scholar] [CrossRef]
- Damgaard, V.; Mariegaard, J.; Lindhardsen, J.M.; Ehrenreich, H.; Miskowiak, K.W. Neuroprotective effects of moderate hypoxia: A systematic review. Brain Sci. 2023, 13, 1648. [Google Scholar] [CrossRef]
- Roeh, A.; Holdenrieder, S.; Schoenfeld, J.; Haeckert, J.; Halle, M.; Falkai, P.; Scherr, J.; Hasan, A. Decreased Serum Brain-Derived Neurotrophic Factor Concentrations 72 Hours Following Marathon Running. Front. Physiol. 2021, 12, 668454. [Google Scholar] [CrossRef]
- Bath, K.G.; Schilit, A.; Lee, F.S. Stress effects on BDNF expression: Effects of age, sex, and form of stress. Neuroscience 2013, 239, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Rothman, S.M.; Mattson, M.P. Signaling and the Quest for Optimal Brain Health. J. Neurosci. 2014, 239, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.A. Hippocampal vulnerability to stress and aging: Possible role of neurotrophic factors. Behav. Brain Res. 1996, 78, 25–36. [Google Scholar] [CrossRef] [PubMed]



| Hypoxia | Normoxia | |||||
|---|---|---|---|---|---|---|
| pre | post | p | pre | post | p | |
| d2-R-test–AP | 208.36 | 218.08 | 0.001 | 203.44 | 221.84 | <0.001 |
| DST-forw. recall | 11.44 | 11.48 | 0.919 | 10.92 | 11.60 | 0.051 |
| DST-backw. recall | 7.96 | 8.24 | 0.514 | 7.88 | 8.28 | 0.266 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duderstadt, Y.; Schreiber, S.; Burtscher, J.; Schega, L.; Müller, N.G.; Brigadski, T.; Braun-Dullaeus, R.C.; Leßmann, V.; Müller, P. Controlled Hypoxia Acutely Prevents Physical Inactivity-Induced Peripheral BDNF Decline. Int. J. Mol. Sci. 2024, 25, 7536. https://doi.org/10.3390/ijms25147536
Duderstadt Y, Schreiber S, Burtscher J, Schega L, Müller NG, Brigadski T, Braun-Dullaeus RC, Leßmann V, Müller P. Controlled Hypoxia Acutely Prevents Physical Inactivity-Induced Peripheral BDNF Decline. International Journal of Molecular Sciences. 2024; 25(14):7536. https://doi.org/10.3390/ijms25147536
Chicago/Turabian StyleDuderstadt, Yves, Stefanie Schreiber, Johannes Burtscher, Lutz Schega, Notger G. Müller, Tanja Brigadski, Rüdiger C. Braun-Dullaeus, Volkmar Leßmann, and Patrick Müller. 2024. "Controlled Hypoxia Acutely Prevents Physical Inactivity-Induced Peripheral BDNF Decline" International Journal of Molecular Sciences 25, no. 14: 7536. https://doi.org/10.3390/ijms25147536
APA StyleDuderstadt, Y., Schreiber, S., Burtscher, J., Schega, L., Müller, N. G., Brigadski, T., Braun-Dullaeus, R. C., Leßmann, V., & Müller, P. (2024). Controlled Hypoxia Acutely Prevents Physical Inactivity-Induced Peripheral BDNF Decline. International Journal of Molecular Sciences, 25(14), 7536. https://doi.org/10.3390/ijms25147536








