Advancements in the Research of New Modulators of Nitric Oxide Synthases Activity
Abstract
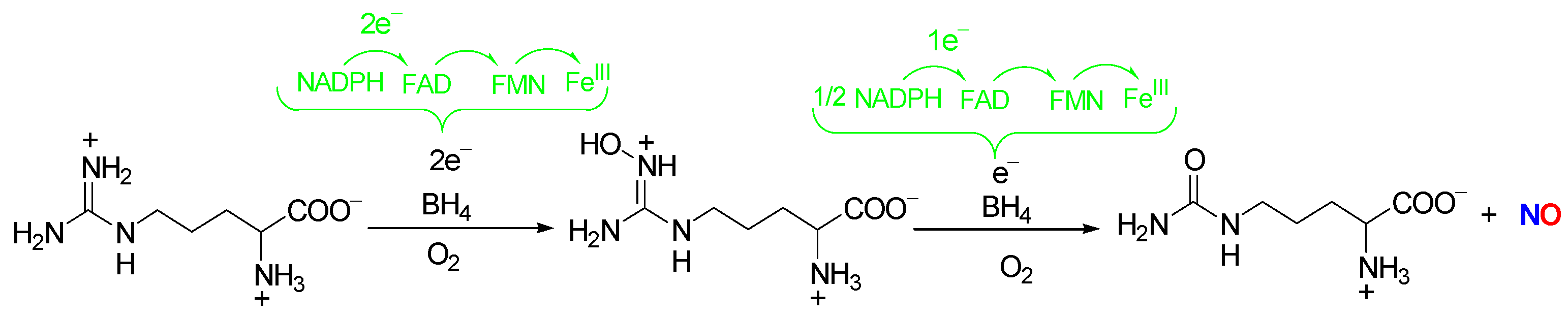
:1. Introduction
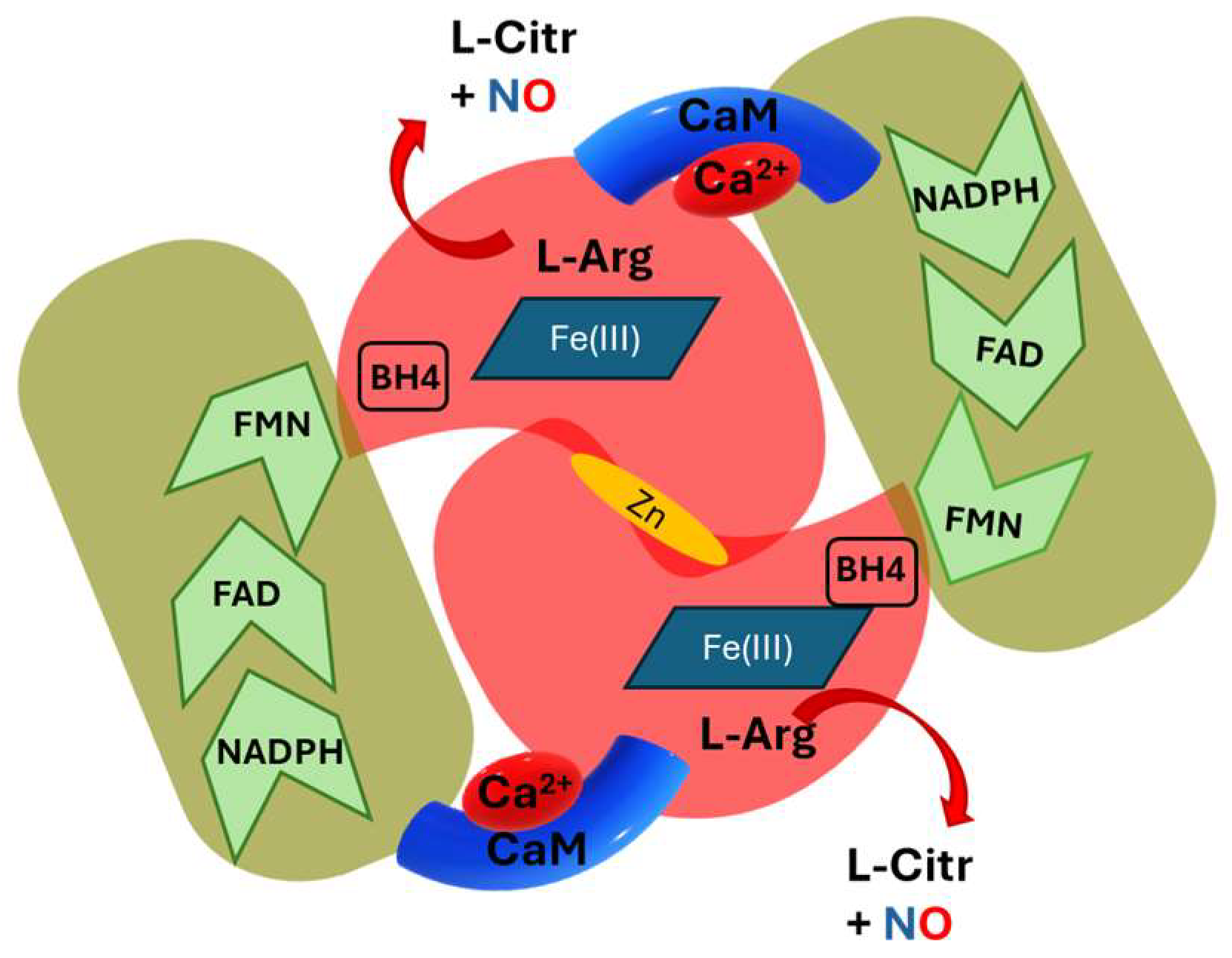
2. The NOS Structure
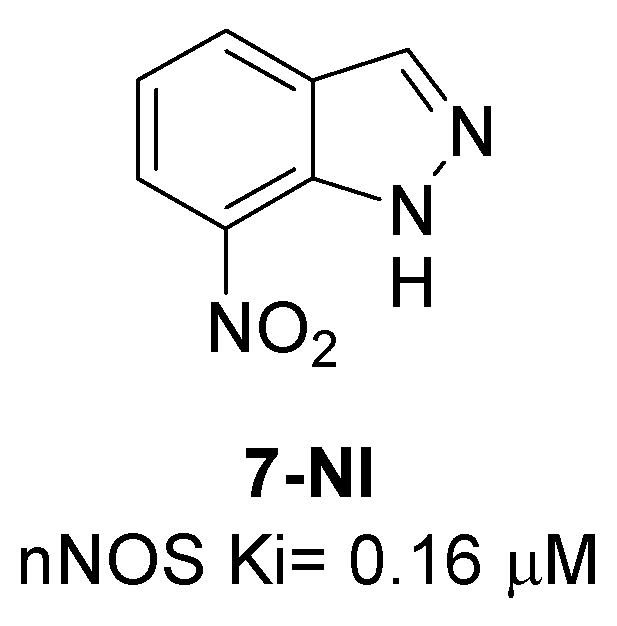
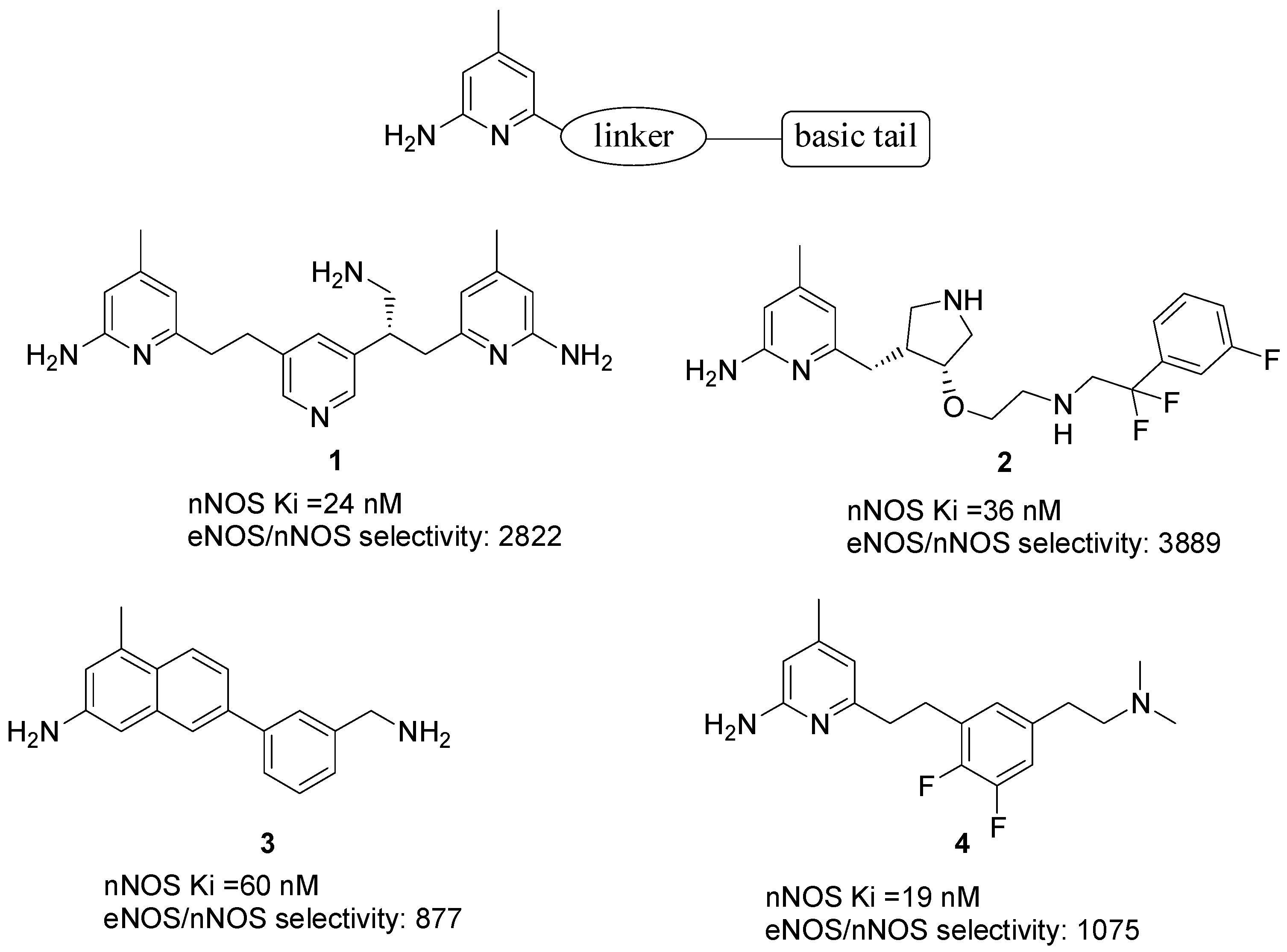
3. nNOS Modulators
| Compound | Target | Therapy Area | Study | Reference |
|---|---|---|---|---|
| 7-NI | NOS heme | neuroprotection | preclinical | [26,27,28] |
| 1–4 | L-Arg catalytic site | neurodegeneration/ neuropathic pain | preclinical | [34] |
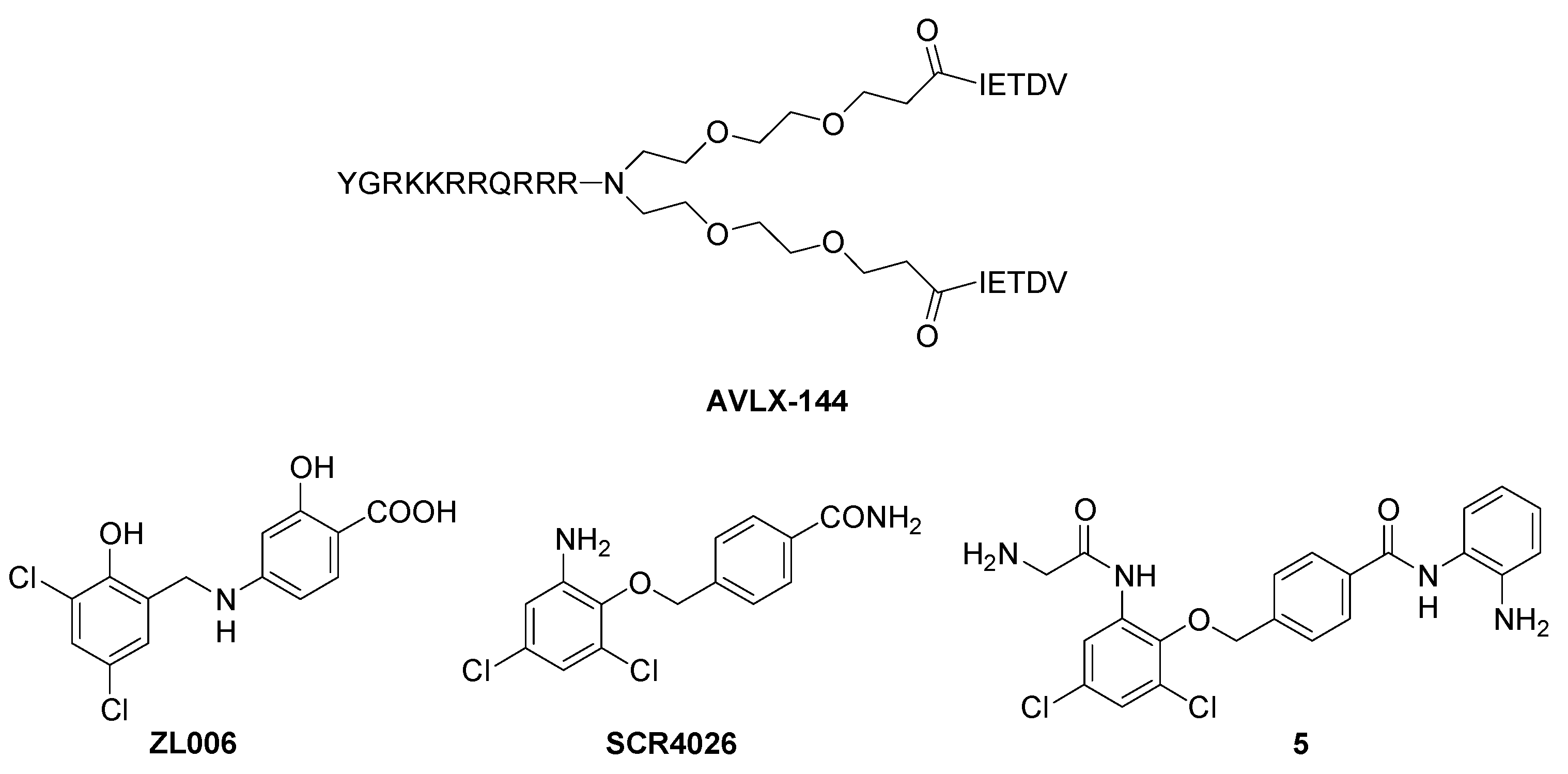
| AVLX-144 | nNOS-PSD95 interaction | stroke | Phase 1 (completed) | [36] |
| ZL006 | nNOS-PSD95 interaction | stroke | preclinical | [37,38,39] |
| SCR4026 | nNOS-PSD95 interaction | stroke | preclinical | [40] |
| 5 | nNOS-PSD95 interaction | stroke | preclinical | [41] |
| nerinetide | NMDAR-PSD95 interaction | stroke | Phase III (completed) | [42] |
4. iNOS Modulators
| Compound | Target | Therapy Area | Study | References |
|---|---|---|---|---|
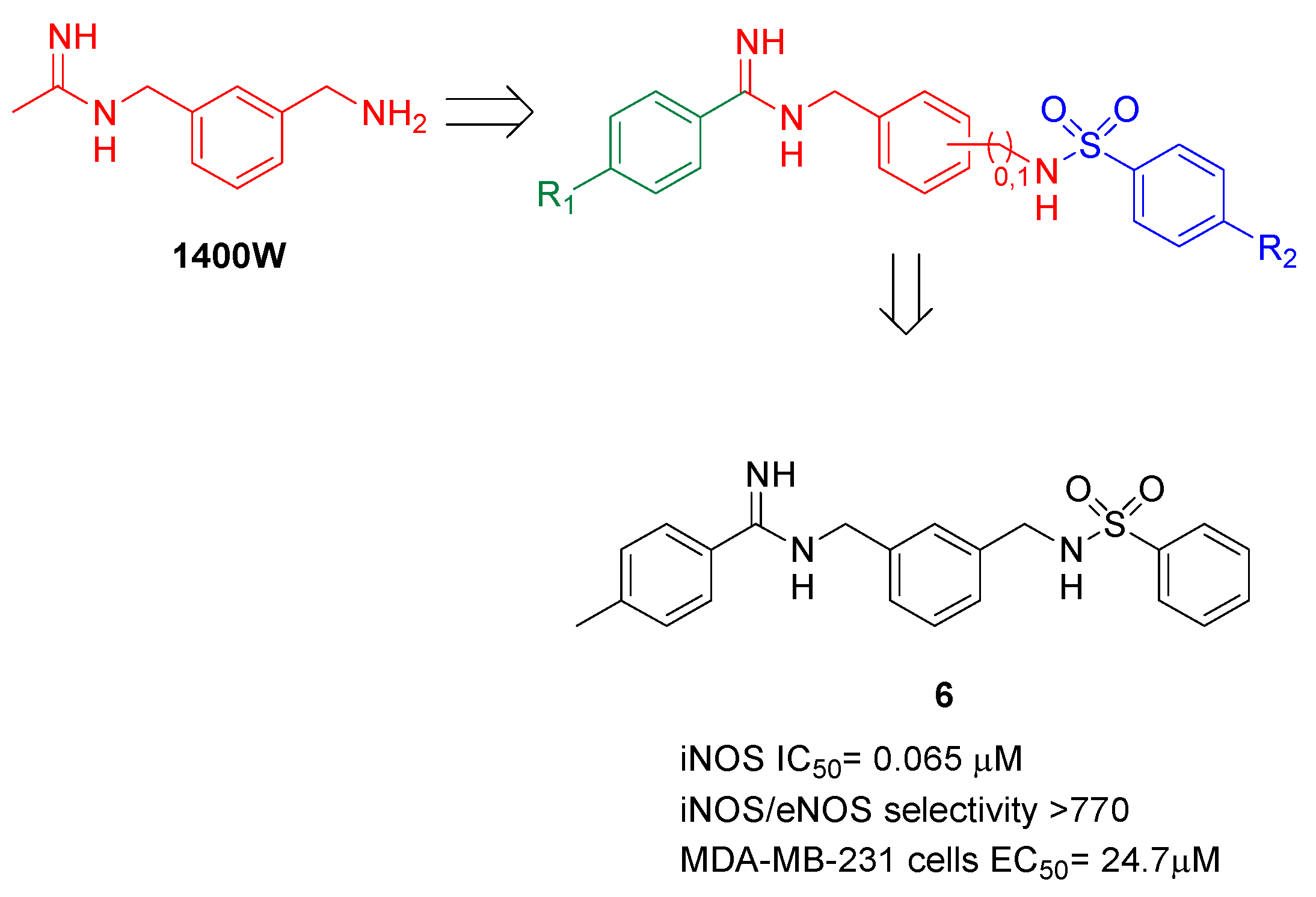
| 1400W | L-Arg catalytic site | Hyperalgesia, stroke, cancer | preclinical | [54,55,56] |
| GW274150 | L-Arg catalytic site | Septic shock, neuroprotection, rheumatoid arthritis | Phase 2 (completed) | [59,60] |
| L-NIL | L-Arg catalytic site | renal ischemia/ reperfusion injury | preclinical | [58] |
| BYK191023 | L-Arg catalytic site | septic shock; cancer | preclinical | [57] |
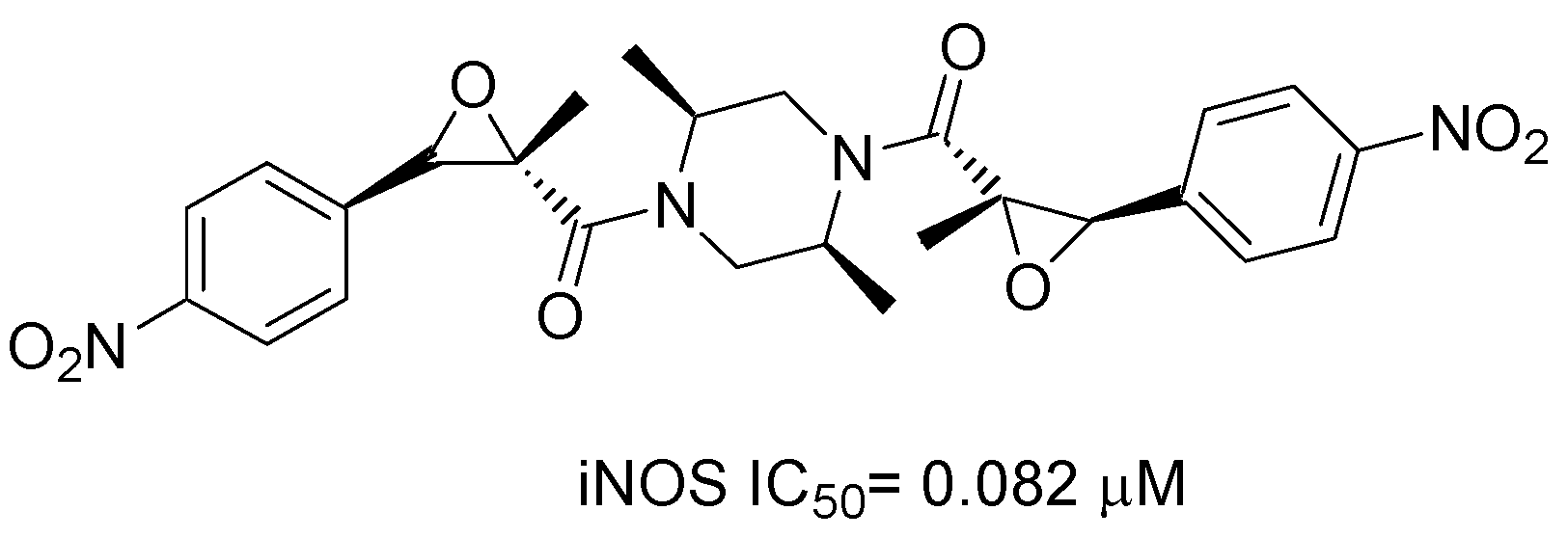
| 6 | L-Arg catalytic site | cancer | preclinical | [65] |
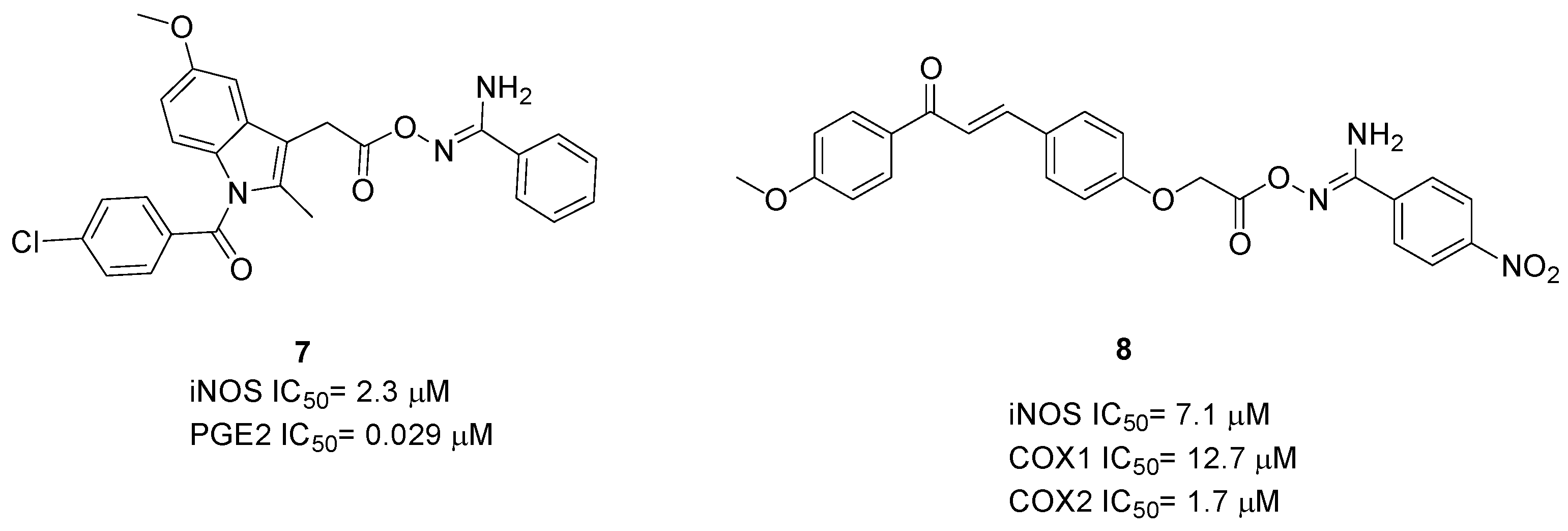
| 7–8 | L-Arg catalytic site | inflammation | preclinical | [66,67] |
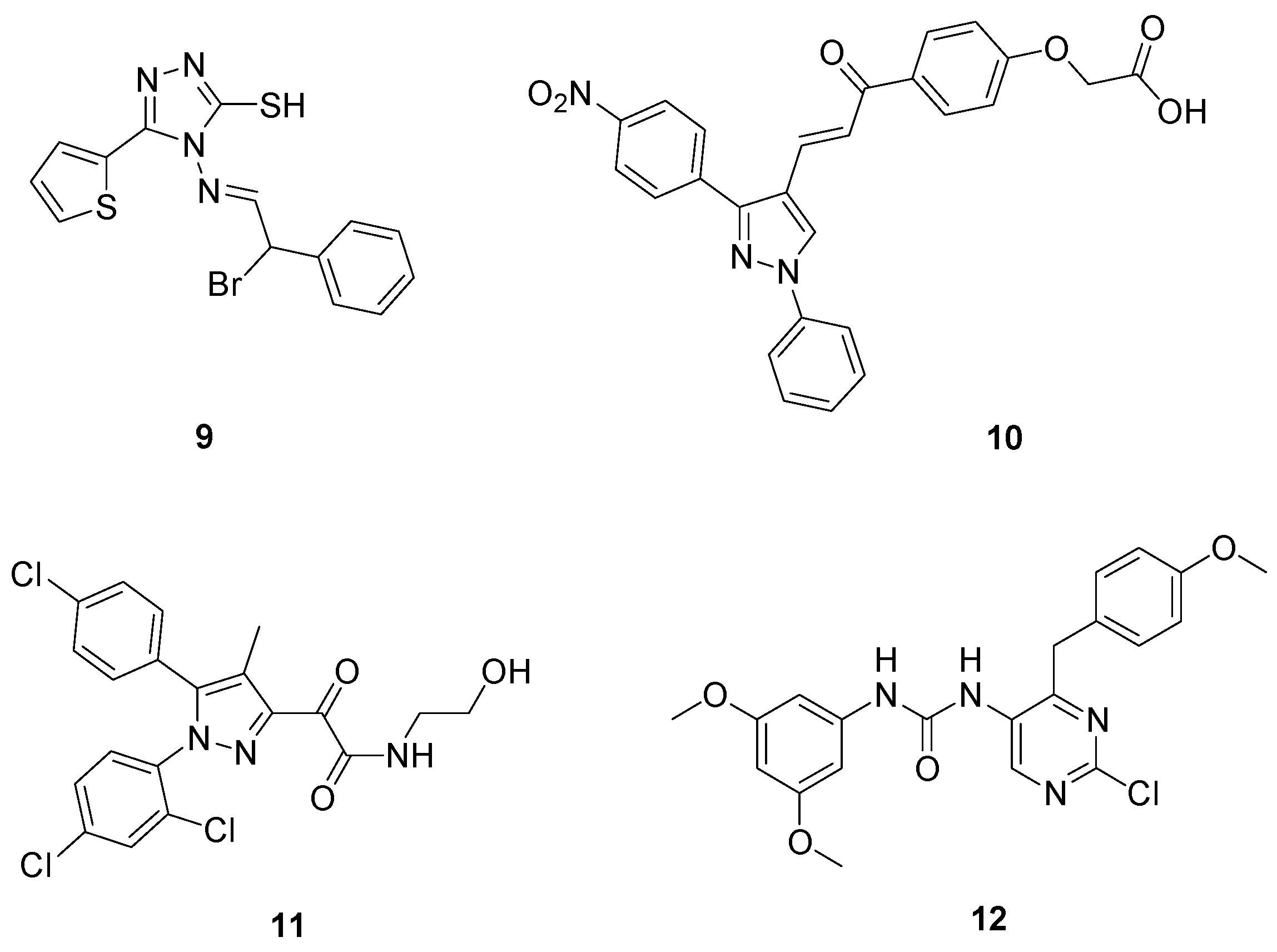
| 9–12 | Inhibition of NF-kB | inflammation, cancer | preclinical | [68,69,70,71] |
| 13–15 | iNOS dimerization | arthritis | preclinical | [72,73] |
| chrysamide B | iNOS dimerization | oedema, septic shock | preclinical | [74] |
5. eNOS Modulators
| Compound | Target | Therapy Area | Study | Reference |
|---|---|---|---|---|
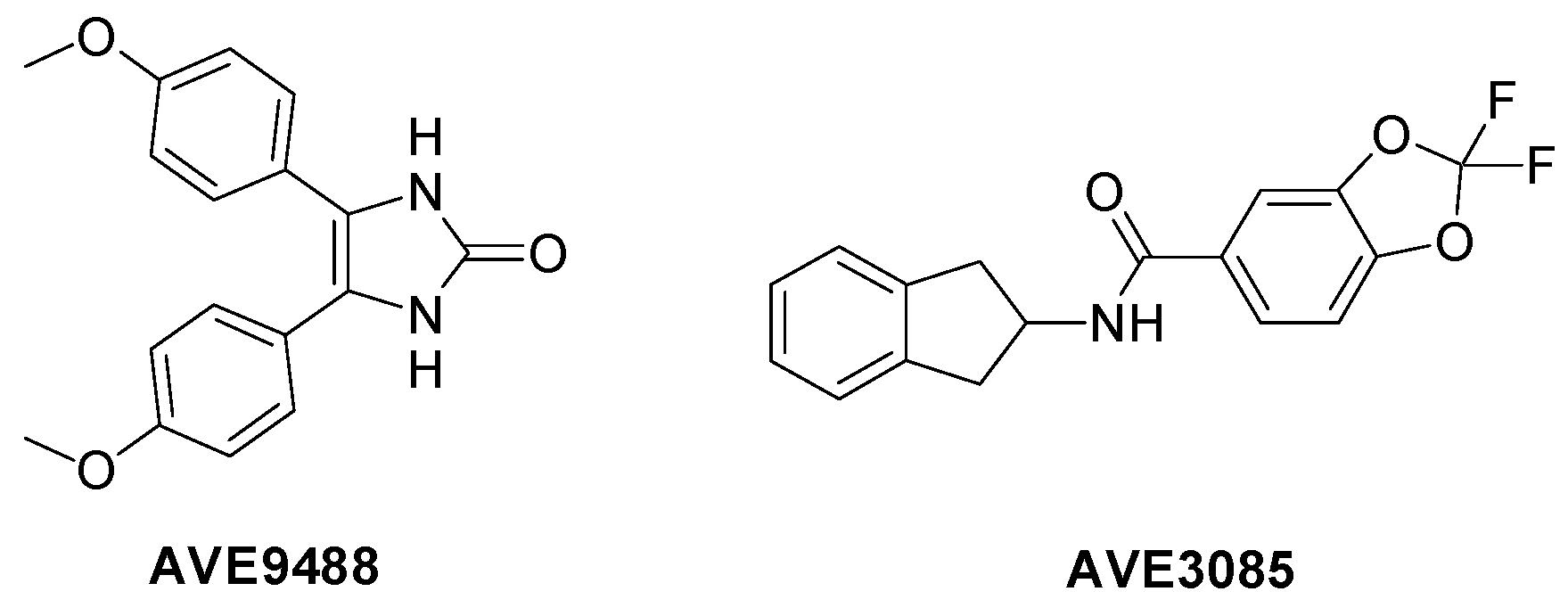
| AVE9488; AVE3085 | transcription enhancers | cardiac remodeling; endothelial dysfunction, hypertension | preclinical | [78,79,80] |
| taxifolin | eNOS phosphorilation | hypertension | preclinical | [89] |
| kaempferol | eNOS phosphorilation | wound healing | preclinical | [85] |
| quercetin | eNOS phosphorilation | endothelial dysfunction | preclinical | [86,87] |
| myricetin | eNOS phosphorilation | endothelial dysfunction | preclinical | [88] |
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Smith, O. Nobel Prize for NO research. Nat. Med. 1998, 11, 1215. [Google Scholar] [CrossRef] [PubMed]
- Moncada, S.; Higgs, E.A. The discovery of nitric oxide and its role in vascular biology. Br. J. Pharmacol. 2006, 147, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Santolini, J. The molecular mechanism of mammalian NO-synthases: A story of electrons and protons. J. Inorg. Biochem. 2011, 105, 127–141. [Google Scholar] [CrossRef] [PubMed]
- Brenman, J.E.; Chao, D.S.; Gee, S.H.; McGee, A.W.; Craven, S.E.; Santillano, D.R.; Wu, Z.; Huang, F.; Xia, H.; Peters, M.F. Interaction of nitric oxide synthase with the postsynaptic density protein PSD-95 and alpha1-syntrophin mediated by PDZ domains. Cell 1996, 84, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Maccallini, C.; Amoroso, R. Neuronal Nitric Oxide Synthase and Post-Translational Modifications in the Development of Central Nervous System Diseases: Implications and Regulation. Molecules 2023, 28, 6691. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Fulton, D. Post-translational regulation of endothelial nitric oxide synthase in vascular endothelium. Front. Physiol. 2013, 4, 347. [Google Scholar] [CrossRef]
- Govers, R.; Rabelink, T.J. Cellular regulation of endothelial nitric oxide synthase. Am. J. Physiol. Renal Physiol. 2001, 280, F193–F206. [Google Scholar] [CrossRef] [PubMed]
- Cinelli, M.A.; Do, H.T.; Miley, G.P.; Silverman, R.B. Inducible nitric oxide synthase: Regulation, structure, and inhibition. Med. Res. Rev. 2020, 40, 158–189. [Google Scholar] [CrossRef]
- Förstermann, U.; Sessa, W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2012, 33, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Silverman, R.B. Revisiting heme mechanisms. A perspective on the mechanisms of nitric oxide synthase (NOS), Heme oxygenase (HO), and cytochrome P450s (CYP450s). Biochemistry 2008, 47, 2231–2243. [Google Scholar] [CrossRef]
- Wei, C.C.; Crane, B.R.; Stuehr, D.J. Tetrahydrobiopterin radical enzymology. Chem. Rev. 2003, 103, 2365–2383. [Google Scholar] [CrossRef] [PubMed]
- Minhas, R.; Bansal, Y.; Bansal, G. Inducible nitric oxide synthase inhibitors: A comprehensive update. Med. Res. Rev. 2020, 40, 823–855. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.G.; Smith, B.C.; Potter, C.S.; Carragher, B.; Marletta, M.A. Molecular architecture of mammalian nitric oxide synthases. Proc. Natl. Acad. Sci. USA. 2014, 111, 3614–3623. [Google Scholar] [CrossRef]
- Venema, R.C.; Sayegh, H.S.; Kent, J.D.; Harrison, D.G. Identification, characterization, and comparison of the calmodulin-binding domains of the endothelial and inducible nitric oxide synthases. J. Biol. Chem. 1996, 271, 6435–6440. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, G.M.; Nishida, C.R.; Mooney, S.D.; Ortiz de Montellano, P.R. Nitric-oxide synthase (NOS) reductase domain models suggest a new control element in endothelial NOS that attenuates calmodulin-dependent activity. J. Biol. Chem. 2003, 278, 31814–31824. [Google Scholar] [CrossRef]
- Jones, R.J.; Smith, S.M.; Gao, Y.T.; DeMay, B.S.; Mann, K.J.; Salerno, K.M.; Salerno, J.C. The function of the small insertion in the hinge subdomain in the control of constitutive mammalian nitric-oxide synthases. J. Biol. Chem. 2004, 279, 36876–36883. [Google Scholar] [CrossRef] [PubMed]
- Panda, K.; Rosenfeld, R.J.; Ghosh, S.; Meade, A.L.; Getzoff, E.D.; Stuehr, D.J. Distinct dimer interaction and regulation in nitric-oxide synthase types I, II, and III. J. Biol. Chem. 2002, 277, 31020–31030. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Li, H.; Flinspach, M.; Poulos, T.L.; Silverman, R.B. Computer modeling of selective regions in the active site of nitric oxide synthases: Implication for the design of isoform-selective inhibitors. J. Med. Chem. 2003, 46, 5700–5711. [Google Scholar]
- Garcin, E.D.; Arvai, A.S.; Rosenfeld, R.J.; Kroeger, M.D.; Crane, B.R.; Andersson, G.; Andrews, G.; Hamley, P.J.; Mallinder, P.R.; Nicholls, D.J.; et al. Anchored plasticity opens doors for selective inhibitor design in nitric oxide synthase. Nat. Chem. Biol. 2008, 4, 700–707. [Google Scholar] [CrossRef]
- Garcin, E.D.; Bruns, C.M.; Lloyd, S.J.; Hosfield, D.J.; Tiso, M.; Gachhui, R.; Stuehr, D.J.; Tainer, J.A.; Getzoff, E.D. Structural basis for isozyme-specific regulation of electron transfer in nitric-oxide synthase. J. Biol. Chem. 2004, 279, 37918–37927. [Google Scholar] [CrossRef]
- Venema, R.C.; Ju, H.; Zou, R.; Ryan, J.W.; Venema, V.J. Subunit interactions of endothelial nitric-oxide synthase. Comparisons to the neuronal and inducible nitric-oxide synthase isoforms. J. Biol. Chem. 1997, 272, 1276–1282. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Ji, H.; Lawton, G.R.; Xue, F.; Roman, L.J.; Silverman, R.B. L337H mutant of rat neuronal nitric oxide synthase resembles human neuronal nitric oxide synthase toward inhibitors. J. Med. Chem. 2009, 52, 4533–4537. [Google Scholar] [CrossRef]
- Bogdan, C. Nitric oxide and the immune response. Nat. Immunol. 2001, 2, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Hollern, D.; Liao, J.; Andrechek, E.; Wang, H. NMDA receptor-mediated excitotoxicity depends on the coactivation of synaptic and extrasynaptic receptors. Cell Death Dis. 2013, 28, e560. [Google Scholar] [CrossRef] [PubMed]
- Bradley, S.A.; Steinert, J.R. Nitric Oxide-Mediated Posttranslational Modifications: Impacts at the Synapse. Oxid. Med. Cell. Longev. 2016, 2016, 5681036. [Google Scholar] [CrossRef]
- Herrero, M.T.; Yuste, J.E.; Cuenca-Bermejo, L.; Almela, P.; Arenas-Betancur, L.; De Pablos, V.; Gonzalez-Cuello, A.; Del Bel, E.; Navarro-Zaragoza, J.; Fernández-Villalba, E. 7-Nitroindazole reduces L-DOPA-induced dyskinesias in non-human Parkinsonian primate. Open Biol. 2023, 13, 220370. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Guo, R.; Ofengeim, D.; Hwang, J.; Zukin, R.S.; Chen, J.; Zhang, F. 5–Molecular and Cellular Mechanisms of Ischemia-Induced Neuronal Death; In Stroke, 7th ed.; Grotta, J.C., Albers, G.W., Broderick, J.P., Day, A.L., Kasner, S.E., Lo, E.H., Sacco, R.L., Wong, L.K.S., Eds.; Elsevier: Amsterdam, The Netherlands, 2022; p. 73.e6. [Google Scholar]
- O‘Toole, E.; Doucet, M.V.; Sherwin, E.; Harkin, A. Chapter 3—Novel Targets in the Glutamate and Nitric Oxide Neurotransmitter Systems for the Treatment of Depression. In Systems Neuroscience in Depression; Thomas, F., Ed.; Academic Press: Cambridge, MA, USA, 2016; pp. 81–113. [Google Scholar]
- Wolff, D.J.; Gribin, B.J. The inhibition of the constitutive and inducible nitric oxide synthase isoforms by indazole agents. Arch. Biochem. Biophys. 1994, 311, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Reiner, A.; Zagvazdin, Y. On the selectivity of 7-nitroindazole as an inhibitor of neuronal nitric oxide synthase. Trends Pharmacol. Sci. 1998, 19, 348–350. [Google Scholar] [CrossRef] [PubMed]
- Xue, F.; Li, H.; Delker, S.L.; Fang, J.; Martásek, P.; Roman, L.J.; Poulos, T.L.; Silverman, R.B. Potent, highly selective, and orally bioavailable gem-difluorinated monocationic inhibitors of neuronal nitric oxide synthase. J. Am. Chem. Soc. 2010, 132, 14229–14238. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Tang, W.; Li, H.; Chreifi, G.; Martásek, P.; Roman, L.J.; Poulos, T.L.; Silverman, R.B. Nitric oxide synthase inhibitors that interact with both heme propionate and tetrahydrobiopterin show high isoform selectivity. J. Med. Chem. 2014, 57, 4382–4396. [Google Scholar] [CrossRef]
- Vasu, D.; Do, H.T.; Li, H.; Hardy, C.D.; Awasthi, A.; Poulos, T.L.; Silverman, R.B. Potent, Selective, and Membrane Permeable 2-Amino-4-Substituted Pyridine-Based Neuronal Nitric Oxide Synthase Inhibitors. J. Med. Chem. 2023, 66, 9934–9953. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, P.; Cinelli, M.A.; Kang, S.; Silverman, R.B. Development of nitric oxide synthase inhibitors for neurodegeneration and neuropathic pain. Chem. Soc. Rev. 2014, 43, 6814–6838. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Hardy, C.D.; Reidl, C.T.; Jing, Q.; Xue, F.; Cinelli, M.; Silverman, R.B.; Poulos, T.L. Crystallographic and Computational Insights into Isoform-Selective Dynamics in Nitric Oxide Synthase. Biochemistry 2024, 63, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.; Clausen, B.H.; Kristensen, L.K.; Andersen, M.G.; Ellman, D.G.; Hansen, P.B.L.; Hasseldam, H.; Heitz, M.; Ozcelik, D.; Tuck, E.J.; et al. Selectivity, efficacy and toxicity studies of UCCB01-144, a dimeric neuroprotective PSD-95 inhibitor. Neuropharmacology 2019, 150, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.; Clausen, B.H.; Møller, M.; Vestergaard, B.; Chi, C.N.; Round, A.; Sørensen, P.L.; Nissen, K.B.; Kastrup, J.S.; Gajhede, M.; et al. A high-affinity, dimeric inhibitor of PSD-95 bivalently interacts with PDZ1-2 and protects against ischemic brain damage. Proc. Natl. Acad. Sci. USA 2012, 109, 3317–3322. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Li, F.; Xu, H.B.; Luo, C.X.; Wu, H.Y.; Zhu, M.M.; Lu, W.; Ji, X.; Zhou, Q.G.; Zhu, D.Y. Treatment of cerebral ischemia by disrupting ischemia-induced interaction of nNOS with PSD-95. Nat. Med. 2010, 16, 1439–1443. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Huang, Z.; Wang, X.; Chen, M.; Chen, W.; Hua, Y.; Ren, J.; Shen, L.; Song, Y.; Zhou, Y.; et al. Preclinical evaluation of ZL006-05, a new antistroke drug with fast-onset antidepressant and anxiolytic effects. Stroke Vasc. Neurol. 2023, 8, 463–474. [Google Scholar] [CrossRef]
- Hu, W.; Guan, L.S.; Dang, X.B.; Ren, P.Y.; Zhang, Y.L. Small-molecule inhibitors at the PSD-95/nNOS interface attenuate MPP+-induced neuronal injury through Sirt3 mediated inhibition of mitochondrial dysfunction. J. Neurochem. Int. 2014, 79, 57–64. [Google Scholar] [CrossRef]
- Mo, S.F.; Liao, G.Y.; Yang, J.; Wang, M.Y.; Hu, Y.; Lian, G.N.; Kong, L.D.; Zhao, Y. Protection of neuronal cells from excitotoxicity by disrupting nNOS-PSD95 interaction with a small molecule SCR-4026. Brain Res. 2016, 1648(Pt. A), 250–256. [Google Scholar] [CrossRef]
- Zhou, X.F. ESCAPE-NA1 Trial Brings Hope of Neuroprotective Drugs for Acute Ischemic Stroke: Highlights of the Phase 3 Clinical Trial on Nerinetide. Neurosci. Bull. 2021, 37, 579–581. [Google Scholar] [CrossRef]
- Chen, W.; Jiang, B.; Zhao, Y.; Yu, W.; Zhang, M.; Liang, Z.; Liu, X.; Ye, B.; Chen, D.; Yang, L.; et al. Discovery of benzyloxy benzamide derivatives as potent neuroprotective agents against ischemic stroke. Eur. J. Med. Chem. 2023, 261, 115871. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.B.; Chen, Z.R.; Yang, S.L.; Hong, F.F. Nitric Oxide Synthases in Rheumatoid Arthritis. Molecules 2023, 28, 4414. [Google Scholar] [CrossRef]
- Kolios, G.; Valatas, V.; Ward, S.G. Nitric oxide in inflammatory bowel disease: A universal messenger in an unsolved puzzle. Immunology 2004, 113, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.; Martins, M.A.; Tibério, I.F. Nitric oxide in asthma physiopathology. ISRN Allergy 2011, 2011, 832560. [Google Scholar] [CrossRef] [PubMed]
- Steinert, J.R.; Chernova, T.; Forsythe, I.D. Nitric Oxide Signaling in Brain Function, Dysfunction, and Dementia. Neuroscientist 2010, 16, 435–452. [Google Scholar]
- Maccallini, C.; Gallorini, M.; Cataldi, A.; Amoroso, R. Targeting iNOS As a Valuable Strategy for the Therapy of Glioma. ChemMedChem 2020, 15, 339–344. [Google Scholar] [CrossRef]
- Kielbik, M.; Szulc-Kielbik, I.; Klink, M. The Potential Role of iNOS in Ovarian Cancer Progression and Chemoresistance. Int. J. Mol. Sci. 2019, 20, 1751. [Google Scholar] [CrossRef] [PubMed]
- Kostourou, V.; Cartwright, J.E.; Johnstone, A.P.; Boult, J.K.; Cullis, E.R.; Whitley, G.; Robinson, S.P. The role of tumour-derived iNOS in tumour progression and angiogenesis. Br. J. Cancer. 2011, 104, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Maccallini, C.; Patruno, A.; Besker, N.; Alì, J.I.; Ammazzalorso, A.; De Filippis, B.; Franceschelli, S.; Giampietro, L.; Pesce, M.; Reale, M.; et al. Synthesis, biological evaluation, and docking studies of N-substituted acetamidines as selective inhibitors of inducible nitric oxide synthase. J. Med. Chem. 2009, 52, 1481–1485. [Google Scholar] [CrossRef]
- Alderton, W.K.; Angell, A.D.; Craig, C.; Dawson, J.; Garvey, E.; Moncada, S.; Monkhouse, J.; Rees, D.; Russell, L.J.; Russell, R.J.; et al. GW274150 and GW273629 are potent and highly selective inhibitors of inducible nitric oxide synthase in vitro and in vivo. Br. J. Pharmacol. 2005, 145, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.K.; Green, B.G.; Stiffey-Wilusz, J.; Durette, P.L.; Shah, S.K.; Kozarich, J.W. Structural requirements for human inducible nitric oxide synthase substrates and substrate analogue inhibitors. Biochemistry 1998, 37, 4174–4180. [Google Scholar] [CrossRef]
- Pérez-Asensio, F.J.; Hurtado, O.; Burguete, M.C.; Moro, M.A.; Salom, J.B.; Lizasoain, I.; Torregrosa, G.; Leza, J.C.; Alborch, E.; Castillo, J.; et al. Inhibition of iNOS activity by 1400W decreases glutamate release and ameliorates stroke outcome after experimental ischemia. Neurobiol. Dis. 2005, 18, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Svensson, C.I.; Fitzsimmons, B.; Webb, M.; Yaksh, T.L.; Hua, X.Y. Inhibition of spinal constitutive NOS-2 by 1400W attenuates tissue injury and inflammation-induced hyperalgesia and spinal p38 activation. Eur. J. Neurosci. 2007, 25, 2964–2972. [Google Scholar] [CrossRef] [PubMed]
- Merenzon, M.A.; Arias, E.H.; Bhatia, S.; Shah, A.H.; Higgins, D.M.O.; Villaverde, M.; Belgorosky, D.; Eijan, A.M. Nitric oxide synthase inhibitors as potential therapeutic agents for gliomas: A systematic review. Nitric Oxide 2023, 138–139, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Strub, A.; Ulrich, W.R.; Hesslinger, C.; Eltze, M.; Fuchss, T.; Strassner, J.; Strand, S.; Lehner, M.D.; Boer, R. The novel imidazopyridine 2-[2-(4-methoxy-pyridin-2-yl)-ethyl]-3H-imidazo[4,5-b]pyridine (BYK191023) is a highly selective inhibitor of the inducible nitric-oxide synthase. Mol. Pharmacol. 2006, 69, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Zahmatkesh, M.; Kadkhodaee, M.; Arab, H.A.; Shams, S. Effects of co-administration of an iNOS inhibitor with a broad-spectrum reactive species scavenger in rat renal ischemia/reperfusion injury. Nephron Exp. Nephrol. 2006, 103, e119–e125. [Google Scholar] [CrossRef] [PubMed]
- Su, F.; Huang, H.; Akieda, K.; Occhipinti, G.; Donadello, K.; Piagnerelli, M.; De Backer, D.; Vincent, J.L. Effects of a selective iNOS inhibitor versus norepinephrine in the treatment of septic shock. Shock 2010, 34, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Broom, L.; Marinova-Mutafchieva, L.; Sadeghian, M.; Davis, J.B.; Medhurst, A.D.; Dexter, D.T. Neuroprotection by the selective iNOS inhibitor GW274150 in a model of Parkinson disease. Free Radic. Biol. Med. 2011, 50, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Seymour, M.; Pétavy, F.; Chiesa, F.; Perry, H.; Lukey, P.T.; Binks, M.; Donatien, P.D.; Freidin, A.J.; Eckersley, R.J.; McClinton, C.; et al. Ultrasonographic measures of synovitis in an early phase clinical trial: A double-blind, randomised, placebo and comparator controlled phase IIa trial of GW274150 (a selective inducible nitric oxide synthase inhibitor) in rheumatoid arthritis. Clin. Exp. Rheumatol. 2012, 30, 254–261. [Google Scholar] [PubMed]
- Barbanti, P.; Egeo, G.; Aurilia, C.; Fofi, L.; Della-Morte, D. Drugs targeting nitric oxide synthase for migraine treatment. Expert. Opin. Investig. Drugs 2014, 23, 1141–1148. [Google Scholar] [CrossRef]
- Høivik, H.O.; Laurijssens, B.E.; Harnisch, L.O.; Twomey, C.K.; Dixon, R.M.; Kirkham, A.J.; Williams, P.M.; Wentz, A.L.; Lunnon, M.W. Lack of efficacy of the selective iNOS inhibitor GW274150 in prophylaxis of migraine headache. Cephalalgia 2010, 30, 1458–1467. [Google Scholar] [CrossRef]
- Dao, V.T.; Elbatrik, M.; Fuchß, T.; Grädler, U.; Schmidt, H.; Shah, A.M.; Knowles, R. Nitric Oxide Synthase Inhibitors into the Clinic at Last. In Handbook of Experimental Pharmacology No. 1; Schmidt, H.H.H.W., Ghezzi, P., Cuadrado, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2021; Volume 1, pp. 169–204. [Google Scholar]
- Carrión, M.D.; Rubio-Ruiz, B.; Franco-Montalban, F.; Amoia, P.; Zuccarini, M.C.; De Simone, C.; Camacho, M.E.; Amoroso, R.; Maccallini, C. New amidine-benzenesulfonamides as iNOS inhibitors for the therapy of the triple negative breast cancer. Eur. J. Med. Chem. 2023, 248, 115112. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.F.A.; Marzouk, A.A.; Nafady, A.; El-Gamal, D.A.; Allam, R.M.; Abuo-Rahma, G.E.A.; El Subbagh, H.I.; Moustafa, A.H. Design, synthesis and molecular modeling of novel aryl carboximidamides and 3-aryl-1,2,4-oxadiazoles derived from indomethacin as potent anti-inflammatory iNOS/PGE2 inhibitors. Bioorg. Chem. 2020, 105, 104439. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, T.S.; Moustafa, A.H.; Almalki, A.J.; Allam, R.M.; Althagafi, A.; Md, S.; Mohamed, M.F.A. Novel chalcone/aryl carboximidamide hybrids as potent anti-inflammatory via inhibition of prostaglandin E2 and inducible NO synthase activities: Design, synthesis, molecular docking studies and ADMET prediction. J. Enzyme Inhib. Med. Chem. 2021, 36, 1067–1078. [Google Scholar] [CrossRef] [PubMed]
- Guillon, C.; Vetrano, A.M.; Saxena, J.; Hunter, A.; Verderone, G.; Finetti, T.M.; Wisnoski, J.; DeMatteo, P.W.; Rapp, R.D.; Heindel, N.D.; et al. Derivatives of 1,2,4-triazole imines acting as dual iNOS and tumor cell growth inhibitors. Bioorg. Chem. 2020, 103, 104128. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.H.H.; Mohamed, M.F.A.; Allam, R.M.; Nafady, A.; Mohamed, S.K.; Gouda, A.E.; Beshr, E.A.M. Design, synthesis, and molecular docking of novel pyrazole-chalcone analogs of lonazolac as 5-LOX, iNOS and tubulin polymerization inhibitors with potential anticancer and anti-inflammatory activities. Bioorg. Chem. 2022, 129, 106171. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Cho, D.Y.; Han, J.H.; Choi, D.K.; Kim, E.; Park, J.Y. Synthesis of 1-(5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazol-3-yl)-2-morpholinoethane-1,2-dione analogues and their inhibitory activities with reduced cytotoxicity in lipopolysaccharide-induced BV2 cells. Bioorg. Med. Chem. Lett. 2023, 79, 129061. [Google Scholar] [CrossRef] [PubMed]
- Elkamhawy, A.; Hassan, A.H.E.; Paik, S.; Sup Lee, Y.; Lee, H.H.; Shin, J.S.; Lee, K.T.; Roh, E.J. EGFR inhibitors from cancer to inflammation: Discovery of 4-fluoro-N-(4-(3-(trifluoromethyl)phenoxy)pyrimidin-5-yl)benzamide as a novel anti-inflammatory EGFR inhibitor. Bioorg. Chem. 2019, 86, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.B.; Chen, L.Z.; Wang, B.S.; Huang, X.; Jiao, M.M.; Liu, M.M.; Tang, W.J.; Liu, X.H. Novel Pyrazolo[4,3- d]pyrimidine as Potent and Orally Active Inducible Nitric Oxide Synthase (iNOS) Dimerization Inhibitor with Efficacy in Rheumatoid Arthritis Mouse Model. J. Med. Chem. 2019, 62, 4013–4031. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.Z.; Shu, H.Y.; Wu, J.; Yu, Y.L.; Ma, D.; Huang, X.; Liu, M.M.; Liu, X.H.; Shi, J.B. Discovery and development of novel pyrimidine and pyrazolo/thieno-fused pyrimidine derivatives as potent and orally active inducible nitric oxide synthase dimerization inhibitor with efficacy for arthritis. Eur. J. Med. Chem. 2021, 213, 113174. [Google Scholar] [CrossRef]
- Zhu, L.Q.; Fan, X.H.; Li, J.F.; Chen, J.H.; Liang, Y.; Hu, X.L.; Ma, S.M.; Hao, X.Y.; Shi, T.; Wang, Z. Discovery of a novel inhibitor of nitric oxide production with potential therapeutic effect on acute inflammation. Bioorg. Med. Chem. Lett. 2021, 44, 128106. [Google Scholar] [CrossRef]
- Karbach, S.; Wenzel, P.; Waisman, A.; Munzel, T.; Daiber, A. eNOS uncoupling in cardiovascular diseases--the role of oxidative stress and inflammation. Curr. Pharm. Des. 2014, 20, 3579–3594. [Google Scholar] [CrossRef] [PubMed]
- Kietadisorn, R.; Juni, R.P.; Moens, A.L. Tackling endothelial dysfunction by modulating NOS uncoupling: New insights into its pathogenesis and therapeutic possibilities. Am. J. Physiol. Endocrinol. Metab. 2012, 302, 481–495. [Google Scholar] [CrossRef]
- Shaito, A.; Aramouni, K.; Assaf, R.; Parenti, A.; Orekhov, A.; Yazbi, A.E.; Pintus, G.; Eid, A.H. Oxidative Stress-Induced Endothelial Dysfunction in Cardiovascular Diseases. Front. Biosci. 2022, 27, 105. [Google Scholar] [CrossRef]
- Fraccarollo, D.; Widder, J.D.; Galuppo, P.; Thum, T.; Tsikas, D.; Hoffmann, M.; Ruetten, H.; Ertl, G.; Bauersachs, J. Improvement in left ventricular remodeling by the endothelial nitric oxide synthase enhancer AVE9488 after experimental myocardial infarction. Circulation 2008, 118, 818–827. [Google Scholar] [CrossRef]
- Yang, Q.; Xue, H.M.; Wong, W.T.; Tian, X.Y.; Huang, Y.; Tsui, S.K.; Ng, P.K.; Wohlfart, P.; Li, H.; Xia, N.; et al. AVE3085, an enhancer of endothelial nitric oxide synthase, restores endothelial function and reduces blood pressure in spontaneously hypertensive rats. Br. J. Pharmacol. 2011, 163, 1078–1085. [Google Scholar] [CrossRef]
- Cheang, W.S.; Wong, W.T.; Tian, X.Y.; Yang, Q.; Lee, H.K.; He, G.W.; Yao, X.; Huang, Y. Endothelial nitric oxide synthase enhancer reduces oxidative stress and restores endothelial function in db/db mice. Cardiovasc. Res. 2011, 92, 267–275. [Google Scholar] [CrossRef]
- Heitzer, T.; Brockhoff, C.; Mayer, B.; Warnholtz, A.; Mollnau, H.; Henne, S.; Meinertz, T.; Münzel, T. Tetrahydrobiopterin improves endothelium-dependent vasodilation in chronic smokers: Evidence for a dysfunctional nitric oxide synthase. Circ. Res. 2000, 86, 36–41. [Google Scholar] [CrossRef]
- Daiber, A.; Steven, S.; Weber, A.; Shuvaev, V.V.; Muzykantov, V.R.; Laher, I.; Li, H.; Lamas, S.; Münzel, T. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017, 174, 1591–1619. [Google Scholar] [CrossRef]
- Serreli, G.; Deiana, M. Role of Dietary Polyphenols in the Activity and Expression of Nitric Oxide Synthases: A Review. Antioxidants 2023, 12, 147. [Google Scholar] [CrossRef]
- Song, X.; Tan, L.; Wang, M.; Ren, C.; Guo, C.; Yang, B.; Ren, Y.; Cao, Z.; Li, Y.; Pei, J. Myricetin: A review of the most recent research. Biomed. Pharmacother. 2021, 134, 111017. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.H.; Wang, H.Y.; Xia, Y.T.; Dai, D.K.; Xiong, Q.P.; Dong, T.T.; Duan, R.; Chan, G.K.; Qin, Q.W.; Tsim, K.W. Kaempferol, a Major Flavonoid in Ginkgo Folium, Potentiates Angiogenic Functions in Cultured Endothelial Cells by Binding to Vascular Endothelial Growth Factor. Front. Pharmacol. 2020, 11, 526. [Google Scholar] [CrossRef]
- Li, P.G.; Sun, L.; Han, X.; Ling, S.; Gan, W.T.; Xu, J.W. Quercetin induces rapid eNOS phosphorylation and vasodilation by an Akt-independent and PKA-dependent mechanism. Pharmacology 2012, 89, 220–228. [Google Scholar] [CrossRef]
- Dagher, O.; Mury, P.; Thorin-Trescases, N.; Noly, P.E.; Thorin, E.; Carrier, M. Therapeutic Potential of Quercetin to Alleviate Endothelial Dysfunction in Age-Related Cardiovascular Diseases. Front. Cardiovasc. Med. 2021, 8, 658400. [Google Scholar] [CrossRef]
- Zhang, S.; Hu, X.; Guo, S.; Shi, L.; He, Q.; Zhang, P.; Yu, S.; Zhao, R. Myricetin ameliorated ischemia/reperfusion-induced brain endothelial permeability by improvement of eNOS uncoupling and activation eNOS/NO. J. Pharmacol. Sci. 2019, 140, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Seong, E.H.; Gong, D.S.; Shiwakoti, S.; Adhikari, D.; Kim, H.J.; Oak, M.H. Taxifolin as a Major Bioactive Compound in the Vasorelaxant Effect of Different Pigmented Rice Bran Extracts. Front. Pharmacol. 2022, 13, 799064. [Google Scholar] [CrossRef]
- Xia, N.; Daiber, A.; Habermeier, A.; Closs, E.I.; Thum, T.; Spanier, G.; Lu, Q.; Oelze, M.; Torzewski, M.; Lackner, K.J.; et al. Resveratrol reverses endothelial nitric-oxide synthase uncoupling in apolipoprotein E knockout mice. J. Pharmacol. Exp. Ther. 2010, 335, 149–154. [Google Scholar] [CrossRef]
- Duarte, J.; Francisco, V.; Perez-Vizcaino, F. Modulation of nitric oxide by flavonoids. Food Funct. 2014, 5, 1653–1668. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.C.; Cotta Filho, C.K.; Lacchini, R. The need for further studies examining the role of endothelial nitric oxide synthase polymorphisms in drug response. Pharmacogenomics 2021, 22, 383–387. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maccallini, C.; Budriesi, R.; De Filippis, B.; Amoroso, R. Advancements in the Research of New Modulators of Nitric Oxide Synthases Activity. Int. J. Mol. Sci. 2024, 25, 8486. https://doi.org/10.3390/ijms25158486
Maccallini C, Budriesi R, De Filippis B, Amoroso R. Advancements in the Research of New Modulators of Nitric Oxide Synthases Activity. International Journal of Molecular Sciences. 2024; 25(15):8486. https://doi.org/10.3390/ijms25158486
Chicago/Turabian StyleMaccallini, Cristina, Roberta Budriesi, Barbara De Filippis, and Rosa Amoroso. 2024. "Advancements in the Research of New Modulators of Nitric Oxide Synthases Activity" International Journal of Molecular Sciences 25, no. 15: 8486. https://doi.org/10.3390/ijms25158486







