The Role of MicroRNAs in Progressive Supranuclear Palsy—A Systematic Review
Abstract
1. Introduction
1.1. Progressive Nuclear Palsy Diagnostic Criteria
1.2. Epidemiology
1.3. Problems in Clinical Practice
1.4. MicroRNAs as Novel Biomarkers
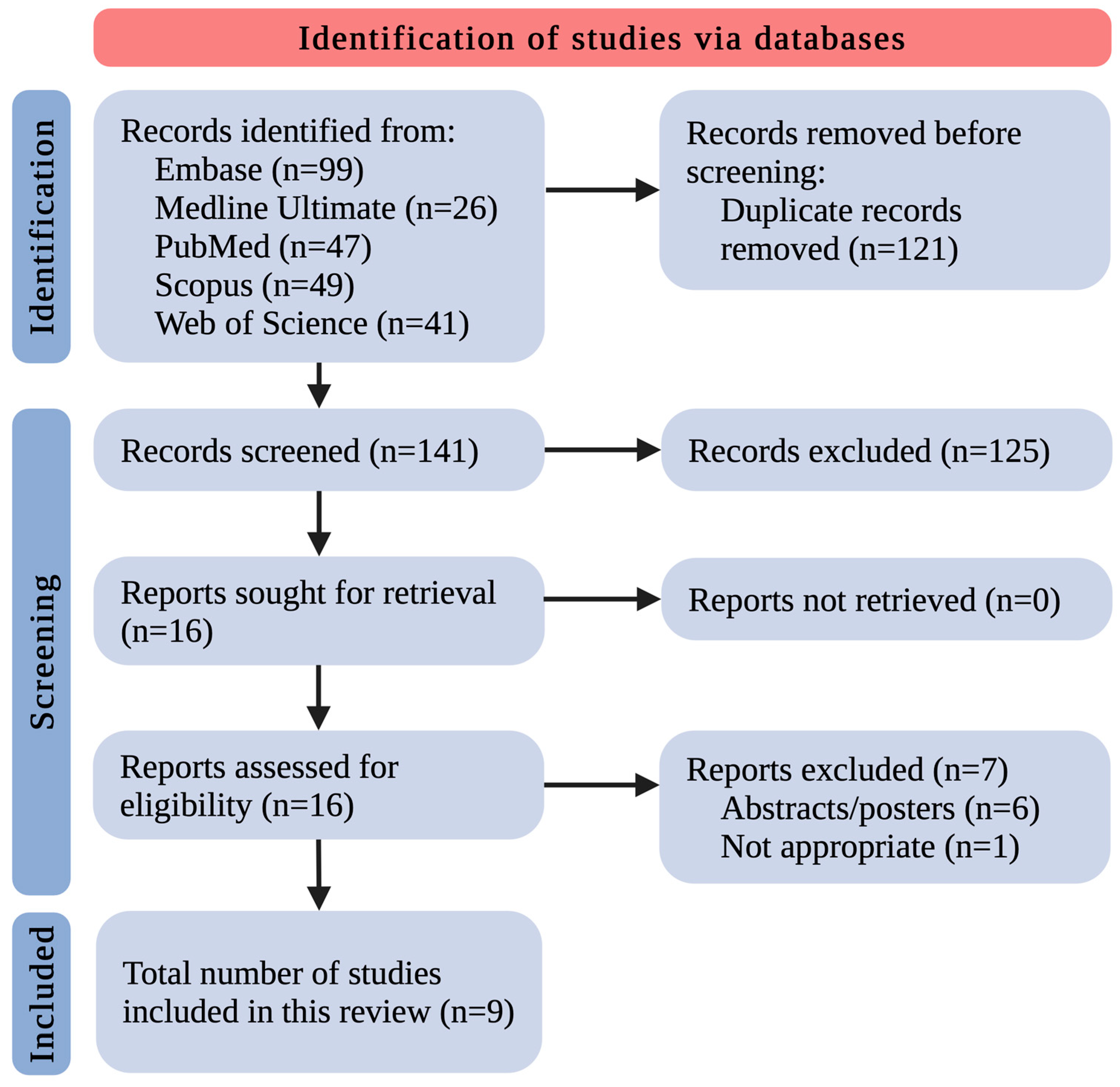
2. Methods
3. Results and Discussion
3.1. miRNA Changes in a Progressive Supranuclear Palsy Animal Model
3.2. miRNA Changes in Human Brain Tissues of Progressive Supranuclear Palsy Patients
3.3. miRNA Changes in the Body Fluids (Cerebrospinal Fluid, Blood/Serum/Plasma) of Progressive Supranuclear Patients
4. Discussion
5. Conclusions and Future Perspectives
6. Limitations
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bhatia, K.P.; Stamelou, M. Nonmotor Features in Atypical Parkinsonism. Int. Rev. Neurobiol. 2017, 134, 1285–1301. [Google Scholar] [CrossRef]
- Levin, J.; Kurz, A.; Arzberger, T.; Giese, A.; Höglinger, G.U. The Differential Diagnosis and Treatment of Atypical Parkinsonism. Dtsch Arztebl. Int. 2016, 113, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Litvan, I.; Agid, Y.; Calne, D.; Campbell, G.; Dubois, B.; Duvoisin, R.C.; Goetz, C.G.; Golbe, L.I.; Grafman, J.; Growdon, J.H.; et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): Report of the NINDS-SPSP international workshop. Neurology 1996, 47, 1–9. [Google Scholar] [CrossRef]
- Kawashima, M.; Miyake, M.; Kusumi, M.; Adachi, Y.; Nakashima, K. Prevalence of progressive supranuclear palsy in Yonago, Japan. Mov. Disord. 2004, 19, 1239–1240. [Google Scholar] [CrossRef] [PubMed]
- McFarland, N.R. Diagnostic Approach to Atypical Parkinsonian Syndromes. Continuum 2016, 22, 1117–1142. [Google Scholar] [CrossRef]
- Höglinger, G.U.; Respondek, G.; Stamelou, M.; Kurz, C.; Josephs, K.A.; Lang, A.E.; Mollenhauer, B.; Müller, U.; Nilsson, C.; Whitwell, J.L.; et al. Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov. Disord. 2017, 32, 853–864. [Google Scholar] [CrossRef]
- Kato, N.; Arai, K.; Hattori, T. Study of the rostral midbrain atrophy in progressive supranuclear palsy. J. Neurol. Sci. 2003, 210, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; de Silva, R.; Paviour, D.C.; Pittman, A.; Watt, H.C.; Kilford, L.; Holton, J.L.; Revesz, T.; Lees, A.J. Characteristics of two distinct clinical phenotypes in pathologically proven progressive supranuclear palsy: Richardson’s syndrome and PSP-parkinsonism. Brain 2005, 128, 1247–1258. [Google Scholar] [CrossRef]
- Respondek, G.; Stamelou, M.; Kurz, C.; Ferguson, L.W.; Rajput, A.; Chiu, W.Z.; van Swieten, J.C.; Troakes, C.; Al Sarraj, S.; Gelpi, E.; et al. The phenotypic spectrum of progressive supranuclear palsy: A retrospective multicenter study of 100 definite cases. Mov. Disord. 2014, 29, 1758–1766. [Google Scholar] [CrossRef]
- Birdi, S.; Rajput, A.H.; Fenton, M.; Donat, J.R.; Rozdilsky, B.; Robinson, C.; Macaulay, R.; George, D. Progressive supranuclear palsy diagnosis and confounding features: Report on 16 autopsied cases. Mov. Disord. 2002, 17, 1255–1264. [Google Scholar] [CrossRef]
- Tsuboi, Y.; Josephs, K.A.; Boeve, B.F.; Litvan, I.; Caselli, R.J.; Caviness, J.N.; Uitti, R.J.; Bott, A.D.; Dickson, D.W. Increased tau burden in the cortices of progressive supranuclear palsy presenting with corticobasal syndrome. Mov. Disord. 2005, 20, 982–988. [Google Scholar] [CrossRef] [PubMed]
- Boeve, B.; Dickson, D.; Duffy, J.; Bartleson, J.; Trenerry, M.; Petersen, R. Progressive nonfluent aphasia and subsequent aphasic dementia associated with atypical progressive supranuclear palsy pathology. Eur. Neurol. 2003, 49, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Pan, P.; Liu, Y.; Zhang, Y.; Zhao, H.; Ye, X.; Xu, Y. Brain gray matter abnormalities in progressive supranuclear palsy revisited. Oncotarget 2017, 8, 80941–80955. [Google Scholar] [CrossRef]
- Koziorowski, D.; Figura, M.; Milanowski, Ł.M.; Szlufik, S.; Alster, P.; Madetko, N.; Friedman, A. Mechanisms of Neurodegeneration in Various Forms of Parkinsonism—Similarities and Differences. Cells 2021, 10, 656. [Google Scholar] [CrossRef]
- Barer, Y.; Chodick, G.; Cohen, R.; Grabarnik-John, M.; Ye, X.; Zamudio, J.; Gurevich, T. Epidemiology of Progressive Supranuclear Palsy: Real World Data from the Second Largest Health Plan in Israel. Brain Sci. 2022, 12, 1126. [Google Scholar] [CrossRef] [PubMed]
- Viscidi, E.; Litvan, I.; Dam, T.; Juneja, M.; Li, L.; Krzywy, H.; Eaton, S.; Hall, S.; Kupferman, J.; Höglinger, G.U. Clinical Features of Patients With Progressive Supranuclear Palsy in an US Insurance Claims Database. Front. Neurol. 2021, 12, 571800. [Google Scholar] [CrossRef] [PubMed]
- Mahale, R.R.; Krishnan, S.; Divya, K.P.; Jisha, V.T.; Kishore, A. Subtypes of PSP and Prognosis: A Retrospective Analysis. Ann. Indian Acad. Neurol. 2021, 24, 56–62. [Google Scholar] [CrossRef]
- Vöglein, J.; Kostova, I.; Arzberger, T.; Roeber, S.; Schmitz, P.; Simons, M.; Ruf, V.; Windl, O.; Herms, J.; Dieterich, M.; et al. First symptom guides diagnosis and prognosis in neurodegenerative diseases-a retrospective study of autopsy proven cases. Eur. J. Neurol. 2021, 28, 1801–1811. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Lees, A.J. Progressive supranuclear palsy: Clinicopathological concepts and diagnostic challenges. Lancet Neurol. 2009, 8, 270–279. [Google Scholar] [CrossRef]
- Park, H.K.; Ilango, S.D.; Litvan, I. Environmental Risk Factors for Progressive Supranuclear Palsy. J. Mov. Disord. 2021, 14, 103–113. [Google Scholar] [CrossRef]
- Moore, T.; Guttman, M. Challenges Faced by Patients With Progressive Supranuclear Palsy and their Families. Mov. Disord. Clin. Pract. 2014, 1, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Höllerhage, M.; Klietz, M.; Höglinger, G.U. Disease modification in Parkinsonism: Obstacles and ways forward. J. Neural Transm. 2022, 129, 1133–1153. [Google Scholar] [CrossRef]
- Piccione, F.; Mancini, E.; Tonin, P.; Bizzarini, M. Botulinum toxin treatment of apraxia of eyelid opening in progressive supranuclear palsy: Report of two cases. Arch. Phys. Med. Rehabil. 1997, 78, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Scelzo, E.; Lozano, A.M.; Hamani, C.; Poon, Y.Y.; Aldakheel, A.; Zadikoff, C.; Lang, A.E.; Moro, E. Peduncolopontine nucleus stimulation in progressive supranuclear palsy: A randomised trial. J. Neurol. Neurosurg. Psychiatry 2017, 88, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Boxer, A.L.; Yu, J.T.; Golbe, L.I.; Litvan, I.; Lang, A.E.; Höglinger, G.U. Advances in progressive supranuclear palsy: New diagnostic criteria, biomarkers, and therapeutic approaches. Lancet Neurol. 2017, 16, 552–563. [Google Scholar] [CrossRef] [PubMed]
- Ha, M.; Kim, V.N. Regulation of microRNA biogenesis. Nat. Rev. Mol. Cell Biol. 2014, 15, 509–524. [Google Scholar] [CrossRef] [PubMed]
- Krol, J.; Loedige, I.; Filipowicz, W. The widespread regulation of microRNA biogenesis, function and decay. Nat. Rev. Genet. 2010, 11, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.C.; Feinbaum, R.L.; Ambros, V.; The, C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell 1993, 75, 843–854. [Google Scholar] [CrossRef]
- Grodzka, O.; Procyk, G.; Gąsecka, A. The Role of MicroRNAs in Myocarditis-What Can We Learn from Clinical Trials? Int. J. Mol. Sci. 2022, 23, 16022. [Google Scholar] [CrossRef] [PubMed]
- Grodzka, O.; Procyk, G.; Wrzosek, M. A Narrative Review of Preclinical In Vitro Studies Investigating microRNAs in Myocarditis. Curr. Issues Mol. Biol. 2024, 46, 1413–1423. [Google Scholar] [CrossRef]
- Procyk, G.; Grodzka, O.; Procyk, M.; Gąsecka, A.; Głuszek, K.; Wrzosek, M. MicroRNAs in Myocarditis-Review of the Preclinical In Vivo Trials. Biomedicines 2023, 11, 2723. [Google Scholar] [CrossRef]
- Krauze, A.; Procyk, G.; Gąsecka, A.; Garstka-Pacak, I.; Wrzosek, M. The Role of MicroRNAs in Aortic Stenosis-Lessons from Recent Clinical Research Studies. Int. J. Mol. Sci. 2023, 24, 13095. [Google Scholar] [CrossRef]
- Kiełbowski, K.; Bakinowska, E.; Procyk, G.; Ziętara, M.; Pawlik, A. The Role of MicroRNA in the Pathogenesis of Duchenne Muscular Dystrophy. Int. J. Mol. Sci. 2024, 25, 6108. [Google Scholar] [CrossRef] [PubMed]
- Nelson, P.T.; Wang, W.X.; Rajeev, B.W. MicroRNAs (miRNAs) in neurodegenerative diseases. Brain Pathol. 2008, 18, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.A.; Baxter, D.H.; Zhang, S.; Huang, D.Y.; How Huang, K.; Jen Lee, M.; Galas, D.J.; Wang, K. The microRNA spectrum in 12 body fluids. Clin. Chem. 2010, 56, 1733–1741. [Google Scholar] [CrossRef] [PubMed]
- de Gonzalo-Calvo, D.; Benítez, I.D.; Pinilla, L.; Carratalá, A.; Moncusí-Moix, A.; Gort-Paniello, C.; Molinero, M.; González, J.; Torres, G.; Bernal, M. Circulating microRNA profiles predict the severity of COVID-19 in hospitalized patients. Transl. Res. 2021, 236, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Qiu, X.-K.; Ma, J. Alteration in microRNA-155 level correspond to severity of coronary heart disease. Scand. J. Clin. Lab. Investig. 2018, 78, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Procyk, G.; Klimczak-Tomaniak, D.; Sygitowicz, G.; Tomaniak, M. Circulating and Platelet MicroRNAs in Cardiovascular Risk Assessment and Antiplatelet Therapy Monitoring. J. Clin. Med. 2022, 11, 1763. [Google Scholar] [CrossRef]
- Baumann, V.; Winkler, J. miRNA-based therapies: Strategies and delivery platforms for oligonucleotide and non-oligonucleotide agents. Future Med. Chem. 2014, 6, 1967–1984. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lauretti, E.; Dincer, O.; Praticò, D. Regional and temporal miRNAs expression profile in a transgenic mouse model of tauopathy: Implication for its pathogenesis. Mol. Psychiatry 2021, 26, 7020–7028. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.Y.; Delay, C.; Girard, J.; Papon, M.-A.; Planel, E.; Sergeant, N.; Buée, L.; Hébert, S.S. MicroRNA-132 loss is associated with tau exon 10 inclusion in progressive supranuclear palsy. Hum. Mol. Genet. 2011, 20, 4016–4024. [Google Scholar] [CrossRef]
- Tatura, R.; Buchholz, M.; Dickson, D.W.; van Swieten, J.; McLean, C.; Höglinger, G.; Müller, U. microRNA profiling: Increased expression of miR-147a and miR-518e in progressive supranuclear palsy (PSP). Neurogenetics 2016, 17, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Starhof, C.; Hejl, A.-M.; Heegaard, N.H.H.; Carlsen, A.L.; Burton, M.; Lilje, B.; Winge, K. The biomarker potential of cell-free microRNA from cerebrospinal fluid in Parkinsonian Syndromes. Mov. Disord. 2019, 34, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Manna, I.; Quattrone, A.; De Benedittis, S.; Vescio, B.; Iaccino, E.; Quattrone, A. Exosomal miRNA as peripheral biomarkers in Parkinson’s disease and progressive supranuclear palsy: A pilot study. Park. Relat. Disord. 2021, 93, 77–84. [Google Scholar] [CrossRef]
- Nonaka, W.; Takata, T.; Iwama, H.; Komatsubara, S.; Kobara, H.; Kamada, M.; Deguchi, K.; Touge, T.; Miyamoto, O.; Nakamura, T.; et al. A cerebrospinal fluid microRNA analysis: Progressive supranuclear palsy. Mol. Med. Rep. 2022, 25, 88. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, P.; Christopher, R.; Kumar Pal, P.; Debnath, M.; Yadav, R. Plasma microRNAs as a Potential Biomarker for Identification of Progressive Supranuclear Palsy. Diagnostics 2022, 12, 1204. [Google Scholar] [CrossRef]
- Simoes, F.A.; Joilin, G.; Peters, O.; Schneider, L.-S.; Priller, J.; Spruth, E.J.; Vogt, I.; Kimmich, O.; Spottke, A.; Hoffmann, D.C.; et al. Potential of Non-Coding RNA as Biomarkers for Progressive Supranuclear Palsy. Int. J. Mol. Sci. 2022, 23, 14554. [Google Scholar] [CrossRef]
- Pavelka, L.; Rauschenberger, A.; Hemedan, A.; Ostaszewski, M.; Glaab, E.; Krüger, R. Converging peripheral blood microRNA profiles in Parkinson’s disease and progressive supranuclear palsy. Brain Commun. 2024, 6, fcae187. [Google Scholar] [CrossRef]
- Zhu, Q.-B.; Unmehopa, U.; Bossers, K.; Hu, Y.-T.; Verwer, R.; Balesar, R.; Zhao, J.; Bao, A.-M.; Swaab, D. MicroRNA-132 and early growth response-1 in nucleus basalis of Meynert during the course of Alzheimer’s disease. Brain 2016, 139, 908–921. [Google Scholar] [CrossRef]

| Ref. | Year | Population | Comparison | miRNA | Outcome | Methodology |
|---|---|---|---|---|---|---|
| [41] | 2021 | hTau mice (n = 3–8/group depending on the experiment) | wild-type C57BL/6J mice (n = 3–8/group depending on the experiment) | miR-22-3p, miR-132-3p, miR-146a-5p, miR-455-5p | 12 months of age: ↑ miR-22-3p, miR-132-3p, miR-146a-5p, miR-455-5p in the hippocampus and ↑ miR-132-3p, miR-146a-5p in the the cerebellum of hTau mice 6 months of age: ↑ miR-146a-5p in the hippocampus and ↑ miR-132-3p, miR-146a-5p in the the cerebellum of hTau mice 3 months of age: no difference | miRNA in brain tissues (cortex, hippocampus, cerebellum) by qRT-PCR |
| Ref. | Year | Population | Comparison | miRNA | Outcome | Methodology |
|---|---|---|---|---|---|---|
| [42] | 2011 | 8 PSP pts | 8 HCs | miR-9, miR-124, miR-132, miR-137, miR-153 | ↓ miR-132 in the temporal lobes of PSP patients compared with HCs | miRNA in brain tissues by qRT-PCR |
| [43] | 2016 | 20 PSP pts | 20 HCs | miR-147, miR-518e, miR-504, miR-525-3p | ↑ miR-147a and miR-518e in the frontal lobes of PSP patients compared with HCs | miRNA in frontal lobe tissue by qRT-PCR |
| Ref. | Year | Population | Comparison | miRNA | Outcome | Methodology |
|---|---|---|---|---|---|---|
| [44] | 2019 | 32 PSP pts | 37 PD pts 29 MSA pts 23 HCS | 46 various miRNAs | ROC analysis (PD vs. PSP) CSF: miR-106b-5p AUC 0.85 (95% Cl: 0.757–0.945) plasma: miR-218-5p AUC 0.71 (95% Cl: 0.594–0.826) | miRNA in CSF and plasma by qRT-PCR |
| [45] | 2021 | 20 PSP pts | 40 PD pts 33 HCs | miR-425-5p, miR-21-3p, miR-223-5p, miR-22-3p, let-7i-5p, miR-199a-5p, miR-29a-3p, miR-483-5p | ↓ miR-425-5p, miR-21-3p, and miR-199a-5p in PSP pts compared with PD pts ROC analysis (PSP vs. PD) combination of miR-425-5p, miR-21-3p, and miR-199a-5p with AUC 0.86 (95% CI: 0.74-0.97) combination of miR-21-3p, miR-199a-5p, miR-425-5p, miR-483-5p, miR-22-3p, and miR-29a-3p with AUC 0.91 (95% CI: 0.82–1.00) | exosomal miRNA in serum by qRT-PCR |
| [46] | 2022 | 11 PSP pts | 8 age- and sex-matched controls | 2632 various miRNAs | ↑ 38 various miRNAs and ↓ miR-6840-5p in PSP pts compared with controls ↑ miR-204-3p and miR-873-3p and ↓ miR-6840-5p in early-stage PSP pts compared with controls ↑ miR-204-3p and miR-873-3p and ↓ miR-6840-5p in advanced-stage PSP pts compared with controls | miRNA in CSF by microarray analysis |
| [47] | 2022 | 18 PSP pts | 17 age-matched HCs | miR-19b-3p, miR-33a-5p, miR-130b-3p, miR-136-3p, miR-210-3p | ↑ miR-19b-3p, miR-33a-5p, miR-130b-3p, miR-136-3p, miR-210-3p in PSP pts ROC analysis: miR-19b-3p AUC 0.7059 miR-33a-5p AUC 0.8578 miR-130b-3p AUC 0.7778 miR-136-3p AUC 0.7882 miR-210-3p AUC 0.7810 combination of all five miRNAs: AUC 0.7817 (95% CI: 0.7126–0.8508) | miRNA in plasma by qPCR |
| [48] | 2022 | 31 PSP pts | 20 age- and sex-matched HCs | let-7a-5p, let-7b-5p, let-7f-2-3p, miR-1-3p, miR-16-5p, miR-92a-3p, miR-148a-3p, miR-626, miR-3168 | ↓ miR-92a-3p, miR-626 in serum of PSP pts ↑ let-7a-5p in CSF of PSP pts | miRNA in CSF and serum by qRT-PCR |
| [49] | 2024 | 35 PSP pts | 367 PD pts 416 HCs | 2549 various miRNAs | ↑ miR-2115-5p, miR-4270, miR-505-3p, miR-769-5p, miR-3065-3p, miR-4638-5p, miR-197-3p, let-7d-3p, and miR-1225-5p and ↓ miR-4762-3p, miR-7975, miR-1233-5p, miR-6085, miR-125a-3p, miR-4465, and miR-564 in PSP pts compared with HCs no difference in miRNA expression between PSP and PD pts | miRNA in whole blood by microarray analysis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ćwiklińska, A.; Procyk, G.; Koziorowski, D.; Szlufik, S. The Role of MicroRNAs in Progressive Supranuclear Palsy—A Systematic Review. Int. J. Mol. Sci. 2024, 25, 8243. https://doi.org/10.3390/ijms25158243
Ćwiklińska A, Procyk G, Koziorowski D, Szlufik S. The Role of MicroRNAs in Progressive Supranuclear Palsy—A Systematic Review. International Journal of Molecular Sciences. 2024; 25(15):8243. https://doi.org/10.3390/ijms25158243
Chicago/Turabian StyleĆwiklińska, Aleksandra, Grzegorz Procyk, Dariusz Koziorowski, and Stanisław Szlufik. 2024. "The Role of MicroRNAs in Progressive Supranuclear Palsy—A Systematic Review" International Journal of Molecular Sciences 25, no. 15: 8243. https://doi.org/10.3390/ijms25158243
APA StyleĆwiklińska, A., Procyk, G., Koziorowski, D., & Szlufik, S. (2024). The Role of MicroRNAs in Progressive Supranuclear Palsy—A Systematic Review. International Journal of Molecular Sciences, 25(15), 8243. https://doi.org/10.3390/ijms25158243








