Humanized-Aquaporin-4-Expressing Rat Created by Gene-Editing Technology and Its Use to Clarify the Pathology of Neuromyelitis Optica Spectrum Disorder
Abstract
1. Introduction
2. Results
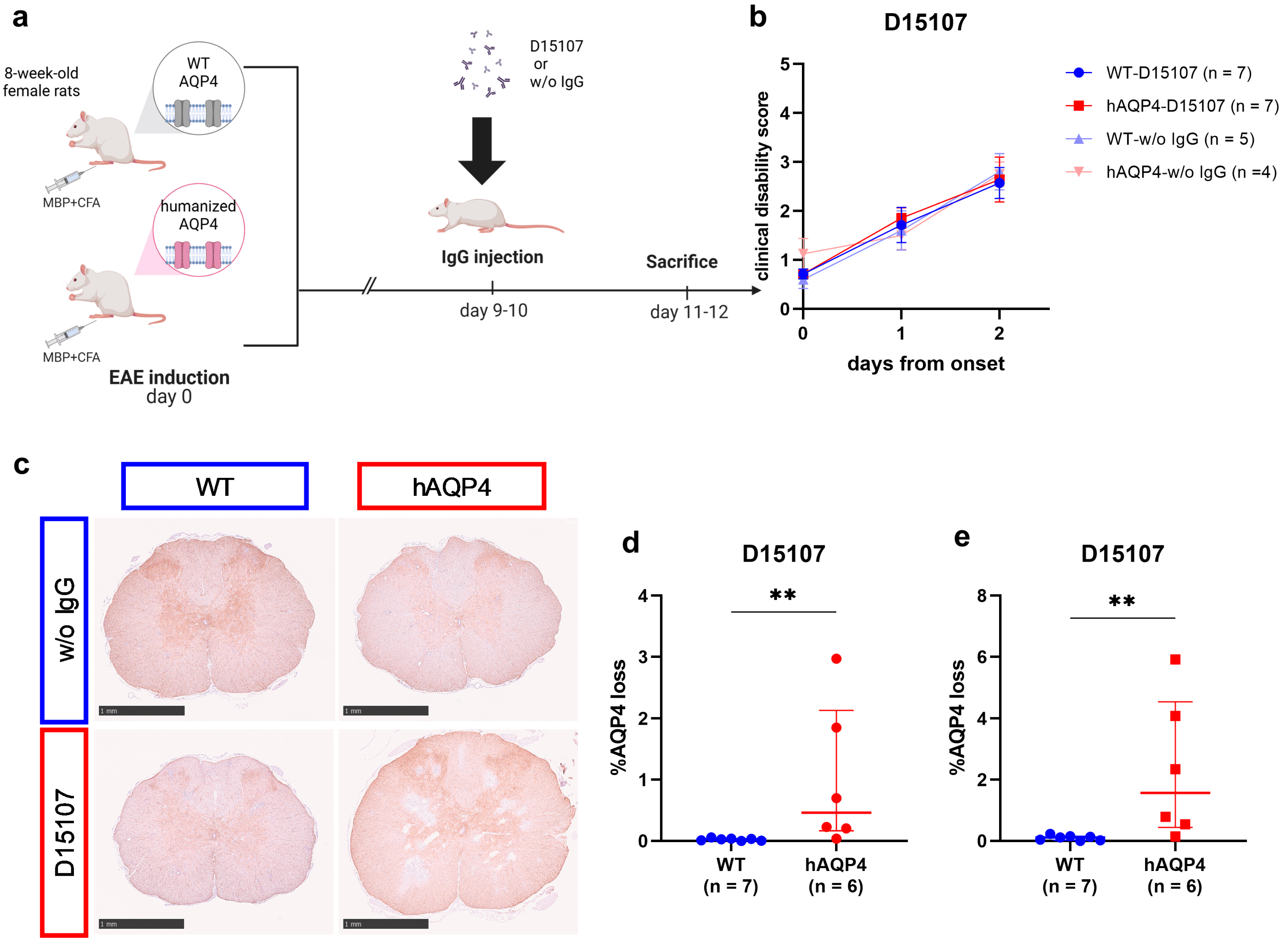
2.1. Human AQP4-Specific Antibody Induced Aastrocyte Injury in the CNS of hAQP4 Rats but Not in WT Rats
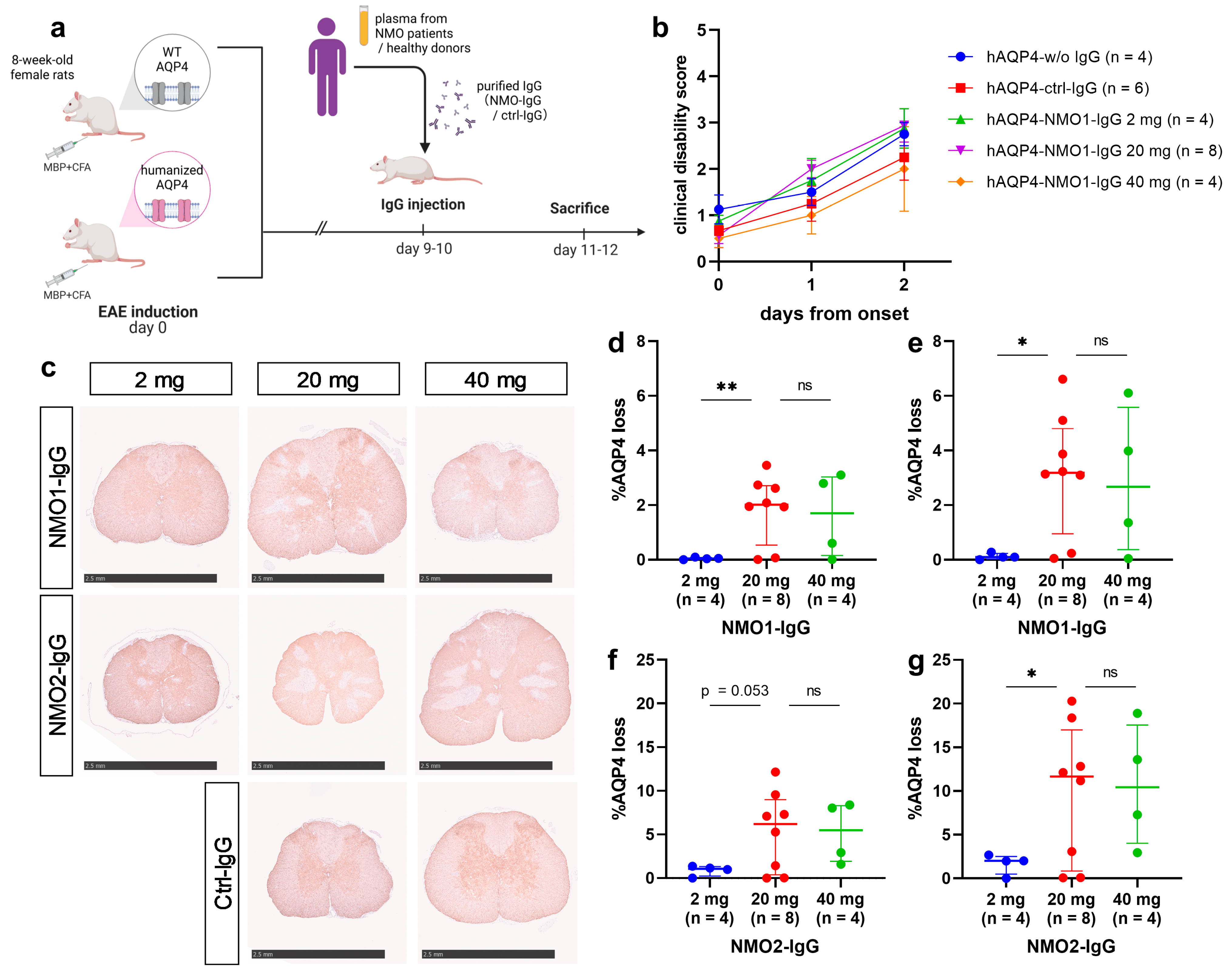
2.2. NMOSD Patient-Derived IgGs Induced Astrocyte Injury in the CNS of hAQP4 Rats and the Lesion Size Was Dose-Related
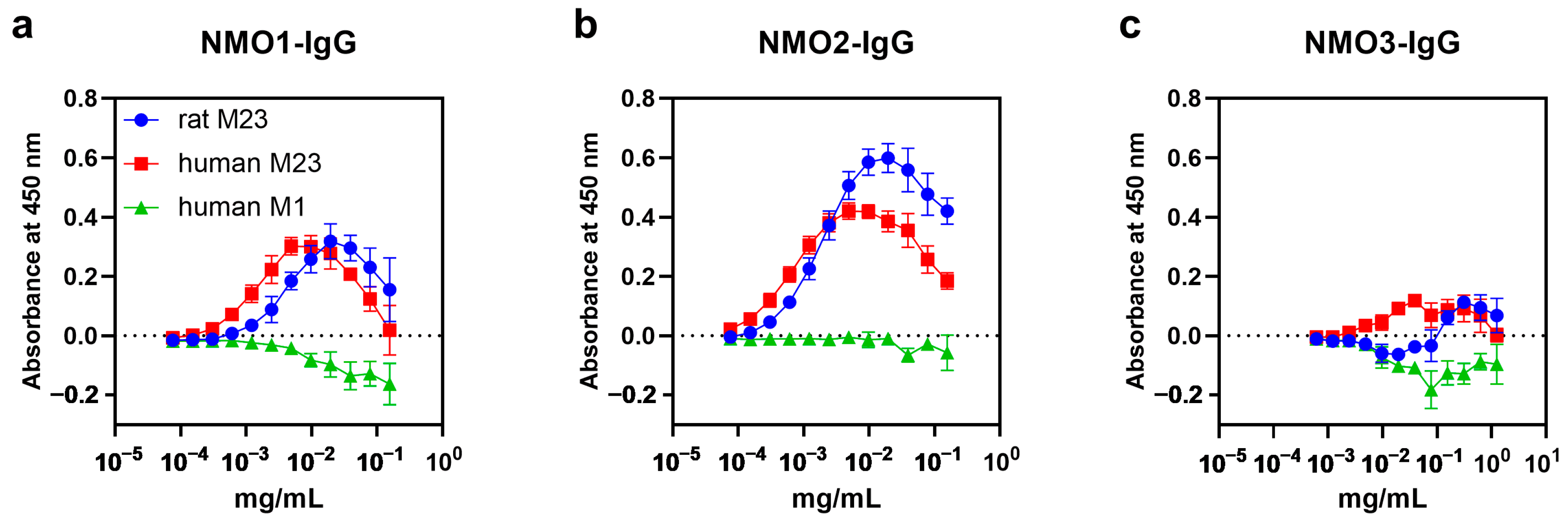
2.3. NMOSD Patient-Derived IgGs Induced AQP4 Loss Lesions in Both hAQP4 and Wild-Type Rats
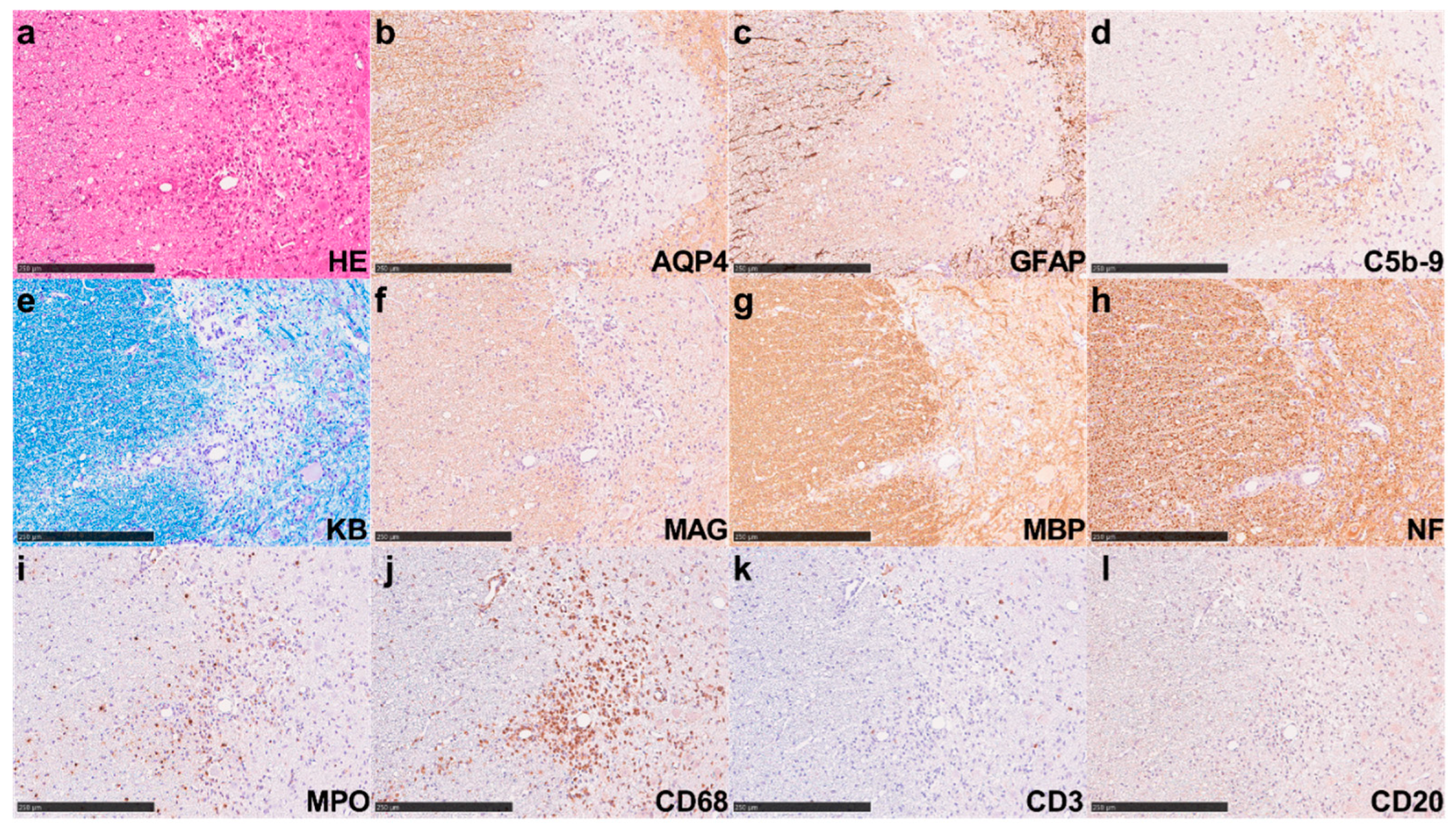
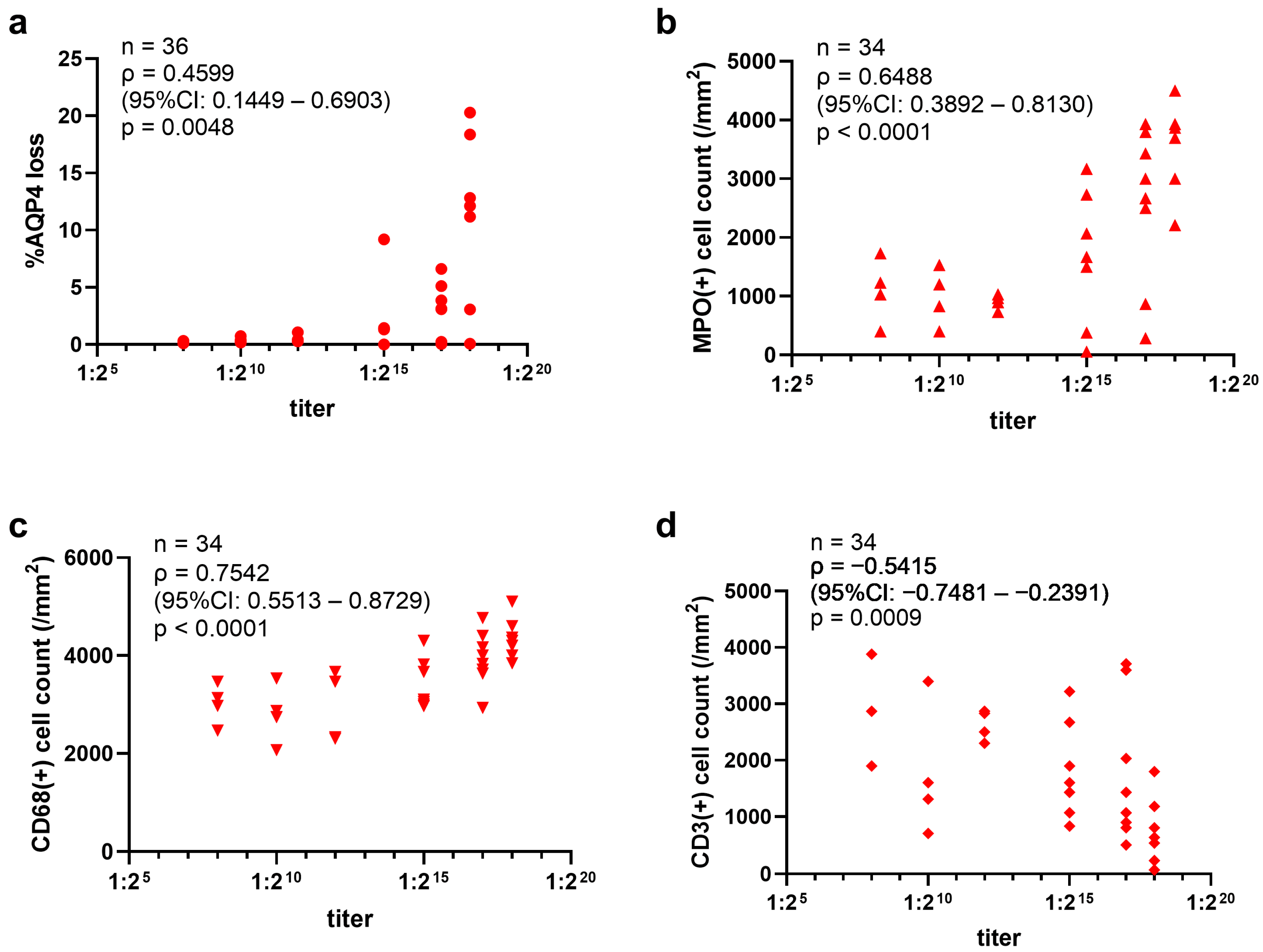
2.4. The Clinical Manifestations of the Patients during Acute Attacks Did Not Correlate with the Lesion Distribution of the Experimental NMOSD Model, Whereas the Anti-AQP4 Titers Correlated with the Lesion Size and Infiltrating Cells
3. Discussion
3.1. Establishment of a New NMOSD Model Using hAQP4 Rats
3.1.1. Reproduction of NMOSD-Like Pathology
3.1.2. Anti-AQP4 Titer and Lesion Formation
3.1.3. Lesion Distribution
3.2. Influence of Differences between Human and Rat AQP4 ECDs on the NMOSD Model
3.3. Limitations
4. Materials and Methods
4.1. Establishment of Humanized-AQP4-Expressing Rats
4.1.1. Plasmid Constructions
4.1.2. Cell Culture and Transfection
4.1.3. ELISA
4.1.4. Animals
4.1.5. Preparation of CRISPR Components and Long Single-Stranded Donor DNAs
4.1.6. Manipulation of Rat Embryos and Electroporation
4.2. Experimental NMOSD Model
4.2.1. Animals
4.2.2. Patients and Antibodies
4.2.3. Induction of Experimental NMOSD
4.2.4. Histology and Immunohistochemistry
4.2.5. Histopathological Analyses
4.2.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wingerchuk, D.M.; Lucchinetti, C.F. Neuromyelitis Optica Spectrum Disorder. N. Engl. J. Med. 2022, 387, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Jiao, Y.; Fryer, J.P.; Lennon, V.A.; Jenkins, S.M.; Quek, A.M.; Smith, C.Y.; McKeon, A.; Costanzi, C.; Iorio, R.; Weinshenker, B.G.; et al. Updated estimate of AQP4-IgG serostatus and disability outcome in neuromyelitis optica. Neurology 2013, 81, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Kleiter, I.; Gahlen, A.; Borisow, N.; Fischer, K.; Wernecke, K.D.; Wegner, B.; Hellwig, K.; Pache, F.; Ruprecht, K.; Havla, J.; et al. Neuromyelitis optica: Evaluation of 871 attacks and 1,153 treatment courses. Ann. Neurol. 2016, 79, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Chihara, N.; Yamamura, T. Immuno-Pathogenesis of Neuromyelitis Optica and Emerging Therapies. In Seminars in Immunopathology; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Preziosa, P.; Amato, M.P.; Battistini, L.; Capobianco, M.; Centonze, D.; Cocco, E.; Conte, A.; Gasperini, C.; Gastaldi, M.; Tortorella, C.; et al. Moving towards a new era for the treatment of neuromyelitis optica spectrum disorders. J. Neurol. 2024, 271, 3879–3896. [Google Scholar] [CrossRef]
- Lennon, V.A.; Kryzer, T.J.; Pittock, S.J.; Verkman, A.S.; Hinson, S.R. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J. Exp. Med. 2005, 202, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Bradl, M.; Misu, T.; Takahashi, T.; Watanabe, M.; Mader, S.; Reindl, M.; Adzemovic, M.; Bauer, J.; Berger, T.; Fujihara, K.; et al. Neuromyelitis optica: Pathogenicity of patient immunoglobulin in vivo. Ann. Neurol. 2009, 66, 630–643. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, M.; Nakatsuji, Y.; Kimura, T.; Moriya, M.; Takata, K.; Okuno, T.; Kumanogoh, A.; Kajiyama, K.; Yoshikawa, H.; Sakoda, S. Neuromyelitis optica: Passive transfer to rats by human immunoglobulin. Biochem. Biophys. Res. Commun. 2009, 386, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.L.; Lam, C.; Kalluri, S.R.; Saikali, P.; Bautista, K.; Dupree, C.; Glogowska, M.; Case, D.; Antel, J.P.; Owens, G.P.; et al. Intrathecal pathogenic anti-aquaporin-4 antibodies in early neuromyelitis optica. Ann. Neurol. 2009, 66, 617–629. [Google Scholar] [CrossRef]
- Duan, T.; Verkman, A.S. Experimental animal models of aquaporin-4-IgG-seropositive neuromyelitis optica spectrum disorders: Progress and shortcomings. Brain Pathol. 2020, 30, 13–25. [Google Scholar] [CrossRef]
- Asavapanumas, N.; Ratelade, J.; Verkman, A.S. Unique neuromyelitis optica pathology produced in naive rats by intracerebral administration of NMO-IgG. Acta Neuropathol. 2014, 127, 539–551. [Google Scholar] [CrossRef]
- Asavapanumas, N.; Verkman, A.S. Neuromyelitis optica pathology in rats following intraperitoneal injection of NMO-IgG and intracerebral needle injury. Acta Neuropathol. Commun. 2014, 2, 48. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Adams, M.S.; Jones, P.D.; Diederich, C.J.; Verkman, A.S. Noninvasive, Targeted Creation of Neuromyelitis Optica Pathology in AQP4-IgG Seropositive Rats by Pulsed Focused Ultrasound. J. Neuropathol. Exp. Neurol. 2019, 78, 47–56. [Google Scholar] [CrossRef]
- Geis, C.; Ritter, C.; Ruschil, C.; Weishaupt, A.; Grunewald, B.; Stoll, G.; Holmoy, T.; Misu, T.; Fujihara, K.; Hemmer, B.; et al. The intrinsic pathogenic role of autoantibodies to aquaporin 4 mediating spinal cord disease in a rat passive-transfer model. Exp. Neurol. 2015, 265, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, H.; Ma, T.; Skach, W.; Matthay, M.A.; Verkman, A.S. Molecular cloning of a mercurial-insensitive water channel expressed in selected water-transporting tissues. J. Biol. Chem. 1994, 269, 5497–5500. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.S.; Bhat, R.V.; Preston, G.M.; Guggino, W.B.; Baraban, J.M.; Agre, P. Molecular characterization of an aquaporin cDNA from brain: Candidate osmoreceptor and regulator of water balance. Proc. Natl. Acad. Sci. USA 1994, 91, 13052–13056. [Google Scholar] [CrossRef]
- Frigeri, A.; Gropper, M.A.; Turck, C.W.; Verkman, A.S. Immunolocalization of the mercurial-insensitive water channel and glycerol intrinsic protein in epithelial cell plasma membranes. Proc. Natl. Acad. Sci. USA 1995, 92, 4328–4331. [Google Scholar] [CrossRef]
- Nagelhus, E.A.; Veruki, M.L.; Torp, R.; Haug, F.M.; Laake, J.H.; Nielsen, S.; Agre, P.; Ottersen, O.P. Aquaporin-4 water channel protein in the rat retina and optic nerve: Polarized expression in Müller cells and fibrous astrocytes. J. Neurosci. 1998, 18, 2506–2519. [Google Scholar] [CrossRef]
- Nielsen, S.; Nagelhus, E.A.; Amiry-Moghaddam, M.; Bourque, C.; Agre, P.; Ottersen, O.P. Specialized membrane domains for water transport in glial cells: High-resolution immunogold cytochemistry of aquaporin-4 in rat brain. J. Neurosci. 1997, 17, 171–180. [Google Scholar] [CrossRef]
- Yang, B.; Ma, T.; Verkman, A.S. cDNA cloning, gene organization, and chromosomal localization of a human mercurial insensitive water channel. Evidence for distinct transcriptional units. J. Biol. Chem. 1995, 270, 22907–22913. [Google Scholar] [CrossRef]
- Lu, M.; Lee, M.D.; Smith, B.L.; Jung, J.S.; Agre, P.; Verdijk, M.A.; Merkx, G.; Rijss, J.P.; Deen, P.M. The human AQP4 gene: Definition of the locus encoding two water channel polypeptides in brain. Proc. Natl. Acad. Sci. USA 1996, 93, 10908–10912. [Google Scholar] [CrossRef]
- Turtzo, L.C.; Lee, M.D.; Lu, M.; Smith, B.L.; Copeland, N.G.; Gilbert, D.J.; Jenkins, N.A.; Agre, P. Cloning and chromosomal localization of mouse aquaporin 4: Exclusion of a candidate mutant phenotype, ataxia. Genomics 1997, 41, 267–270. [Google Scholar] [CrossRef]
- Yang, B.; Brown, D.; Verkman, A.S. The mercurial insensitive water channel (AQP-4) forms orthogonal arrays in stably transfected Chinese hamster ovary cells. J. Biol. Chem. 1996, 271, 4577–4580. [Google Scholar] [CrossRef]
- Verbavatz, J.-M.; Ma, T.; Gobin, R.; Verkman, A.S. Absence of orthogonal arrays in kidney, brain and muscle from transgenic knockout mice lacking water channel aquaporin-4. J. Cell Sci. 1997, 110, 2855–2860. [Google Scholar] [CrossRef]
- Rash, J.E.; Yasumura, T.; Hudson, C.S.; Agre, P.; Nielsen, S. Direct immunogold labeling of aquaporin-4 in square arrays of astrocyte and ependymocyte plasma membranes in rat brain and spinal cord. Proc. Natl. Acad. Sci. USA 1998, 95, 11981–11986. [Google Scholar] [CrossRef]
- Furman, C.S.; Gorelick-Feldman, D.A.; Davidson, K.G.; Yasumura, T.; Neely, J.D.; Agre, P.; Rash, J.E. Aquaporin-4 square array assembly: Opposing actions of M1 and M23 isoforms. Proc. Natl. Acad. Sci. USA 2003, 100, 13609–13614. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, C.; Bouley, R.; Huang, Y.; Fang, P.; Pastor-Soler, N.; Brown, D.; Van Hoek, A.N. Membrane organization and function of M1 and M23 isoforms of aquaporin-4 in epithelial cells. Am. J. Physiol. Renal Physiol. 2004, 287, F501–F511. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Fujihara, K.; Nakashima, I.; Misu, T.; Miyazawa, I.; Nakamura, M.; Watanabe, S.; Ishii, N.; Itoyama, Y. Establishment of a new sensitive assay for anti-human aquaporin-4 antibody in neuromyelitis optica. Tohoku J. Exp. Med. 2006, 210, 307–313. [Google Scholar] [CrossRef][Green Version]
- Hinson, S.R.; Pittock, S.J.; Lucchinetti, C.F.; Roemer, S.F.; Fryer, J.P.; Kryzer, T.J.; Lennon, V.A. Pathogenic potential of IgG binding to water channel extracellular domain in neuromyelitis optica. Neurology 2007, 69, 2221–2231. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Bazzi, S.A.; Schmitz, F.; Tanno, H.; McDaniel, J.R.; Lee, C.H.; Joshi, C.; Kim, J.E.; Monson, N.; Greenberg, B.M.; et al. Molecular Level Characterization of Circulating Aquaporin-4 Antibodies in Neuromyelitis Optica Spectrum Disorder. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1034. [Google Scholar] [CrossRef]
- Tani, T.; Sakimura, K.; Tsujita, M.; Nakada, T.; Tanaka, M.; Nishizawa, M.; Tanaka, K. Identification of binding sites for anti-aquaporin 4 antibodies in patients with neuromyelitis optica. J. Neuroimmunol. 2009, 211, 110–113. [Google Scholar] [CrossRef]
- Owens, G.P.; Ritchie, A.; Rossi, A.; Schaller, K.; Wemlinger, S.; Schumann, H.; Shearer, A.; Verkman, A.S.; Bennett, J.L. Mutagenesis of the aquaporin 4 extracellular domains defines restricted binding patterns of pathogenic neuromyelitis optica IgG. J. Biol. Chem. 2015, 290, 12123–12134. [Google Scholar] [CrossRef] [PubMed]
- Tuller, F.; Holzer, H.; Schanda, K.; Aboulenein-Djamshidian, F.; Hoftberger, R.; Khalil, M.; Seifert-Held, T.; Leutmezer, F.; Berger, T.; Reindl, M. Characterization of the binding pattern of human aquaporin-4 autoantibodies in patients with neuromyelitis optica spectrum disorders. J. Neuroinflamm. 2016, 13, 176. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, K.; Abe, Y.; Iwanari, H.; Suzuki, Y.; Kikuchi, T.; Ito, T.; Kato, J.; Kusano-Arai, O.; Takahashi, T.; Nishiyama, S.; et al. Establishment of monoclonal antibodies against the extracellular domain that block binding of NMO-IgG to AQP4. J. Neuroimmunol. 2013, 260, 107–116. [Google Scholar] [CrossRef]
- Kurosawa, K.; Misu, T.; Takai, Y.; Sato, D.K.; Takahashi, T.; Abe, Y.; Iwanari, H.; Ogawa, R.; Nakashima, I.; Fujihara, K.; et al. Severely exacerbated neuromyelitis optica rat model with extensive astrocytopathy by high affinity anti-aquaporin-4 monoclonal antibody. Acta Neuropathol. Commun. 2015, 3, 82. [Google Scholar] [CrossRef] [PubMed]
- Misu, T.; Höftberger, R.; Fujihara, K.; Wimmer, I.; Takai, Y.; Nishiyama, S.; Nakashima, I.; Konno, H.; Bradl, M.; Garzuly, F.; et al. Presence of six different lesion types suggests diverse mechanisms of tissue injury in neuromyelitis optica. Acta Neuropathol. 2013, 125, 815–827. [Google Scholar] [CrossRef]
- Takai, Y.; Misu, T.; Suzuki, H.; Takahashi, T.; Okada, H.; Tanaka, S.; Okita, K.; Sasou, S.; Watanabe, M.; Namatame, C.; et al. Staging of astrocytopathy and complement activation in neuromyelitis optica spectrum disorders. Brain 2021, 144, 2401–2415. [Google Scholar] [CrossRef]
- Lucchinetti, C.F.; Mandler, R.N.; McGavern, D.; Bruck, W.; Gleich, G.; Ransohoff, R.M.; Trebst, C.; Weinshenker, B.; Wingerchuk, D.; Parisi, J.E.; et al. A role for humoral mechanisms in the pathogenesis of Devic’s neuromyelitis optica. Brain 2002, 125 Pt 7, 1450–1461. [Google Scholar] [CrossRef] [PubMed]
- Chai, A.C.; Cui, M.; Chemello, F.; Li, H.; Chen, K.; Tan, W.; Atmanli, A.; McAnally, J.R.; Zhang, Y.; Xu, L.; et al. Base editing correction of hypertrophic cardiomyopathy in human cardiomyocytes and humanized mice. Nat. Med. 2023, 29, 401–411. [Google Scholar] [CrossRef]
- Lebek, S.; Caravia, X.M.; Straub, L.G.; Alzhanov, D.; Tan, W.; Li, H.; McAnally, J.R.; Chen, K.; Xu, L.; Scherer, P.E.; et al. CRISPR-Cas9 base editing of pathogenic CaMKIIδ improves cardiac function in a humanized mouse model. J. Clin. Investig. 2024, 134, e175164. [Google Scholar] [CrossRef]
- Ratelade, J.; Verkman, A.S. Inhibitor(s) of the classical complement pathway in mouse serum limit the utility of mice as experimental models of neuromyelitis optica. Mol. Immunol. 2014, 62, 104–113. [Google Scholar] [CrossRef]
- Rodin, R.E.; Chitnis, T. Soluble biomarkers for Neuromyelitis Optica Spectrum Disorders: A mini review. Front. Neurol. 2024, 15, 1415535. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Fujihara, K.; Nakashima, I.; Misu, T.; Miyazawa, I.; Nakamura, M.; Watanabe, S.; Shiga, Y.; Kanaoka, C.; Fujimori, J.; et al. Anti-aquaporin-4 antibody is involved in the pathogenesis of NMO: A study on antibody titre. Brain 2007, 130 Pt 5, 1235–1243. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Tan, G.; Li, B.; Zhang, J.; Gao, Y.; Cao, Y.; Jia, Z.; Sugimoto, K. Serum Aquaporin 4-Immunoglobulin G Titer and Neuromyelitis Optica Spectrum Disorder Activity and Severity: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 746959. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Kokubun, N.; Aoki, R.; Hamaguchi, M.; Matsuda, H.; Suzuki, K. Possible role of neutrophils in astrocyte injury in neuromyelitis optica spectrum disorder. J. Neurol. Sci. 2022, 438, 120293. [Google Scholar] [CrossRef] [PubMed]
- Duan, T.; Smith, A.J.; Verkman, A.S. Complement-independent bystander injury in AQP4-IgG seropositive neuromyelitis optica produced by antibody-dependent cellular cytotoxicity. Acta Neuropathol. Commun. 2019, 7, 112. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, S.; Waters, P.; MacDonald, C.; Bell, B.A.; Vincent, A.; Verkman, A.S.; Papadopoulos, M.C. Neutrophil protease inhibition reduces neuromyelitis optica-immunoglobulin G-induced damage in mouse brain. Ann. Neurol. 2012, 71, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Murata, H.; Kinoshita, M.; Yasumizu, Y.; Motooka, D.; Beppu, S.; Shiraishi, N.; Sugiyama, Y.; Kihara, K.; Tada, S.; Koda, T.; et al. Cell-Free DNA Derived From Neutrophils Triggers Type 1 Interferon Signature in Neuromyelitis Optica Spectrum Disorder. Neurol. Neuroimmunol. Neuroinflamm. 2022, 9, e1149. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, S.; Waters, P.; Macdonald, C.; Bridges, L.R.; Bell, B.A.; Vincent, A.; Verkman, A.S.; Papadopoulos, M.C. T cell deficiency does not reduce lesions in mice produced by intracerebral injection of NMO-IgG and complement. J. Neuroimmunol. 2011, 235, 27–32. [Google Scholar] [CrossRef]
- Bradl, M.; Reindl, M.; Lassmann, H. Mechanisms for lesion localization in neuromyelitis optica spectrum disorders. Curr. Opin. Neurol. 2018, 31, 325–333. [Google Scholar] [CrossRef]
- Lindner, M.; Klotz, L.; Wiendl, H. Mechanisms underlying lesion development and lesion distribution in CNS autoimmunity. J. Neurochem. 2018, 146, 122–132. [Google Scholar] [CrossRef]
- Zeka, B.; Hastermann, M.; Hochmeister, S.; Kogl, N.; Kaufmann, N.; Schanda, K.; Mader, S.; Misu, T.; Rommer, P.; Fujihara, K.; et al. Highly encephalitogenic aquaporin 4-specific T cells and NMO-IgG jointly orchestrate lesion location and tissue damage in the CNS. Acta Neuropathol. 2015, 130, 783–798. [Google Scholar] [CrossRef] [PubMed]
- Itoyama, Y.; Webster, H.D. Immunocytochemical study of myelin-associated glycoprotein (MAG) and basic protein (BP) in acute experimental allergic encephalomyelitis (EAE). J. Neuroimmunol. 1982, 3, 351–364. [Google Scholar] [CrossRef] [PubMed]
- Karlik, S.J.; Munoz, D.; St. Louis, J.; Strejan, G. Correlation between MRI and clinico-pathological manifestations in Lewis rats protected from experimental allergic encephalomyelitis by acylated synthetic peptide of myelin basic protein. Magn. Reson. Imaging 1999, 17, 731–737. [Google Scholar] [CrossRef]
- Duan, T.; Tradtrantip, L.; Phuan, P.W.; Bennett, J.L.; Verkman, A.S. Affinity-matured ‘aquaporumab’ anti-aquaporin-4 antibody for therapy of seropositive neuromyelitis optica spectrum disorders. Neuropharmacology 2020, 162, 107827. [Google Scholar] [CrossRef]
- Phuan, P.W.; Ratelade, J.; Rossi, A.; Tradtrantip, L.; Verkman, A.S. Complement-dependent cytotoxicity in neuromyelitis optica requires aquaporin-4 protein assembly in orthogonal arrays. J. Biol. Chem. 2012, 287, 13829–13839. [Google Scholar] [CrossRef]
- Soltys, J.; Liu, Y.; Ritchie, A.; Wemlinger, S.; Schaller, K.; Schumann, H.; Owens, G.P.; Bennett, J.L. Membrane assembly of aquaporin-4 autoantibodies regulates classical complement activation in neuromyelitis optica. J. Clin. Investig. 2019, 129, 2000–2013. [Google Scholar] [CrossRef]
- Tradtrantip, L.; Yeaman, M.R.; Verkman, A.S. Cytoprotective IgG antibodies in sera from a subset of patients with AQP4-IgG seropositive neuromyelitis optica spectrum disorder. Sci. Rep. 2021, 11, 21962. [Google Scholar] [CrossRef]
- Matsuya, N.; Komori, M.; Nomura, K.; Nakane, S.; Fukudome, T.; Goto, H.; Shiraishi, H.; Wandinger, K.P.; Matsuo, H.; Kondo, T. Increased T-cell immunity against aquaporin-4 and proteolipid protein in neuromyelitis optica. Int. Immunol. 2011, 23, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Serizawa, K.; Miyake, S.; Katsura, Y.; Yorozu, K.; Kurasawa, M.; Tomizawa-Shinohara, H.; Yasuno, H.; Matsumoto, Y. Intradermal AQP4 peptide immunization induces clinical features of neuromyelitis optica spectrum disorder in mice. J. Neuroimmunol. 2023, 380, 578109. [Google Scholar] [CrossRef]
- Morita, Y.; Itokazu, T.; Nakanishi, T.; Hiraga, S.I.; Yamashita, T. A novel aquaporin-4-associated optic neuritis rat model with severe pathological and functional manifestations. J. Neuroinflamm. 2022, 19, 263. [Google Scholar] [CrossRef]
- Miyazaki-Komine, K.; Takai, Y.; Huang, P.; Kusano-Arai, O.; Iwanari, H.; Misu, T.; Koda, K.; Mitomo, K.; Sakihama, T.; Toyama, Y.; et al. High avidity chimeric monoclonal antibodies against the extracellular domains of human aquaporin-4 competing with the neuromyelitis optica autoantibody, NMO-IgG. Br. J. Pharmacol. 2016, 173, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Concordet, J.-P.; Haeussler, M. CRISPOR: Intuitive guide selection for CRISPR/Cas9 genome editing experiments and screens. Nucleic Acids Res. 2018, 46, W242–W245. [Google Scholar] [CrossRef] [PubMed]
- Yoshimi, K.; Kunihiro, Y.; Kaneko, T.; Nagahora, H.; Voigt, B.; Mashimo, T. ssODN-mediated knock-in with CRISPR-Cas for large genomic regions in zygotes. Nat. Commun. 2016, 7, 10431. [Google Scholar] [CrossRef]
- Miyasaka, Y.; Uno, Y.; Yoshimi, K.; Kunihiro, Y.; Yoshimura, T.; Tanaka, T.; Ishikubo, H.; Hiraoka, Y.; Takemoto, N.; Tanaka, T.; et al. CLICK: One-step generation of conditional knockout mice. BMC Genom. 2018, 19, 318. [Google Scholar] [CrossRef] [PubMed]
- Wingerchuk, D.M.; Banwell, B.; Bennett, J.L.; Cabre, P.; Carroll, W.; Chitnis, T.; de Seze, J.; Fujihara, K.; Greenberg, B.; Jacob, A.; et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015, 85, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Fishman, J.B.; Berg, E.A. Preparation of Antibody Using Caprylic Acid. Cold Spring Harb. Protoc. 2018, 2018, pdb-prot099127. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]

| Patient | NMO1 | NMO2 | NMO3 | NMO4 | NMO5 | NMO6 |
|---|---|---|---|---|---|---|
| Age | 64 | 62 | 52 | 28 | 49 | 59 |
| Sex | F | F | F | F | F | M |
| Clinical phenotype | C | ON | ON | ON + C | APS + My | ON + APS + My |
| Relapse or first attack | Relapse | Relapse | Relapse | First attack | First attack | First attack |
| EDSS on nadir | 7.5 | 6 | 5 | 4 | 5 | 5 |
| EDSS after treatment | 6 | 5 | 5 | 1.5 | 2.5 | 3 |
| Anti-AQP4 titer of serum at attack | 1:524,288 | 1:32,768 | 1:131,072 | 1:4096 | 1:1024 | 1:1024 |
| Anti-AQP4 titer of purified-IgG | 1:131,072 | 1:262,144 | 1:32,768 | 1:4096 | 1:1024 | 1:256 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Namatame, C.; Abe, Y.; Miyasaka, Y.; Takai, Y.; Matsumoto, Y.; Takahashi, T.; Mashimo, T.; Misu, T.; Fujihara, K.; Yasui, M.; et al. Humanized-Aquaporin-4-Expressing Rat Created by Gene-Editing Technology and Its Use to Clarify the Pathology of Neuromyelitis Optica Spectrum Disorder. Int. J. Mol. Sci. 2024, 25, 8169. https://doi.org/10.3390/ijms25158169
Namatame C, Abe Y, Miyasaka Y, Takai Y, Matsumoto Y, Takahashi T, Mashimo T, Misu T, Fujihara K, Yasui M, et al. Humanized-Aquaporin-4-Expressing Rat Created by Gene-Editing Technology and Its Use to Clarify the Pathology of Neuromyelitis Optica Spectrum Disorder. International Journal of Molecular Sciences. 2024; 25(15):8169. https://doi.org/10.3390/ijms25158169
Chicago/Turabian StyleNamatame, Chihiro, Yoichiro Abe, Yoshiki Miyasaka, Yoshiki Takai, Yuki Matsumoto, Toshiyuki Takahashi, Tomoji Mashimo, Tatsuro Misu, Kazuo Fujihara, Masato Yasui, and et al. 2024. "Humanized-Aquaporin-4-Expressing Rat Created by Gene-Editing Technology and Its Use to Clarify the Pathology of Neuromyelitis Optica Spectrum Disorder" International Journal of Molecular Sciences 25, no. 15: 8169. https://doi.org/10.3390/ijms25158169
APA StyleNamatame, C., Abe, Y., Miyasaka, Y., Takai, Y., Matsumoto, Y., Takahashi, T., Mashimo, T., Misu, T., Fujihara, K., Yasui, M., & Aoki, M. (2024). Humanized-Aquaporin-4-Expressing Rat Created by Gene-Editing Technology and Its Use to Clarify the Pathology of Neuromyelitis Optica Spectrum Disorder. International Journal of Molecular Sciences, 25(15), 8169. https://doi.org/10.3390/ijms25158169







