Association of SDF-1-3′ Gene A Variant with Diabetic Retinopathy in the Hungarian Population
Abstract
:1. Introduction
2. Results
2.1. Patient Characteristics
2.2. Genotype Distribution and Allele Frequencies
2.3. Genetic Association with Sight-Threatening Retinal Complications
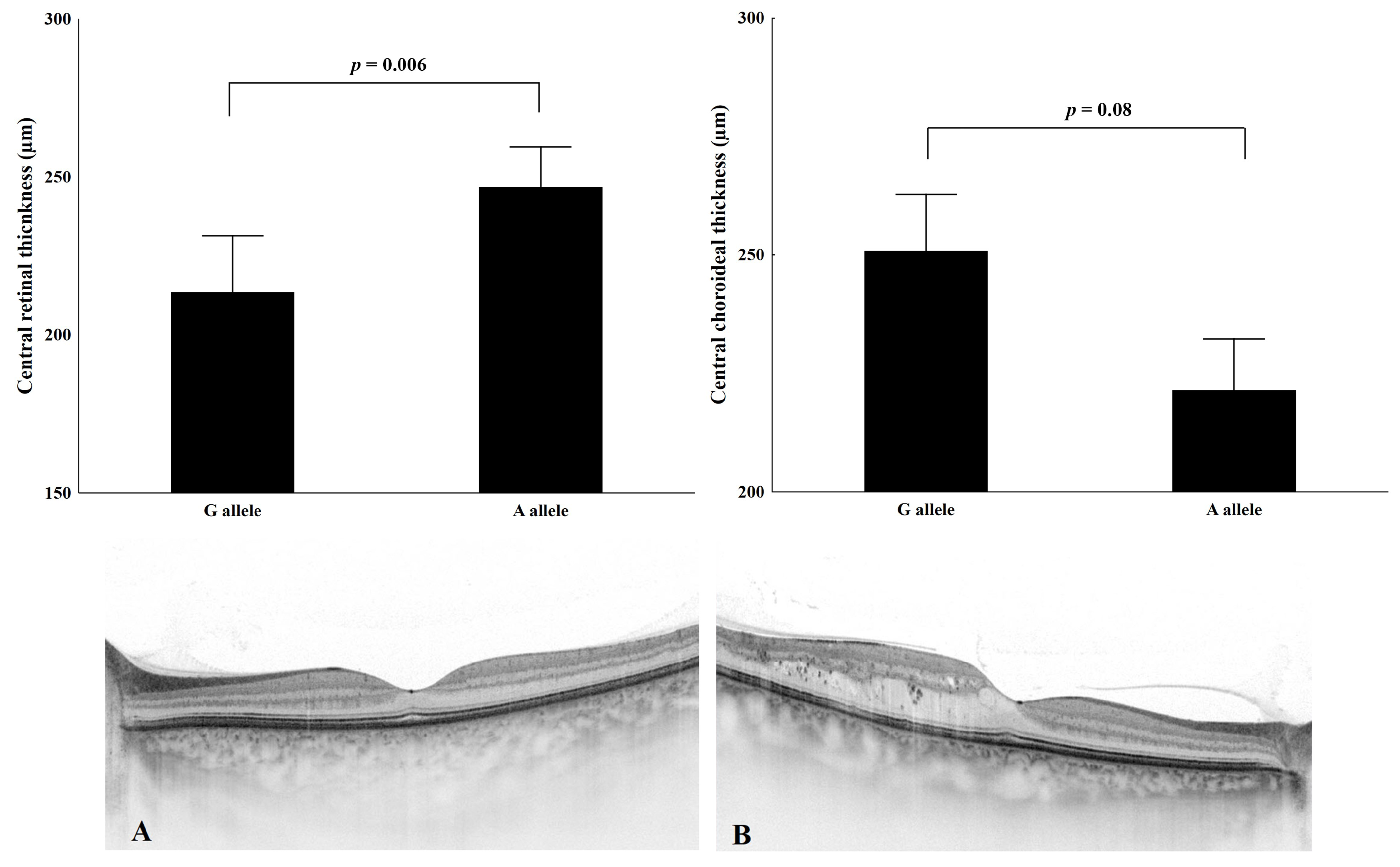
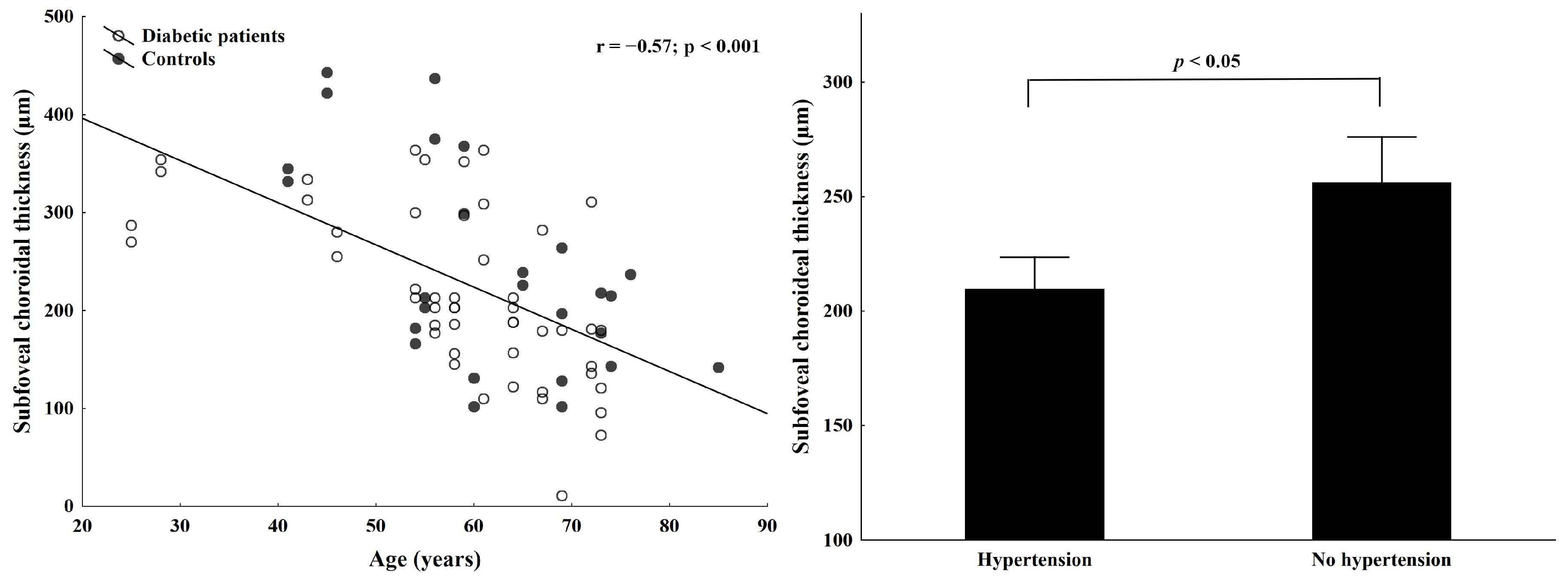
2.4. Association of Macular and Choroidal Thickness with SDF1 (c801A) Allele
2.5. Onset of DME and Genetic Background
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. Clinical History and Routine Laboratory Parameters
4.3. Ophthalmological Examination
4.4. DNA Extraction and Genotyping
4.5. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thomas, R.; Halim, S.; Gurudas, S.; Sivaprasad, S.; Owens, D. IDF Diabetes Atlas: A review of studies utilising retinal photography on the global prevalence of diabetes related retinopathy between 2015 and 2018. Diabetes Res. Clin. Pract. 2019, 157, 107840. [Google Scholar] [CrossRef]
- Cabrera, A.P.; Monickaraj, F.; Rangasamy, S.; Hobbs, S.; McGuire, P.; Das, A. Do genomic factors play a role in diabetic retinopathy? J. Clin. Med. 2020, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Warpeha, K.M.; Chakravarthy, U. Molecular genetics of microvascular disease in diabetic retinopathy. Eye 2003, 17, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Aldhahi, W.; Hamdy, O. Adipokines, inflammation, and the endothelium in diabetes. Curr. Diabetes Rep. 2003, 3, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Luster, D.A. Chemokines—Chemotactic cytokines that mediate inflammation. N. Engl. J. Med. 1998, 338, 436–445. Available online: http://www.ncbi.nlm.nih.gov/pubmed/9459648 (accessed on 2 July 2024). [CrossRef] [PubMed]
- Aiuti, A.; Webb, I.J.; Bleul, C.; Springer, T.; Gutierrez-Ramos, J.C. The chemokine SDF-1 is a chemoattractant for human CD34+ hematopoietic progenitor cells and provides a new mechanism to explain the mobilization of CD34+ progenitors to peripheral blood . J. Exp. Med. 1997, 185, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Bleul, C.; Fuhlbrigge, R.C.; Casasnovas, J.M.; Aiuti, A.; Springer, T. A Highly Efficacious Lymphocyte Chemoattractant, Stromal Cell-derived Factor-1 (SDF-1). J. Exp. Med. 1996, 184, 1101–1109. [Google Scholar] [CrossRef]
- You, S.; Chen, H.; Miao, M.; Du, J.; Che, B.; Xu, T.; Liu, C.-F.; Zhang, Y.; He, J.; Zhong, X.; et al. Prognostic significance of plasma SDF-1 in acute ischemic stroke patients with diabetes mellitus: The CATIS trial. Cardiovasc. Diabetol. 2023, 22, 274. [Google Scholar] [CrossRef]
- Liu, W.-S.; Hua, L.-Y.; Zhu, S.-X.; Xu, F.; Wang, X.-Q.; Lu, C.-F.; Su, J.-B.; Qi, F. Association of serum stromal cell-derived factor 1 levels with EZSCAN score and its derived indicators in patients with type 2 diabetes. Endocr. Connect. 2022, 11, e210629. [Google Scholar] [CrossRef]
- Butler, J.M.; Guthrie, S.M.; Koc, M.; Afzal, A.; Caballero, S.; Brooks, H.L.; Mames, R.N.; Segal, M.S.; Grant, M.B.; Scott, E.W. SDF-1 is both necessary and sufficient to promote proliferative retinopathy. J. Clin. Investig. 2005, 115, 86–93. [Google Scholar] [CrossRef]
- Humpert, P.M.; Neuwirth, R.; Battista, M.J.; Voronko, O.; von Eynatten, M.; Konrade, I.; Rudofsky, G.; Wendt, T.; Hamann, A.; Morcos, M.; et al. SDF-1 Genotype Influences Insulin-Dependent Mobilization of Adult Progenitor Cells in Type 2 Diabetes. Diabetes Care 2005, 28, 934–936. [Google Scholar] [CrossRef] [PubMed]
- Sei, S.; O’Neill, D.P.; Stewart, S.K.; Yang, Q.; Kumagai, M.; Boler, A.M.; Adde, M.A.; Zwerski, S.L.; Wood, L.V.; Venzon, D.J.; et al. Increased level of stromal cell-derived factor-1 mRNA in peripheral blood mononuclear cells from children with AIDS-related lymphoma. Cancer Res. 2001, 61, 5028–5037. [Google Scholar] [PubMed]
- Brooks, H.L.; Caballero, S.; Newell, C.K.; Steinmetz, R.L.; Watson, D.; Segal, M.S.; Harrison, J.K.; Scott, E.W.; Grant, M.B. Vitreous Levels of Vascular Endothelial Growth Factor and Stromal-Derived Factor 1 in Patients with Diabetic Retinopathy and Cystoid Macular Injection of Triamcinolone. Arch. Ophthalmol. 2004, 122, 1801–1807. [Google Scholar] [CrossRef]
- Winkler, C.; Modi, W.; Smith, M.W.; Nelson, G.W.; Wu, X.; Carrington, M.; Dean, M.; Honjo, T.; Tashiro, K.; Yabe, D.; et al. Genetic restriction of AIDS pathogenesis by an SDF-1 chemokine gene variant. Science 1998, 279, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Ide, A.; Kawasaki, E.; Abiru, N.; Sun, F.; Fukushima, T.; Takahashi, R.; Kuwahara, H.; Fujita, N.; Kita, A.; Oshima, K.; et al. Stromal-cell derived factor-1 chemokine gene variant is associated with type 1 diabetes age at onset in Japanese population. Hum. Immunol. 2003, 64, 973–978. [Google Scholar] [CrossRef]
- Dubois-Laforgue, D.; Hendel, H.; Caillat-Zucman, S.; Zagury, J.-F.; Winkler, C.; Boitard, C.; Timsit, J. A common stromal cell–derived factor-1 chemokine gene variant is associated with the early onset of type 1 diabetes. Diabetes 2001, 50, 1211–1213. [Google Scholar] [CrossRef]
- Peng, S.-Y.; Chuang, C.-C.; Hwang, Y.-S.; Yen, C.-H.; Lee, C.-Y.; Yang, S.-F. Association of SDF-1 and its receptor CXCR4 polymorphisms on the susceptibility of diabetic retinopathy in the Taiwanese population. Front. Genet. 2023, 14, 1296773. [Google Scholar] [CrossRef]
- Ikuno, Y.; Kawaguchi, K.; Nouchi, T.; Yasuno, Y. Choroidal thickness in healthy Japanese subjects. Investig. Opthalmol. Vis. Sci. 2010, 51, 2173–2176. [Google Scholar] [CrossRef]
- Ouyang, Y.; Heussen, F.M.; Mokwa, N.; Walsh, A.C.; Durbin, M.K.; Keane, P.A.; Sanchez, P.J.; Ruiz-Garcia, H.; Sadda, S.R. Spatial distribution of posterior pole choroidal thickness by spectral domain optical coherence tomography. Investig. Opthalmol. Vis. Sci. 2011, 52, 7019–7026. [Google Scholar] [CrossRef]
- Ruiz-Medrano, J.; Flores-Moreno, I.; Peña-García, P.; Montero, J.A.; Duker, J.S.; Ruiz-Moreno, J.M. Macular choroidal thickness profile in a healthy population measured by swept-source optical coherence tomography. Investig. Opthalmol. Vis. Sci. 2014, 55, 3532–3542. [Google Scholar] [CrossRef]
- Kempen, J.H.; O’Colmain, B.J.; Leske, M.C.; Haffner, S.M.; Klein, R.; Moss, S.E.; Taylor, H.R.; Hamman, R.F. The prevalence of diabetic retinopathy among adults in the United States. Arch. Ophthalmol. 2004, 122, 552–563. [Google Scholar] [CrossRef]
- Hove, M.N.; Kristensen, J.K.; Lauritzen, T.; Bek, T. The relationships between risk factors and the distribution of retinopathy lesions in type 2 diabetes. Acta Ophthalmol. Scand. 2006, 84, 619–623. [Google Scholar] [CrossRef]
- Cunha-Vaz, J.; Ribeiro, L.; Lobo, C. Phenotypes and biomarkers of diabetic retinopathy. Prog. Retin. Eye Res. 2014, 41, 90–111. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. The expert committee on the diagnosis and classification of diabetes mellitus* report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2002, 25, S5–S20. [Google Scholar] [CrossRef]
- Guleng, B.; Tateishi, K.; Ohta, M.; Kanai, F.; Jazag, A.; Ijichi, H.; Tanaka, Y.; Washida, M.; Morikane, K.; Fukushima, Y.; et al. Blockade of the stromal cell–derived factor-1/CXCR4 axis attenuates in vivo tumor growth by inhibiting angiogenesis in a vascular endothelial growth factor–independent manner. Cancer Res. 2005, 65, 5864–5871. [Google Scholar] [CrossRef]
- Dar, A.; Kollet, O.; Lapidot, T. Mutual, reciprocal SDF-1/CXCR4 interactions between hematopoietic and bone marrow stromal cells regulate human stem cell migration and development in NOD/SCID chimeric mice. Exp. Hematol. 2006, 34, 967–975. [Google Scholar] [CrossRef] [PubMed]
- Jin, D.K.; Shido, K.; Kopp, H.G.; Petit, I.; Shmelkov, S.V.; Young, L.M.; Hooper, A.T.; Amano, H.; Avecilla, S.T.; Heissig, B.; et al. Cytokine-mediated deployment of SDF-1 induces revascularization through recruitment of CXCR4+ hemangiocytes. Nat. Med. 2006, 12, 557–567, Erratum in Nat Med. 2006, 12, 978.. [Google Scholar] [CrossRef] [PubMed]
- A Bhutto, I.; McLeod, D.S.; Merges, C.; Hasegawa, T.; A Lutty, G. Localisation of SDF-1 and its receptor CXCR4 in retina and choroid of aged human eyes and in eyes with age related macular degeneration. Br. J. Ophthalmol. 2006, 90, 906–910. [Google Scholar] [CrossRef] [PubMed]
- Mirshahi, F.; Pourtau, J.; Li, H.; Muraine, M.; Trochon, V.; Legrand, E.; Vannier, J.-P.; Soria, J.; Vasse, M.; Soria, C. SDF-1 activity on microvascular endothelial cells. Thromb. Res. 2000, 99, 587–594. [Google Scholar] [CrossRef]
- Salcedo, R.; Wasserman, K.; Young, H.A.; Grimm, M.C.; Howard, O.M.Z.; Anver, M.R.; Kleinman, H.K.; Murphy, W.J.; Oppenheim, J.J. Vascular endothelial growth factor and basic fibroblast growth factor induce expression of CXCR4 on human endothelial cells. Am. J. Pathol. 1999, 154, 1125–1135. [Google Scholar] [CrossRef]
- Wu, D.; Jin, L.; Xu, H. The effects of the CXCR4 antagonist, AMD3465, on Human Retinal Vascular Endothelial Cells (hRVECs) in a high glucose model of diabetic retinopathy. Med. Sci. Monit. 2019, 25, 6957–6965. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.M. Role of Stromal Cell-Derived Factor 1 in Proliferative Retinopathy. Ph.D. Thesis, University of Florida, Gainesville, FL, USA, 2006. [Google Scholar]
- Regatieri, C.V.; Branchini, L.; Carmody, J.; Fujimoto, J.G.; Duker, J.S. Choroidal thickness in patients with diabetic retinopathy analyzed by spectral-domain optical coherence tomography. Retina 2012, 32, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Gerendas, B.S.; Waldstein, S.M.; Deak, G.; Hajnajeeb, B.; Zhang, L.; Bogunovic, H.; Abramoff, M.D.; Kundi, M.; Sonka, M.; Schmidt-Erfurth, U. Three-dimensional automated choroidal volume assessment on standard spectral-domain optical coherence tomography and correlation with the level of diabetic macular edema. Am. J. Ophthalmol. 2014, 158, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Querques, G.; Lattanzio, R.; Querques, L.; Del Turco, C.; Forte, R.; Pierro, L.; Souied, E.H.; Bandello, F. Enhanced depth imaging optical coherence tomography in type 2 diabetes. Investig. Opthalmology Vis. Sci. 2012, 53, 6017–6024. [Google Scholar] [CrossRef] [PubMed]
- Akkaya, S. Macular and peripapillary choroidal thickness in patients with keratoconus. Ophthalmic Surg. Lasers Imaging Retin. 2018, 49, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Xu, L.; Du, K.F.; Shao, L.; Chen, C.X.; Zhou, J.Q.; Wang, Y.X.; You, Q.S.; Jonas, J.B.; Bin Wei, W. Subfoveal choroidal thickness in diabetes and diabetic retinopathy. Ophthalmology 2013, 120, 2023–2028. [Google Scholar] [CrossRef]
- Yazici, A.; Sari, E.S.; Koc, R.; Sahin, G.; Kurt, H.; Ozdal, P.C.; Ermis, S.S. Alterations of choroidal thickness with diabetic neuropathy. Investig. Opthalmology Vis. Sci. 2016, 57, 1518. [Google Scholar] [CrossRef]
- Horváth, H.; Kovács, I.; Sándor, G.L.; Czakó, C.; Mallár, K.; Récsán, Z.; Somogyi, A.; Nagy, Z.Z.; Ecsedy, M. Choroidal thickness changes in non-treated eyes of patients with diabetes: Swept-source optical coherence tomography study. Acta Diabetol. 2018, 55, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Chen, M.; Forrester, J.V.; Lois, N. Cataract surgery induces retinal pro-inflammatory gene expression and protein secretion. Investig. Ophthalmol. Vis. Sci. 2011, 52, 249–255. [Google Scholar] [CrossRef]
- Szemészeti, K.A. Kollégium, A szemészeti szövõdmények terápiája diabetes mellitusban. Diabetologia Hungarica 2005, 12 (Suppl. S5), 22–28. [Google Scholar]
- Cheung, N.; Mitchell, P.; Wong, T.Y. Diabetic retinopathy. Lancet 2010, 376, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Conrath, J.; Giorgi, R.; Raccah, D.; Ridings, B. Foveal avascular zone in diabetic retinopathy: Quantitative vs qualitative assessment. Eye 2004, 19, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Early Treatment Diabetic Retinopathy Study Research Group. Classification of Diabetic Retinopathy from Fluorescein Angiograms. Ophthalmology 1991, 98, 807–822. [CrossRef]

| Variables | Controls (n = 31) | T1DM (n = 28) | T2DM (n = 75) | p-Value (T1 vs. T2DM2) | p-Value (DM vs. Control) |
|---|---|---|---|---|---|
| Age (years) | 61.0 ± 15.0 | 52.7 ± 18.0 | 64.6 ± 9.76 | 0.001 | 0.63 |
| Gender (male/female) | 13/24 | 13/15 | 37/38 | 0.698 | 0.06 |
| PDR (eyes) | NA | 19/28 | 40/75 | 0.015 | NA |
| DME (eyes) | NA | 14/28 | 30/75 | 0.295 | NA |
| DM duration (years) | NA | 25.3 ± 12.3 | 16.6 ± 8.12 | 0.011 | NA |
| HbA1C (mmol/L) | <6.5 | 8.07 ± 1.51 | 7.59 ± 1.73 | 0.307 | NA |
| Microalbuminuria (Y/N) | 0/31 | 13/28 | 12/75 | 0.002 | NA |
| Hypertension (patients n) | 11/31 | 20/28 | 75/75 | 0.007 | <0.001 |
| CRT (microns, eyes) | 270 ± 49.8 | 277 ± 95.9 | 362 ± 188 | 0.006 | 0.02 |
| CSI (microns, eyes) | 249 ± 109 | 245 ± 67.2 | 225 ± 80.9 | 0.23 | 0.09 |
| Alleles | A Allele (n) | G Allele (n) | p-Value |
|---|---|---|---|
| Control patients (n = 62) | 14 (22.5%) | 48 (77.5%) | 0.48 |
| DM patients (n = 206) | 58 (27.2%) | 148 (71.8%) | |
| Genotypes | AA | AG + GG | |
| Control patients (n = 31) | 3 (9.7%) | 28 (90.3%) | 0.99 |
| DM patients (n = 103) | 10 (9.7%) | 93 (90.3%) | |
| Genotypes | AA + AG | GG | |
| Control patients (n = 31) | 11 (35.5%) | 20 (64.5%) | 0.38 |
| DM patients (n = 103) | 48 (46.6%) | 55 (54.4%) |
| Alleles | An Allele (n) | G Allele (n) | p-Value |
|---|---|---|---|
| DM eyes without PDR (n = 234) | 73 (31.2%) | 161 (68.8%) | 0.14 |
| DM eyes with PDR (n = 178) | 43 (24.2%) | 135 (75.8%) | |
| DM eyes without DME (n = 224) | 50 (22.3%) | 174 (77.7%) | 0.006 |
| DM eyes with DME (n = 188) | 66 (35.1%) | 122 (64.9%) | |
| Genotypes | AA + AG | GG | |
| DM eyes without PDR (n = 117) | 60 (51.3%) | 57 (48.7%) | 0.16 |
| DM eyes with PDR (n = 89) | 36 (40.4%) | 53 (59.5%) | |
| DM eyes without DME (n = 112) | 43 (38.4%) | 69 (61.6%) | 0.01 |
| DM eyes with DME (n = 94) | 53 (56.38%) | 41 (43.61%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ecsedy, M.; Kovacs, I.; Szigeti, A.; Horvath, H.; Lenart, L.; Recsan, Z.; Medveczki, T.; Nagy, Z.Z.; Fekete, A. Association of SDF-1-3′ Gene A Variant with Diabetic Retinopathy in the Hungarian Population. Int. J. Mol. Sci. 2024, 25, 8036. https://doi.org/10.3390/ijms25158036
Ecsedy M, Kovacs I, Szigeti A, Horvath H, Lenart L, Recsan Z, Medveczki T, Nagy ZZ, Fekete A. Association of SDF-1-3′ Gene A Variant with Diabetic Retinopathy in the Hungarian Population. International Journal of Molecular Sciences. 2024; 25(15):8036. https://doi.org/10.3390/ijms25158036
Chicago/Turabian StyleEcsedy, Monika, Illes Kovacs, Andrea Szigeti, Hajnalka Horvath, Lilla Lenart, Zsuzsanna Recsan, Timea Medveczki, Zoltan Zsolt Nagy, and Andrea Fekete. 2024. "Association of SDF-1-3′ Gene A Variant with Diabetic Retinopathy in the Hungarian Population" International Journal of Molecular Sciences 25, no. 15: 8036. https://doi.org/10.3390/ijms25158036




