Optimization of an Ischemic Retinopathy Mouse Model and the Consequences of Hypoxia in a Time-Dependent Manner
Abstract
:1. Introduction
2. Results
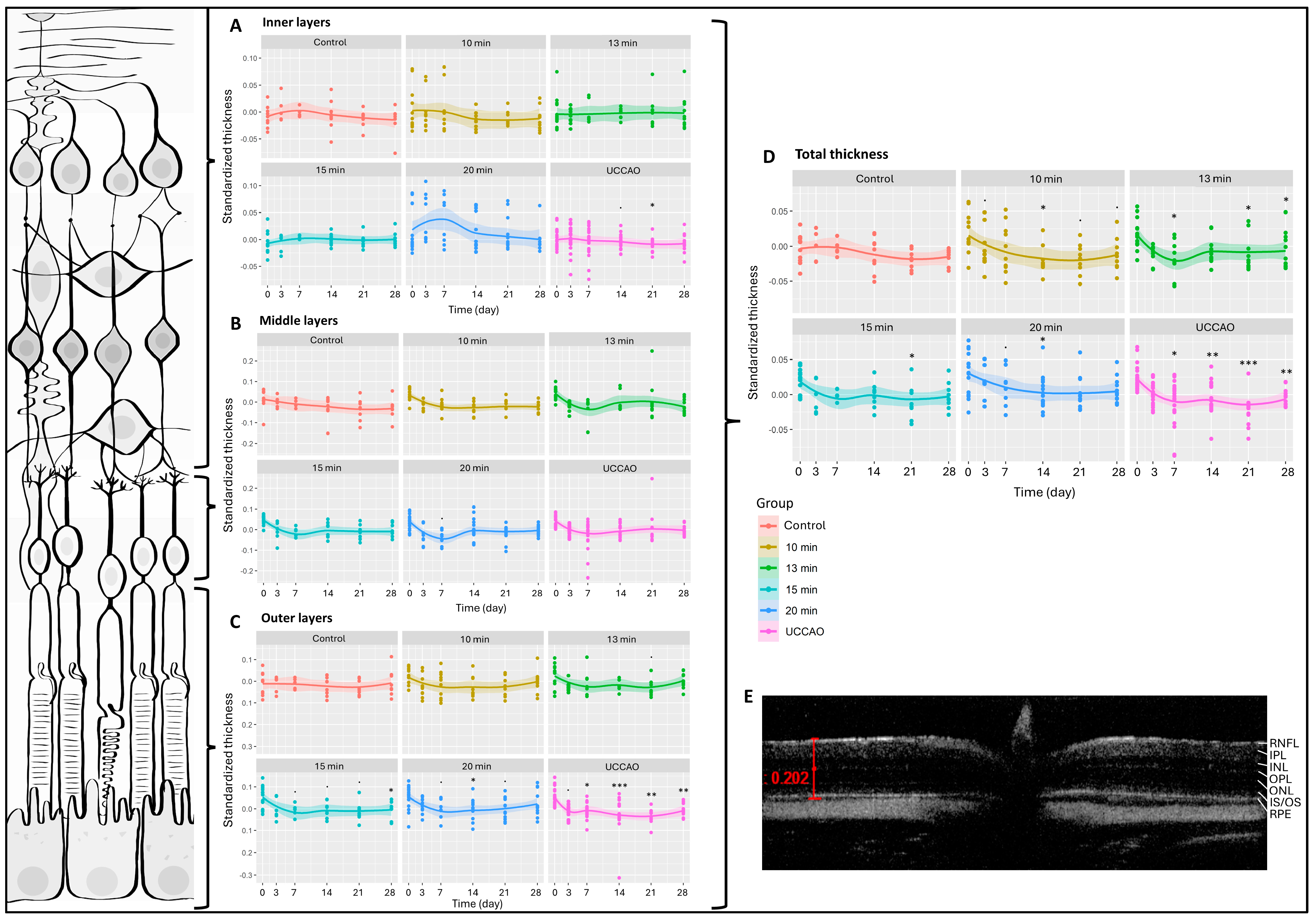
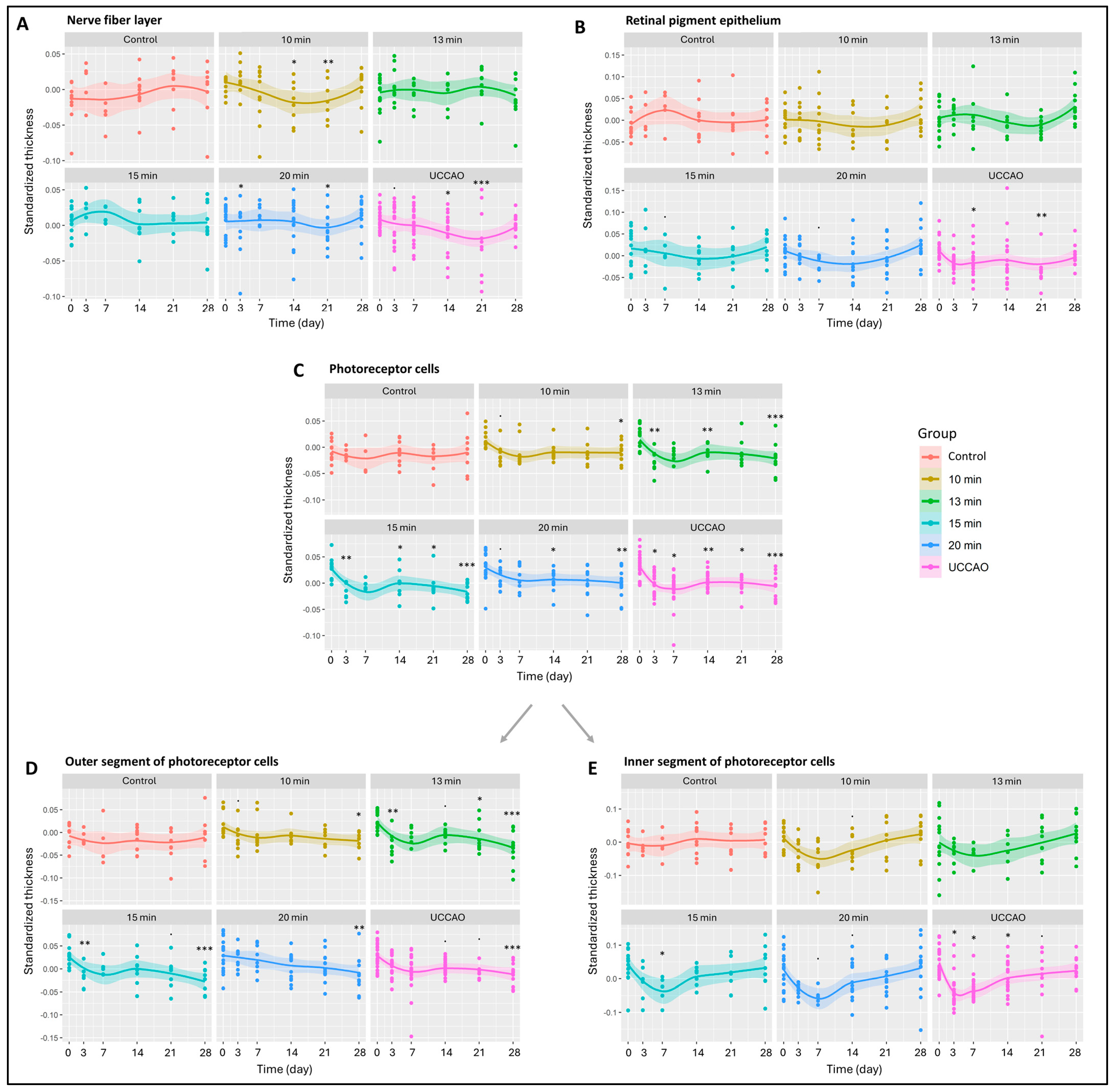
2.1. Optical Coherence Tomography (OCT)
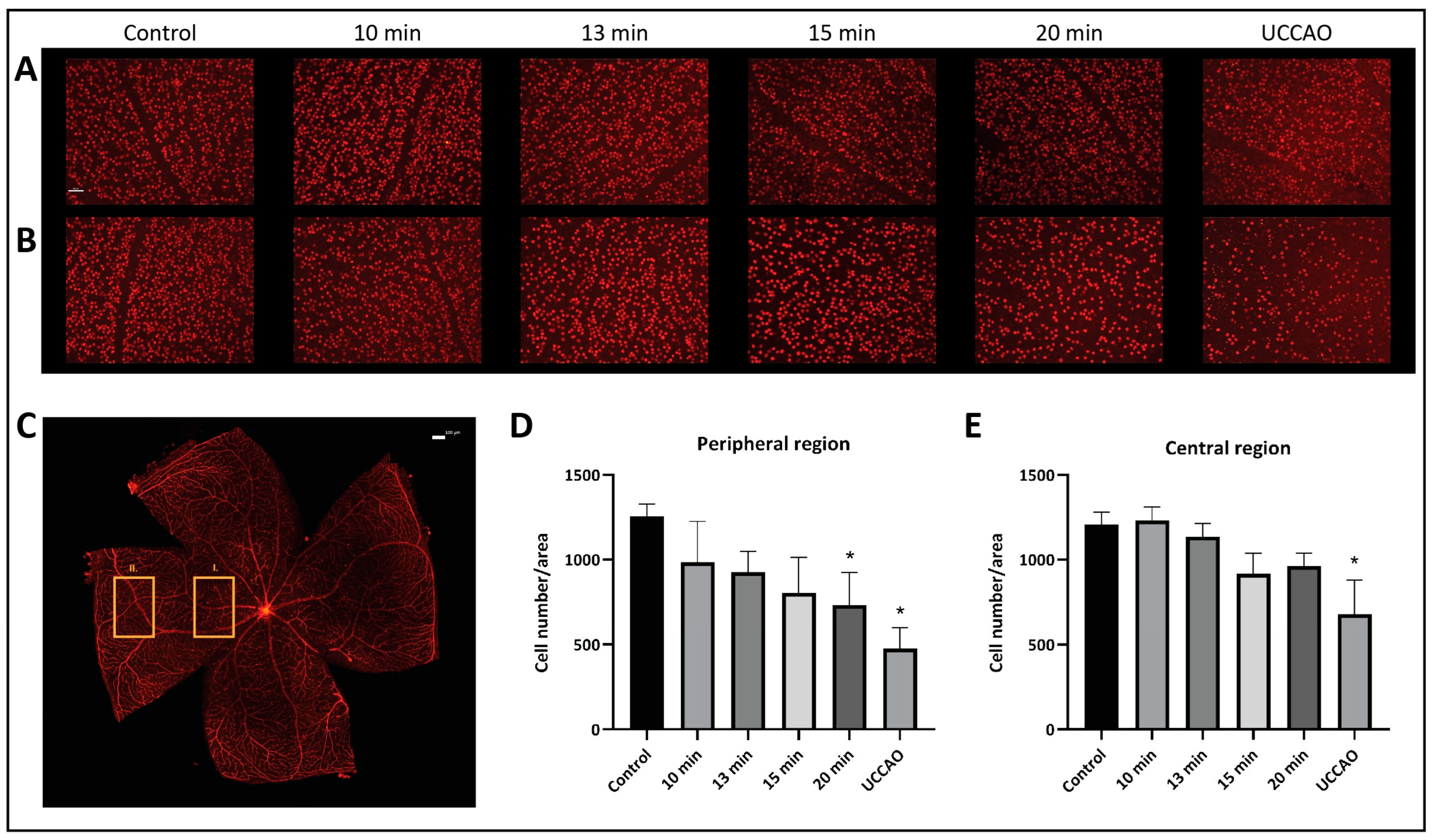
2.2. Retinal Ganglion Cells (Brn3a)
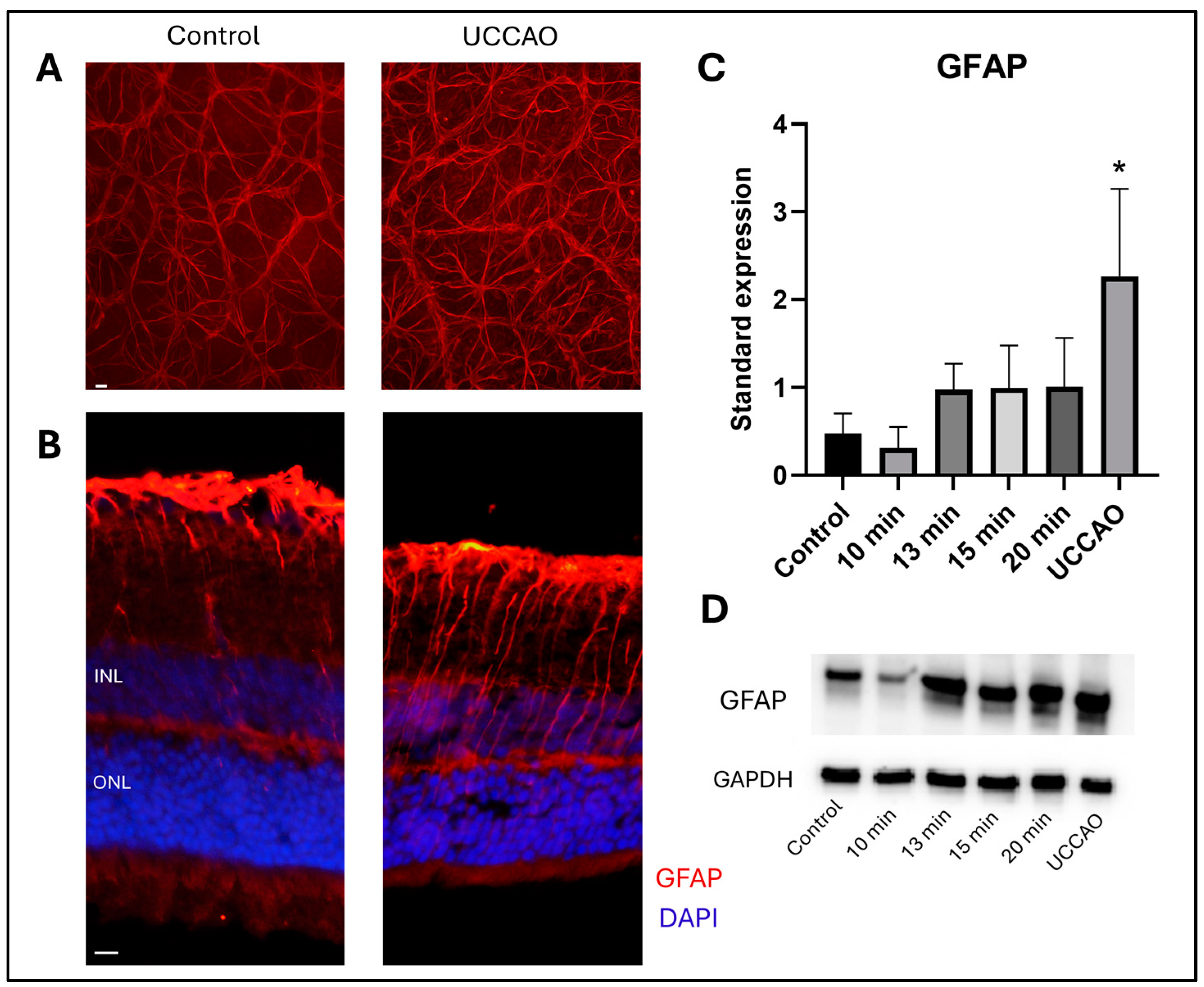
2.3. Retinal Stress (GFAP)
3. Discussion
4. Materials and Methods
4.1. Animals
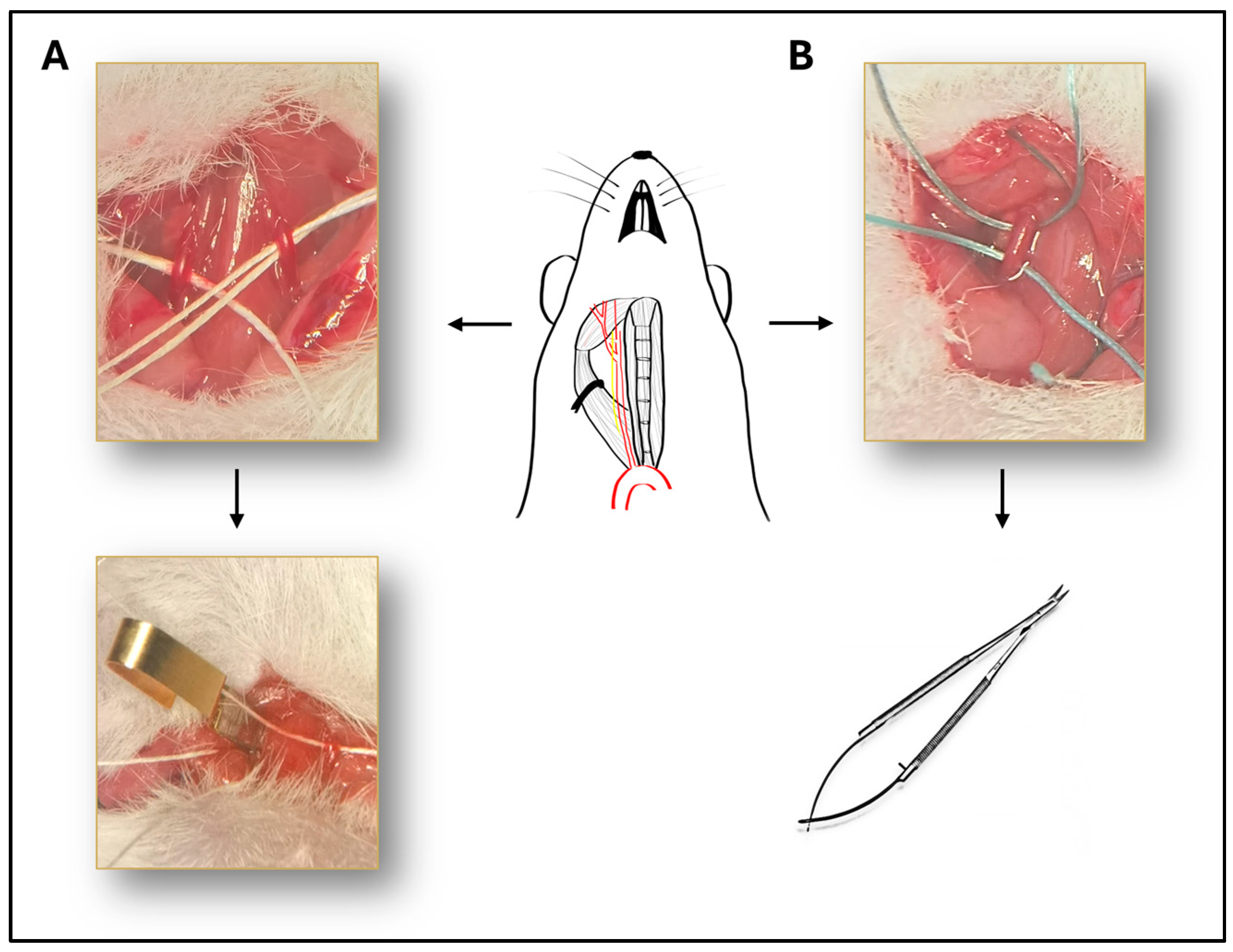
4.2. Surgeries
4.3. Optical Coherence Tomography (OCT)
4.4. Immunohistochemistry
4.5. Western Blot
4.6. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Niven, J.E.; Laughlin, S.B. Energy Limitation as a Selective Pressure on the Evolution of Sensory Systems. J. Exp. Biol. 2008, 211, 1792–1804. [Google Scholar] [CrossRef] [PubMed]
- Youngblood, H.; Robinson, R.; Sharma, A.; Sharma, S. Proteomic Biomarkers of Retinal Inflammation in Diabetic Retinopathy. Int. J. Mol. Sci. 2019, 20, 4755. [Google Scholar] [CrossRef]
- Lai, Y.-F.; Lin, T.-Y.; Chen, Y.-H.; Lu, D.-W. Erythropoietin in Glaucoma: From Mechanism to Therapy. Int. J. Mol. Sci. 2023, 24, 2985. [Google Scholar] [CrossRef]
- Thomas, C.J.; Mirza, R.G.; Gill, M.K. Age-Related Macular Degeneration. Med. Clin. N. Am. 2021, 105, 473–491. [Google Scholar] [CrossRef]
- Arden, G.B.; Sivaprasad, S. Hypoxia and Oxidative Stress in the Causation of Diabetic Retinopathy. Curr. Diabetes Rev. 2011, 7, 291–304. [Google Scholar] [CrossRef] [PubMed]
- Leley, S.P.; Ciulla, T.A.; Bhatwadekar, A. Diabetic Retinopathy in the Aging Population: A Perspective of Pathogenesis and Treatment. Clin. Interv. Aging 2021, 16, 1367–1378. [Google Scholar] [CrossRef]
- Stahl, A.; Sukgen, E.A.; Wu, W.-C.; Lepore, D.; Nakanishi, H.; Mazela, J.; Moshfeghi, D.M.; Vitti, R.; Athanikar, A.; Chu, K.; et al. Effect of Intravitreal Aflibercept vs Laser Photocoagulation on Treatment Success of Retinopathy of Prematurity. JAMA 2022, 328, 348. [Google Scholar] [CrossRef]
- Liu, Y.; Wu, N. Progress of Nanotechnology in Diabetic Retinopathy Treatment. Int. J. Nanomed. 2021, 16, 1391–1403. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-N.; Chen, S.-J.; Wu, T.-T.; Wu, W.-C.; Yang, C.-H.; Yang, C.-M. Refining Vitrectomy for Proliferative Diabetic Retinopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2023, 261, 3659–3670. [Google Scholar] [CrossRef]
- Patko, E.; Szabo, E.; Vaczy, A.; Molitor, D.; Tari, E.; Li, L.; Csutak, A.; Toth, G.; Reglodi, D.; Atlasz, T. Protective Effects of Pituitary Adenylate-Cyclase-Activating Polypeptide on Retinal Vasculature and Molecular Responses in a Rat Model of Moderate Glaucoma. Int. J. Mol. Sci. 2023, 24, 13256. [Google Scholar] [CrossRef]
- Nashine, S. Potential Therapeutic Candidates for Age-Related Macular Degeneration (AMD). Cells 2021, 10, 2483. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liu, X.; Zhong, H.; Fang, J.; Li, X.; Shi, R.; Yu, Q. Research Progress on the Pathogenesis of Diabetic Retinopathy. BMC Ophthalmol. 2023, 23, 372. [Google Scholar] [CrossRef]
- Klemm, P.; Hurst, J.; Dias Blak, M.; Herrmann, T.; Melchinger, M.; Bartz-Schmidt, K.U.; Zeck, G.; Schultheiss, M.; Spitzer, M.S.; Schnichels, S. Hypothermia Protects Retinal Ganglion Cells against Hypoxia-induced Cell Death in a Retina Organ Culture Model. Clin. Exp. Ophthalmol. 2019, 47, 1043–1054. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, M.; Tiwari, P.; Dada, T.; Dada, R. Beyond the Optic Nerve: Genetics, Diagnosis, and Promising Therapies for Glaucoma. Gene 2024, 894, 147983. [Google Scholar] [CrossRef] [PubMed]
- Szabo, M.E.; Droy-Lefaix, M.T.; Doly, M.; Carré, C.; Braquet, P. Ischemia and Reperfusion-Induced Histologic Changes in the Rat Retina. Demonstration of a Free Radical-Mediated Mechanism. Investig. Ophthalmol. Vis. Sci. 1991, 32, 1471–1478. [Google Scholar]
- Crespo-Garcia, S.; Reichhart, N.; Skosyrski, S.; Foddis, M.; Wu, J.; Figura, A.; Herrspiegel, C.; Füchtemeier, M.; Sassi, C.; Dirnagl, U.; et al. Individual and Temporal Variability of the Retina after Chronic Bilateral Common Carotid Artery Occlusion (BCCAO). PLoS ONE 2018, 13, e0193961. [Google Scholar] [CrossRef]
- Werling, D.; Banks, W.; Salameh, T.; Kvarik, T.; Kovacs, L.; Vaczy, A.; Szabo, E.; Mayer, F.; Varga, R.; Tamas, A.; et al. Passage through the Ocular Barriers and Beneficial Effects in Retinal Ischemia of Topical Application of PACAP1-38 in Rodents. Int. J. Mol. Sci. 2017, 18, 675. [Google Scholar] [CrossRef]
- Vaczy, A.; Reglodi, D.; Somoskeoy, T.; Kovacs, K.; Lokos, E.; Szabo, E.; Tamas, A.; Atlasz, T. The Protective Role of PAC1-Receptor Agonist Maxadilan in BCCAO-Induced Retinal Degeneration. J. Mol. Neurosci. 2016, 60, 186–194. [Google Scholar] [CrossRef]
- Linsenmeier, R.A.; Zhang, H.F. Retinal Oxygen: From Animals to Humans. Prog. Retin. Eye Res. 2017, 58, 115–151. [Google Scholar] [CrossRef]
- Iwasaki, M.; Inomata, H. Relation between Superficial Capillaries and Foveal Structures in the Human Retina. Investig. Ophthalmol. Vis. Sci. 1986, 27, 1698–1705. [Google Scholar]
- Schröder, H.; Moser, N.; Huggenberger, S. Neuroanatomy of the Mouse; Springer International Publishing: Cham, Switzerland, 2020; ISBN 978-3-030-19897-8. [Google Scholar]
- Lee, D.; Kang, H.; Yoon, K.Y.; Chang, Y.Y.; Song, H.B. A Mouse Model of Retinal Hypoperfusion Injury Induced by Unilateral Common Carotid Artery Occlusion. Exp. Eye Res. 2020, 201, 108275. [Google Scholar] [CrossRef] [PubMed]
- Leahy, S.; Farzad, S.; Blair, N.P.; Shahidi, M. Retinal Oxygen Delivery, Metabolism, and Extraction Fraction during Long-Term Bilateral Common Carotid Artery Occlusion in Rats. Sci. Rep. 2020, 10, 10371. [Google Scholar] [CrossRef] [PubMed]
- Kiseleva, T.N.; Chudin, A.V.; Khoroshilova-Maslova, I.P.; Shchipanova, A.I.; Maibogin, A.M.; Zaitsev, M.S. Morphological Changes in the Retina Under Conditions of Experimental In Vivo Regional Ischemia/Reperfusion. Bull. Exp. Biol. Med. 2019, 167, 287–292. [Google Scholar] [CrossRef]
- Wanek, J.; Teng, P.; Blair, N.P.; Shahidi, M. Inner Retinal Oxygen Delivery and Metabolism Under Normoxia and Hypoxia in Rat. Investig. Opthalmol. Vis. Sci. 2013, 54, 5012. [Google Scholar] [CrossRef] [PubMed]
- Kim, U.S.; Mahroo, O.A.; Mollon, J.D.; Yu-Wai-Man, P. Retinal Ganglion Cells—Diversity of Cell Types and Clinical Relevance. Front. Neurol. 2021, 12, 661938. [Google Scholar] [CrossRef] [PubMed]
- Adamiec-Mroczek, J.; Zając-Pytrus, H.; Misiuk-Hojło, M. Caspase-Dependent Apoptosis of Retinal Ganglion Cells During the Development of Diabetic Retinopathy. Adv. Clin. Exp. Med. 2015, 24, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Munemasa, Y.; Kitaoka, Y. Molecular Mechanisms of Retinal Ganglion Cell Degeneration in Glaucoma and Future Prospects for Cell Body and Axonal Protection. Front. Cell Neurosci. 2013, 6, 60. [Google Scholar] [CrossRef] [PubMed]
- Kuehn, M.; Fingert, J.; Kwon, Y. Retinal Ganglion Cell Death in Glaucoma: Mechanisms and Neuroprotective Strategies. Ophthalmol. Clin. N. Am. 2005, 18, 383–395. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Sha, O.; Cho, E.Y.P. Remote Ischemic Postconditioning Promotes the Survival of Retinal Ganglion Cells after Optic Nerve Injury. J. Mol. Neurosci. 2013, 51, 639–646. [Google Scholar] [CrossRef]
- Ingensiep, C.; Schaffrath, K.; Denecke, B.; Walter, P.; Johnen, S. A Multielectrode Array-based Hypoxia Model for the Analysis of Electrical Activity in Murine Retinae. J. Neurosci. Res. 2021, 99, 2172–2187. [Google Scholar] [CrossRef]
- Ruzafa, N.; Rey-Santano, C.; Mielgo, V.; Pereiro, X.; Vecino, E. Effect of Hypoxia on the Retina and Superior Colliculus of Neonatal Pigs. PLoS ONE 2017, 12, e0175301. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Yokoi, T.; Tanaka, T.; Matsuzaka, E.; Saida, Y.; Nishina, S.; Takada, S.; Shimizu, S.; Azuma, N. Modeling of Retina and Optic Nerve Ischemia-Reperfusion Injury through Hypoxia-Reoxygenation in Human Induced Pluripotent Stem Cell-Derived Retinal Ganglion Cells. Cells 2024, 13, 130. [Google Scholar] [CrossRef]
- Jakobs, T.C.; Libby, R.T.; Ben, Y.; John, S.W.M.; Masland, R.H. Retinal Ganglion Cell Degeneration Is Topological but Not Cell Type Specific in DBA/2J Mice. J. Cell Biol. 2005, 171, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Lambrou, G.N.; Sahel, J.A.; Hicks, D. Hypoglycemia Induces General Neuronal Death, Whereas Hypoxia and Glutamate Transport Blockade Lead to Selective Retinal Ganglion Cell Death in Vitro. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2695–2705. [Google Scholar]
- Wang, A.Y.; Lee, P.Y.; Bui, B.V.; Jobling, A.I.; Greferath, U.; Brandli, A.; Dixon, M.A.; Findlay, Q.; Fletcher, E.L.; Vessey, K.A. Potential Mechanisms of Retinal Ganglion Cell Type-specific Vulnerability in Glaucoma. Clin. Exp. Optom. 2020, 103, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Koronyo, Y.; Rentsendorj, A.; Mirzaei, N.; Regis, G.C.; Sheyn, J.; Shi, H.; Barron, E.; Cook-Wiens, G.; Rodriguez, A.R.; Medeiros, R.; et al. Retinal Pathological Features and Proteome Signatures of Alzheimer’s Disease. Acta Neuropathol. 2023, 145, 409–438. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Schmidt-Kastner, R.; Hamasaki, D.I.; Yamamoto, H.; Parel, J.-M. Complex Neurodegeneration in Retina Following Moderate Ischemia Induced by Bilateral Common Carotid Artery Occlusion in Wistar Rats. Exp. Eye Res. 2006, 82, 767–779. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Fan, Y.; Zhang, L.; Wang, Y.-X.J.; Qi, W.; Liang, W.; Wang, C.; TW Yew, D.; Ye, C.; Sha, O. Bilateral Common Carotid Artery Occlusion in Spontaneously Hypertensive Rats: A Feasible Animal Model for Ocular Ischemic Syndrome. Anat. Rec. 2016, 299, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Karamian, P.; Burford, J.; Farzad, S.; Blair, N.P.; Shahidi, M. Alterations in Retinal Oxygen Delivery, Metabolism, and Extraction Fraction During Bilateral Common Carotid Artery Occlusion in Rats. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3247–3253. [Google Scholar] [CrossRef]
- Matei, N.; Leahy, S.; Auvazian, S.; Thomas, B.; Blair, N.P.; Shahidi, M. Relation of Retinal Oxygen Measures to Electrophysiology and Survival Indicators after Permanent, Incomplete Ischemia in Rats. Transl Stroke Res. 2020, 11, 1273–1286. [Google Scholar] [CrossRef]
- Bello, S.M.; Perry, M.N.; Smith, C.L. Know Your Model: A Brief History of Making Mutant Mouse Genetic Models. Lab Anim. 2021, 50, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Szpirer, C. Rat Models of Human Diseases and Related Phenotypes: A Systematic Inventory of the Causative Genes. J. Biomed. Sci. 2020, 27, 84. [Google Scholar] [CrossRef] [PubMed]
- Ebner, L.J.A.; Samardzija, M.; Storti, F.; Todorova, V.; Karademir, D.; Behr, J.; Simpson, F.; Thiersch, M.; Grimm, C. Transcriptomic Analysis of the Mouse Retina after Acute and Chronic Normobaric and Hypobaric Hypoxia. Sci. Rep. 2021, 11, 16666. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Kitagawa, K.; Matsushita, K.; Mabuchi, T.; Yagita, Y.; Yanagihara, T.; Matsumoto, M. C57BL/6 Strain Is Most Susceptible to Cerebral Ischemia Following Bilateral Common Carotid Occlusion among Seven Mouse Strains: Selective Neuronal Death in the Murine Transient Forebrain Ischemia. Brain Res. 1997, 752, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Venkat, P.; Chopp, M.; Chen, J. Models and Mechanisms of Vascular Dementia. Exp. Neurol. 2015, 272, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Zaitoun, I.S.; Shahi, P.K.; Suscha, A.; Chan, K.; McLellan, G.J.; Pattnaik, B.R.; Sorenson, C.M.; Sheibani, N. Hypoxic–Ischemic Injury Causes Functional and Structural Neurovascular Degeneration in the Juvenile Mouse Retina. Sci. Rep. 2021, 11, 12670. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, G.V.; Forrest, M.D.; Clarke, R.H.; Schoene, W.C. Focal Occlusion of the Rabbit Carotid Artery by Endovascular Laser Therapy. Cardiovasc. Interv. Radiol. 1988, 11, 322–324. [Google Scholar] [CrossRef]
- Chen, Y.; Zhu, W.; Zhang, W.; Libal, N.; Murphy, S.J.; Offner, H.; Alkayed, N.J. A Novel Mouse Model of Thromboembolic Stroke. J. Neurosci. Methods 2015, 256, 203–211. [Google Scholar] [CrossRef]
- Szabadfi, K.; Atlasz, T.; Kiss, P.; Danyadi, B.; Tamas, A.; Helyes, Z.; Hashimoto, H.; Shintani, N.; Baba, A.; Toth, G.; et al. Mice Deficient in Pituitary Adenylate Cyclase Activating Polypeptide (PACAP) Are More Susceptible to Retinal Ischemic Injury In Vivo. Neurotox. Res. 2012, 21, 41–48. [Google Scholar] [CrossRef]
- Lee, D.; Miwa, Y.; Jeong, H.; Ikeda, S.-I.; Katada, Y.; Tsubota, K.; Kurihara, T. A Murine Model of Ischemic Retinal Injury Induced by Transient Bilateral Common Carotid Artery Occlusion. J. Vis. Exp. 2020, 165, e61865. [Google Scholar] [CrossRef]
- Fukunaga, K.; Yabuki, Y. SAK3-Induced Neuroprotection Is Mediated by Nicotinic Acetylcholine Receptors. In Nicotinic Acetylcholine Receptor Signaling in Neuroprotection; Springer: Singapore, 2018; pp. 159–171. [Google Scholar]
- Qin, J.; An, L. Optical Coherence Tomography for Ophthalmology Imaging. In Optical Imaging in Human Disease and Biological Research; Springer: Singapore, 2021; pp. 197–216. [Google Scholar]
- Mojahed, D.; Applegate, M.B.; Guo, H.; Taback, B.; Ha, R.; Hibshoosh, H.; Hendon, C.P. Optical Coherence Tomography Holds Promise to Transform the Diagnostic Anatomic Pathology Gross Evaluation Process. J. Biomed. Opt. 2022, 27, 096003. [Google Scholar] [CrossRef] [PubMed]
- Ma, D.; Deng, W.; Khera, Z.; Sajitha, T.A.; Wang, X.; Wollstein, G.; Schuman, J.S.; Lee, S.; Shi, H.; Ju, M.J.; et al. Early Inner Plexiform Layer Thinning and Retinal Nerve Fiber Layer Thickening in Excitotoxic Retinal Injury Using Deep Learning-Assisted Optical Coherence Tomography. Acta Neuropathol. Commun. 2024, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Jeong, H.; Miwa, Y.; Shinojima, A.; Katada, Y.; Tsubota, K.; Kurihara, T. Retinal Dysfunction Induced in a Mouse Model of Unilateral Common Carotid Artery Occlusion. PeerJ 2021, 9, e11665. [Google Scholar] [CrossRef] [PubMed]
- Mesentier-Louro, L.A.; Rangel, B.; Stell, L.; Shariati, M.A.; Dalal, R.; Nathan, A.; Yuan, K.; de Jesus Perez, V.; Liao, Y.J. Hypoxia-Induced Inflammation: Profiling the First 24-Hour Posthypoxic Plasma and Central Nervous System Changes. PLoS ONE 2021, 16, e0246681. [Google Scholar] [CrossRef] [PubMed]
- Lange, J.; Hadziahmetovic, M.; Zhang, J.; Li, W. Region-specific Ischemia, Neovascularization and Macular Oedema in Treatment-naïve Proliferative Diabetic Retinopathy. Clin. Exp. Ophthalmol. 2018, 46, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Gunes, A.; Inal, E.E.; Demirci, S.; Tok, L.; Tok, O.; Demirci, S. Changes in Retinal Nerve Fiber Layer Thickness in Patients with Cerebral Infarction: Evidence of Transneuronal Retrograde Degeneration. Acta Neurol. Belg. 2016, 116, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Vujosevic, S.; Midena, E. Retinal Layers Changes in Human Preclinical and Early Clinical Diabetic Retinopathy Support Early Retinal Neuronal and Müller Cells Alterations. J. Diabetes Res. 2013, 2013, 905058. [Google Scholar] [CrossRef]
- Gemelli, H.; Fidalgo, T.M.; Gracitelli, C.P.B.; de Andrade, E.P. Retinal Nerve Fiber Layer Analysis in Cocaine Users. Psychiatry Res. 2019, 271, 226–229. [Google Scholar] [CrossRef] [PubMed]
- Abtahi, S.-H.; Nourinia, R.; Mazloumi, M.; Nouri, H.; Arevalo, J.F.; Ahmadieh, H. Retinal Ischemic Cascade: New Insights into the Pathophysiology and Imaging Findings. Surv. Ophthalmol. 2023, 68, 380–387. [Google Scholar] [CrossRef]
- Palmhof, M.; Frank, V.; Rappard, P.; Kortenhorn, E.; Demuth, J.; Biert, N.; Stute, G.; Dick, H.B.; Joachim, S.C. From Ganglion Cell to Photoreceptor Layer: Timeline of Deterioration in a Rat Ischemia/Reperfusion Model. Front. Cell. Neurosci. 2019, 13, 174. [Google Scholar] [CrossRef]
- Kurihara, T. Roles of Hypoxia Response in Retinal Development and Pathophysiology. Keio J. Med. 2017, 67, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Datlinger, F.; Wassermann, L.; Reumueller, A.; Hajdu, D.; Steiner, I.; Salas, M.; Drexler, W.; Pircher, M.; Schmidt-Erfurth, U.; Pollreisz, A. Assessment of Detailed Photoreceptor Structure and Retinal Sensitivity in Diabetic Macular Ischemia Using Adaptive Optics-OCT and Microperimetry. Investig. Opthalmol. Vis. Sci. 2021, 62, 1. [Google Scholar] [CrossRef]
- Nesper, P.L.; Scarinci, F.; Fawzi, A.A. Adaptive Optics Reveals Photoreceptor Abnormalities in Diabetic Macular Ischemia. PLoS ONE 2017, 12, e0169926. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.E.G.; Sundelin, S.P.; Wihlmark, U.; Brunk, U.T. Aging of Cultured Retinal Pigment Epithelial Cells: Oxidative Reactions, Lipofuscin Formation and Blue Light Damage. Doc. Ophthalmol. 2003, 106, 13–16. [Google Scholar] [CrossRef]
- Piskova, T.; Kozyrina, A.N.; Di Russo, J. Mechanobiological Implications of Age-Related Remodelling in the Outer Retina. Biomater. Adv. 2023, 147, 213343. [Google Scholar] [CrossRef] [PubMed]
- Stefánsson, E.; Geirsdóttir, Á.; Sigurdsson, H. Metabolic Physiology in Age Related Macular Degeneration. Prog. Retin. Eye Res. 2011, 30, 72–80. [Google Scholar] [CrossRef]
- Cheng, K.-C.; Hsu, Y.-T.; Liu, W.; Huang, H.-L.; Chen, L.-Y.; He, C.-X.; Sheu, S.-J.; Chen, K.-J.; Lee, P.-Y.; Lin, Y.-H.; et al. The Role of Oxidative Stress and Autophagy in Blue-Light-Induced Damage to the Retinal Pigment Epithelium in Zebrafish In Vitro and In Vivo. Int. J. Mol. Sci. 2021, 22, 1338. [Google Scholar] [CrossRef]
- Masland, R.H. The Neuronal Organization of the Retina. Neuron 2012, 76, 266–280. [Google Scholar] [CrossRef]
- Li, L.; Huang, H.; Fang, F.; Liu, L.; Sun, Y.; Hu, Y. Longitudinal Morphological and Functional Assessment of RGC Neurodegeneration After Optic Nerve Crush in Mouse. Front. Cell. Neurosci. 2020, 14, 109. [Google Scholar] [CrossRef]
- Shindler, R.E.; Yue, J.; Chaqour, B.; Shindler, K.S.; Ross, A.G. Repeat Brn3a Immunolabeling Rescues Faded Staining and Improves Detection of Retinal Ganglion Cells. Exp. Eye Res. 2023, 226, 109310. [Google Scholar] [CrossRef]
- Potilinski, M.C.; Lorenc, V.; Perisset, S.; Gallo, J.E. Mechanisms behind Retinal Ganglion Cell Loss in Diabetes and Therapeutic Approach. Int. J. Mol. Sci. 2020, 21, 2351. [Google Scholar] [CrossRef] [PubMed]
- Almasieh, M.; Wilson, A.M.; Morquette, B.; Cueva Vargas, J.L.; Di Polo, A. The Molecular Basis of Retinal Ganglion Cell Death in Glaucoma. Prog. Retin. Eye Res. 2012, 31, 152–181. [Google Scholar] [CrossRef]
- Porciatti, V.; Chou, T.-H. Modeling Retinal Ganglion Cell Dysfunction in Optic Neuropathies. Cells 2021, 10, 1398. [Google Scholar] [CrossRef]
- Yang, Y.; Sun, X. Retinal Ganglion Cell Death in Glaucoma: Advances and Caveats. Curr. Eye Res. 2023, 48, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Atlasz, T.; Szabadfi, K.; Kiss, P.; Tamas, A.; Toth, G.; Reglodi, D.; Gabriel, R. Evaluation of the Protective Effects of PACAP with Cell-Specific Markers in Ischemia-Induced Retinal Degeneration. Brain Res. Bull. 2010, 81, 497–504. [Google Scholar] [CrossRef]
- Choudhary, T.R.; Ball, D.; Fernandez Ramos, J.; McNaught, A.I.; Harvey, A.R. Assessment of Acute Mild Hypoxia on Retinal Oxygen Saturation Using Snapshot Retinal Oximetry. Investig. Opthalmol. Vis. Sci. 2013, 54, 7538. [Google Scholar] [CrossRef] [PubMed]
- Mathew, B.; Chennakesavalu, M.; Sharma, M.; Torres, L.A.; Stelman, C.R.; Tran, S.; Patel, R.; Burg, N.; Salkovski, M.; Kadzielawa, K.; et al. Autophagy and Post-Ischemic Conditioning in Retinal Ischemia. Autophagy 2021, 17, 1479–1499. [Google Scholar] [CrossRef]
- Fernandez, D.C.; Bordone, M.P.; Chianelli, M.S.; Rosenstein, R.E. Retinal Neuroprotection against Ischemia-Reperfusion Damage Induced by Postconditioning. Investig. Opthalmol. Vis. Sci. 2009, 50, 3922. [Google Scholar] [CrossRef]
- Kvarik, T.; Reglodi, D.; Werling, D.; Vaczy, A.; Kovari, P.; Szabo, E.; Kovacs, K.; Hashimoto, H.; Ertl, T.; Gyarmati, J.; et al. The Protective Effects of Endogenous PACAP in Oxygen-Induced Retinopathy. J. Mol. Neurosci. 2021, 71, 2546–2557. [Google Scholar] [CrossRef]
- Willems, E.; Leyns, L.; Vandesompele, J. Standardization of Real-Time PCR Gene Expression Data from Independent Biological Replicates. Anal. Biochem. 2008, 379, 127–129. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Wickham, H. Ggplot2—Elegant Graphics for Data Analysis; Springer International Publishing: Cham, Switzerland, 2016; ISBN 978-3-319-24275-0. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bosnyak, I.; Farkas, N.; Molitor, D.; Meresz, B.; Patko, E.; Atlasz, T.; Vaczy, A.; Reglodi, D. Optimization of an Ischemic Retinopathy Mouse Model and the Consequences of Hypoxia in a Time-Dependent Manner. Int. J. Mol. Sci. 2024, 25, 8008. https://doi.org/10.3390/ijms25158008
Bosnyak I, Farkas N, Molitor D, Meresz B, Patko E, Atlasz T, Vaczy A, Reglodi D. Optimization of an Ischemic Retinopathy Mouse Model and the Consequences of Hypoxia in a Time-Dependent Manner. International Journal of Molecular Sciences. 2024; 25(15):8008. https://doi.org/10.3390/ijms25158008
Chicago/Turabian StyleBosnyak, Inez, Nelli Farkas, Dorottya Molitor, Balazs Meresz, Evelin Patko, Tamas Atlasz, Alexandra Vaczy, and Dora Reglodi. 2024. "Optimization of an Ischemic Retinopathy Mouse Model and the Consequences of Hypoxia in a Time-Dependent Manner" International Journal of Molecular Sciences 25, no. 15: 8008. https://doi.org/10.3390/ijms25158008





